Abstract
Myroides spp., formerly Flavobacterium spp., are gram-negative, non-motile, traditionally opportunistic pathogens that are infrequent clinical isolates. Myroides spp. have been pathogenically implicated in only 52 reported cases since the discovery of the Flavobacterium genus in the 1920s. We present a case of Myroides spp. lower extremity cellulitis and bacteremia. To our knowledge, this is the 16th case of cutaneous infection caused by Myroides spp. Etiology of this patient’s infection was felt to be related to exposure of his pre-existing lower extremity wounds to soil and water versus a dog lick in the context of relative immunosuppression from type 2 diabetes and chronic inhaled steroid use. Given the characteristic multi-drug resistance of Myroides spp., resistance to usual empiric antimicrobials given for cellulitis, and potential for fatal infection in cases of pan-resistance, it is important that clinicians remain alert to the possibility of this rare pathogen.
Keywords: Myroides, Cellulitis, Bacteremia
Introduction
The Myroides genus, formerly Flavobacterium genus, is composed of 2 clinically relevant species of traditionally opportunistic aerobic, non-motile gram-negative bacilli including M. odoratus and M. odoratimimus [1]. Though ubiquitous in marine and soil environments, Myroides species have been implicated in 52 documented infections since the 1920s when F. odoratum was first identified, not including the present case [2,3]. While typically found in immunocompromised patients, two cases have been documented in immunocompetent individuals [4,5]. Regardless of immune status, Myroides spp. are frequently multi-drug resistant with incompletely understood mechanisms of resistance [6].
Case
A 69-year-old male with a past medical history significant for chronic obstructive pulmonary disease on chronic inhaled steroids, 40 pack-year smoking history with cessation 7 years ago, hypertension, hyperlipidemia, and type 2 diabetes mellitus (HbA1c during admission 10.2%) presented with confusion and lower extremity redness and swelling. One month prior to presentation, he sustained a fall during which lower extremities were wounded, left greater than right, by a sharp furniture edge. Wound care was performed by the patient with topical antibiotics and bandages, however, wounds worsened with increasing pain. On presentation, the patient was febrile (38.1C) with sinus tachycardia. Physical examination revealed left lower extremity erythema, swelling, and warmth of the anterior shin with a central abrasion that was severely tender to palpation with minimal discharge. Examination of the right lower extremity was also notable for anterior shin erythema and swelling. Multiple healing lesions were noted bilaterally. Laboratory studies were significant for leukocytosis (17,400 cells/ccm with 86.8% neutrophils) and acute kidney injury (serum creatinine 1.84 mg/dL).
Infectious workup revealed mildly elevated procalcitonin (2.13 ng/mL) and CRP (30.07 mg/dL) with normal lactic acid. Blood cultures taken from a peripheral intravenous access site grew Myroides spp., presumably from the patient’s left lower extremity wound. Speciation was achieved via the VITEK 2 system. Susceptibility data revealed multi-drug resistance with susceptibility to ciprofloxacin, imipenem, levofloxacin, and piperacillin/tazobactam (Fig. 1). The patient was started on doxycycline in the emergency department (hospital day 1) given history of possible tick exposure. Upon admission, (hospital day 2), cefazolin was initiated for Gram-positive coverage in the context of cellulitis. Speciation of Myroides (hospital day 3), resulted in expansion to meropenem, which was de-escalated to ciprofloxacin (hospital day 4) based on susceptibilities. Blood cultures drawn on hospital day 3 showed no growth at 5 days. Fig. 2 illustrates progression of this patient’s cellulitis.
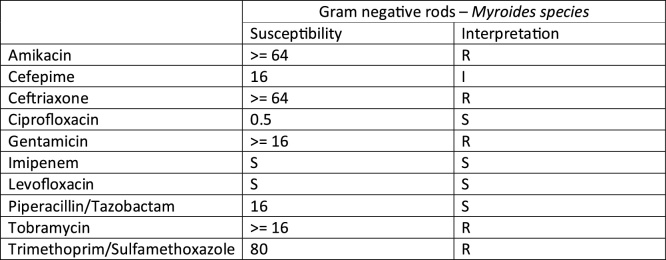
Fig. 1.
Susceptibility data of Myroides spp. isolated from patient’s blood culture. ‘S’ indicates sensitive, ‘R’ indicates resistant, and ‘I’ indicates intermediate sensitivity.
