Abstract
Purpose:
Patients with metastatic breast cancer (MBC) experience high levels of symptoms. Yoga interventions have shown promise for improving cancer symptoms but have rarely been tested in patients with advanced disease. This study examined the acceptability of a comprehensive yoga program for MBC and the feasibility of conducting a randomized trial testing the intervention.
Methods:
63 women with MBC were randomized with a 2:1 allocation to yoga or a support group comparison condition. Both interventions involved 8 weekly group sessions. Feasibility was quantified using rates of accrual, attrition, and session attendance. Acceptability was assessed with a standardized self-report measure. Pain, fatigue, sleep quality, psychological distress, mindfulness, and functional capacity were assessed at baseline, post-intervention, and 3 and 6 months post-intervention.
Results:
We met goals for accrual and retention, with 50% of eligible patients enrolled and 87% of randomized participants completing post-intervention surveys. 65% of women in the yoga condition and 90% in the support group attended ≥ four sessions. 80% of participants in the yoga condition and 65% in the support group indicated they were highly satisfied with the intervention. Following treatment, women in the yoga intervention had modest improvements in some outcomes, however overall symptom levels were low for women in both conditions.
Conclusions:
Findings suggest that the yoga intervention content was highly acceptable to patients with MBC, but that there are challenges to implementing an intervention involving eight group-based in-person sessions. Alternative modes of delivery may be necessary to reach patients most in need of intervention.
Keywords: yoga, symptom management, metastatic breast cancer, randomized trial
Structured abstract:
Patients with metastatic breast cancer experience a high level of symptom burden that may be alleviated through yoga. Results indicate that a comprehensive yoga intervention was highly acceptable to patients, but that the intervention’s mode of delivery involving eight in-person group sessions may need to be modified to improve feasible for this population.
Introduction
There is an increasing number of women living with metastatic breast cancer (MBC), likely due to improvements in cancer treatment which are extending survival time [1] Many women with MBC experience a high level of symptom burden, including pain, fatigue, sleep disturbance, psychological distress, and functional impairment.[2] Interventions are need to help patients cope with these symptoms and ongoing medical treatments as well as existential concerns regarding the life-limiting nature of their diagnosis.
Yoga is a potentially promising approach to addressing the range of symptoms seen in MBC [3]. A growing number of studies have tested yoga interventions for patients with early-stage disease. Systematic reviews and meta-analyses of RCTs concluded that yoga has at least short-term benefits, with moderate to large effects on psychosocial outcomes and small effects on functional well-being [4,5].
However, to date, there have been no RCTs of yoga interventions that target patients with advanced cancer. Given the growing interest in yoga among women with breast cancer [3,6], it may be a particularly acceptable intervention approach for women with MBC. Yoga’s emphasis on the ability to accept one’s moment-to-moment experience may also make it relevant and beneficial for a patient population dealing with a life-limiting illness [7].
We have developed a novel Mindful Yoga intervention based on the Kripalu school of yoga, a widely taught form of Hatha yoga that emphasizes mindfulness techniques [8]. It uses a comprehensive approach including gentle and functional physical postures (asanas) complemented by breathing exercises (pranayama), meditation techniques (dhyana), study of pertinent topics (swadhyaya), and group discussions (satsang). This approach may be particularly acceptable to women with MBC whose emotional and/or physical limitations may preclude their benefiting fully from yoga interventions focused primarily on physical poses.
Previous studies found that Mindful Yoga (previously published as ‘Yoga of Awareness’) led to improvements in pain, fatigue, sleep disturbances and depression among breast cancer survivors [9] and women with fibromyalgia [10,11]. In addition, a small single-arm pilot study testing Mindful Yoga among 13 women with MBC found that the intervention showed promise in improving cancer-related pain, fatigue and emotional distress and was not associated with any adverse events [12]. However, the study had significant limitations including the very small sample size, relatively high attrition (33%), and lack of a control group or randomized design.
Accordingly, the primary aim of the current study was to determine the acceptability of the Mindful Yoga intervention for women with MBC, and the feasibility of conducting an RCT testing the intervention including randomization in cohorts to yoga versus a social support group (SSG) control condition. Secondary aims were to (a) examine associations between baseline patient characteristics and intervention dose; and (b) explore the impact on pain, fatigue, sleep disturbance, psychological distress, and functional capacity.
Methods
Participants
Patient eligibility: (a) receiving treatment for MBC; (b) age ≥ 18; (c) had a life expectancy ≥ 9 months as estimated by their treating oncologist; (d) could speak and read English. Exclusion criteria were: (a) cognitive impairment as assessed by the 6-item Mini-Mental Status Exam; (b) Eastern Cooperative Oncology Group (ECOG) rating of ≥ 3 or Karnofsky Performance Status (KPS) < 60 as rated by the oncology provider; (c) treatment for serious psychiatric illness (e.g., schizophrenia, severe depression) in the past 6 months; (d) current engagement in yoga practice ≥ 1 day per week; (e) unable or unwilling to give written informed consent.
