Abstract
Background
Teledermatology may improve dermatologic care access in underserved areas and expand the clinical experience of dermatologists-in-training. The potential for teledermatology to supplement global health curricula in dermatology residency education has not been explored.
Methods
An international virtual grand rounds (VGR) curriculum was created based on teledermatology cases from Kabul, Afghanistan. The learning objectives included understanding the diagnosis and management of skin diseases in unfamiliar resource-limited settings and highlighting socioeconomic, cross-cultural, and ethical issues. A 17-item, Likert scale questionnaire was used to assess the effectiveness of the curriculum, including specific Accreditation Council for Graduate Medical Education (ACGME) competencies, as well as interest in global health and teledermatology.
Results
The survey was completed by 85 of 118 VGR attendees (72% response rate). Most respondents considered the curriculum valuable to their education (mean 4.5 on a 5-point Likert scale; standard deviation, 0.5), learned more about diagnosis and treatment of skin diseases in international settings (4.5; 0.6) and in the US (4.1; 0.8), and learned more about socioeconomic, cultural, and ethical issues in skin health (4.6; 0.5). The majority also reported being more interested in global dermatology (4.1; 0.8) and would recommend VGR to a colleague (4.5; 0.6).
Conclusion
This pilot curriculum provided an innovative platform to enhance undergraduate and graduate medical education in international dermatology. International teledermatology education may be used to address multiple ACGME core competencies and increase resident awareness of sociocultural determinants of skin health.
Introduction
Teledermatology and teledermatopathology are emerging healthcare delivery platforms that improve access to care for patients in resource-limited settings by facilitating timely remote consultations about clinical and pathologic findings with dermatologists and pathologists around the world.1,2 This model of care predominantly relies on static, store-and-forward (asynchronous) images but may also utilize live video. Studies have indicated that teledermatology and telepathology are feasible and may be reliable in terms of diagnostic accuracy and management when compared with conventional diagnosis via face-to-face consultation and glass slides.1–4
Beyond serving as a platform for delivering clinical care, teledermatology may also serve as a valuable educational tool for medical students, residents, and attending physicians. This technology has been used as an educational tool across a number of specialties to improve residents’ medical knowledge and diagnostic acuity in nonglobal dermatology care. A survey of United States (US) dermatology residency program directors revealed that 68% were interested in incorporating teledermatology education into their curricula.5 Several dermatology residency curricula have already integrated teledermatology to improve residents’ diagnostic acumen of skin diseases through cased-based practice and supervision from trained dermatologists. Integration of this technology into dermatology resident curricula may also fulfill certain competencies, such as medical knowledge and practice-based learning, in the Dermatology Milestone Project by the Accreditation Council for Graduate Medical Education (ACGME).6–8
While the capacity of teledermatology to improve skin healthcare and general aspects of education has been studied, it remains unclear whether it may be used to improve global health education for dermatologists and dermatology trainees. With the expansion of international commerce and travel, many “exotic” diseases are no longer isolated to a particular region, thereby necessitating a broad global health exposure while in medical training. In one study, German-trained dermatologists reported feeling unprepared to provide care for patients abroad and in tropical nations and requested additional training in tropical dermatology.9 Limited access to global health education has also been described by trainees in the US and Canada.10,11 Previous global health educational endeavors have also failed to address specific ACGME core competencies such as Interpersonal and Communication Skills and Professionalism.6
We hypothesized that an international teledermatology consultation platform may provide untapped educational opportunities for trainees to learn about the socioeconomic, cross-cultural, and ethical issues that influence global skin health. Our study aimed to assess the educational value of an innovative international virtual grand rounds (VGR) pilot curriculum utilizing cases from an international teledermatology collaboration.
Methods
This study was exempted from review by the Emory University Institutional Review Board.
