Abstract
Background:
The aim of this study is to highlight the importance of cryptococcosis as one of the most common fungal infections of the central nervous system, stressing the consideration of a cryptococcoma within the list of differential diagnosis of intraventricular masses in immunocompetent hosts.
Case Description:
We present the case of an immunocompetent 41-year-old female from Philippines with an intraventricular cryptococcoma due to Cryptococcus neoformans, mimicking an intraventricular primary brain tumor, who had hydrocephalus. She was approached as having a neoplastic lesion and underwent surgical resection plus third ventriculostomy through endoscopy. Later in her evolution, we realized the infectious nature of the lesion, and antifungal systemic therapy was initiated. In the end, she needed the placement of a ventriculoperitoneal shunt to maintain a good neurologic status. Despite all our efforts, she had a fatal outcome due to various complications.
Conclusion:
Our case is the first intraventricular cryptococcoma due to C. neoformans, as far as we know, to be reported in English, German, or Spanish literature. Our report stresses the importance to consider this kind of infection in immunocompetent patients, to raise the level of suspicion of this diagnosis, and to know the complications and management options.
Keywords: Cryptococcoma, Cryptococcus neoformans, Hydrocephalus, Immunocompetent, Intraventricular, Neoplastic, Neuroendoscopy

INTRODUCTION
The encapsulated yeasts Cryptococcus neoformans and Cryptococcus gattii cause invasive fungal infections known as cryptococcosis. It is among the most common fungal infection in patients with human immunodeficiency virus (HIV).[2,11,13] C. neoformans is commonly related with immunocompromised patients causing mainly meningitis, and C. gattii is the usual suspect in immunocompetent population and is associated with cryptococcoma formation in the brain and lungs.[2,6,7] The case we report in this article is the first intraventricular cryptococcoma due to C. neoformans to be reported in English, German, or Spanish literature and stresses the importance to consider this infection in immunocompetent patients.
CASE REPORT
A 41-year-old Filipino female, with no medical record of interest, presented with a history of 4 months of gait imbalance, occasional urinary incontinence, and memory impairment. She was afebrile; laboratory investigations were normal; and the chest X-ray showed no evidence of pathology. Chronic hydrocephalus of the adult was initially suspected.
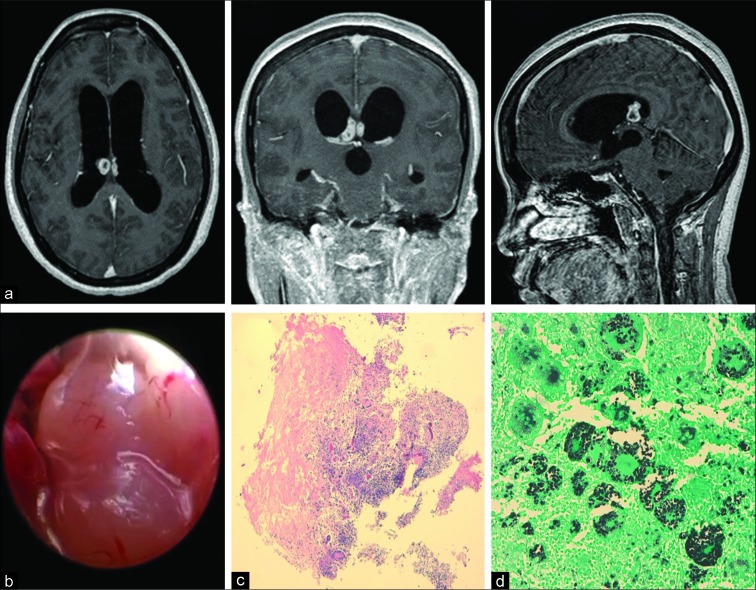
A computed tomography (CT) of the head was performed. It showed an intraventricular mass attached to the posterior third of the septum pellucidum and the fornix commissure and enlargement of the lateral and third ventricles. A magnetic resonance image confirmed an intraventricular polylobulated tumor of 1.6 cm in diameter, enhancing in a ring-like fashion with gadolinium. Furthermore, active hydrocephalus was present [Figure 1a]. Glioma was considered the primary diagnosis.
