Abstract
Objective:
In panic-focused psychodynamic psychotherapy (PFPP), exploration and interpretation of avoided and conflicted emotions and fantasies surrounding anxiety are thought to promote panic-specific reflective functioning (PSRF), which drives panic disorder (PD) improvements. Patient emotional expression within a session may be a marker of engaged processing and experiencing of affectively charged material. Degree of in-session expressed emotion, indicating both verbal and nonverbal emotions, was examined across three early therapy sessions for prediction of subsequent outcomes. We further investigated whether personality disorder traits, theorized to relate to constricted (obsessive-compulsive) or heightened (borderline) emotions moderated this relationship.
Method:
Emotional expression in Sessions 2, 5, and 10 of a 24-session PFPP protocol was assessed by blinded observers in 44 patients randomized to PFPP in a two-site randomized controlled trial of psychotherapies for PD. Robust regressions were conducted to examine the relationship between average emotional expression across the measured sessions and symptom and PSRF changes subsequent to the sampled sessions, as well as moderation by personality disorder criteria, controlling for early outcomes.
Results:
Higher levels of emotional expression across the early sessions predicted greater subsequent symptom and PSRF improvement. Elevations in expression of grief/sadness drove the symptomatic finding. Patients meeting more borderline criteria experienced a smaller and potentially negative relationship between emotional expression and symptom improvement.
Conclusions:
Emotional expression in PFPP may be an indicator of positive therapy process for patients without comorbid borderline personality traits, predicting prospective improvements in both a key mediator (PSRF) and symptoms.
Keywords: psychodynamic therapy, panic disorder, emotion, process
Panic-focused psychodynamic psychotherapy (PFPP) (Busch, Milrod, Singer, & Aronson, 2012) is a 24-session, 12-week evidence-based treatment for panic disorder (PD; Beutel et al., 2013; Keefe, McCarthy, Dinger, Zilcha-Mano, & Barber, 2014; Milrod et al., 2016; Milrod et al., 2007) that focuses on understanding and working through unrealized or disavowed meanings surrounding the onset of acute attacks and associated anxiety in patients with panic disorder. One common meaning might be real or imagined loss of attachment figures, as suggested by epidemiological data showing high comorbidity or past history of separation anxiety among panic patients (Kossowsky et al., 2013; Milrod et al., 2014), and the fact that emotional stressors, such as relationship conflict and interpersonal loss, frequently precede the development of panic disorder (Klass et al., 2009; Scocco, Barbieri, & Frank, 2007). Recognizing the sometimes conflicted emotions and fantasies connected with experiences of panic and anxiety (such as unacknowledged rage at attachment figures) is hypothesized to improve panic-specific reflective functioning (PSRF; Rudden, Milrod, Target, Ackerman, & Graf, 2006). PSRF is an interview-based measured intended to tap into the degree to which patients can identify and discuss potential psychological meanings surrounding and triggers to experiences of panic and anxiety (Rudden et al., 2006). Early improvement in PSRF has been shown to predict subsequent improvement in panic symptoms in both PFPP and cognitive-behavioral therapy (CBT) (Barber et al., under review).
The theory that informs CBTs for panic disorder focuses on patients’ tendencies to catastrophically misinterpret bodily sensations (Clark et al., 1997) and thereby to fear those sensations (Boswell et al., 2013). However, specific problems in emotional recognition and acceptance have also been observed in studies of patients with panic disorder, suggesting that these factors may also contribute to panic experiences. Patients with PD report higher rates of alexithymia, experiential avoidance, and lack of emotional acceptance, compared to psychiatrically healthy controls and persons with simple phobias (Galderisi et al., 2008; Izci et al., 2014; Parker, Taylor, Bagby, & Acklin, 1993; Tull & Roemer, 2007). Relative to non-psychiatric controls, panic patients have also been observed to use relatively more emotional avoidance strategies in response to viewing negatively or positively-valenced film clips (Tull & Roemer, 2007). Experimentally instructing use of such strategies in healthy controls (relative to allowing emotional experience) promotes subjective distress, heightened physiological arousal in the moment, and also physiological reactivity in a subsequent stressful interpersonal task (Tull, Jakupcak, & Roemer, 2010).
Avoidance of emotions in day-to-day life may promote development of panic attacks if emotional contents are not addressed—for example, a person may get strongly physiologically aroused due to unacceptable emotions, but be unable to dissipate that arousal due to lack of emotional awareness and a consequent inability to acknowledge what is upsetting him/her. A patient may also attribute emotional arousal to frightening somatic causes that can psychologically stand in for conflicted feelings. In support of this conceptualization, a recent process study of CBT for panic disorder found that reductions in patient reports of emotional suppression preceded improvements in catastrophic, body-focused cognitions and panic symptoms (Strauss, Kivity, & Huppert, 2018).
Emotions and Outcome in Psychodynamic Therapies
Psychodynamic frameworks conceptualize attempts to avoid affects and particular affectively charged contents as contributing to the emergence of psychiatric symptoms and psychosocial dysfunction (Subic-Wrana et al., 2016). Within these frameworks, defense mechanisms work to maintain lack of awareness (Perry & Bond, 2012), which occurs to protect the person from experiencing psychic danger, yet precludes the individual’s ability to process and address the relevant conflicts or wishes. Panic patients have been observed to have heightened use of so-called neurotic and immature defenses relative to healthy controls (Busch, Shear, Cooper, Shapiro, & Leon, 1995; Calati, Oasi, De Ronchi, & Serretti, 2010; Kipper et al., 2004), and to exhibit a unique defensive profile compared to depression patients (Busch et al., 1995).
Therapeutic focus on difficult-to-express or disavowed affect has been commonly considered to be a feature distinguishing psychodynamic therapies (PDT) from cognitive-behavioral approaches (Blagys & Hilsenroth, 2000; McCarthy & Barber, 2009). In PDT, such focus can be achieved via supportive interventions encouraging expression of affect, clarification/confrontation highlighting important areas of affective exploration, or interpretations of affectively-laden meanings. In a meta-analytic examination, psychodynamic therapies in which therapists were coded by observers as being especially affect-focused were more successful in symptomatic outcomes, with a medium effect size (Diener, Hilsenroth, & Weinberger, 2007), although temporal precedence was not established in most studies and some studies in fact involved patient expression. In two recent studies assessing psychodynamic therapist technique specifically in anxiety disorder therapies (Pitman, Slavin-Mulford, & Hilsenroth, 2014) and in a transdiagnostic sample examining anxiety symptom improvement (Pitman, Hilsenroth, Weinberger, Conway, & Owen, 2017), higher focus by the therapist on unexpressed/avoided affects was related to more pre-to-post treatment symptom improvement.
In PDTs, links (often temporally sequenced) have been found between the degree to which a patient engages in emotional experiencing or processing and positive outcomes (Abbass, Town, Ogrodniczuk, Joffres, & Lilliengren, 2017; Fisher, Atzil-Slonim, Bar-Kalifa, Rafaeli, & Peri, 2016; Friederich et al., 2017; Johansson, Town, & Abbass, 2014; Kramer, Pascual-Leone, Despland, & de Roten, 2015; Town, Abbass, & Bernier, 2013; Town, Salvadori, Falkenström, Bradley, & Hardy, 2017), convergent with findings in humanistic-experiential therapies (Pascual-Leone & Yeryomenko, 2016). A recent meta-analysis suggested that, across psychotherapies and psychiatric disorders, increased expression of emotion by the patient although many of the included studies had unclear temporal precedence between the affective measurement and outcome (Peluso & Freund, 2018). In their transtheoretical conception of the importance of emotional expression and experiencing in psychotherapy, Lane, Ryan, Nadel, & Greenburg (2015) propose that emotional activation of episodic and semantic memory content facilitates the reconsolidation of those memories into new, potentially more adaptive forms. From a psychodynamic perspective, heightened affective experiences in therapy may indicate that a patient is tolerating more affectively charged material, allowing for working through of conflicts and ultimately improvements in reflective functioning. Heightened patient emotional experiencing has been examined as a positive predictor of improvement in a study of intensive short-term psychodynamic therapy for patients with generalized anxiety disorder (Lilliengren, Johansson, Town, Kisely, & Abbass, 2017), but we are not aware of any other such study in anxiety.
Study Hypotheses: Main Effects and Moderators
PFPP’s clinical theory predicts that patient affective engagement is important to exploration of meanings and conflicts surrounding panic and anxiety experiences (Busch et al., 2012). To examine the relationships between early in-session emotional engagement and subsequent changes in symptoms and PSRF, we developed a measure of in-session emotional expression. Emotional expression can be thought of as a broad process marker of engaged emotions, incorporating basic aspects of both emotional experience (i.e., does the patient exhibit non-verbal signs of emotional activation?; McCullough et al., 2003) and processing (i.e., does the patient speak in an identifiable manner about specific, current emotional experiences; Klein, Mathieu, Gendlin, & Kiesler, 1969; Pascual-Leone & Greenburg, 2005)? Levels of emotional expression were assessed in early sessions (2, 5, and 10) of a 24-session PFPP protocol from a two-site randomized controlled trial comparing PFPP to CBT and applied relaxation training for panic (<citation masked>). We hypothesized that patients with higher levels of emotional expression in early PFPP sessions would experience greater symptom and PSRF improvement subsequent to the process-measured sessions. Moreover, we examined both overall patient emotional expression and expression of specific emotional states, to help determine whether patient engagement with particular affects is especially important to treatment process (e.g., grief; anger) or potentially deleterious to treatment (e.g., anxiety in-session, as might be predicted by psychodynamic conflict models).
Moderators.
