Abstract
Introduction:
Management of type 1 diabetes (T1D) is labor-intensive, requiring multiple daily blood glucose measurements and insulin injections. Patients are seen quarterly by providers, but evidence suggests more frequent contact is beneficial. Current technology allows secure, remote sharing of diabetes data and video-conferencing between providers and patients in their home settings.
Methods:
Home-based video visits were provided for six months to pediatric T1D patients with poor glycemic control, indicated by a hemoglobin A1c (HbA1c) ≥8% at enrollment. Video visits were conducted every 4–8 weeks in addition to regularly scheduled clinic visits. Dates of clinic visits and HbA1c values were abstracted from the medical record at baseline and six months. Patients were surveyed at video visits regarding technical issues, and after six months a standardized survey was administered to assess satisfaction with video-based care.
Results:
Fifty-seven patients enrolled and thirty-six completed six months of video visits. Patients completing six months averaged 4.0 video visits (SD 1.1). Their frequency of in-person care also increased from 3.2 clinic visits/year at baseline to 3.7 clinic visits/year during the study (p = 0.04). Mean HbA1c reduction among patients completing six months was 0.8% (95% CI 0.2–1.4%), and 94% of these patients were “very satisfied” while 6% were “somewhat satisfied” with the experience.
Discussion:
This study demonstrates that home-based video visits are feasible and satisfactory for pediatric patients with poorly controlled T1D. Furthermore, use of video visits can improve frequency of subspecialty care and resulting glycemic control in this population.
Introduction
Type 1 diabetes (T1D) is one of the three most common chronic diseases of childhood, along with asthma and obesity.1 Over 160,000 children and adolescents in the U.S. have been diagnosed with T1D,2 and incidence continues to rise for unknown reasons.1–3 Patients with T1D are dependent on exogenous insulin, which is delivered via multiple daily injections or insulin pump, and doses are calibrated to blood glucose levels and dietary intake. Guidelines recommend quarterly visits with a subspecialist,4–7 which are sufficient for some pediatric patients, but many others fail to achieve optimal glycemic control, defined as a hemoglobin A1c (HbA1c) of <7.5%.7
Evidence suggests that more frequent contact with providers can improve outcomes for high-risk T1D patients.8–10 However, there are multiple barriers to achieving more frequent care in this population. Undersupply of pediatric diabetes specialists,11 an expanding number of youth with T1D,3 and poor reimbursement for multidisciplinary services in an office setting12 combine to limit clinic appointments. For patients and families, attending clinic visits leads to missed school hours, parental time away from work, and transportation expenses. And until recently, home glucose meter data – an essential element of diabetes treatment decisions – could only be accessed by providers in a medical setting.
Recent advances in diabetes technology and telemedicine have the potential to solve these issues and improve healthcare access for T1D patients. New glucose meters13 and continuous glucose monitors14 are Bluetooth enabled, and secure, internet-based platforms now interface with a wide variety of diabetes devices,15–17 enabling patients to upload data from home and share it with providers remotely. In addition, support for telehealth technologies has expanded dramatically in the last decade,18 and several internet-based video platforms are now compliant with the Health Insurance Portability and Accountability Act (HIPAA).19–21 In light of these technological developments, the purpose of this study was to examine the feasibility of home-based video visits for children and adolescents with poorly controlled T1D, and to evaluate the impact of such visits on frequency of diabetes care, HbA1C levels, and patient satisfaction after six months.