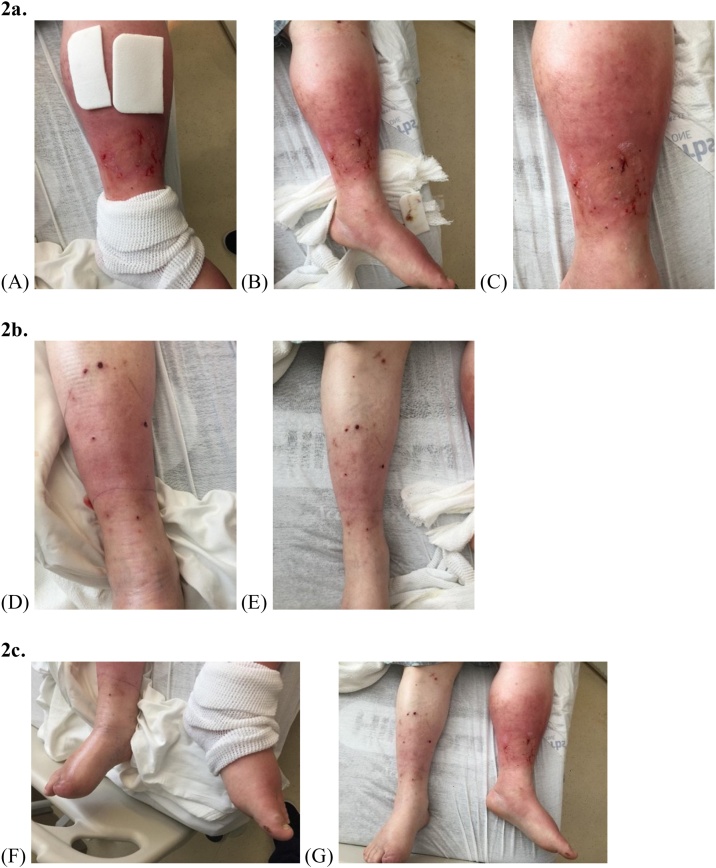
Fig. 2.
Progression of cellulitis over 2 days of antibiotic treatment. Antibiotics included doxycycline (Day 1, duration one day), Cefazolin (Day 2, duration each one day), Meropenem (Day 3, duration one day), Ciprofloxacin (Day 4, duration 10 days).
a. Left Extremity: (A) Day 2 (B) Day 3 (C) Day 3 Close-Up.
b. Right Extremity: (D) Day 2 (E) Day 3.
c. Bilateral Extremities: (F) Day 2 (G) Day 3.
Upon further questioning, the patient reported living in a heavily wooded area, frequently walking on soil and into the woods wearing shorts and sandals. He also reported being licked by his domesticated dog at his open wounds. The patient was discharged on hospital day 5 with a 10-day course of ciprofloxacin, which he completed. His cellulitis was noted to be improving at outpatient follow-up one month later.
Discussion
A case report and literature review published in 2017 cited 48 total cases of Myroides infections since the 1920s when the Flavobacterium genus was first described [2]. Four additional cases have been recorded, including recurrent calcaneal ulcer infection, urinary tract infection, cellulitis and bacteremia in the context of alcoholic cirrhosis, and the current case of lower extremity cellulitis and bacteremia [[7], [8], [9]]. Most Myroides spp. infections occur in skin and soft tissue, ranging from foot gangrene to amputation stump infection, cellulitis, necrotizing fasciitis, and erysipelas [2,4,5,7,[10], [11], [12], [13], [14]]. To our knowledge, the present case is the 16th Myroides spp. cutaneous infection [2,4,5,9,[11], [12], [13], [14]]. Our patient had several comorbidities that could have caused relative immunosuppression, predisposing him to Myroides infection, including type 2 diabetes mellitus and use of chronic inhaled steroids. Although the exact source of his infection is unclear, his wounds may have provided a site for inoculation from his dog’s lick or from soil/water encountered during his nature walks. One prior report implicated Myroides odoratimimus in a case of cellulitis following a pig bite [4]. Flavobacterium spp. have been infrequently isolated from dog bite wounds [15,16]. The close relation of Flavobacterium and Myroides genera may support the rare occurrence of Myroides spp. in dog saliva. Further, in 2012, Myroides phaeus, was isolated from human saliva [17]. More likely in this case is inoculation of our patient’s lower extremity wounds with dirt or water, as Myroides is common in these environments. As in the present case, Myroides spp. are frequently multi-drug resistant due to mechanisms that seem to involve resistance genes, drug efflux pumps, and biofilms [6,18]. 3 fatal cases of Myroides infection have been reported due to pan-resistance in 2 of the 3 cases [8,12,19]. Given the potential for severe morbidity/mortality and resistance of Myroides spp. to usual empiric cellulitis antimicrobials, it is important that providers are alert to Myroides spp. in skin and soft tissue infections such as the present case, which was ultimately successfully treated.
Author statement
Roland conceived the idea of the case report. Dang and Meyer performed chart review and wrote first draft of the manuscript. Dang, Meyer, and Roland performed further revisions. Final manuscript was approved by all authors prior to submission.
Author contributions
Roland conceived the idea of the case report. Dang and Meyer wrote first draft of the manuscript. Dang, Meyer, and Roland performed further revisions. Final manuscript was approved by all authors prior to submission.
Declaration of Competing Interest
None relevant to this study among authors.