Figure 1:
(a) Initial magnetic resonance imaging sequences confirmed a right predominant mass with biventricular expression clearly attached to the septum pellucidum and invasion of the fornix commissure, as shown in axial, coronal, and sagittal T1WI C+ sequences, with gadolinium enhancement of the lesion in a ring-like fashion. (b) The lesion, as seen through the endoscope, was polylobulated, avascular, shiny, and of fibrous consistency. (c) Intraoperative examination showed a nonencapsulated, partially necrotic lesion surrounded by a dense cellular component that included “atypical” multinucleated cells with hyperchromatic nuclei (Hematoxylin-Eosin, ×2). (d) Numerous round yeasts with a characteristic thick capsule were found both in the cytoplasm of the histiocytes and giant cells (Gomori Methenamine silver stain, ×20).
She underwent removal of the lesion plus third ventriculostomy through endoscopy [Figure 1b]. An external ventricular drainage (EVD) was placed in situ on the right side to control cerebrospinal fluid (CSF) outflow. Intraoperative histologic examination showed a partially necrotic lesion surrounded by a dense cellular component that included atypical multinucleated cells and reactive glial proliferation, favoring the diagnosis of primary glioma [Figure 1c].
The EVD was removed after 72 h. Routine culture of the EVD tip identified Cryptococcus spp. (>15 colony-forming-units). Cultures confirmed C. neoformans. Systemic antifungal treatment was given immediately. We started amphotericin B 400 mg q24h IV plus 5-flucytosine 1500 mg q6h IV. Blood tests for HIV Types 1 and 2 were negative. Immunoglobulin levels and CD4 cell counts were normal.
The definitive histology identified numerous round yeasts with a characteristic thick capsule found both inside the cytoplasm of the histiocytes and giant cells, confirming its fungal nature [Figure 1d].
Four days later, she deteriorated and she developed a clinical situation of perplexity, reiterative speech, and bradypsychia and progressive loss of consciousness. Worsening ventriculomegaly was revealed in a head CT scan. She was moved to the intensive care unit (ICU) and a new EVD was placed. In the subsequent days, she had complications consisting in malfunction due to obstruction in the setting of infection and intraventricular hemorrhage. Several EVD replacements and raised intracranial pressure (ICP) despite maximal antifungal therapy led us to place a ventriculoperitoneal (VP) shunt. Neurological status was recovered at the beginning. Eventually, she showed neurological worsening, intraventricular hemorrhage, and VP malfunction. CSF cultures remained positive and no bacterial coinfection was reported. New CSF analysis from the EVD demonstrated worsening compatible with ventriculitis. In the end, after 10 days of antifungal treatment, the patient died due to complications related to infection, electrolyte imbalance, and multiorganic failure.
DISCUSSION
In this article, we describe an infection caused by C. neoformans in an immunocompetent patient, which is a rare sighting. Nonetheless, there are many reports describing this agent in these patients.[7] Nowadays, it is known that they can have some form of immunodeficiency not demonstrated with conventional tests.[6]
C. neoformans is found globally and is related with avian feces, whereas C. gattii is prevalent in zones with tropical climates, grows in soil, is not found on avian guanos, and has a relationship with eucalypt trees.[5] In Spain, from 1998 to 2003, a prevalence study was conducted where all the strains in human cryptococcosis belonged to C. neoformans until 2004 when the first human case of C. gattii was reported.[2]
There are two forms of cryptococcosis in the central nervous system (CNS): meningeal and parenchymal. The first one is the most frequent. The intraventricular formation of cryptococcomas is a rare finding. In a short review of 17 cases, only one was intraventricular.[7] A cryptococcoma is an organized mass of Cryptococcus and inflammatory cells. The infection is generally believed to be caused by C. neoformans. However, C. gattii is significantly associated with cryptococcoma formation particularly in immunocompetent hosts, where the appropriate inflammatory response permits the mass formation.[7,2,10] In the series reported by Li et al., concerning only cryptococcomas in immunocompetent patients, 18% (3 of 17) were reported to be caused by C. gattii.[7] Our case is the first intraventricular cryptococcoma due to C. neoformans to be reported in English, German, or Spanish literature. A previous intraventricular case reported by Popovich et al. had no species or strain confirmation.[12]
Cryptococcomas can be mistaken for malignant lesions in half of cases. Accurate diagnosis is only achieved following histological analysis.[10,13] When intraparenchymal, differential diagnosis should include pyogenic abscess, toxoplasma, lymphoma, CNS gliomas, metastasis, and tuberculoma. Furthermore, they share some of the features of a malignant glioma, like the thick ring-like gadolinium enhancement.[4,7] Despite these coincidences, the first diagnosis in mind should not be a cryptococcoma because when globally analyzing fungal granulomas, the main responsible is Aspergillus spp., followed by Mucor and Cladosporium.[4,9]
CSF analysis can reveal some important features such as high opening pressure, positive India ink stain, and detection of its capsular antigen. Important note is to point out that we achieved the diagnosis by culturing the EVD tip after the first surgery, which is a routine behavior after removal in our department.
