Abstract
Background:
Mental health concerns are prevalent among primary care patients, but many do not utilize services for these conditions.
Objective:
This study aims to conduct a comprehensive assessment of barriers and facilitators to mental healthcare utilization among veteran primary care patients with common mental health concerns. We hypothesized that beliefs and knowledge about mental illness and mental healthcare would be more strongly associated with recent mental healthcare utilization than stigma, help-seeking behaviors, or logistical barriers.
Methods:
Veterans (n=116) enrolled in primary care with current symptoms of depression (58%), PTSD (37%), and/or hazardous alcohol use (50%) who either recently used mental health services (47%) or had no recent mental health treatment utilization (53%) completed a telephone-based screening, medical records review, and mail survey of ten measures of barriers and facilitators to mental health treatment utilization.
Results:
Recognition of problems as a cause for concern, OR[95%CI] =5.95[2.36,15.01], and beliefs about psychotherapy, OR[95%CI] =2.53[1.39,4.60], emerged as stronger correlates of recent mental healthcare utilization than stigma, self-efficacy, and external barriers to treatment.
Conclusions:
Results suggest the use of specific theories, measures, and interventions that focus on patient recognition of problems and beliefs about treatment over those that focus on other treatment barriers and facilitators.
Keywords: Mental Health Services, Help-Seeking Behavior, Patient Acceptance of Health Care, Primary Health Care, Veterans
Introduction
Primary care physicians commonly report concerns about access to outpatient mental health services for their patients (Cunningham, 2009). Among individuals reporting current or recent mental health concerns (concerns within the last twelve months) in the United States, less than half (41%) report receiving treatment (Wang et al., 2005). Of those who attend treatment the dropout rate is approximately 20% and the median number of visits until dropout ranges from 4–6 in specialty mental health sectors (Olfson et al., 2009). One population with low rates of utilization of mental health services is military veterans (Fikretoglu, Guay, Pedlar, & Brunet, 2008; Hoge et al., 2004). Even though some logistic barriers (e.g., finding an in-network provider) may not be a concern for veterans seeking treatment within the Veterans Affairs (VA) healthcare system, one large national study of VA patients with new mental health diagnoses indicated that only 49% received any mental health services at all with only 22% receiving psychotherapy (Cully et al., 2008). Findings also suggest that among those who attend psychotherapy, most veterans do not continue with treatment; only 46% attended more than two sessions and only 19% attended eight or more sessions (Cully et al., 2008). Low treatment-seeking and high dropout rates are a significant public health problem because mental health concerns are associated with significant disease burden and effective treatment is an important step to alleviating that burden (Ustün, 1999).
To facilitate access to mental health care, the VA has implemented efforts including integrating mental health providers into primary care, annual mental health screenings, distribution of informational materials, and individual interventions to increase mental health treatment utilization (Dollar, Kearney, Pomerantz, & Wray, 2018; McFall, Malte, Fontana, & Rosenheck, 2000; Seal et al., 2008; Stecker, McGovern, & Herr, 2012; Stecker, McHugo, Xie, Whyman, & Jones, 2014b; Tsan, Zeber, Stock, Sun, & Copeland, 2012). Primary Care Mental Health Integration (PCMHI), an integration model which has become the typical pathway to mental health treatment within the VA, in particular has demonstrated a significant improvement in facilitating engagement in mental health services (Kearney, Post, Zeiss, Goldstein, & Dundon, 2011; Possemato et al., 2018), but has not entirely resolved utilization concerns. For example, although psychotherapy utilization appears to be increasing, rates are still low (Mott, Hundt, Sansgiry, Mignogna, & Cully, 2014). Identifying which correlative factors have the strongest relationship to treatment utilization status can help identify populations and targets for intervention to further improve mental health treatment engagement.
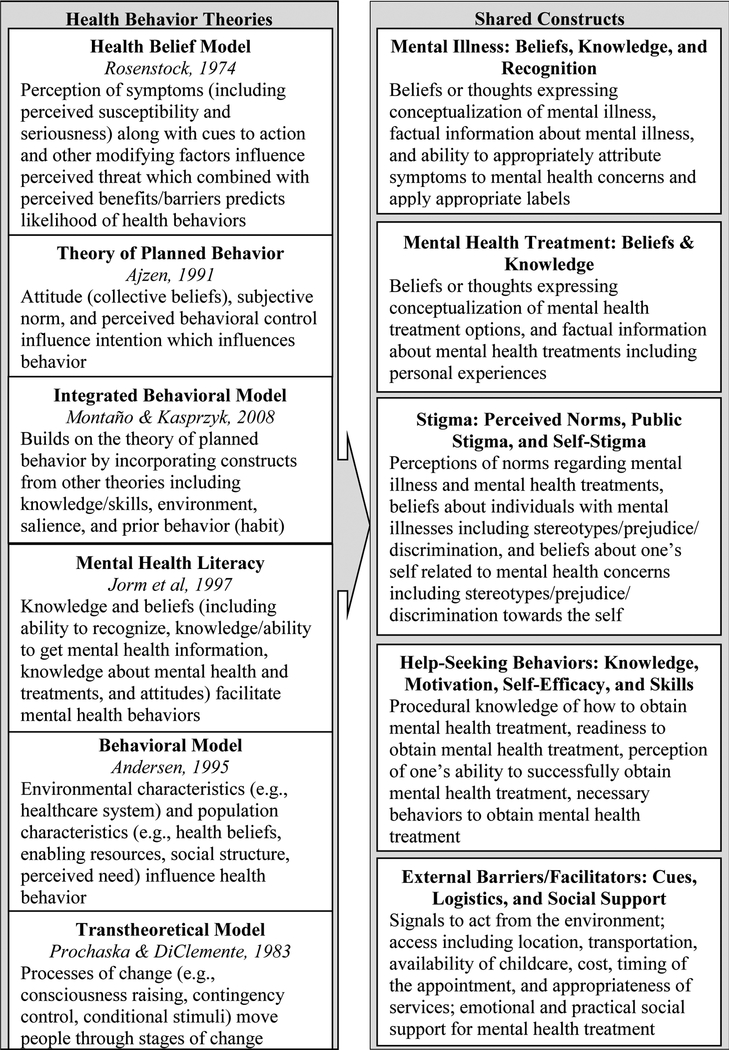
To enact change in treatment-seeking behaviors, it is important to understand and integrate health behavior theories into interventions. The literature was reviewed and five prominent theories of health behavior change were identified: the Health Belief Model (Rosenstock, 1974b), the Theory of Planned Behavior (Ajzen, 1991), the Integrated Behavioral Model (Montaño & Kasprzyk, 2015), Mental Health Literacy (Jorm et al., 1997), the Behavioral Model (Andersen, 1995), and the Transtheoretical Model (Prochaska & DiClemente, 1983). These theories share several overlapping concepts. One example is that mental health treatment beliefs are included in the health belief model (perceived barriers/benefits), theory of planned behavior (behavioral beliefs/attitudes), integrated behavioral model (behavioral beliefs/attitudes, experiential/instrumental attitudes), mental health literacy (knowledge of treatment), and behavioral model (health beliefs). We carefully reviewed the concepts within each theory and identified five shared constructs reflecting modifiable barriers or facilitators to mental healthcare: (1) mental illness beliefs, knowledge, and recognition; (2) mental health treatment beliefs and knowledge; (3) stigma including perceived norms, public stigma, and self-stigma; (4) help-seeking behaviors including knowledge, motivation, self-efficacy, and skills, and (5) external barriers and facilitators including cues, logistics, and social support (Figure 1 presents full definitions of these constructs and overviews of the cited theories; Table 2 lists measures included within each construct) (Johnson & Possemato, Unpublished Work-b). We used these five shared constructs to guide our investigation of modifiable factors influencing mental health utilization.
Figure 1.
