Abstract
Many adults with Prader-Willi syndrome are affected by behaviors such as tantrums, skin-picking, and compulsions. The nature and extent of these problems suggest more attention be directed to their emergence in childhood. Our purpose was to investigate behavior problems in children with this syndrome and identify the age at which these behaviors emerge. Parents of children with Prader-Willi syndrome, Down syndrome, and those developing typically completed questionnaires. Children with Prader-Willi syndrome exhibited more compulsions, skin-picking, and tantrums than did the other groups. A discriminant analysis of behavior variables derived two statistically significant functions that were interpreted as developmental milestones and problematic behavior. These functions correctly predicted membership for 79% of grouped cases.
Prader-Willi syndrome, a genetic disorder first described by Prader, Labhart, and Willi (1956), is characterized by a severe eating disorder, consisting of hyper-phagia and insatiable appetite, that inevitably leads to obesity if food-seeking is not monitored. In addition, people with this disorder may have mild to moderate mental retardation and behavioral and emotional problems, ranging from temper tantrums and stubbornness to impulsivity and compulsive behavior (see reviews by Butler, 1990; Cassidy, 1997; Dykens et al., 1992; Thompson, Butler, MacLean, & Joseph, 1996). Prader-Willi syndrome occurs in 1 out of 10,000 to 1 out of 25,000 live births (Burd, Vesely, Martsolf, & Kerveshian, 1990; Butler, 1990). For approximately 70% of people with Prader-Willi syndrome, the disorder results from the deletion of a portion of the proximal long arm of chromosome 15, which is paternal in origin (Ledbetter et al., 1980). Another 25% receive two maternally derived chromosome 15 regions. This is known as maternal uniparental disomy (Nicholls, Knoll, Butler, Karam, & Lalande, 1989). Physical traits characteristic of Prader-Willi syndrome include short stature, small hands and feet, and underdeveloped genitalia (Butler & Meaney, 1987; Butler, Meaney, & Palmer, 1986). At birth, infants with Prader-Willi syndrome suffer from hypotonia (floppiness), poor suck reflex, and consequently, failure to thrive. Often, neonates are tube-fed for several months before the onset of the eating disorder occurs (Butler, 1990; Greenswag & Alexander, 1995).
A significant subset of people with Prader-Willi syndrome are affected by behavioral problems, such as temper tantrums, stubbornness, skin-picking, and compulsive behavior (Cassidy, 1984; Dykens et al., 1992; Dykens et al., 1996; Hall & Smith, 1972; Sulzbacher, Crnic, & Snow, 1981; Whitman & Accardo, 1987). Clarke, Boer, Chung, Sturmey, and Webb (1996) compared adults with Prader-Willi syndrome to people with nonspecific learning disabilities who were matched for age, gender, and severity of mental retardation and found that people with Prader-Willi syndrome exhibited more temper tantrums, self-injury, impulsiveness, lability of mood, inactivity, and repetitive speech than did participants in the control group. Stein, Keating, Zar, and Hollander (1994) found that classic compulsive behaviors (e.g., hoarding, arranging and counting, along with frequent temper outbursts) were significantly associated with this syndrome. Hoarding and ordering or arranging of items were also shown by Dykens et al. (1996) to be significant problems for people with the syndrome, and other researchers have identified skin-picking as a significant self-injury problem for this population (Stein et al., 1994; Symons, Butler, Sanders, Feurer, & Thompson, 1999; Whitman & Accardo, 1987). Recently, Symons et al. (1999) found 81% of people with Prader-Willi syndrome surveyed engaged in self-injury, with skin-picking being the predominant form of injury.
Until recently, early diagnosis was not possible, and young children with Prader-Willi syndrome have received little attention, particularly with regard to their behavioral and emotional characteristics. For this reason, behavior problems have been reported mainly in the adult population. Furthermore, the existing research that does include children has not focused on how these problematic behaviors develop and why they persist through adulthood. For example, compulsive behavior has not been studied systematically in younger children with the syndrome, even though some suggest that compulsive-like symptomology develops before adulthood (Dykens et al., 1996; Stein et al., 1994). Although parents have often described very young children with Prader-Willi syndrome as affectionate, friendly, and placid, it has been suggested that in late infancy to the early toddler years there is a marked change in behavior (e.g., Curfs, Verhust, & Fryns, 1991). Behavior problems such as temper tantrums and stubbornness begin to arise in children who were once easy-going and friendly (Beange & Caradus, 1974; Cassidy, 1984). A study by Curfs et al. (1991) of children and adolescents with Prader-Willi syndrome revealed that 81% of the sample had Child Behavior Checklist (Achenbach & Edelbrock, 1983) total behavior problem scores greater than the 90th percentile. Similarly, Dykens, Hodapp, Walsh, and Nash (1992) using the Child Behavior Checklist found the behavior problems most often reported for adolescents and adults with Prader-Willi syndrome included temper tantrums, arguing, irritability, stubbornness, lying, and skin-picking.