Methods:
Patients were recruited during visits to the Pediatric Diabetes Clinic at the University of California, Davis Medical Center from November 27th, 2017 to February 2nd, 2018. Inclusion criteria for the study were 1) age 1–17 years, 2) a known diagnosis of T1D, 3) a current hemoglobin A1c (HbA1c) level of ≥8%, indicating suboptimal glycemic control, 4) access to the internet via a device with video and audio capability (e.g. computer, tablet, mobile phone), and 5) ability to connect the patient’s home glucose meter (as well as insulin pump and/or continuous glucose meter, if applicable) to an internet-capable device via Bluetooth or physical cable. The only exclusion criterion was the need for English language interpretation services, due to the difficulty in securing interpretation services remotely. Written, informed consent was obtained from each patient’s parent or guardian, and patients 8–17 years of age also provided assent to participate. All participants received the study intervention, which consisted of home-based video visits with a diabetes specialist in addition to regularly scheduled clinic visits. The frequency of video visits was determined by HbA1c value at enrollment, such that patients received video visits every 4 weeks (if HbA1c >12%), 6 weeks (if HbA1c 10–12%), or 8 weeks (if HbA1c <10%). Baseline data was collected from each participant’s electronic health record (EHR) at enrollment, including demographic and insurance information, most recent HbA1c, and frequency of clinic visits during the preceding year.
Video visits were conducted using Vidyo Desktop, a home-to-clinic web-based video conferencing platform which is HIPAA compliant.19 The majority of visits connected the provider with the patient and a parent or guardian, but patients ≥16 years of age were permitted to have solo visits with the provider if the parent or guardian consented to this arrangement. A single pediatric endocrinologist conducted all video visits for this study, eliminating any inter-provider variability in clinical approach. Participants uploaded glucose meter data (as well as insulin pump and/or continuous glucose monitor data, if applicable) prior to each visit, using free and secure internet platforms that were compatible with their diabetes devices and home computers, tablets, or mobile phones.14, 16, 17, 22–25 Research team members provided initial guidance in the selection and setup of these platforms for each participant, as well as ongoing support for any technical issues encountered during the study.
Each video visit included discussion of interval health events and patient or family concerns, review of shared blood glucose data and insulin dose information, and provision of recommendations by the physician including changes in behavioral strategies and insulin dose adjustments. This content was equivalent to the physician portion of in-person clinic visits, except that a detailed physical exam could not be performed. During each video visit, participants were also asked about any technical issues they faced while uploading diabetes data or using the video application. Six months after study enrollment, the research team surveyed participants – via telephone, secure video application, or in-person, depending on availability – regarding the experience of using video visits for T1D management. Survey questions assessed overall satisfaction, perceived benefits of the video visits, frequency of technical glitches, and time (including transit) required to complete video visits compared to in-person clinic visits. See Table 4 for a complete list of survey questions and possible responses. Survey responses were elicited from patients and parents together in most cases, and from patients alone for those participants ≥16 years of age who engaged in solo video visits with the provider.
TABLE 4.
Survey Responses After Six Months
| N (%) | |
| Overall, how satisfied are vou with vour experience using telemedicine so far? | |
| Very satisfied | 34 (94%) |
| Somewhat satisfied | 2 (6%) |
| Somewhat dissatisfied | 0 (0%) |
| Very dissatisfied | 0 (0%) |
| What part of the study have you found most helpful? | |
| The program or app 1 use to share my diabetes data | 4 (11%) |
| The doctor’s changes to my insulin doses | 11 (31%) |
| Other advice or encouragement given by the doctor | 15 (42%) |
| Assistance with issues that come up between clinic visits | 6 (17%) |
| None of the above | 0 (0%) |
| Has the telemedicine study helped you with any of the following? | |
| Improved monitoring of my blood glucose levels | 32 (89%) |
| Improvement in my Alc | 20 (56%) |
| Improved access to diabetes technology | 19 (53%) |
| Fewer visits to the ED or hospital | 20 (56%) |
| Improved access to my care team between clinic visits | 33 (92%) |
| None of the above | 0 (0%) |
| Median (Range) | |
| How many times did vou need help from the team with technology? | |
| The Vidyo program | 0(0–3) |
| Sharing diabetes device data from home | 1 (0–4) |
| Please estimate the number of minutes it takes in your day for: | |
| A visit to our clinic | 240 (120–4320) |
| A telemedicine visit | 30 (10–90) |
| Uploading diabetes device data from home | 5(0–60) |
Finally, the dates of participants’ visits to the pediatric diabetes clinic during the study period, and their HbA1c levels measured at those clinic visits, were abstracted from the EHR. The numbers of clinic and video visits completed by each participant during the study period were used to calculate annualized rates of care for these categories. The latest HbA1c measured within six months following enrollment for each patient was used to calculate change in HbA1c experienced during the study. Point-of-care HbA1c monitors in clinic were unable to measure values above 14%, therefore values of >14% were treated as 14% in our analysis. Univariable comparisons between baseline and six month values were made using a two-tailed t-test for paired samples. The University of California, Davis Institutional Review Board approved this study.
