Abstract
Objective:
The purpose of the study was to evaluate the degree to which registered nurses perceive their labor and delivery units to be adhering to AWHONN staffing guidelines.
Design:
This was a prospective cross-sectional study via an online survey of labor nurses recruited from hospitals in three states.
Setting:
In late 2016 and early 2017, labor nurses in selected hospitals in California, Michigan, and New Jersey were contacted via email invitation to participate in a study about nursing care during labor and birth. Nurse leaders in each hospital facilitated the invitations.
Participants:
Six hundred and 15 nurses from 67 hospitals.
Measurements:
Descriptive statistics and linear regression models were used for data analysis.
Results:
Most nurses reported the AWHONN nurse staffing guidelines were frequently or always followed in all aspects of care surveyed. Hospitals with annual birth volumes in the 500–999 range compared to hospitals with 2500 or more annual births were significantly more likely to be perceived as compliant with AWHONN staffing guidelines.
Conclusion:
When the AWHONN staffing guidelines were first published in 2010, there was concern among some nurse leaders that they would not be adopted into clinical practice, yet nurses in our sample overwhelmingly perceived their hospitals to be guideline compliant. There remains much more work to be done to determine nurse-sensitive outcomes for maternity care and to ensure that all women in labor in the United States are cared for by nurses who are not overburdened and distracted by more patients than can be safely handled.
Keywords: Obstetric nursing, nursing staff, hospital, delivery rooms
Precis:
Hospitals in our study appear to have incorporated the 2010 AWHONN staffing guidelines into clinical practice.
Background
As part of ongoing efforts to promote safe care for mothers and babies, the Association of Women’s Health, Obstetric, and Neonatal Nurses (AWHONN) sponsored a study from 2012 to 2017 about nurse staffing during labor and birth. The scope and details of the project were based in part on the feedback of 887 AWHONN members who participated in an online survey in June 2010 (Simpson, Lyndon, Wilson, & Ruhl, 2012) about issues they felt the AWHONN nurse staffing taskforce should consider when developing Guidelines for professional registered nurse staffing for perinatal units (AWHONN, 2010) that were published later that year. Members provided rich, detailed descriptions of the consequences of inadequate staffing (Simpson, Lyndon, & Ruhl, 2016) and offered suggestions for safe staffing that were integrated into the staffing guidelines (Simpson et al., 2012).
In 2012, a science team was assembled and a research plan developed. Review of the literature revealed little research on nurse staffing in perinatal units. No studies were found attempting to link perinatal nurse staffing to patient outcomes. In contrast, there was a growing body of evidence about nurse staffing in general medical-surgical units and intensive care units and the impact of staffing on various patient outcomes including risk of death (Aiken et al., 2011; Kane, Shamliyan, Mueller, Duval, & Wilt, 2007; Lucero, Lake, & Aiken, 2010; Rafferty et al., 2007). Based on review of existing evidence on nurse staffing and AWHONN member feedback on the consequences of inadequate nurse staffing, the science team chose the concept of missed nursing care, which was in wide use to study nurse staffing in medical-surgical units, as a framework for further study of maternity nursing (Kalisch, Gosselin, & Choi, 2012; Kalisch, Landstrom, & Williams, 2009; Kalisch, Landstrom, & Hinshaw, 2009; Kalisch & Lee, 2012; Kalisch, McLaughlin, & Dabney, 2012; Kalisch, Tschannen, & Lee, 2011). The science team designed a research plan to develop the science base for evaluating potential relationships between missed nursing care during labor and birth, nurse staffing during labor and birth, selected measures of the practice environment, and patient outcomes. Stages of this research plan completed to date include adapting a measure of missed nursing care to the context of labor and birth, and field testing the Nursing Care during Labor Survey which included the missed nurse care measure, nurse-reported perceptions of their unit’s compliance with AWHONN staffing guidelines, and several other measures deemed relevant. Our instrument development process and outcomes are described elsewhere (Lyndon, Simpson, & Spetz, 2017; Simpson & Lyndon, 2016, 2017); Simpson et al., under review) Here we report findings from this larger study regarding incorporation of the AWHONN nurse staffing guidelines into clinical practice as reported by registered nurses working in inpatient settings who care for patients during labor and birth.
