Abstract
Background:
Cavernomas arising in the region of the optic apparatus are extremely rare, accounting for <1% of all the central nervous system cavernomas. Most patients are affected by acute visual disturbances related to hemorrhagic events. A prompt resection of the lesion together with a decompression of the optic apparatus may lead to a functional improvement. Almost all patients reported in literature were treated by means of a craniotomy, whereas only few papers described the use of a transnasal approach.
Case Description:
We report the case of a 53-year-old woman with a hemorrhagic, cavernous malformation of the optic chiasm region and we discuss the technical nuances of the endoscopic transnasal approach we employed. We also review literature for patients with cavernomas treated with a transsphenoidal approach. In our case, the patient underwent the gross-total resection of the lesion through a fully endoscopic transnasal route and the visual disturbances improved immediately after the operation. The ventral access allowed an adequate exposure of the chiasm/anterior circulation complex, thus avoiding an excessive dissection and retraction of neurovascular structures. Moreover, with the aid of angled scopes, we were able to identify the frail vascular supply of the chiasm by employing the suprachiasmatic corridor as well as the infrachiasmatic one. We stress the need for a careful reconstruction of the skull base to avoid a postoperative cerebrospinal fluid leak.
Conclusions:
With the evolution and spreading of the neuroendoscopic techniques, in selected cases, we advocate the use of the transnasal route for the removal of cavernomas arising in the region of the anterior optic pathways.
Keywords: Anterior optic pathways, cavernoma, endoscopic transnasal approach

INTRODUCTION
Cavernous malformations (CMs) are developmental vascular abnormalities consisting of sinusoid-like capillary vessels with very slow circulation which could arise throughout the whole nervous system. The walls of the cavernous vessels are fragile and these lesions usually become clinically evident during hemorrhagic events.[3] They account approximately for 5–15% of all vascular abnormalities in the central nervous system, with an estimated incidence of 0.15–0.56/100,000 persons per year[6] with a slight predominance for the female gender. Intracranially, these lesions could arise supratentorially (80%) and infratentorially (15–20%). In <1%, CMs could also arise in the context of the sovrasellar region located in the cranial nerves, usually the optic one in its chiasm, the third, the seventh, and the eighth ones.[10] In particular, the CMs arising from either the optic nerve, chiasm, optic tract, or hypothalamus are called optic pathways and hypothalamus CM (OPH CMs). OPH CMs usually become clinically significant due to hemorrhagic events, the so-called “chiasmal apoplexies.” As described by Liu et al.,[10] chiasmal apoplexy usually results in visual acuity impairment, visual field deficit, or both (98%), and headache and/or retro-orbital pain (60%): in 73% of the cases, the onset is acute or subacute, whereas 26% of the cases have a progressive course. Prior episodes of headache and visual loss are reported in half of the cases. Consciousness and endocrine disturbances are rare and are associated only with a large amount of bleeding and compression of the infundibulum. In case of hemorrhagic events, a prompt resection and decompression of the optic apparatus are needed to ensure the best potential functional recovery and to prevent rebleeding.[16] In the past few years, both the accesses, the exploration and the working possibilities in the sellar and parasellar areas became easier with the evolution and the spreading of the neuroendoscopic techniques. However, only three papers to date[2,11,17] reported a suprasellar decompression by a ventral endoscopic approach. We report our experience dealing with the decompression of the optic structures through an endoscopic, endonasal, transsphenoidal approach in a case of acute hemorrhage caused by a cavernous angioma.