Results:
Fifty-seven patients were enrolled over a ten-week period, representing a 60% recruitment rate among approached patients (Figure 1). Forty-six percent of the enrolled cohort had a HbA1c <10%, 28% had a HbA1c of 10–12%, and 26% had a HbA1c >12% at enrollment (Table 1). Only 21% had attended the recommended 4 clinic visits per year in the 12 months preceding enrollment. Twenty-one patients dropped out of the study, the majority (13 patients) before completing any video visits. Reasons for dropout included voluntary withdrawal (43%) due to insufficient time, inability of the research team to contact the patient or family (38%), and technological barriers (14%) such as loss of internet access. One patient required intensive psychiatric care and was therefore withdrawn from the study. Patients who dropped out did not differ significantly from patients who completed the study on any baseline characteristics (Table 1).
FIGURE 1.
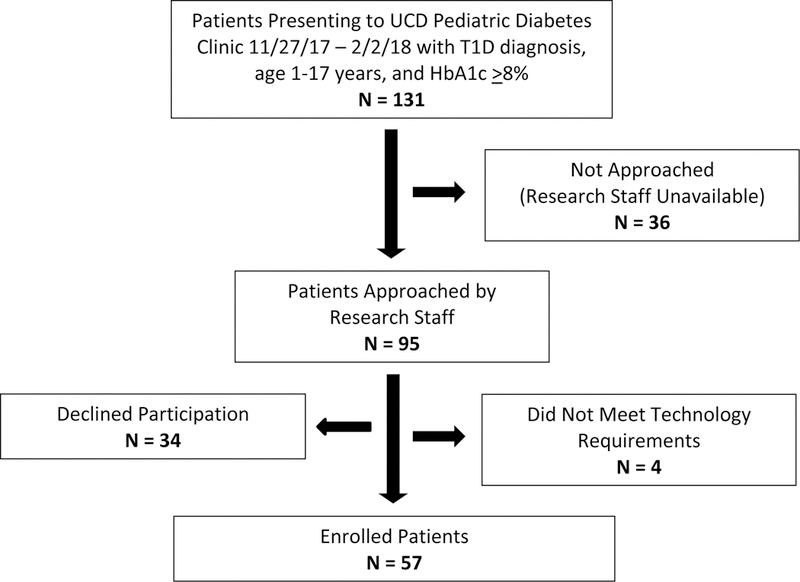
Consort diagram depicting study recruitment
TABLE 1.