The nature and extent of the behavior and emotional problems that exist in adults and adolescents with Prader-Willi syndrome suggests that more attention should be paid to the emergence of these problems in early childhood. In the few studies involving children with Prader-Willi syndrome that appear in the literature, investigators have examined the occurrence of these behaviors within a wide range of ages, sometimes including adults in the sample as well (Stein et al., 1994; Curfs et al., 1991; Curfs, Hoondert, van Lieshout, & Fryns, 1995; Dykens & Kasari, 1997). Moreover, researchers to date have not attempted to examine the temporal emergence of these behaviors. Identifying the emergence of the these behaviors may be critical to understanding the causal mechanisms associated with them. For instance, if behavior problems that are seen in adults with the syndrome also occur in children as young as 2 years of age, that suggests that the mechanisms may be of biological origin. If the onset of the eating disorder occurs at approximately the same time as the onset of certain behavior difficulties, that may indicate one of a number of possible mechanisms may be occurring. These mechanisms may be biologically based (neurochemically triggered by the same mechanism that triggers the eating disorder), environmentally based (driven by the insatiable appetite and need for food), or a possible combination of the two. In addition, because genetic identification of this disorder can now be accomplished soon after birth, it is important to begin to understand what problems associated with Prader-Willi syndrome are evident during childhood. Early identification and treatment may greatly benefit these children. Anecdotal reports (from parents and clinicians) suggest diet restriction at an early age may have lasting effects on obesity and temper outbursts as compared to restrictions later in life. Researchers identifying the emergence of the eating disorder and behavior problems may lead to better diet modification and behavioral management beginning before characteristic features of Prader-Willi syndrome fully emerge.
The purpose of this research was not only to identify the range of behavior problems of preschoolers with Prader-Willi syndrome but also to better understand the emergence and development of these behaviors. The present investigation included one of the larger samples of children with Prader-Willi syndrome that has been collected to date (n = 105). We investigated the development of behavior problems in a sample of children with Prader-Willi syndrome and identified the approximate age at which various types of behavior problems developed. Our study was designed to determine whether compulsive behavior and tantrums exhibited by children with Prader-Willi syndrome differed from those observed in a developmentally delayed comparison group and a typically developing group of children. An additional aim was to identify whether group membership (Prader-Willi syndrome, Down syndrome, and typically developing) could be predicted on the basis of sets of psychological/behavioral predictor variables. The ability to distinguish among three groups with reasonable accuracy on the basis of behaviorally related dimensions would provide further evidence that the nature of Prader-Willi syndrome and the characteristic behaviors that encompass the disorder are specific to that population.
Method
Participants
Prader-Willi syndrome.
The full Prader-Willi syndrome sample included 105 children (48 boys, 57 girls), ranging in age from 2 to 6 years (M = 3.96, standard deviation [SD] = 1.34). Within-group analyses that addressed questions specific to Prader-Willi syndrome included the full sample of children with this syndrome. Seventy-four percent of them were reported to have 15q11-q13 deletion, 15% had maternal disomy, and subtype was not reported in 10%. Eighty-nine percent were Caucasian, 2.9% were African American, 5.7% were of other race, and 2.9% did not report race. Approximately 4% were taking behavior medications at the time of the study.
The between-group analyses included only children between the ages of 2 and 5 (n = 84) in order to preserve between-group comparability on chronological age (CA). The 84 children included in the between-group analyses included 38 boys and 46 girls ranging in age from 2 to 5 years (M = 3.45, SD = .97). Seventy-three percent of these children were reported to have 15q11-q13 deletion; 17% had maternal disomy; and genetic subtype was not reported in 10%. Eighty-seven percent were Caucasian, 3.6% were African American, 6% were of other race, and 3.6% did not report race. Approximately 4% were taking behavior medications at the time of the study. The majority of the 2- to 5-year olds (65.5%) were reported by parents as developing below age expectations according to Early Child Developmental Inventory/Preschool Developmental Inventory (Ireton, 1988a, 1988b).
All children with Prader-Willi syndrome were recruited from the Prader-Willi Syndrome Association (USA) mailing list, referrals from local sources, and parents who attended the national Prader-Willi syndrome meetings (survey return rate: 81%). Children in the Prader-Willi syndrome sample resided in 32 (U.S.) states, Canada, and England.
Down syndrome.
Fifty-six children with Down syndrome (35 males, 21 females) were also included. Children ranged in age from 2 to 5 years (M = 3.05, SD = 1.24). Ninety-four percent of children with Down syndrome were reported to have trisomy 21, and 6% had another form of Down syndrome or were without additional genetic information. All of these participants were Caucasian, and approximately 7% were taking behavior medications at the time of the study. Early Child Developmental Inventory/Preschool Child Developmental Inventory data indicated that 89.3% of children with Down syndrome were developing below age expectations. The proportion of children who scored below the typical developmental cutoff differed for the Prader-Willi syndrome and Down syndrome groups, χ2(1, N = 140) =10.16, p = .001. Children with Down syndrome were recruited from a local database maintained by the Down Syndrome Association of Middle Tennessee (survey return rate: 20%). Although children with Down syndrome fall in a fairly lower range of functioning than do children with Prader-Willi syndrome, because of its homogeneity and high frequency of occurrence, we found this to be the most suitable developmentally delayed comparison group.
Typically developing.
This group included 76 typically developing children (38 males, 38 females), ranging in age from 2 to 5 years (M = 3.25 years, SD = 1.10). Ninety-one percent of the participants were Caucasian, 4% were African American, 1% were of other race, and 4% did not report race. No children with typical development were taking behavior medications at the time of the study. Early Child Developmental Inventory/Preschool Child Developmental Inventory data indicated that all children in this group were functioning at or above age expectations. Parents of children with typical development were recruited from a local ongoing database for child development research maintained by the Department of Psychology and Human Development at Vanderbilt University (survey return rate: 51.2%).
All groups.
For some analyses performed, subject groups were divided into age groups (2 to 3 year olds, 4 to 5 year olds; see Table 1).
Table 1.