Summary of modifiable health behavior predictors from prominent health behavior theories applied to mental health treatment.
Table 2.
Final Multivariate Logistic Regression Results and Biserial Correlations with Treatment Seeking Status for Each Barrier/Facilitator Measure Organized by Shared Construct
| Shared Constructs | Measure | Subscale | rb | t | p | OR | 95% CI |
|---|---|---|---|---|---|---|---|
| Mental Illness: Beliefs, Knowledge, & Recognition | Perceived Problem | N/A | 0.64 | −3.77 | <.001 | 5.95 | (2.36,15.01) |
| Perceived Need for Treatment | N/A | 0.60 | |||||
| Endorsed and Anticipated Stigma Inventory (EASI) (Vogt, Di Leone, et al., 2014) | Beliefs about Mental Illness | −0.24 | |||||
| Barriers to Help Seeking Scale (BHSS) Modified (Mansfield et al., 2005) | Minimizing Problem and Resignation | −0.17 | |||||
| Barriers to Help Seeking Scale (BHSS) Modified (Mansfield et al., 2005) | Emotional Control | −0.03 | |||||
| Mental health treatment: Beliefs and Knowledge | Beliefs about Psychotropic Medication and Psychotherapy (BAPMP) (Bystritsky et al., 2005) | Beliefs about Psychotherapy | 0.44 | 3.04 | .002 | 2.53 | (1.39,4.60) |
| Attitudes Toward Seeking Professional Psychological Help Short Form (ATSPPH-SF) (Elhai et al., 2008; Fischer & Farina, 1995) | N/A | 0.38 | |||||
| Endorsed and Anticipated Stigma Inventory (EASI) (Vogt, Di Leone, et al., 2014) | Beliefs about Mental Health Treatment | −0.37 | |||||
| Beliefs about Psychotropic Medication and Psychotherapy (BAPMP) Modified (Bystritsky et al., 2005) | Beliefs about Medications | 0.31 | |||||
| Endorsed and Anticipated Stigma Inventory (EASI) (Vogt, Di Leone, et al., 2014) | Beliefs about Treatment Seeking | −0.30 | |||||
| Stigma | Internalized Stigma of Mental Illness Scale (ISMI) (Ritsher et al., 2003) | Alienation | 0.25 | 0.65 | .513 | 1.23 | (0.66,2.28) |
| Internalized Stigma of Mental Illness Scale (ISMI) (Ritsher et al., 2003) | Social Withdrawal | 0.19 | |||||
| Self-Stigma of Seeking Help Scale (SSOSH) (Vogel et al., 2006) | N/A | −0.16 | |||||
| Internalized Stigma of Mental Illness Scale (ISMI) (Ritsher et al., 2003) | Discrimination Experience | 0.13 | |||||
| Internalized Stigma of Mental Illness Scale (ISMI) (Ritsher et al., 2003) | Stereotype Endorsement | 0.08 | |||||
| Endorsed and Anticipated Stigma Inventory (EASI) (Vogt, Di Leone, et al., 2014) | Concerns about Stigma from Loved Ones | 0.05 | |||||
| Internalized Stigma of Mental Illness Scale (ISMI) (Ritsher et al., 2003) | Stigma Resistance | −0.02 | |||||
| Barriers to Help Seeking Scale (BHSS) Modified (Mansfield et al., 2005) | Need for Control and Self-Reliance | 0.01 | |||||
| Help-seeking behaviors: knowledge, motivation, self-efficacy, and skills | Self-Efficacy for Managing Chronic Disease Scale (SEMCD) Modified (K. Lorig et al., 1996) | N/A | −0.36 | −1.32 | .186 | 0.66 | (0.36,1.22) |
| Empowerment Scale (ES) (Rogers et al., 1997; Rogers et al., 2010) | Self-Esteem/Self-efficacy | 0.25 | |||||
| Empowerment Scale (ES) (Rogers et al., 1997; Rogers et al., 2010) | Community Activism and Autonomy | −0.21 | |||||
| Empowerment Scale (ES) (Rogers et al., 1997; Rogers et al., 2010) | Righteous Anger | −0.11 | |||||
| Empowerment Scale (ES) (Rogers et al., 1997; Rogers et al., 2010) | Optimism and Control over the Future | 0.07 | |||||
| Health Literacy screener (Chew et al., 2008) | N/A | 0.05 | |||||
| Empowerment Scale (ES) (Rogers et al., 1997; Rogers et al., 2010) | Power-Powerlessness | 0.02 | |||||
| External barriers | Perceived Stigma and Barriers to Care for Psychological Problems (PSBCPP) Modified (Britt, Greene–Shortridge, et al., 2008) | Logistic Barriers | −0.18 | −0.76 | 0.45 | 0.82 | (0.49,1.37) |
| Barriers to Help Seeking Scale (BHSS) Modified (Mansfield et al., 2005) | Concrete Barriers and Distrust of Caregivers | 0.07 |
Several recent reviews of the literature suggest a number of different barriers and facilitators to mental health treatment utilization (Coleman, Stevelink, Hatch, Denny, & Greenberg, 2017; Hom, Stanley, Schneider, & Joiner, 2017; Johnson & Possemato, Unpublished Work-a; Kantor, Knefel, & Lueger-Schuster, 2016; Sharp et al., 2015). Modifiable individual and system barriers identified in these reviews are consistent with the shared constructs (Figure 1) and include the characteristics of the healthcare episode in which a veteran is identified with a mental health concern, structural barriers, symptom recognition, self-perceived need, knowledge about mental health, beliefs about mental health, mental health stigma, and health behaviors. Further, these reviews suggest that mental health beliefs are frequently related to treatment utilization in the expected direction (Hom et al., 2017; Johnson & Possemato, Unpublished Work-a). Other constructs, such as mental health stigma, seem to have less consistent relationships with utilization, with some studies about stigma indicating increased stigma related to in decreased utilization, some studies indicating the opposite pattern, and some studies with null results for utilization and interest in help-seeking (Sharp et al., 2015). In general, less research has been conducted about help seeking behaviors, and studies evaluating external individual barriers/facilitators (e.g., transportation) have not been significantly correlated with utilization in many studies (Hom et al., 2017; Johnson & Possemato, Unpublished Work-a).
Research findings among veteran populations largely mirror these findings, although some studies also demonstrate unique barriers to mental healthcare for veteran and military populations. A wealth of literature supports the relationship between beliefs about mental healthcare and mental illness and mental health treatment in veteran and service member populations (Adler, Britt, Riviere, Kim, & Thomas, 2015; Blais, Tsai, Southwick, & Pietrzak, 2015; Britt et al., 2011; Fox, Meyer, & Vogt, 2015; Kehle et al., 2010; Pietrzak, Johnson, Goldstein, Malley, & Southwick, 2009; Spoont et al., 2014; Valenstein et al., 2014; Vogt, Fox, & Di Leone, 2014). Some research specifically suggests that perceived need for treatment (in which individuals apply attributions of symptoms and beliefs about treatment to their own situation) is specifically related to mental health treatment (Fikretoglu et al., 2008; Spoont et al., 2014). The relationship between stigma and mental health treatment demonstrates less consistent results with stigma being unrelated to treatment (Adler et al., 2015; Arbisi, Rusch, Polusny, Thuras, & Erbes, 2013; Britt et al., 2011; Kehle et al., 2010; Kim, Britt, Klocko, Riviere, & Adler, 2011; Valenstein et al., 2014), significantly predicting increased treatment (Harpaz-Rotem, Rosenheck, Pietrzak, & Southwick, 2014; Hoerster et al., 2012; Rae Olmsted et al., 2011; Rosen et al., 2011), and significantly predicting decreased treatment (Kulesza, Pedersen, Corrigan, & Marshall, 2015). Other possible barriers and facilitators with some support include symptom severity, characteristics of the clinic where diagnosis was received, and desire for treatment (Breland, Greenbaum, Zulman, & Rosen, 2015; Rosen et al., 2011; Shiner et al., 2014; Spoont et al., 2014). One of the reviews referenced above found that military service members experience some unique barriers to care (e.g., concerns about harm to military career, stigma related to military culture), but also reflects many of the same constructs prevalent in the general population including perceived need for treatment, treatment beliefs (including concerns about providers), and structural barriers (Hom et al., 2017). Overall findings about barriers and facilitators to mental health treatment among military service members and veterans are highly consistent with other research despite some unique population considerations.
