Abstract
Background:
Type 2 Diabetes Mellitus (T2DM) poses an ever-increasing threat to people's health worldwide. India has reported high rates of incidence of T2DM. The dangers make accurate assessment of its burden and intervention of lifestyle change, an urgent necessity.
Aims and Objectives:
The aim of the study was to estimate the nationwide prevalence of prediabetes and diabetes, followed by a translational lifestyle trial.
Methodology:
The Indian Yoga Association was commissioned in 2016–2017 by the Government of India to conduct this study which was undertaken in two phases: Phase 1 was to estimate the prevalence of prediabetes and diabetes across the country, and Phase 2 was to conduct a randomized controlled trial using a validated yoga lifestyle protocol. This paper highlights the unique methodology of Phase 1 of the study. The first stage was screening (February to April 2017) for adults (>20 years) with high risk for diabetes on Indian diabetes risk score (IDRS) on mobile app, using a random cluster sampling survey method. All households in the rural (4 villages with about 500 adult population/village) and urban (2 census enumeration blocks [CEBs] of about 1000 adult population/block) sectors of 65 districts (one per ten districts in the entire country) from 29 out of 35 states of India were approached. In the second stage, detailed assessments (sociodemographic, clinical details, A1c, lipid profile, body mass index, stress, and tobacco) were carried out on those with high risk on IDRS and on all self-reported diabetes individuals.
Results:
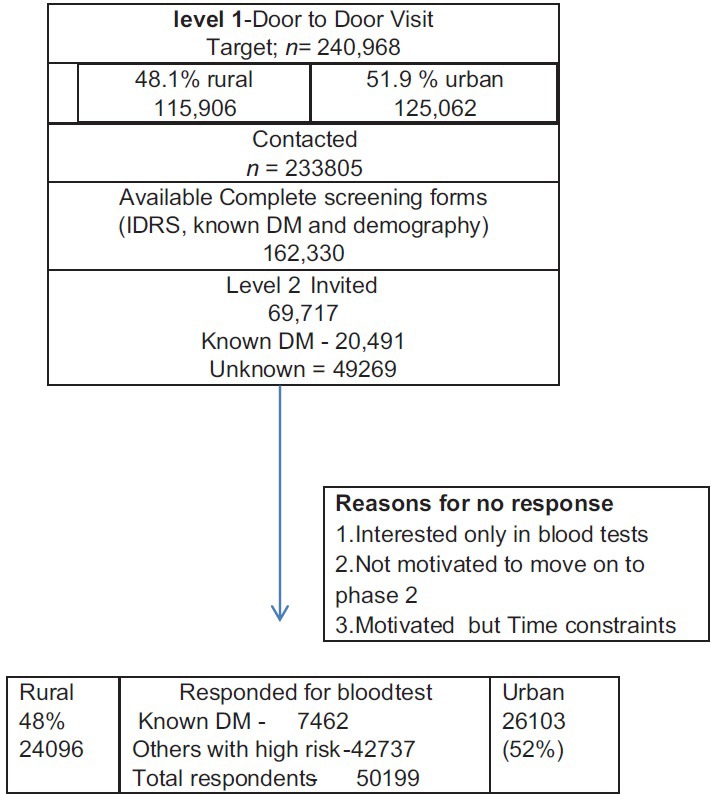
In the first stage of door-to-door visit, 240,968 adults in all households of the selected clusters of villages and CEBs were approached. Of these, 162,330 responded. The respondents in the second stage for detailed assessments in the selected cohort were 50,199 (48% rural and 52% urban) adults. Of these, 7472 were self-reported known diabetes adults and the remaining were 42,737. Prevalence estimates for the country will follow in the future publications.
Conclusion:
This rapid survey completed within 3 months in the entire country using trained volunteers offers the methodology to obtain a quick estimate of diabetes and high-risk population to implement any lifestyle program.
Keywords: Diabetes, India, methodology, prevalence, yoga practices
Introduction
Diabetes mellitus (T2DM) is a major noncommunicable disease, presenting great challenges for healthcare and to the healthcare industry across the globe, especially in recent decades. Management of T2DM and its comorbidities imposes a huge economic burden on nations and their healthcare systems.[1] In India, a series of recent studies suggest that this increasing prevalence will make the country world leader in diabetes by 2025.[2,3,4,5,6,7]
Indian Council of Medical Research-India Diabetes study completed between 2008 and 2015 showed an overall prevalence of 7.3% in 15 states of India, varying from 4.3% in Bihar to 10.0% in Punjab; 47% of those with diabetes had not been diagnosed previously; rates were higher in urban (11.2%) than in rural areas (5.2%) and higher in men than in women below 65 years that reverse after 65 years with take-off age group of 25–34 years.[2,3] A study in Punjab, a northwestern state of India, showed that age factor, marital status, hypertension, and obesity were significantly associated with the prevalence of diabetes.[8]
A multistage survey had pointed to increased prevalence of diabetes and impaired glucose tolerance in urban areas than rural areas.[9] However, a more recent 10-year follow-up study on the prevalence of diabetes and obesity has shown increasing prevalence of diabetes and prediabetes in rural areas when compared to urban areas[10] and much higher increase in low-income group (increase by 135%) than in middle-income group (increase by 24%).[11] This seems to be due to the economic boom resulting in urbanization and corresponding change in lifestyle.[12] It has also been observed that the prevalence of diabetes as seen by glucose tolerance test increases by increasing age, body mass index (BMI), waist score, and monthly income.[13] Interestingly, a stratified random survey has revealed that waist-to-height ratio is a better predictor of diabetes prevalence than BMI.[14] Table 1 summarizes the publications related to the prevalence of T2DM.
Table 1.