Patient Characteristics
| Enrolled Patients (57) | Completed Study (36) | Dropped Out (21) | P-value* | |
|---|---|---|---|---|
| Age at Enrollment in Years | ||||
| 3–7 | 7 (12%) | 6 (17%) | 1 (5%) | 0.38 |
| 8–12 | 22 (39%) | 12 (33%) | 10 (48%) | |
| 13–17 | 28 (49%) | 18 (50%) | 10 (48%) | |
| Sex | ||||
| Female | 25 (44%) | 16 (44%) | 9 (43%) | 0.91 |
| Male | 32 (56%) | 20 (56%) | 12 (57%) | |
| Race | ||||
| Asian | 2 (4%) | 1 (3%) | 1 (5%) | 0.51 |
| Black/African American | 7 (12%) | 6 (17%) | 1 (5%) | |
| White/Caucasian | 41 (72%) | 26 (72%) | 15 (71%) | |
| More Than One Race | 3 (5%) | 1 (3%) | 2 (10%) | |
| Unknown/Not Reported | 4 (7%) | 2 (6%) | 2 (10%) | |
| Ethnicity | ||||
| Hispanic/Latino | 6 (11%) | 2 (6%) | 4 (19%) | 0.18 |
| Not Hispanic/Latino | 51 (89%) | 34 (94%) | 17 (81%) | |
| Insurance | ||||
| Public | 33 (58%) | 20 (56%) | 13 (62%) | 0.64 |
| Private | 24 (42%) | 16 (44%) | 8 (38%) | |
| Hemoglobin A1c at Enrollment | ||||
| 8 to <10% | 26 (46%) | 16 (44%) | 10 (48%) | 0.23 |
| 10 to 12% | 16 (28%) | 8 (22%) | 8 (38%) | |
| >12% | 15 (26%) | 12 (33%) | 3 (14%) | |
| Clinic Visits During Preceding Year | ||||
| 0–1 | 4 (7%) | 1 (3%) | 3 (14%) | 0.48 |
| 2 | 14 (25%) | 9 (25%) | 5 (24%) | |
| 3 | 26 (46%) | 17 (47%) | 9 (43%) | |
| 4+ | 13 (23%) | 9 (25%) | 4 (19%) | |
| Distance in Kilometers to Clinic | ||||
| <50 | 24 (42%) | 13 (36%) | 11 (52%) | 0.69 |
| 51–100 | 15 (26%) | 11 (31%) | 4 (19%) | |
| 101–200 | 7 (12%) | 5 (14%) | 2 (10%) | |
| >200 | 11 (19%) | 7 (19%) | 4 (19%) | |
P-values calculated using Pearson’s χ2 test or Fisher’s exact test, comparing patients completing study with those dropping out
The 36 patients who completed six months of visits averaged 4.0 video visits per person (SD 1.1) during this time, and the vast majority of them met or exceeded their prescribed number of video visits, with just 2 patients in the >12% HbA1c group completing four visits instead of the assigned five. The cohort who completed six months also experienced an increase in frequency of in-person visits, from 3.2 clinic visits/year on average at baseline to 3.7 clinic visits/year on average during the study (p = 0.04), giving them an average overall visit frequency during the study of 11.6 visits/year (SD 2.9) including both clinic and video visits (Table 2). Analysis of HbA1c values revealed that among patients completing the 6-month study period, 27 (75%) experienced a decline in HbA1c. The mean HbA1c improvement for all patients who completed the study was 0.8% (95% CI 0.2 – 1.4%). Among those who demonstrated a decline in HbA1c, the mean improvement was 1.5% (95% CI 1.0 – 2.0%) (Table 3).
TABLE 2.
Change in Frequency of Diabetes Care
| Mean Visits Per Patient (SD) 12 Months Prior to Study |
Mean Visits Per Patient (SD) 6 Month Study Period |
Mean Visits/Year Per Patient (SD) 6 Month Study Period |
P-Value* |
|
|---|---|---|---|---|
| Clinic Visits | 3.2 (1.1) | 1.8 (0.6) | 3.7 (1.1) | 0.04 |
| Video Visits | - | 4.0 (1.1) | 7.9 (2.3) | - |
| Total Diabetes Visits | 3.2 (1.1) | 5.8 (1.5) | 11.6 (2.9) | <0.001 |
P-values calculated using two-tailed t-test for paired samples, comparing visits during 12 months prior to study with annualized rate during study
TABLE 3.
