Introduction
You arrive at your clinic and check the schedule, in preparation for a day of patient care. An initial evaluation has been added to your first treatment slot with a referral from an orthopedist for “jumper’s knee”. “I’ve seen this before,” you think to yourself – “patellar tendinopathy, no question.” In preparation, you pull out your patellar tendon loading protocol and make some assumptions about how the patient will present, and how you might approach the shared decision-making for appropriate management. When you begin your assessment, to your surprise, the patient complains of pain in the quadriceps tendon, not in the patellar tendon. What do you do now?
Jumper’s knee is not synonymous with patellar tendinopathy.4 The term includes patellar tendinopathy and quadriceps tendinopathy.4 Patellar tendinopathy has been extensively researched while quadriceps tendinopathy has been largely ignored.8,16,18,24 As a result, clinicians may have resorted to treating quadriceps tendinopathy with rehabilitation programs designed for patellar tendinopathy. Although the patellar and quadriceps tendons work in tandem as part of the extensor mechanism of the knee, they have distinct anatomy and functional roles. As a result, there are probable differences in risk factors, etiology, and response to treatment.
It is time to clinically separate patellar and quadriceps tendinopathy and design more specific rehabilitation programs. In this Viewpoint, we will (1) provide a rationale for distinguishing the two clinical entities – patellar tendinopathy and quadriceps tendinopathy – for treatment decision-making, and (2) identify areas of research priority in quadriceps tendinopathy.
Anatomical and Biomechanical Differences
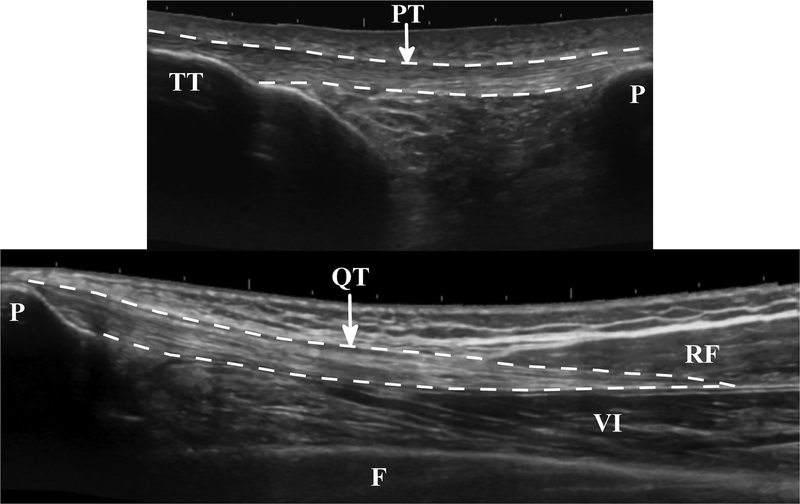
The patellar tendon attaches bone to bone, whereas the quadriceps tendon attaches muscle to bone (Figure 1). The patellar tendon connects two structures of similar stiffness, whereas the quadriceps tendon connects two structures with dramatically different stiffness. Tendon mechanical properties mimic their adjacent structures.2 Tendon has greater extensibility (less stiffness) at the region closest to the muscle. Conversely, regions closer to the bone are less extensible (stiffer).
FIGURE 1.
Longitudinal ultrasound images of uninjured patellar and quadriceps tendons. PT = patellar tendon; TT = tibial tuberosity; P = patella; QT = quadriceps tendon, RF = rectus femoris; VI = vastus intermedius; F = femur.