Methods
Design
This was a prospective cross-sectional study of nurse perceptions of their units’ degree of compliance with AWHONN staffing guidelines during labor and birth.
Measures
We used an iterative process involving 17 focus groups of nurses, women who had recently given birth, and physicians and described elsewhere (Lyndon, et al., 2017; Simpson & Lyndon, 2016, 2017a; Simpson et al., under review) to develop the survey from which we drew the data for this analysis. In brief, we followed Kalisch’s model (Kalisch & Williams, 2009) to develop a measure of missed nursing care (the Perinatal MissCare Scale) and the complete Nursing Care during Labor survey included questions about missed nursing care (25 items), reasons for missed nursing care (16 items), their unit’s adherence to recommended staffing guidelines for specific aspects of care as per AWHONN (2010) (19 items), safety culture and work environment (17 items), and demographics (8 items). Response options for the items about staffing guideline adherence included rarely, occasionally, frequently, always, and not applicable.
Setting and Participants
In late 2016 and early 2017, nurse leaders in selected birthing hospitals in three states (California, Michigan, and New Jersey) were contacted via email to seek permission to invite labor nurses at their hospital to participate in a study about nursing care during labor and birth. The birthing hospitals selected for invitation to participate in the study were those identified as involved in various perinatal quality care collaboratives that were ongoing in each state. Telephone calls were held as needed between some of the nurse leaders and the investigators to facilitate participation by answering questions and offering additional information or clarification. Labor nurses in hospitals that agreed to participate were invited to complete an online survey that included the Perinatal Missed Nursing Care Survey and other questions about the respondent’s demographics and work environment. Inclusion criterion was nurses who care for women during labor and birth. Institutional review board (IRB) approval was obtained at the researchers’ institutions, an independent IRB for academic and nonacademic institutions, and from participating hospitals that required IRB approval specific to their facilities.
Survey Administration
Labor nurses were invited to participate via an email directly from the study center or an email that was prepared by the study center and sent from a nurse leader in their hospital. The method was based on the preference of the leadership team at the hospital. A link to the survey was included in the email. Direct emails from the study center allowed for up to two follow-up reminder emails. Nurse leaders were encouraged to send follow-up reminder emails as well. A description of the study and acknowledgement of their consent to participate was included in the first section of the on-line survey prior to beginning responses to survey items. Consent, enrollment, and data collection were handled directly by the study center.
Data Analysis
Descriptive statistics were used to describe demographic characteristics of survey participants and their hospitals, and to quantify individual survey items and overall survey results. A staffing score was created for each participant based on their responses to the items about recommended staffing guidelines for specific aspects of care as per AWHONN (2010) ranging from 1 (rarely) to 4 (always). For analyses of nurse-reported staffing by hospital birth volume, hospitals were categorized by birth volume per year (<500; 500 to 999; 1000 to 2499; and ≥2500 births). To obtain reliable estimates of nurse-reported staffing for each hospital, only hospitals with at least 4 completed nurse surveys were included in analyses of nurse staffing by hospital birth volume as per procedures used in previous nurse staffing research (Lake et al., 2017). A minimum of 4 respondents resulted in an adequate (>0.60) intraclass correlation coefficient (Glick, 1985). We examined the association between hospital birth volume and overall adherence to AWHONN (2010) staffing guidelines using mixed-effects linear regression with robust variance estimation, where individual hospital was a random effect and birth volume was a fixed effect; this method accounts for the clustering of nurses within hospitals. Models were bootstrapped with 1000 draws due to non-normal distributions of staffing adherence scores and Bonferroni post-hoc testing was used to identify specific group differences. A significance level of p<0.05 and Stata SE 15 (Stata Corp, College Station, TX) were used for all analyses.
Results
Labor nurses (N = 2,650) in CA, MI, and NJ were invited via email to participate; 783 nurses opened the survey online; 615 surveys had useable nurse-reported staffing data and were included in the analysis. Responses represented 67 hospitals, with an average of 18.3 respondents per facility (range 1–52). Forty-four hospitals had at least four participants and a known 2016 birth volume and thus were included in analyses of nurse-reported staffing by hospital birth volume. For these 44 facilities the average number of respondents was 19.5.