Age Groups by Participant Groups
| Age group | CA | |||||
|---|---|---|---|---|---|---|
| 2–3 | 4–5 | 2–3 | 4–5 | |||
| Group | n | n | Mean | SD | Mean | SD |
| Prader Willi syndrome | 45 | 39 | 2.67 | .48 | 4.4 | .49 |
| Down syndrome | 36 | 20 | 2.2 | .40 | 4.6 | .50 |
| Typically developing | 45 | 31 | 2.4 | .50 | 4.4 | .50 |
Procedure
The present research was approved by the Institutional Review Board of Vanderbilt University. The parents of all eligible subjects (via the age criterion) from each mailing list were sent a questionnaire packet that included four questionnaires: a demographic information survey, the Compulsive Behavior Checklist (Gedye, 1992), a tantrum behavior survey, and the Early Child Developmental Inventory or Preschool Child Developmental Inventory (Ireton, 1988a, 1988b). Upon receipt of the return packet, we checked questionnaires for completion, and all computer database data entry was done by a research assistant. If questionnaires were returned incomplete, parents were contacted by telephone within 2 weeks to obtain missing information. The majority of respondents were mothers (94%), 4% were fathers, and 2% of surveys were completed by both parents.
Measures
Demographic information survey.
This survey included questions regarding date of birth, height, weight, genetic status, family history of mental retardation, and medications.
Compulsive Behavior Checklist for clients with mental retardation.
Compulsive characteristics were assessed using this checklist (Gedye, 1992), which includes 25 behaviors that are grouped loosely into five categories. Parents were asked to rate each type of behavior occurring as mild, moderate, severe, or never observed (Stein et al., 1994). The reliability and validity of the instrument have been evaluated in 210 people with intellectual disability (Bodfish et al., 1995). Feurer et al. (1998) demonstrated that 24 of 25 Compulsive Behavior Checklist items should be tallied as a single score and that skin-picking should be scored as a unique item; thus, skin-picking will be treated as a unique item in all analyses.
Tantrum behavior survey.
Tantrum behavior and eating patterns were assessed using a questionnaire measuring specific characteristics of temper tantrums exhibited by the child in relation to food and nonfood events. A 6-point rating scale, ranging from almost always exhibits the behavior (1) to almost never exhibits the behavior (6) was used for this close-ended questionnaire. For those children with Prader-Willi syndrome, questions pertaining to the eating disorder focused on the age at which the appetite increase occurred, the events that surrounded the appetite increase, specific eating patterns, and how the child’s behavior was affected by the eating disorder and food-related situations. Because a suitable measure of tantrum behavior could not be identified in the literature, the questionnaire was specifically designed to assess issues germane to tantrum behavior in people with Prader-Willi syndrome (e.g., food-related tantrums).
Early Child Development Inventory/Preschool Development Inventory.
The child’s achievement of developmental milestones was assessed using both Early Child Developmental Inventory (for 2 year olds) and the Preschool Child Developmental Inventory (for 3 to 5 year olds) (Ireton, 1988a, 1988b). These inventories consist of 60 questions regarding overall development and age-appropriate milestones. The total score (range: 1 to 60) obtained from either the Early Child Developmental Inventory or the Preschool Child Developmental Inventory is used to identify apparently low-functioning children. Children are considered as developing below-age expectations if they obtain total scores that are lower than the average total score for children who are 25% younger (Ireton, 1988a, 1988b).
Results
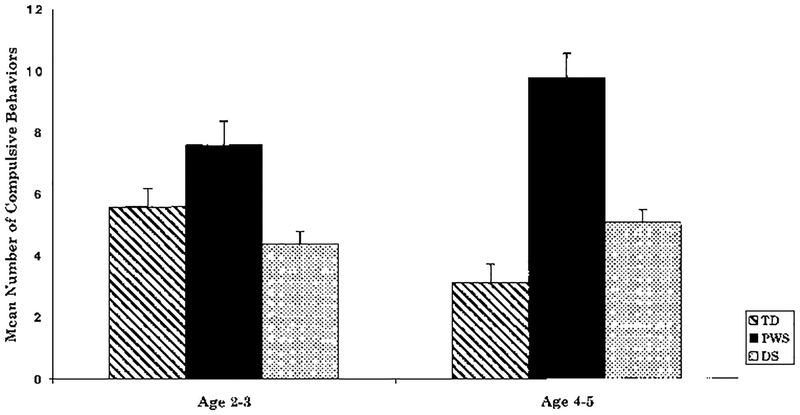
Compulsive Behavior
The number of compulsive behaviors exhibited by the child was assessed for children with Prader-Willi syndrome, Down syndrome, and typically developing children. An analysis of variance was conducted with group and age as independent variables and the number of items endorsed on the Compulsive Behavior Checklist as the dependent variable. The main effect of group (i.e., Prader-Willi syndrome, Down syndrome, and typically developing) regarding number of compulsive behaviors was significant, F(2, 216) = 17.14, p < .001 (see Figure 1). Results indicate a significant interaction effect between age group and subject group for number of compulsive behaviors, F(2, 216) = 4.293, p < .05. A greater number of compulsive behaviors were endorsed in children with Prader-Willi syndrome than in both the Down syndrome and typically developing groups. Post hoc comparisons indicated statistically significant differences between children with Prader-Willi syndrome and Down syndrome for ages 2 to 3, p ≤ .05, and between children with Prader-Willi syndrome and both comparison groups for ages 4 to 5, p <.05. Although older typically developing children exhibited fewer compulsive behaviors than did the younger group, p <.01, there was a trend, p = .13, towards an increase in compulsive behaviors among the children with Prader-Willi syndrome.