CASE REPORT
A 53-year-old woman was admitted to our institution complaining of a mild fever, severe headache, and progressive visual loss that had started 4 days before. On admission, the general condition of the patient and the results of the gross neurological examination were unremarkable. Goldmann perimetry testing showed bitemporal hemianopsia. Her visual acuity was 20/400 in the right and 20/200 in the left eye. A computed tomography scan showed a hyperdense, hemorrhagic mass measuring approximately 2.5 cm in diameter in the suprasellar region [Figure 1]. A magnetic resonance (MR) imaging scan [Figure 2 and 3] better outlined the mass: it affected both the pituitary stalk and the hypothalamus while reaching cranially the left Monro foramen and compressing the optic nerves and chiasm, a clear signal of an ongoing edema. Cerebral angiography showed no vascular malformation. The results of routine blood and serum examinations were normal. Endocrinological studies of the pituitary function were unremarkable. After 3 days, the patient underwent a gross-total resection of the lesion through an extended endoscopic, endonasal, transsphenoidal route. The resection of the lesion was combined with the opening of the third ventricle through the lamina terminalis. A careful reconstruction of the skull base was performed, with abdominal fat, nasal septal flap, and fibrin glue. After the operation, the visual symptoms improved immediately. On discharge, visual acuity was 20/50 in the right eye and 20/20 in the left eye. The patient had a transient incomplete hypopituitarism and mild diplopia which improved after few weeks. After 1 month, the neurological examination was unremarkable. Postoperative MR scan is showed in Figure 4 and 5. Histological findings confirmed the presence of a CM, showing hemosiderin, reactive fibrohistiocytic, ectatic vascular channels, and dilated cavernous spaces. On immunohistochemistry, the lesion was positive for CD34 staining, marker for endothelial lining, and was negative for elastin staining, thus ruling out an arteriovenous malformation. See video 1 showing the main steps of the endoscopic surgery.
Figure 1:

Preoperative axial head computed tomography scan.
Figure 2:
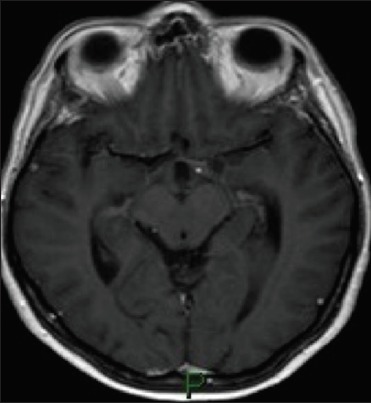
Preoperative axial head magnetic resonance T2 scan.
Figure 3:
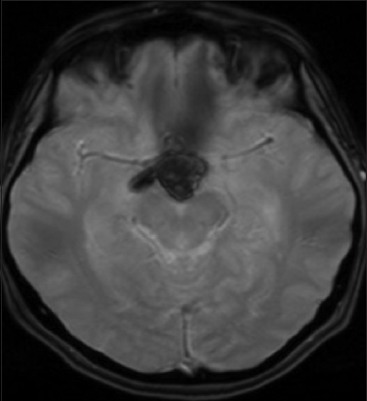
Preoperative axial head magnetic resonance FLAIR scan.
Figure 4:
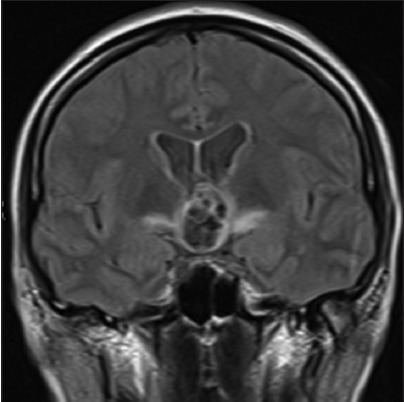
Postoperative coronal head magnetic resonance T1 scan.
Figure 5:
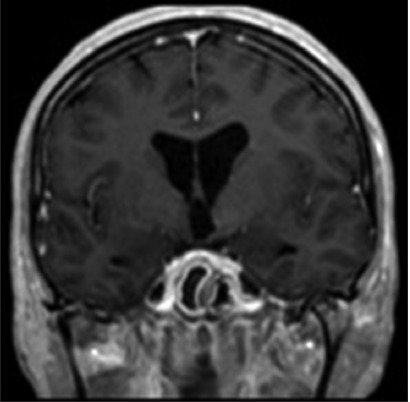
Postoperative coronal head magnetic resonance T1 scan after constrast enhancement.
Methods
The PubMed search engine (www.pubmed.gov) was used to perform an internet Medline literature research based on the following keywords “chiasma,” “optic,” “sovrasellar,” “CM,” “endoscopic,” and “transsphenoidal” with different combination. There were no limitations as to the timeframe, language, and publication type on the search process. We also cross-checked the references of the articles retrieved by looking for further papers of potential interest.