Combined, these findings suggest that in a comprehensive assessment, cognitive factors (e.g., beliefs, knowledge, and recognition) related to mental illness and mental health treatment are likely to more related to treatment utilization than other considerations such as stigma and external barriers. However, each study in this field takes a different perspective of the most important concepts predicting mental healthcare utilization and no individual study incorporates all of these concepts within one design.
Study Aims
The overall objective of this study was to conduct a comprehensive assessment of modifiable barriers and facilitators to mental healthcare utilization within veteran VA primary care patients. Because the goal of this project is to identify targets on which to intervene to increase utilization of mental healthcare, we focused on modifiable correlates (i.e., those which would be susceptible to change such as beliefs rather than those which cannot be changed such as age, race, and gender). Because there is no consensus gold standard on how to measure any one of these correlates, we administered multiple previously developed measures assessing at least one of the five barrier/facilitator constructs. A preliminary aim of this study was to answer the question about how best to measure each of these five shared constructs in this population. Our primary aim was to investigate which of the mental healthcare barriers/facilitator shared constructs are most closely associated with recent mental healthcare utilization. We expected that different barrier constructs would better correlate with past 12-month mental healthcare utilization. Specifically, we hypothesized that the constructs of (1) mental illness beliefs, knowledge, and recognition and (2) mental health treatment beliefs and knowledge would be most strongly associated with mental healthcare utilization.
Methods
Participants and Procedures
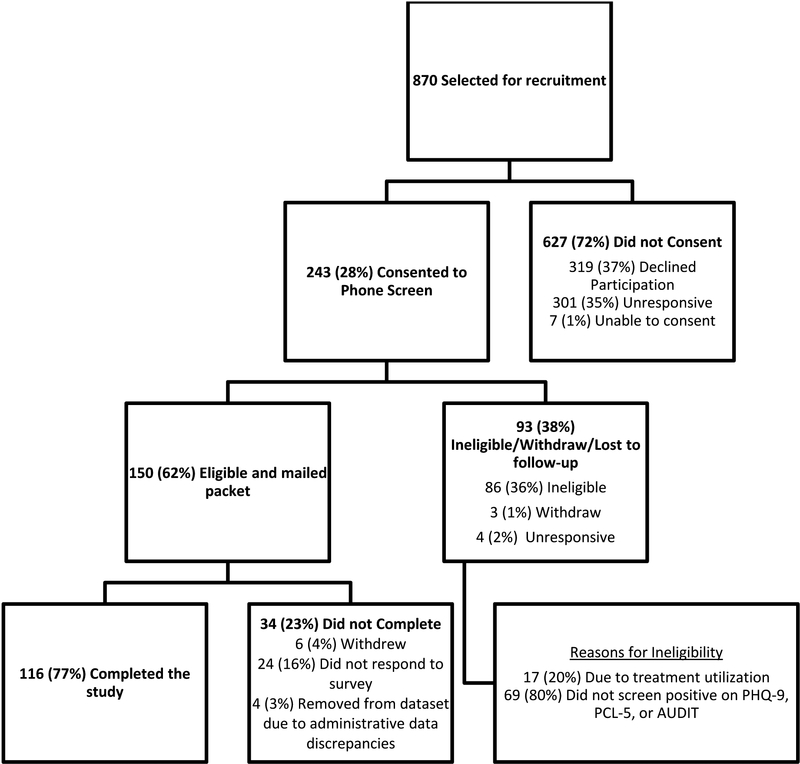
Participants were veterans enrolled in VA primary care (age 18 or older) with current symptoms of depression, PTSD, and/or hazardous alcohol use. Depression, PTSD, and hazardous alcohol use were selected because they are common diagnoses among veterans and are routinely screened for in primary care allowing us to identify potentially eligible veterans based on electronic medical record (EMR) review. Exclusion criteria included a dementia diagnosis and inability to provide oral informed consent by correctly answering comprehension questions. Individuals with additional co-morbid conditions were not excluded although other mental health cocnerns were not measured as a part of the study. Potentially eligible participants were identified via EMR review and invited to participate in a phone screen to confirm eligibility (see Figure 2). Current symptoms of these diagnoses were confirmed via telephone screen (Patient Health Questionnaire [PHQ-9] ≥ 10), PTSD (PTSD Checklist for DSM-5 [PCL-5] ≥ 33), and/or hazardous alcohol use (Alcohol Use Disorders Identification Test [AUDIT] ≥8 for men and ≥7 for women). Potential participants were stratified for recruitment based on EMR indicators of diagnosis and mental healthcare utilization in an effort to achieve relative balance in the treatment utilization groups and diagnosis. We defined treatment utilizers as patients who attended three or more appointments within the 12 months prior to the phone screen with at least one appointment being in PCMHI.1 All administrative record counts for eligibility were confirmed by individual chart review to ensure that no coding errors affected eligibility determination. We required three appointments in an effort to ensure this group reflected veterans who engaged in treatment beyond one intake appointment. We required one visit in PCMHI because this study sought to characterize patterns of mental health utilization among primary care patients and capture veterans able to engage through the typical treatment pathway within VA (starting in PCMHI and being referred from PCMHI to specialty treatment as needed); however we did not specify a particular order of appointments (PCMHI vs. other mental health first) for veterans who obtained treatment in both PCMHI and specialty mental health settings. Twenty-eight percent of veterans consented to the phone screen, and 62% of those were eligible (Figure 2). Following the phone screen, eligible participants were mailed a survey packet containing a series of self-report questionnaires about barriers and facilitators to mental health treatment. Participants were paid $10 for completing phone screens (estimated 20 minutes of effort) and $20 returned survey packets (estimated 45 minutes of effort). All procedures were approved by the local Institutional Review Board.
Figure 2.
Recruitment flowchart.
Seventy-seven percent of eligible veterans completed and returned the survey packet resulting in a final sample size of 116 (Figure 2). The final sample includes two groups: treatment utilizers (three or more mental health appointments within the last year, n = 54) or non-treatment utilizers (no mental health appointments within the last year, N = 62) (Table 1).
Table 1.