Although many psychotherapy processes are thought of as universally positive (e.g., the therapeutic alliance), it may be that some processes are more important in some psychotherapies, relative to others. Also, the same process, depending on traits that can capture an aspect of specific functioning relating to affect, may yield strong positive effects in some patients, little effect in others, and negative effects in still others (cf. Lorenzo-Luaces et al., 2017). We hypothesized that patient personality disorder traits related to constrained (obsessive-compulsive personality disorder; OCPD) versus heightened (borderline personality disorder; BPD) affect would moderate the relationship between emotional expression and symptom improvement.
A psychodynamic conception of OCPD might focus on OCPD patients’ tendency to intellectualize emotional experiences (Caligor, Kernberg, & Clarkin, 2007; Summers & Barber, 2010). The typically theorized repertoire of defense for OCPD patients emphasizes focus on cognition and circumstance over affects (e.g., intellectualization; isolation of affect; rationalization); a strong need for control, order, and perfection defends against the dangers of experiencing and acting on affect and wishes that feel destabilizing. Relative to psychiatrically healthy individuals, OCPD patients report being less accepting of their emotions, less clear about what their emotions mean, and more distressed by feeling emotional (Steenkamp, Suvak, Dickstein, Shea, & Litz, 2015). In treatment with OCPD patients, focusing on affect may help to counteract defenses that represent avoidance of emotional conflicts (Barber & Muenz, 1996). We thus hypothesized that patients with more OCPD personality traits as indicated by the SCID-II (First, Gibbon, Spitzer, Williams, & Benjamin, 1997) would show a stronger relationship between early levels of emotional expression and later symptomatic improvements, as for these patients emotional expression may particularly indicate a more flexible use of defense in-session, relative to their typical profile.
In contrast, we hypothesized that patients with increasingly more BPD traits would show no or even negative relationships between early emotional expression and later improvements. While BPD is a relatively uncommon comorbidity to PD (Friborg, Martinussen, Kaiser, Overgard, & Rosenvinge, 2013), many patients exhibit elevated BPD pathology. In general and clinical populations, qualifying for even one DSM-defined BPD criterion is uniquely prognostic of significant interpersonal dysfunction and psychosocial disability (Ellison, Rosenstein, Chelminski, Dalrymple, & Zimmerman, 2016; Zimmerman, Chelminski, Young, Dalrymple, & Martinez, 2012), indicating that even non-diagnostic BPD may be clinically relevant. Affective dysregulation is a common if not defining feature of BPD. BPD patients show stronger reactivity to interpersonal events (Santangelo, Bohus, & Ebner-Priemer, 2012), as well as more labile mood around a more negative baseline (Ebner-Priemer et al., 2015), relative to healthy controls and MDD patients. Accordingly, the therapist’s efforts to help patients regulate, understand, and usefully work with difficult-to-comprehend affects has been identified as a common feature across many empirically supported psychotherapies for BPD (Bateman, Gunderson, & Mulder, 2015). For patients with more BPD traits, relatively lower levels of emotional expression in PFPP may reflect successful work by the therapist and patient to contain affect in order to better work with the meanings and circumstances surrounding panic and anxiety (Fonagy & Luyten, 2009). Relatively lower emotional expression may also indicate defensive flexibility among BPD patients, who typically engage in defenses focusing on prominent, moment-to-moment affects (e.g., splitting; acting out; Kramer, de Roten, Perry, & Despland, 2013; Perry, Presniak, & Olson, 2013), such that emotional expression per se may sometimes involve typical defensive processes and not primarily a flexible use of defense or processing of conflict.
Method
Participants
Patients.
The present study is a secondary analysis of patients randomized to the PFPP condition (N = 80) of a two-site randomized controlled trial comparing PFPP, CBT, and applied relaxation training among patients with primary DSM-IV panic disorder with or without agoraphobia. Patients were recruited at <site A> and <site B>. Participants received study treatment gratis. Participants gave informed written consent. Both sites’ institutional review boards approved the protocol, and the study is registered with ClinicalTrials.gov (identifier: <masked>).
Patients were included in the trial if they had one or more weekly spontaneous panic attacks for the month before trial entry, and qualified for DSM-IV diagnosis of primary panic disorder with or without agoraphobia determined as per the ADIS-IV (DiNardo, Brown, & Barlow, 1995). Cross-site agreement on ADIS ratings for panic severity (with a “4” indicating the diagnostic threshold) was excellent (ICC = 1.00; per the norms of Portney & Watkins, 2000). See <masked> for further details.
Non-study psychotherapy was prohibited. Medications were permitted if stable for at least two months at presentation, and were recorded, held constant, and monitored during the trial. Exclusion criteria were: active substance dependence (less than 6 months’ remission), a history of psychosis or bipolar disorder, acute suicidality, and organic mental syndrome. Additional details on trial design, independent evaluator training, and therapy adherence can be consulted in the primary outcome paper (<citation masked>).
Assessment of personality disorder (PersD).
The Structured Clinical Interview for Axis-II disorders (First et al., 1997) was used to assess the presence of PersD criteria and diagnoses as defined by DSM-IV. Trained, independent masters’ level diagnosticians uninformed to treatment condition administered the interviews. Cross-site interrater reliability was excellent for number of OCPD criteria scored as present (ICC[2,1] = 1.00), and moderate for BPD criteria (ICC[2,1] = 0.78).
Therapists.
All therapists were experienced therapists (Ph.D. or M.D.) who were specifically trained in PFPP over the span of a 2-day, 12-hour course. Therapists had an average of 15 years of post-graduate experience (SD = 8.2), and an average of 5 years’ experience in some form of time-limited psychodynamic therapy (SD = 6.3). Therapists participated in monthly group supervision and received regular individual supervision from senior clinicians. For the primary outcome paper, adherence to PFPP was established, and additional information on the number and training of therapists can be found there (<citation masked>).
Outcome Indices
Panic Disorder Severity Scale (PDSS; Shear et al., 1997).
The PDSS is a diagnosis-based, composite, global observer rating of panic disorder severity, with acceptable psychometric properties. The PDSS was administered by trained, master’s-level diagnosticians, uninformed as to treatment condition, based on an interview guide. Interrater reliability on the PDSS was excellent (ICC[2,1] = 0.95). The PDSS was administered five times during treatment: at baseline (Week 0), Week 1, Week 5, Week 9, and termination (Week 12).
Panic-Specific Reflective Functioning (PSRF; Rudden et al., 2006).
PSRF is an interview-based measure that assesses the degree to which patients can recognize the psychological contributions to their panic symptoms. Respondents are queried as to their understanding of panic, how it has changed over time, and whether they notice any concordance between panic and emotional states. Each response is rated for psychological mindedness and complexity, and an overall score is based on item scores. An example of a more impaired PSRF answer might be: “It’s the heat, the heat brings them on” in response to “Why do you think you have panic attacks?”; a less impaired response to that question might be: “I notice that I get them when I am feeling a lack of control in my personal relationships. I fear that others will leave me, or that I may want to leave them.” PSRF narratives were reliably scored by trained raters (ICC[2,1] = 0.80).
Process Measures
Emotional Expression Rating Scale (EERS; <citation masked>).
The EERS is an observer-rated scale developed to assess the degree to which patients are engaged in emotional discourse. It was developed for this investigation by two study authors, with reference to prior attempts to rate emotions in-session (e.g., Klein et al., 1969; McCullough et al., 2003). The measure was designed to be relatively atheoretical and broadly descriptive rather than reflecting a particular perspective on what constitutes (for example) adaptive emotional experience or deep emotional processing. Contrasted with other scales, it was designed for ease of use by individuals with less theoretical or clinical training. To incorporate information on both verbal and non-verbal indicators of emotional expression, only sessions with usable video recordings could be sampled. Ratings were made every five minutes to allow for a more precise and potentially valid assessment of patient emotion expression relative to whole-session ratings, and to collect temporal information about development of emotional responses throughout a session. Raters made both an omnibus rating for overall emotional expression, and ratings for 4 broad emotion categories.
The primary rating concerns a patient’s overall emotional expression, which is rated on a 0 to 5 scale. Higher scores are dependent on the peak of emotional intensity during the rated segment, but also on the duration of non-neutral emotional expressivity. A score of 0 indicates no notable emotional expression, or a relatively neutral or flat affective state. A score of 2 indicates a low-to-medium but clear presence of emotional expression lasting more than a few seconds, up to a minute, with use of affectively charged language or verbal statements of feeling, and non-verbal indicators such as choking up, tearing up, emphatic gestures, muscular tension, smiling, or physical agitation/restlessness. Scores of 4 and 5 indicate a high, unconstrained peak affective arousal with sustained emotional expression across the majority of the rated segment. Ratings were made for emotional expression within-session, and not when a patient reported how they were feeling in the past, with no clear indication that they are currently feeling that particular emotion (e.g., reporting with a neutral tone that they were sad when a parent died). In Table 2, examples of transcripts from higher-versus lower-emotional expression therapy sessions from the present study are given.
Table 2.