Procedures
All study procedures were approved by the Duke Medical Center Institutional Review Board (IRB). Informed consent was obtained from all individual participants included in the study. Participants were recruited between May, 2014 and January, 2018 from the Duke breast oncology clinic. Contact with potential participants was initiated by each patient’s oncologist via an IRB-approved introductory letter. Individuals who did not refuse further contact were called by study staff who explained the study, answered questions, and verified eligibility. If the patient was eligible and chose to participate, arrangements were made to obtain written consent and administer the baseline assessment. Each participant was paid $190 for full study participation.
After completing consent and baseline assessment, participants were randomized with 2:1 allocation to: (a) Mindful Yoga, or (b) SSG. Study statisticians generated the randomization scheme prior to the start of recruitment; it was kept in a study database inaccessible to blinded study personnel. The study coordinator who executed the randomization schedule did not have access to the data and was not involved in the outcome assessments. Due to the group nature of the interventions, enrollment proceeded in cohorts. Randomization was stratified within each cohort using variable block sizes of 3 and 6. After completing the intervention, participants completed the post-treatment assessment, with additional follow up assessments occurring 3 months and 6 months post-intervention. The Principal Investigator, study statisticians, and study staff involved in collecting outcome assessments were blinded to treatment condition.
Measures
Demographic information was collected from patients at baseline and medical information was collected via medical record review at time points corresponding with each assessment.
Acceptability was assessed at post-treatment with the Client Satisfaction Questionnaire-8 [13]. This measure has good reliability and is frequently used to assess participants’ satisfaction with the services they received. Items are rated on a four-point scale.
Pain was assessed with the Brief Pain Inventory-Short Form, a 9-item self-report measure that assesses worst, least, and average levels of pain and interference due to pain. This measure is widely used with cancer patients, has evidence of reliability and validity, and is considered the preferred method of assessing pain endpoints [14,15].
Fatigue was assessed with the Brief Fatigue Inventory, a 9-item measure assessing current, worst, and usual fatigue, and interference due to fatigue. This measure has excellent psychometric properties. [16]. The total scale score was used.
Sleep quality was assessed by the Pittsburgh Sleep Quality Index [17]. Higher scores indicate poorer sleep quality. The scale has been widely used with breast cancer patients with good internal consistency [18].
Psychological distress was assessed using the Hospital Anxiety and Depression Scale (HADS), a 14-item, 2-domain (depression and anxiety) scale widely used with cancer patients with evidence of reliability, validity, and responsiveness [19,20]. Domain scores ≥ 8 indicate either likely depression or anxiety.
Mindfulness was assessed with the Five Facet Mindfulness Questionnaire-Short Form (FFMQ-SF)[21]. The FFMQ-SF is a 24-item short form of the Five Facet Mindfulness Questionnaire, a comprehensive measure for assessing mindfulness with demonstrated reliability and validity [22].
Functional capacity was assessed by the 6-Minute Walk Test administered according to American Thoracic Society (ATS) guidelines [23].
Interventions
General factors.
Each intervention consisted of eight 120-minute weekly group sessions. Yoga instructors and the support group leader received training in the protocols prior to delivering the interventions and followed detailed treatment manuals. All sessions were video recorded and reviewed by investigators who provided feedback to the instructors on a weekly basis.
Mindful Yoga.
Each session included gentle postures (approx. 40 minutes), breathing techniques (10 minutes), meditation (25 minutes), presentations on the application of yogic principles to optimal coping (20 minutes), and group discussions (25 minutes). To enhance feasibility, acceptability, and safety, yoga poses were specifically selected and tailored to meet the needs of women with MBC, including minimizing risks of falls and vertebral facture. Chairs were readily available to enhance balance, and the instructor emphasized gentle performance. Participants were encouraged to practice yoga techniques daily at home, guided by professionally produced videos. Participants also received handouts each week, which included instructions for applying yoga practice to daily life. There were a total of six yoga groups with 5–8 patients per group, each of which was led by one of three certified yoga instructors.
Social support group (SSG).
A support group was chosen as a comparison condition as patients view this type of intervention is viewed as highly credible [24–26] and it controls for attention, time, and nonspecific treatment effects such as general social support. This intervention was modeled after the protocol utilized by Breitbart and colleagues [24]. Scheduling of sessions was identical to that for the yoga intervention. Sessions focused on discussion of issues relevant to patients coping with MBC, including coping with medical tests, communicating with healthcare providers, coping with family and friends, vocational issues, body image and physical functioning concerns, fears about disability, recurrence, and mortality, and plans for the future. There were a total of four groups with 5–7 patients per group which were led by one interventionist, a licensed clinical social worker experienced in leading groups and working with patients with advanced cancer.
Statistical analysis
Descriptive analyses examined recruitment rates, feasibility and acceptability measures, associations between patient baseline characteristics and intervention dose, and means on the outcome measures for the two study conditions. The benchmark for feasibility was at least 70% of patients attending ≥ 4 of 8 sessions and completing post-treatment assessments. Adequate acceptability of the yoga intervention was indicated by ≥ 80% of participants reporting a mean satisfaction score ≥ 3 on the Client Satisfaction Questionnaire-8. Our original sample size of 60 patients (40 intervention and 20 control) was based on the primary aim of intervention feasibility and acceptability. While we increased the sample size slightly to ensure the final cohort had an adequate number of participants, the study was not powered to detect significant treatment effects. For each scale domain, a repeated-measures general linear model was used to estimate means over time, with 95% confidence intervals. As recommended by guidelines for pilot studies with small sample sizes, [27,28] we did not conduct statistical tests of group differences. Instead, to quantify clinically important differences, we compared group mean differences to 0.5 of the baseline SD of each scale domain.