Demographic, Military, and Clinical Characteristics of the Sample with Comparison of Treatment Users and Non-Users
| Mental Health Treatment | Total Sample | |||
|---|---|---|---|---|
| Users (n = 54) n (%) |
Non-Users (n = 62) n (%) |
χ2 | (n = 116) n (%) |
|
| Positive Screens | ||||
| PHQ-9 | 34 (64%) | 33 (53%) | 1.40 | 67 (58%) |
| PCL-5 | 28 (55%) | 15 (28%) | 7.98** | 43 (37%) |
| AUDIT | 24 (44%) | 34 (55%) | 1.25 | 58 (50%) |
| Number of Positive Screens (t-test) M(SD) | 1.59 (.66) | 1.32 (.56) | −2.37* | 1.45 (.62) |
| Quality of Life (t-tests) | ||||
| Physical Health M(SD) | 10.96 (3.11) | 12.34 (3.40) | 2.26* | 11.69 (3.33) |
| Psychological M(SD) | 10.70 (2.65) | 12.77 (3.28) | 3.69*** | 11.81 (3.17) |
| Social Relations M(SD) | 10.09 (3.70) | 12.14 (4.04) | 2.83** | 11.18 (4.01) |
| Environment M(SD) | 13.08 (2.60) | 14.18 (2.44) | 2.35* | 13.67 (2.56) |
| Female Gender | 12 (22%) | 7 (12%)1 | 2.40 | 19 (16%) |
| Person of Color2 | 7 (13%) | 5 (8%) | .70 | 12 (10%) |
| Hispanic/Latino Ethnicity | 2 (4%) | 0 (0%) | −−3 | 2 (2%) |
| Currently married | 31 (57%) | 31 (51%) | 0.50 | 62 (54%) |
| Employed Outside the Home | 7 (14%) | 22 (37%) | 7.82** | 29 (26%) |
| Currently a Student | 3 (6%) | 0 (0%) | −−3 | 3 (3%) |
| Education Level | 9.11* | |||
| High School, GED, or less | 10 (19%) | 28 (46%) | 38 (34%) | |
| Some college | 19 (37%) | 15 (25%) | 34 (30%) | |
| 2-yr college degree | 10 (19%) | 9 (15%) | 19 (17%) | |
| 4-yr college degree or more | 13 (25%) | 9 (15%) | 22 (20%) | |
| Household Income | 5.21 | |||
| <$20,000 | 7 (14%) | 15 (25%) | 22 (20%) | |
| $20,000-$39,999 | 18 (35%) | 12 (21%) | 30 (28%) | |
| $40,000-$59,999 | 9 (18%) | 15 (26%) | 24 (22%) | |
| $60,000+4 | 17 (33%) | 16 (28%) | 33 (30%) | |
| Branch5 | ||||
| Army | 30 (56%) | 43 (69%) | 2.36 | 73 (63%) |
| Air Force | 7 (13%) | 7 (11%) | 0.08 | 14 (12%) |
| Navy | 14 (26%) | 9 (15%) | 2.36 | 23 (20%) |
| Marines | 9 (17%) | 4 (7%) | 3.03 | 13 (11%) |
| Era6 | ||||
| Vietnam | 14 (28%) | 42 (69%) | 19.05*** | 56 (50%) |
| Persian Gulf War I | 16 (31%) | 11 (18%) | 2.70 | 27 (24%) |
| Gulf War II | 17 (33%) | 12 (20%) | 2.70 | 29 (26%) |
| Combat Exposure | 28 (55%) | 32 (55%) | 0.001 | 60 (55%) |
Notes.
p ≤ .05;
p ≤ .01;
p ≤ .001;
One Veteran in the mental health treatment non-users group endorsed both genders and was excluded from the gender χ2 analysis reported in this table;
Veterans identifying as Black/African American (n=8, 7%), Native Hawaiian/Pacific Islander (n=1, 1%), and Mixed Race (n=3, 3%) were collapsed into a single group for reporting and for the χ2 analysis due to small expected cell size;
χ2 analysis not conducted because expected cell size was less than 5;
The top three bands of income were collapsed for reporting and for the χ2 analysis due to small expected cell size.;
One veteran reported service in the Coast Guard;
The three most common eras are reported here, 1 veteran reported Korean era service and 11 veterans reported Grenada era service
Measures
Mental healthcare utilization was measured using both EMR review for VA healthcare appointments, and self-report interview questions for non-VA healthcare appointments. Current mental health symptoms were measured using standard measures within the field with good validity and reliability. The PCL-5 was used to measure PTSD symptoms (Blevins, Weathers, Davis, Witte, & Domino, 2015; Bovin et al., 2016), the PHQ-9 was used to measure depression symptoms (Kroenke, Spitzer, & Williams, 2001), and the AUDIT was used to measure hazardous alcohol use (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001). The PCL-5, PHQ-9, and AUDIT display strong psychometric detection of PTSD, depression, and hazardous alcohol use respectively (Bovin et al., 2016; Kroenke et al., 2001; Saunders, Aasland, Babor, De la Fuente, & Grant, 1993). The World Health Organization Quality of Life BREF (WHOQOL-BREF) is a 26 item inventory administered to evaluate overall mental health, well-being, and functioning (Group, 1998). The WHOQOL-BREF demonstrates good validity and reliability (Skevington, Lotfy, & O’Connell, 2004).
In line with the preliminary aim to identify the best measure for each shared construct, veterans’ healthcare literature was reviewed to identify measures which capture the five broad constructs of barriers and facilitators to mental healthcare utilization which are targeted in this study (Figure 1). At least two measures per construct were selected based on the following criteria: scope of coverage of relevant construct, psychometric properties, and/or common utilization as an outcome measure in the field (Table 2 lists each measure by construct). The following self-report inventories were selected: Endorsed and Anticipated Stigma Inventory (40 items, measured 5 domains of mental health beliefs and stigma2; Cronbach’s α=.931; Vogt, Di Leone, et al., 2014), Barriers to Help Seeking Scale-Modified (31 items, measured various domains of barriers to seeking professional help, modified for this study to remove items specific to physical evaluations which were many of the questions in the privacy subscale therefore that subscale was not analyzed; Cronbach’s α=.936; Mansfield, Addis, & Courtenay, 2005), Beliefs about Psychotropic Medication and Psychotherapy-Modified (14 items, assessed beliefs about psychotropic medications and psychotherapy, medication subscale items reflecting anxiety-specific symptoms were modified to state “mental health symptoms” or “mental health problems”; Cronbach’s α=.852; Bystritsky et al., 2005), Attitudes Towards Seeking Professional Psychological Help Short Form (10 items, measured attitudes towards help-seeking; Cronbach’s α=.763; Elhai, Schweinle, & Anderson, 2008; Fischer & Farina, 1995), Internalized Stigma of Mental Illness Scale (29 items, measured five components of stigma including alienation, stereotype endorsement, discrimination experience, social withdrawal, and stigma resistance; Cronbach’s α=.951; Ritsher, Otilingam, & Grajales, 2003), Self-Stigma of Seeking Help Scale (10 items, measured self-stigma associated with engaging in therapy; Cronbach’s α=.850; Vogel, Wade, & Haake, 2006), Self-Efficacy for Managing Chronic Disease Scale (6 items, measured self-efficacy related to self-management behaviors for chronic diseases, given the sample we changed the word “disease” in this scale to specify “mental health symptoms”; Cronbach’s α=.925; adapted from items used in Lorig, Sobel, Ritter, Laurent, & Hobbs, 2001, originally reported in Lorig et al., 1996), Empowerment Scale (28 items, measures subjective empowerment including self-efficacy and perceived power; Cronbach’s α=.845; Rogers, Chamberlin, Ellison, & Crean, 1997; Rogers, Ralph, & Salzer, 2010), Perceived Stigma and Barriers to Care for Psychological Problems-Modified (7 items, used the logistical barriers subscale to evaluate external barriers to access and two additional questions assessing childcare and family support; Cronbach’s α=.688; Britt, Greene-Shortridge, et al., 2008), Health Literacy Screener (1 item, identifies individuals who have poor health literacy; Chew et al., 2008).
Two additional self-report items were written for this project to measure self-perception of a mental health concern and self-perception of a need for treatment which were not captured in other measures. Based on the literature review, these two constructs are commonly measured via single item measures written for study specific needs and we were unable to find any scales or subscales measuring these constructs specifically. The items we used were: (1) In your opinion, do you believe that you need treatment of any kind (including professional help, self-help, and alternative treatments) for: feeling depressed, anxious, or “stressed out,” personal problems (like when a loved one dies or when there are problems at work), family problems (like marriage problems or when parents and children have trouble getting along), needing help with drug or alcohol use, or for mental or emotional illness? (perceived need for treatment) and (2) In your opinion, are any of the above concerns a problem for you? (perceived problem). Both were rated using the following scale: yes, no, unsure. We based the language of these items on items in the Consumer Assessment of Healthcare Providers and Systems (CAHPS) Experience of Care & Health Outcomes (ECHO) Adult Managed Behavioral Healthcare Organization Version 3.0 English survey (CAHPS Experience of Care & Health Outcomes (ECHO) Survey). To estimate validity, we ran selected correlations with other measures in the study which we anticipated would have a specific relationship with each our single items. All findings were in the expected direction. We predicted these two items would have a strong positive correlation with each other which was supported (r=0.70, p<.001), and a weak correlation with logistic barriers which was supported (r=−0.13, p=.178). We also predicted a negative correlation with minimizing symptoms and the direction was negative although the result was not significant (r=−0.03, p=.718). Table 2 lists all measures within each of the five shared constructs.