Example transcripts from sessions rated high/low in emotional expression
| High Emotional Expression Transcript (Session Average 1.75) |
Low Emotional Expression Transcript (Session Average 0.28) |
|---|---|
| T: Is your boyfriend being on this nocturnal schedule and maybe not finishing his program a worry for you? I feel that you’re frustrated and anxious in an immediate sense of what’s going on right now, but there’s some concern about getting married, proceeding with that. | P: It’s awful. I hate saying goodbyes. I hate driving my son to the station to say goodbye. I hate driving my sister to say goodbye. <neutral tone and facial expression> |
| T: How does it make you feel when you do that? | |
| P: No, I mean, the pros outweigh the cons < quiet, restrained tone of voice>. | P: I guess, and this is just pure speculation, but I guess… |
| T: I think maybe part of what might go on inside is that thinking about these concerns is at times a scary, anxiety-provoking thought… because you want to proceed with marrying him, and the pros outweigh the cons, but he’s not taking care of himself. | T: What is it that you feel? / P: Um. / T: Sorry I cut you off. / P: No, that’s fine. It makes me feel anxious, it makes me feel sad, um, it’s just very hard, I don’t like it at all <laughter; smiling incongruously to statement>. |
| T: Just like the way you feel here. | |
| P: Yes… yes, I guess so. <tearing up> Maybe that’s why… I don’t know, I mean, he’s really smart, I just hope that he’ll soon figure what he wants to focus on. I know that in a few years if he didn’t he’d… <begins to fully cry, cries for a few moments>…<therapist offers tissue>. Thank you… | P: When I have tears, they could literally be for you and what you’re going through, they could be for us, or it could be, I don’t know. Because, I mean, there would have to be a thought associated with the emotion. A thought that, I’m assuming, triggered the emotion. <continued neutral tone/expression> And I don’t know what that thought is. I’d like to know what that thought is. But, um, the leaving I don’t like. I don’t like goodbyes. Never liked goodbyes. Well, I don’t know if that’s true, but I don’t like goodbyes. <coded small elevation in Anxiety/Distress from increase in physical agitation and pace of speech, but overall still relatively neutral/flat> |
| T: You’re worried about that, and what might happen to you both if that were to happen. | |
| P: <teary, weepy> I don’t know. He’s such a Type-A perfectionist, I don’t know how he keeps spiraling. I’m so worried about him all the time, it really gets to me. I’m really sad… <coded elevation in Grief/Sadness> |
Note. Both transcripts are adapted from sessions from the trial, particularly Session 10, for a patient with one of the top 3 ratings for emotional expression at this session versus a patient with one of the bottom 3 ratings for emotional expression. Transcripts have been edited for clarity and to eliminate potentially identifying information.
Expressions of four specific broad categories of emotions were coded, three of which are referenced in the following analyses1
Grief/Sadness: Grief/Sadness referred to the expression of grief, sadness, sorrow, or regret. Raters were trained to distinguish between sadness surrounding (for example) an interpersonal figure, and indistinct depressive distress or self-attack, which was rated as Anxiety/Distress. Nonverbal indicators included tearing up, sad vocal tone, choking up, quavering voice, frowning, and crying. Raters were trained to pay attention to clear verbal expressions of sadness, regret, or loss, or particular expressions such as feelings of closeness and tenderness while talking about a close attachment figure who died or whom they fear may no longer be available to them.
Anger/Assertion: Anger/Assertion made a distinction between anger directed toward an external or interpersonal figure, and anger directed toward the self (e.g., self-attack; self-punishment), which was rated as Anxiety/Distress. Anger/Assertion was rated if patients indicated clear anger, criticized someone, asserted their needs or desires to someone, or voiced wishes for recompense for a past misdeed. Nonverbal markers included patients’ showing angry facial expressions, angry vocal tone, becoming more tense, clenching their fists, gesturing aggressively, or gritting their teeth.
Anxiety/Distress: Anxiety/Distress was intended to be rated when a patient appeared activated with clearly negative feeling and arousal, such as negative global feelings about the self, anxious tension, or experiencing undifferentiated aversive affect. Non-verbal Anxiety/Distress indicators included visible discomfort, fidgeting and drawing inwards, hyperventilating or full panic attack, and uncontrollable negative affect. Verbal indicators included explicit references to feeling anxious or distressed or statements of self-attack and hopelessness.
Correlations between emotion ratings on a per-5 minute basis indicated independence of the specific emotions (see Supplemental Table 1).2
A total of 15 undergraduate psychology majors were trained on this measure by study authors <masked>. Raters were trained by rating sessions not used in this investigation until they reliably rated within one point of the trainers. Weekly-to-biweekly anti-drift sessions were held to maintain reliability and discuss rating challenges. Raters were uninformed to patient outcomes and other study patient data. Videotapes were coded in a random order, and the average score between three raters was used for all analyses.
Interrater reliability (Shrout & Fleiss, 1979) as calculated in a linear mixed model (Bates et al., 2017) was good to moderate per-5 minutes for all emotions (ICC [2,3] Overall = 0.74, Grief/Sadness = 0.71, Anger/Assertion = 0.76, Anxiety/Distress = 0.66).
Statistical Analyses
All analyses were conducted in the R statistical computing language (R Core Team, 2017). All primary analyses were run using robust regressions as implemented in the R package “Robustbase” (Maechler et al., 2016). Given the effective sample size (n = 44), robust regression was selected over standard regression for its superior properties of robustness against multivariate outliers and deviation from homoscedasticity (Huber & Ronchetti, 2009). Semi-partial correlation effect sizes (sr) were estimated for parameters of interest.
Missing data.
In the parent clinical trial, a not missing at random (NMAR) pattern of treatment dropout was detected, such that patients with worse PDSS symptom trajectories were more likely to terminate from treatment prematurely <citation masked>. When outcomes for treatment noncompleters are imputed in the NMAR context, imputation and other missing data methods can lead to biased estimates and confidence intervals (Graham, 2009). As such, only individuals who provided data up to Week 9 (the 4th assessment) were eligible for inclusion (n = 65; 81.3% of the intent-to-treat sample). Moreover, due to the need for video to rate nonverbal indicators of emotional expression, only individuals with videotaped sessions (rather than audio backups) were used. The final sample size having videotaped sessions was n = 44.
Some trial completers were missing one out of three videotaped session due to technical issues or therapist/research assistant error (n = 13, 29.5% of the reduced sample). In contrast to noncompleters, process ratings for completers missing a video-recording of a session can be presumed to be missing at random in relation to panic symptom outcomes (Rubin & Little, 2002), and psychotherapy process ratings have been imputed in past investigations (Keefe, Solomonov, et al., 2018; Lorenzo-Luaces et al., 2017). Random forest imputation (Stekhoven & Bühlmann, 2011) was used to impute missing data for completers. For this dataset, a normalized root mean square error of prediction was estimated at 0.12, indicating that imputation accuracy was estimated to be more than adequate (Stekhoven & Bühlmann, 2011).
Analytic strategy.
Using robust linear regressions, the average level of overall emotional expression between Sessions 2, 5, and 10 (i.e., three sessions between baseline and Week 5) was used to predict subsequent change in PDSS-measured panic symptomatology between Week 5 and treatment termination (Week 12). We also analyzed PSRF as a secondary outcome. Because site differences were detected in the parent trial (<citation masked>), we explored whether site moderated focal effects for this and all subsequently described analyses at a significance of at least p <.10. Control covariates in each regression included the baseline value for either outcome, and the degree of change in the variable of interest that occurred between baseline and Week 5 (i.e., during the measurement of emotional expression). In addition, two planned analyses of moderators of the relationship between average emotional expression and PDSS symptom improvement were conducted: baseline SCID-II OCPD criteria, and SCID-II BPD criteria.
We also performed two secondary, exploratory analyses. First, for both PDSS and PSRF change, we examined whether any of three specific types of emotional expression (i.e., Grief/Sadness, Anger/Assertion, Anxiety/Distress) were predictive of subsequent change. Second, in the context of recent debates about the degree to which stable therapy process across sessions merely reflects trait-like features of patients (Falkenström, Finkel, Sandell, Rubel, & Holmqvist, 2017), we examined whether having emotional expression at Session 10 greater than one’s average across Sessions 2, 5, and 10 predicted subsequent symptom change (i.e., a term reflecting Session 10 minus the average of all sessions). This analysis also simultaneously controlled for average emotional expression within the same model.
Results
Descriptive Statistics
The average patient in this study had a baseline PDSS score of 13.8 (range 9 to 20), considered to be in the moderately-ill severity range for patients with comorbid agoraphobia (Furukawa et al., 2009). Other patient demographics and clinical information can be found in Table 1.
Table 1.
Descriptive Data for Baseline Characteristics and for Symptom Change
| Baseline Measure | Mean (SD) or # (%) |
|---|---|
| Baseline PDSS | 13.8 (2.9) |
| Baseline to Week 5 PDSS Change | −3.9 (4.0) |
| Week 5 to Termination PDSS Change | −2.9 (2.9) |
| Baseline PSRF | 3.3 (1.1) |
| Baseline to Week 5 PSRF Change | 0.9 (1.4) |
| Week 5 to Termination PSRF Change | 0.0 (1.2) |
| SDS | 16.9 (6.1) |
| HAM-D | 10.4 (3.8) |
| Agoraphobia Diagnosis | 35 (79.5%) |
| Age | 37.8 (14.0) |
| Gender (Female) | 31 (70.5%) |
| Concurrent Psychopharmacology | 12 (27.3%) |
| Age of Panic Onset (years) | 26.6 (11.2) |
| SCID-II OcPD Criteria | 2.1 (1.7) |
| SCID-II BPD Criteria | 1.0 (1.7) |
Note. HAM-D = Hamilton Rating Scale for Depression; IIP = Inventory of Interpersonal Problems; PDSS = Panic Disorder Severity Scale; SCID-II = Structured Clinical Interview for the Diagnosis of Axis-II Disorders; SDS = Sheehan Disability Scale
Descriptive statistics on mean levels of emotional expression across each session can be found in Supplemental Table 2. We also examined the consistency of emotional expression across measured sessions, using a linear mixed model framework (Bates et al., 2017; Supplemental Table 3), which revealed that the majority of variance in emotional expression was not trait-like across sessions.
PDSS Symptom Change
Patients who had higher levels of emotional expression across the three sampled sessions (2, 5, and 10) experienced more panic symptom improvement subsequent to Session 10 (B = −3.10 [95% CI: −5.27 to −0.93], SE = 1.07, t[40] = −2.88, p = 0.006, sr = 0.31), controlling for baseline panic symptoms and prior change in panic symptoms.
