Abstract
The aim was to identify latent class trajectories of depression symptoms among HIV+ women in Uganda. Depression was assessed at four time points using the Hopkins Symptom Checklist among 288 women caring for a child 2–5 years old. Mixture modeling was used to estimate the number and nature of classes defined by trajectories of depressive symptoms over time. Maternal and child characteristics were explored as predictors of class. Three trajectories of symptoms of depression were identified; 1) stable-low, 2) moderate-subclinical, and 3) chronic-high. About 8% of women reported moderately or highly elevated symptoms at the first assessment and consistently onward (i.e. chronically). Higher anxiety levels, less social support, more functionality problems, and more executive behavior problems in children predicted membership in the moderate-subclinical and chronic-high classes. Identifying patterns of depression trajectories can help target intervention efforts for women who are likely to experience the most chronic and impairing symptomatology.
Keywords: Latent trajectory, women, depression, HIV, low- and middle-income countries (LMIC)
RESUMEN
El objetivo de este estudio fue identificar trayectorias de síntomas depresivos en mujeres HIV+ en Uganda. Evaluamos síntomas de depresión en 288 mujeres usando el Hopkins Symptom Checklist en cuatro ocasiones. Utilizando modelaje mixto, describimos el número y tipo de clases definidas por las trayectorias de síntomas depresivos a través del tiempo, así como las características de la mujer y un hijo índice asociadas con cada clase. Se identificaron tres trayectorias: 1) estable-leve, 2) moderada-sub clínica y 3) crónica-elevada. Aproximadamente 8% de las mujeres reportaron síntomas depresivos moderados o elevados en todas las evaluaciones (síntomas crónicos). Mayores niveles de ansiedad, menor apoyo social, mayores problemas de funcionamiento y mayores problemas de conducta ejecutiva en niños se asociaron con las clases moderada-sub clínica o crónica-elevada. Identificar patrones y trayectorias de síntomas depresivos sirve para enfocar intervenciones a individuos con mayor probabilidad de experimentar síntomas crónicos e incapacitantes.
Keywords: Trayectorias latentes, mujeres, depresión, HIV
INTRODUCTION
Depression is the most common psychiatric disorder among people living with HIV (PLHIV); a meta-analysis of studies in western countries reported that the frequency of depressive symptoms was nearly two times higher among HIV-infected compared non-HIV infected adults (OR=1.99, 95% CI 0.28–1.1, p<0.05) (1). Pooled estimates of depression prevalence among PLHIV reported in a meta-analysis ranged between 9% and 32%(2) with substantial variability given by low socio-economic factors, antiretroviral treatment (ART) and female sex, among others.
Women make up most of PLHIV in Sub-Saharan Africa (SSA) with 71% of the estimated prevalence reported in 2014 (3). Studies from women in high income countries describe the course of depressive symptoms with different levels (i.e. severity) and chronicity (i.e. stability) patterns over time, with some women showing both stable and severe symptoms, others mild but persistent symptoms, and still others declining or episodic symptoms over time (4–6). A systematic review of depression symptoms among women in the perinatal period using latent variable modeling methods found that eight of 11 studies reported three types of trajectories: a stable, a moderate-high and a high symptom trajectory (7). A review of 25 studies examining depressive symptoms over time among non-HIV infected individuals found that chronic depressive symptoms were more likely to occur in females, minorities, and individuals of low socioeconomic and educational status (8), as well as among women who are diagnosed earlier in life and with more severe depressive symptoms (9).
Understanding the trajectories of depression symptoms in women living with HIV is essential to understanding interruptible pathways that can disadvantage child development in HIV-affected families. Negative developmental and behavioral outcomes in children have been linked to the presence of depressive symptoms in their mothers, especially in relationship with symptom severity and chronicity (10). Among women living with HIV, anxiety and stress have been negatively associated with compromised parenting that in turn are negatively associated with child development and behavior, suggesting a possible mechanism of action (11). Chronic depression in women has been found to double the likelihood of child behavioral and emotional disorders in high-income countries (12). Cents et al. assessed 4,167 mother-child dyads in The Netherlands and found that besides severity and chronicity of maternal depression, symptom trajectories (ie. mothers reporting similar patterns of depressive symptoms over time) were an independent predictor of child executive functioning (13).
