Abstract
Objective:
Assess and analyse the awareness, knowledge, and attitudes of university students regarding HPV and its vaccine.
Methods:
A cross-sectional study was designed with questionnaire serving as the research instrument. A total of 425 university students were recruited voluntarily. Thirteen assessable questions were analysed to reveal the mean total knowledge score of HPV and its vaccine. Both descriptive and statistical approach were employed to analyse the research outcomes.
Results:
Students were moderately aware as 59.8% and 49.6% have heard about HPV and its vaccine, respectively. The mean total knowledge score was 5.26 ± 3.10 out of 13 which was found to be moderately knowledgeable. Female (N= 235) have a significantly higher mean knowledge score in comparison to male (N= 190) at 5.58 ± 2.80 versus 4.87 ± 3.40, respectively (p<0.05), likely due to the disease profiles favouring female. As hypothesised, health-related school students (N= 171) outperformed other schools (N= 254) at 7.00 ± 2.95 versus 4.10 ± 2.62, respectively (p<0.001). In general, the score depends on participant’s gender and educational background (χ2= 25.426, p<0.01 and χ2= 105.337, p<0.001, respectively). Despite low vaccination uptakes (28.5%), students accept the vaccine following physician’s recommendation and reject due to its cost. A positive attitude was seen as majority (88.7%) wished to know more about HPV.
Conclusion:
Moderation in awareness, knowledge and attitudes reflect the lifestyle of an urbanised population where information is accessible. Healthcare professionals, media campaign, and educational talk refinement are therefore essential in controlling the disease by spreading awareness.
Key Words: Human Papillomavirus (HPV)- cervical cancer- vaccine- perceptions- students
Introduction
With more than half a million of incidence worldwide, cervical cancer is one of the most common female cancers globally (Bruni et al., 2016). Recent estimation suggests that 2,145 cases were reported in Malaysia alone, with 29% mortality rate. Elderly Malaysian women were found to be the most vulnerable age-based group affected due to the delayed carcinogenesis profile of the disease (Bruni et al., 2017). In short, nearly all the reported cases of cervical cancer were found to be HPV-mediated.
In the context of sexually transmitted infection (STI), HPV is a double-stranded DNA (dsDNA) virus transmissible by unprotected sexual activity through micro-abrasion (Tomaić, 2016). Endocytosis towards the host’s basal cell layer of cervical stratified-squamous epithelium induces viral replication, and the integration of its genetic material into the host’s genome separates the nature of HPV classification. High-risk HPV (HRHPV) integrate its genetic material towards host DNA and disrupts normal cell cycle regulators via transcribed HPV oncoprotein while low-risk HPV (LRHPV) are incapable for integration (Gómez and Santos, 2007; Tomaić, 2016). As the name suggests, HRHPV are the main causative agent responsible for near all the anogenital cancers affecting both gender in Malaysia (Bruni et al., 2017).
As endocytosis requires viral antigen and host receptor interaction, this simple yet vulnerable step serves as one of the aetiologies in preventing the crucial event of the pathogenesis. Antibodies produced by the host or exogenous administration neutralise this docking mechanism to prevent further action (Franco and Harper, 2005). Extensive research has been done to test this hypothesis, until 2006 when the first vaccine was approved by USFDA for use (Stanley, 2010). Together with the screening programme, it has been shown to be effective in preventing cervical cancer for sexually active young adults, despite minimal responses in the US alone (Lauri et al., 2013). Costless vaccination program has been established worldwide to reverse the insignificant uptake rate, including Malaysia back in 2010 (Zaridah, 2014).
Research has to be conducted to evaluate and promote public awareness and knowledge regarding HPV and its consequences, especially in a conservative country like Malaysia, where STI-related matter is considered taboo for discussion (Wong et al., 2009). Utilising cross-sectional design, various local studies claimed that university students were found to be the least aware group in comparison to secondary school students and general public. Further questioning revealed that the cost, safety and efficacy of the vaccine hinder vaccination acceptance (Wong and Sam, 2009; Chung et al., 2011; Ng et al., 2014; Jalani et al., 2016; Wong et al., 2016).