Figure 1.
Mean (±SE) number of compulsive behaviors by age group among children with typical development, Prader-Willi syndrome, and Down syndrome. Analysis of variance tests indicated a significant interaction effect, p < .05, between age group and subject group.
To identify patterns of endorsement of specific compulsive behaviors, we performed chi-square analyses for the Prader-Willi syndrome versus Down syndrome group and the Prader-Willi syndrome versus typical development group. More specific compulsive behaviors were manifested by children with Prader-Willi syndrome in comparison with both other groups (see Table 2). In addition, the frequency of skin-picking (Compulsive Behavior Checklist item “picks at face/body to point of gouging skin”) differed significantly between groups, χ2(1, N = 212) = 28.32, p < .01. As expected, skin-picking was prevalent among children with Prader-Willi syndrome and not prevalent in the Down syndrome or typically developing groups. Approximately one third of the sample of children with Prader-Willi syndrome engaged in skin-picking. Although there was no statistically significant effect of age group on skin-picking among these children with Prader-Willi syndrome (ages 2 to 3: 26.7%; ages 4 to 5: 40%), given what we know about the prevalence of skin-picking in the adult Prader-Willi syndrome population, we would expect skin-picking to vary with age across a broader age range. Other behaviors (such as hoarding) that have been identified in adolescents and adults with Prader-Willi syndrome did not appear to differ between age groups in these children.
Table 2.
Percentage of Children Exhibiting Specific Compulsive Behaviors
| Endorsement (%) | |||
|---|---|---|---|
| Item | TD | PWS | DS |
| Repeatedly removes then replaces items | 15.8* | 56.6 | 34.6 |
| Insists on doing chore; resists letting others | 34.2 | 51.8 | 15.4* |
| Arranges objects into certain patterns | 50 | 45.8 | 23.1 |
| Insists on doing activities/chores same time daily | 19.7* | 43.4 | 19.2* |
| Picks at face/body to point of gouging skin | 3.9* | 32.5 | 3.8* |
| Hides away, collects/hoards particular objects | 23.7 | 30.5 | 15.4 |
| Cleans body part(s) excessively | 6.6* | 25.3 | 3.8* |
Note. Scores from the Compulsive Behavior Checklist. TD = typically developing, PWS = Prader Willi syndrome, DS = Down syndrome.
p ≤ .05 after Bonferroni correction (Prader Willi syndrome vs. comparison group).
Tantrums
Within-group analyses (Prader-Willi syndrome only).
The analysis of tantrum onset and eating behavior was performed by correlating the age of eating disorder onset with the age of tantrum onset among the 76 children with Prader-Willi syndrome who had exhibited an appetite increase. Those 17 children (M age = 3.41 years) who had not exhibited the appetite increase were excluded from this analysis, and 12 children were excluded due to missing data. Among children with Prader-Willi syndrome who had exhibited the appetite increase, the age of eating disorder onset (M = 2.40 years), and the age of tantrum onset (M = 2.79 years) were significantly associated, r = .46, p < .01, n = 76. The majority of children with Prader-Willi syndrome (42%) exhibited the eating disorder at approximately 2 years of age; 10%, during their first year; 21%, during their third year; 5%, during their fourth year, and 17.5% had not yet experienced an appetite increase.
Between-group analyses.
Age of tantrum onset differed significantly between the groups (ANOVA), F(2, 216) = 11.164, p < .001. Post hoc comparisons indicated significant differences between each of the delayed groups (Prader-Willi syndrome: M = 2.55 years; Down syndrome: M = 2.37 years) versus the typically developing group (M = 1.99 years). Tantrum characteristics (latency of tantrum onset and conclusion as well as whether or not the child becomes angry in relation to food being withheld) were evaluated between groups using chi-square. Latency was characterized as either rapid or delayed. Analyses revealed a significant difference in latency of tantrum onset between children with Prader-Willi syndrome and children with Down syndrome, χ2(1, N =123) = 8.74, p <.01, and typical development, χ2(1, N = 148) = 14.90, p < .001. Children with Prader-Willi syndrome (89.5%) were reported as having a rapid tantrum onset, whereas 68% of children with Down syndrome and 63% of typically developing children exhibited rapid tantrum onset. Latency of tantrum conclusion did not differ significantly between groups. Groups differed with regard to whether or not children became angry in relation to food being withheld. Chi-square analysis indicated that older children with Prader-Willi syndrome (4 to 5 years of age) differed significantly from both comparison groups on whether they became angry when food was withheld from them (Prader-Willi syndrome vs. Down syndrome: χ2(1, N = 59) = 4.39, p <.05; Prader-Willi syndrome vs. typically developing, χ2(1, N = 70) = 8.92, p <.01). The majority of children with Prader-Willi syndrome (77%) were reported as becoming angry when food was withheld, whereas only 50% of children with Down syndrome and 42% of typically developing children exhibited this behavior.
Discriminant Analysis
A discriminant analysis was conducted in an effort to identify whether the three groups of children could be distinguished on the basis of a collection of behavioral measures. Key variables that independently distinguish children with Prader-Willi syndrome from other groups were used in the analysis. Each variable had a statistically significant Wilks’ lambda at the univariate level: age of tantrum onset, how often child becomes angry about food, Compulsive Behavior Checklist item skin-picking, total score for Early Child Developmental Inventory/Preschool Child Developmental Inventory, and the total score for the remaining 24 Compulsive Behavior Checklist items. Two statistically significant functions were derived from the analysis.