However, current evidence is mainly restricted to the assessment of depressive symptomatology among women in the post-partum period, or living in high-income countries (7). Given that risk factors for the persistence of depressive symptoms, such as lower educational attainment, poverty, and social support may vary substantially in prevalence and nature in and between low and middle-income countries (LMIC) and among populations affected by HIV, research from more diverse samples that include women living with HIV in SSA are needed to inform services on how and when to identify subgroups of women at high risk for depression(7).
To address the gap in literature, the aim of this study was to model the longitudinal patterns of depressive symptoms among HIV-infected women in rural Uganda. Using mixture modeling, the objectives of analyses were to 1) describe the number and nature of distinct classes defined by the trajectories of depressive symptoms over time, and 2) explore maternal and child characteristics that predicted class membership.
METHODS
This is a secondary analysis using data from 288 HIV-infected women participating in a randomized controlled trial (RCT) that tested the Meditational Intervention for Sensitizing Caregivers (MISC), a one-year program aimed at enhancing child physical and neuropsychological development (14). Details of the parent study are described in Bass et al 2016 (15). Briefly, the RCT was conducted between 2011 and 2014 with women attending health clinics in Tororo District and recruited as caregiver-child dyads into two cohorts: one where the child was living with HIV (n=118), and one where the child was perinatally-exposed to HIV but was uninfected (n=221). Women’s inclusion criteria included being aged 18 or older, the principal caregiver of a child aged 2–5 years, and willing and able to participate in a year of MISC training. For analyses reported here, only HIV-infected women were included (n=228).
The original parent study randomized women to one of two arms: MISC or a treatment-as-usual (TAU) control condition that consisted of basic hygiene, health, and prevention education for PLHIV. As no differences were found by arm for depression in either cohort at baseline, we pooled the two study arms for the present analysis.
After informed consent, participants responded to a questionnaire administered by trained Ugandan research assistants in one of three local languages (Dhopadhola, Ateso, or Luganda) in a private setting. The Institutional Review Board of Michigan State University and the School of Medicine Research Ethics Committee at Makerere University approved this study.
Women and children were assessed at study intake, month 6 (mid-intervention), month 12 (immediate post-intervention), and month 24 (one-year post-intervention follow-up). Women provided information on the following characteristics: age, education level (e.g. highest level of schooling completed), marital status, occupation, and relation to the child. Women’s HIV status was established based on clinical data extracted from medical records. Child HIV status was confirmed during the RCT with an ELISA test.
Women’s depressive and anxiety symptoms were assessed by self-report with the Hopkins Symptom Checklist-25 (HSCL-25)(16, 17), where each symptom is reported for the prior 2 weeks using a 4-point Likert scale ranging from 1 (not at all) to 4 (all the time). The HSCL-15 has previously been adapted and validated among adults in HIV-affected Ugandan communities (18, 19). Average scores were generated for depression (15 item) and anxiety (10 item) subscales, with higher scores indicating more frequent and/or severe symptoms. A cut-off score >1.75 was used to define clinically relevant depression (20). Internal consistency (Cronbach’s alpha) was 0.73 and 0.84 for the depression and anxiety subscales, respectively, which is consistent with previous reports (21).
Perceived social support was assessed using the Multidimensional Scale for Perceived Social Support (MSPSS) (22, 23), previously validated for use in Uganda among HIV-infected and uninfected adults (24) (25). We adapted 8 items from the original family and friends subscales to ask participants about people in their community, instead of referring specifically to friends. Exploratory factor analysis yielded two factors jointly explaining 55% of the variance: 1) “Family Support” (4 items), and 2) “Community Support”, (3 items). One item (Do you quarrel with members of your family) did not load on either factor and had high uniqueness (.79). This item was excluded from further analyses. Each item is scored with a 4-point Likert scale ranging from 0 (never) to 3 (often). Separate scores for family and community support were constructed as averages of the items within the scales, with higher scores indicating better social support. Cronbach’s α for the family and community support subscales were. 77 and .63, respectively.
Women’s functional impairment was measured using a self-report of 16 daily tasks identified during a brief qualitative study that local women regularly do to care for themselves, their family, their community and their young child (26). Caregivers indicated how much difficulty they had completing each task, with response options ranging from 0 (no difficulty at all) to 4 (cannot complete it). Cronbach’s α alpha was .73.
We used the Behavior Rating Inventory of Executive Function–Preschool version (BRIEF-P)(27) to evaluate child behavior, attention, and cognitive disorders related to disruption of executive function as reported by the principal caregiver. The combined Global Executive Composite (GEC) score was used in analyses.