The adjustment of stiffness along a tendon allows for efficient and safe transmission of force, from compliant muscle to stiff bone.2 When landing from a jump, the knee flexes to absorb the impact. Simultaneously, the quadriceps muscle contracts eccentrically to control knee flexion. The quadriceps tendon must act as a shock absorber, lengthening along with the quadriceps. Where materials of different stiffness join, there can be stress concentrations at their interface.19 Consequently, if the tendon was overly stiff close to the muscle and unable to lengthen, then the quadriceps musculotendinous junction and muscle may be at increased risk of injury. Due to the difference in attachments sites, the patellar tendon is stiffer than the quadriceps tendon.14
There are differences in structure between the patellar and quadriceps tendons. The patellar tendon is a relatively linear structure, composed of a superficial and deep layer, running in parallel, without direct muscular attachments.3 The superficial layer is a continuation of quadriceps tendon fibers from the rectus femoris.1 Fibers of the deep layer begin at the most distal aspect of the patella and insert, along with the superficial fibers, at the tibial tuberosity.1 In contrast, the quadriceps tendon is a more complex and variable structure, arising from four separate muscles. Typically, the quadriceps tendon has three layers, a superficial layer (rectus femoris), intermediate layer (vastus lateralis and medialis), and deep layer (vastus intermedius).1 However, the number of layers and relative contribution of each muscle is highly variable.25
Interactions between these layers and the surrounding matrix may have implications for the pathogenesis, symptom and imaging presentation, or treatment of quadriceps tendinopathy,20 but has not yet been considered in the literature. Each quadriceps muscle has a unique line of action subjecting the quadriceps tendon to non-uniform load and shear forces. The force transmitted through the patellar tendon is more uniform.11,23
Epidemiology of Patellar and Quadriceps Tendinopathy
Patellar tendinopathy presents as pain at the inferior pole of the patella. Up to 14% of recreational and 45% of elite jumping athletes experience symptoms at any given time.9,10 Conversely, quadriceps tendinopathy presents as pain at the superior pole of the patella with symptoms most pronounced with deep knee flexion. The initial onset of symptoms is usually related to an acute incident involving high levels of eccentric quadriceps loading, such as occurs with knee flexion when landing from a rebound in basketball. However, symptoms are typically preceded by a period of excessive load.5 Although few studies have examined the prevalence of quadriceps tendinopathy, the prevalence estimates range from 0.2% to 2% in athletic populations.9,21 Among athletes with extensor mechanism pain, up to one in four experience pain at the superior pole of the patella.9,21
Treatment of Patellar and Quadriceps Tendinopathy: Similarities and Differences
Clinicians and patients are challenged by a lack of scientific evidence to help them make quality decisions when managing quadriceps tendinopathy.16 In the absence of evidence, understanding the anatomy and biomechanics of the quadriceps tendon can help the clinician tailor a treatment program for quadriceps tendinopathy. In this section we highlight the common principles for treating patellar and quadriceps tendinopathy, and provide suggestions for how the clinician might tailor a program for quadriceps tendinopathy (Table 1).
TABLE 1.
Key principles of quadriceps tendinopathy treatment
| Key Principles |
|---|
|
Key principles: activity modification and graduated loading
All tendinopathies, including patellar and quadriceps tendinopathies, are overuse injuries resulting from tendon overload with inadequate recovery.5 The primary symptom is load-dependent tendon pain, where greater loads result in a higher degree of pain, during or immediately after activity. Therefore, these injuries may benefit from activity modification.
In addition to pain, tendinopathies are accompanied by changes in tendon structure (tendinosis) and mechanical properties. Thus, tendinopathies benefit from controlled tendon loading programs to reduce pain, promote remodeling and restore mechanical properties. However, these similarities do not mean that the treatment strategies can be identical for patellar and quadriceps tendinopathy.
Preferentially loading the quadriceps tendon
The patellar tendon and quadriceps tendon are not loaded equally throughout knee motion. The quadriceps tendon experiences greater loads than the patellar tendon as the knee moves further into flexion.12 This relationship is due to an increasing mechanical advantage of the patellar tendon and greater passive tension in the quadriceps muscle as it approaches end-range. This may explain why pain in quadriceps tendinopathy is most pronounced in activities that involve deep knee flexion. Graduated loading programs for quadriceps tendinopathy should include appropriate loading in deep knee flexion. However, bony abnormalities are common and some patients may experience excess compression from the patella. In highly symptomatic cases, the patient may not tolerate loading in deep knee flexion in the early phases of treatment.
The load generated by the four quadriceps muscles causes nonuniform load through the quadriceps tendon. Some areas of the tendon are stress-shielded, and areas close to the patella may be compressed. Areas of lower stress, and areas of increased compression may be more susceptible to injury. Therefore, additional modifications may be needed, based on the patient’s response, to avoid compression and stress-shielding when loading the tendon across the region of injury.11 Based on the multidirectional nature of the quadriceps line of action, tibial rotation may preferentially load or unload specific regions. Combining hip extension with deep knee flexion loading may increase forces in the superficial layer of the tendon.