Results
Participants
Baseline demographic and medical data for participants are presented in Table 1.
Table 1.
Patient Baseline Characteristics
| Overall N=63 |
Yoga Group N=43 |
Support Group N=20 |
|
|---|---|---|---|
| Age, Mean (SD) | 57.3 (11.5) | 56.3 (11.6) | 59.4 (11.3) |
| Partner status, n (%) | |||
| Married/Living Together | 40 (63.5) | 28 (65.1) | 12 (60.0) |
| Other | 22 (34.9) | 14 (32.6) | 8 (40.0) |
| Missing | 1 (1.6) | 1 (2.3) | 0 (0.0) |
| Dependent children, n (%) | 22 (3.49) | ||
| Race, n (%) | |||
| Caucasian | 47 (74.6) | 34 (79.1) | 13 (65.0) |
| Other | 16 (25.4) | 9 (20.9) | 7 (35.0) |
| Highest education level, n (%) | |||
| High School/Some College | 18 (28.6) | 11 (25.6) | 7 (35.0) |
| Other | 45 (71.4) | 32 (74.4) | 13 (35.0) |
| Total years of education, Mean (SD) | 17.0 (6.9) | 16.7 (2.8) | 17.7 (11.6) |
| Employment, n (%) | |||
| Working Part-time/Full-time | 18 (28.6) | 15 (34.9) | 3 (15.0) |
| Other | 45 (71.4) | 28 (65.1) | 17 (85.0) |
| Household income, n (%) | |||
| ≤ $50,000 per year | 25 (39.7) | 18 (41.9) | 7 (35.0) |
| >$50,000 per year | 36 (57.1) | 23 (53.5) | 13 (65.0) |
| Missing | 2 (3.2) | 2 (4.7) | 0 (0.0) |
Feasibility and Acceptability
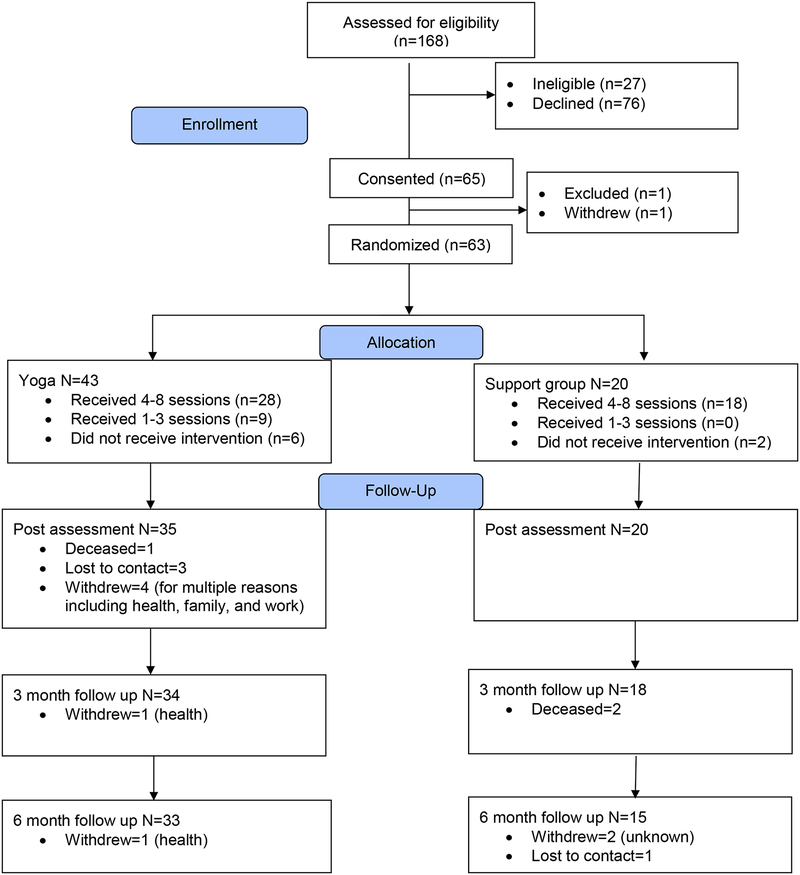
Study Enrollment and Participation (see Figure 1).
Figure 1.
Study Consort Diagram
65 of 129 eligible patients (50%) enrolled in the trial. Reasons for ineligibility included cognitive impairment, lack of transportation, and current yoga practice. Among eligible patients, reasons for refusal included lack of time (n=26), lack of interest (n=13), and distance/difficulty with transportation (n=9). 63 of the 65 patients who consented were randomized; one was excluded at baseline due to high heart rate during the walk test, and one changed her mind.
65% of women in the yoga arm and 90% of women in the SSG arm attended ≥ four sessions. Mean attendance was 4.6 (SD=2.9) sessions in the yoga arm and 6.0 (SD=2.2) in the SSG arm. The most common reasons for missing sessions were transportation issues, conflicts with family, work, or medical appointments, and vacation.