In a secondary analysis, having emotional expression at Session 10 that was higher than one’s average emotional expression across Sessions 2, 5, and 10 was also predictive of having more symptom improvement subsequent to Session 10 (B = −3.58 [95% CI: −5.78 to −1.37], SE = 1.09, t[39] = −3.28, p = 0.002, sr = 0.38). This was true even though the model also controlled for a patient’s average level of emotional expression, which remained itself a statistically significant predictor of subsequent panic symptom improvements (B = −2.90 [95% CI: −4.70 to −1.09], SE = 0.89, t[39] = −3.24, p = 0.002, sr = 0.29).3
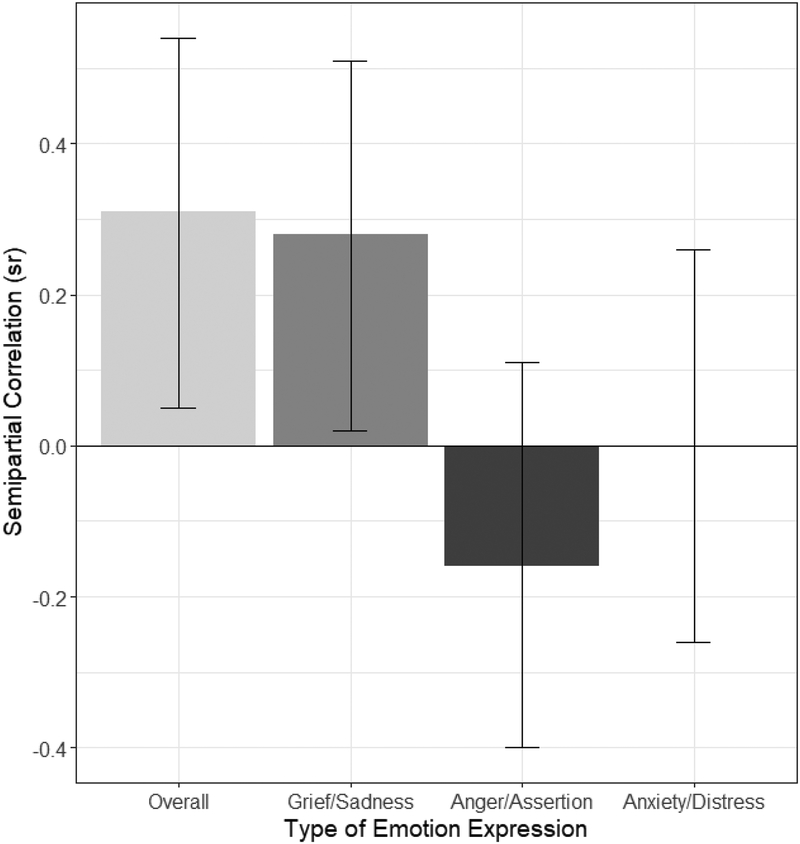
We further explored whether any specific type of emotional expression was particularly responsible for this relationship, employing a model simultaneously including as predictors average expression levels of grief/sadness, anger/assertion, and anxiety/distress. Patients who expressed more grief/sadness across the sampled sessions had superior subsequent panic outcomes (B = −5.25 [95% CI: −9.38 to −1.14], SE = 2.18, t[38] = −2.41, p = 0.021, sr = 0.28), while neither anger/assertion (B = 2.43 [95% CI: −1.61 to 6.46], SE = 1.93, t[38] = 1.25, p = 0.217, sr = −0.16) nor anxiety/distress (B = 0.01 [95% CI: −5.37 to 5.40], SE = 2.68, t[38] = 0.01, p = 0.996, sr = 0.00) were significant predictors of symptom change. Figure 1 displays these relationships for overall emotional expression and specific emotions.
Figure 1.
Estimated effect sizes for the relationship between the average level of emotion expression across sessions 2, 5, and 10, and subsequent improvement in panic symptoms as measured by the PDSS. Positive semipartial correlations indicate that higher levels of expression are associated with more subsequent symptom improvement. Bars are 95% confidence intervals.
Personality Moderators of Symptom Change
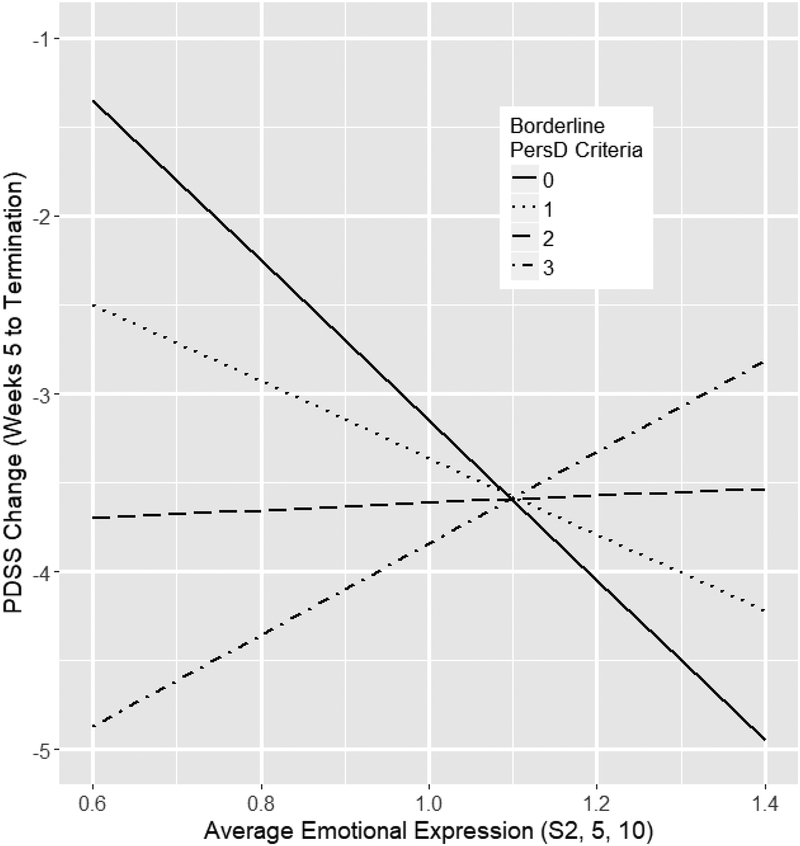
Next, we examined our moderation hypotheses as to whether BPD and OCPD personality traits would predict a smaller or greater relationship (respectively) between emotional expression and symptom improvements. Consistent with our hypothesis, the number of baseline SCID-II BPD criteria a patient met significantly interacted with overall emotional expression, such that meeting more BPD criteria attenuated the relationship between overall emotional expression and symptom improvement (B = 2.36 [95% CI: 1.09 to 3.63], SE = 0.63, t[38] = 3.76, p <.001, sr = 0.29). Unpacking this continuous interaction using the Johnson-Neyman technique, we found that patients meeting 1 or no BPD criteria evidenced a significant, positive relationship between emotional expression and symptom improvement (sr = 0.33, p = 0.003; see Figure 2). By contrast, there was a nonsignificant, negative relationship between emotional expression and improvement for patients meeting 2 or more BPD criteria (sr = −0.20, p = 0.062). Thus, patients qualifying for a relatively low number of DSM-defined BPD criteria (2 or more) exhibited no beneficial (or potentially even a negative) relationship to degree of emotional expression compared to those with minimal (1) or no BPD pathology, who had a significant, positive relationship.
Figure 2.
Estimated change in panic symptoms as measured by the PDSS between Weeks 5 to Termination (Week 12), as a function of the average overall emotional expression between sessions 2, 5, and 10, and their interaction with the number of SCID-II borderline personality disorder criteria a patient met at baseline. Increasingly negative values represent greater predicted symptom improvement. All regression variables not displayed in the figure were set to the sample means.
However, as concerned SCID-II OCPD criteria, there was a significant interaction between OCPD criteria, emotional expression, and site (p = 0.036). At Site A, the hypothesized interaction was obtained, whereby patients meeting more OCPD criteria at baseline had an increasingly positive relationship between early emotional expression and subsequent symptom improvement (B = −4.48 [95% CI: −7.72 to −1.24], SE = 1.59, t[34] = −2.81, p = 0.008, sr = 0.34). At Site B, there was no significant interaction (B = 0.48 [95% CI: −2.11 to 3.07], SE = 1.27, t[34] = 0.38, p = 0.707, sr = −0.04). Thus, OCPD criteria cannot be considered a clear moderator.
Panic-Specific Reflective Functioning Change
Mirroring the model analyzing symptomatic outcomes, patients with a higher level of emotional expression across the three sessions had greater gains in PSRF subsequent to the measured sessions (B = 0.93 [95% CI: 0.03 to 1.83], SE = 0.45, t[40] = 2.10, p = 0.042, sr = 0.23), controlling for their baseline PSRF and early PSRF changes. Neither the number of OCPD (B = 0.42 [95% CI: −0.27 to 1.11], t[38] = 1.24, p = 0.223, sr = 0.21) nor BPD criteria (B = −0.42 [95% CI: −1.12 to 0.27], t[38] = −1.23, p = 0.226, sr = 0.20) a patient met significantly moderated this relationship.
We examined whether any specific type of emotional expression drove this relationship. In this case, there were no specific significant relations as concerned expression of grief/sadness (B = 1.43 [95% CI: −1.62 to 4.48], SE = 1.51, t[38] = 0.95, p = 0.350, sr = 0.15), anger/assertion (B = 1.20 [95% CI: −0.54 to 2.95], SE = 0.86, t[38] = 1.40, p = 0.170, sr = 0.17), or anxiety/distress (B = −0.15 [95% CI: −2.02 to 1.71], SE = 0.92, t[38] = −0.17, p = 0.869, sr = −0.02).