Pain as a guide for clinical decision making
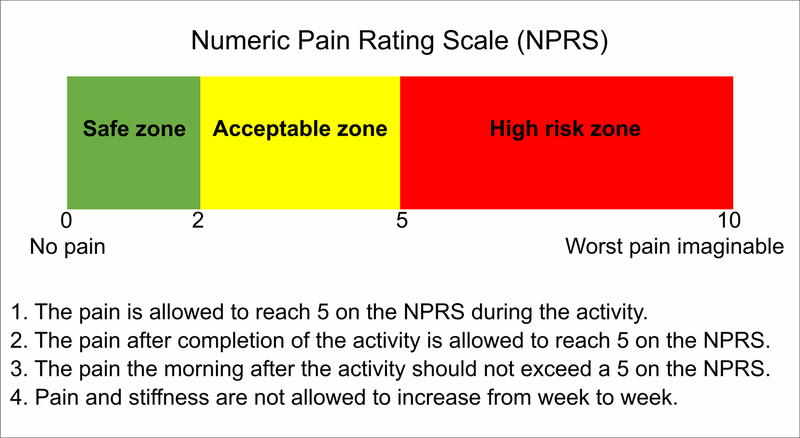
Mild to moderate pain is typically acceptable in patellar tendinopathy treatment protocols. There is no reason to believe this should not be the case for quadriceps tendinopathy. Pain may be a good clinical guide to appropriate tendon loading.17 Because of the complex structure of the quadriceps tendon, it is possible for force transfer to occur without force transmission through the pathological region of the tendon. There may be injury-induced alterations in quadriceps muscle function that unload the pathological region.13 Therefore, provoking pain during tendon loading may help clinicians identify positions where force is transmitted through the appropriate part of the tendon. We suggest that pain should not exceed 5 out of 10 on the numeric pain rating scale (0 = no pain, 10 = worst pain imaginable) during or immediately after treatment (Figure 2).15 Symptoms should subside to baseline levels by the following morning and not increase from week to week. Pain thresholds may need to be modified based on the irritability of the patient.
FIGURE 2.
The pain-monitoring model. Abbreviation: NPRS, numeric pain-rating scale.
Addressing altered muscle function
Changes in corticospinal excitability to the quadriceps muscle in patients with patellar tendinopathy may alter muscle activation.13 In pilot studies, many individuals with patellar tendinopathy had reduced voluntary activation of the quadriceps. Therefore, we expect that there may be changes in quadriceps muscle function among patients with quadriceps tendinopathy. However, these changes may pose additional problems in quadriceps tendinopathy that are not present in patellar tendinopathy. In patellar tendinopathy, the force from the quadriceps is ultimately transferred through the patella to the patellar tendon, even if this force is diminished. In quadriceps tendinopathy, changes in relative activation of the four muscles may underload or stress shield the pathological area. Neuromuscular electrical stimulation or functional electrical stimulation may help offset these changes, augmenting quadriceps activation and ensuring adequate loading of all regions of the tendon.
Restoration of mechanical properties
The mechanical properties of tendon are altered by tendinopathy, and performance is impaired.7,22 One aim of treatment for tendon injuries is to restore mechanical properties, although the clinical goals may be different. The mechanical properties of healthy patellar and quadriceps tendons differ, and may also respond differently to injury. We have observed in patients with unilateral quadriceps tendinopathy (using sonoelastography – a non-invasive method of measuring mechanical properties in-vivo) that symptomatic quadriceps tendons have lower stiffness in the pathological region than the uninjured limb.6 In contrast, in patellar tendinopathy, increased stiffness correlates with symptom severity.26
Summary
There are differences in anatomy, function and response to injury that warrant clinical distinction of patellar tendinopathy and quadriceps tendinopathy. To help clinicians and patients with quadriceps tendinopathy make quality decisions, we suggest future research must focus on 3 key areas:
Investigating the etiology and characteristics of patellar tendinopathy, addressing what regions or layers of the tendon are most commonly involved. Alterations to exercises that preferentially load the most common areas of pathology should be identified and tested.
Developing quadriceps tendinopathy-specific outcome measures, including measures of symptom severity and tendon mechanical properties, to provide a more complete picture of tendon health.
Conducting clinical trials to ascertain the efficacy of current and proposed treatments so clinicians can design and implement effective, tailored treatment programs.