Studies on prevalence estimates of diabetes in different parts of India from 2001 to 2015
| Authors/year | Design | Sample size Total n, male/female Urban/rural | Estimated prevalence of diabetes in different parts of India 2001-2015 | |||
|---|---|---|---|---|---|---|
| Area | Overall prevalence | Urban | Rural | |||
| Prospective studies | ||||||
| Ramachandran et al. 2001[12] | Stratified random sampling 1998 | Total - 11216, male - 5288, female - 5928 |
All India | Diabetes 12.1% impaired glucose tolerance-14% | ||
| Sadikot et al., 2004[9] | Random multistage cross-sectional population survey | Urban Total - 10,617 Male - 5379 Female - 5238 Rural Total - 7746 Male - 3629 Female - 4117 |
All India | Prevalence diabetes - 4.3% | 5.9% | 2.7% |
| Ajay et al., 2008[13] | Stratified random technique | Total - 10,930 Male - 6764 Female - 4166 |
All India | Diabetes - 10.1% and impaired FBG - 5.3% | ||
| ICMR 2008-2014[2,3,4,5,6,7] | Stratified multistage design | 16,607 | All India | Prevalence DM Tamil Nadu - 10.4% Maharashtra - 8.4% Jharkhand - 5.3% Chandigarh - 13.6% Prediabetes Tamil Nadu - 8.3% Maharashtra - 12.8% Jharkhand - 8.1% Chandigarh - 14.6% |
DM Tamil Nadu - 13.7% Maharashtra - 10.9 Jharkhand - 13.5 Chandigarh - 14.2 Pre-DM Tamil Nadu - 9.8 Maharashtra - 15.2 Jharkhand - 10.7 Chandigarh - 14.5 |
DM Tamil Nadu - 7.8 Maharashtra - 6.5 Jharkhand - 3.0 Chandigarh - 8.3 Pre-DM Tamil Nadu - 7.1 Maharashtra - 11.1 Jharkhand - 7.4 Chandigarh - 14.7 |
| Tripathy et al., 2017[8] | Cross-sectional survey 2014-2015 | 2463 | Punjab | Prevalence of DM - 8.3% (95% CI 7.3%-9.4%) Prediabetes - 6.3% (5.4%-7.3%) |
DM 9.4 (7.7%-11.4%) Prediabetes 7.0 (5.6%-8.8%) |
DM 7.6 (6.4%-9.1%) Prediabetes 5.8 (4.7%-7.1%) |
| Studies on increasing prevalence over the decade | ||||||
| Deepa M et al., 2011[11] | 10 years’ follow-up survey study from 1998 to 2008 | Number of middle income 1998-479 2008-526 Low income 1998-783 2008-596 |
Chennai | Prevalence increased (1998 versus 2008 P<0.001) in Middle-income GP: From 12.4% to 15.4% (24%) Low-income GP: From 6.5% to 15.3% (135%) Central obesity: LIG male: Increase from 30.8 to 50.9%; female: Increase from 16.9 to 49.8% |
||
| India State-Level Disease Burden Initiative Diabetes Collaborators-2018[10] | Retrospective study | Global (India) | Projected prevalence in India In 1990-26 million In 2016-65 million |
|||
| Studies on projected prevalence of diabetes in India | ||||||
| King H et al., 1998[16] | Prospective study | India | 84-228 million, in the developing countries by 2025 | |||
| Kaveeshwar et al., 2014[15] | Prospective study | India | Predicted by 2030 diabetes may afflict 79.4 million individuals in India | |||
ICMR=Indian Council of Medical Research, DM=Diabetes mellitus, FBG=Fasting blood glucose
Considering the alarming increase in diabetes observed in recent studies,[15,16] in response to call of the Hon’ble Prime Minister of India, the nationwide “Niyantrita Madhumeha Bharata Abhiyaan” (NMB 2017) was launched. The study titled, “Yoga and Diabetes: A Multi Centric Research Study,” was planned with an aim to control the proliferation of diabetes in India using yoga-based lifestyle intervention. The funding was provided by the Ministry of Health and Family Welfare and the Ministry of AYUSH through its Council of Research in Yoga, Government of India, New Delhi (CCRYN, http://www.ccryn.org/). A memorandum of understanding was signed with the Indian Yoga Association (IYA; http://www.yogaiya.in), for planning, designing, and conducting the study. The IYA is a professional national body with representatives from all the major traditional schools of yoga in the country, has prior publications regarding randomized control trials (RCTs) on yoga for diabetes, and has the capacity to recruit the required number of volunteers and researchers and monitor and supervise the implementation of the study.[17,18]
The twin objectives of the study were (a) to estimate the prevalence of diabetes and prediabetes in 2017 simultaneously in all zones of India and (b) to conduct an RCT using a validated yoga lifestyle protocol. This paper is the report of the methodology adopted for the first objective of the study.
Methodology
Sample size calculation
Keeping in mind the twin objectives of the study, the sample size estimation was based on the relative risk reduction in individuals with prediabetes in the Diabetes Community Lifestyle Improvement Program study which was a RCT on 578 overweight/obese Asian Indian adults.[19] The annual incidence rate of diabetes was 11.1% at control condition and 7.8% at intervention condition. This provided a conversion rate at 3-month follow-up to be 3% at control condition and 2% at intervention condition. Based on this, the required sample size for a two-group design, with α = 0.05 and (1− α) = 0.80, was estimated to be 5320 in each group (total 10,640 for two groups). The sample size calculator provided by the University of California San Francisco Clinical and Translational Science Institute (http://www.sample-size.net) was used. Factoring an attrition of 20% in an intervention-based follow-up study, the final sample size required was 12,768. To obtain the required 12,768 individuals with prediabetes, it was calculated a need to screen 232,145 adults above the age of 20 years (12,768 × 100/5.5; the best estimate of prevalence of prediabetes in India was about 5.5%). Thus, we planned to screen about 240,000 individuals across all zones of India. Consequently, the target was 4000 adults/district to be drawn from 60 districts (10% of all districts as in the 2011 Census of India).[20]
Study design
Phase 1 of the study was a nationwide cross-sectional survey using a multilevel stratified cluster sampling technique, with random selection among urban and rural populations covering all states and union territories (UTs) of the country. The first step was to acquire information on diabetes by door-to-door survey using a mobile app and the second step was to invite all individuals with known diabetes and those on high risk to camps for blood tests and other assessments, which were held simultaneously in all locations in the country.
Sampling strategy
The sampling was undertaken at four levels [Figures 1 and 2].
Figure 1.
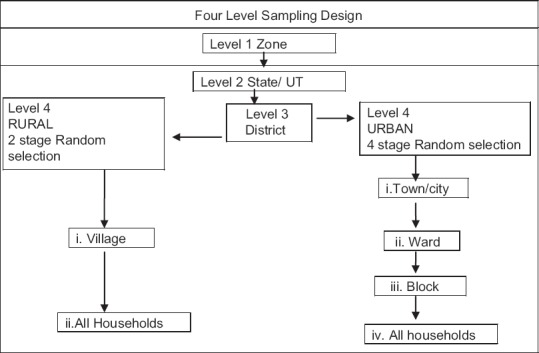
Four-level sampling design. UT = Union territory
Figure 2.
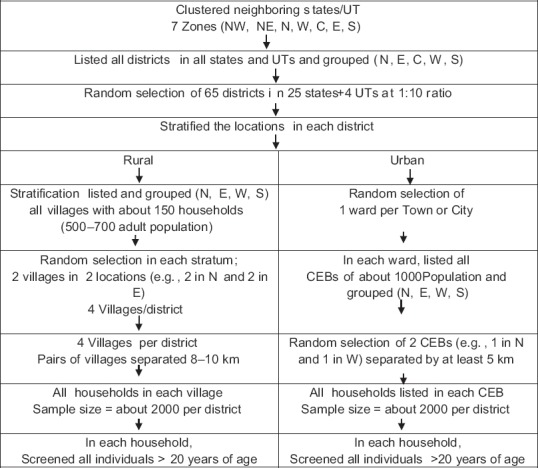
Niyantrita Madhumeha Bharata Abhiyaan 2017, Phase 1 - stratification and random selection. NW = Northwest, NE = Northeast, N = North, W = West, C = Central, E = East, S = South, CEB = Census enumeration block
Level 1 – Zones
Of the 29 states and seven UTs in India in 2017, we planned to cover 26 most populous states and four UTs. The National Family Health-3 sampling methodology was adopted. The first level considered the geographic distribution with each zone comprising contiguous state/UTs. These were grouped as seven zones (northwest, northeast, north, west, central, east, and south) based on cultural homogeneity. Although the earlier grouping as per the website (https://www.mapsofindia.com/zonal) was six zones, we considered Jammu and Kashmir as a separate zone based on their unique social and cultural factors.
