Abstract
Background:
Multiple factors increase the risk for spinal surgical site infection (SSI): prior SSI, obesity, diabetes mellitus, advanced age, American Society of Anesthesiologists class, alcohol abuse, low prealbumin levels, smoking, history of cancer, chronic steroids, immunosuppressive drugs, rheumatoid arthritis, and hypothyroidism.
Methods:
Here, we performed a retrospective medical record review at one facility involving 5065 patients from 2010 to 2015. In 2011, there was an increase in the infection rate (1.07%) which prompted this analysis, resulting in the subsequent introduction of a protocol to reduce the infection risk.
Results:
The overall infection rate in this series was 0.59%. The lowest infection rate was 0.00% for anterior cervical discectomy and fusion. The highest rate of infections occurred among patients undergoing posterior cervical fusions, lumbar fusions, and tumor resections. Higher infection rates were also correlated with diabetes mellitus, obesity, and increased surgical time.
Conclusions:
Since 2011, we instituted a protocol to limit the risks of spinal SSIs, particularly for patients exhibiting increased medical comorbidities.
Keywords: Infection, Risk factors, Spine surgery, Surgical site infection

INTRODUCTION
Postoperative infection in spine surgery occurs from <1% to as high as 12% of the time.[1] The mean direct hospital cost of a single readmission for a postoperative spine surgical site infection (SSI) had been reported as high as $ 16,242.[2]
In 2011, we noted an increase in SSI at our institution. These SSI correlated with the following predisposing risk factors/comorbidities: obesity, diabetes mellitus, advanced age, higher American Society of Anesthesiologists (ASA) class, alcohol abuse, low prealbumin levels and malnutrition status, smoking, history of cancer, chronic steroid use, rheumatoid arthritis, and hypothyroidism. Here, we reviewed our findings and the protocol we introduced to avoid SSI in 2011 along with a review of literature.
METHODS
We performed a retrospective medical record review of SSI from 2010 to 2015 with the institutional review board approval. The multiple risk factors and comorbidities studied included diabetes, obesity, smoking, age, and ASA. In 2012, we implemented new additional preoperative and perioperative measures to reduce SSI infection risk.
Preoperative counseling and measures
Preoperatively, as appropriate, patients were advised regarding; weight loss, smoking cessation, and discontinuation of immunosuppressant medications. Those with inadequate prealbumin levels received high protein supplements.[5] For those with a history of diabetes about to undergo spinal surgery,[4] hemoglobin A1C levels had to be below 7.5 for those without additional risk factors and below 7.0 for those with additional SSI risk factors.
Skin prep protocol
Three days before surgery, patients were advised to perform local washing of the operative site with Hibiclens. For high- risk patients, a three-step regimen was initiated that included; first isopropyl alcohol, next Betadine, and finally Hibiclens. In the preoperative holding area, the patients’ surgical site was wiped with chlorhexidine gluconate.
Preoperative antibiotic protocol
Cefazolin was used as a first-line antibiotic; we utilized a standard dose of 2 g. However, patients over 80 kg received 3 g. The second-line antibiotic was vancomycin dosed at 1 g; patients over 90 kg received 1.5 g. The antibiotic chosen was redosed when the length of the operative procedure exceeded 4 h. Intravenous antibiotics were continued for 24–48 h postoperatively, dependent on the drain status. In high-risk patients, 5 days of additional oral antibiotics were given at discharge.
Intraoperative irrigation
In high-risk patients, the surgical wound was irrigated with 3 l of saline with antibiotics before skin closure. In addition, in 2014, vancomycin powder was introduced and placed topically in the operative bed.
Silver dressing
In high-risk patients, silver nitrate impregnated dressings were utilized over wounds with staples or sutures. The operative dressing was maintained for 3 days in most cases, followed by daily dry dressing changes and a Betadine cleanse of staples when present. The wound was kept dry and covered for 1 week.
Foley catheter
The Foley catheter was discontinued on postoperative day 1, unless longer placement was indicated.
Glucose monitoring
In diabetic patients, glucose levels were monitored closely intraoperatively, and postoperatively; they were treated appropriately.
Immunosuppressant medications
These medications were routinely discontinued 2 weeks before surgery and resumed at the first 2 weeks postoperative visit.
RESULTS AND DISCUSSION
The population comprised a total of 5065 spine cases performed by one service in the same facility. A total of 30 (0.59%) infections were documented utilizing positive wound cultures taken during operative wound revisions. The peak rate was seen in 2011, with 11 (1.07%) SSIs out 1031 cases performed that year.