The percentage of variance accounted for by Functions 1 and 2 was 87% and 13%, respectively. The test of Function 1 through 2 was statistically significant, Wilks’ = .285; χ2(10, N = 216) = 221.18, p <.001. The test of Function 2 was also significant, Wilks’ = .790; χ2(4, N = 216) = 41.41, p <.001. Table 3 shows the pooled within-groups correlations between the discriminating variables and the standardized discriminant functions. The total score for the Early Child Developmental Inventory/Preschool Child Developmental Inventory and anger about food was more highly correlated with Function 1, whereas problematic behavior appeared to be more highly correlated with Function 2. Children with Down syndrome generally scored low on both development and problematic behavior. In contrast, children with Prader-Willi syndrome scored higher on development than did children with Down syndrome but generally lower than typical children. Typically developing children appeared to score high on development and low on problematic behavior. As expected, children with Prader-Willi syndrome tended to score higher on problematic behavior than did both other groups. Table 4 shows the predicted group membership for all children: 79% of the grouped cases were correctly classified via the two functions. With cross-validation, overall correct classification decreased slightly to 76.2%.
Table 3.
Functions Derived from the Discriminant Analysis
| Variable | Function 1 | Function 2 |
|---|---|---|
| ECDI/PDIa total score | ||
| How often angers about | ||
| food issues | .82* | −.003 |
| Picks at face/body to point of | .42* | .33 |
| gouging skin | −.17 | .78* |
| CBCb total score | −.15 | .63* |
| Age of first tantrum | −.25 | .28* |
Note. Largest absolute correlation between each variable and any discriminant function.
ECD1 = Early Child Development Inventory/PreSchool Child Developmental Inventory.
Compulsive Behavior Checklist. Total score excludes “picks at face/body to point of gouging skin.”
Table 4.
Group Classification of Children by Group via Discriminant Analysis
| Predicted groupa membership (%) | |||
|---|---|---|---|
| Cases | TD | PWS | DS |
| All cases | |||
| TD | 94.4 | 5.6 | 0 |
| PWS | 15.7 | 68.6 | 15.7 |
| DS | 5.1 | 28.2 | 66.7 |
| Cross-validated | |||
| TD | 94.4 | 5.6 | 0 |
| PWS | 20 | 62.9 | 17.1 |
| DS | 5.1 | 28.2 | 66.7 |
Note. Boldface signifies correct classification of subjects into groups.
TD = typically developing, PWS = Prader-Willi syndrome, DS = Down syndrome.
Discussion
Findings reported here indicate that compulsive behavior emerges among many children with Prader-Willi syndrome within the first 2 years of life and is displayed by half of these children by the time they enter kindergarten. A substantial portion of children with Prader-Willi syndrome engage in skin-picking during this time. Though onset of tantrums is correlated with onset of appetite increase, the causal link between the eating disorder and the behavior problems is not entirely clear. The emergence of tantrums, compulsive behavior, and related behavior problems clearly distinguishes preschoolers with Prader-Willi syndrome from those with Down syndrome and children with typical development, and recent findings point to possible combined peptidergic, neurochemical, and environmental factors as contributors to the Prader-Willi syndrome behavioral phenotype.
Evidence of Compulsive Behavior and Skin-Picking in Prader-Willi Syndrome
Not only do compulsions appear early in life for children with Prader-Willi syndrome, but the extent of the behavior appears to increase with age. Although children with Down syndrome and those with typical development exhibited some compulsive behavior, the extent of such behavior in Prader-Willi syndrome seems to be considerably greater. Further, these compulsions do not appear to be a function of general developmental delay because the children with Down syndrome exhibited compulsiveness more similar to typically developing children than did children with Prader-Willi syndrome, even though the children with Down syndrome exhibited more developmental delay.
Evans et al. (1997) found that typically developing children between the ages of 2 and 4 years engaged in more compulsive-like behavior than did typically developing children older than 4 years. These behaviors included ordering-and-arranging activities and displaying a need for balance and symmetry. Such behavioral rituals are typical during early development, but usually decrease and eventually drop off as the typically developing child ages. Our findings are consistent with this drop in compulsive behavior for children with typical development as they age, which lends support to the hypothesis that children with Prader-Willi syndrome exhibit a different developmental trajectory with regard to compulsive behavior and serves a different role for children with than for those without Prader-Willi syndrome.
It might be expected that compulsive behavior in children with Prader-Willi syndrome would be linked to their eating disorder, but our results indicate that the behaviors exhibited by these children are not limited to food-related compulsions (e.g., ordering and arranging of items and engaging in ritualistic and routine behaviors). In addition, the number of these nonfood-related behaviors appears to increase with age and may well continue into adulthood; similar behaviors have been found among adults with Prader-Willi syndrome (Dykens, Leckman, & Cassidy, 1996; Stein et al., 1994).
In addition to nonfood-related compulsions, 40% of children with Prader-Willi syndrome 4 to 5 years of age engaged in skin-picking and approximately one third of them exhibited skin-picking to the point of drawing blood. Skin-picking is among the most serious behavior and health problems associated with Prader-Willi syndrome because persistent skin-picking can lead to death if left untreated. Previous investigators have reported skin-picking to be a problem for approximately 70% to 80% of adults with Prader-Willi syndrome (Stein et al., 1994; Thornton & Dawson, 1990; Whitman & Accardo, 1987), and findings reported here indicate that this severe feature of Prader-Willi syndrome is evident in children as young as 2 and 3 years of age. Given this, we expect the number of people with Prader-Willi syndrome affected by skin-picking will increase as children age.