Key Points:
Patellar and quadriceps tendinopathies are often grouped under the umbrella diagnosis of Jumper’s Knee.
Although the patellar and quadriceps tendons work in tandem as part of the extensor mechanism, they have distinct anatomy and functional roles.
Quadriceps tendon loading should be performed in deep knee flexion and additional alterations may be necessary to preferentially load the pathological region.
Recognition and research of quadriceps tendinopathy as a distinct diagnosis is needed to improve patient outcomes.
Acknowledgements:
Funding: This works was supported in part by Promotion of Doctoral Studies I and Florence P. Kendall Doctoral Scholarships from the Foundation for Physical Therapy, by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under award number T32HD007490–18, and by an Endowment Scholarship from the University of Delaware Department of Physical Therapy.
Footnotes
Statement of Financial Disclosure and Conflict of Interest: The authors affirm that we have no financial affiliation (including research funding) or involvement with any commercial organization that has a direct financial interest in any matter included in this manuscript.
Statement of Institutional Review Board Approval: Not required.
Citations
- 1.Andrikoula S, Tokis A, Vasiliadis HS, Georgoulis A. The extensor mechanism of the knee joint: An anatomical study. Knee Surgery, Sport Traumatol Arthrosc. 2006;14(3):214–220. doi: 10.1007/s00167-005-0680-3. [DOI] [PubMed] [Google Scholar]
- 2.Arruda EM, Calve S, Dennis RG, Mundy K, Baar K. Regional variation of tibialis anterior tendon mechanics is lost following denervation. J Appl Physiol. 2006;101(4):1113–1117. doi: 10.1152/japplphysiol.00612.2005. [DOI] [PubMed] [Google Scholar]
- 3.Basso O, Johnson DP, Amis AA. The anatomy of the patellar tendon. Knee Surgery, Sport Traumatol Arthrosc. 2001;9(1):2–5. doi: 10.1007/s001670000133. [DOI] [PubMed] [Google Scholar]
- 4.Blazina ME, Kerlan RK, Jobe FW, Carter VS, Carlson GJ. Jumper’s knee. Orthop Clin North Am. 1973;4(3):665–678. doi: 10.1097/RHU.0000000000000123. [DOI] [PubMed] [Google Scholar]
- 5.Ferretti A Epidemiology of Jumper’s Knee. Sport Med. 1986;3(4):289–295. [DOI] [PubMed] [Google Scholar]
- 6.Klauser AS, Miyamoto H, Bellmann-Weiler R, Feuchtner GM, Wick MC, Jaschke WR. Sonoelastography: Musculoskeletal Applications. Radiology. 2014;272(3):622–633. doi: 10.1148/radiol.14121765. [DOI] [PubMed] [Google Scholar]
- 7.Kubo K, Kawakami Y, Fukunaga T. Influence of elastic properties of tendon structures on jump performance in humans. J Appl Physiol. 1999;87(6):2090–2096. doi:http://jap.physiology.org/content/87/6/2090. [DOI] [PubMed] [Google Scholar]
- 8.Larsson MEH, Käll I, Nilsson-Helander K. Treatment of patellar tendinopathy—a systematic review of randomized controlled trials. Knee Surgery, Sport Traumatol Arthrosc. 2012;20(8):1632–1646. doi: 10.1007/s00167-011-1825-1. [DOI] [PubMed] [Google Scholar]
- 9.Lian OB, Engebretsen L, Bahr R. Prevalence of jumper’s knee among elite athletes from different sports: a cross-sectional study. Am J Sports Med. 2005;33(4):561–567. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- 10.Lian ØB, Engebretsen L, Bahr R. Prevalence of Jumper’s Knee among Elite Athletes from Different Sports: A Cross-sectional Study. Am J Sports Med. 2005;33(4):561–567. doi: 10.1177/0363546504270454. [DOI] [PubMed] [Google Scholar]
- 11.Maganaris CN, Narici MV., Almekinders LC, Maffulli N. Biomechanics and pathophysiology of overuse tendon injuries: Ideas on insertional tendinopathy. Sport Med. 2004;34(14):1005–1017. doi: 10.2165/00007256-200434140-00005. [DOI] [PubMed] [Google Scholar]