Level 2 – States
Figure 3 gives the states grouped under each zone. In the south zone, the two states (Telangana and Andhra Pradesh) were considered as one undivided Andhra Pradesh due to its cultural homogeneity. We did not include remote or small states/UTs (Nagaland, Mizoram, Sikkim, Daman and Diu, Dadar and Nagar Haveli, and Lakshadweep), the key reason being that the IYA did not have a representative in these areas.
Figure 3.
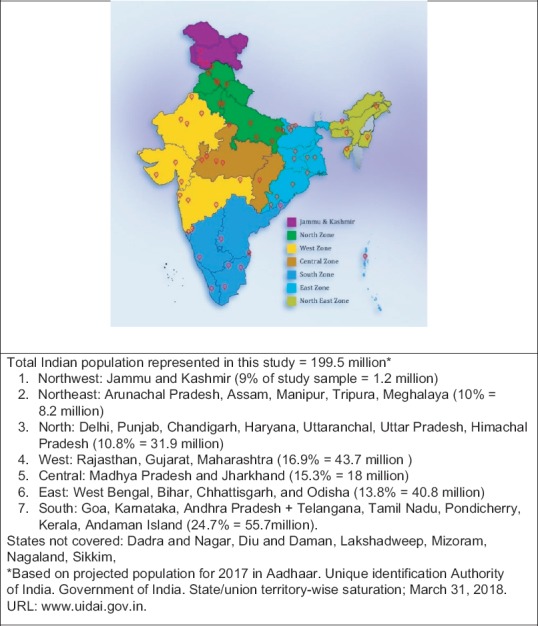
Map of India showing zones covered in survey
Level 3 – Districts
The districts in the state were the first level of sampling. A list of all districts in the state was downloaded (http://districts.nic.in). As per the sampling plan, it was decided to select 10% of the total number of districts in the country. And correspondingly 10% of districts within each state. As the number of districts in different states varied between 1 (e.g., Chandigarh) to 75 (in Uttar Pradesh), there was wide variation in the number of districts selected in each state [Table 2]. In any state with 10–30 districts, two districts were chosen, and in states with ≤10 districts, one district was chosen.
Table 2.
Names of districts selected in different zones
| Zone | State or UT | Names of randomized districts | Names of selected districts | Reasons for change |
|---|---|---|---|---|
| Northwest | Jammu and Kashmir | Kathua, Samba | Jammu, Kulgam, Kathua, Samba | Terrorist activity |
| Northeast | Arunachal Pradesh | Papum Pare | Papum Pare | |
| Northeast | Assam | Golaghat, Baksa | Dibrugarh, Jorhat, Kamrup, Sibsagar, Tinsukia | Spread out population |
| Northeast | Manipur | Imphal West | Imphal West | |
| Northeast | Meghalaya | Jaintia hills | East Khasi Hills | Proximity to YVDM |
| Northeast | Tripura | Dhalai | Dhalia | |
| North | Uttar Pradesh | Allahabad, Lucknow, Mau, Gorakhpur, Meerut, Jhansi | Varanasi, Mau, Lucknow, Ghaziabad, Balliaa, and Allahabad | Proximity to YVDM |
| North | Uttarakhand | Dehradun | Dehradun, Haridwar | Village in next district |
| North | NCT Delhi (UT) | West Delhi | West Delhi | |
| North | Haryana | Jind, Hisar | Panchkula | Proximity to YVDM |
| North | Himachal Pradesh | Kullu | Kangra | Proximity to YVDM |
| North | Chandigarh (UT) | Chandigarh | Chandigarh | |
| North | Punjab | Jalandhar, Amritsar | Jalandar | |
| Central | Bihar | Patna, Vaishali, Nevada, Gaya | Patna, Muzaffarpur, Vaishali | Political |
| Central | Chhattisgarh | Dhamtari, Bilasapur | Raipur, Dhamtari | Proximity to YVDM |
| Central | Madhya Pradesh | Gwalior, Umaria, Neemuch, Bhopal, Ujjain | Gwalior, Raisen, Neemuch, Bhopal, Ujjain | Proximity to SRF |
| West | Goa | North Goa | North Goa | |
| West | Gujarat | Ahmedabad Surat, Navsari | Navsari, Ahmedabad Surat | |
| East | Jharkhand | Ranchi, Gumla | Hazaribag, Ranchi | Proximity to YVDM |
| East | Odisha | Baleshwar, Bargarh | Baleshwar, Bargarh | |
| East | West Bengal | Burdwan, Bankura | Burdwan, Bankura | |
| West | Maharashtra | Nagpur, Thane, Ahmed Nagar | Nagpur, Thane, Ahmednagar | |
| West | Rajasthan | Ajmer, Alwar, Sikar | Sriganganagar, Nagaur, Ajmer | Proximity to YVDM |
| South | Andhra Pradesh and Telangana | Anantapur, Vishakapatnam, Vizainagar | Anantapur, Vishakapatnam, Vizainagar | |
| South | Karnataka | Belgaum, Bengaluru, DK | Belgaum, Bengaluru, Mysore | Town in Mysore added. Spread out less population in DK |
| South | Kerala | Ernakulam | Ernakulam | |
| South | Puducherry (UT) | Puducherry | Puducherry | |
| South | Tamil Nadu | Kancheepuram, Madurai, Salem | Kancheepuram, Madurai, Salem |
YVDM=Yoga Volunteer for Diabetes Movement, UT=Union territory, DK=Dakshina Kannada, NCT=National Capital Territory
To ensure that districts chosen are not clustered, depending on the number of districts needed, the state was grouped accordingly. For example, if the five districts were needed, we divided the state into five groups from north, south, east, west, and central locations, or if three districts were needed, three groups were formed, i.e., north, south, and central on the map.
A statistician in the next step selected two districts randomly in each group, i.e., double the number of districts needed from each state. The concerned field senior research fellow (SRF) after review of the local conditions within each district and in consultation with the zonal coordinator and central office purposively sampled one out of two districts listed from each group.
Level-4 – Villages (rural) and towns/cities (urban)
Level 4 was rural and urban areas as defined by the census. The list of villages and towns as available from the websites (mohua.gov.in/cms/number-of-cities-towns-by-city-size-class.php and India Village Directory @VList.in) was downloaded.
Rural
Keeping in mind the Phase 2 of our study, very small (<500 adult population) and large (>1000 population) villages were excluded, especially to prevent contamination of the intervention. Hence, villages with an adult population of about 500 (100–175 households) were specifically listed. The list of all these selected villages was grouped according to four locations (north, south, east, and west). The statistician selected two villages randomly in each location and provided a list of eight villages to the field SRF. The concerned SRF in consultation with the zonal coordinator, depending on the local conditions, purposively sampled four villages, one in each location.