Curriculum development
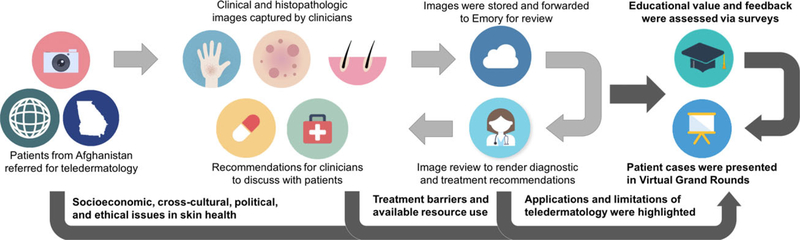
Based upon perceived educational value, four cases were selected from an established store-and-forward teledermatology and teledermatopathology consultation service between a board-certified dermatologist and dermatopathologist at Emory University (BKS) and a board-certified dermatologist at a teaching hospital in Kabul, Afghanistan (JM). Each 15-minute VGR case presentation was structured as follows: clinical history, de-identified clinical images, differential diagnosis, static teledermatopathology images obtained by a general pathologist in Kabul, key discussion points, and relevance to US-based practice (Fig. 1). The learning objectives included understanding the diagnosis and management of skin diseases in unfamiliar resource-limited settings and highlighting socioeconomic, cross-cultural, and ethical issues. The cases were presented in four quarterly conferences (i.e., one case per conference) during Emory University Dermatology Department Grand Rounds from October 2015 to June 2016. Table 1 presents the four cases by diagnosis and key discussion points, including specific socioeconomic, cross-cultural, and/or ethical issues, as well as relevant teledermatology and teledermatopathology issues.
Figure 1.
Creation of Emory dermatology virtual grand rounds case presentations
Table 1.
Case diagnoses and key discussion points
| Diagnosis | Socioeconomic, cross-cultural, and/or ethical issues | Teledermatology and teledermatopathology issues |
|---|---|---|
| Lupus vulgaris |
|
|
| Chromoblastomycosis |
|
|
| Kaposi sarcoma |
|
|
| Mycosis fungoides |
|
|
HIV, human immunodeficiency virus; US, United States.
Participants and surveys
Participants in our study consisted of dermatology faculty, dermatology residents, and medical students attending Emory University Department of Dermatology Grand Rounds. Verbal consent was obtained after informing participants of the anonymous evaluation survey prior to each VGR case presentation. After each case presentation, a 17-item anonymous and voluntary questionnaire was provided to the Grand Rounds audience to collect participant demographics and to assess the educational value of the case presentation. Survey items were developed from the six core competencies for resident education (i.e. patient care and procedural skills, medical knowledge, practice-based learning and improvement, interpersonal and communication skills, professionalism, systems-based practice), as specified by the ACGME.12 Likert scales were used to assess 11 statements regarding the curriculum, with 1 being “strongly disagree” and 5 being “strongly agree.”
Statistical analysis
Descriptive statistics were used to summarize the data. Likert scales were additionally dichotomized as “agree” and “strongly agree” for positive statements and “disagree” and “strongly disagree” for negative statements, as appropriate. Potential associations between survey mean scores and participant demographics were explored using student’s t test or ANOVA, with P < 0.05 considered significant.
Results
Among 118 Grand Rounds attendees, 85 chose to complete the survey for a response rate of 72% (Table 2). All respondents were US-based and physically attended the Grand Rounds sessions, including 31 attending physicians (both Emory-based faculty and community physicians), 36 resident physicians, 13 medical students, and four others. Most respondents (97%) indicated that the curriculum was valuable to their education (mean 4.5, standard deviation (SD) 0.5). Mean score did not differ by training level, prior in-person exposure to the diagnosis, or substantial experience with international dermatology or teledermatology (each P > 0.05).
Table 2.