The medical treatment of choice is the systemic antifungal regimen as a two-step approach: induction and consolidation.[11] Induction is achieved for 6 weeks with amphotericin B and 5-flucytosine and consolidation with fluconazole for 6–18 months. Corticosteroids, such as dexamethasone, can be used to reduce edema but have been not evaluated in clinical trials.[11]
Antifungal therapy alone is unlikely to penetrate large lesions enough to lead a remission. In these cases, if the lesion is accessible, a cryptococcoma should be treated by a combination of surgical and medical approaches as suggested by Ulett et al.[13] We share the opinion that a complete approach to this entity should consist of antifungal treatment, relief of ICP, and debulking of the lesion (especially if it is >3 cm in size). There is no clinical data to determine the best timing of surgical resection of cryptococcomas, but prolonged antifungal therapy is generally advised.[9,13]
In the presence of meningitis, the most important prognostic factor is increased ICP.[1,3,8] Patients can receive intravenous mannitol or repeated lumbar punctures (LP) with removal of CSF as a treatment. Serial LP is a frequent practice, but not all patients have the ability to tolerate this approach, and the VP shunting can offer them the possibility of a more permanent solution. There are three known issues about placing a VP shunt in these patients: infection, obstruction, and seeding, but several case series reports good outcomes and results in HIV-positive patients.[1,3,8] In our patient, the decision to place a VP shunt was based on persistent infection, active hydrocephalus, and high ICP despite the best medical therapy. There is no standard recommendation about the time to place a VP shunting, and the median time can range from 0.5 to 5 months.[1] Corti et al. suggest that patients with Cryptococcal meningoencephalitis who have increased ICP must be considered for VP shunting even when having positive CSF cultures.[3] Of important note, all the patients in these series were in the late stage of AIDS, and those recommendations are not elucidated in immunocompetent patients like our case.
We think our patient developed meningitis after Cryptococcus seeding during her first surgery (mass resection), and most probably related to the fact that she did not receive any antifungal treatment before the intervention. Our case was approached as a glioma, and the working space was exclusively inside the ventricles. We assume that we broke the cryptococcoma capsule during surgery which contributed to seeding and the subsequent ventriculitis and meningoencephalitis. Such risks are reported in the literature and are the main cause of death in these patients.[9] Most authors recommend the use of antifungal therapy before elective surgery for fungal granulomas so that the drugs can ameliorate the risks of postsurgical meningoencephalitis.[9,13]
Cryptococcomas, as fungal granulomas in general, have bad prognosis even in light of medical treatment and surgery, especially if the intraventricular space is violated during the procedure, causing the subsequent infection. Yeh et al. reported a case of a parenchymal cryptococcoma in a non- HIV patient who, despite the medical treatment and surgical resection, died in the end.[14] Ulett et al. reported a case of a cryptococcoma mimicking a glioblastoma who also died afterward, in spite of maximal antifungal therapy and surgical resection.[13] The overall mortality by all intracranial fungal granulomas is around 36%. Identified risk factors are poor neurologic status before surgery, emergency craniotomy, severe edema, and the opening of ventricles during surgery.[9]
Despite our efforts and multidisciplinary treatment, our patient died. She had a vegetative status before her death. This development is not extraordinary in such setting, even in immunocompetent patients.[3,4,12,13]
CONCLUSION
Cryptococcosis is misdiagnosed in HIV-negative patients because of the misconception that it only affects immunocompromised patients. Cryptococcomas have no specific radiologic findings and sometimes, even the histology can be confused with CNS tumors. When the ventricles are compromised, a course of antifungal treatment should be initiated before any surgical procedure. The mainstay of treatment of any fungal granuloma should be radical surgical resection (especially if it is >3 cm in diameter), antifungal therapy, and aggressive treatment of ICH. Placement of a VP shunt should be considered as part of the arsenal if CSF cultures remain positive in spite of optimal antifungal therapy. Finally, our case highlights the importance to obtain cultures from the tip of ventricular catheters as a routine behavior in any neurosurgical procedure.
Contributor Information
Xavier A. Santander, Email: xavier.santander@gmail.com.
Raquel Gutiérrez-González, Email: rgutierrezgonzalez@yahoo.es.