Acceptability.
Of participants who completed the post-treatment assessment, 82% (28/34) in the yoga condition and 65% (11/17) in SSG reported a mean rating of ≥3 indicating high satisfaction with the intervention. Mean ratings were 3.4 (SD=0.5) for yoga and 3.3 (SD=0.4) for SSG.
No adverse events were associated with participation in either intervention.
Associations between attendance and baseline characteristics
We examined the demographic and medical characteristics for associations with session attendance (see Table 2). Among women in the yoga condition, those who were <50 years old, had dependent children, and those who were working attended the fewest number of sessions. No discernable patterns were evident in SSG, likely due to the small number of participants in this condition.
Table 2.
Associations between baseline characteristics and attendance
| Overall | Yoga Group | Support Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Sessions Attended | >= 4 Sessions | Total Sessions Attended | >= 4 Sessions | Total Sessions Attended | >= 4 Sessions | |||||||
| N | SD | Count | N | SD | Count | N | SD | Count | ||||
| Age Group | ||||||||||||
| < 50 | 18 | (2.8) | 11 | 12 | (2.6) | 5 | 6 | (0.8) | 6 | |||
| 50–59 | 17 | (2.7) | 13 | 13 | (2.6) | 10 | 4 | (3.4) | 3 | |||
| 60–69 | 18 | (3.0) | 13 | 13 | (3.2) | 8 | 5 | (1.3) | 5 | |||
| >= 70 | 10 | (2.6) | 9 | 5 | (1.7) | 5 | 5 | (3.1) | 4 | |||
| Dependent Children | 22 | (2.8) | 12 | 17 | (2.6) | 7 | 5 | (1.1) | 5 | |||
| Race | ||||||||||||
| Caucasian | 47 | (2.9) | 33 | 34 | (3.0) | 21 | 13 | (2.1) | 12 | |||
| Other | 16 | (2.6) | 13 | 9 | (2.8) | 7 | 7 | (2.6) | 6 | |||
| Partner Status | ||||||||||||
| Married/Living Together | 40 | (3.0) | 26 | 28 | (3.0) | 16 | 12 | (2.9) | 10 | |||
| Other | 22 | (2.2) | 20 | 14 | (2.8) | 12 | 8 | (0.7) | 8 | |||
| Missing | 1 | 1 | ||||||||||
| Education | ||||||||||||
| High School/Some College | 18 | (2.8) | 14 | 11 | (2.6) | 8 | 7 | (2.8) | 6 | |||
| Other | 45 | (2.8) | 32 | 32 | (3.1) | 20 | 13 | (2.0) | 12 | |||
| Employment | ||||||||||||
| Working Part/Full Time | 18 | (2.6) | 7 | 15 | (2.3) | 4 | 3 | (0.6) | 3 | |||
| Other | 45 | (2.5) | 39 | 28 | (2.7) | 24 | 17 | (2.4) | 15 | |||
| Radiation Therapy | ||||||||||||
| Yes | 44 | (2.8) | 32 | 30 | (3.0) | 19 | 14 | (2.0) | 13 | |||
| No | 16 | (2.5) | 13 | 11 | (2.3) | 11 | 5 | (3.1) | 4 | |||
| Missing | 3 | (4.0) | 1 | 2 | (0.0) | 2 | 1 | 1 | ||||
| Surgery | ||||||||||||
| Yes | 16 | (1.8) | 15 | 11 | (2.1) | 10 | 5 | (1.1) | 5 | |||
| No | 46 | (2.9) | 31 | 31 | (3.0) | 18 | 15 | (2.5) | 13 | |||
| Missing | 1 | 1 | ||||||||||
| Chemotherapy Ongoing | ||||||||||||
| Yes | 42 | (2.8) | 31 | 28 | (2.8) | 19 | 14 | (2.6) | 12 | |||
| No | 13 | (2.9) | 10 | 7 | (3.8) | 4 | 6 | (1.1) | 6 | |||
| Missing | 1 | 1 | 1 | 1 | ||||||||
We also examined associations between scores on baseline measures of pain, fatigue, sleep disturbance, psychological distress, and mindfulness and session attendance, based on median splits on the scales (see Table 3). Among patients in the yoga condition, those who were more depressed attended somewhat fewer sessions than those who were less depressed. No other patterns were discerned.
Table 3.