An economic wealth index was constructed from a checklist of 8 material possessions (shoes, radio, mattress, blanket, bicycle, motorcycle, cows, goats) and 6 housing quality items (type of roof, availability of water supply, type of fuel used, frequency of meat in diet and food security). Respondents reported presence/absence of each asset at their homes. Top 20th, middle 60th, and bottom 20th percentiles were defined based on factor scores derived from exploratory factor analysis of the 14 items.
Descriptive statistics were calculated for the outcome of maternal depression, and potential predictors of depression identified in the literature: women’s age, education, socioeconomic status, anxiety, women’s functioning, and child’s executive behaviors.
Finite mixture modeling was used to analyze women’s depression symptoms assessed at intake, and months 6, 12, and 24 after intake. This semi-parametric group-based modeling strategy assumes that a population is comprised of several unobserved subpopulations (i.e. classes). Class membership probabilities are estimated based on pattern of change over time. The following covariates were included in the model: maternal age, education level, and wealth index percentile group; child’s HIV status; and, trial arm to reflect the design of the parent study. Additional predictors of class membership entered into the model were women’s baseline anxiety and functional measures, and child’s executive behaviors at study intake. A censored normal (CNORM) model was used (28) based on the observed distribution of women’s depression symptoms. A series of mixture models with varying numbers of classes were fit in order to assess: a) the optimal number of classes over time, and b) key predictors of class membership. We used the Bayesian Information Criterion (BIC), calculated as the log-likelihood evaluated at the maximum likelihood estimate less one-half the number of parameters in the model times the log of the sample size, to determine the optimal number of classes. The highest BIC was indicative of the best fitting model. Note that in other software such as Mplus, the BIC is calculated as above with a factor of −2, then the lowest BIC indicates the best fit (29). BIC was also used to select the best fitting model (30) based on the optimal number of classes. Probabilities of class membership were estimated, and women were assigned to a latent class based on the highest posterior probability of class membership (31). The analyses were performed in SAS 9.4 using the TRAJ procedure (32).
RESULTS
Demographic characteristics and average depression and anxiety scores reported at baseline are presented in Table I. Women in this sample were on average 33.5 years old (range 18–54 years), majority were married (69%), had a primary-level education (69%), and were subsistence farmers (82%). Using the standard cut-off score >1.75 on the average HSCL-depression score, more than half (61%) of women could be classified as having clinically significant depression at baseline. This is consistent with the overall mean of 2.0 (standard deviation 0.5) for the depressive symptoms at baseline. (Table I).
Table I.
Socio-demographic characteristics, depression and anxiety scores among mothers living with HIV in Tororo, Uganda (n=288)
| Variable | N | % | |
|---|---|---|---|
| Marital status | |||
| Married | 199 | 69 | |
| Single/Divorced | 40 | 14 | |
| Widowed | 49 | 17 | |
| Education level | |||
| None | 56 | 19 | |
| Primary | 190 | 66 | |
| Secondary | 39 | 13 | |
| Technical | 3 | 1 | |
| Employment status | |||
| Farmer | 235 | 82 | |
| Trades/small business/employee | 28 | 10 | |
| Professional | 12 | 4 | |
| Unemployed/house wife | 13 | 4 | |
| Relationship to the child | |||
| Biological mother | 281 | 98 | |
| Other | 7 | 2 | |