Most of the studies mentioned took place either in rural areas and/or have a limited access to the knowledge of HPV and its vaccine, where the measured level of their knowledge was well-correlated with the unfamiliarity of the topic. Hence, we aim to evaluate the level of awareness, knowledge and attitudes of HPV and its vaccine within university student scope in urban area. We hypothesised that the readily available information about HPV should familiarise students about HPV and its consequences. In addition, spreading the awareness and knowledge about HPV and its vaccine hopefully bring further initiative to direct the population in accepting all preventable measures, which we had done by providing a short discussion following participation.
Materials and Methods
Research Methodology
Study design
We employed a cross-sectional design to carry out the research in one of the private universities in Selangor, Malaysia. In short, a set of validated research questionnaire and consent form were formulated as previously described (Rashwan et al., 2011; Hammar and Stridh, 2013). Evaluation of both awareness, knowledge and attitudes was based on the given responses. Only consented students from the university were eligible to participate in this study, excluding all the university staff and non-university students. Further parameters were derived as we proceed with the study, including gender, year of study, and subject based analysis.
Research Instrument and approach
A questionnaire consisting of 4 sections was constructed to reveal participants’ sociodemographic information, awareness and knowledge of HPV and its vaccine, and the attitudes towards the vaccination. The questionnaire was pretested online towards students (N= 30) beforehand and revised to university students’ level of understanding (Cronbach’s alpha value > 0.70) . Research components were thoughtfully considered to ensure standard research protocols by excluding all potentially-offensive words. In addition to ethic approval (reference number: HEC20171001), a consent form was also generated to further ensure their voluntary involvement in this present study. Our calculation revealed a minimum of 384 participations to satisfy the statistical power (Charan and Biswas, 2013; Jalani et al., 2016). Simple random sampling was performed by approaching random students for a 3-months period from April to June 2017 within the university grounds. The questionnaire was also disseminated over the closed-University group online to boost the responses. Elaboration of HPV information was given following completion to ensure their knowledge remains up to date.
Data collection and analysis
Participants’ demographic distribution was visualised in the first section of the questionnaire, followed by a total of 13 questions in the second and third sections revealing individual knowledge level. Each correct response worth a point while unattempted or incorrect responses worth no mark. Hence, a possible range of 0 – 13 marks are expected to assess students’ knowledge regarding HPV and its vaccine. The mean knowledge score can be grouped as poor (0 – 4), moderate (5 – 9), and knowledgeable (>10) to help us analyse the result, as previously described (Ng et al., 2014; Rashwan et al., 2011).
Collected data were then constructed in a spreadsheet and statistical analysis was performed by utilising Statistical Package for Social Science (SPSS) Version 23.0 for Mac (IBM Corp., United States). The questionnaire was pretested by validity and reliability test (Cronbach’s alpha test). Each data set was then statistically described and mean-compared using Student’s T-test. Chi-square test was employed to analyse the data behaviour to check relationship between categorical data. The collected data has never been revealed to any parties and only used for the purpose of the study itself.
Results
Sociodemographic profile
A total of 425 participants had agreed to participate with the distribution of 300 approached students and 125 online responses. In short, female predominates male in terms of frequency (55.3% and 44.7%, respectively). The majority of students (56.7%) claimed to be within 21-24 years old. Ethnicity profile revealed Chinese to be the major ethnical group (54.1%), followed by Malay (17.4%), Indian (12.9%), and other races (15.6%). More than half of the participants (59.8%) were non-health related school students while 40.2% were health related school students (School of Medicine, School of Pharmacy and School of Biosciences). Most of the respondents were in their second-year (41.6%), followed with first-year (26.8%) and third-year students (24.0%). Only 8 participants (1.9%) were found to be in their post-graduate year. Lastly, 24.0% of research populations had previous sexual intercourse engagement while 76.0% had not. The key characteristic of the mentioned figures can be found in Table 1.
Table 1.