- 12.Powers CM, Chen Y-J, Scher IS, Lee TQ. Multiplane loading of the extensor mechanism alters the patellar ligament force/quadriceps force ratio. J Biomech Eng. 2010;132(2):024503. doi: 10.1115/1.4000852. [DOI] [PubMed] [Google Scholar]
- 13.Rio E, Kidgell D, Moseley GL, Cook J. Elevated corticospinal excitability in patellar tendinopathy compared with other anterior knee pain or no pain. Scand J Med Sci Sports. 2016;26(9):1072–1079. doi: 10.1111/sms.12538. [DOI] [PubMed] [Google Scholar]
- 14.Shani RH, Umpierez E, Nasert M, Hiza EA, Xerogeanes J. Biomechanical comparison of quadriceps and patellar tendon grafts in anterior cruciate ligament reconstruction. Arthrosc - J Arthrosc Relat Surg. 2016;32(1):71–75. doi: 10.1016/j.arthro.2015.06.051. [DOI] [PubMed] [Google Scholar]
- 15.Silbernagel KG, Thomeé R, Eriksson BI, Karlsson J. Continued sports activity, using a pain-monitoring model, during rehabilitation in patients with Achilles tendinopathy: a randomized controlled study. Am J Sports Med. 2007;35(6):897–906. doi: 10.1177/0363546506298279. [DOI] [PubMed] [Google Scholar]
- 16.Simpson M, Smith TO. Quadriceps tendinopathy — a forgotten pathology for physiotherapists? A systematic review of the current evidence-base. Phys Ther Rev. 2011;16(6):455–461. doi: 10.1179/1743288X11Y.0000000035. [DOI] [Google Scholar]
- 17.Smith BE, Hendrick P, Smith TO, et al. Should exercises be painful in the management of chronic musculoskeletal pain? A systematic review and meta-analysis. Br J Sports Med. 2017;51(23):1679–1687. doi: 10.1136/bjsports-2016-097383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sprague AL, Smith AH, Knox P, Pohlig RT, Grävare Silbernagel K. Modifiable risk factors for patellar tendinopathy in athletes: a systematic review and meta-analysis. Br J Sports Med. 2018;52(24):1575–1585. doi: 10.1136/bjsports-2017-099000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomopoulos S, Birman V, Genin GM. Structural Interfaces and Attachments in Biology.; 2013. doi: 10.1007/978-1-4614-3317-0. [DOI] [Google Scholar]
- 20.Thorpe CT, Riley GP, Birch HL, Clegg PD, Screen HRC. Fascicles and the interfascicular matrix show adaptation for fatigue resistance in energy storing tendons. Acta Biomater. 2016;42:308–315. doi: 10.1016/j.actbio.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Visnes H, Tegnander A, Bahr R. Ultrasound characteristics of the patellar and quadriceps tendons among young elite athletes. Scand J Med Sci Sport. 2015;25(2):205–215. doi: 10.1111/sms.12191. [DOI] [PubMed] [Google Scholar]
- 22.De Vries AJ, Koolhaas W, Zwerver J, et al. The impact of patellar tendinopathy on sports and work performance in active athletes. Res Sport Med. 2017;25(3):253–265. doi: 10.1080/15438627.2017.1314292. [DOI] [PubMed] [Google Scholar]
- 23.Wilson NA, Sheehan FT. Dynamic in vivo quadriceps lines-of-action. J Biomech. 2010;43(11):2106–2113. doi: 10.1016/j.jbiomech.2010.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Van Der Worp H, de Poel HJ, Diercks RL, et al. Jumper’s knee or lander’s knee? A systematic review of the relation between jump biomechanics and patellar tendinopathy. Int J Sports Med. 2014;35(8):714–722. doi: 10.1055/s-0033-1358674. [DOI] [PubMed] [Google Scholar]
- 25.Zeiss J, Saddemi SR, Ebraheim NA. MR imaging of the quadriceps tendon: normal layered configuration and its importance in cases of tendon rupture. AJR Am J Roentgenol. 1992;159(5):1031–1034. doi: 10.2214/ajr.159.5.1414770. [DOI] [PubMed] [Google Scholar]
- 26.Zhang ZJ, Ng GY, Lee WC, Fu SN. Changes in morphological and elastic properties of patellar tendon in athletes with unilateral patellar tendinopathy and their relationships with pain and functional disability. PLoS One. 2014;9(10):e108337. doi: 10.1371/journal.pone.0108337. [DOI] [PMC free article] [PubMed] [Google Scholar]