Discussion
In panic-focused psychodynamic psychotherapy, patients who engage in more emotional expression over the course of the first five weeks of therapy have superior symptomatic outcomes across the remainder of the treatment. For interpretive context, just under half of the average symptomatic change occurs after the first five weeks of treatment (see Table 1). Our results are convergent with findings from psychodynamic psychotherapy process studies investigating other operationalizations of emotional processing or experiencing in-session (Abbass et al., 2017; Fisher et al., 2016; Friederich et al., 2017; Johansson et al., 2014; Kramer et al., 2015; Town et al., 2013; Town, Salvadori et al., 2017). These findings expand the literature on emotions in psychodynamic therapy to the context of short-term manualized panic disorder-focused treatment, and provide further evidence that emotional expression precedes rather than contemporaneously occurs with improvements. This study thus provides relatively stronger evidence that emotional expression is a therapy process that may help give rise to good outcomes, rather than being merely a product of symptomatic alleviation.
Notably, early emotional expression also predicted subsequent gains in PSRF, which were found in the broader trial to predict subsequent panic improvements (Barber et al., under review). Emotional expression may be reflective of mentalization in-session of emotional meanings and conflicts contributing to instances of panic and anxiety. As the patient works to tolerate and understand affectively-laden meanings and conflicts, they are expected to be able to engage with them rather than feel them as undifferentiated anxiety or frightening somatic fantasy (Busch et al., 2012). Emotionally working through conflict may also serve to detoxify certain affects, meanings, or wishes for patients, which may be typically experienced as distressing, dangerous, uncontrollable, or guilt-provoking to the point of having a panic attack.
Clinically, our results suggest that emotionally flat or withdrawn discussions of the contributors and contexts of anxiety are unlikely to help a patient substantively experience and work with these meanings in psychodynamic therapy. Concordantly, past work has found that psychodynamic interventions focused on expression of difficult-to-express affects appear to be correlated with improvements in anxiety (Pitman et al., 2014; Pitman et al., 2017), and that anxiety patients rate as especially helpful attempts to explore unexpressed/avoided feelings in-session (Glock, Hilsenroth, & Curtis, 2018). The presence versus absence of emotional expression may help a therapist distinguish between a patient’s compliant or pseudo-insightful (intellectualized) acquiescence to the therapist’s attempts to explore the emotional underpinnings of their anxiety, versus productive, affective engagement in the therapeutic process.
In our exploratory analyses concerning which specific emotions contribute to the observed relationships, only expression of grief/sadness significantly predicted subsequent symptom outcomes. PFPP’s clinical theory emphasizes the degree to which actual or prospective attachment losses can precipitate panic disorder itself, often because patients have difficulty acknowledging the emotional importance of the loss (Busch et al., 2012; Klass et al., 2009; Milrod, Leon, & Shear, 2004). Expression of grief/sadness may sometimes reflect patients engaging with and becoming more tolerant of the true emotional impact of the actual or feared loss.
Anger may not have emerged as a significant predictor despite its role in psychodynamic models of panic (Busch et al., 1999; Busch et al., 2012), as anger may sometimes have been directed toward figures regarding whom the patient already feels comfortable experiencing anger. In PFPP, anger is conceptualized as being repressed particularly when the patient is worried that his/her anger will provoke separation/retaliation and hence loss of an ambivalently-held attachment figure (Busch et al., 1999; Busch et al., 2012; Rudden et al., 2003). As such, access to and expression of grief/sadness about loss that might be imagined to emerge as a result of angry feelings might indicate a deeper processing of the underlying conflict. Expression of disavowed or unconscious anger, for instance regarding attachment figures, may be found to have stronger relationships to outcomes compared to general anger. Interestingly, in contrast with our findings, in an investigation of intensive short-term dynamic psychotherapy for treatment-resistant major depressive disorder, experiencing of anger but not grief was related to better depression outcomes (Town, Falkenstrom, Abbass, & Stride, 2017; Town, Salvadori et al., 2017). It may be that difficulties tolerating particular, core emotions are more common to specific symptoms.
Finally, anxiety/distress in-session was nonpredictive of outcome. In PFPP, presence of anxiety in-session is not considered negative per se, as for example the patient may feel anxious because the therapeutic work is addressing important conflicted material, and that anxiety can be dealt with in real-time (Busch et al., 2012). From the perspective of PFPP, a therapy that transpires without affects sometimes considered “negative” or “inhibitory” (McCullough et al., 2003) may reflect that particular important dynamics are not being brought into the treatment by the patient or pursued by the therapist. Our metric of Overall emotional expression incorporated all deviations from a neutral emotional state—which could include so-called negative/inhibitory affects—in part to reflect our interest in emotional engagement in treatment writ large relative to therapies in which comparatively minimal affect was mobilized in-session. Other investigations with different goals may choose to use a modified version of the EERS explicitly excluding Anxiety/Distress codes from consideration in the Overall score, or other metrics that attempt to explicitly distinguish negative/inhibitory affects, such as the Achievement of Therapeutic Objectives Scale (McCullough et al., 2003).
We also examined whether personality disorder traits theoretically related to constrained (OCPD) or heightened (BPD) emotional expression moderated the relationship between emotional expression and symptom change. OCPD traits only moderated the predictive value of emotional expression at one of the two treatment sites, such that perhaps unmeasured differences in process or patient population further affected this relationship—for instance, patients at Site B in the trial were much more likely to be on psychotropic medications and had a significantly higher number of medication classes taken (Milrod et al., 2016). On the other hand, the presence of elevated BPD traits diminished the relationship between emotional expression and symptom improvements. With patients meeting relatively more BPD criteria (>1), the PFPP therapist may wish to focus on helping a patient slow down and contain their strong affects to better work with the meanings giving rise to powerful emotional experiences. Of note, meeting relatively more subthreshold BPD criteria per se was not a negative prognostic indicator for PFPP patients in this trial and in fact BPD symptoms improved more in PFPP than in CBT in this study (Keefe, Milrod, Gallop, Barber, & Chambless, 2018), suggesting that these patients can benefit from PFPP, given therapeutic processes that are tailored to their needs. However, few patients in this study met SCID II criteria for a full comorbid BPD diagnosis, potentially because acute suicidality was an exclusion criterion, limiting our assessments to PD patients with low levels of borderline pathology.
Limitations and future directions
Several patients had one session (of three) unavailable to be rated due to videotape missingness (n = 13, 29.5% of the reduced sample). However, we employed a standard, validated method for imputing missing ratings (Stekhoven & Bühlmann, 2011), and a complete data analysis showed similar results. In addition, our effective sample size was small (n = 44).
In our study, average levels of emotional expression on the level of the session were relatively low (around a 1 on the 5-point scale), with the range of rated values consisting of emotionally flat sessions (mean 0) to heightened but not (consistently) highly activated sessions (mean 2). Our obtained relationships for emotional expression generally do not include representation of consistently high-to-extremely emotional sessions, and it is possible that such consistently high expression would not relate to positive outcomes. There was mixed evidence whether maximum emotional expression rated in a session (rather than average across segments) was predictive of outcomes (see Footnote 2), with a trend level relationship for grief/sadness (cf. Kramer et al., 2015). Emotional expression may also have a different relationship to outcome later in treatment.
Our process measure to assess emotional expression, based on the apparent intensity and duration of expression, consisted of a simpler operationalization of emotional experiencing/processing than other measures used heretofore by psychodynamic and process-experiential researchers. For example, there is compelling evidence that in emotion-focused experiential psychotherapy (Greenberg, 2015), a prototypical sequence of emotional processing moves from feelings of undifferentiated global distress toward feeling self-assertive anger or adaptive, relieving experiences of grief over past hurts and losses (Pascual-Leone, 2017). It could also be that emotional expression at particular moments in therapy—such as discussing specific relationship episodes—may be a stronger marker of good process.
Emotional expression as measured by the EERS also did not attempt to distinguish between more versus less adaptive expressions. We were instead primarily interested in how manifest emotional expression was a marker of good clinical process in this treatment. Defining adaptive versus maladaptive/inhibitory affect in-session is a potentially important but complex task, and different psychodynamic approaches use varying lenses for understanding affect as a treatment mechanism (for a broad survey of heterogeneity in defining adaptiveness of affect in different therapy schools, see the different measures used in the Peluso & Freund et al., 2018 meta-analysis). What is “adaptive” affect may also strongly differ from patient to patient: for many patients entering PFPP, expressing anger to a romantic partner might be a novel experience contra their typical defenses against aggression, whereas for a patient with a more borderline personality organization this same action could more frequently reflect splitting as a defense. To our knowledge, our study is one of the first to examine how patient context (e.g., BPD traits) influences how emotional expression relates to treatment success; such personalized examinations may more specifically elucidate the vagaries of emotional process in-session, even when using scales that aim to identify only adaptive or deep emotional expression.
However, one advantage of our method is that, by definition, for more nuanced emotional experiencing or processing to take place, a basic level of emotional expression must nearly always also be present. Future work on this dataset might use our assay of emotional expression across segments of sessions to orient and focus more detailed research.
This study does not address the question of how a therapist may best affectively engage patients in-session. Process work in psychodynamic therapy indicates that focused confrontation interventions (Town, Hardy, McCullough, & Stride, 2012) or interventions attempting to orient patients to their affects (Ulvenes et al., 2014) tend to be associated with greater emotional experiencing on the part of the patient. Preliminary work in this sample suggests that panic-focused interpretations—found to relate to subsequent outcomes in PFPP (Keefe, Solomonov et al., 2018)—in one segment of treatment may predict higher emotional expression in the next segment of treatment when patients were discussing an attachment relationship (Keefe, Huque et al., 2018). This research is ongoing.
