Abstract
Korean Americans report the lowest and declined rates of colorectal cancer (CRC) screening, compared to general population in the United States. The present study aimed to evaluate the efficacy of a community-based multifaceted intervention designed to improve CRC screening among Korean Americans. A cluster-randomized trial involving 30 Korean church-based community organizations (n = 925) was conducted. Fifteen churches were assigned to intervention (n=470) and the other 15 to control (n = 455) groups. Main components of the intervention included interactive group education, patient navigation, physician engagement, and provision of fecal immunochemical test (FIT) kit. CRC screening rates were assessed at a 12-month follow-up. Participants in the intervention group were significantly more likely to receive CRC screening (69.3%) as compared with those in the control group (16%). The intervention was particularly effective in promoting FIT among the more disadvantaged individuals in the Korean American community. Regression analysis revealed that controlling for the intervention effect, male gender, high school education, annual income of $20,000–40,000 were significantly associated with increased screening by FIT, whereas English inefficiency was significantly and lack of health insurance was marginally significantly associated with decreased screening by colonoscopy/sigmoidoscopy. Culturally and linguistically appropriate multifaceted intervention combining FIT provision with community-clinical linkage has a potential to be a cost-effective and practical approach to effectively targeting hard-to-reach disadvantaged minority populations and enhance CRC screening to reduce cancer disparities.
Keywords: colorectal cancer (CRC) screening, Korean American, Intervention, FIT, community-based participatory research
INTRODUCTION
Colorectal cancer (CRC) is the second most common cancer among Korean Americans, after lung cancer for Korean men and breast cancer for Korean women (Miller et al., 2008). In the United States, CRC incidence rates have decreased over the past decade, with the change of rates by more than 4% per year in both men and women (American Cancer Society, 2017). However, unlike the general trend, the CRC incidence rates among Korean Americans have increased with the annual percent change (APC) of 3.6% between 1988 and 2007 (Giddings et al., 2012; Lee et al., 2007). Despite the high burden from CRC among Korean Americans, CRC screening rates in this population are significantly lower than the national average (Maxwell and Crespi, 2009; Maxwell et al., 2010; Hwang, 2013; Oh and Jacobsen, 2014).
Currently, several screening tests can be used to find polyps or colorectal cancer. The fecal immunochemical test (FIT) uses antibodies to detect blood in the stool, which is an early sign of cancer. Colonoscopy and sigmoidoscopy both use a thin flexible lighted tube with a camera at the end to check for polyps or cancer inside the rectum and the colon. The difference between the two procedures is that a flexible sigmoidoscopy examines the left lower third of the colon with a short tube, while colonoscopy examines the entire colon with a longer tube (Center for Disease Control and Prevention, 2017). The prevalence of CRC screening in accordance with guidelines among the general US population 50 years of age and older and overall Asian Americans in 2015 was 62.6% vs 49.4% (American Cancer Society, 2014). However, a systematic review of thirteen studies on CRC screening among Korean Americans published until May 2013 (Oh and Jacobsen, 2014) indicated that only one in four Korean Americans aged 50 and older reported having ever had FIT and approximately 40% reported having ever had a sigmoidoscopy or colonoscopy in different studies. In addition, screening rates decreased for both colonoscopy and FIT in Korean Americans, while the rates increased or were stable in the US general population (Maxwell and Crespi, 2009).
The factors contributing to the low rates of and declining trend in screening among Korean Americans are complex. Inadequate knowledge about screening, screening methods, and its benefits, as well as low perceived risks of CRC have been identified as major factors related to low rates of screening among Koreans (Juon et al., 2003; Ma et al., 2009; Maxwell et al., 2010). These studies suggest that Korean Americans may be less familiar with utilizing health care system to detect health problems before the onset of symptoms than other groups, emphasizing the need for education of the benefit of screening before symptoms develop. In addition, the decline of CRC screening rates of this population has been associated with limited access to health system due to lack of insurance, language inefficiency, and lack of transportation (Jo et al., 2008; Lee and Im, 2013; Lee and Lee, 2013).