Average age of nurse participants was 42.9 years (range 23–77 years). Nurses had an average of 16.7 years of experience as a nurse (range 0 to 54 years) and an average of 13.8 years as a labor nurse (range 0 to 46 years). Most (62%) had a Bachelor’s degree or higher, 70% had five or more years of experience in caring for women during labor and birth, 75% worked full-time, and 55% usually worked day shift.
Most nurses reported the AWHONN nurse staffing guidelines were being followed frequently or always in all of the aspects of care surveyed (see Table 1). Incorporation of the guidelines ranged from 63% (1 nurse at the beside of a woman receiving magnesium sulfate for the first hour of administration) to 94% (1 nurse at the bedside for active pushing during second stage labor). For most aspects of care, ≥70% of respondents indicated that the nurse staffing recommendation was followed frequently or always. For four aspects, <70% reported the recommendation was followed frequently or always. For five aspects, ≥80% reported frequently or always; and for one aspect it was >90%.
Table 1.
Proportion of survey respondents reporting that their unit frequently or always adheres to specific AWHONN staffing guidelines
| Clinical Situation | Recommended Nurse to Patient Staffing | Frequently / Always Have | N |
|---|---|---|---|
| OB triage | 1 to 2–3 | 77% | 461/595 |
| Antepartum with complications stable | 1 to 3 | 78% | 488/571 |
| Cervical ripening | 1 to 2 | 84% | 505/603 |
| Epidural initiation | 1 to 1 (@ bedside) | 88% | 527/597 |
| VBAC labor | 1 to 1 | 75% | 408/546 |
| Oxytocin in labor | 1 to 1 | 65% | 396/608 |
| Minimal to no pain relief | 1 to 1 | 66% | 403/609 |
| Diabetes | 1 to 1 | 64% | 388/604 |
| Pulmonary disease | 1 to 1 | 69% | 352/511 |
| Cardiac disease | 1 to 1 | 72% | 374/518 |
| Preeclampsia | 1 to 1 | 71% | 428/607 |
| Magnesium sulfate 1st hour | 1 to 1 (@ bedside) | 63% | 380/605 |
| Multiple gestation | 1 to 1 | 78% | 498/600 |
| Fetal demise | 1 to 1 | 83% | 505/605 |
| Category II FHR | 1 to 1 | 71% | 428/605 |
| Category III FHR | 1 to 1 | 83% | 503/605 |
| Active pushing (2nd stage of labor) | 1 to 1 (@ bedside) | 94% | 567/604 |
| Birth | 2 to 1 (1 for mother and 1 for baby) |
78% | 477/610 |
| Postpartum recovery for at least 2 hours | 1 to 2 (1 per mother-baby couplet) |
78% | 466/598 |
Adherence to AWHONN staffing guidelines varied based on annual hospital birth volume (p=0.0265) (See Figure 1). Hospitals reporting 500–999 births per year had the highest average nurse-reported staffing adherence, particularly compared to the largest hospitals, which had the lowest levels of staffing adherence. Specific items that differed significantly based on birth volume included 1-to-1 nursing care during an indeterminate (category II) fetal heart rate tracing (p=0.0032), for women receiving oxytocin for induction or augmentation of labor (p=0.0033), for women with minimal to no pain relief during labor (p=0.0035), and for women with diabetes (p=0.0042), preeclampsia (p=0.0012), multiple gestation (p=0.0002), or fetal demise (p=0.0056), as well as 2 nurses at every birth (p=0.0014). Nurse staffing levels consistent with AWHONN nurse staffing guidelines for each of these aspects of care were significantly more likely in hospitals with annual birth volumes in the 500–999 range compared to hospitals with ≥2500 annual births.
Figure 1.