We also did not examine the extent to which patients engaged in emotional expressions in the CBT and applied relaxation therapies in the trial. In CBT for depression, some studies report that emotional processing in-session may predict better post-treatment outcomes (Aafjes-van Doorn & Barber, 2017), but the role of emotional processing and experiencing is less commonly explored in this family of treatments. In CBT for panic, we might expect emotional expression to be unrelated or positively related to treatment outcomes (e.g., restructuring “hot cognitions”; intensely engaging in interoceptive exposure). For applied relaxation, emotional expression may have a negative relationship to outcomes, given the goal of in-session progressive relaxation. Future work could apply the EERS or other experiencing scales to less affect-focused psychotherapies for panic.
Finally, in psychotherapy research, there has been increasing attention on distinguishing a patient’s tendency to have a given process score across all sessions (i.e., the “between-patients” component) from within-patient changes in process scores, accounting for their average levels of that process (Falkenström et al., 2017). Our secondary analysis partially addresses this critique, suggesting that having higher than one’s average level of emotional expression (Sessions 2, 5, 10) at Session 10 predicted superior subsequent symptom improvement, even when simultaneously modeling the predictive value of one’s average (i.e., “between-patients”) emotional expression. This provides limited evidence that, even among patients who have a relatively higher level of emotional expression across their early therapy, emotional expression over one’s typical level at a later session is positively prognostic of symptom improvement. Moreover, the majority of variance in emotional expression was not trait-like and consistent across patient sessions, indicating that it is less likely (though not impossible) that the “between-patients” component of emotional expression is primarily driving the observed relations. On the other hand, consistently high levels of a particular process, such as emotional expression, may also reflect specific work within a unique therapeutic dyad, such that the same patient working with a different or more/less skillful therapist would not show such a pattern.
Conclusion
Emotional expression in short-term psychodynamic treatment of panic disorder early in the course of therapy predicts greater symptomatic improvements later in treatment, possibly through encouraging insight into the emotional meanings and conflicts surrounding episodes of panic and anxiety. These results require replication.
Supplementary Material
Clinical Impact Statement.
Question:
Does patient in-session emotional expression in an anxiety-focused psychodynamic psychotherapy facilitate symptom relief and developing the capacity to understand the psychological meanings of symptoms?
Findings:
Degree of patient emotional expression across three early sessions of panic-focused psychodynamic therapy predicted higher panic symptom improvement and symptom-specific mentalizing improvements subsequent to those early sessions.
Meaning:
Therapeutically facilitating a patient’s ability to affectively explore and engage with meanings and conflicts surrounding symptoms may be a part of good process in panic-focused psychodynamic therapy.
Next Steps:
Emotional engagement at particular moments, such as exploration of attachment-related relationship episodes and fantasies, may be particularly important in this treatment.
Acknowledgements
We would like to thank our undergraduate coders for their time and skill in making the emotional expression ratings in this study: Amanda Izes, Brianna Owairu, Erin Kim, Ian Fiedler, Ilana Liss, Kay Gottlieb, Liam McGrother, Meghana Nallerja, Morgan Wu, Syed Aajmain, Stephen Metas, Tanya Datta, Taylor McCorkle, Tara Rajagopal, and Victoria Rio. We would also like to thank Dr. Nili Solomonov for statistical consultation, and Mary Minges and Serena Chen for helping provide relevant clinical transcripts from the clinical sample.
Footnotes
Positive Affect was rarely rated as present and had low variance, and consequently we did not analyze these scores.
One reason Overall ratings were made in addition to specific codes was in order to capture all deviations from a neutral emotional tone even if they were not covered by the specific codes. Another reason was to account for the fact that adding together single codes might not correctly relate to the peak intensity or duration of emotionality in the segment (e.g., three specific emotions getting a “1” rating could indicate that the total Overall duration of non-neutral emotionality truly met criteria for a “1,” or that the patient expressed several different non-neutral affects over a long enough duration to potentially merit a “2”).
A reviewer for this article expressed an interest in whether the patient’s maximum expression score attained in a given session was as predictive of improvement as their average score for the whole session, and they requested we perform such an exploratory analysis. In this analysis, neither the patient’s average maximum overall expression score (t[40] = −1.02, p = 0.314) nor their maximum grief/sadness expression score (t[40] = 1.83, p = 0.075) attained statistical significance. This may suggest that presence of a single, relatively expressive 5-minute period in a PFPP session is not as strong a predictor of outcome as taking into account expression across the whole of the session. However, there was a significant, positive relationship with improvement when analyzing the relationship of maximum overall expression at Session 10 (t[39] = 3.10, p = 0.004), controlling for the patient’s typical maximum expression (t[39] = 1.25, p = 0.219). Nevertheless, this analysis suffers from limited range (possible values 0–5, with few 0s, 4s, and 5s) and should be interpreted with caution.
Contributor Information
John R. Keefe, University of Pennsylvania
Zeeshan M. Huque, University of Pennsylvania
Robert J. DeRubeis, University of Pennsylvania
Jacques P. Barber, Adelphi University
Barbara L. Milrod, Weill Cornell Medical College
Dianne L. Chambless, University of Pennsylvania
References
- Aafjes-van Doorn K, & Barber JP (2017). Systematic Review of In-Session Affect Experience in Cognitive Behavioral Therapy for Depression. Cognitive Therapy and Research, 41(6), 807–828. doi: 10.1007/s10608-017-9865-6 [DOI] [Google Scholar]
- Abbass A, Town J, Ogrodniczuk J, Joffres M, & Lilliengren P (2017). Intensive Short-Term Dynamic Psychotherapy Trial Therapy: Effectiveness and Role of “Unlocking the Unconscious”. The Journal of Nervous and Mental Disease, 205(6), 453–457. doi: 10.1097/nmd.0000000000000684 [DOI] [PubMed] [Google Scholar]
- Barber JP, & Muenz LR (1996). The role of avoidance and obsessiveness in matching patients to cognitive and interpersonal psychotherapy: empirical findings from the treatment for depression collaborative research program. J Consult Clin Psychol, 64(5), 951–958. [DOI] [PubMed] [Google Scholar]
- Bateman AW, Gunderson J, & Mulder R (2015). Treatment of personality disorder. Lancet, 385(9969), 735–743. doi: 10.1016/s0140-6736(14)61394-5 [DOI] [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B, Walker S, Christensen RHB, Singmann H, … Green P (2017). lme4: Linear Mixed-Effects Models using ‘Eigen’ and S4 (Version 1.1–13): Comprehensive R Archive Network. Retrieved from https://cran.r-project.org/web/packages/lme4/index.html
- Beutel ME, Scheurich V, Knebel A, Michal M, Wiltink J, Graf-Morgenstern M, … Subic-Wrana C (2013). Implementing panic-focused psychodynamic psychotherapy into clinical practice. Canadian journal of psychiatry, 58(6), 326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blagys MD, & Hilsenroth MJ (2000). Distinctive Features of Short-Term Psychodynamic-Interpersonal Psychotherapy: A Review of the Comparative Psychotherapy Process Literature. Clinical Psychology: Science and Practice, 7(2), 167–188. doi: 10.1093/clipsy.7.2.167 [DOI] [Google Scholar]
- Boswell JF, Farchione TJ, Sauer-Zavala S, Murray HW, Fortune MR, & Barlow DH (2013). Anxiety Sensitivity and Interoceptive Exposure: A Transdiagnostic Construct and Change Strategy. Behavior Therapy, 44(3), 417–431. doi: 10.1016/j.beth.2013.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Busch FN, Milrod BL, Rudden M, Shapiro T, Singer M, Aronson A, & Roiphe J (1999). Oedipal Dynamics in Panic Disorder. J Am Psychoanal Assoc, 47(3), 773–790. doi: 10.1177/00030651990470030401 [DOI] [PubMed] [Google Scholar]
- Busch FN, Milrod BL, Singer MB, & Aronson AC (2012). Manual of panic focused psychodynamic psychotherapy - extended range (Vol. 36). New York, NY: Routledge. [Google Scholar]