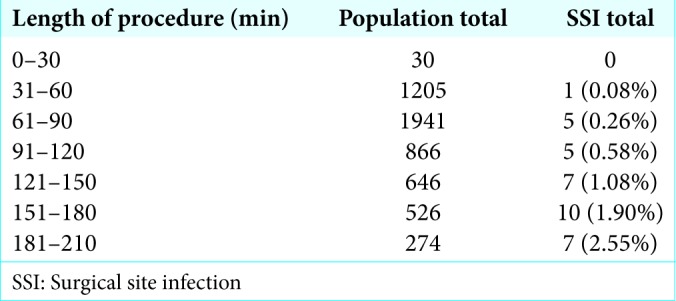
In general, longer procedures were associated with an increased risk of SSI.[6] Notably, of 1684 of 5065 cases (33.2%) lasting 61–90 min, the infection rate was 0.26%. However, with 526 (10.4%) procedures lasting 151–180 min, the infection rate increased to 1.9% and constituted 33.3% (10 of 30) of the total infections in that sample [Table 1].
Table 1:
Procedure length in the population and SSI group.
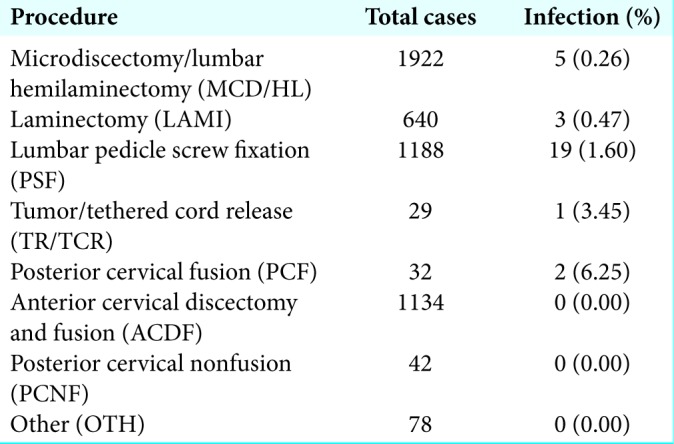
The 5065 cases were divided into eight categories [Table 2]. The peak rate of infection was seen in the posterior cervical fusion category (e.g., 2 [6.25%] SSIs in 32 procedures). Tumors yielded the next highest rate of infection (3.45%). This was followed by 19 (1.60%) infections of 1188 lumbar fusion procedures. Notably, lumbar fusions exhibited the highest risk of infection among other spine surgeries due to the length of the procedure, the higher frequency of revision surgery, age >60, and additional risk factors. The lowest rate of infection was seen for anterior cervical discectomy and fusion, posterior cervical nonfusion cases, and other categories (e.g., [0%] of 1254 cases). The rate of SSI in revision surgery was 8 (1.03%) of 775.
Table 2:
A numerical representation of the infection rate for each category of surgical procedure performed over the period of 2010-2015 in this single surgeon practice.
We were not able to identify a correlation between the risk of infection and the ASA classification score.
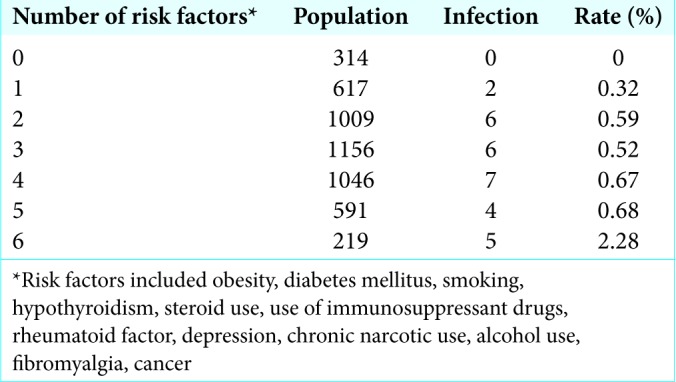
With the initiation of the current protocol, since 2011, over the next 6 years, despite a gradual increase in the medical complexity/comorbidities of the patient population, there were no further increases in the SSI rates [Tables 3 and 4].
Table 3:
Rate of surgical site infection based on risk factor.
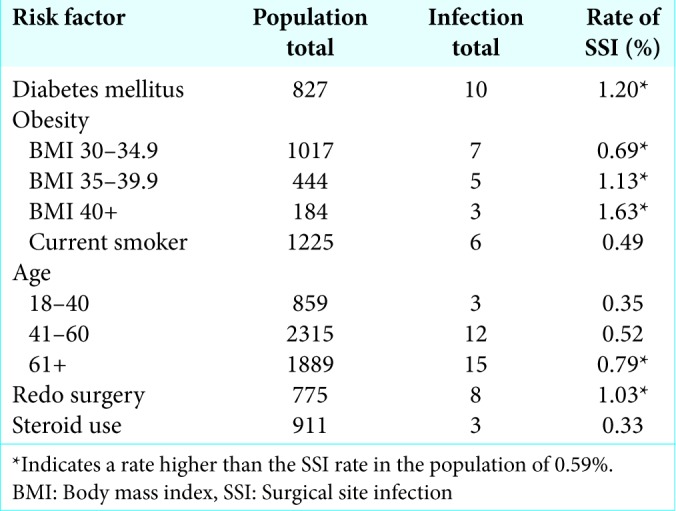
Table 4:
Number of risk factors.