Tantrums and the Eating Disorder
The ages of onset of tantrums and the eating disorder were moderately correlated, suggesting that the onsets may be causally linked or may share a common cause. Furthermore, the onset of tantrums was delayed in children with Prader-Willi syndrome and in those with Down syndrome as compared to typically developing children. However, although both delayed groups showed a similar delay in onset of tantrums, more severe tantrum behavior was displayed by older children with Prader-Willi syndrome than by the other groups. These findings together imply that the tantrum behavior exhibited by children with Prader-Willi syndrome may follow a different developmental trajectory than that of typically developing children and those with Down syndrome.
Other analyses of tantrum behavior indicated that more older children with Prader-Willi syndrome (compared to older children in other groups) displayed anger when food was withheld from them. In addition, children with Prader-Willi syndrome 2 to 5 years of age experienced a rapid episodic onset of tantrums more often than did typically developing children and children with Down syndrome.
Because tantrums have been suggested as a means of communication for children with language delays (Bath, 1994; Vollmer, Northup, Ringdahl, Le-Blanc, & Chauvin, 1996), one might expect that delayed language skills in children with Prader-Willi syndrome might lead to frustration and more frequent use of tantrums as a means of communication. However, it is not evident from these results that this late tantrum onset in both groups is merely due to developmental delay. If a language delay were the cause of more frequent tantrums and frustration in children with Prader-Willi syndrome or Down syndrome, an earlier tantrum onset would be expected. In addition, because tantrum behavior is more apparent in children with Prader-Willi syndrome 4 to 5 years of age than in younger children with Prader-Willi syndrome, typical development, or Down syndrome, anxiety and frustration may be more troubling in the older group as the eating disorder becomes more severe.
Group Identification Predicted by Behavior
The two functions that emerged from the discriminant analysis can be distinguished generally on the basis of “developmental milestones” versus “problematic behavior.” Because the tests of both functions were statistically significant, children were not classified solely on the basis of developmental milestones (Function 1). In fact, children with Prader-Willi syndrome were differentiated from the other groups by their higher scores regarding problematic behavior (Function 2). Other investigators who have used discriminant analysis techniques to predict group membership for older children with Prader-Willi syndrome have found similar results (Dykens & Kasari, 1997).
The behavior variables that form problematic behavior (Function 2) were shown to differ between groups at the individual level in addition to distinguishing group membership in this analysis. This further strengthens the argument that there exist behaviors (skin-picking, compulsions, and onset of tantrums) that may be unique to children with Prader-Willi syndrome and that distinguish them as a group from other developmentally delayed populations. In addition, this suggests that these behaviors may very well be related.
Possible Contributors to the Prader-Willi Syndrome Behavioral Phenotype
One possible mechanism contributing to the Prader-Willi syndrome behavioral phenotype is that the onset of the eating disorder (and chronic hunger) increases frustration, causing both food-related and nonfood-related tantrums. Differing schedules of diet and exercise may account for individual differences in children with Prader-Willi syndrome and the moderate correlation. Children who are kept on heavily restricted diets and routine exercise programs may exhibit more frustration and tantrums than those who are not as heavily controlled. In addition, as the child gets older and more signs of the appetite disorder appear, parents may begin to restrict and monitor food access more rigorously, which may further intensify the frustration and anxiety the child feels. Another possibility is that a neurochemically based obsessive-compulsive disorder (OCD) causes both the tantrums and exacerbates or even triggers the intense preoccupation with food, leading to constant food-seeking and eating. The fact that compulsive behaviors emerge as early as 2 years of age and occur in nearly half of children with Prader-Willi syndrome by age 5 strongly suggests that compulsivity may be a biologically driven phenomenon.
Although few studies to date have been focused on identifying the possible mechanisms underlying compulsivity in the Prader-Willi syndrome population, there are some data from adults with Prader-Willi syndrome to consider. One possible link to understanding compulsivity in Prader-Willi syndrome is oxytocin, a neuropeptide synthesized in the hypothalamus. Swaab, Purba, and Hofman (1995) reported a 42% decrease in the number of oxytocin-expressing neurons in the paraventricular nucleus of the hypothalamus in 5 adults with Prader-Willi syndrome compared with 27 control subjects. In addition, Martin et al. (1998) found that oxytocin found in cerebral spinal fluid was elevated in adults with Prader-Willi syndrome as compared with typical control subjects. Oxytocin has also been implicated in compulsivity in autism and OCD (Insel, O’Brien, & Leckman, 1999; Leckman et al., 1994).
Another possible mechanism involves a neurotransmitter receptor defect. Genes regulating expression of proteins involved in three components of the GABA (gamma-aminobutyric acid) receptor are located within the 15q11q13 region. Ebert, Schmidt, Thompson, and Butler (1997) found elevated levels of GABA in plasma of individuals with Prader-Willi syndrome and Angelman syndrome. These elevated levels of GABA may reflect up-regulation of GABA due to improper binding at GABA receptors. It may be possible that the dopaminergic and serotonergic neurons in frontal cortical areas may have less GABAnergic inhibition, which could account for excessive compulsivity among individuals with Prader-Willi syndrome.