Association between baseline measures and session attendance
| Overall | Yoga Group | Support Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total Sessions Attended | Attended >= 4 Sessions | Total Sessions Attended | Attended >= 4 Sessions | Total Sessions Attended | Attended >= 4 Sessions | |||||||
| N | SD | Count | N | SD | Count | N | SD | Count | ||||
| FFMQ: Total Score | ||||||||||||
| Below Median | 27 | (2.8) | 18 | 19 | (2.9) | 11 | 8 | (2.3) | 7 | |||
| At or Above Median | 3 | (2.6) | 26 | 21 | (2.8) | 15 | 12 | (2.3) | 11 | |||
| Missing | 3 | (4.4) | 2 | 3 | (4.4) | 2 | ||||||
| BFI: Brief Fatigue Inventory | ||||||||||||
| Below Median | 31 | (2.5) | 25 | 18 | (2.7) | 13 | 13 | (2.1) | 12 | |||
| At or Above Median | 32 | (3.0) | 21 | 25 | (3.0) | 15 | 7 | (2.7) | 6 | |||
| BPI: Pain Severity | ||||||||||||
| Below Median | 29 | (2.3) | 25 | 17 | (2.5) | 14 | 12 | (2.2) | 11 | |||
| At or Above Median | 34 | (3.0) | 21 | 26 | (3.1) | 14 | 8 | (2.5) | 7 | |||
| BPI: Pain Interference | ||||||||||||
| Below Median | 29 | (2.3) | 24 | 16 | (2.3) | 12 | 13 | (2.1) | 12 | |||
| At or Above Median | 34 | (3.1) | 22 | 27 | (3.2) | 16 | 7 | (2.5) | 6 | |||
| HADS Anxiety | ||||||||||||
| Below Median | 23 | (2.9) | 17 | 14 | (3.1) | 9 | 9 | (2.4) | 8 | |||
| At or Above Median | 38 | (2.8) | 27 | 29 | (2.9) | 19 | 9 | (2.4) | 8 | |||
| Missing | 2 | (0.7) | 2 | 2 | (0.7) | 2 | ||||||
| HADS Depression | ||||||||||||
| Below Median | 26 | (2.6) | 22 | 17 | (2.7) | 14 | 9 | (2.4) | 8 | |||
| At or Above Median | 34 | (2.9) | 21 | 25 | (2.8) | 13 | 9 | (2.4) | 8 | |||
| Missing | 3 | (1.5) | 3 | 1 | 1 | 2 | (0.7) | 2 | ||||
| HADS Total Score | ||||||||||||
| Below Median | 27 | (2.8) | 21 | 17 | (3.0) | 12 | 10 | (2.3) | 9 | |||
| At or Above Median | 33 | (2.9) | 22 | 25 | (2.9) | 15 | 8 | (2.6) | 7 | |||
| Missing | 3 | (1.5) | 3 | 1 | 1 | 2 | (0.7) | 2 | ||||
| PSQI: Total Score | ||||||||||||
| Below Median | 27 | (2.6) | 21 | 16 | (2.9) | 11 | 11 | (2.2) | 10 | |||
| At or Above Median | 27 | (2.9) | 19 | 21 | (3.0) | 13 | 6 | (1.0) | 6 | |||
| Missing | 9 | (3.1) | 6 | 6 | (2.9) | 4 | 3 | (4.2) | 2 | |||
Changes in outcomes
Inspection of the means and 95% confidence intervals on outcome variables suggests little change over time in the outcomes for participants in either condition (see Table 4). Reported levels of symptoms remained low throughout the study in both groups. Women in the yoga condition had modest improvements in fatigue at post-treatment and 6-month follow-up, and on anxiety and total HADS total scores across all time points. They also walked a greater distance at post-treatment and 6-month follow-ups.
Table 4.
Estimated means and 95% confidences intervals of scales, over time and by intervention arm
| Scale | Timepoint | Yoga Group (95% CI) | Support Group (95% CI) | Difference, Yoga vs Support (95% CI) | .5 SD at Baseline |
|---|---|---|---|---|---|
| FFMQ: Mindfulness Total Score (24–120, 120=Most Mindful) | Baseline | 84.6 (81.4, 87.7) | 84.6 (81.4, 87.7) | 6.26 | |
| Post Treatment | 90.1 (86.3, 93.8) | 87.0 (82.4, 91.6) | 3.1 (−2.1, 8.2) | ||
| 3-Month FUp | 89.9 (85.8, 93.9) | 87.6 (82.6, 92.6) | 2.3 (−3.2, 7.8) | ||
| 6-Month FUp | 90.7 (86.5, 94.9) | 89.9 (84.5, 95.4) | 0.8 (−5.2, 6.8) | ||
| BFI: Brief Fatigue Inventory (0–10, 0=No Fatigue) | Baseline | 3.4 (2.7, 4.0) | 3.4 (2.7, 4.0) | 1.23 | |
| Post Treatment | 2.7 (2.0, 3.4) | 3.3 (2.4, 4.1) | −0.6 (−1.5, 0.4) | ||
| 3-Month FUp | 3.0 (2.3, 3.6) | 2.8 (2.0, 3.7) | 0.1 (−0.8, 1.0) | ||
| 6-Month FUp | 2.7 (2.0, 3.5) | 3.4 (2.4, 4.3) | −0.6 (−1.7, 0.4) | ||
| BPI: Pain Severity (0–10, 0=No Pain) | Baseline | 2.0 (1.6, 2.4) | 2.0 (1.6, 2.4) | 0.75 | |