| Wealth group | |||
| Lowest 20% | 41 | 14 | |
| Middle 60% | 193 | 67 | |
| Top 20% | 53 | 18 | |
| Probable depression or anxiety | 176 | 61 | |
| OnARV | 232 | 81 | |
| Variable | Mean | SD | Range |
| Age | 33.5 | 5.8 | 18–54 |
| Perceived Social Support | |||
| Family support | 2.1 | 0.7 | 0–3 |
| Community support | 0.7 | 0–3 | |
| Depression score | 2.0 | 0.5 | 1–3.4 |
| Anxiety score | 1.8 | 0.6 | 1–4 |
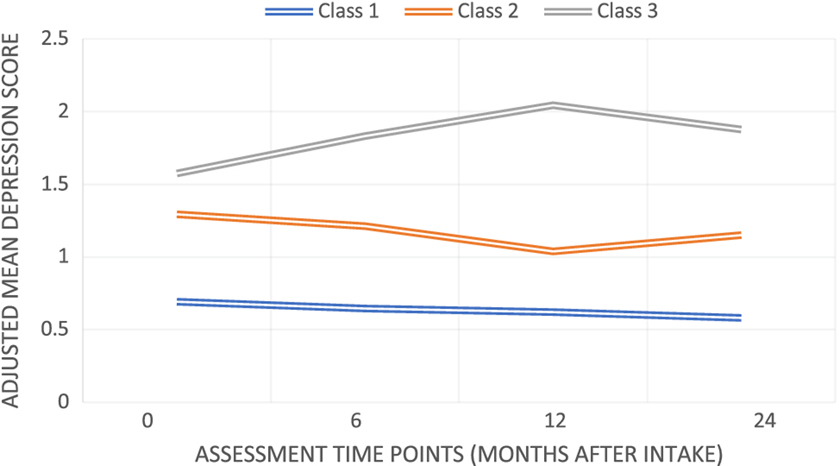
In the analysis of the trajectories of depressive symptoms over time, the BIC was best for a 3-class (−750.91) model, as compared with the 2- (−774.18), 4- (−754.33) and 5- (−763.80) class solutions. This 3-class solution resulted in three distinct trajectories of depression symptoms over time (Figure 1). The two largest classes were characterized by low or moderate subclinical (i.e. mean HSCL score <1.75) symptoms of depression. Class 1 represented the largest percentage of women (53%, n=152). In this class, depression symptoms were low and stable across the 24-month period of the study. Class 2 (39%, n=113) was characterized by moderate subclinical symptoms with varying degrees of intensity over time. Specifically, mean depression scores dropped at the 12-month assessment (when the MISC and TAU interventions stopped), and then rose again to a moderate level at 24 months. A small percentage of women (8%, n=23) were classified in Class 3 given their reported high levels of depression symptoms across the entire 24-month period of the study. Mean depression score among women in this class increased at the 12-month assessment, and returned to the high level reported at baseline, suggesting that their symptoms were relatively chronic and severe. Overall, about 8% of women reported symptoms that were moderately or highly elevated from the first assessment and consistently onward (i.e. chronically).
Figure 1.
Regarding the significance of predictors in the trajectory modeling, the probability of being in a particular trajectory class was not associated with baseline socio-demographic or child characteristics (Table II). In the multivariable mixture model, compared to women with low or moderate subclinical depression (Class 1), women who reported moderate (e.g. Class 2) and consistently high symptoms of depression (e.g. Class 3) were both more likely to report greater symptoms of anxiety at baseline (2.49, SE= 0.47, p<0.01; 3.09, SE=0.61, p<0.01, respectively). Women with moderate symptoms (Class 2) were more likely to report greater functional impairment (1.39, SE= 0.65, p=0.03), less family support (−0.76, SE= 0.31, p=0.02), and more child behavioral problems (0.05, SE=0.02, p<0.01) compared to women in the low or moderate subclinical class. The unadjusted comparisons of the three classes yielded similar conclusions (Table III), with the exception of a significant association of wealth with class membership when not controlling for other factors.
Table II.
Predictors of latent class membership: coefficients from the multivariable finite mixture model, their standard errors (SEs), and p-values
| Predictor | Class 2 versus Class 1 | Class 3 versus Class 1 | ||
|---|---|---|---|---|
| Coefficient (SE) | P-value | Coefficient (SE) | P-value | |
| Caregiver age | 0.00 (0.04) | .99 | −0.04 (0.05) | .44 |
| Exposed child HIV status v. infected |
0.76 (0.50) | .13 | 1.53 (0.93) | .10 |
| MISC trial arm v. TAU trial arm | 1.25 (0.44) | .57 | 1.62 (0.78) | .04 |
| Wealth group | 0.15 (0.36) | .66 | −0.50 (0.56) | .38 |
| Caregiver functional impairment | 1.40 (0.65) | .03 | 1.40 (0.95) | .14 |
| Caregiver anxiety | 2.49 (0.46) | <.01 | 3.09 (0.61) | <01 |
| Family support | −0.76 (0.31) | .02 | −0.32 (0.45) | .49 |
| Global Executive Composite score (BRIEF) |
0.05 (0.02) | <.01 | 0.02 (0.02) | .37 |
Table III.