Limitations and Conclusions
As is common with all data collected retrospectively, limitations to the findings may be due to the method of data collection. Based on the young age of the participants and the difficulty in recruiting these populations, parental report was found to be the most appropriate method of data collection. In addition, because data were collected by cross-sectional method, developmental inferences must be interpreted with caution. Future researchers should attempt to employ longitudinal studies to further identify the emergence of these behaviors. Although genetic diagnosis was obtained via parental report and subtype was not reported in 10% of children with Prader-Willi syndrome, those children did not differ in key features (e.g., developmental delay, behavior endorsement) from participants whose parents who did report genetic testing. The findings from this study may be interpreted with appropriate caution because nonvalidated instruments were used for several aspects of the study. By choosing frequently used instruments to assess developmental milestones and behavioral features, we attempted to minimize these limitations. Furthermore, mental age differences were not adequately addressed in the present investigation (IQ was not obtained); thus, additional research may be necessary to replicate these findings. Differences between groups may be due to developmental delay in children with Prader-Willi syndrome and Down syndrome. However, results indicate that children with Prader-Willi syndrome exhibited problem behavior more often than either comparison group, which indicates that there is possibly an alternative mechanism specific to Prader-Willi syndrome that accounts for these differences.
Overall, the present study is a beginning in the quest to identify the developmental trajectory of behavior problems in Prader-Willi syndrome. For many children with this syndrome, behavior problems develop as early as 2 years of age but are more evident after age 4. In addition, tantrums, compulsiveness, and skin-picking are evident, particularly after 3 years of age. It is possible that these behavior problems stem from a lack of control associated with restricted food access, frustration, and increased anxiety due to the onset of the eating disorder. However, the mechanism driving the behavior is yet to be identified. Future researchers should focus on identifying what neurochemical, neuroanatomical, and environmental factors contribute to these behaviors.
Acknowledgments
This research was supported in part by United States Public Health Service Grant No. P01HD30329 and by Grant No. T32HD07226 from the National Institute of Child Health and Human Development to Vanderbilt University and by a grant from the Prader-Willi Syndrome Association of America. Requests for reprints should be sent to A. Dimitropoulos, John F. Kennedy Center, Box 156 GPC, Vanderbilt University, Nashville, TN 37203.
Contributor Information
M. G. Butler, Children’s Mercy Hospital (Kansas City, Missouri)
T. Thompson, Vanderbilt University
References
- Achenbach TM, & Edelbrock C (1983). Manual for the Child Behavior Checklist and Revised Behavior Profile. Burlington: University of Vermont, Department of Psychiatry. [Google Scholar]
- Bath HI (1994). Temper tantrums in group care. Child and Youth Care Forum, 23, 5–27. [Google Scholar]
- Beange H, & Caradus V (1974). The Prader-Willi syndrome. Australian Journal of Mental Retardation, 3, 9–11. [Google Scholar]
- Bodfish JW, Crawford TW, Powell SB, Parker DE, Golden RN, & Lewis MH (1995). Compulsions in adults with mental retardation: Prevalence, phenomenology, and comorbidity with stereotypy and self-injury. American Journal on Mental Retardation, 100, 183–192. [PubMed] [Google Scholar]
- Burd L, Vesely B, Martsolf J, & Kerveshian J (1990). Prevalence study of Prader-Willi syndrome in North Dakota. American Journal of Medical Genetics, 37, 97–99. [DOI] [PubMed] [Google Scholar]
- Butler MG (1990). Prader-Willi syndrome: Current understanding of cause and diagnosis. American Journal of Medical Genetics, 35, 319–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, & Meaney FJ (1987). An anthropometric study of 38 individuals with Prader-Labhart-Willi syndrome. American Journal of Medical Genetics, 26, 445–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Butler MG, Meaney FJ, & Palmer CG (1986). Clinical and cytogenetic survey of 39 individuals with Prader-Labhart-Willi syndrome. American Journal of Medical Genetics, 23, 793–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassidy SB (1984). Prader-Willi syndrome. Current Problems in Pediatrics, 14(1), 1–55. [DOI] [PubMed] [Google Scholar]
- Cassidy SB, (1997). Prader-Willi syndrome. Journal of Medical Genetics, 34, 917–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke DJ, & Boer H (1995). Genetic and behavioural aspects of Prader-Willi syndrome: A review with a translation of the original paper. Mental Handicap Research, 8, 38–53. [Google Scholar]
- Clarke DJ, Boer H, Chung MC, Sturmey P, & Webb T (1996). Maladaptive behaviour in Prader-Willi syndrome in adult life. Journal of Intellectual Disability Research, 40, 159–165. [DOI] [PubMed] [Google Scholar]
- Curfs LMG, Verhust FC, & Fryns JP (1991). Behavioral and emotional problems in youngsters with Prader-Willi syndrome. Genetic Counseling, 2, 33–41. [PubMed] [Google Scholar]