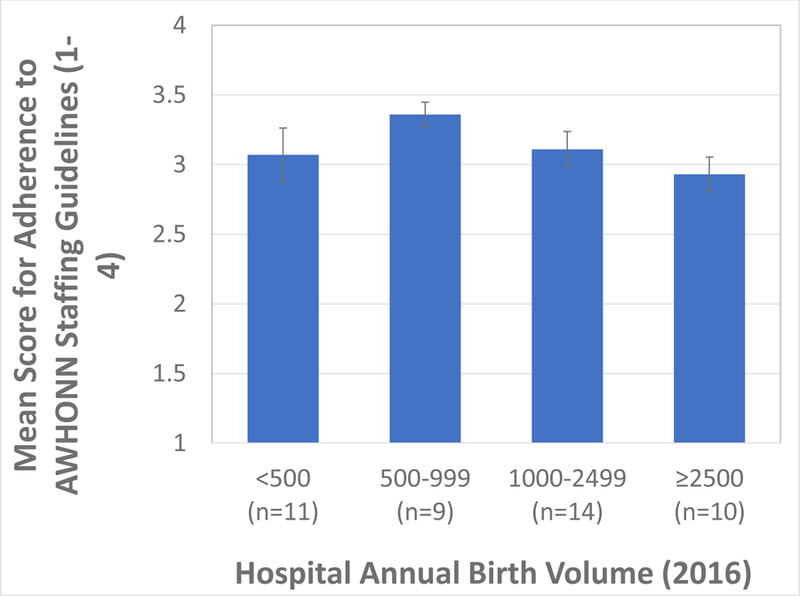
Adherence to AWHONN staffing guidelines by hospital birth volume.
Implications for Practice
Hospitals in this study have largely incorporated the AWHONN nurse staffing guidelines into clinical practice since their publication in September 2010. Based on comparison of our data with the Scheich and Bingham (2015) report on whether 183 hospitals in 43 states were following the staffing guidelines in 2011 and 2012, shortly after the guidelines were published, there appears to be an increase in adherence. An exact comparison cannot be made because the method of determining adherence in the Scheich and Bingham (2015) study varied slightly from this study. In their study, a percentage of yes/no responses was collected from nurse leaders at each hospital for each aspect of perinatal nursing care with an associated recommendation for nurse staffing from AWHONN (2010). In our study, participants may have included the nurse leader in some hospitals, but most were staff nurses and the options for reporting nurse staffing consistent with each aspect of care included rarely, occasionally, frequently, always, and not applicable. Nevertheless, while acknowledging these limitations, several differences between our results and those from Schiech and Bingham (2015) are worth noting. For women receiving oxytocin for induction of labor, Schiech and Bingham found 33% of hospitals reporting adherence to the recommended 1 nurse to 1 woman ratio, while we found 66% of participants reporting adherence. Similarly, for 1 nurse to 1 woman with minimal to no pain relief during labor, 38% were adherent per Schiech and Bingham (2015) versus 66% in this study, and for 1 nurse during postpartum recovery care of mother and baby for at least 2 hours after birth, 44% versus 78% of hospitals were adherent in the two studies, respectively.
Hospitals in this study with annual birth volumes of ≥2500 were less likely to be following the nurse staffing guidelines compared to hospitals with 500–999 annual births. These findings are similar to Schiech and Bingham (2015). It is unknown why larger volume hospitals may be less likely to follow the AWHONN staffing guidelines than smaller volume hospitals, although it is possible that the larger numbers of staff nurses on large units create conditions that allow for immediate rescue of a mother or baby with complications, whereas a smaller volume unit would have to call in nurses to help in these situations. The flexibility that exists in larger volume units of having more nurses on site may be one possible explanation. In many small volume hospitals, there are a minimum of two obstetric skilled registered nurses in-house on a 24/7 basis (Simpson, 2011). That staffing pattern may result in smaller volume hospitals following the staffing guidelines more routinely, as the patient census rarely exceeds the need for more than two OB nurses at one time.
Limitations of our study include requiring hospital participation to reach our sample of labor nurses, which may result in selection bias where only higher performing or higher-resourced facilities agree to participate. However, we had a relatively even distribution of participation across hospital volumes and demonstrated differences in reported staffing performance. The recruitment strategy was necessary as there is no database of labor nurses that is not highly selective, as the AWHONN and National Certification Corporation mailing lists would be. Other studies of nurse staffing have randomly sampled from all registered nurses in given states. This strategy is not feasible for a study only directed at labor nurses. Another limitation is the number of invitees that did not open the email. This is a limitation of electronic surveys, and may be increased by facility firewalls and spam filters and as well as email and survey fatigue. The response rate among nurses who opened the survey was reasonable for an electronic distribution method (Tourangeau, Couper, & Couper, 2013). Finally, this study evaluated nurse perceptions of staffing guideline adherence and did not relate these to the actual staffing or to patient outcomes. Future studies with larger samples of nurses and hospitals will be needed to evaluate these relationships.