References
- 1.Vancanneyt M., Segers P., Torck U., Hoste B., Bernardet J.-F., Vandamme P. Reclassification of Flavobacterium odoratum (Stutzer 1929) strains to a new genus, Myroides, as Myroides odoratus comb. nov. and Myroides odoratimimus sp. nov. Int J Syst Bacteriol. 1996;46(4):926–932. [Google Scholar]
- 2.Holmes B., Snell J.J., Lapage S.P. Flavobacterium odoratum: a species resistant to a wide range of antimicrobial agents. J Clin Pathol. 1979;32(1):73–77. doi: 10.1136/jcp.32.1.73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steinberg J.P., Burd E.M. Elsevier/Saunders; Philadelphia, PA: 2015. Other Gram-Negative and Gram-Variable Bacilli. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. Updated eighth edition; 2015. [Google Scholar]
- 4.Maraki S., Sarchianaki E., Barbagadakis S. Myroides odoratimimus soft tissue infection in an immunocompetent child following a pig bite: case report and literature review. Braz J Infect Dis. 2012;16(4):390–392. doi: 10.1016/j.bjid.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 5.Benedetti P., Rassu M., Pavan G., Sefton A., Pellizzer G. Septic shock, pneumonia, and soft tissue infection due to Myroides odoratimimus: report of a case and review of Myroides infections. Infection. 2011;39(2):161–165. doi: 10.1007/s15010-010-0077-1. [DOI] [PubMed] [Google Scholar]
- 6.Ming D.S., Chen Q.Q., Chen X.T. Analysis of resistance genes in pan-resistant Myroides odoratimimus clinical strain PR63039 using whole genome sequencing. Microb Pathog. 2017;112:164–170. doi: 10.1016/j.micpath.2017.09.012. [DOI] [PubMed] [Google Scholar]
- 7.Pompilio A., Galardi G., Gherardi G., Verginelli F., Geminiani C., Pilloni A.P. Infection of recurrent calcaneal ulcer caused by a biofilm-producer Myroides odoratimimus strain. Folia Microbiol (Praha) 2018;63(2):203–207. doi: 10.1007/s12223-017-0552-5. [DOI] [PubMed] [Google Scholar]
- 8.Ahamed I., Annapandian V.M., Muralidhara K.D. Myroides odoratimimus urinary tract infection. Saudi J Kidney Dis Transplant. 2018;29(5):1220–1222. doi: 10.4103/1319-2442.243957. [DOI] [PubMed] [Google Scholar]
- 9.LaVergne S., Gaufin T., Richman D. Myroides injenensis bacteremia and severe cellulitis. Open Forum Infect Dis. 2019;6(7) doi: 10.1093/ofid/ofz282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beharrysingh R. Myroides bacteremia: a case report and concise review. IDCases. 2017;8:34–36. doi: 10.1016/j.idcr.2017.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bachmeyer C., Entressengle H., Khosrotehrani K., Goldman G., Delisle F., Arlet G. Cellulitis due to Myroides odoratimimus in a patient with alcoholic cirrhosis. Clin Exp Dermatol. 2008;33(1):97–98. doi: 10.1111/j.1365-2230.2007.02590.x. [DOI] [PubMed] [Google Scholar]
- 12.Crum-Cianflone N.F., Matson R.W., Ballon-Landa G. Fatal case of necrotizing fasciitis due to Myroides odoratus. Infection. 2014;42(5):931–935. doi: 10.1007/s15010-014-0626-0. [DOI] [PubMed] [Google Scholar]
- 13.Green B.T., Green K., Nolan P.E. Myroides odoratus cellulitis and bacteremia: case report and review. Scand J Infect Dis. 2001;33(12):932–934. doi: 10.1080/00365540110077065. [DOI] [PubMed] [Google Scholar]
- 14.Bachman K.H., Sewell D.L., Strausbaugh L.J. Recurrent cellulitis and bacteremia caused by Flavobacterium odoratum. Clin Infect Dis. 1996;22(6):1112–1113. doi: 10.1093/clinids/22.6.1112. [DOI] [PubMed] [Google Scholar]
- 15.Abrahamian F.M., Goldstein E.J. Microbiology of animal bite wound infections. Clin Microbiol Rev. 2011;24(2):231–246. doi: 10.1128/CMR.00041-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Talan D.A., Citron D.M., Abrahamian F.M., Moran G.J., Goldstein E.J., Emergency Medicine Animal Bite Infection Study Group Bacteriologic analysis of infected dog and cat bites. N Engl J Med. 1999;340(2):85–92. doi: 10.1056/NEJM199901143400202. [DOI] [PubMed] [Google Scholar]
- 17.Yan S., Zhao N., Zhang X.H. Myroides phaeus sp. nov., isolated from human saliva, and emended descriptions of the genus Myroides and the species Myroides profundi Zhang et al. 2009 and Myroides marinus Cho et al. 2011. Int J Syst Evol Microbiol. 2012;62(Pt 4):770–775. doi: 10.1099/ijs.0.029215-0. [DOI] [PubMed] [Google Scholar]
- 18.Pompilio A., Galardi G., Verginelli F., Muzzi M., Di Giulio A. Di bonaventura g: forms structurally complex and inherently antibiotic-resistant biofilm in a wound-like. Front Microbiol. 2017;8:2591. doi: 10.3389/fmicb.2017.02591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prateek S., Gupta P., Mittal G., Singh A.K. Fatal case of pericardial effusion due to myroides odoratus: a rare case report. J Clin Diagn Res. 2015;9(11):DD01–02. doi: 10.7860/JCDR/2015/15120.6740. [DOI] [PMC free article] [PubMed] [Google Scholar]