Urban
A list of all towns/cities in the selected district was downloaded (http://censusindia.gov.in/). A existing coded list of the towns/cities in the district was grouped into four groups (from north, east, west, and south). The statistician selected one town/city randomly in each location and thus prepared a list of four towns/cities. The field SRF reviewing local conditions and in consultation with the zonal coordinator purposively sampled one town/city. In the identified city/town, the list of all wards was downloaded. One ward was selected randomly by the SRF. In the selected ward, all census enumeration blocks (CEBs) were listed. The CEBs, depending on the adult population, were grouped into north, south, east, and west groups. Considering that about 2000 adults were needed for the study, either two or four CEBs (depending on the population within CEBs) were selected using lottery method by the SRFs (2 CEBs of 1000 population or 4 CEBs of 500 population).
The criteria of purposive sampling procedure were nonaccessibility due to geographical terrain or terrorist activity or political disturbances and proximity to the yoga volunteer's residence, who had to commute daily for the intervention in the Phase 2 of the study.
Level 5 – Household
All households (http://censusindia.gov.in/Data_Products/Data_Highlights/Data_Highlights_link/concepts_def_hh.pdf) within the selected village or CEBs in rural or urban locations, respectively, were surveyed. The census location map was used to identify correctly all boundaries of the selected sampling unit (villages or CEB). In every village/CEB selected, a mapping and household listing was carried out with the help of the local village leader. A “household listing operation” then assigned consecutive unique numbers to each and every household. Figures 1 and 2 give the details of the study design.
Study methods and quality assurance
Quality was assured in all aspects of the study by (a) formation of international research advisory committee, (b) standardization of survey protocol and common yoga protocol, (c) selection of standardized assessment tools, (d) standardization of software developed as mobile app, (e) selection of personnel, and (f) training of research personnel for documentation.
Formation of international research advisory committee
An International Research Advisory Committee [Table 3] was constituted with experts having >10 years of experience in research in yoga and diabetes to provide guidance at all stages of the study. This committee supported at all stages of the study by: (a) giving inputs during the conceptualization, (b) reviewing the research protocol critically, (c) suggesting standard assessment tools, (d) giving innovative inputs for development of userfriendly software to be used in the field on mobile app, (e) offering inputs for training of personnel to ensure standard documentation, (f) oversee yoga training of research personnel, (g) guidance to write the report and (h) also participating in the focused discussion group for the standardization of the common yoga protocol for the Phase 2 of the study.
Table 3.
16 experts of International research advisory committee
| Institution | Specialty | Name of expert | Designation |
|---|---|---|---|
| S-VYASA university Chancellor | Research on yoga and its applications | Dr. HR Nagendra† | Trial-Chairperson |
| VYASA | Research on clinical applications of yoga | Dr. R Nagarathna‡,§,* | Medical Director and Principal investigator for this project |
| S-VYASA university | Research on physiology of Yoga | Dr. NK Manjunath Sharma||,§ | Joint Director, R and D |
| Tajen University Taiwan and S-VYASA University | Distinguished research professor | Prof. G Agora Moorthy||,** | College of Environmental and Health Sciences Scientific Advisor |
| University of Manchester UK | Diabetology | Prof. Andrew Boulton||,** | Prof. of Medicine, Division of Diabetes, Endocrinology and Gastroenterology |
| University of Manchester UK | Diabetology | Dr. Kashinath Dixit||,** | Consultant Physician Endocrinologist Manchester Royal Infirmary |
| Kaivalyadhama Yoga Institute | Yoga philosophy and applications | Mr. SubodhTiwari||,†† | CEO |
| MDRF | Diabetes clinician and researcher on diabetes in India | Dr. Vishwanathan Mohan|| | Chairman of MDRF and Chief Consultant |
| MDRF | Molecular biology research on diabetes | Dr. M Balasubramanyam|| | Dean of Research Studies and Senior Scientist MDRF |
| MDRF | Diabetes clinician and researcher on diabetes in India | Dr. RM Anjana|| | Managing Director and Consultant MDRF |
| MDRF | Diabetes Researcher and yoga in diabetes | Dr. Ranjani Harish||,* | Research Officer and Project Manager MDRF |
| AIIMS New Delhi, India | Diabetology | Dr. Nikhil Tandon|| | Professor and Head, Department of Endocrinology and Metabolic Disorders |
| AIIMS, New Delhi | Diabetes research fellow | Dr. Yashdeep Gupta||,* | Assistant Professor Department of Endocrinology and Metabolic Disorders |
| PGIMER Chandigarh, India | Molecular biology neurosciences Yoga expert | Dr. Akshay Anand||,§,††,** | Professor, Department of Neurology |
| Patanjali YogPeeth, Haridwar | Neuroscientist researcher physiology of yoga | Dr. Shirley Telles||,* | Director, Patanjali Research Foundation |
| CYTER Puducherry | Medical professional | Dr. Ananda||,§,* Balayogi | Director of CYTER Chairman research wing of Indian yoga association |
†Conceptualization of the trial and Guidance at all stages, ||Wet the design of research protocol, ‡Monitoring the project at all levels, §Oversee yoga training and monitoring, ††Support training of personnel, **Guidance to write the manuscript, *FGD for yoga protocol. MDRF=Madras diabetes research foundation, S-VYASA=Swami Vivekananda Yoga Anusandhana Samsthana, FGD=Focus group discussion
Standardization of survey protocol
The study protocol had two steps. The first step was the screening using a questionnaire which had standardized questions to assess diabetes risk score and also enlist individuals with known diabetes.
The cases of self-reported known diabetes were confirmed by checking their medical reports if available or checking the names of the medicines they were consuming for their diabetes.
The second step involved assessment camps for blood tests and detailed questionnaire in the subsampled population that included all diabetes subjects and only those in high risk (>60 on IDRS).
Development of standard assessment tools
The study used two separate sets of assessment forms for the two steps of the survey. The form for the first step contained sociodemographic data (age, gender, education, income) for which the Kuppuswamy scale for classification of socioeconomic status of individuals[21] was used. There were also questions from IDRS, a diabetes risk score measure with four factors validated for Indian condition,[22] and questions related to diabetes and its management. The presence of self-reported diabetes was confirmed by checking their medical reports if available or checking the names of the medicines they were advised for their diabetes. The form for the second step was more elaborate which included standard questionnaires validated for India and also more developed for the study after a review of the published literature with appropriate translation [Table 4]. Standardization for biochemical assessments in the NABL-accredited laboratory was assured by checking with the standards for each set of samples as per the NABL requirements. Two rounds of interactive discussions with the research advisory committee helped in finalizing the formats.
Table 4.