Caregiver and child characteristics by caregiver depression class: unadjusted means and frequencies
| Caregiver Depression Class | P-value* | |||
|---|---|---|---|---|
| Low stable N (%) or Mean (SD) | Moderate intermittent N (%) or Mean (SD) | High chronic N (%) or Mean (SD) | ||
| Caregiver age | 33. (59) | 33.61 (5.91) | 32.17 (5.65) | .53 |
| HIV infected child | 50 (33%) | 39 (35%) | 3 (13%) | .12 |
| HTV exposed child | 102 (67%) | 74 (66%) | 20 (87%) | |
| TAU trial arm | 86 (57%) | 58 (51%) | 5 (22%) | .01 |
| MISC trial arm | 66 (43%) | 55 (49%) | 18 (78%) | |
| MISC trial arm | 66 (43%) | 55 (49%) | 18 (78%) | |
| Wealth group 1 | 22 (14%) | 28 (25%) | 9 (39%) | .01 |
| Wealth group 2 | 89 (59%) | 67 (59%) | 12 (52%) | |
| Wealth group 3 | 41 (27%) | 18 (16%) | 2 (9%) | |
| Functional impairment score | 0.23 (0.29) | 0.47 (0.42) | 0.35 (0.28) | <.01 |
| Anxiety score | 0.54 (0.41) | 1.22 (0.58) | 1.61 (0.69) | <.01 |
| Family support | 2.25 (0.67) | 1.89 (0.79) | 2.25 (0.40) | <.01 |
| Global Executive Composite score (BRIEF) |
62.61 (13.61) | 71.19 (12.99) | 66.09 (13.96) | <.01 |
P-value for the difference in means
DISCUSSION
Using latent variable methods, we identified three distinct trajectories of depressive symptoms over a two-year period in a group of women living with HIV in rural Uganda; 1) stable-low, 2) moderate-subclinical, and 3) chronic-high. Results suggest that depression symptoms in this population are heterogeneous, in line with previous studies describing depressive symptom trajectories that vary in terms of severity (low, medium, high) and stability (stable or unstable) (35–36). To the best of our knowledge, this is the first study to examine depressive symptom trajectories among a sample of women living with HIV in sub-Saharan Africa. Results from this analysis show that high symptom burden trajectories were associated with less family support and more functional impairment.
The instability of depression symptoms over time was more frequent than stability, especially in the moderate and high symptom classes. Transient trajectories (eg. increasing, decreasing or episodic) seem to be frequent patterns; a systematic review of studies of depression symptom trajectories in the general population found that six out of 11 studies included reported these type of trajectories (7). However, the proportion of individuals falling in unstable trajectories is highly variable, with reviews reporting ranges between 2.4–37% for increasing symptoms and from 2.1–71% for decreasing symptoms (8).
The majority of women in this sample had minimal or low depressive symptoms over time (Classes 1 and 2). Only a small proportion of the sample (< 10%) had a trajectory characterized by moderate or chronic depressive symptoms. Women following this type of trajectory had more anxiety symptoms, less functionality, and less family support. None of the demographic or socio-economic characteristics investigated differentiated groups of women with different depression trajectories. This finding underscores the importance of family support in this context and the need to increase the availability of social and tangible resources that may improve self-esteem and women’s sense of well-being. This might prove to be a potential strategy for mental health promotion and prevention of depression among women living with HIV, as even informal social networks can be an important resource for coping (33).
More than half (61%) of the sample had a depression score considered clinically meaningful symptomatology, which is higher than the pooled prevalence of depressive symptoms using the HSCL among PLWH on ART summarized in a meta-analysis of studies from Sub-Saharan Africa (13%, 95% CI:11–15) (2). As depression symptoms can have deleterious consequences on women’s life and child development, this high prevalence of depressive symptoms should prompt local stakeholders into revising and expanding efficient screening and management programs that can be integrated into services for this population. For example, integrated programs combining early childhood development curriculums with maternal psychological well-being support have been successful in reducing depression symptoms and bolstering child neurodevelopment in LMIC (34, 35).
The persistence of high depression symptoms in 8% of the sample is within the rate of <10% reported in a meta-analysis of studies from western countries in general population samples (8). To some extent, this finding is surprising given that other studies have found greater symptom burden among samples of PLWH (1) and increased risk in women (OR= 1.23; 95% CI: 1.56–1.93) (36). One possibility is that women in our sample benefited from their participation in the home-based child-development intervention. This program required 60-minute visits twice a month for 12 months, creating a predictable and reliable bond between the participant and her program facilitator. Trial results showed that women in both intervention and control arms experienced improvements in mental health (lower anxiety and depression symptoms) and functionality over time (37). However, as Sherr and colleagues (38) recently reviewed in 90 studies from mostly North America and Europe, depression prevalences among PLWH can range widely (from 0 to 80%) depending on the instrument and cut-off used.