- Busch FN, Shear MK, Cooper AM, Shapiro T, & Leon AC (1995). An empirical study of defense mechanisms in panic disorder. Journal of Nervous and Mental Disease, 183(5), 299–303. doi: 10.1097/00005053-199505000-00004 [DOI] [PubMed] [Google Scholar]
- Calati R, Oasi O, De Ronchi D, & Serretti A (2010). The use of the defence style questionnaire in major depressive and panic disorders: A comprehensive meta-analysis. Psychology and Psychotherapy: Theory, Research and Practice, 83(1), 1–13. doi: 10.1348/147608309X464206 [DOI] [PubMed] [Google Scholar]
- Caligor E, Kernberg OF, & Clarkin JF (2007). Handbook of dynamic psychotherapy for higher level personality pathology (1st ed). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Clark DM, Salkovskis PM, Öst L-G, Breitholtz E, Koehler KA, Westling BE, … Gelder M (1997). Misinterpretation of body sensations in panic disorder. Journal of Consulting and Clinical Psychology, 65(2), 203–213. doi: 10.1037/0022-006X.65.2.203 [DOI] [PubMed] [Google Scholar]
- Diener MJ, Hilsenroth MJ, & Weinberger J (2007). Therapist Affect Focus and Patient Outcomes in Psychodynamic Psychotherapy: A Meta-Analysis. American Journal of Psychiatry, 164(6), 936–941. doi: 10.1176/ajp.2007.164.6.936 [DOI] [PubMed] [Google Scholar]
- Ebner-Priemer UW, Houben M, Santangelo P, Kleindienst N, Tuerlinckx F, Oravecz Z, … Kuppens P (2015). Unraveling affective dysregulation in borderline personality disorder: a theoretical model and empirical evidence. J Abnorm Psychol, 124(1), 186–198. doi: 10.1037/abn0000021 [DOI] [PubMed] [Google Scholar]
- Ellison WD, Rosenstein L, Chelminski I, Dalrymple K, & Zimmerman M (2016). The Clinical Significance of Single Features of Borderline Personality Disorder: Anger, Affective Instability, Impulsivity, and Chronic Emptiness in Psychiatric Outpatients. J Pers Disord, 30(2), 261–270. doi: 10.1521/pedi_2015_29_193 [DOI] [PubMed] [Google Scholar]
- Falkenström F, Finkel S, Sandell R, Rubel JA, & Holmqvist R (2017). Dynamic models of individual change in psychotherapy process research. Journal of Consulting and Clinical Psychology, 85(6), 537–549. doi: 10.1037/ccp0000203 [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, & Benjamin LS (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders, (SCID-II). Washington, DC: American Psychiatric Press. [Google Scholar]
- Fisher H, Atzil-Slonim D, Bar-Kalifa E, Rafaeli E, & Peri T (2016). Emotional experience and alliance contribute to therapeutic change in psychodynamic therapy. Psychotherapy, 53(1), 105–116. doi: 10.1037/pst0000041 [DOI] [PubMed] [Google Scholar]
- Fonagy P, & Luyten P (2009). A developmental, mentalization-based approach to the understanding and treatment of borderline personality disorder. Dev Psychopathol, 21(4), 1355–1381. doi: 10.1017/s0954579409990198 [DOI] [PubMed] [Google Scholar]
- Friborg O, Martinussen M, Kaiser S, Overgard KT, & Rosenvinge JH (2013). Comorbidity of personality disorders in anxiety disorders: a meta-analysis of 30 years of research. J Affect Disord, 145(2), 143–155. doi: 10.1016/j.jad.2012.07.004 [DOI] [PubMed] [Google Scholar]
- Friederich HC, Brockmeyer T, Wild B, Resmark G, de Zwaan M, Dinkel A, … Herzog W (2017). Emotional Expression Predicts Treatment Outcome in Focal Psychodynamic and Cognitive Behavioural Therapy for Anorexia Nervosa: Findings from the ANTOP Study. Psychotherapy and Psychosomatics, 86(2), 108–110. [DOI] [PubMed] [Google Scholar]
- Furukawa TA, Katherine Shear M, Barlow DH, Gorman JM, Woods SW, Money R, … Leucht S (2009). Evidence-based guidelines for interpretation of the Panic Disorder Severity Scale. Depress Anxiety, 26(10), 922–929. doi: 10.1002/da.20532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galderisi S, Mancuso F, Mucci A, Garramone S, Zamboli R, & Maj M (2008). Alexithymia and cognitive dysfunctions in patients with panic disorder. Psychother Psychosom, 77(3), 182–188. doi: 10.1159/000119738 [DOI] [PubMed] [Google Scholar]
- Glock G, Hilsenroth M, & Curtis R (2018). Therapeutic interventions patients with anxiety problems find most helpful: A case for integration? Journal of Psychotherapy Integration, 28(2), 233–241. doi: 10.1037/int0000075 [DOI] [Google Scholar]
- Graham JW (2009). Missing data analysis: making it work in the real world. Annu Rev Psychol, 60, 549–576. doi: 10.1146/annurev.psych.58.110405.085530 [DOI] [PubMed] [Google Scholar]
- Greenberg L (2015). Emotion-focus therapy: Coaching clients to work through their feelings (2nd ed). Washington, DC: American Psychological Association. [Google Scholar]
- Huber PJ, & Ronchetti EM (2009). Robust statistics. Hoboken, NJ: Wiley. [Google Scholar]
- Izci F, Gultekin BK, Saglam S, Koc MI, Zincir SB, & Atmaca M (2014). Temperament, character traits, and alexithymia in patients with panic disorder. Neuropsychiatr Dis Treat, 10, 879–885. doi: 10.2147/ndt.s62647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johansson R, Town JM, & Abbass A (2014). Davanloo’s Intensive Short-Term Dynamic Psychotherapy in a tertiary psychotherapy service: overall effectiveness and association between unlocking the unconscious and outcome. PeerJ, 2, e548. doi: 10.7717/peerj.548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe JR, Huque ZM, DeRubeis RJ, Chambless D, Barber JP, & Milrod BL (2018). A cross-lagged examination of panic-focused psychodynamic interventions and emotional expression in-session. Paper presented at the Society for Psychotherapy Research, Amsterdam, the Netherlands. [Google Scholar]
- Keefe JR, McCarthy KS, Dinger U, Zilcha-Mano S, & Barber JP (2014). A meta-analytic review of psychodynamic therapies for anxiety disorders. Clinical Psychology Review, 34(4), 309–323. doi: 10.1016/j.cpr.2014.03.004 [DOI] [PubMed] [Google Scholar]
- Keefe JR, Milrod BL, Gallop R, Barber JP, & Chambless DL (2018). What is the effect on comorbid personality disorder of brief panic-focused psychotherapy in patients with panic disorder? Depression and Anxiety, 35(3), 239–247. doi: 10.1002/da.22708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefe JR, Solomonov N, Derubeis RJ, Phillips AC, Busch FN, Barber JP, … Milrod BL (2018). Focus is key: Panic-focused interpretations are associated with symptomatic improvement in panic-focused psychodynamic psychotherapy. Psychotherapy Research, 1–12. doi: 10.1080/10503307.2018.1464682 [DOI] [PubMed] [Google Scholar]
- Kipper L, Blaya C, Teruchkin B, Heldt E, Isolan L, Mezzomo K, … Manfro GG (2004). Brazilian Patients with Panic Disorder: The Use of Defense Mechanisms and Their Association with Severity. J Nerv Ment Dis, 192(1), 58–64. doi: 10.1097/01.nmd.0000106001.84359.0f [DOI] [PubMed] [Google Scholar]
- Klass ET, Milrod BL, Leon AC, Kay SJ, Schwalberg M, Li C, & Markowitz JC (2009). Does Interpersonal Loss Preceding Panic Disorder Onset Moderate Response to Psychotherapy? An Exploratory Study. The Journal of clinical psychiatry, 70(3), 406–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein MH, Mathieu P, Gendlin ET, & Kiesler DJ (1969). The experiencing scale: A research and training manual (Vol. 1). Madison, WI: Wisconsin Psychiatric Institute. [Google Scholar]
- Kossowsky J, Pfaltz MC, Schneider S, Taeymans J, Locher C, & Gaab J (2013). The separation anxiety hypothesis of panic disorder revisited: a meta-analysis. Am J Psychiatry, 170(7), 768–781. doi: 10.1176/appi.ajp.2012.12070893 [DOI] [PubMed] [Google Scholar]
- Kramer U, de Roten Y, Perry JC, & Despland J-N (2013). Beyond splitting: Observer-rated defense mechanisms in borderline personality disorder. Psychoanalytic Psychology, 30(1), 3–15. doi: 10.1037/a0029463 [DOI] [Google Scholar]
- Kramer U, Pascual-Leone A, Despland J-N, & de Roten Y (2015). One minute of grief: Emotional processing in short-term dynamic psychotherapy for adjustment disorder. Journal of Consulting and Clinical Psychology, 83(1), 187–198. doi: 10.1037/a0037979 [DOI] [PubMed] [Google Scholar]
- Lane RD, Ryan L, Nadel L, & Greenberg L (2015). Memory reconsolidation, emotional arousal, and the process of change in psychotherapy: New insights from brain science. Behav Brain Sci, 38, e1. doi: 10.1017/s0140525x14000041 [DOI] [PubMed] [Google Scholar]
- Lilliengren P, Johansson R, Town JM, Kisely S, & Abbass A (2017). Intensive Short-Term Dynamic Psychotherapy for generalized anxiety disorder: A pilot effectiveness and process-outcome study. Clinical Psychology & Psychotherapy, 24(6), 1313–1321. doi: 10.1002/cpp.2101 [DOI] [PubMed] [Google Scholar]
- Lorenzo-Luaces L, Driessen E, DeRubeis RJ, Van HL, Keefe JR, Hendriksen M, & Dekker J (2017). Moderation of the Alliance-Outcome Association by Prior Depressive Episodes: Differential Effects in Cognitive-Behavioral Therapy and Short-Term Psychodynamic Supportive Psychotherapy. Behavior Therapy, 48(5), 581–595. doi: 10.1016/j.beth.2016.11.011 [DOI] [PubMed] [Google Scholar]
- Maechler M, Rousseeuw P, Croux C, Todorov V, Ruckstuhl A, Salibian-Barrera M, … diPalma MA (2016). robustbase: Basic Robust Statistics (Version 0.92–7). Retrieved from https://cran.r-project.org/web/packages/robustbase/index.html