Level 2 assessments on mobile app
| Assessment variable | Method | Instrument used | Validation | |
|---|---|---|---|---|
| 1 | Diabetes risk | Hard copy and mobile app | IDRS score 0-90 | Mohan et al., 2005 |
| 2 | Screening form | Hard copy and mobile app | Demography, self-reported diabetes | |
| 3 | Height cm | Hard copy and app | Stand-meter | |
| 4 | Weight | Entered in app | Digital weighing scale | KRUPS co. 2016 |
| Design no. 161856 | ||||
| 5 | Questionnaires | Details in app | SES | Int J Recent Trends Sci Technol 2014;11:1-2. |
| Income and expenditure | Kuppaswamy’s SES scale revised for 2014 | |||
| Gururaj and Maheshwaran 2914 | ||||
| 6 | Known diabetes | Self-reported | Entered into apps | |
| Duration of DM, complications, and associated conditions | ||||
| 7 | Sleep | Quantity, quality, and sleep routine | Taken from many studies | |
| Prepared for the purpose by the psychology department of S-VYASA | ||||
| 8 | Quality of life | PHQ | Thour A, Das S, Sehrawat T, Gupta Y. Indian J Endocrinol Metab 2015;19:252. | |
| Kroenke K, Spitzer RL, Williams JB. J General Internal Med 2001;16:606-13. | ||||
| 9 | Stress | PSS | Cohen S, Kamarck T, Mermelstein R. Perceived Stress Scale. Measuring Stress: A Guide For Health And Social Scientists. 1994. P. 235-83. | |
| Ross A, Thomas S. J Alternat Complementary Med 2010;16:3-12. | ||||
| 10 | Six stress measures for work, family, health, social, financial, others | Numerical analog scale | ||
| 11 | Physical activity | Typical daily work/home activity level, frequency, and amount of mild, moderate, and vigorous activities | Compiled from different studies and modified to be validated in this study | |
| 12 | Alcohol | Alcohol-quantity, frequency, and duration | Modified Version of Babor TF, de la Fuente JR, Saunders J, Grant M. 2011. | |
| 13 | Tobacco | Tobacco smokeless and smoked | Compiled from different studies and modified to be validated in this study |
SES=Socioeconomic status, PSS=Perceived stress scale, PHQ=Patient health questionnaire, DM=Diabetes mellitus
Development and standardization of the common yoga protocol for T2DM for Phase 2 of the study are described separately in the next article as Part 2 Methodology (IJOY).
Development and standardization of software mobile apps
A team of developers headed by a senior project manager with >10 years’ experience in developing software for Indian rural conditions, developed the mobile app under continuous interaction with the principal investigator (PI) and the research associates (RAs). Two versions of the app were made available free of charge on play store: one supporting Android version of <4 and one for higher versions of Android. Provision for capturing data online and offline was provided which remained available throughout the study period for updating and assisting the field staff. The user had to key in the data from the hard copy when internet was available at his office. In addition, the image of the hard copy was also uploaded which was checked randomly on a day-to-day basis by the data operators in the central office for accuracy; feedback was given to the volunteers who uploaded it and also the SRF in charge. Data were stored in Amazon Web Services.
Pilot study for software quality
A prepilot study to check the software was done on 40 purposively selected subjects, 20 with diabetes and 20 without diabetes, admitted at the Yoga Research Health Home for lifestyle change and stress management. The app was frozen after two revisions based on the feedback about the difficulties faced during the keying in process.
Selection of study personnel
Research associates
Two RAs (one with PhD in yoga and the other, a medical doctor with MD in yoga therapy) with >5 years’ experience in research were selected. Table 5 shows the responsibilities of the research personnel.
Table 5.
Responsibilities of research personnel
| Number | Research personnel | Responsibility |
|---|---|---|
| 1 | Principal investigators | Preparation of proposal |
| Monitoring the trial at all levels | ||
| Manuscript writing for publications | ||
| 2 | Advisory committee | Wet the design |
| Guidance/co-author publications | ||
| 3 | Research associate-1 | Preparation of proposal |
| Monitoring the trial at all levels at field level | ||
| 4 | Research associate-2 | Preparation of proposal |
| Monitoring the trial at all levels from central office | ||
| 5 | Zonal coordinators-(n=5) | Select YVDMs with the help of SRFs |
| Organize training program camps for YVDMs | ||
| Monitor and guide SRFs during the trial | ||
| 6 | SRF (1/2 districts) in different zones) | Select YVDMs |
| Manage the orientation camps for YVDMs | ||
| Daily visit to all selected site in allotted district sites by rotation to monitor the trial | ||
| Documentation | ||
| Support the central office in writing the manuscript | ||
| 7 | YVDMs (20/district- field personnel) | House-to-house visit for screening |
| Conduct field training |
YVDMs=Yoga volunteer for diabetes movements, SRFs=Senior research fellows
Zonal coordinators
These were seniors who had experience of working in the rural and urban communities for yoga and other community service activities for >10 years. They volunteered as zonal coordinators and gave constructive inputs while monitoring the progress of the survey through surprise visits to the site that helped in quality assurance.
Senior research fellows
Thirty-five SRFs (1 for 2 districts except in the central office with one/district as they had other responsibilities) with postgraduate diploma or degree in yoga therapy with >5 years’ experience as a trainer of trainers were chosen. The other major criteria were residence being in the selected study location, capacity to interact with local community in local language, and work in harmony with field volunteers, the zonal coordinators, and the central office.
Yoga volunteer for diabetes movement
The SRF selected 20 yoga volunteers within each district (a total of 1200) from among those who were available locally as certified yoga teachers from member organizations of the IYA. Written permission was obtained from the chief of their respective organizations. The criteria for selection were residing near (within 5 km) the selected location (urban or rural), commitment to the cause, and willingness to change their style of teaching to the standardized protocol.
Training of research personnel
Zonal training programs
Zonal training programs of 1 day each were organized in five zones of India (Delhi, Bhopal, Bengaluru, Salem in Tamil Nadu, and Mumbai) to orient zonal coordinators and SRFs to implement the research study in the presence of the PI and any one member of the research advisory committee. They were given orientation to studying protocol and standard procedures for house visits, arranging camps for data acquisition and intervention, training their yoga volunteer for diabetes movements (YVDMS) on use of mobile app and administration of the yoga protocol, and maintaining log books of the regular meetings with their team. A strong communication system between all the researchers was established by developing a common WhatsApp group after clearing all the concerns of these field personnel.
Training of yoga volunteer for diabetes movements
The SRFs arranged residential camps of 5 days each (total 20 camps) for training of yoga volunteers. All YVDMs were certified yoga instructors from different member organizations of the IYA and needed to undergo reorientation in their teaching techniques. The aim of these camps was (a) the introduction to study protocol and accurate documentation of both the subjective (in the two sets of assessment forms) and objective measurements and (b) the orientation for homogeneous teaching methods of the Common Yoga Protocol. The camp ended by a certifying examination (practical, theory, and oral) by the RA who was present in all these camps to check the homogeneity of their documentation on mobile app and uniformity of teaching the yoga practice. Quality control check for interrater variations was done by doing interrater reliability (IRR) test. Two YVDMs were asked to key in the data on both the forms (Step 1 and 2 forms) on the mobile app independently on 120 subjects in a nearby medical center, and IRR was calculated which showed an IRR of 0.7. Table 5 describes the responsibilities of the research personnel.
Quality assurance was ensured through communication between SRFs and YVDMs. A central NMB WhatsApp group, consisting of 35 SRFs, two RAs, and seven zonal coordinators, was created to stay connected with PIs. The regional SRFs also created local WhatsApp groups of 1200 YVDMs (20/district) in their zones for efficient information exchange, seek guidance, and share daily pre- and post-pictures of yoga sessions and online troubleshooting. This helped to maintain good communication and internal audit. It also coincided with a free national internet service that continued for the entire period of study enabling seamless connectivity in the national team.
Assessments
All assessments as indicated in Table 4 were carried out in two stages, i.e., screening for IDRS scoring and diabetes followed by blood tests and detailed data on those with high risk on IDRS and with known diabetes.