DISCUSSION
In literature, the first relevant article about OPH CMs was published in 1978. To date, there are approximately 70 cases of histologically confirmed OPH CM. Still, only three papers[2,11,17] reported the cases of OPH CM treated by means of an endoscopic endonasal, transsphenoidal approach. Natural history of OPH CM is not clear partly because most reported cases have been surgically treated and partly because there is a small amount of data. The overall bleed rate for all types of intracranial CMs ranges from 0.7% to 3.1% per year[14] and prior hemorrhage is a known risk factor for subsequent bleeding (from 3.8% to 22.9%).[1,8] The hemorrhage and rehemorrhage rates of OPH CMs are not well-defined in large case series, even if some authors report them to be higher than those for cerebral lesions.[9,12] As seen for the brainstem CMs, the reported higher rebleed rates of OPH CMs may be partially explained by the eloquent nature of the optic apparatus, i.e. likely to develop a clinically detachable neurological deficit even with a small bleeding. A literature review by Liu et al.[10] showed a significative improvement of visual disturbances in both gross-total resection and biopsy plus decompression (85% and 77%, respectively). Even if the decompression without complete resection of the optic apparatus has resulted in visual improvement, the risk of rebleed and future visual deteriorations may not be ruled out. Given the high rebleed rate of OPH CMs, in accordance with other authors, we believe that the gross-total resection should be the gold standard treatment.[4,7,9,12,13,15] There are three papers reporting the use of an endoscopic endonasal transsphenoidal approach: the first one[17] showed gross-total resection reporting only a transient postoperative worsening of the left temporal field defect, whereas the second one[11] reported a gross-total resection and no postoperative deficit. The third paper[2] instead presented a case of a large CM that extended into the sella and the sovrasellar region without signs of bleeding. Still, the patient was operated on for neurological deterioration from direct tissue compression (decreased visual acuity in the left eye, bitemporal homonymous hemianopsia, and 6th nerve palsy). The authors performed an endoscopic, endonasal, transsphenoidal route with a subtotal resection. The residual cavernous angioma was managed by stereotactic radiosurgery with good clinical and radiological results. In our case, we performed a gross-total resection through a fully endoscopic endonasal, transsphenoidal approach with a sovrachiasmatic extension to open the third ventricle and avoid possible compressive hydrocephalus in case of further rebleeding. The ventral access and the magnification of the endoscope enabled an adequate dissection of the chiasm from the anterior circulation complex, thus avoiding an excessive retraction of the nervous and vascular structures. With the aid of angled scopes, we were able to fully identify chiasmatic structures not only by employing the suprachiasmatic corridor but also by reaching it from an infrachiasmatic route. In our opinion, this is a non-negligible advantage in dealing with the delicate vascular supply of the optic chiasm. Almost all cases of OPH CMs in literature were treated by means of a craniotomy through an anterolateral or midline approach. The endoscopic transsphenoidal route has become the gold standard for many sellar and sovrasellar pathologies: the ventral access, the magnification, and the angled scopes extend exploration and dissection possibilities. For these reason, the development of endoscopic surgery increased the successfully resected numbers of suprasellar tumors, despite the satisfactory results of craniotomy for the treatment of suprasellar lesions.[5]
CONCLUSIONS
Symptomatic OPH CMs are extremely rare and both early decompression and complete resection are indicated to improve the visual dysfunction in cases of hemorrhage. The endoscopic endonasal, transsphenoidal route may be a valid choice to decompress and remove selected lesions. Further studies about the natural history of these specific lesions are needed to evaluate the role of surgery in cases of asymptomatic OPH CMs.
Contributor Information
Cesare Zoia, Email: gioiaoffice@gmail.com.
Daniele Bongetta, Email: danielebongetta@hotmail.com.
Gianluigi Dorelli, Email: gianluigi.dorelli@gmail.com.
Sabino Luzzi, Email: sabino.luzzi@unipv.it.
Mattia Del Maestro, Email: mattiadelmaestro@gmail.com.