Conclusion
When the AWHONN (2010) staffing guidelines were first published, there was concern among some nurse leaders that they would not be adopted into clinical practice. These concerns appear to have been unfounded for most hospitals based on our results; however, there is much more work to be done to ensure that all women in labor in the United States are cared for by nurses who are not overburdened and distracted by more patients than can be safely handled. It is unrealistic to expect that each of the aspects of care outlined in the AWHONN staffing guidelines will be reflected in the staffing patterns on every perinatal unit at all times, but the guidelines offer a reasonable approach to safe nurse staffing that can be used to plan staffing based on historical unit data. Knowing the pattern of patient presentations, elective procedures, and overall patient volume is one of the keys to safe nurse staffing, as is an effective nurse on-call system to cover surges in census and acuity (Simpson, 2015). Garnering budgetary support from the administrative team to follow the AWHONN nurse staffing guidelines is essential. Nurse leaders can use these results as evidence that the AWHONN nurse staffing guidelines are being incorporated into clinical practice and are a reasonable expectation to support safe care for mothers and babies.
Clinical Implications.
The AWHONN nurse staffing guidelines offer suggested nurse to patient ratios for most aspects of inpatient nursing care during pregnancy, labor, birth, and the postpartum-newborn periods.
Nurses caring for women during labor and birth reported observations of nurse staffing in their hospitals via online survey.
Over time based on our results, there has been an increase in incorporation of the AWHONN nurse staffing guidelines into clinical practice.
Labor nurses in hospitals with annual birth volumes ≥2500 reported less adherence to the staffing guidelines than in hospitals with less births per year.
Acknowledgments
Funding: Supported in part by the Association of Women’s Health, Obstetric and Neonatal Nurses and from the Agency for Healthcare Research and Quality grant number R01HS025715. The content is solely the responsibility of the authors and does not necessarily represent the official views of AWHONN or the Agency for Healthcare Research and Quality.
Contributor Information
Kathleen Rice Simpson, Mercy Hospital Saint Louis, Saint Louis, MO.
Audrey Lyndon, James P. and Marjorie A. Livingston Chair in Nursing Excellence, Department of Family Health Care Nursing, University of California San Francisco School of Nursing, 2 Koret Way, Rm N411F, San Francisco, CA 94143-0606.
Joanne Spetz, Philip R. Lee Institute for Health Policy Studies, University of California San Francisco 3333 California Street, Suite 265, San Francisco, CA 94143-0936.
Caryl L. Gay, Department of Family Health Care Nursing, University of California San Francisco School of Nursing, 2 Koret Way, San Francisco, CA 94143-0606.
Gay L Landstrom, Trinity Health, Livonia, MI.
References
- Aiken LH, Cimiotti JP, Sloane DM, Smith HL, Flynn L, & Neff DF (2011). Effects of nurse staffing and nurse education on patient deaths in hospitals with different nurse work environments. Medical Care, 49(12), 1047–1053. doi: 10.1097/MLR.0b013e3182330b6e [DOI] [PMC free article] [PubMed] [Google Scholar]
- Association of Women’s Health, Obstetric, and Neonatal Nurses. (2010). Guidelines for professional registered nurse staffing for perinatal units (pp. 1–54). Washington, DC: Author [Google Scholar]
- Glick WH, (1985). Conceptualizing and measuring organizational and psychological climate: Pitfalls in multilevel research. Academy of Management Review, 10(3), 601–616. 10.5465/amr.1985.4279045 [DOI] [Google Scholar]