- McCarthy KS, & Barber JP (2009). The Multitheoretical List of Therapeutic Interventions (MULTI): Initial report. Psychotherapy Research, 19(1), 96–113. doi: 10.1080/10503300802524343 [DOI] [PubMed] [Google Scholar]
- McCullough L, Larsen AE, Schanche E, Andrews S, Kuhn N, Hurley C, & Wolf J (2003). Achivement of Therapeutic Objectives Scale: ATOS scale. Harvard Medical School. [Google Scholar]
- Milrod B, Chambless DL, Gallop R, Busch FN, Schwalberg M, McCarthy KS, … Barber JP (2016). Psychotherapies for Panic Disorder: A Tale of Two Sites. Journal of clinical psychiatry, 77(7), 927–935. doi: 10.4088/JCP.14m09507 [DOI] [PubMed] [Google Scholar]
- Milrod B, Leon AC, Busch F, Rudden M, Schwalberg M, & Clarkin J (2007). A randomized controlled clinical trial of psychoanalytic psychotherapy for panic disorder. American Journal of Psychiatry, 164, 265–272. [DOI] [PubMed] [Google Scholar]
- Milrod B, Leon AC, & Shear MK (2004). Can interpersonal loss precipitate panic disorder? Am J Psychiatry, 161(4), 758–759. doi: 10.1176/appi.ajp.161.4.758 [DOI] [PubMed] [Google Scholar]
- Milrod B, Markowitz JC, Gerber AJ, Cyranowski J, Altemus M, Shapiro T, … Glatt C (2014). Childhood separation anxiety and the pathogenesis and treatment of adult anxiety. Am J Psychiatry, 171(1), 34–43. doi: 10.1176/appi.ajp.2013.13060781 [DOI] [PubMed] [Google Scholar]
- Parker JD, Taylor GJ, Bagby RM, & Acklin MW (1993). Alexithymia in panic disorder and simple phobia: a comparative study. American Journal of Psychiatry, 150(7), 1105–1107. doi: 10.1176/ajp.150.7.1105 [DOI] [PubMed] [Google Scholar]
- Pascual-Leone A (2017). How clients “change emotion with emotion”: A programme of research on emotional processing. Psychotherapy Research, 1–18. doi: 10.1080/10503307.2017.1349350 [DOI] [PubMed] [Google Scholar]
- Pascual-Leone A, & Greenburg LS (2005). Classification of Affective-Meaning States (CAMS) In Pascual-Leone A (Ed.), Emotional processing in the therapeutic hour: Why “The only way out is through” (pp. 289–366). Toronto, Ontario, Canada: York University. [Google Scholar]
- Pascual-Leone A, & Yeryomenko N (2016). The client “experiencing” scale as a predictor of treatment outcomes: A meta-analysis on psychotherapy process. Psychotherapy Research, 1–13. doi: 10.1080/10503307.2016.1152409 [DOI] [PubMed] [Google Scholar]
- Peluso PR, & Freund RR (2018). Therapist and client emotional expression and psychotherapy outcomes: A meta-analysis. Psychotherapy, 55(4), 461–472. doi: 10.1037/pst0000165 [DOI] [PubMed] [Google Scholar]
- Perry JC, & Bond M (2012). Change in defense mechanisms during long-term dynamic psychotherapy and five-year outcome. Am J Psychiatry, 169(9), 916–925. doi: 10.1176/appi.ajp.2012.11091403 [DOI] [PubMed] [Google Scholar]
- Perry JC, Presniak MD, & Olson TR (2013). Defense Mechanisms in Schizotypal, Borderline, Antisocial, and Narcissistic Personality Disorders. Psychiatry: Interpersonal and Biological Processes, 76(1), 32–52. doi: 10.1521/psyc.2013.76.1.32 [DOI] [PubMed] [Google Scholar]
- Pitman S, Slavin-Mulford J, & Hilsenroth M (2014). Psychodynamic techniques related to outcome for anxiety disorder patients at different points in treatment. J Nerv Ment Dis, 202(5), 391–396. doi: 10.1097/nmd.0000000000000137 [DOI] [PubMed] [Google Scholar]
- Pitman SR, Hilsenroth MJ, Weinberger J, Conway F, & Owen J (2017). Psychotherapy Technique Related to Changes in Anxiety Symptoms With a Transdiagnostic Sample. J Nerv Ment Dis, 205(6), 427–435. doi: 10.1097/nmd.0000000000000689 [DOI] [PubMed] [Google Scholar]
- Portney LG, & Watkins MP (2000). Foundations of clinical research: Applications to practice. New Jersey: Prentice Hall. [Google Scholar]
- R Core Team. (2017). R: A Language and Environment for Statistical Computing (Version 3.4.3). Vienna, Austria: R Foundation for Statistical Computing; Retrieved from https://www.R-project.org/ [Google Scholar]
- Rubin DB, & Little RJA (2002). Statistical analyses with missing data (2nd ed). New York, NY: Wiley. [Google Scholar]
- Rudden M, Busch FN, Milrod B, Singer M, Aronson A, Roiphe J, & Shapiro T (2003). Panic disorder and depression: A psychodynamic exploration of comorbidity. The International Journal of Psychoanalysis, 84(4), 997–1015. doi: 10.1516/VCKY-5EWM-7PT4-LRWJ [DOI] [PubMed] [Google Scholar]
- Rudden M, Milrod B, Target M, Ackerman S, & Graf E (2006). Reflective functioning in panic disorder patients: a pilot study. J Am Psychoanal Assoc, 54(4), 1339–1343. [DOI] [PubMed] [Google Scholar]
- Santangelo P, Bohus M, & Ebner-Priemer UW (2012). Ecological Momentary Assessment in Borderline Personality Disorder: A Review of Recent Findings and Methodological Challenges. Journal of Personality Disorders, 28(4), 555–576. doi: 10.1521/pedi_2012_26_067 [DOI] [PubMed] [Google Scholar]
- Scocco P, Barbieri I, & Frank E (2007). Interpersonal Problem Areas and Onset of Panic Disorder. Psychopathology, 40(1), 8–13. [DOI] [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, … Papp LA (1997). Multicenter collaborative panic disorder severity scale. Am J Psychiatry, 154(11), 1571–1575. doi: 10.1176/ajp.154.11.1571 [DOI] [PubMed] [Google Scholar]
- Shrout PE, & Fleiss JL (1979). Intraclass correlations: uses in assessing rater reliability. Psychol Bull, 86(2), 420–428. [DOI] [PubMed] [Google Scholar]
- Steenkamp MM, Suvak MK, Dickstein BD, Shea MT, & Litz BT (2015). Emotional Functioning in Obsessive-Compulsive Personality Disorder: Comparison to Borderline Personality Disorder and Healthy Controls. J Pers Disord, 29(6), 794–808. doi: 10.1521/pedi_2014_28_174 [DOI] [PubMed] [Google Scholar]
- Stekhoven DJ, & Bühlmann P (2011). MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics, 28(1), 112–118. doi: 10.1093/bioinformatics/btr597 [DOI] [PubMed] [Google Scholar]
- Strauss AY, Kivity Y, & Huppert JD (2018). Emotion Regulation Strategies in Cognitive Behavioral Therapy for Panic Disorder. Behavior Therapy. doi: 10.1016/j.beth.2018.10.005 [DOI] [PubMed] [Google Scholar]
- Subic-Wrana C, Greenberg LS, Lane RD, Michal M, Wiltink J, & Beutel ME (2016). Affective Change in Psychodynamic Psychotherapy: Theoretical Models and Clinical Approaches to Changing Emotions. Z Psychosom Med Psychother, 62(3), 207–223. doi: 10.13109/zptm.2016.62.3.207 [DOI] [PubMed] [Google Scholar]
- Summers RF, & Barber JP (2010). Psychodynamic therapy: A guide to evidence-based practice. New York, NY: Guilford Press. [Google Scholar]
- Town J, Falkenstrom F, Abbass A, & Stride C (2017). Predicting change in depression with Intensive Short-Term Dynamic Psychotherapy for Treatment Resistant Depression. Paper presented at the Society for Psychotherapy Research, Toronto, Ontario. [Google Scholar]
- Town JM, Abbass A, & Bernier D (2013). Effectiveness and cost effectiveness of Davanloo’s intensive short-term dynamic psychotherapy: does unlocking the unconscious make a difference? Am J Psychother, 67(1), 89–108. [DOI] [PubMed] [Google Scholar]
- Town JM, Hardy GE, McCullough L, & Stride C (2012). Patient affect experiencing following therapist interventions in short-term dynamic psychotherapy. Psychother Res, 22(2), 208–219. doi: 10.1080/10503307.2011.637243 [DOI] [PubMed] [Google Scholar]
- Town JM, Salvadori A, Falkenström F, Bradley S, & Hardy G (2017). Is affect experiencing therapeutic in major depressive disorder? Examining associations between affect experiencing and changes to the alliance and outcome in intensive short-term dynamic psychotherapy. Psychotherapy, 54(2), 148–158. doi: 10.1037/pst0000108 [DOI] [PubMed] [Google Scholar]
- Tull MT, Jakupcak M, & Roemer L (2010). Emotion Suppression: A Preliminary Experimental Investigation of Its Immediate Effects and Role in Subsequent Reactivity to Novel Stimuli. Cogn Behav Ther, 39(2), 114–125. doi: 10.1080/16506070903280491 [DOI] [PubMed] [Google Scholar]
- Tull MT, & Roemer L (2007). Emotion regulation difficulties associated with the experience of uncued panic attacks: evidence of experiential avoidance, emotional nonacceptance, and decreased emotional clarity. Behavior Therapy, 38(4), 378–391. doi: 10.1016/j.beth.2006.10.006 [DOI] [PubMed] [Google Scholar]
- Ulvenes PG, Berggraf L, Wampold BE, Hoffart A, Stiles T, & McCullough L (2014). Orienting patient to affect, sense of self, and the activation of affect over the course of psychotherapy with cluster C patients. Journal of Counseling Psychology, 61(3), 315–324. doi: 10.1037/cou0000028 [DOI] [PubMed] [Google Scholar]
- Zimmerman M, Chelminski I, Young D, Dalrymple K, & Martinez J (2012). Does the presence of one feature of borderline personality disorder have clinical significance? Implications for dimensional ratings of personality disorders. The Journal of clinical psychiatry, 73(1), 8–12. doi: 10.4088/JCP.10m06784 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.