Procedure for biochemical measures
All biochemical assays were carried out by the same method throughout the study period. HbA1c was estimated by high-pressure liquid chromatography using the Variant™ II Turbo machine (Bio-Rad, Hercules, CA, USA), which is certified by the National Glyco-hemoglobin Standardization Program as having documented traceability to the Diabetes Control and Complications Study reference method.[9] Serum cholesterol (cholesterol esterase oxidase–peroxidase–amidopyrine method), serum triglycerides (glycerol phosphate oxidase–peroxidase–amidopyrine method), and high-density lipoprotein cholesterol (direct method; polyethylene glycol–pretreated enzymes) were measured using an autoanalyzer (Model 2700/480; Beckman Coulter AU [Olympus, County Clare, Ireland]). Serum creatinine was measured using the Jaffe method. The intra- and inter-assay coefficients of variation for the biochemical assays ranged from target goals for A1C, blood pressure (BP), and low-density lipoprotein (LDL) measures were based on the ADA's Standards of Medical Care for most people with diabetes, including A1C <7.0% (<53 mmol/mol), BP <130/80 mmHg, and LDL <100 mg/dL. Glycemic targets were the primary endpoints of the study.
Data collection
The SRFs, along with the zonal coordinators, visited all places initially to discuss with the village/town leaders, introduced the YVDM and gave awareness talks to prepare for doortodoor screening followed by assessment camps. Table 5 shows the details of the procedure followed.
Step 1: House-to-house survey
The volunteers who had the ID cards of IYA did door-to-door visits with the help of local volunteers. When the doors were locked, or no responsible person of the household was available, the house was visited again within the next 3 days (mop up visits). When necessary, cooperation from the neighbor was sought to contact the members of the household. In the final mop-up round in the last week of the survey, efforts were made to include all such households with the help of the local leaders.
Step 2: Assessment camps
Screened subjects satisfying inclusion/exclusion criteria were invited to assessment camps. Two phlebotomists drew the venous blood in vacutainers and were supported by local volunteers assisting the participants and sticking the coded labels for the tubes (3 aliquots for each participant). The sample was centrifuged at the site for separation of plasma within 1 h, stored in portable cold storage containers, and transported to the nearest laboratory where the assessments were completed within 6 h after drawing the blood [Table 6 and Figure 4].
Table 6.
Assessment camp procedure
| Step | Procedure | Details |
|---|---|---|
| 1 | Registration | Participants showed their tokens |
| Given individual serial numbers | ||
| Noted serial number in their form and also in logbook | ||
| Affixed blue sticker to answer form | ||
| 2 | Anthropometric data | Weight in kilograms; height in meters |
| Hip and waist circumferences (cm) | ||
| BP (SBP and DBP) - 2 readings mm of Hg | ||
| 2-page answer form for manual data entry | ||
| Affixed yellow sticker to answer form | ||
| 3 | Blood collection (fasting) | Draw blood, stick labels, store in cold storage |
| Paste unique bar code on sample tube and answer form | ||
| Affix red sticker to the answer form | ||
| Note time of drawing blood for 2 h PPBG on form | ||
| 4 | Breakfast | Breakfast served to participants |
| Time of breakfast was noted on the answer form | ||
| Affix orange sticker to answer form | ||
| 5 | Questionnaire completion | YVDMs check if all questions are completed |
| Affix purple sticker on the answer form | ||
| 6 | Wait for PPBG | Engage with video and/or lectures on lifestyle diet, health, diabetes, etc. |
| Fill up the detailed registration forms | ||
| Answer questions by participants regarding NMBA | ||
| 7 | Postprandial blood Collection (2 h post) | 2 h after noted breakfast time |
| Paste unique bar code on blood sample tubes, store in cold storage | ||
| Affix green sticker on answer form | ||
| 8 | Final check and data entry by SRF/YVDM | Check completion of answers |
| Collect answer forms with all six stickers before exit | ||
| Transport the blood samples to laboratory | ||
| Key data into NMB android app |
NMBA=Niyantrita Madhumeha Bharata Abhiyaan, YVDMs=Yoga volunteer for diabetes movements, SRF=Senior research fellow, BP=Blood pressure, SBP=Systolic BP, DBP=Diastolic BP, NMB=Niyantrita Madhumeha Bharata
Figure 4.
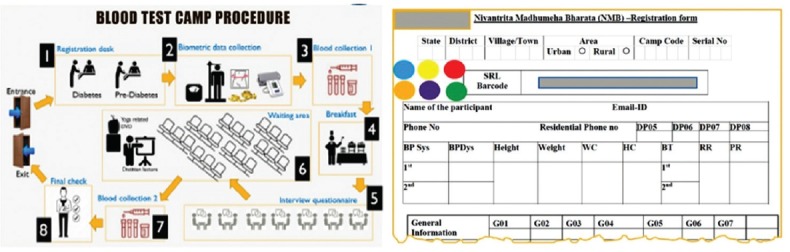
Study protocol during assessments
The quality assurance measures during data acquisition period included regular visits of SRFs to all places by rotation and random visits of zonal coordinators to all places in the zone during the 3-month period. The SRFs and RAs were available to the YVDM continuously on phone and WhatsApp group to solve problems and also to get feedback. The YVDMs sent daily report of the number of houses/persons completed and photographs of their work to the SRF. The RAs and staff of the central office at Swami Vivekananda Yoga Anusandhana Samsthana (S-VYASA) University, Bengaluru, were available all days (7 days/week) for 3 months on phone and WhatsApp group with SRFs for monitoring, guiding, and solving problems. Figure 1 gives a complete assessment procedure.
Compilation of data and statistical analysis
RAs and the software team compiled, matched, cleaned, and analyzed the data. A unique serial number was assigned to each participant. Manually captured data from screening forms were keyed into Mobile Android Apps by trained YVDMs under supervision of SRFs. IRR test was carried out on a subsample of 120 subjects rates by two YVDMs. The accuracy of entries from hard copies into mobile apps was verified by the central office during the analysis phase. All data obtained from the cloud were downloaded and decoded. The uploaded data from the two assessment forms of Step 1 (about 4000/district) and Step 2 and the laboratory data (about 50,000) were checked for perfect matching of coding. Errors in entry (spelling, reversal of first name and second name between pre and post files) were edited using fuzzy logic followed by manual checking. While cleaning the dataset on Excel, cases with wrong entries such as extreme values (e.g., fasting blood glucose values of >1000 mg/dl) were excluded. All cases that had missing data were excluded before analysis. Analyses were done using SPSS version 21.0 and R software version 3.5.1.
Ethical clearance
The institutional ethical committee of IYA after scrutinizing the complete project proposal including informed consent forms approved the proposal. Participants were informed about the procedures involved in detail and their consent for voluntary participation was taken without offering any financial incentives. In addition, in order to obtain full acceptance of the study, an overview of the study including their purpose and objectives, were presented to local community leaders, and their queries answered.
All information was coded and kept confidential. Precautions related to assessments such as availability of medical facility during blood collection were taken. Standardization of assessment procedures during camps was ensured by following the protocol as in Table 6. Laboratory standardization processes were assured by conducting the blood tests in all parts of the country by the same NABL-accredited laboratory. The study was registered on CTRI (Registration Number– Study REF/2018/02/017724).