Key Characteristic of Participants’ Sociodemographic. Percentage was Expressed Vertically for Each Characteristic
| Characteristic | Total Sample (N= 425) | Heard of HPV (Yes) (N= 254; 59.8%) |
Heard of HPV Vaccine (Yes) (N= 210; 49.6%) |
HPV-Vaccinated (N = 121; 28.5%) |
|---|---|---|---|---|
| Gender | ||||
| Male | 190 (44.7%) | 89 (35.0%) | 74 (35.2%) | 17 (14.0%) |
| Female | 235 (55.3%) | 165 (65.0%) | 136 (64.8%) | 104 (86.0%) |
| Ethnicity | ||||
| Chinese | 230 (54.1%) | 140 (55.1%) | 109 (51.9%) | 70 (57.9%) |
| Malay | 74 (17.4%) | 44 (17.3%) | 37 (17.6%) | 18 (14.9%) |
| Indian | 55 (12.9%) | 32 (12.6%) | 35 (16.7%) | 21 (17.4%) |
| Others | 66 (15.6%) | 38 (15.0%) | 29 (13.8%) | 12 (9.9%) |
| Education Background | ||||
| Health-related Schools | 171 (40.2%) | 145 (57.1%) | 122 (58.1%) | 45 (37.2%) |
| Others | 254 (59.8%) | 109 (42.9%) | 88 (41.9%) | 76 (62.8%) |
| Education Years | ||||
| First year | 114 (26.8%) | 66 (26.0%) | 50 (23.8%) | 48 (39.7%) |
| Second year | 177 (41.6%) | 98 (38.6%) | 87 (41.4%) | 47 (38.8%) |
| Third year | 102 (24.0%) | 69 (27.2%) | 56 (26.7%) | 17 (14.0%) |
| Fourth year | 24 (5.6%) | 15 (5.9%) | 12 (5.7%) | 5 (4.1%) |
| Postgraduate year | 8 (1.9%) | 6 (2.4%) | 5 (2.4%) | 4 (3.3%) |
| Sexual Intercourse Exposure | ||||
| Had been | 102 (24.0%) | 64 (25.2%) | 55 (26.2%) | 25 (20.7%) |
| Had not | 323 (76.0%) | 190 (73.8%) | 155 (73.8%) | 96 (79.3%) |
University students possess moderate awareness about HPV and its vaccine
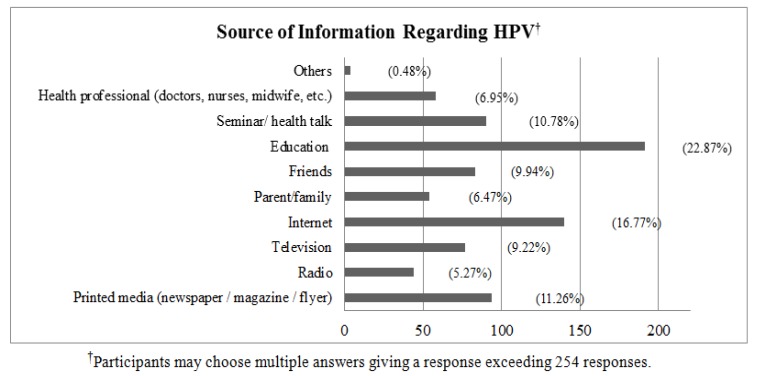
We identified approximately half of the research population have heard about HPV (59.8%) and its vaccine (49.6%), despite low vaccination uptake rates (28.5%; Table 1). It is noteworthy to address that female was found to be superior in term of previous HPV and vaccine information at 65.0% and 64.8%, respectively, in comparison to male (35% and 35.2% respectively). Further assessment revealed that majority (22.9%) had access to HPV-related information from their education, followed by internet (16.8%) printed media such as newspaper, magazine, and leaflet (11.2%), health talk (10.8%), and other sources (Figure 1).
Figure 1.
Summary of Source of Information the Participants Obtained for Those Who Have Heard HPV Prior to the Study. Participants who never heard of HPV before had to choose the questionnaire as their source of information, giving a response of 171 (40.24%)
University students possess a moderate knowledge level of HPV and its vaccine
Overall, research participants have demonstrated a moderate level of knowledge regarding HPV and its vaccine with a mean total score of 5.26 ± 3.10 out of 13. We formulated two additional variables to check the fidelity of our data by grouping the total knowledge level based on students’ gender and their chosen subject. We identified that female had a higher total mean knowledge score in comparison to male (5.58 ± 2.80 versus 4.87 ± 3.40, respectively; p< 0.05; Table 2). Subject-wise, health-related school students had a higher knowledge compared to other schools (7.00 ± 2.95 versus 4.10 ± 2.62, respectively; p< 0.001). Question-structured responses from the participants with said variable are tabulated in Table 2. Chi-square analysis was employed to check the dependency relationship of each variable suggesting that both gender and education background serve as a predictor of the knowledge level of HPV and its vaccine (χ2 = 25.426, p< 0.01 and χ2= 105.337, p< 0.001, respectively).