Renato J. Galzio, Email: r.galzio@smatteo.pv.it.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos available on:
REFERENCES
- 1.Aiba T, Tanaka R, Koike T, Kameyama S, Takeda N, Komata T. Natural history of intracranial cavernous malformations. J Neurosurg. 1995;83:56–9. doi: 10.3171/jns.1995.83.1.0056. [DOI] [PubMed] [Google Scholar]
- 2.Al-Sharydah AM, Al-Suhibani SS, Al-Jubran SA, Al-Abdulwahhab AH, Al-Bar M, Al-Jehani HM, et al. Endoscopic management of atypical sellar cavernous hemangioma: A case report and review of the literature. Int J Surg Case Rep. 2018;42:161–4. doi: 10.1016/j.ijscr.2017.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Curling OD, Kelly DL, Elster AD, Craven TE. An analysis of the natural history of cavernous angiomas. J Neurosurg. 1991;75:702–8. doi: 10.3171/jns.1991.75.5.0702. [DOI] [PubMed] [Google Scholar]
- 4.Deshmukh VR, Albuquerque FC, Zabramski JM, Spetzler RF. Surgical management of cavernous malformations involving the cranial nerves. Neurosurgery. 2003;53:352–7. doi: 10.1227/01.neu.0000073531.84342.c2. [DOI] [PubMed] [Google Scholar]
- 5.Divitiis ED, Cavallo LM, Cappabianca P, Esposito F. Extended endoscopic endonasal transsphenoidale approach for the removal of suprasellar tumors. Neurosurgery. 2007;60:46–59. doi: 10.1227/01.NEU.0000249211.89096.25. [DOI] [PubMed] [Google Scholar]
- 6.Goldstein HE, Solomon RA. Epidemiology of cavernous malformations. Handb Clin Neurol. 2017;143:241–7. doi: 10.1016/B978-0-444-63640-9.00023-0. [DOI] [PubMed] [Google Scholar]
- 7.Hempelmann RG, Mater E, Schröder F, Schön R. Complete resection of a cavernous haemangioma of the optic nerve, the chiasm, and the optic tract. Acta Neurochir. 2007;149:699–703. doi: 10.1007/s00701-007-1163-8. [DOI] [PubMed] [Google Scholar]
- 8.Kim DS, Park YG, Choi JU, Chung SS, Lee KC. An analysis of the natural history of cavernous malformations. Surg Neurol. 1997;48:9–17. doi: 10.1016/s0090-3019(96)00425-9. [DOI] [PubMed] [Google Scholar]
- 9.Lehner M, Fellner FA, Wurm G. Cavernous haemangiomas of the anterior visual pathways. Short review on occasion of an exceptional case. Acta Neurochir. 2006;148:571–8. doi: 10.1007/s00701-006-0751-3. [DOI] [PubMed] [Google Scholar]
- 10.Liu JK, Lu Y, Raslan AM, Gultekin SH, Delashaw JB. Cavernous malformations of the optic pathway and hypothalamus: Analysis of 65 cases in the literature. Neurosurg Focus. 2010;29:E17. doi: 10.3171/2010.5.FOCUS10129. [DOI] [PubMed] [Google Scholar]
- 11.Meng X, Feng X, Wan J. Endoscopic endonasal transsphenoidal approach for the removal of optochiasmatic cavernoma: Case report and literature review. World Neurosurg. 2017;106:1053.e11–1053.e14. doi: 10.1016/j.wneu.2017.07.026. [DOI] [PubMed] [Google Scholar]
- 12.Muta D, Nishi T, Koga K, Yamashiro S, Fujioka S, Kuratsu JI. Cavernous malformation of the optic chiasm: Case report. Br J Neurosurg. 2006;20:312–5. doi: 10.1080/02688690601000238. [DOI] [PubMed] [Google Scholar]
- 13.Ozer E, Kalemci O, Yücesoy K, Canda S. Optochiasmatic cavernous angioma: Unexpected diagnosis. Case report. Neurol Med Chir. 2007;47:128–31. doi: 10.2176/nmc.47.128. [DOI] [PubMed] [Google Scholar]
- 14.Robinson JR, Awad IA, Little JR. Natural history of the cavernous angioma. J Neurosurg. 1991;75:709–14. doi: 10.3171/jns.1991.75.5.0709. [DOI] [PubMed] [Google Scholar]
- 15.Son DW, Lee SW, Choi CH. Cavernous malformation of the optic chiasm: Case report. J Korean Neurosurg Soc. 2008;44:88. doi: 10.3340/jkns.2008.44.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sorenson TJ, Chen J, Burrows A, Lanzino G. Surgical resection of cavernous malformation of the optic nerve. Oper Neurosurg (Hagerstown) 2018;14:314. doi: 10.1093/ons/opx125. [DOI] [PubMed] [Google Scholar]
- 17.Venkataramana N, Rao SV, Arun L, Krishna C. Cavernous malformation of the optic chiasm: Neuro-endoscopic removal. Asian J Neurosurg. 2016;11:71. doi: 10.4103/1793-5482.145114. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