Survey results (N = 85)
| Survey statement (relevant ACGME core competencies) | Mean (SD)a |
|---|---|
| This presentation was valuable to my education | 4.5 (0.5) |
| I learned more about the presentation, diagnostic approach, and/or treatment of skin disease in international and/or resource-limited settings (MK, PC) | 4.5 (0.6) |
| I learned more about the presentation, diagnostic approach, and/or treatment of skin disease that may be useful for my current practice in the US (MK, PC) | 4.1 (0.8) |
| I learned more about socioeconomic, cultural, and/or political determinants of health in international and/or resource-limited settings (ICS, P) | 4.6 (0.5) |
| I learned to better appreciate ethical dilemmas, differences in cultural values, and/or challenges confronted in practicing medicine in international and/or resource-limited settings (ICS, P) | 4.5 (0.6) |
| I feel more comfortable in engaging individuals and communities from different socioeconomic, cultural, and/or political backgrounds in my current practice in the US (ICS, P) | 4.1 (0.9) |
| I learned more about different healthcare systems and utilizing available resources needed to diagnose or treat patients in international and/or resource-limited settings (SBP) | 4.2 (0.7) |
| I learned more about the applications, strengths, and/or limitations of teledermatology consultations in providing specialist care in international and/or resource-limited settings (SBP) | 4.2 (0.7) |
| I would rather discuss only US-based cases for future Grand Rounds | 1.6 (0.8) |
| This presentation made me more interested in global dermatology | 4.1 (0.8) |
| I would recommend Global Teledermatology Virtual Grand Rounds to a colleague | 4.5 (0.6) |
MK, medical knowledge; PC, patient care; ICS, interpersonal and communication skills; P, professionalism; SBP, systems-based practice
Based on 5-point Likert scales with 1 being strongly disagree and 5 being strongly agree with each statement.
Most participants agreed or strongly agreed on learning more about diagnosis and treatment of skin diseases internationally (94%) and that this knowledge may be useful for current practices in the US for the US-based attendees (77%). Most agreed or strongly agreed on learning more about strengths and limitations of international teledermatology (87%). In addition, almost all respondents (95%) found the curriculum to be beneficial in improving their interpersonal and communication skills, such as understanding cultural and ethical issues in skin health, learning more about social determinants of health in international settings, and becoming more comfortable engaging with communities from different cultural backgrounds. Notably, most respondents (91%) disagreed or strongly disagreed with the statement that they would rather discuss only US-based cases for future Grand Rounds.
The majority of respondents (82%) reported being more interested in international dermatology as a result of the curriculum, with higher mean scores for those without prior in-person exposure to the diagnosis (mean 4.3 [SD 0.7] vs. 4.0 [SD 0.8], P < 0.05). The majority (95%) would recommend the curriculum to a colleague; this result did not differ by participant training levels (P > 0.05).
Discussion
This pilot curriculum utilized an innovative platform of teledermatology and teledermatopathology to supplement dermatology education for attending physicians, residents, and medical students. In terms of the six core clinical competencies adopted by the US ACGME and the American Board of Dermatology,12 one study suggested that US dermatology trainees exposed to teledermatology were most satisfied with improving medical knowledge and practice-based learning and improvement but least satisfied with interpersonal and communication skills and professionalism.6 Our results suggest a formal curriculum in international teledermatology can supplement education across multiple ACGME core competencies, such as Medical Knowledge, Interpersonal and Communication Skills, and Professionalism, as well as cultivate interest in global health.
Prior studies have described the potential benefit of teledermatology for diagnostic consultation and general medical education. For example, a free, web-based, open-access, store-and-forward consultation and educational modality entitled “Virtual Grand Rounds in Dermatology” presents complex medical cases using a VGR-style platform. It has received cases from across the globe and positive qualitative feedback regarding the platform’s potential to improve international collaboration and access to dermatologic care in remote areas.13 Another study evaluated the benefits of the African Teledermatology Project, a collaborative teledermatology program involving dermatology providers in Africa, Europe, and the US.14 This platform not only demonstrated value in fostering remote access to care of skin diseases, it also enabled dissemination of educational materials to underserved areas and continued medical education for both local and international healthcare providers.14 Expanding on these reports, the current study describes how a teledermatology global health curriculum can successfully integrate with ACGME core competencies not routinely addressed by traditional teledermatology, including Interpersonal and Communication Skills and Professionalism. Such integration is vital to gain traction in US residency programs.