| Post Treatment | 1.9 (1.3, 2.4) | 1.8 (1.1, 2.5) | 0.1 (−0.8, 0.9) | ||
| 3-Month FUp | 2.3 (1.6, 2.9) | 2.0 (1.1, 2.8) | 0.3 (−0.7, 1.3) | ||
| 6-Month FUp | 1.8 (1.2, 2.3) | 1.7 (1.0, 2.5) | 0.0 (−0.8, 0.9) | ||
| BPI: Pain Interference (0–10, 0=No Interference) | Baseline | 2.6 (2.0, 3.2) | 2.6 (2.0, 3.2) | 1.21 | |
| Post Treatment | 2.2 (1.6, 2.8) | 2.1 (1.3, 2.9) | 0.1 (−0.7, 0.9) | ||
| 3-Month FUp | 2.4 (1.7, 3.0) | 2.3 (1.5, 3.2) | 0.0 (−0.9, 0.9) | ||
| 6-Month FUp | 2.1 (1.4, 2.8) | 2.7 (1.8, 3.5) | −0.6 (−1.5, 0.3) | ||
| HADS Anxiety (0–21, 21=Highest Anxiety) | Baseline | 6.6 (5.6, 7.7) | 6.6 (5.6, 7.7) | 2.07 | |
| Post Treatment | 5.5 (4.4, 6.5) | 6.2 (4.9, 7.5) | −0.7 (−2.2, 0.7) | ||
| 3-Month FUp | 5.6 (4.4, 6.7) | 6.3 (4.8, 7.7) | −0.7 (−2.4, 1.0) | ||
| 6-Month FUp | 5.1 (4.0, 6.1) | 6.2 (4.7, 7.6) | −1.1 (−2.8, 0.6) | ||
| HADS Depression (0–21, 21=Highest Depression) | Baseline | 4.3 (3.5, 5.1) | 4.3 (3.5, 5.1) | 1.64 | |
| Post Treatment | 4.0 (3.1, 5.0) | 4.1 (3.0, 5.2) | −0.1 (−1.2, 1.0) | ||
| 3-Month FUp | 4.1 (3.1, 5.0) | 4.0 (2.8, 5.2) | 0.1 (−1.2, 1.4) | ||
| 6-Month FUp | 3.6 (2.6, 4.6) | 4.6 (3.3, 5.9) | −0.9 (−2.3, 0.4) | ||
| HADS Total (0–42, 42=Highest Distress) | Baseline | 10.9 (9.2, 12.6) | 10.9 (9.2, 12.6) | 3.33 | |
| Post Treatment | 9.4 (7.7, 11.1) | 10.4 (8.4, 12.4) | −1.0 (−3.1, 1.1) | ||
| 3-Month FUp | 9.6 (7.7, 11.4) | 10.4 (8.1, 12.7) | −0.8 (−3.3, 1.6) | ||
| 6-Month FUp | 8.6 (6.8, 10.3) | 10.9 (8.6, 13.2) | −2.3 (−4.8, 0.3) | ||
| PSQI: Total Score (0–21, 21=Worse Sleep Quality) | Baseline | 8.6 (7.6, 9.6) | 8.6 (7.6, 9.6) | 1.96 | |
| Post Treatment | 7.6 (6.4, 8.8) | 7.6 (6.1, 9.1) | 0.0 (−1.7, 1.7) | ||
| 3-Month FUp | 7.8 (6.7, 8.8) | 5.8 (4.3, 7.2) | 2.0 (0.4, 3.7) | ||
| 6-Month FUp | 7.2 (6.1, 8.3) | 6.5 (5.1, 8.0) | 0.7 (−1.0, 2.3) | ||
| 6MWT: Total distance walked (meters) | Baseline | 388.3 (369.4, 407.2) | 388.3 (369.4, 407.2) | 36.50 | |
| Post Treatment | 404.0 (364.1, 444.0) | 377.5 (326.3, 428.8) | 26.5 (−34.9, 88.0) | ||
| 3-Month FUp | 413.7 (385.4, 442.1) | 382.3 (343.3, 421.3) | 31.5 (−12.2, 75.1) | ||
| 6-Month FUp | 417.4 (392.4, 442.5) | 394.2 (360.4, 427.9) | 23.3 (−13.4, 60.0) |
Notes: A repeated measures general linear model was used to estimate mean scale measures over time via PROC MIXED in SAS (v 9.4, Cary, NC). Each model was constrained at baseline and contained dummy variables for time, an indicator variable for intervention arm and intervention by time interaction terms. An unstructured covariance measure was included to account for patients’ repeated measurements over time.
Five Facet Mindfulness Questionnaire;
Hospital Anxiety and Depression Scale;
SQI=Pittsburgh Sleep Quality Index; higher scores indicate worse sleep disturbance;
Six minute walk test.
Discussion
The primary aim of this pilot study was to determine the feasibility and acceptability of a yoga intervention among women with MBC. With regard to feasibility, we met accrual and overall retention goals, with 87% and 76% of participants providing data at post-intervention and 6-month follow up, respectively. We also met acceptance goals with 80% of yoga participants reporting high levels of satisfaction with the intervention. Overall, 73% of participants attended at least 4 of 8 intervention sessions. However, participants in the yoga intervention attended fewer sessions than those in the support group. Among women in the yoga condition, those who were younger, had dependent children at home, were employed, and more depressed attended the fewest sessions. While these variables did not appear to affect attendance in the control condition, there were also few women in that condition who were employed or had children.