Analysis
Descriptive statistics as well as independent samples t tests and chi square tests of independence were calculated to compare demographics for treatment users and non-users using IBM SPSS Statistics 22. A large proportion of participants (77%) were missing at least one variable of data although this reflected a small percentage (2%) of the overall data used in the analyses. To accommodate, multiple imputation (MI) was used to impute missing values of outcome variables (Berglund & Heeringa, 2014). We first computed the percentage of items of each measure that were missing. If less than 20% of items in a given measure were missing, the missing items were imputed using the non-missing items as predictors. The summary value of these measures could then be calculated. If more than 20% of items of a measure were missing, the summary value was set to missing. The summary value of all measures was then entered into SAS (v9.4) Proc MI using FCS regression (Raghunathan, Lepkowski, Van Hoewyk, & Solenberger, 2001). Twenty repetitions achieved a relative efficiency greater than .975, and most outcome measures resulted in less than a 1% loss of data. After achieving good efficiency, the data was ready for analysis using SAS Proc MIAnalyze.
All pairwise biserial correlations of each of the subscales and treatment utilization status were calculated and sorted within each of the five shared constructs. The subscale associated with the highest biserial correlation with treatment utilization status within each shared construct was selected for representation in the final statistical model. A logistic regression model consisting of the five best predictors and treatment seeking status was applied to each of the 20 imputation data sets. Parameter estimates, variance and covariances were then entered into SAS Proc MIAnalyze to produce the final set of parameter estimates, SEs and associated p-values.
Results
Veterans who recently or currently were receiving mental health treatment were significantly different than veterans who had not received mental health treatment on several variables. Veterans recently or currently receiving mental health treatment were more likely to have a positive PCL screen, have a higher number of positive mental health screens, worse quality of life, have lower levels of employment, have higher education, and were less likely to serve in the Vietnam era compared to other service eras (Table 1). We evaluated three demographics (gender, race/ethnicity, and employment) to understand how our sample compared with national statistics reflecting the veteran population (National Center for Veterans Analysis and Statistics, “Key Statistics by Veteran Status and Period of Service,”). Using a χ2 Goodness of Fit test, our sample differed from national veteran statistics in the three demographic categories: higher proportion of women (χ2=7.81, p=.005), lower proportion of participants identifying as a racial or ethnic minority (χ2=253.85, p<.001), and lower rates of employment (χ2=13, p<.001).
Table 2 shows the biserial correlations demonstrating the performance of the measures within each shared construct in predicting treatment utilization status. The ‘Mental Illness: Beliefs, Knowledge, and Recognition’ construct contained the scales with the strongest correlations (biserial correlations range from −0.03 to 0.64); within that construct, the two one item questions (presented as a pair but evaluated separately) assessing whether veterans perceive a problem and whether they believe they need help performed the strongest for predicting treatment seeking status. The single item assessing whether veterans perceive a problem was the best indicator of utilization (rb = 0.64). The shared construct with the second highest correlations was the ‘Mental Health Treatment: Beliefs and Knowledge’ construct (biserial correlations range from −0.30–0.44); within this construct, the ‘Beliefs about psychotherapy’ subscale of the ‘Beliefs about Psychotropic Medication and Psychotherapy’ scale had the strongest correlation with treatment seeking status (rb = 0.44) (Bystritsky et al., 2005). For the remaining three shared constructs, the measures which demonstrated the strongest correlations with treatment seeking status were as follows: ‘Internalized Stigma of Mental Illness’ ‘Alienation’ subscale for the ‘Stigma’ shared construct (rb = 0.25), ‘Self Efficacy for Managing Chronic Disease’ (SEMCD) modified scale for the ‘Help-Seeking Behaviors: Knowledge, Motivation, Self-Efficacy, and Skills’ shared construct (rb = −0.36), and ‘Perceived Stigma and Barriers to Care for Psychological Problems’ modified scale ‘Logistic barriers’ subscale for the ‘External Barriers’ shared construct (rb = −0.18). All measures noted above except the modified SEMCD demonstrated correlations in the direction expected based on health behavior theories. Health behavior skills, such as self-management skills measured by the SEMCD, are typically hypothesized to be facilitators which would aid in ability to access treatment, but this study found a correlation in the opposite direction. The single measure with the strongest correlation with treatment seeking status within each shared construct, the single item assessing Perceived Problem, the Beliefs about Psychotherapy subscale (BAPMP), the Alienation subscale (ISMI), SEMCD modified, and Logistic Barriers subscale (PSBCPP), were included in the overall model.
The overall model was significant with two correlates of treatment utilization status demonstrating significant effects. Specifically, Veterans recognizing emotional symptoms, personal problems, family problems, substance use, or a mental illness as a concern were more likely to be currently/recently in treatment than to have no past year treatment, p < .001, OR [95%CI] = 5.95 [2.36,15.01]. Additionally, Veterans endorsing more positive (e.g., “therapy often offers patients new and beneficial perspectives”) and less negative beliefs (e.g., “therapy is ineffective for most people”) about psychotherapy were more likely to be current/recent treatment utilizers, p = .002, OR [95%CI] = 2.53 [1.39, 4.60]. Correlates in the final model which did not significantly differ based on treatment seeking status include stigma (specifically alienation), self-efficacy to manage symptoms, and perceived external barriers.
Discussion
Several measures with strong correlations with mental healthcare utilization status were identified in line with the preliminary aim of this study. Consistent with our hypotheses, the measures within the constructs of (1) mental illness beliefs, knowledge, and recognition and (2) mental health treatment beliefs and knowledge demonstrated the strongest correlation with treatment seeking status and were the only two constructs which achieved statistical significance in the overall model. These findings are consistent with a large body of previous research demonstrating that patient perceptions of symptoms as a cause for concern and beliefs about mental health treatment are highly related to treatment utilization in veteran and military populations (for example, Adler et al., 2015; Fikretoglu et al., 2008; Spoont et al., 2014). These findings have implications for advancing theory, clinical practice, and additional research.
The two single items developed for this study measuring recognition of a mental health concern and perceived need for treatment were the best predictors of mental health treatment utilization status for this sample. These items might provide a brief screening tool and conversation starter for providers wishing to have a conversation with patients about mental health referrals. The Beliefs about Psychotherapy subscale of the modified Beliefs about Psychotropic Medication and Psychotherapy demonstrated the strongest correlation within mental health treatment beliefs and knowledge construct. The Beliefs about Psychotropic Medication and Psychotherapy scale is designed to measure beliefs about each of the two primary modalities of mental health treatment, medication management and psychotherapy, and includes items assessing beliefs about treatment efficacy, beliefs about expected treatment experiences, and beliefs about people who engage in treatment (Bystritsky et al., 2005). Although the Beliefs about Psychotherapy subscale specifically performed better in this sample, administering the whole measure assesses patients’ preferences and beliefs regarding both treatment modalities. This might be helpful given that previous research has shown that beliefs about specific treatment types predict treatment utilization patterns (Spoont et al., 2014; Spoont et al., 2015). Administering this scale also might inform psychoeducation content based on endorsed beliefs, and inform the shared decision-making process to help tailor referrals to patients’ preferred treatment modality.