With the high CRC burden combined with low rates of screening uptake due to multilevel barriers, Korean Americans, particularly, disadvantaged groups with limited English proficiency and low income are an important target group for implementation of innovative and culturally tailored programs to enhance CRC screening. Collaboration among multisector stakeholders, the community members and leaders, clinical providers and researchers, has great potential to enhance cancer screening for this population. Community-based organizations (CBOs) who work directly with the target population serve as a venue for promotion of knowledge and awareness of CRC screening and reduction of barriers to screening (Israel et al., 2005). Engaging CBOs and clinical providers (primary care practices, PCPs) can deliver screening test more effectively by reaching the underserved and hard-to-reach individuals who rarely visit doctors for preventive care. Therefore, implementation of CRC screening in this underserved population requires establishing strategic partnerships between community and clinical settings and sharing their infrastructure and capacity to enhance engagement of potential patients and PCPs in CRC screening, and follow-up care (Ockene et al., 2007; Krist et al., 2013; Persson, 2016).
However, there is clear paucity of culturally and linguistically appropriate CRC community clinical linkage intervention (CCL), designed to improve CRC screening among Korean Americans. To our knowledge, no study has investigated the impact of the CCL intervention for CRC screening in Korean Americans, except for the one we conducted in a small scale quasi-experimental design (Ma et al., 2009). In our previous study, we reported that a culturally and linguistically tailored church-based intervention combined with patient navigation assistance and physician engagement (including screening reminder, scheduling appointment, transportation assistance to clinic sites, navigation for screening, follow up care and medical record verification) was effective in increasing CRC screening rate. Building on our preliminary data (Ma et al., 2009), the present study was designed to evaluate the impact of a large-scale cluster group randomized trial on CRC screening.
Regarding CRC screening methods or modalities, colonoscopy is most commonly recommended in the United States. Colonoscopy has a high sensitivity for polyps and cancer, but is invasive, cumbersome, expensive, and thus, has limited availability in many underserved minority populations (Lieberman et al., 2000; Inadomi et al., 2012; Elmunzer et al., 2015). Although FIT has less sensitivity for polyps and cancer than colonoscopy, it has advantage of being non-invasive, easy-to-do at home, inexpensive, and more readily available as a first step of detecting abnormality. Indeed, when offered or recommended, individuals, particularly from underserved communities, were more likely to complete FIT than colonoscopy, suggesting that FIT based outreach was more effective than colonoscopy-based outreach in increasing screening rates among underserved populations (Inadomi et al., 2012; Gupta et al., 2013; Singal et al., 2016). According to these studies, a programmatic method with less invasiveness and more availability with minimal resources and infrastructure such as FIT appears to be a promising intervention modality for improvement of CRC screening among underserved populations.
This article evaluated the primary outcome, efficacy of a culturally and linguistically appropriate community- clinical linkage intervention that included provision of FIT, group education, patient navigation, and physician engagement on CRC screening.
METHODS
Participants
Korean Americans (N = 925) enrolled in this study were members of Korean churches (N = 30) in Philadelphia and New Jersey regions that serve a predominately underserved immigrant population. More than 78% of Koreans in the US are affiliated with churches (Chang, 2003; Ma et al., 2009; Min, 2002) and the churches serve as one of the community-based organizations facilitating discussion of and participation in various cultural, social and personal activities. Thus, Korean church is one of the important venues to deliver culturally appropriate intervention to provide health education and promote CRC screening among Korean Americans. Participants were eligible to participate in this study if they: (1) were self-identified Korean Americans; (2) were 50 years and older; (3) did not have a colorectal polyp, CRC cancer, or a family history of CRC (first degree relative); and (4) non-adherent to CRC screening guidelines (never had any CRC screening or were overdue for screening). Based on the CRC screening guidelines recommended by the ACS, “overdue” was defined by no FIT in the past year or no sigmoidoscopy in the past five years, no double-contrast barium enema in the past five years, or no colonoscopy within the past ten years.
Procedures
The study was designed as a collaborative partnership among an academic institution, Korean churches, community-based organizations (CBOs), and healthcare providers/organizations. A framework for community-clinical linkages was used to guide the current study and collaboratively established CRC screening program and referral systems that connect individuals with abnormal screening results to clinical care. As part of collaboration, Korean churches provided facilities and resources to promote awareness and knowledge about CRC screening through provision of education sessions and FIT kits. Academic researchers coordinated each stage of study by linking community and clinical settings and provided navigation services as needed.