Carlos Cotúa, Email: elcotua34@gmail.com.
Eva Tejerina, Email: etejegon@telefonica.net.
Gregorio-Boto Rodríguez, Email: groboto@yahoo.es.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understands that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Calvo A, Hernández P, Spagnuolo E, Johnston E. Surgical treatment of intracranial hypertension in encephalic cryptococcosis. Br J Neurosurg. 2003;17:450–5. doi: 10.1080/02688690310001611242. [DOI] [PubMed] [Google Scholar]
- 2.Colom-Valiente MF, Frasés S, Ferrer C, Martín-Mazuelos E, de Mendoza MH, Torres-Rodríguez M, et al. Epidemiologic study of cryptococcosis in Spain: First results. Rev Iberoam Micol. 2001;18:99–104. [PubMed] [Google Scholar]
- 3.Corti M, Priarone M, Negroni R, Gilardi L, Castrelo J, Arechayala A, et al. Ventriculoperitoneal shunts for treating increased intracranial pressure in cryptococcal meningitis with or without ventriculomegaly. Rev Soc Bras Med Trop. 2004;47:524–7. doi: 10.1590/0037-8682-0176-2013. [DOI] [PubMed] [Google Scholar]
- 4.Dubey A, Patwardhan RV, Sampth S, Santosh V, Kolluri S, Nanda A. Intracranial fungal granuloma: Analysis of 40 patients and review of the literature. Surg Neurol. 2005;63:254–60. doi: 10.1016/j.surneu.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 5.Ellis DH, Pfeifer TJ. Natural habitat of Cryptococcus neoformans var. Gattii. J Clin Microbiol. 1990;28:1642–4. doi: 10.1128/jcm.28.7.1642-1644.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Harris JR, Lockhart SR, Debess E, Marsden-Haug N, Goldoft M, Wohrle R, et al. Cryptococcus gattii in the United States: Clinical aspects of infection with an emerging pathogen. Clin Infect Dis. 2011;53:1188–95. doi: 10.1093/cid/cir723. [DOI] [PubMed] [Google Scholar]
- 7.Li Q, You C, Liu Q, Liu Y. Central nervous system cryptococcoma in immunocompetent patients: A short review illustrated by a new case. Acta Neurochir. 2010;152:129–36. doi: 10.1007/s00701-009-0311-8. [DOI] [PubMed] [Google Scholar]
- 8.Liu L, Zhang R, Tang Y, Lu H. The use of ventriculoperitoneal shunts for uncontrollable intracranial hypertension in patients with HIV-associated cryptococcal meningitis with or without hydrocephalus. Biosci Trends. 2014;8:327–32. doi: 10.5582/bst.2014.01070. [DOI] [PubMed] [Google Scholar]
- 9.Naik V, Ahmed FU, Gupta A, Garg A, Sarkar C, Sharma B, et al. Intracranial fungal granulomas: A single institutional clinicopathologic study of 66 patients and review of the literature. World Neurosurg. 2015;83:1166–72. doi: 10.1016/j.wneu.2015.01.053. [DOI] [PubMed] [Google Scholar]
- 10.Oliveira M, Severo CB, Guazzelli LS, Severo LC. Cryptococcus gattii fungemia: Report of a case with lung and brain lesions mimicking radiological features of malignancy. Rev Inst Med Trop Sao Paulo. 2007;49:263–5. doi: 10.1590/s0036-46652007000400014. [DOI] [PubMed] [Google Scholar]
- 11.Perfect JR, Dismukes WE, Dromer F, Goldman DL, Graybill JR, Hamill RJ, et al. Clinical practice guidelines for the management of cryptococcal disease: 2010 update by the Infectious Diseases Society of America. Clin Infect Dis. 2010;50:291–322. doi: 10.1086/649858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Popovich MJ, Arthur RH, Helmer E. CT of intracranial cryptococcosis. Am J Roentgenol. 1990;154:603–18. doi: 10.2214/ajr.154.3.2106227. [DOI] [PubMed] [Google Scholar]
- 13.Ulett K, Cockburn J, Jefree R, Woods M. Cerebral cryptococcoma mimicking glioblastoma. BMJ Case Rep. 2017;2017:218824. doi: 10.1136/bcr-2016-218824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yeh CH, Wang CS, Yeh TC, Lai CC. Central nervous system infection caused by Cryptococcus. Intern Med. 2013;52:2387–8. doi: 10.2169/internalmedicine.52.0613. [DOI] [PubMed] [Google Scholar]