The EASI (Vogt, Di Leone, et al., 2014) also performed well in this sample as an overall measure given that it covers multiple constructs and most subscales demonstrate moderate correlations with treatment utilization status. Other measures which performed well in this sample can be used to measure specific constructs were the ATSPPH-SF (Elhai et al., 2008; Fischer & Farina, 1995) for mental health treatment beliefs, and the ISMI (Ritsher et al., 2003) for stigma.
The findings that problem recognition and mental health treatment beliefs have the strongest relationship with treatment utilization status help inform which health behavior theories and models may be particularly relevant to veterans’ mental health treatment utilization process. Personal health beliefs are incorporated into all the models reviewed, but self-perceived symptoms are not universal. Perception and/or recognition of symptoms is directly noted in the Health Belief Model (Rosenstock, 1974a), Mental Health Literacy framework (Jorm et al., 1997), and Transtheoretical Model (Prochaska & DiClemente, 1983). The related construct of perceived need is incorporated in the Behavioral Model (Andersen, 1995). The models which emphasize these constructs may be most relevant to current mental healthcare utilization trends.
Similarly, interventions and public health initiatives which target symptom recognition and health beliefs may be more impactful than other targets (e.g., skills or knowledge) for this population at this time. One strategy which address these constructs is Cognitive Behavioral Therapy for Treatment Seeking (CBT-TS) (Stecker, Fortney, & Sherbourne, 2011; Stecker et al., 2012; Stecker, McHugo, Xie, Whyman, & Jones, 2014a; Stecker et al., 2014b) which identifies cognitive barriers to treatment seeking and uses a cognitive restructuring approach to facilitate treatment seeking within 1–2 treatment sessions. One study focused on implementing CBT-TS in a PCMHI setting to enhance treatment utilization among veterans with PTSD and found that veterans from the clinic where CBT-TS was implemented were more likely to engage in psychotherapy for PTSD compared to veterans from the control clinic (Possemato, Johnson, Wray, Webster, & Stecker, 2017). Another is Motivational Interviewing which explores patients’ ambivalence to change through highlighting discrepancies between current status and patients’ goals and values to highlight problem recognition and strategies to reconcile concerns about behavior change (in this case, treatment-seeking behaviors) (Miller & Rollnick, 2002). One specific study demonstrated that veterans screening positive for one or more mental health concerns were more likely to engage in mental health treatment if they received telephone based motivational interviewing (Seal et al., 2012). This particular intervention involves four 20–30 minute telephone sessions making it a good fit to be implemented through integrated primary care services, such as PCMHI within VA. Health promotion strategies (e.g., public awareness campaigns to increase recognition and screenings) can also be used to address one or both of these constructs on a population level. Decision aids are one tool which can be widely disseminated to assist with following up on screening results and new diagnoses to help educate patients about treatment options and inform decision making; a recent study evaluating a decision aid for PTSD found that those receiving the decision aid had lower decisional conflict, greater knowledge, and were more likely to arrive at a treatment choice (Watts et al., 2015). Mental health clinicians integrated into medical settings, are well suited to help facilitate these efforts.
An interesting and unexpected finding in the study was that veterans from the Vietnam era were more likely to belong in the non-treatment group. Although this particular study was not designed to draw conclusions about differences in treatment utilization between veterans from different eras, this finding is consistent with previous research demonstrating differences in treatment seeking among veterans based on age (Hankin, Spiro III, Miller, & Kazis, 1999). One potential direction for future research is to explore differences in treatment seeking rates and barriers between eras.
This study has several strengths including the incorporation of constructs across a range of theories and the focus on modifiable constructs to facilitate intervention. However, three key limitations should be noted. First, there are some concerns related to sampling. Specifically, our sample had a low number of respondents identify as member of a racial or ethnic minority group. Further, a large number of potential participants were lost during early recruitment efforts (i.e., between the recruitment letter and phone screen phases). This might have affected the sample since it is likely that veterans with strong concerns related to the constructs measured within the study (e.g., negative beliefs about mental illness) are among those who did not choose to participate. Second, despite the comprehensive missing data analysis approach, the amount of missing data remains a limitation of the dataset. Finally, the retrospective design only allows for correlational data and does not allow for causal attribution. Future studies with prospective designs would allow for inferences regarding causality.
Conclusions
The findings from this study have implications for theories of health behavior relevant to mental health treatment utilization, clinical efforts to increase mental health treatment utilization in the U.S. military veteran populations, and research and quality improvement efforts to measure the impact of interventions designed to change mental health treatment barriers or facilitators. Clinical efforts and theories related to mental health treatment utilization should focus on identifying and addressing mental health treatment beliefs and recognition as part of a coordinated effort to better engage with veterans and use assessments to measure these efforts which have been demonstrated to relate to treatment utilization outcomes in this population.
Acknowledgments
This material is based upon work supported by the Department of Veterans Affairs, Center for Integrated Healthcare Pilot Research Grant awarded to Dr. Johnson.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Footnotes
Appointments were counted as PCMHI if they had a clinic stop code of 534 or 539; and all other clinic stop codes in the 500s were counted as other mental health appointments.
The Workplace Stigma subscale of the EASI was administered as designed but had a large amount of missing data (12 veterans, 10% of the sample, with partially missing data and 11 veterans, 9% of the sample missing the whole section). Since several veterans who skipped this section wrote in the margins that they did not perceive this section as applicable to them, we did not believe the missing data in this subscale generalized to the other subscales of this measure. We were also not easily able to discern patterns in veterans missing this subscale even when comparing missingness with our employment data. This subscale was therefore not included in the final analysis but the other subscales were retained unchanged.