Participants who performed FIT testing were asked to mail the samples in a provided envelope to their providers. Participants do not have regular physicians or health insurance, were encouraged to mail the samples to the partnering clinicians or health centers of our network. Participants with an abnormal FIT result were notified with a letter written by a clinician and referred to diagnostic colonoscopy. The CAH research team at Temple University has an established network of participating clinical partners who provide a range of health services either at reduced cost to patients who are uninsured or underinsured. Thus, those who had no primary care physician or medical insurance were sent to the collaborating clinical partners for the diagnostic test. This study was approved by the Temple University Institutional Review Board.
Study design
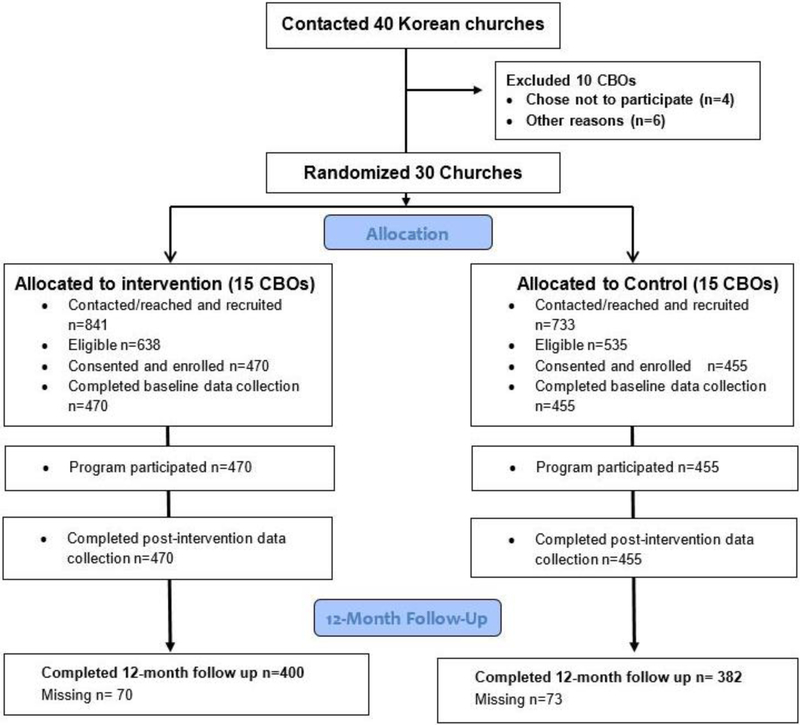
The study utilized a two-arm cluster randomized design with churches as the unit of randomization (Fig 1). Based on organization profile information provided by collaborating church leaders, we paired the 30 churches by size and geographic location. Then, each CBO of the 15 pairs was randomly assigned to the intervention or control group. We conducted baseline evaluation, post-intervention assessment, and a 12-month follow-up on screening outcome. Baseline and post-intervention assessments were administered in person while the 12-month follow-up assessments were conducted by telephone interviews and primary outcome of screening was verified through medical record.
Figure 1.
Study design flow chart.
Intervention and control conditions
The intervention was designed to improve CRC screening among participants who are non-adherent to CRC screening guidelines by addressing multilevel barriers. Main intervention components included interactive group education, navigation services and engagement of health care providers for referrals, and linkage to care. The interactive group education was aimed to increase participant overall understanding of CRC, screening methods, and utilization of available resources such as home test kit and navigation services, with the ultimate goal of increasing screening rates. Bilingual health educators facilitated discussion on CRC susceptibility and severity among Korean Americans and the U.S. general population, benefits of CRC screening, and CRC screening options and their associated clinical procedures, as well as the pros and cons of each option. To increase their motivation for CRC screening and awareness of the different methods, FIT home kit was offered to the participants with instructions in Korean. Although it is provided to all participants in intervention group, they were encouraged to choose any screening methods convenient for them. Clinical partners provided clinical support and ensured successful screening assessment and follow-ups by offering more flexible hours of clinic operation with bilingual medical staff on site. Patient navigation assistance was also offered based on participants’ needs. The range of assistance included scheduling appointments with clinical partners for sigmoidoscopy/colonoscopy for screening and diagnosis after a FIT positive result, assisting paper In the control condition, participants (n = 455) received a group education session in a similar format with that of the intervention group delivered by trained Korean community health educators. Different from the intervention group, the education focused on general health education and primary prevention issues, including routine health examinations and screening for various diseases such as cancer. Korean version of work and communication with a physician, and arranging transportation. standard printed materials and guidelines related to the education contents were also provided, including CRC screening guidelines.