We implemented a number of strategies to enhance attendance (e.g., offering sessions in the evening to accommodate participants who worked, reminder emails about upcoming sessions). However it is possible that women who were employed and had dependent children may have had too many competing demands to feasibly attend 8 weekly two-hour sessions, particularly in the context of ongoing cancer treatments. In light of a diagnosis that portends shortened life expectancy, women with MBC may also be likely to prioritize time with family above other obligations. For example, after randomization, one woman who was assigned to the yoga condition and expressed enthusiasm about the intervention learned her child was selected for an elite sports team with games that conflicted with yoga sessions; she understandably chose to attend her child’s games rather than the intervention.
Despite challenges to attendance, satisfaction ratings were high among participants in both conditions, indicating the interventions’ acceptability. Open-ended feedback indicated that women in the yoga intervention found the breathing, meditation, and gentle poses components helpful. Comments from women in both groups highlighted the value of group interactions with other women with MBC, speaking to the need for more interventions emphasizing supportive care for this population. Interestingly, while attendance rates were higher among participants in the support group, satisfaction ratings were somewhat lower,
We observed little change in outcome variables in participants in either treatment condition. Feasibility trials with small samples are not powered to be informative about efficacy potential [28]. However, in light of previous research suggesting the efficacy of Mindful Yoga [9–12] and other yoga interventions [4, 5], the modest changes observed was surprising. One contributing factor could have been the low baseline levels of symptoms, which is unusual in a population of patients with advanced cancer. The study demands – including a total of 12 in-person study visits – may have precluded patients experiencing a higher symptom burden from participating, thus creating a floor effect.
The study was also limited by the unequal allocation of participants to the treatment arms, resulting in a particularly small control group. However, the study also had a number of strengths including a control condition that equated for time, attention, and social support, follow up assessments at 3 and 6 months, and an objective measure of functional capacity. In light of the participant comments regarding the importance of group interactions, future studies testing group-based yoga interventions should consider using active control groups that equate for social support.
As the first RCT of a yoga intervention for MBC, findings from this study suggest that the yoga intervention content was highly acceptable to patients with MBC and was not associated with adverse events. The feasibility and acceptability of randomizing patients to yoga or a social support group was also supported. However, we found that it was difficult for some women, particularly those who were employed and/or had dependent children, to attend eight group-based in-person sessions. Future studies should consider alternative modes of delivery such as open rather than closed groups, adding or substituting home-based modules, and/or conducting sessions via videoconference. These adaptations may also make it possible to target patients with high levels of symptoms who are more likely to benefit from intervention.
In conclusion, findings indicate that the yoga intervention and the RCT design were highly acceptable to patients, but that modifications to the intervention’s mode of delivery are required to improve feasible for this population. Given that prior research as well as theory suggest that yoga is likely to benefit a range of patients who struggle with cancer-related symptoms, further research is needed to develop accessible means of delivering a group-based yoga intervention to patients with MBC.
Acknowledgements
This work was supported by the National Institutes of Health [R01 AT007572]. Dr. Jones is supported by AKTIV Against Cancer, the Kavli Trust, and the Memorial Sloan Kettering Cancer Center Support Grant/Core Grant (P30 CA008748).
The authors gratefully acknowledge the contributions of study staff including Jessyka Glatz, M.A., Emily Patterson, M.S.W., L.C.S.W., Barbara Walukas, B.S.R.N., C.C.R.P., Nancy Kimberly, M.A., E-RYT, Katheryn Harlan, R.N, E-RYT, Robin Turner, M.D., and the Data Safety Monitoring Board members: Diana Wilkie, PhD, RN, FAAN; Mary Jane Ott, NP, MN, RYT; Christopher Corcoran, PhD; and Beverly Moy, MD. They also extend their gratitude to all of the study participants for their time and effort.
Disclosure/Conflict of Interest
The work of Drs. Porter, Carson, Olsen, Keefe, Westbrook, Ms. Carson, and Ms. Sanders on this study was supported by a grant from the National Institutes of Health. Dr. Jones owns stock in Pacylex, Inc.
Footnotes
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- 1.Mariotto AB, Etzioni R, Hurlbert M, Penberthy L, Mayer M (2017) Estimation of the number of women living with metastatic breast cancer in the United States. Cancer Epidemiology Biomarkers Prev. doi: 10.1158/1055-9965.EPI-16-0889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Irvin WJ, Muss H, Mayer D (2011) Symptom management in metastatic breast cancer. Oncologist 16 (9):1203–1214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. [September 23, 2016]; Office of Cancer Complementary and Alternative Medicine Yoga and Cancer. https://cam.cancer.gov/health_information/highlights/yoga_cancer_highlight.htm. Accessed.