Table 2.
Percentage of Correct Response Answered by Participants in Gender and Educational Background Perspective
| Statement | Correct responses (%) |
p-value |
Correct responses (%) |
p-value |
||
|---|---|---|---|---|---|---|
| Male | Female | Health-related school | other schools | |||
| HPV can cause cervical cancer. | 36.5 | 63.5 | 0.009** | 59.1 | 40.9 | p<0.001*** |
| HPV is a type of sexually transmitted disease (STD). | 41.1 | 58.9 | 0.007** | 52.8 | 47.2 | |
| HPV does infect male and female equally. | 45.7 | 54.3 | 0.509 | 42.8 | 57.2 | 0.011* |
| Antibiotic is the treatment for HPV infection. | 40.7 | 59.3 | 0.432 | 62.3 | 37.7 | |
| HPV can be prevented by using condom during sexual intercourse. | 37.8 | 62.2 | 0.201 | 58 | 42 | |
| A simple screening test (pap smear) can be done to diagnose cervical cancer. | 38.5 | 61.5 | 0.036* | 55 | 45 | |
| Its important for women to be screened regarding HPV infection on a timely basis. | 40 | 60 | 0.017* | 47.7 | 52.3 | p<0.001*** |
| HPV is very common in Malaysia. | 38.7 | 61.3 | 0.045* | 60.5 | 39.5 | |
| People who are infected has a visible sign and symptom. | 48.2 | 51.8 | 0.005** | 60 | 40 | |
| Under circumstances, the vaccination is offered free in government hospital setting. | 39.3 | 60.7 | 0.039* | 51.5 | 48.5 | |
| Taking vaccine after infection has the same effectiveness as taking it before exposure to HPV. | 42.3 | 57.7 | 0.688 | 58.9 | 41.1 | |
| The vaccine gives a lifetime protection against HPV. | 41.9 | 55.3 | 0.491 | 46.5 | 53.5 | 0.094 |
| Only female could take the vaccine. | 56.2 | 43.8 | 0.001*** | 43.8 | 56.2 | 0.003** |
| Mean total knowledge score | 4.87 ± 3.40 | 5.58 ± 2.80 | 0.021* χ2 = 25.43 p<0.01** |
7.00 ± 2.95 | 4.10 ± 2.62 | p<0.001*** χ2 = 105.38 p<0.001*** |
p<0.05;
p<0.01;
p<0.001
Attitudes towards HPV vaccination programme
Our data demonstrated that the participants’ agreed to be vaccinated following healthcare professional’s suggestion (27.4%), followed by parental or partner’s force (22.6%) and self-awareness regarding HPV infection (22.5%; Table 3). To the contrary, participants refused the vaccine mainly due to the pricing (27.2%), followed by unawareness of the vaccine (19.6%), the safety and efficacy of the vaccine (15.9%), self-embarrassment (14.6%) and inability to bare 3 injections at a different time frame (12.8%). Minority (4.3%) stated that parental restriction serves as a burden to get HPV vaccinations (Table 3). We explored participant’s willingness to be more educated about HPV-related information and found that the majority (88.7%) wished to be more educated about HPV knowledge while 11.3% of them refused to know more about HPV, without any specified reasoning.
Table 3.