Hemoglobin A1c Changes After Six Months
| Mean HbA1c | Mean HbA1c | |||
|---|---|---|---|---|
| Enrollment | 6 Months | Mean Decline in HbA1c | P-value* | |
| All Patients Completing Study (N = 36) | 10.9% | 10.0% | 0.8% (95% CI 0.2 – 1.4%) | 0.007 |
| Patients with Decline in HbA1c (N = 27) | 10.8% | 9.3% | 1.5% (95% CI 1.0–2.0%) | <0.001 |
P-values calculated using two-tailed t-test for paired samples, comparing mean HbA1c at enrollment versus at 6 months
In terms of patients’ experience of care, 94% of participants who completed the study stated they were “very satisfied” and the remaining 6% stated they were “somewhat satisfied” with the video visit experience (Table 4). Forty-two percent rated “advice or encouragement given by the doctor” as the most beneficial aspect of their video visits, followed by “the doctor’s changes to my insulin doses” (31%), “assistance with issues that come up between clinic visits” (17%) and “the program or app I use to share my diabetes data” (11%). When asked to designate any perceived improvements in diabetes care as a result of the study, 92% cited “improved access to my care team between clinic visits”, 89% cited “improved monitoring of my blood glucose levels”, and just over half of patients each cited “improvement in my A1c”, “fewer visits to the emergency department or hospital” and “improved access to diabetes technology.”
Difficulty with remote diabetes data sharing was reported at 20% of initial video visits and 13% of subsequent visits, and difficulty with the video application was reported at 18% of initial visits but only 2% of subsequent visits. Survey responses after six months (Table 4) indicated that participants required help with the video application 0–3 times (median of 0 times) in six months, and help with sharing their diabetes device data 0–4 times (median of 1 time) in six months. Participants were also asked to estimate the number of minutes required in their days to attend clinic visits, to attend video visits, and to upload their diabetes device data from home. Visits to clinic were estimated to require a median of 240 minutes (including transportation time), with a range of 120 to 4320 minutes – the latter for a patient who travels from a great distance and stays locally overnight to attend clinic visits. Video visits were estimated to take 30 minutes with a range of 10 to 90 minutes, and uploading diabetes devices was estimated at a median time of 5 minutes with a range of 0 to 60 minutes (Table 3). The median combined time per patient for a video visit and to upload diabetes devices was 33 minutes (range 12 – 110 minutes), and median estimated time savings for a video visit (including visit time and upload time) compared to a clinic visit was 186 minutes (range 70 – 4274 minutes).
Discussion:
This study demonstrates that pediatric T1D patients with poor glycemic control find home-based video visits an acceptable and highly satisfactory modality for receiving diabetes care. Furthermore, our results illustrate that video visits can successfully deliver more frequent subspecialist care to a population that was not achieving the recommended quarterly visits at baseline, and that this care can result in significant improvement in HbA1c levels over six months. These results are novel in several ways. The bulk of telemedicine research in diabetes to date has involved adult patients with type 2 diabetes, and published studies of telemedicine in type 1 diabetes (adult and pediatric) have primarily utilized telephone, texting, Smartphone applications, and asynchronous data transfer.26, 27 Very few published studies have employed videoconferencing in the treatment of pediatric type 1 diabetes.28–31 Among these, only one has provided home-based video visits and this study targeted adolescents and young adults;29 none have aimed to deliver visits more frequently than every three months. While all four of these published studies demonstrated some improvement in frequency of care resulting from video visits, none achieved the high frequency of visits that we have demonstrated with our intervention, and none documented a significant improvement in HbA1c for participants. The improvement in HbA1c in our study may therefore relate directly to the frequency of video visits delivered.
Our study’s high dropout rate suggests that this clinical population is not always able or willing to engage in additional care encounters, and that uploading diabetes data to online platforms and accessing video applications may present excessive technical challenges for some. Patients who dropped out did not differ significantly from patients who completed six months of video visits on any of their baseline characteristics, including demographics, insurance status, HbA1c at enrollment, baseline frequency of clinic visits, or distance from home to clinic. However, we do not have information about other factors, such as household income, education level, and comfort with technology, which could be associated with study retention. In order to determine patients’ reasons for discontinuing the study, our research team will be undertaking focused interviews with study participants – both those who completed the study and those who dropped out – in the near future. We hope the feedback from these interviews will identify patient-level barriers to adoption of our intervention, and allow us to hone its effectiveness for a broader subset of patients prior to our next research study.