- 4.Harder H, Parlour L, Jenkins V (2012) Randomised controlled trials of yoga interventions for women with breast cancer: a systematic literature review. Supportive Care in Cancer 20(12):3055–3064. doi:DOI 10.1007/s00520-012-1611-8 [DOI] [PubMed] [Google Scholar]
- 5.Buffart LM, van Uffelen JGZ, Riphagen II, Brug J, van Mechelen W, Brown WJ, Chinapaw MJM (2012) Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer 12 (559) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Office of Cancer Complementary and Alternative Medicine Research Priorities. https://cam.cancer.gov/about_us/about_occam.htm#priorities Accessed September 23, 2016
- 7.Clark D (2002) Between hope and acceptance: the medicalisation of dying. BMJ 324:905–907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alliance Yoga (2010–2012) Styles of Yoga http://yogaalliance.org/content/understanding-different-styles-yoga Accessed October 18, 2012
- 9.Carson JW, Carson KM, Porter LS, Keefe FJ, Seewaldt VL (2009) Yoga of Awareness program for menopausal symptoms in breast cancer survivors: results from a randomized trial. Support Care Cancer 17 (10):1301–1309 [DOI] [PubMed] [Google Scholar]
- 10.Carson JW, Carson KM, Jones KD, Bennett RM, Wright CL, Mist SD (2010) A pilot randomized controlled trial of the Yoga of Awareness program in the management of fibromyalgia. Pain 151 (2):530–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carson JW, Carson KM, Jones KD, Mist SD, Bennett RM (2012) Follow-up of Yoga of Awareness for fibromyalgia: Results at 3 months and replication in the wait-list group. Clinical Journal of Pain 28 (9):804–813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carson J, Carson KM, Porter LS, Keefe FJ, Shaw H, Miller JM. (2007) Yoga for women with metastatic breast cancer: results from a pilot study. Journal of Pain and Symptom Management 33 (3):331–341 [DOI] [PubMed] [Google Scholar]
- 13.Nguyen TD, Attkisson CC, Stegner BL (1983) Assessment of patient satisfaction: Development and refinement of a service evaluation questionnaire. Evaluation and program planning 6:299–314 [DOI] [PubMed] [Google Scholar]
- 14.Atkinson TM, Mendoza TR, Sit L, Passik S, Scher HI, Cleeland C, Basch E (2010) The Brief Pain Inventory and its “pain at its worst in the last 24 hours” item: clinical trial endpoint considerations. Pain medicine (Malden, Mass) 11 (3):337–346. doi: 10.1111/j.1526-4637.2009.00774.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cleeland CS, Ryan KM (1994) Pain assessment: Global use of the Brief Pain Inventory Annals of the Academy of Medicine, Singapore: 23:129–138 [PubMed] [Google Scholar]
- 16.Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL (1999) The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer 85 (5):1186–1196. doi:10.1002/(SICI)1097–0142(19990301)85:5<1186::AIDCNCR24>3.0.CO;2-N [pii] [DOI] [PubMed] [Google Scholar]
- 17.Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research 28 (2):193–213 [DOI] [PubMed] [Google Scholar]
- 18.Carpenter JS, Andrykowski MA (1998) Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of psychosomatic research 45 (1):5–13 [DOI] [PubMed] [Google Scholar]
- 19.Herrmann C (1997) International experiences with the Hospital Anxiety and Depression Scale--a review of validation data and clinical results. Journal of psychosomatic research 42(1):17–41 [DOI] [PubMed] [Google Scholar]
- 20.Zigmond AS, Snaith RP (1983) The hospital anxiety and depression scale. Acta psychiatrica Scandinavica 67 (6):361–370 [DOI] [PubMed] [Google Scholar]
- 21.Bohlmeijer E, ten Klooster PM, Fledderus M, Veehof M, Baer R (2011) Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment 18 (3):308–320. doi: 10.1177/1073191111408231 [DOI] [PubMed] [Google Scholar]
- 22.Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Walsh E, Duggan D, Williams JMG (2008) Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment 15 (3):329–342 [DOI] [PubMed] [Google Scholar]
- 23.American Thoracic Society (2002) ATS statement: guidelines for the six-minute walk test. American journal of respiratory and critical care medicine 166 (1):111–117. doi: 10.1164/ajrccm.166.1.at1102 [DOI] [PubMed] [Google Scholar]
- 24.Breitbart W, Rosenfeld B, Gibson C, Pessin H, Poppito S, Nelson C, Tomarken A, Timm AK, Berg A, Jacobson C, Sorger B, Abbey J, Olden M (2010) Meaning-centered group psychotherapy for patients with advanced cancer: a pilot randomized controlled trial. Psycho-Oncology 19 (1):21–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Helgeson VS, Cohen S, Schulz R, Yasko J (1999) Education and peer discussion group interventions and adjustment to breast cancer. Archives of general psychiatry 56 (4):340–347 [DOI] [PubMed] [Google Scholar]
- 26.Keefe FJ, Caldwell DS, Baucom D, Salley A, Robinson E, Timmons K, Beaupre P, Weisberg J, Helms M (1996) Spouse-assisted coping skills training in the management of osteoarthritic knee pain. Arthritis care and research : the official journal of the Arthritis Health Professions Association 9 (4):279–291 [DOI] [PubMed] [Google Scholar]
- 27.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA (2006) Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry 63 (5):484–489 [DOI] [PubMed] [Google Scholar]
- 28.Eldridge SM, Lancaster GA, Campbell MJ, Thabane L, Hopewell S, Coleman CL, Bond CM (2016) Defining feasibility and pilot studies in preparation for randomized controlled trials: Development of a conceptual framework. PLoS ONE 11 (3):e0150205. doi: 10.137/journal.pone/0150205 [DOI] [PMC free article] [PubMed] [Google Scholar]