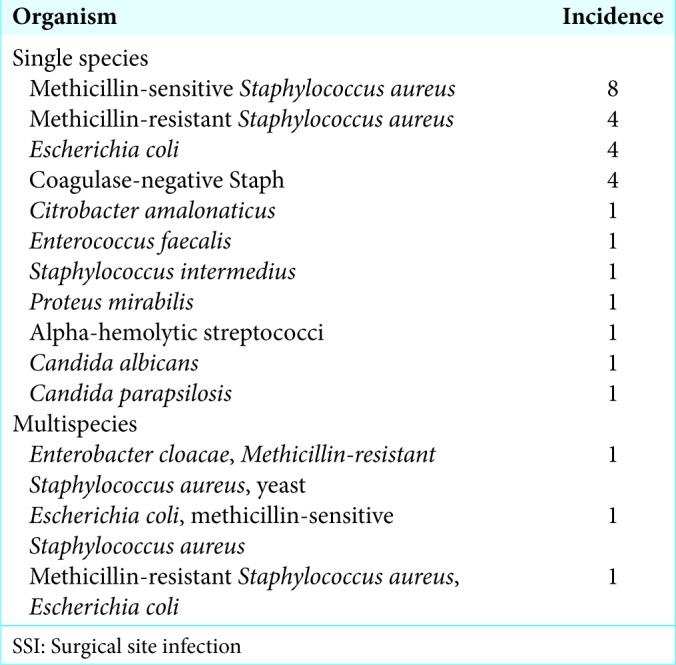
Organisms involved in infection
In literature, Staphylococcus aureus is the principal agent cited in SSI following spine surgery.[3] Other agents commonly identified include coagulase-negative staphylococci, Staphylococcus epidermidis, beta-hemolytic Streptococcus, and Gram-negative organisms such as Proteus, Pseudomonas aeruginosa, Escherichia coli, Klebsiella, and Enterobacter [Table 5].[3]
Table 5:
Organisms isolated during intraoperative cultures in the SSI group.
CONCLUSIONS
SSIs increase the costs of spinal surgery, resulting in readmissions and/or increased length of hospital stay. Obesity and diabetes independently contributed to higher SSI rates. Our data showed that multiple risk factors may quadruple the expected SSI rate. However, the introduction of a new infection prevention protocol in 2011 kept the infection rate as low as 0.59%, regardless of the case complexity, attendant comorbidities, and increased case mix index over the ensuing 6 years.
Contributor Information
Matt El-Kadi, Email: elkadim@upmc.edu.
Erin Donovan, Email: donovanec@upmc.edu.
Laurel Kerr, Email: sinkolk@upmc.edu.
Coby Cunningham, Email: cobycunningham5@gmail.com.
Victor Osio, Email: osiovictor1@gmail.com.
Samah Abdallah, Email: samahabdallah467@gmail.com.
Joseph Kazan, Email: jfk05@mail.aub.edu.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Beiner JM, Grauer J, Kwon B, Vaccaro AR. Postoperative wound infections of the spine. Neurosurg Focus. 2003;15:1–5. doi: 10.3171/foc.2003.15.3.14. [DOI] [PubMed] [Google Scholar]
- 2.Blumberg T, Woelber E, Bellabarba C, Bransford R, Spina N. Predictors of increased cost and length of stay in the treatment of postoperative spine surgical site infection. Spine J. 2017;18:300–6. doi: 10.1016/j.spinee.2017.07.173. [DOI] [PubMed] [Google Scholar]
- 3.Chahoud J, Kanafani Z, Kanj SS. Surgical site infections following spine surgery: Elmininating the controversies in the diagnosis. Front Med. 2014;1:1–10. doi: 10.3389/fmed.2014.00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein NE. Predominantly negative impact of diabetes on spinal surgery: A review and recommendation for better preoperative screening. Surg Neurol Int. 2017;8:107. doi: 10.4103/sni.sni_101_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guan J, Holland CM, Schmidt MH, Dailey AT, Mahan MA, Bisson EF. Association of low perioperative prealbumin level and surgical complications in long-segment spinal fusion patients: A retrospective cohort study. Int J Surg. 2017;39:135–40. doi: 10.1016/j.ijsu.2017.01.082. [DOI] [PubMed] [Google Scholar]
- 6.Veeravagu A, Patil CG, Lad SP, Boakye M. Risk factors for postoperative spinal wound infections after spinal decompression and fusion surgeries. Spine. 2009;34:1869–72. doi: 10.1097/BRS.0b013e3181adc989. [DOI] [PubMed] [Google Scholar]