While exposure to global health experiences has been shown to increase residents’ cultural awareness and competency, the use of teledermatology in increasing cultural awareness and competency in resident education has not been thoroughly evaluated. Multiple studies across various specialties have described the benefits of in-person international health experiences (i.e. clinical rotations abroad) on residents’ cultural awareness and competency.15–17 Exposure to international health has also been shown to improve resident leadership skills and future involvement in service.18 Where international rotations are not possible, other studies have shown that didactics or classroom-based education can play a role in improving international health exposure and cultural appreciation.15,19 In a telemedicine-based, patient-case focused, ethics in nephrology curriculum, one study reported high trainee exposure to additional contextual features of medicine and cross-cultural appreciation, illustrating that telemedicine could be used to address cultural sensitivity goals in education.20 These experiences demonstrate that international travel is not always necessary to obtain meaningful educational experiences in international health. Our study provides additional evidence that novel educational tools, such as teledermatology-based virtual grand rounds, can improve international health and cross-cultural medical training among residents while addressing ACGME core competencies. Our experience suggests that international teledermatology can be a unique and rewarding tool to expose larger numbers of residents to international health experiences and improve their understanding of the socioeconomic, cross-cultural, and ethical issues in dermatologic care.
The study was limited by its sample size and the scope and number of cases presented. Participants’ knowledge of dermatologic diagnoses and competency in cross-cultural care or international health were not directly assessed. Psychometric validation of the evaluation instrument regarding global health competencies was not performed.21 Implementation and evaluation of an expanded international teledermatology curriculum will allow further assessment of its impact on trainees’ competency in cross-cultural dermatology training and on their perception, interests, and participation in international dermatology work.
Conclusion
This international teledermatology VGR series provided an innovative pedagogical platform to enhance undergraduate and graduate medical education in international dermatology. Survey results suggest that international teledermatology education may address multiple ACGME core competencies and increase resident awareness of sociocultural determinants of skin health.
Acknowledgments
This study was supported in part by the Fund for Innovative Teaching Grant from the Center for Faculty Development and Excellence at Emory University (SCC), the Dermatology Foundation (HY), and the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR002378 and KL2TR002381 (HY). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We gratefully appreciate the assistance of the dermatologists, pathologists, residents, and staff in Kabul, Afghanistan, who participated in the evaluation and management of patients in this study.
Footnotes
Conflicts of interest: None.