In addition to the numeric results reported here, patients and families in our study commented on multiple other benefits of home-based video visits. The video platform used allowed for three-way conferences, and several families found it convenient for the parent to join from work and the patient to join from home or school. We were able to conduct video visits at lunchtime for patients who had after-school activities, and in the late afternoon or early evening for parents who could not get off work until 4:30 or 5:00pm. Due to the lack of transit time, this scheduling allowed participants to join visits without missing school or work, and allowed the diabetes provider to complete all video visits by 5:30pm. We also found during the study that several patients’ parents or caretakers who had not been attending clinic visits (often the father, stepparent, or grandparent) were able to join the video visits, and sometimes even took the lead role for these visits, which allowed them to re-engage in diabetes management. Similarly, for several patients whose parents are divorced, the parents alternated attending video visits for the child, whereas in-person clinic visits had disproportionately involved one parent over the other. Interestingly, while technology engagement proved to be the most difficult part of the study for some participants, others found that the diabetes device application or platform they used for the study was one of the most helpful aspects of our intervention. Having easy access to blood glucose values on patients’ and parents’ phones, as well as receiving regular reminders – just prior to video visit appointments – to upload and review this data prompted patients and caregivers to pay closer attention to diabetes management between clinic visits.
The current analysis is limited as a result of its focus on feasibility and satisfaction, involving a non-randomized design and a single cohort with pre- and post-intervention comparison. However, our study adds important data to a very small body of literature about use of video telemedicine for pediatric T1D, and represents the first published study of home-based video visits resulting in improved glycemic control for the pediatric age range. Further trials of home-based video visits for pediatric T1D are needed, coupled with robust analysis of health outcomes via a randomized, controlled design. Our research team intends to conduct such a randomized trial in the near future, while exploring options to continue providing home-based telemedicine on a clinical basis to patients who may benefit. We feel that the application of existing technology to improve care access and outcomes for pediatric patients with T1D presents an opportunity to achieve the Institute for Healthcare Improvement’s “triple aim” of improving health, improving patient experience, and reducing costs.
Acknowledgements:
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant number UL1 TR001860 and linked award KL2 TR001859. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Footnotes
Declarations: The authors have no conflicts of interest to declare relevant to this research.
References
- 1.Stanescu DE, Lord K and Lipman TH. The epidemiology of type 1 diabetes in children. Endocrinology and metabolism clinics of North America. 2012; 41: 679–94. [DOI] [PubMed] [Google Scholar]
- 2.Pettitt DJ, Talton J, Dabelea D, et al. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes care. 2014; 37: 402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tuomilehto J The emerging global epidemic of type 1 diabetes. Current diabetes reports. 2013; 13: 795–804. [DOI] [PubMed] [Google Scholar]
- 4.Pihoker C, Forsander G, Wolfsdorf J and Klingensmith GJ. The delivery of ambulatory diabetes care to children and adolescents with diabetes. Pediatric diabetes. 2009; 10 Suppl 12: 58–70. [DOI] [PubMed] [Google Scholar]
- 5.Chiang JL, Kirkman MS, Laffel LM, Peters AL and Type 1 Diabetes Sourcebook A. Type 1 diabetes through the life span: a position statement of the American Diabetes Association. Diabetes care. 2014; 37: 2034–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. Standards of medical care in diabetes-2015 abridged for primary care providers. Clin Diabetes. 2015; 33: 97–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes Association. Children and adolescents. Diabetes care. 2015; 38 Suppl: S70–6. [DOI] [PubMed] [Google Scholar]
- 8.Nathan DM, Bayless M, Cleary P, et al. Diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: advances and contributions. Diabetes. 2013; 62: 3976–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maldonado MR, D’Amico S, Rodriguez L, Iyer D and Balasubramanyam A. Improved outcomes in indigent patients with ketosis-prone diabetes: effect of a dedicated diabetes treatment unit. Endocrine practice : official journal of the American College of Endocrinology and the American Association of Clinical Endocrinologists. 2003; 9: 26–32. [DOI] [PubMed] [Google Scholar]
- 10.Franklin VL, Waller A, Pagliari C and Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabetic medicine : a journal of the British Diabetic Association. 2006; 23: 1332–8. [DOI] [PubMed] [Google Scholar]
- 11.Lee JM, Davis MM, Menon RK and Freed GL. Geographic distribution of childhood diabetes and obesity relative to the supply of pediatric endocrinologists in the United States. The Journal of pediatrics. 2008; 152: 331–6. [DOI] [PubMed] [Google Scholar]
- 12.Jewett EA, Anderson MR and Gilchrist GS. The pediatric subspecialty workforce: public policy and forces for change. Pediatrics. 2005; 116: 1192–202. [DOI] [PubMed] [Google Scholar]
- 13.Diabetes Forecast. www.diabetesforecast.org/2015/mar-apr/images/glucose-meters-2015-revised8-7.pdf, Last accessed November 1, 2016.