Participant’s Attitude Towards HPV Vaccination
| Statements | Frequency |
|---|---|
| Acceptance statements† | |
| Suggested by healthcare professional. | 217 (27.4%) |
| Benefits of vaccination regardless of the pricing. | 118 (14.9%) |
| I can be sexually active to everyone after the injection. |
64 (8.1%) |
| Forced by parent / partner. | 179 (22.6%) |
| Self-awareness regarding HPV infection. | 178 (22.5%) |
| Discounted price of vaccination. | 35 (4.4%) |
| Others. | 1 (0.1%) |
| Refusal statements† | |
| I feel shy to talk about it to my parent/healthcare professional. |
99 (14.6%) |
| I don’t have time to bare 3 injections to the hospital. | 87 (12.8%) |
| My parents do not allow me to take the vaccine. | 29 (4.3%) |
| Safety and efficacy regarding the vaccine. | 108 (15.9%) |
| Price. | 186 (27.2%) |
| I’m not sure where to get the vaccination. | 133 (19.6%) |
| Others | 39 (5.7%) |
| Intentional Attitudes | |
| Willing to be more educated. | 377 (88.7%) |
| Not interested with further elaboration. | 48 (11.3%) |
Difference in response rate is due to the participants’ ability to choose multiple responses
Discussion
The present findings are in line with hypothesis, where the readily access of information reflects the level of perception towards HPV and its vaccine. While we identified more than half of the respondent were aware of HPV and its vaccine, some consideration must be taken into account before concluding our results. Those who aware of the HPV (N= 254; 59.8%) were found to be health-related school students (N=145; 57.1%) and hence made up to the number. It is possible that the nature of their chosen subject has familiarised themselves with HPV-related information, as previously described in one local study assessing the knowledge level exclusive to medical students (Shafei et al., 2014).
On the other hand, we found out that students acquired HPV-related knowledge from the education system (22.9%). Although the elaboration of HPV is reflected by the total knowledge score obtained, various improvements can be addressed to further enhance the present result. For instance, a compulsory health talk for students can be facilitated by inviting experts, or, to our case, social media influencers. With the urban lifestyle, internet seemed to be their second of source to obtain HPV-related information (16.8%). It appears that socio-demographical backgrounds contrasting previous studies conducted in rural area, as they claimed that internet was one of the least informative sources about HPV and its vaccine (Rashwan et al., 2011; Wong et al., 2016). Hence, a short interactive and informative video can be disseminated to attract more awareness in the urban setting while a school-based visits by the health enforcement could be directed in the rural area.
Comparing the knowledge level across gender, we found out that female scored higher in comparison to male. It is possible that the rationale of female’s superiority lies to the fact that the majority of the disease prevalence, campaign preference, and social assumption are skewed towards female population (Ng et al., 2009; Jalani et al., 2016). Through this fact, male ignorance towards HPV and its vaccine overcame the mind set of HPV prevention, as they assume HPV affects female exclusively, or to some extent, herd immunity. In other words, vaccinating female is simply sufficient in controlling disease transmission with normal sexual behaviour assumption. Men-exclusive study by Little et al., (2015) demonstrated the male ignorance towards HPV vaccine and found that only 6.3% of their research population claimed to be vaccinated, which is comparable to our findings at 8.4% of male-population.
In the context of participants’ study background, health-related school students have a higher knowledge score in comparison to other schools (Table 2; p< 0.001). We believe that the extensive exposure towards health subject equipped the knowledge of HPV and its vaccine and thus reflected in their total knowledge score, as previously described (Shafei et al., 2014; Rajiah et al., 2015). Furthermore, Shafei et al., (2014) postulated that educational years affect the knowledge level amongst health-related school students as higher knowledge score was achieved by third-years or more in their study (p< 0.001). We identified a similar conclusion as there were only 22.2% of first-year health-related school students categorised as highly knowledgeable compared to 45.5% of fourth-year students (see Table S1). To further justify our findings, we employed a chi-square analysis and found that the mean total knowledge score was associated by their gender and educational background (χ2= 25.426, p< 0.01 and χ2= 105.337, p< 0.001, respectively). Female and health-related school students are more likely to have a significantly higher knowledge score compared to their counterpart, respectively.
Lastly, participants’ attitudes were assessed to analyse the proper strategy to further increase the awareness and knowledge of HPV and its vaccine. Table 3 suggests that improvements within healthcare services might serve as a key strategy in directing a positive perspective within the society. This rationale is one of the common insights across literature (Perkins and Clark, 2012; Ng et al., 2014). Parental perceptions should be directed as participants agreed to take the vaccine following their guardians’ consent. Previous studies suggested that vaccinated and/or educated parents have the tendency to accept the vaccine and therefore consent for their children (Perkins and Clark, 2012; Awadh et al., 2014; Rajiah et al., 2015).