References
- 1.Coates SJ, Kvedar J, Granstein RD. Teledermatology: from historical perspective to emerging techniques of the modern era: part I: history, rationale, and current practice. J Am Acad Dermatol 2015; 72: 563–574; quiz 75–76. [DOI] [PubMed] [Google Scholar]
- 2.Coates SJ, Kvedar J, Granstein RD. Teledermatology: from historical perspective to emerging techniques of the modern era: part II: emerging technologies in teledermatology, limitations and future directions. J Am Acad Dermatol 2015; 72: 577–586; quiz 87–88. [DOI] [PubMed] [Google Scholar]
- 3.Levin YS, Warshaw EM. Teledermatology: a review of reliability and accuracy of diagnosis and management. Dermatol Clin 2009; 27: 163–176, vii. [DOI] [PubMed] [Google Scholar]
- 4.Piccolo D, Soyer HP, Burgdorf W, et al. Concordance between telepathologic diagnosis and conventional histopathologic diagnosis: a multiobserver store-and-forward study on 20 skin specimens. Arch Dermatol 2002; 138: 53–58. [DOI] [PubMed] [Google Scholar]
- 5.Wanat KA, Newman S, Finney KM, et al. Teledermatology education: current Use of teledermatology in US residency programs. J Grad Med Educ 2016; 8: 286–287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boyers LN, Schultz A, Baceviciene R, et al. Teledermatology as an educational tool for teaching dermatology to residents and medical students. Telemed J E Health 2015; 21: 312–314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel J, Parr K, Buehler-Bota T, et al. Integrating outpatient teledermatology education into the dermatology resident curriculum. J Grad Med Educ 2016; 8: 468–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nelson CA, Wanat KA, Roth RR, et al. Teledermatology as pedagogy: diagnostic and management concordance between resident and attending dermatologists. J Am Acad Dermatol 2015; 72: 555–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elsner P Dermatology in the tropics and in medical missions: consequences for the training of dermatologists and for continuing medical education. Hautarzt 2015; 66: 355–359. [DOI] [PubMed] [Google Scholar]
- 10.Izadnegahdar R, Correia S, Ohata B, et al. Global health in Canadian medical education: current practices and opportunities. Acad Med 2008; 83: 192–198. [DOI] [PubMed] [Google Scholar]
- 11.Pitt MB, Gladding SP, Suchdev PS, et al. Pediatric global health education: past, present, and future. JAMA Pediatr 2016; 170: 78–84. [DOI] [PubMed] [Google Scholar]
- 12.Accreditation Council for Graduate Medical Education. ACGME Program Requirements for Graduate Medical Education in Dermatology. Available at: https://www.acgme.org/Portals/0yPFAssets/ProgramRequirements/080_dermatology_2017-07-01.pdf. Accessed December 8, 2017.
- 13.Hu SW, Foong HB, Elpern DJ. Virtual Grand Rounds in Dermatology: an 8-year experience in web-based teledermatology. Int J Dermatol 2009; 48: 1313–1319. [DOI] [PubMed] [Google Scholar]
- 14.Weinberg J, Kaddu S, Gabler G, et al. The African Teledermatology Project: providing access to dermatologic care and education in sub-Saharan Africa. Pan Afr Med J 2009; 3: 16. [PMC free article] [PubMed] [Google Scholar]
- 15.Battat R, Seidman G, Chadi N, et al. Global health competencies and approaches in medical education: a literature review. BMC Med Educ 2010; 10: 94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haq C, Rothenberg D, Gjerde C, et al. New world views: preparing physicians in training for global health work. Fam Med 2000; 32: 566–572. [PubMed] [Google Scholar]
- 17.Campbell A, Sullivan M, Sherman R, et al. The medical mission and modern cultural competency training. J Am Coll Surg 2011; 212: 124–129. [DOI] [PubMed] [Google Scholar]
- 18.Yao CA, Swanson J, McCullough M, et al. The medical mission and modern core competency training: a 10-year follow-up of resident experiences in global plastic surgery. Plast Reconstr Surg 2016; 138: 531e–538e. [DOI] [PubMed] [Google Scholar]
- 19.Juarez JA, Marvel K, Brezinski KL, et al. Bridging the gap: a curriculum to teach residents cultural humility. Fam Med 2006; 38: 97–102. [PubMed] [Google Scholar]
- 20.Bramstedt KA, Prang M, Dave S, et al. Telemedicine as an ethics teaching tool for medical students within the nephrology curriculum. Prog Transplant 2014; 24: 294–297. [DOI] [PubMed] [Google Scholar]
- 21.Veras M, Pottie K, Welch V, et al. Reliability and validity of a new survey to assess global health competencies of health professionals. Glob J Health Sci 2012; 5: 13–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Centers for Disease Control and Prevention. Infectious Diseases Pathology Branch Specimen Submission Guidelines. Available at: http://www.cdc.gov/ncezid/dhcpp/idpb/specimen-submission/index.html. Accessed August 5, 2017.