- 14.Dexcom Clarity. https://clarity.dexcom.com/, Last accessed November 21, 2018.
- 15.Diasend. https://www.diasend.com/us/, Last accessed November 21, 2018.
- 16.Glooko. https://www.glooko.com, Last accessed November 21, 2018.
- 17.Tidepool. http://www.tidepool.org, Last accessed November 21, 2018.
- 18.Utidjian L and Abramson E. Pediatric Telehealth: Opportunities and Challenges. Pediatr Clin North Am. 2016; 63: 367–78. [DOI] [PubMed] [Google Scholar]
- 19.Vidyo. www.vidyo.com/solutions/healthcare, Last accessed November 21, 2018.
- 20.Zoom. https://zoom.us/plan/healthcare, Last accessed November 1, 2016.
- 21.Cisco. www.cisco.com/c/en/us/solutions/industries/healthcare/care-at-a-distance.html, Last accessed November 1, 2016.
- 22.Carelink. https://carelink.medtronic.com/, Last accessed November 21, 2018.
- 23.OneTouch Reveal. https://onetouchreveal.com/, Last accessed November 21, 2018.
- 24.Accuchek Connect. https://www.accu-chekconnect.com, Last accessed November 21, 2018.
- 25.TConnect. https://tconnect.tandemdiabetes.com, Last accessed November 21, 2018.
- 26.Tchero H, Kangambega P, Briatte C, Brunet-Houdard S, Retali GR and Rusch E. Clinical Effectiveness of Telemedicine in Diabetes Mellitus: A Meta-Analysis of 42 Randomized Controlled Trials. Telemed J E Health. 2018. [DOI] [PubMed] [Google Scholar]
- 27.Su D, Zhou J, Kelley MS, et al. Does telemedicine improve treatment outcomes for diabetes? A meta-analysis of results from 55 randomized controlled trials. Diabetes Res Clin Pract. 2016; 116: 136–48. [DOI] [PubMed] [Google Scholar]
- 28.Wood CL, Clements SA, McFann K, Slover R, Thomas JF and Wadwa RP. Use of Telemedicine to Improve Adherence to American Diabetes Association Standards in Pediatric Type 1 Diabetes. Diabetes Technol Ther. 2016; 18: 7–14. [DOI] [PubMed] [Google Scholar]
- 29.Reid MW, Krishnan S, Berget C, et al. CoYoT1 Clinic: Home Telemedicine Increases Young Adult Engagement in Diabetes Care. Diabetes Technol Ther. 2018; 20: 370–9. [DOI] [PubMed] [Google Scholar]
- 30.Smith AC, Batch J, Lang E and Wootton R. The use of online health techniques to assist with the delivery of specialist paediatric diabetes services in Queensland. J Telemed Telecare. 2003; 9 Suppl 2: S54–7. [DOI] [PubMed] [Google Scholar]
- 31.Malasanos TH, Burlingame JB, Youngblade L, Patel BD and Muir AB. Improved access to subspecialist diabetes care by telemedicine: cost savings and care measures in the first two years of the FITE diabetes project. J Telemed Telecare. 2005; 11 Suppl 1: 74–6. [DOI] [PubMed] [Google Scholar]