Positive attitudes were nevertheless seen within research population, given the fact that only minority (8.08%) believed that vaccination encourages sexual engagement as they are now feel protected. During the short discussion session, we have elaborated the coverage of the vaccine which excludes all other STI like the human immunodeficiency virus and others. The present result is somewhat opposing literature stating that more than half (71.7%) agreed with the former statement (Rajiah et al., 2015). However, it is still assumable that there might be confusion with the original statement in the first place.
On the other hand, the price of the vaccine is still a burden for research participants to be vaccinated. In fact, we identified half of both unvaccinated female and total female population to support this claim (See Table S2). Perhaps, the unaffordable pricing is due to their ineligibility towards government programme and the fact that they are yet to receive any income (Hammar and Stridh, 2013; Ng et al., 2014;). Hence, one may voice out a suggestion to the government to subsidise the vaccine price for those who are self-aware yet ineligible individuals. Interestingly, a shift in study population revealed that secondary-school students refused the vaccine due to its delivery profile (intramuscular) which is too painful and inconvenient follow-ups (Wong et al., 2016). Pricing was found to be their least concern as they are the main target of government programme.
Another alarming concern about the vaccine refusal lies to the fact that society (19.6%) were unaware of its availability, which was reflected by a low uptake rate (28.5%). In addition, the safety and efficacy of the vaccine raised a doubt for 15.9% of research population. Hence, improvement-based strategies should be emphasised towards the publicity of the vaccine information. Previous study claimed that visual aid should be reconstructed and critically managed in term of the choice of words, by eliminating any influential word of STI stigma in Malaysia’s perspective (Wong et al., 2009). In addition, focusing on its benefits with gender-neutral expression can be considered while still encouraging male vaccination.
In the future, it is suggested that a more diverse recruitment can be considered, and research area can be greatly expanded to various urban landscapes. Although the majority of the university population was found to be Chinese descendant, we believe our findings are nevertheless reliable and representable to conclude. Due to the time constraint, we were unable to identify parental perspective about HPV and its vaccine. Having such data will enable us to draw further justified rationales about the vaccine attitudes that may have affected the present results, and positively redirect their mind set about vaccination, as addressed in previous study (Awadh et al., 2014). In addition, a follow-up (longitudinal) study can be employed to check the effectiveness of short discussion we have provided after their participation.
In summary, university students with an urban background possess a moderate awareness and knowledge level regarding HPV and its vaccine, where gender and educational background may have determined the said predictor. We identified that female and health-related school participants scored significantly higher than its counterpart due to the disease prevalence and the nature of their study, respectively. Participants accepted the vaccine following healthcare professional guidance and refused it due to the pricing. Improving the healthcare service and media campaign while addressing the vaccine price towards government might raise society awareness and knowledge regarding HPV and its vaccine.
Acknowledgements
The author is beyond grateful for the guidance given by Dr Ooi Yin Yin (YinYin.Ooi@taylors.edu.my) throughout the project and for her valuable input making this article achievable. This research is fully supported under Taylor’s University Final Year Project general funding scheme (2017 round) and made possible by those who participated during data collection.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- Awadh AI, Hassali MA, Al-lela OQ et al. Does an educational intervention improve parents’ knowledge about immunization? Experience from Malaysia. BMC Pediatrics. 2014;14:1–7. doi: 10.1186/1471-2431-14-254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruni L, Barrionuevo-Rosas L, Albero G, et al. Human papillomavirus and related diseases in the world. Summary Report 15 December 2016; ICO Information Centre on HPV and Cancer (HPV Information Centre); 2016. [Google Scholar]