Results
Table 7 and Figure 3 show the names of the states included under each zone with the numbers and percentage of individuals screened. Response was highest in south zone followed by the west, northwest, and northeast zones; poor responders in north and central zones.
Table 7.
States and union territories surveyed in seven zones of India
| Number | Zone | Number screened (%) | States and UTS |
|---|---|---|---|
| 1 | Northwest | 21,530 (8.9) | Jammu |
| 2 | Northeast | 24,139 (10) | Arunachal Pradesh, Assam, Manipur, Meghalaya, Tripura |
| 3 | North | 26 145 (10.8) | Himachal Pradesh, Chandigarh (UT), NCT of Delhi (UT), Haryana, Punjab, Uttar Pradesh, Uttarakhand |
| 4 | West | 40,640 (17) | Gujarat, Maharashtra, Rajasthan, Goa |
| 5 | Central | 36,917 (15.3) | Bihar, Chhattisgarh, Madhya Pradesh |
| 6 | East | 33,317 (13.8) | Jharkhand, Odisha, West Bengal |
| 7 | South | 58,280 (24) | Andaman (UT), Andhra Pradesh+Telangana, Karnataka, Kerala, Puducherry (UT), Tamil Nadu |
UT=Union territory
Zones, states, and districts included for the study
Table 2 shows the names of the randomly selected districts by the central team at the time of planning and the changes made. Changes were requested by the SRFs in 14 locations (4.7%; 14 out of 240 villages and 60 towns/cities) and were spread across nine states. Because of this, although the total number of villages surveyed did not change, 5 of the changed villages were in the neighboring districts and hence the number of the districts surveyed increased to 65.
Rural (villages) and urban (census enumeration blocks) households
Total number of samples contacted in level 1 of door to door survey were 233805. The complete level 1 screening data was available on 162,330 individuals; 48.1% rural and 51.9% urban. Those with known diabetes and those with not know diabetes but in high risk on IDRS were invited; Of these 69717 (48% rural and 52% urban) invited, 50199 responded to level 2 assessment camps. The distribution of age groups were similar to the national figures in 2017. The overall Indian adult population between 20 50 yrs were 70% while it was 73% in the present study; and those above 50 yrs was 30% in national figures while it was 27% in the present study. Looking at the gender distribution, the percentage of females in our study was marginally higher than the national figures in 2017: all India adultmales were 55% vs 52% in the present study; all India females were 45% vs 48 % in the present study(population pyramid. net) [Figure 5].
Figure 5.
Niyantrita Madhumeha Bharata Abhiyaan 2017 - Phase 1 study profile. IDRS = Indian diabetes risk score, DM = Diabetes mellitus
Discussion
This was the India's largest nationwide rapid survey designed for. This study highlights a three-level screening in almost a quarter-million people in representative urban and rural areas of all populous states in India during a well-defined period of 3 months. Screening of 162,310 adult individuals by random selection method represented 95% of the country's adult population; the age and gender distribution of the screened population was representative of the national figures. After completing IDRS in the first level, blood samples were taken from those most at-risk based on IDRS. Entire ward or village recruitment means that long-term follow-up can compare trends in different parts of the country; further, lifestyle factors (sleep and stress) omitted in earlier nationwide surveys were assessed; cost-effectiveness and volunteer enthusiasm augured well for using India's youth in future national diabetes prevention programs.
Earlier surveys on diabetes in India over the last 25 years used the WHO STEPS procedure.[13] A prevalence estimate by cluster sampling method preceding a lifestyle intervention used in the present study design may be a good option because it answers two important research questions at once, namely prevalence and effects of an intervention. This should be more cost-effective both in time and money as interviewers do not have to travel large distances in the selected areas to interview single members of selected households.[12]
To cover all parts of the country and finish on time, the sampling rate needed to be faster than conventional survey methods. This was achieved by involving 1200 trained yoga volunteers for the study which was provided by the IYA, a professional body with renowned traditional yoga member organizations in India. This is potentially the problem of interrater variations that could influence the accuracy of the documentation.
To reduce interrater variations between the YVDMs, (a) all of them underwent preparatory 5-day training workshops, to achieve homogeneity in their teaching techniques and documentation procedures, (b) the senior RA who was present in all these camps conducted an examination (practical, theory, and oral) to check the uniformity of their data acquisition and teaching skills, and (c) a substudy was done on data acquired on 120 subjects rated independently by two raters (YVDMs) which showed an IRR of 0.7.
Some villages and towns selected by the random selection process by blinded central research team had to be replaced during the purposive selection by the SRFs due to unsuitable local conditions. There were changes of 14 districts in nine states (4.7%) as requested by the field SRFs [Table 2]. The same procedure of random selection of clusters in these changed districts by the blinded central office as before was followed, to avoid bias or reduction in representativeness. The reasons for the requested changes were terrorist activity or political disturbances during the screening period and proximity to the trained YVDM who had to commute daily for survey and intervention in Phase 2. Total number of districts has increased to 65 as the changed villages or towns were in the neighboring districts.
The response of the people in remote districts (Dakshina Kannada in Karnataka and Jorhat and Sibsagar districts in Assam where the houses were spread out over large forest areas) was poor as many adults were out of the village on business during the 3 months of the survey. Hence, the screening was expanded to neighboring wards or villages to complete the numbers required for the sample (4000). We believe this would not have affected the overall results because of the lifestyle similarities in surrounding cohorts.
Problems faced and lessons learned
Difficulty finding committed volunteers
The major challenge of getting motivated skilled yoga instructors who also could be trained in acquisition and management of survey data was solved by the enthusiastic member organizations of the IYA. Many preliminary discussions and meetings had to be conducted before fixing the SRFs and YVDMs in all locations.
Arranging venues in the selected rural and urban areas for camps and motivating the household adults to participate in the study in all parts of the country were a challenge which was solved by enthusiastic participation by the zonal coordinators, local administrators, and philanthropic leaders in the community.
In some areas, the rapidity of the planned survey made it difficult to find sufficient laboratory technicians in the designated period. Nevertheless, the task was successfully completed by shifting the camp dates so that the same phlebotomist could reach different camps in the district. Data entry and analysis took longer than expected because of the errors in entry that needed manual editing of names, e.g., matching the names (although coded) which were spelled differently or interchanged between first and second names in pre–post files, e.g., Rahul Agarwal may have been written in the post as Agarwal Rahul. In Kerala, the program was discontinued due to illness of the SRF. We presume that this may not impact the conclusions of prevalence or intervention effect at all India level as this is a small state, and we had good data from a neighboring state of Tamil Nadu with similar level of epidemiological transition in 2016,[23] although we may not get state-wise details during subanalyses at a later stage.
Conclusion
This Phase 1 of the NMB-2017 study describes that the unique methodology of a two-level rapid survey which was completed within 3 months (representative sample from 95% of India's adult population) was designed to pick up individuals at high risk and avoided costly investigations for diabetes. This template of using the nation's patriotic volunteer force for a nationwide intervention-based study justifies the urgent need to prevent India from becoming the global capital of diabetes.