Results show that higher rates of behavior problems in infants independently predicted more severe and chronic depression trajectory in their mothers. Several mechanisms could explain this association, including 1) an actual increase in child behavior problems due to maternal depressive symptomatology (39), 2) a negative perception bias in the mother, leading to over-reporting of child adjustment difficulties (40), or 3) the possibility that child behavior problems worsen or precipitate depression symptoms in the mother. These opposing models were extensively discussed in the seminal report by Richters (41) and the debate was more recently picked up by Ordway (42) in an integral review highlighting the methodological challenges of maternal report of child behavior. Overall, these reports underscore the need to incorporate multiple informants when assessing child behavior, as well as contextual factors related to depressive symptomatology in mothers that can guide our understanding of maternal reports of child behavior.
One of the strengths of this manuscript is the use of latent class analyses over traditional longitudinal assessment. This type of methodology allows the identification of subgroups of women with different depression profiles. Findings can be used to tailor mental health screening, prevention, and treatment strategies for women living with HIV. For example, women in this sample reporting low family support and high anxiety symptoms were more likely to have high and sustained depression symptomatology throughout the 24-months of follow-up (Class 3). This sub-group of women would likely benefit the most from depression treatment (43). On the other hand, women with high functionality (e.g. were employed) and less symptoms are likely candidates for general supportive services that decrease social isolation and buffer some of the effects of living with HIV. Given the prevailing context of significant under-funding of mental health services and research, integrating mental health screening into existing infrastructure and programs that allow targeting of services to sub-groups of women who most need them is essential.
A few limitations should be considered. All data were collected by self-report and thus social desirability bias may have led to underreporting, or similarly worded items may have influenced women to respond consistently regardless of actual experience. However, this effect is likely to have remained consistent over time and thus provided acceptable assessment of symptom change. Although social and economic factors were included as predictors of depression symptom trajectories, other recognized risk factors such as trauma, stigma, violence and abuse were not included. In particular, bereavement, maternal role difficulties, HIV-related social isolation, partner conflict, and stigma have all been to be associated with changes over time in depression symptoms among women living with HIV in high income countries (44, 45). While these issues were not explored in this study, they remain important avenues for future research. Finally, the use of secondary data limits the interpretation of findings since data are constrained by the original study design.
Despite limitations, information on depression symptom trajectories can aid in targeting preventive and intervention efforts that are specific to women living with HIV in low resource settings such as Uganda, particularly those that may experience chronic or recurring symptoms in the absence of treatment. More prospective studies that extend through points in development across life phases of women, delineate the trajectory of depressive symptoms, and identify factors that may be associated with increases in depressive symptoms in subgroups of women are needed.
Acknowledgments
We wish to thank the participants and the Global Health Uganda-Tororo team that made this research possible. This research was supported by NIH grant R01 HD070723. SM was supported by NIMH of the National Institutes of Health under award number T32MH10321.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- 1.Ciesla JA, Roberts JE. Meta-analysis of the relationship between HIV infection and risk for depressive disorders. The American Journal of Psychiatry. 2001;158(5):725–30. [DOI] [PubMed] [Google Scholar]
- 2.Bernard C, Dabis F, de Rekeneire N. Prevalence and factors associated with depression in people living with HIV in sub-Saharan Africa: A systematic review and meta-analysis. PLoS One. 2017;12(8):e0181960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.UNAIDS U. The gap report. Geneva, Switzerland: 2014. [Google Scholar]