- Kalisch BJ, Gosselin K, & Choi SH (2012). A comparison of patient care units with high versus low levels of missed nursing care. Health Care Management Review, 37(4), 320–328. doi: 10.1097/HMR.0b013e318249727e [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom G, & Williams RA (2009). Missed nursing care: errors of omission. Nursing Outlook, 57(1), 3–9. doi: 10.1016/j.outlook.2008.05.007 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Landstrom GL, & Hinshaw AS (2009). Missed nursing care: A concept analysis. Journal of Advanced Nursing, 65(7), 1509–1517. doi: 10.1111/j.1365-2648.2009.05027.x [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, & Lee KH (2012). Congruence of perceptions among nursing leaders and staff regarding missed nursing care and teamwork. Journal of Nursing Administration, 42(10), 473–477. doi: 10.1097/NNA.0b013e31826a1fa4 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, McLaughlin M, & Dabney BW (2012). Patient perceptions of missed nursing care. Joint Commission Journal on Quality and Patient Safety, 38(4), 161–167. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, Tschannen D, & Lee KH (2011). Do staffing levels predict missed nursing care? International Journal for Quality in Health Care, 23(3), 302–308. doi: 10.1093/intqhc/mzr009 [DOI] [PubMed] [Google Scholar]
- Kalisch BJ, & Williams RA (2009). Development and psychometric testing of a tool to measure missed nursing care. Journal of Nursing Administration, 39(5), 211–219. doi: 10.1097/NNA.0b013e3181a23cf5 [DOI] [PubMed] [Google Scholar]
- Kane RL, Shamliyan T, Mueller C, Duval S, & Wilt TJ (2007). Nurse staffing and quality of patient care. Evidence Report Technology Assessment (151), 1–115. Rockville, MD: Agency for Healthcare Research and Quality. [PMC free article] [PubMed] [Google Scholar]
- Lake ET, de Cordova PB, Barton S, Singh S, Agosto PD, Ely B, Roberts KE, Aiken LH (2017). Missed nursing care in pediatrics. Hospital Pediatrics, 7(7), 378–384. 10.1542/hpeds.2016-0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucero RJ, Lake ET, & Aiken LH (2010). Nursing care quality and adverse events in US hospitals. Journal of Clinical Nursing, 19(15–16), 2185–2195. doi: 10.1111/j.1365-2702.2010.03250.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyndon A, Simpson KR, & Spetz J (2017). Thematic analysis of US stakeholder views on the influence of labour nurses’ care on birth outcomes. BMJ Quality and Safety, 26(10), 824–831. doi: 10.1136/bmjqs-2016-005859 [DOI] [PubMed] [Google Scholar]
- Rafferty AM, Clarke SP, Coles J, Ball J, James P, McKee M, & Aiken LH (2007). Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. International Journal of Nursing Studies, 44(2), 175–182. doi: 10.1016/j.ijnurstu.2006.08.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheich B & Bingham D (2015). Key findings from the AWHONN perinatal staffing data collaborative. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 44(2), 317–328. doi: 10.1111/1552-6909.12548 [DOI] [PubMed] [Google Scholar]
- Simpson KR (2015). Predicting nurse staffing needs for a labor and birth unit in a large volume perinatal service. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 44(2), 329–338. doi: 10.1111/1552-6909.12549 [DOI] [PubMed] [Google Scholar]
- Simpson KR (2011). Distribution of births in United States hospitals in 2008: Implications for small volume perinatal units in rural hospitals, Journal of Obstetric, Gynecologic and Neonatal Nursing, 40(4), 432–439. 10.1111/j.1552-6909.2011.01262.x [DOI] [PubMed] [Google Scholar]
- Simpson KR, & Lyndon A (2017a). Consequences of delayed, unfinished, or missed nursing care during labor and birth. Journal of Perinatal of Neonatal Nursing, 31(1), 32–40. doi: 10.1097/JPN.0000000000000203 [DOI] [PubMed] [Google Scholar]
- Simpson KR, & Lyndon A (2017b). Labor nurses’ views of their influence on cesarean birth. MCN The American Journal of Maternal Child Nursing, 42(2), 81–87. doi: 10.1097/nmc.0000000000000308 [DOI] [PubMed] [Google Scholar]
- Simpson KR, Lyndon A, & Ruhl C (2016). Consequences of inadequate staffing include missed care, potential failure to rescue, and job stress and dissatisfaction. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 45(4), 481–490. doi: 10.1016/j.jogn.2016.02.011 [DOI] [PubMed] [Google Scholar]
- Simpson KR, Lyndon A, Wilson J, & Ruhl C (2012). Nurses’ perceptions of critical issues requiring consideration in the development of guidelines for professional registered nurse staffing for perinatal units. Journal of Obstetric, Gynecologic, and Neonatal Nursing, 41(4), 474–482. doi: 10.1111/j.1552-6909.2012.01383.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tourangeau R, Couper MP, & Couper MP (2013). Nonresponse in web surveys. Science of web surveys pp. 36–56. Retrieved from https://ebookcentral-proquest-com.proxy.library.nyu.edu