References
- Adler AB, Britt TW, Riviere LA, Kim PY, & Thomas JL (2015). Longitudinal determinants of mental health treatment-seeking by US soldiers. The British Journal of Psychiatry, 207, 346–350. [DOI] [PubMed] [Google Scholar]
- Ajzen I (1991). The theory of planned behavior. Organizational behavior and human decision processes, 50, 179–211. [Google Scholar]
- Andersen RM (1995). Revisiting the behavioral model and access to medical care: does it matter? Journal of health and social behavior, 1–10. [PubMed] [Google Scholar]
- Arbisi PA, Rusch L, Polusny MA, Thuras P, & Erbes CR (2013). Does cynicism play a role in failure to obtain needed care? Mental health service utilization among returning US National Guard soldiers. Psychological Assessment, 25, 991. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). AUDIT The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care (Second ed., pp. 41): World Health Organization Department of Mental Health and Substance Dependence. [Google Scholar]
- Berglund P, & Heeringa SG (2014). Multiple imputation of missing data using SAS: SAS Institute. [Google Scholar]
- Blais RK, Tsai J, Southwick SM, & Pietrzak RH (2015). Barriers and facilitators related to mental health care use among older veterans in the United States. Psychiatric Services, 66, 500–506. [DOI] [PubMed] [Google Scholar]
- Blevins C, Weathers F, Davis M, Witte T, & Domino J (2015). The Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5): Development and Initial Psychometric Evaluation. Journal of traumatic stress, 28, 489. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, & Keane TM (2016). Psychometric Properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in Veterans. Psychological Assessment, 28, 1379–1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Breland JY, Greenbaum MA, Zulman DM, & Rosen CS (2015). The effect of medical comorbidities on male and female veterans’ use of psychotherapy for PTSD. Medical care, 53, S120–S127. doi: 10.1097/mlr.0000000000000284 [DOI] [PubMed] [Google Scholar]
- Britt TW, Bennett EA, Crabtree M, Haugh C, Oliver K, McFadden A, & Pury CL (2011). The theory of planned behavior and reserve component veteran treatment seeking. Military Psychology, 23, 82–96. [Google Scholar]
- Britt TW, Greene-Shortridge TM, Brink S, Nguyen QB, Rath J, Cox AL, … Castro CA. (2008). Perceived stigma and barriers to care for psychological treatment: Implications for reactions to stressors in different contexts. Journal of Social and Clinical Psychology, 27, 317–335. [Google Scholar]
- Britt TW, Greene–Shortridge TM, Brink S, Nguyen QB, Rath J, Cox AL, … Castro CA. (2008). Perceived stigma and barriers to care for psychological treatment: Implications for reactions to stressors in different contexts. Journal of Social and Clinical Psychology, 27, 317–335. [Google Scholar]
- Bystritsky A, Wagner AW, Russo JE, Stein MB, Sherbourne CD, Craske MG, & Roy-Byrne PP (2005). Assessment of beliefs about psychotropic medication and psychotherapy: development of a measure for patients with anxiety disorders. General hospital psychiatry, 27, 313–318. [DOI] [PubMed] [Google Scholar]
- CAHPS Experience of Care & Health Outcomes (ECHO) Survey. (May 2018). Retrieved May 31, 2018, from http://www.ahrq.gov/cahps/surveys-guidance/echo/index.html
- Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Snyder A, … VanRyn M. (2008). Validation of screening questions for limited health literacy in a large VA outpatient population. Journal of General Internal Medicine, 23, 561–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman S, Stevelink S, Hatch S, Denny J, & Greenberg N (2017). Stigma-related barriers and facilitators to help seeking for mental health issues in the armed forces: a systematic review and thematic synthesis of qualitative literature. Psychological medicine, 1–13. [DOI] [PubMed] [Google Scholar]
- Cully JA, Tolpin L, Henderson L, Jimenez D, Kunik ME, & Petersen LA (2008). Psychotherapy in the Veterans Health Administration: missed opportunities? Psychological Services, 5, 320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham PJ (2009). Beyond parity: primary care physicians’ perspectives on access to mental health care. Health Affairs, 28, w490–w501. [DOI] [PubMed] [Google Scholar]
- Dollar K, Kearney L, Pomerantz A, & Wray L (2018). Achieving same-day access in integrated primary care. Families, systems & health: the journal of collaborative family healthcare, 36, 32. [DOI] [PubMed] [Google Scholar]
- Elhai JD, Schweinle W, & Anderson SM (2008). Reliability and validity of the attitudes toward seeking professional psychological help scale-short form. Psychiatry research, 159, 320–329. [DOI] [PubMed] [Google Scholar]
- Fikretoglu D, Guay S, Pedlar D, & Brunet A (2008). Twelve month use of mental health services in a nationally representative, active military sample. Medical care, 46, 217–223. [DOI] [PubMed] [Google Scholar]
- Fischer EH, & Farina A (1995). Attitudes toward seeking professional psychologial help: A shortened form and considerations for research. Journal of College Student Development. [Google Scholar]
- Fox AB, Meyer EC, & Vogt D (2015). Attitudes about the VA health-care setting, mental illness, and mental health treatment and their relationship with VA mental health service use among female and male OEF/OIF veterans. Psychological Services, 12, 49. [DOI] [PubMed] [Google Scholar]
- Group W (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological medicine, 28, 551–558. [DOI] [PubMed] [Google Scholar]
- Hankin CS, Spiro A III, Miller DR, & Kazis L (1999). Mental disorders and mental health treatment among US Department of Veterans Affairs outpatients: the Veterans Health Study. American Journal of Psychiatry, 156, 1924–1930. [DOI] [PubMed] [Google Scholar]
- Harpaz-Rotem I, Rosenheck RA, Pietrzak RH, & Southwick SM (2014). Determinants of prospective engagement in mental health treatment among symptomatic Iraq/Afghanistan veterans. The Journal of nervous and mental disease, 202, 97–104. [DOI] [PubMed] [Google Scholar]
- Hoerster KD, Malte CA, Imel ZE, Ahmad Z, Hunt SC, & Jakupcak M (2012). Association of perceived barriers with prospective use of VA mental health care among Iraq and Afghanistan veterans. Psychiatric Services, 63, 380–382. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, & Koffman RL (2004). Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N engl J med, 2004, 13–22. [DOI] [PubMed] [Google Scholar]
- Hom MA, Stanley IH, Schneider ME, & Joiner TE (2017). A systematic review of help-seeking and mental health service utilization among military service members. Clinical Psychology Review. [DOI] [PubMed] [Google Scholar]
- Johnson EM, & Possemato K (Unpublished Work-a). Correlates and Predictors of Mental Health Treatment Utilization for Veterans with PTSD: A Systematic Review. [DOI] [PMC free article] [PubMed]
- Johnson EM, & Possemato K (Unpublished Work-b). Defining the Things We Can Change to Improve Access to Mental Healthcare. [DOI] [PMC free article] [PubMed]
- Jorm A, Korten A, Jacomb P, Christensen H, Rodgers B, & Pollitt P (1997). “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. The Medical journal of Australia, 166, 182. [DOI] [PubMed] [Google Scholar]
- Kantor V, Knefel M, & Lueger-Schuster B (2016). Perceived barriers and facilitators of mental health service utilization in adult trauma survivors: A systematic review. Clinical Psychology Review. [DOI] [PubMed] [Google Scholar]
- Kearney LK, Post EP, Zeiss A, Goldstein MG, & Dundon M (2011). The role of mental and behavioral health in the application of the patient-centered medical home in the Department of Veterans Affairs. Translational behavioral medicine, 1, 624–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kehle SM, Polusny MA, Murdoch M, Erbes CR, Arbisi PA, Thuras P, & Meis LA (2010). Early mental health treatment‐seeking among US National Guard soldiers deployed to Iraq. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies, 23, 33–40. [DOI] [PubMed] [Google Scholar]
- National Center for Veterans Analysis and Statistics. “Key Statistics by Veteran Status and Period of Service.” Retrieved January 16, 2019, from https://www.va.gov/vetdata/docs/SpecialReports/KeyStats.pdf
- Kim PY, Britt TW, Klocko RP, Riviere LA, & Adler AB (2011). Stigma, negative attitudes about treatment, and utilization of mental health care among soldiers. Military Psychology, 23, 65–81. [Google Scholar]
- Kroenke K, Spitzer RL, & Williams JBW (2001). The PHQ-9. Journal of General Internal Medicine, 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulesza M, Pedersen ER, Corrigan PW, & Marshall GN (2015). Help-seeking stigma and mental health treatment seeking among young adult veterans. Military behavioral health, 3, 230–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorig K, Stewart A, Ritter P, González V, Laurent D, & Lynch J (1996). Outcome Measures for Health Education and other Health Care Interventions. Thousand Oaks, CA: Sage Publications, Inc. [Google Scholar]