- Bruni L, Barrionuevo-Rosas L, Albero G, et al. Human papillomavirus and related diseases in the Malaysia. Summary Report 27 July 2017; ICO Information Centre on HPV and Cancer (HPV Information Centre); 2017. [Google Scholar]
- Charan J, Biswas T. How to calculate sample size for different study design in medical research? Indian J Psychol Med. 2013;35:121–6. doi: 10.4103/0253-7176.116232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung LK, Teoh S, Rashid AK, et al. Awareness of cervical cancer and HPV vaccination and its affordability among rural folks in penang Malaysia. Asian Pac J Cancer Prev. 2011;12:1429–33. [PubMed] [Google Scholar]
- Franco EL, Harper DM. Vaccination against human papillomavirus infection: A new paradigm in cervical cancer control. Vaccine. 2005;23:2388–94. doi: 10.1016/j.vaccine.2005.01.016. [DOI] [PubMed] [Google Scholar]
- Gómez DT, Santos JL. Human papillomavirus infection and cervical cancer: Pathogenesis and epidemiology. In: A Mendez-Vilas., editor. Communicating Current Research and Educational Topics and Trends in Applied Microbiology. 2007. pp. 680–8. [Google Scholar]
- Hammar S, Stridh S. Knowledge of human papillomavirus (HPV) and attitudes towards HPV-vaccine among Thai female university Students, Bachelor Thesis. Upsalla University, Thailand; 2013. [Google Scholar]
- Jalani FFM, Rani MDM, Isahak I, Aris MSM, Roslan N. Knowledge, attitudes, and practice of human papillomavirus (HPV) among secondary school students in rural areas of Negeri Sembilan, Malaysia. Int J Collab Res Intern Med Public Health. 2016;8:420–34. [Google Scholar]
- Lauri E, Susan H, Carol L. Reduction in human papillomavirus (HPV) prevalence among young women following HPV vaccine introduction in the United States, National Health and Nutrition Examination Surveys, 2003–2010. J Infect Dis. 2013;208:385–93. doi: 10.1093/infdis/jit192. [DOI] [PubMed] [Google Scholar]
- Little KQ, Ogivile G, Mirwaldt P. Human papillomavirus awareness, knowledge, andvaccination status in a diverse population of male postsecondary students in Greater Vancouver. B C Med J. 2015;57:64–9. [Google Scholar]
- Ng BK, Choy MY, Lim PS, et al. Knowledge, perception, and attitudes towards human papillomavirus among Pre-University Students in Malaysia. Asian Pac J Cancer Prev. 2014;15:9917–23. doi: 10.7314/apjcp.2014.15.21.9117. [DOI] [PubMed] [Google Scholar]
- Perkins RB, Clark JA. What affects human papillomavirus vaccination rates? A qualitative analysis of provider’s perception. Womens Health Issues. 2012;22:379–86. doi: 10.1016/j.whi.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Rajiah K, Maharahan MK, Nang SC, Sze KFN. Awareness and acceptance of human papillomavirus vaccination among health science students in Malaysia’. Virus Dis. 2015;26:297–303. doi: 10.1007/s13337-015-0287-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rashwan H, Lubis SH, Kiat AN. Knowledge of cervical cancer and acceptance of HPV vaccination among secondary school students in Sarawak. Asian Pac J Cancer Prev. 2011;12:1837–41. [PubMed] [Google Scholar]
- Shafei MN, Zainon N, Zulkifli NF, Ibrahim MI. Knowledge and perception on human papillomavirus infection and vaccination among medical students of a University in Malaysia. Proc Soc Behav Sci. 2014;116:2707–10. [Google Scholar]
- Stanley M. Human papillomavirus immune response to infection and vaccination. Infect Agent Cancer. 2010;5:1–6. doi: 10.1186/1750-9378-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomaić V. Functional role of E6 and E7 oncoprotein in HPV induced malignancies at diverse anatomical sites. Cancers. 2016;8:1–22. doi: 10.3390/cancers8100095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong LP, Sam IC. Ethnically diverse female university students’ knowledge and attitudes toward human papillomavirus (HPV), HPV vaccination, and cervical cancer. Eur J Obstet Gynaecol Reprod Biol. 2009;148:90–5. doi: 10.1016/j.ejogrb.2009.10.002. [DOI] [PubMed] [Google Scholar]
- Wong LP, Yusoff RNARM, Edib Z, Sam IC, Zimet GD. Nationwide survey of knowledge and health beliefs regarding human papillomavirus among HPV-vaccinated female students in Malaysia. PLoS One. 2016;11:1–11. doi: 10.1371/journal.pone.0163156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaridah S. A review of cervical cancer research in Malaysia. Int Med J Malays. 2014;69:33–41. [PubMed] [Google Scholar]