- 4.Kessing LV. Severity of depressive episodes during the course of depressive disorder. Br J Psychiatry. 2008;192(4):290–3. [DOI] [PubMed] [Google Scholar]
- 5.Otto MW, Teachman BA, Cohen LS, Soares CN, Vitonis AF, Harlow BL. Dysfunctional attitudes and episodes of major depression: Predictive validity and temporal stability in never-depressed, depressed, and recovered women. J Abnorm Psychol. 2007;116(3):475–83. [DOI] [PubMed] [Google Scholar]
- 6.Bengtson AM, Pence BW, Powers KA, Weaver MA, Mimiaga MJ, Gaynes BN, et al. Trajectories of Depressive Symptoms Among a Population of HIV-Infected Men and Women in Routine HIV Care in the United States. AIDS Behav. 2018;22(10):3176–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baron E, Bass J, Murray SM, Schneider M, Lund C. A systematic review of growth curve mixture modelling literature investigating trajectories of perinatal depressive symptoms and associated risk factors. Journal of affective disorders. 2017;223:194–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Musliner KL, Munk-Olsen T, Eaton WW, Zandi PP. Heterogeneity in long-term trajectories of depressive symptoms: Patterns, predictors and outcomes. J Affect Disord. 2016;192:199–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pereverseff RS, Beshai S, Dimova M. First episode indices associated with lifetime chronicity of depression among formerly depressed participants: an exploratory study. J Ment Health. 2017:1–7. [DOI] [PubMed] [Google Scholar]
- 10.Goodman SH, Gotlib IH. Risk for psychopathology in the children of depressed mothers: a developmental model for understanding mechanisms of transmission. Psychol Rev. 1999;106(3):458–90. [DOI] [PubMed] [Google Scholar]
- 11.Murphy DA, Marelich WD, Armistead L, Herbeck DM, Payne DL. Anxiety/stress among mothers living with HIV: effects on parenting skills and child outcomes. AIDS Care. 2010;22(12):1449–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Giallo R, Woolhouse H, Gartland D, Hiscock H, Brown S. The emotional-behavioural functioning of children exposed to maternal depressive symptoms across pregnancy and early childhood: a prospective Australian pregnancy cohort study. Eur Child Adolesc Psychiatry. 2015;24(10):1233–44. [DOI] [PubMed] [Google Scholar]
- 13.Cents RA, Diamantopoulou S, Hudziak JJ, Jaddoe VW, Hofman A, Verhulst FC, et al. Trajectories of maternal depressive symptoms predict child problem behaviour: the Generation R study. Psychol Med. 2013;43(1):13–25. [DOI] [PubMed] [Google Scholar]
- 14.Boivin MJ, Bangirana P, Nakasujja N, Page CF, Shohet C, Givon D, et al. A year-long caregiver training program improves cognition in preschool Ugandan children with human immunodeficiency virus. J Pediatr. 2013;163(5):1409–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bass JK, Nakasujja N, Familiar-Lopez I, Sikorskii A, Murray SM, Opoka R, et al. Association of caregiver quality of care with neurocognitive outcomes in HIV-affected children aged 2–5 years in Uganda. AIDS Care. 2016;28 Suppl 1:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hesbacher PT, Rickels K, Morris RJ, Newman H, Rosenfeld H. Psychiatric illness in family practice. J Clin Psychiatry. 1980;41(1):6–10. [PubMed] [Google Scholar]
- 17.Winokur A, Winokur DF, Rickels K, Cox DS. Symptoms of emotional distress in a family planning service: stability over a four-week period. Br J Psychiatry. 1984;144:395–9. [DOI] [PubMed] [Google Scholar]
- 18.Bolton P, Bass J, Neugebauer R, Verdeli H, Clougherty KF, Wickramaratne P, et al. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289(23):3117–24. [DOI] [PubMed] [Google Scholar]
- 19.Kaida A, Matthews LT, Ashaba S, Tsai AC, Kanters S, Robak M, et al. Depression during pregnancy and the postpartum among HIV-infected women on antiretroviral therapy in Uganda. J Acquir Immune Defic Syndr. 2014;67 Suppl 4:S179–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. Prevalence and risk factors of major depressive disorder in HIV/AIDS as seen in semi-urban Entebbe district, Uganda. BMC Psychiatry. 2011;11:205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mollica RF, Sarajlic N, Chernoff M, Lavelle J, Vukovic IS, Massagli MP. Longitudinal study of psychiatric symptoms, disability, mortality, and emigration among Bosnian refugees. JAMA : the journal of the American Medical Association. 2001;286(5):546–54. [DOI] [PubMed] [Google Scholar]
- 22.Dahlem NW, Zimet GD, Walker RR. The Multidimensional Scale of Perceived Social Support: a confirmation study. J Clin Psychol. 1991;47(6):756–61. [DOI] [PubMed] [Google Scholar]
- 23.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess. 1990;55(3–4):610–7. [DOI] [PubMed] [Google Scholar]