- Curfs LMG, Hoondert V, van Lieshout CFM, & Fryns JP (1995). Personality profiles of youngsters with Prader-Willi syndrome and youngsters attending regular schools. Journal of Intellectual Disability Research, 39, 241–248. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Hodapp RM, Walsh K, & Nash L (1992). Adaptive and maladaptive behavior in Prader-Willi syndrome. Journal of the American Academy of Child and Adolescent Psychiatry, 31, 1131–1136. [DOI] [PubMed] [Google Scholar]
- Dykens EM, & Cassidy SB (1995). Correlates of maladaptive behavior in children and adults with Prader-Willi syndrome. American Journal of Medical Genetics, 60, 546–549. [DOI] [PubMed] [Google Scholar]
- Dykens EM, Leckman JF, & Cassidy SB (1996). Obsessions and compulsions in Prader-Willi syndrome. Journal of Child Psychology and Psychiatry, 37, 995–1002. [DOI] [PubMed] [Google Scholar]
- Ebert MH, Schmidt DE, Thompson T, & Butler MG (1997). Elevated plasma Gamma-Aminobutyric Acid (GABA) levels in individuals with either Prader-Willi syndrome or Angelman syndrome. Journal of Neuropsychiatry and Clinical Neurosciences, 9, 75–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans DW, Leckman JF, Carter AJ, Resnick S, Henshaw D, King RA, & Pauls D (1997). Ritual, habit, and perfectionism: The prevalence and development of compulsive-like behavior in normal young children. Child Development, 68, 58–68. [PubMed] [Google Scholar]
- Feurer ID, Dimitropoulos A, Stone WL, Roof E, Butler M, & Thompson T (1998). The latent variable structure of the Compulsive Behaviour Checklist in people with Prader-Willi syndrome. Journal of Intellectual Disability Research, 42, 472–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gedye A (1992). Compulsive Behavior Checklist for Clients With Mental Retardation. Habilitative Mental Healthcare Newsletter, 11, 73–77. [Google Scholar]
- Greenswag LR, & Alexander RC (1995). Management of Prader-Willi syndrome. New York: Springer-Verlag. [Google Scholar]
- Hall BD, & Smith DW (1972). Prader-Willi syndrome. Journal of Pediatrics, 81, 286–293. [DOI] [PubMed] [Google Scholar]
- Insel TR, O’Brien DJ, & Leckman JF (1999). Oxytocin, vasopressin and autism: Is there a connection? Biological Psychiatry, 454, 145–157. [DOI] [PubMed] [Google Scholar]
- Ireton H (1988a). Early Child Development Inventory manual. Minneapolis: Behavior Science Systems. [Google Scholar]
- Ireton H (1988b). Preschool Development Inventory manual. Minneapolis: Behavior Science Systems. [Google Scholar]
- Leckman JF, Goodman WK, North WG, Chappel PB, Price LH, Pauls DL, Anderson GM, Riddle MA, McDougle CJ, Barr LC, & Cohen DJ (1994). The role of central oxytocin in obsessive compulsive disorder and related normal behavior. Psychoneuroendocrinology, 19, 723–749. [DOI] [PubMed] [Google Scholar]
- Ledbetter DH, Riccardi VM, Youngbloom SA, Strobel RJ, Keenan BS, Crawford JD, & Louro JM (1980). Deletion (15q) as a cause of the PWS (Prader-Willi syndrome). American Journal of Human Genetics, 32, 77A. [Google Scholar]
- Martin A, State M, Anderson GM, Kaye WM, Hanchett JM, McConahay CW, North WG, & Leckman JF (1998). Cerebrospinal fluid levels of oxytocin in Prader-Willi syndrome: A preliminary report. Biological Psychiatry, 44, 1349–1352. [DOI] [PubMed] [Google Scholar]
- Nicholls RD, Knoll JHM, Butler MG, Karam S, & Lalande M (1989). Genetic imprinting suggested by maternal heterodisomy in non-deletion Prader-Willi syndrome. Nature, 342, 281–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prader A, Labhart A, & Willi H (1956). Ein Syndrome von Adipositas, Kleinwuchs, Kryptochismus und Oligophrenie nach myatonieartigem Zustand in Neugeborenenalter. Schweizerische Medizinische Wochenschrift, 86, 1260–1261. [Google Scholar]
- Stein DJ, Keating J, Zar HJ, & Hollander E (1994). A survey of the phenomenology and pharmacotherapy of compulsive and impulsive-aggressive symptoms in Prader-Willi syndrome. Journal of Neuropsychiatry and Clinical Neurosciences, 6, 23–29. [DOI] [PubMed] [Google Scholar]
- Sulzbacher S, Crnic KA, & Snow J (1981). Behavioral and cognitive disabilities in Prader-Willi syndrome In Holm VA, Sulzbacher S, & Pipes P (Eds.), Prader-Willi syndrome (pp. 147–160). Baltimore: University Park Press. [Google Scholar]
- Swaab DF, Purba JS, & Hofman MA (1995). Alterations in the hypothalamic paraventricular nucleus and its oxytocin neurons (putative satiety cells) in Prader-Willi syndrome: A study of five cases. Journal of Clinical Endocrinology and Metabolism, 80, 573–579. [DOI] [PubMed] [Google Scholar]
- Symons FJ, Butler MG, Sanders MD, Feurer ID, & Thompson T (1999). Self-injurious behavior and Prader-Willi syndrome: Behavioral forms and body locations. American Journal on Mental Retardation, 104, 260–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson T, Butler MG, MacLean WE, & Joseph B (1996). Prader-Willi syndrome: Genetics and behavior. Peabody Journal of Education, 71, 187–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornton L, & Dawson KP (1990). Prader-Willi syndrome in New Zealand: A survey of 36 affected people. New Zealand Medical Journal, 103, 97–98. [PubMed] [Google Scholar]
- Vollmer TR, Northup JR, Ringdahl JE, LeBlanc LA, & Chauvin TM (1996). Functional analysis of severe tantrums displayed by children with language delays: An outclinic assessment. Behavior Modification, 20, 97–115. [Google Scholar]
- Whitman B, & Accardo P (1987). Emotional symptoms in Prader-Willi syndrome adolescents. American Journal of Medical Genetics, 28, 897–905. [DOI] [PubMed] [Google Scholar]