Financial support and sponsorship
We thank the Ministry of Health and Family Welfare, and the Ministry of AYUSH (through CCRYN), Government of India, New Delhi, India, for funding this nationwide project.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We thank the Ministry of Health and Family Welfare, and the Ministry of AYUSH (through CCRYN), Government of India, New Delhi, India, for funding this nationwide project. We thank Dr. Ishwar Acharya, Director CCRYN, for monitoring the project and his timely help in preparing the necessary DVDs (by Mr. Advait, Mrs. Akanksha, and team) and books during the rapid progression of the project. We are grateful to all members of scientific advisory committee of NMB. We thank the advisory committee members, executive board members, members involved in developing common yoga protocol for NMBA and Dr. Anand Balayogi Bhavanani, Director, Standing Research Committee of the IYA, for their concurrence and active participation at different phases of the project. We thank Mr. Sunil Hosur, Mr. Srikanta B, and their team of software developers for continued support with service attitude during the entire period of the project. We thank the directors and gurus of all major yoga institutions around the country who provided trained and committed yoga volunteers. We are grateful to all YVDMs and SRFs who worked with great enthusiasm to complete the project within the scheduled timelines under difficult weather conditions and political and other problems with minimal financial support. We thank Mr. Jain and NMBA office staff; our gratitude to faculty of VYASA and students of S-VYASA for their immense commitment for service to mother India.
References
- 1.Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:293–301. doi: 10.1016/j.diabres.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 2.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucosetolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 3.Anjana RM, Shanthi Rani CS, Deepa M, Pradeepa R, Sudha V, Divya Nair H, et al. Incidence of diabetes and prediabetes and predictors of progression among Asian Indians: 10-year follow-up of the Chennai Urban Rural Epidemiology Study (CURES) Diabetes Care. 2015;38:1441–8. doi: 10.2337/dc14-2814. [DOI] [PubMed] [Google Scholar]
- 4.Deepa M, Grace M, Binukumar B, Pradeepa R, Roopa S, Khan HM, et al. High burden of prediabetes and diabetes in three large cities in South Asia: The Center for cArdio-metabolic Risk Reduction in South Asia (CARRS) study. Diabetes Res Clin Pract. 2015;110:172–82. doi: 10.1016/j.diabres.2015.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mohan V, Deepa M, Anjana RM, Lanthorn H, Deepa R. Incidence of diabetes and pre-diabetes in a selected urban South Indian population (CUPS-19) J Assoc Physicians India. 2008;56:152–7. [PubMed] [Google Scholar]
- 6.Mohan V, Deepa R, Rani SS, Premalatha G. Chennai Urban Population Study (CUPS No. 5). Prevalence of coronary artery disease and its relationship to lipids in a selected population in South India: The Chennai Urban Population Study (CUPS No. 5) J Am Coll Cardiol. 2001;38:682–7. doi: 10.1016/s0735-1097(01)01415-2. [DOI] [PubMed] [Google Scholar]
- 7.Anjana RM, Deepa M, Pradeepa R, Mahanta J, Narain K, Das HK, et al. Prevalence of diabetes and prediabetes in 15 states of India: Results from the ICMR. INDIAB population-based cross-sectional study. Lancet Diabetes Endocrinol. 2017;5:585–96. doi: 10.1016/S2213-8587(17)30174-2. [DOI] [PubMed] [Google Scholar]
- 8.Tripathy JP, Thakur JS, Jeet G, Chawla S, Jain S, Pal A, et al. Prevalence and risk factors of diabetes in a large community-based study in North India: Results from a STEPS survey in Punjab, India. Diabetol Metab Syndr. 2017;9:8. doi: 10.1186/s13098-017-0207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sadikot SM, Nigam A, Das S, Bajaj S, Zargar AH, Prasannakumar KM, et al. The burden of diabetes and impaired glucose tolerance in India using the WHO 1999 criteria: Prevalence Of Diabetes in India Study (PODIS) Diabetes Res Clin Pract. 2004;66:301–7. doi: 10.1016/j.diabres.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 10.India State-Level Disease Burden Initiative Diabetes Collaborators; India State-Level Disease Burden Initiative Diabetes Collaborators. The increasing burden of diabetes and variations among the states of India: The global burden of disease study 1990-2016. Lancet Glob Health. 2018;6:e1352–62. doi: 10.1016/S2214-109X(18)30387-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deepa M, Anjana RM, Manjula D, Narayan KM, Mohan V. Convergence of prevalence rates of diabetes and cardiometabolic risk factors in middle and low income groups in urban India: 10-year follow-up of the Chennai Urban Population Study. J Diabetes Sci Technol. 2011;5:918–27. doi: 10.1177/193229681100500415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National urban diabetes survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 13.Ajay VS, Prabhakaran D, Jeemon P, Thankappan KR, Mohan V, Ramakrishnan L, et al. Prevalence and determinants of diabetes mellitus in the Indian industrial population. Diabet Med. 2008;25:1187–94. doi: 10.1111/j.1464-5491.2008.02554.x. [DOI] [PubMed] [Google Scholar]
- 14.Rajput R, Rajput M, Bairwa M, Singh J, Saini O, Shankar V, et al. Waist height ratio: A universal screening tool for prediction of metabolic syndrome in urban and rural population of Haryana. Indian J Endocrinol Metab. 2014;18:394–9. doi: 10.4103/2230-8210.131201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kaveeshwar SA, Cornwall J. The current state of diabetes mellitus in India. Australas Med J. 2014;7:45–8. doi: 10.4066/AMJ.2013.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995-2025: Prevalence, numerical estimates, and projections. Diabetes Care. 1998;21:1414–31. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 17. [Last accessed on 2018 Mar 14]. Available from: http://www.pmindia.gov.in/en/news_updates/pm-participates-in-mass-yoga-demonstration-in-chandiga rh/
- 18.PM Releasing Yoga Protocol. [Last accessed on 2016 Jul 02]. Available from: http://svyasa.edu. in/niyantrita-madhumeha-bharata-abhiyaan/
- 19.Weber MB, Ranjani H, Staimez LR, Anjana RM, Ali MK, Narayan KM, et al. The stepwise approach to diabetes prevention: Results from the D-CLIP randomized controlled trial. Diabetes Care. 2016;39:1760–7. doi: 10.2337/dc16-1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Census of India 2011. New Delhi: Registrar General and Census Commissioner of India; 2011. [Last accessed on 2016 Jul 02]. Available from: http://censusindiagov.in/ [Google Scholar]
- 21.Khairnar MR, Wadgave U, Shimpi PV. Kuppuswamy's socio-economic status scale: A revision of occupation and income criteria for 2016. Indian J Pediatr. 2017;84:3–6. doi: 10.1007/s12098-016-2223-y. [DOI] [PubMed] [Google Scholar]
- 22.Mohan V, Deepa R, Deepa M, Somannavar S, Datta M. A simplified Indian diabetes risk score for screening for undiagnosed diabetic subjects. J Assoc Physicians India. 2005;53:759–63. [PubMed] [Google Scholar]
- 23.India State-Level Disease Burden Initiative Collaborators. Nations within a nation: Variations in epidemiological transition across the states of India, 1990-2016 in the global burden of disease study. Lancet. 2017;390:2437–60. doi: 10.1016/S0140-6736(17)32804-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