- 24.Nakigudde J, Musisi S, Ehnvall A, Airaksinen E, Agren H. Adaptation of the multidimensional scale of perceived social support in a Ugandan setting. Afr Health Sci. 2009;9 Suppl 1:S35–41. [PMC free article] [PubMed] [Google Scholar]
- 25.Nakimuli-Mpungu E, Musisi S, Katabira E, Nachega J, Bass J. Prevalence and factors associated with depressive disorders in an HIV+ rural patient population in southern Uganda. J Affect Disord. 2011;135(1–3):160–7. [DOI] [PubMed] [Google Scholar]
- 26.Bass J, Neugebauer R, Clougherty KF, Verdeli H, Wickramaratne P, Ndogoni L, et al. Group interpersonal psychotherapy for depression in rural Uganda: 6-month outcomes. The British Journal of Psychiatry. 2006;188(6):567–73. [DOI] [PubMed] [Google Scholar]
- 27.Gioia GA, Isquith PK. Behavior rating inventory for executive functions. Springer; New York; 2011. [Google Scholar]
- 28.Nagin D, Tremblay RE. Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Dev. 1999;70(5):1181–96. [DOI] [PubMed] [Google Scholar]
- 29.Muthen LK, Muthen BO. Mplus User’s Guide. Sixth Edition. Los Angeles CA: (1998–2011). [Google Scholar]
- 30.Schwarz G Estimating the dimension of a model. The annals of statistics. 1978;6(2):461–4. [Google Scholar]
- 31.Vermunt JK, Magidson J. Latent class cluster analysis. Applied latent class analysis. 2002; (11) 89–106. [Google Scholar]
- 32.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological methods & research. 2001;29(3):374–93. [Google Scholar]
- 33.Casale M ‘I am living a peaceful life with my grandchildren. Nothing else. ‘Stories of adversity and ‘resilience’ of older women caring for children in the context of HIV/AIDS and other stressors. Ageing and Society. 2011;31(08):1265–88. [Google Scholar]
- 34.Singla DR, Kumbakumba E, Aboud FE. Effects of a parenting intervention to address both maternal psychological wellbeing and child development and growth in rural Uganda: a community-based, cluster randomised trial. The Lancet Global health. 2015;3(8):e458–69. [DOI] [PubMed] [Google Scholar]
- 35.Boivin MJ, Nakasujja N, Familiar-Lopez I, Murray SM, Sikorskii A, Awadu J, et al. Effect of Caregiver Training on the Neurodevelopment of HIV-Exposed Uninfected Children and Caregiver Mental Health: A Ugandan Cluster-Randomized Controlled Trial. Journal of Developmental & Behavioral Pediatrics. 2017;38(9):753–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Olley BO, Seedat S, Nei DG, Stein DJ. Predictors of major depression in recently diagnosed patients with HIV/AIDS in South Africa. AIDS Patient Care and STDs. 2004;18(8):481–7. [DOI] [PubMed] [Google Scholar]
- 37.Bass JK, Opoka R, Familiar I, Nakasujja N, Sikorskii A, Awadu J, et al. Randomized controlled trial of caregiver training for HIV-infected child neurodevelopment and caregiver well being. Aids. 2017;31(13):1877–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sherr L, Clucas C, Harding R, Sibley E, Catalan J HIV and depression–a systematic review of interventions. Psychology, health & medicine. 2011;16(5):493–527. [DOI] [PubMed] [Google Scholar]
- 39.Hughes C, Roman G, Hart MJ, Ensor R. Does maternal depression predict young children’s executive function? - a 4-year longitudinal study. J Child Psychol Psychiatry. 2013;54(2):169–77. [DOI] [PubMed] [Google Scholar]
- 40.Hennigan KM, O’Keefe M, Noether CD, Rinehart DJ, Russell LA. Through a mother’s eyes: Sources of bias when mothers with co-occurring disorders assess their children. J Behav Health Serv Res. 2006;33(1):87–104. [DOI] [PubMed] [Google Scholar]
- 41.Richters JE. Depressed mothers as informants about their children: a critical review of the evidence for distortion. Psychol Bull. 1992;112(3):485–99. [DOI] [PubMed] [Google Scholar]
- 42.Ordway MR. Depressed mothers as informants on child behavior: methodological issues. Res Nurs Health. 2011;34(6):520–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bengtson AM, Pence BW, Gaynes BN, Quinlivan EB, Heine AD, O’donnell JK, et al. Improving depression among HIV-infected adults: transporting the effect of a depression treatment intervention to routine care. Journal of acquired immune deficiency syndromes (1999). 2016;73(4):482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Milan S, Ickovics J, Vlahov D, Boland R, Schoenbaum E, Schuman P, et al. Interpersonal predictors of depression trajectories in women with HIV. J Consult Clin Psychol. 2005;73(4):678–88. [DOI] [PubMed] [Google Scholar]
- 45.Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: a review. Int J Inj Contr Saf Promot. 2008;15(4):221–31. [DOI] [PMC free article] [PubMed] [Google Scholar]