- Lorig KR, Sobel DS, Ritter PL, Laurent D, & Hobbs M (2001). Effect of a self-management program for patietns with chronic disease. Effective Clinical Practice, 4, 256–262. [PubMed] [Google Scholar]
- Mansfield AK, Addis ME, & Courtenay W (2005). Measurement of Men’s Help Seeking: Development and Evaluation of the Barriers to Help Seeking Scale. Psychology of Men & Masculinity, 6, 95. [Google Scholar]
- McFall M, Malte C, Fontana A, & Rosenheck RA (2000). Effects of an outreach intervention on use of mental health services by veterans with posttraumatic stress disorder. Psychiatric Services, 51, 369–374. [DOI] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2002). Motivational Interviewing: Preparing People for Change (Second Edition ed.). New York, NY: Guilford Press. [Google Scholar]
- Montaño DE, & Kasprzyk D (2015). Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. Health behavior: Theory, research and practice, 95–124. [Google Scholar]
- Mott JM, Hundt NE, Sansgiry S, Mignogna J, & Cully JA (2014). Changes in psychotherapy utilization among veterans with depression, anxiety, and PTSD. Psychiatric Services, 65, 106–112. [DOI] [PubMed] [Google Scholar]
- Olfson M, Mojtabai R, Sampson NA, Hwang I, Druss B, Wang PS, … Kessler RC. (2009). Dropout from outpatient mental health care in the United States. Psychiatric Services, 60, 898–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pietrzak RH, Johnson DC, Goldstein MB, Malley JC, & Southwick SM (2009). Perceived stigma and barriers to mental health care utilization among OEF-OIF veterans. Psychiatric Services, 60, 1118–1122. [DOI] [PubMed] [Google Scholar]
- Possemato K, Johnson EM, Beehler GP, Shepardson RL, King P, Vair CL, … Wray LO. (2018). Patient outcomes associated with primary care behavioral health services: A systematic review. General hospital psychiatry, 53, 1–11. doi: 10.1016/j.genhosppsych.2018.04.002 [DOI] [PubMed] [Google Scholar]
- Possemato K, Johnson EM, Wray LO, Webster B, & Stecker T (2017). The Implementation and Testing of a Referral Management System to Address Barriers to Treatment Seeking Among Primary Care Veterans With PTSD. [DOI] [PubMed]
- Prochaska JO, & DiClemente CC (1983). Stages and processes of self-change toward smoking: Toward an integrative model of change. Journal of Consulting and Clinical Psychology, 51, 390–395. [DOI] [PubMed] [Google Scholar]
- Rae Olmsted KL, Brown JM, Vandermaas-Peeler JR, Tueller SJ, Johnson RE, & Gibbs DA (2011). Mental health and substance abuse treatment stigma among soldiers. Military Psychology, 23, 52–64. [Google Scholar]
- Raghunathan TE, Lepkowski JM, Van Hoewyk J, & Solenberger P (2001). A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey methodology, 27, 85–96. [Google Scholar]
- Ritsher JB, Otilingam PG, & Grajales M (2003). Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry research, 121, 31–49. [DOI] [PubMed] [Google Scholar]
- Rogers ES, Chamberlin J, Ellison ML, & Crean T (1997). A consumer-constructed scale to measure empowerment among users of mental health services. Psychiatric Services. [DOI] [PubMed] [Google Scholar]
- Rogers ES, Ralph RO, & Salzer MS (2010). Validating the empowerment scale with a multisite sample of consumers of mental health services. Psychiatric Services, 61, 933–936. [DOI] [PubMed] [Google Scholar]
- Rosen CS, Greenbaum MA, Fitt JE, Laffaye C, Norris VA, & Kimerling R (2011). Stigma, help-seeking attitudes, and use of psychotherapy in veterans with diagnoses of posttraumatic stress disorder. The Journal of nervous and mental disease, 199, 879–885. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM (1974a). The health belief model and preventive health behavior. Health education monographs, 2, 354–386. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM (1974b). Historical origins of the health belief model. Health education monographs, 2, 328–335. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction, 88, 791–804. [DOI] [PubMed] [Google Scholar]
- Seal KH, Abadjian L, McCamish N, Shi Y, Tarasovsky G, & Weingardt K (2012). A randomized controlled trial of telephone motivational interviewing to enhance mental health treatment engagement in Iraq and Afghanistan veterans. General hospital psychiatry, 34, 450–459. doi: 10.1016/j.genhosppsych.2012.04.007 [DOI] [PubMed] [Google Scholar]
- Seal KH, Bertenthal D, Maguen S, Gima K, Chu A, & Marmar CR (2008). Getting beyond “Don’t ask; don’t tell”: an evaluation of US Veterans Administration postdeployment mental health screening of veterans returning from Iraq and Afghanistan. American journal of public health, 98, 714–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharp M-L, Fear NT, Rona RJ, Wessely S, Greenberg N, Jones N, & Goodwin L (2015). Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemiologic reviews, 37, 144–162. [DOI] [PubMed] [Google Scholar]
- Shiner B, Tang C, Trapp AC, Konrad R, Bar-On I, & Watts BV (2014). The provision of mental health treatment after screening: exploring the relationship between treatment setting and treatment intensity. Gen Hosp Psychiatry, 36, 581–588. doi: 10.1016/j.genhosppsych.2014.07.009 [DOI] [PubMed] [Google Scholar]
- Skevington SM, Lotfy M, & O’Connell KA (2004). The World Health Organization’s WHOQOL-BREF quality of life assessment: Psychometric properties and results of the international field trial. A Report from the WHOQOL Group. Quality of Life Research, 13, 299–310. doi: 10.1023/b:qure.0000018486.91360.00 [DOI] [PubMed] [Google Scholar]
- Spoont MR, Nelson DB, Murdoch M, Rector T, Sayer NA, Nugent S, & Westermeyer J (2014). Impact of treatment beliefs and social network encouragement on initiation of care by VA service users with PTSD. Psychiatric Services, 65, 654–662. [DOI] [PubMed] [Google Scholar]
- Spoont MR, Nelson DB, Murdoch M, Sayer NA, Nugent S, Rector T, & Westermeyer J (2015). Are there racial/ethnic disparities in VA PTSD treatment retention? Depression and anxiety, 32, 415–425. [DOI] [PubMed] [Google Scholar]
- Stecker T, Fortney JC, & Sherbourne CD (2011). An intervention to increase mental health treatment engagement among OIF veterans: A pilot trial. Military Medicine, 176, 613–619. [DOI] [PubMed] [Google Scholar]
- Stecker T, McGovern MP, & Herr B (2012). An intervention to increase alcohol treatment engagement: A pilot trial. Journal of substance abuse treatment, 43, 161–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stecker T, McHugo G, Xie H, Whyman K, & Jones M (2014a). A randomized controlled trial of a phone-based cognitive-behavioral intervention to improve PTSD treatment utilization among returning service members. Psychiatric services (Washington, DC), 65, 1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stecker T, McHugo G, Xie H, Whyman K, & Jones M (2014b). RCT of a brief phone-based CBT intervention to improve PTSD treatment utilization by returning service members. Psychiatric Services, 65, 1232–1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsan JY, Zeber JE, Stock EM, Sun F, & Copeland LA (2012). Primary care–mental health integration and treatment retention among Iraq and Afghanistan war veterans. Psychological Services, 9, 336. [DOI] [PubMed] [Google Scholar]
- Ustün T (1999). The global burden of mental disorders. American journal of public health, 89, 1315–1318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenstein M, Gorman L, Blow AJ, Ganoczy D, Walters H, Kees M, … Wadsworth SM. (2014). Reported barriers to mental health care in three samples of US Army National Guard soldiers at three time points. Journal of traumatic stress, 27, 406–414. [DOI] [PubMed] [Google Scholar]
- Vogel DL, Wade NG, & Haake S (2006). Measuring the self-stigma associated with seeking psychological help. Journal of Counseling Psychology, 53, 325. [Google Scholar]
- Vogt D, Di Leone BA, Wang JM, Sayer NA, Pineles SL, & Litz BT (2014). Endorsed and Anticipated Stigma Inventory (EASI): A tool for assessing beliefs about mental illness and mental health treatment among military personnel and veterans. Psychological Services, 11, 105. [DOI] [PubMed] [Google Scholar]
- Vogt D, Fox AB, & Di Leone BA (2014). Mental health beliefs and their relationship with treatment seeking among US OEF/OIF veterans. Journal of traumatic stress, 27, 307–313. [DOI] [PubMed] [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, & Kessler RC (2005). Twelve-month use of mental health services in the united states: Results from the national comorbidity survey replication. Archives of General Psychiatry, 62, 629–640. doi: 10.1001/archpsyc.62.6.629 [DOI] [PubMed] [Google Scholar]
- Watts BV, Schnurr PP, Zayed M, Young-Xu Y, Stender P, & Llewellyn-Thomas H (2015). A randomized controlled clinical trial of a patient decision aid for posttraumatic stress disorder. Psychiatric Services, 66, 149–154. [DOI] [PubMed] [Google Scholar]