Measures
This study assessment was designed to evaluate the multilevel intervention including individual participants’ level, CBO organization level and clinical linkage to care level, as a result of education, patient navigation, and physician engagement for linkage to care. At participants’ level, we assessed participants’ satisfaction on each component of intervention, screening behaviors and knowledge improvement. In addition, as a process outcome, we assessed the adherence of main stakeholders (CBOs, Patient Navigators and clinical providers) to basic CBPR principles of collaboration in various stages of the project implementation. Since the main purpose of this article was to report the efficacy of the intervention on participants’ screening behaviors, we only reported CRC screening as primary outcome measures and relevant results.
Participant characteristics.
Demographic information such as age gender, education, marital status, household income, employment was collected at baseline. Acculturation related information such as years living in the US and the English ability was also collected. In addition, information on health insurance and regular physician status was collected to learn the levels of health care access of the participants.
Barriers to screening.
Barriers to CRC screening were evaluated by asking them the question: “If you have never had any of the screening such as stool blood test, sigmoidoscopy or colonoscopy, what are the major reasons?” The choices include ‘Do not know what it is’, ‘Do not know where to get it’, ‘Do not have time’, and ‘Feel healthy and do not think needing a test.’
Screening behavior.
The primary outcome was CRC screening status (completion of either FIT kit, sigmoidoscopy, or colonoscopy) at the 12-month follow-up. Bilingual interviewers contacted participants at 12-month follow-up and assessed screening behavior using self-report (“Over the past 12 months, have you had a test for colorectal cancer?”; yes/no, and “If you had, what is the test?”; stool blood test using FIT kit/colonoscopy/sigmoidoscopy). Participants who reported receiving FIT were verified with the list of those who returned the stool sample and received the test results from the collaborating clinical laboratory. Participants who reported receiving colonoscopy or sigmoidoscopy were asked to provide a medical release consent to allow project staff to contact their health care providers to validate self-reported testing. Participants who received positive FIT results and were referred to diagnostic colonoscopy were also followed-up.
Data analysis
Participant characteristics were described using frequencies and percentages within each of the treatment groups (intervention versus control). The chi-square test was used to assess whether the distributions differed between the treatment groups. The chi-square test was also used to compare the proportion of participants in the intervention and control groups who completed CRC screening within 12 months of the intervention. The proportion of participants who completed screening was compared by different CRC screening methods and by recruitment sites. To investigate whether the intervention was particularly effective in disadvantaged individuals, the comparison of screening rates between intervention and control groups was conducted only among the disadvantaged group (i.e., high school or less education, income of <$40,000, no insurance etc.). Finally, logistic regression analyses were conducted to explore the factors associated with FIT and colonoscopy/sigmoidoscopy. In the models, the covariance matrix was adjusted to account for clustering of individuals at the church level. All analyses were performed in SAS version 9.3 assuming a type 1 error of 0.05.
RESULTS
Participant characteristics
Overall, there were slightly more women (59.2%) than men enrolled in the study. Majority of participants were married (80.4%) and did not speak English well (74.1 %). Roughly half were college or higher level educated (50.4), insured (49.7%), and had a regular physician (55.5%). More than half were employed (56.8%) and earned less than $40,000 (66.1%). Table 1 describes and compares sociodemographic characteristics for the intervention and control groups. More participants in the control group than in the intervention group earned greater than $40,000 in annual income (28.1% vs. 21.2%; p = 0.050), and had health insurance (55.5% vs. 46%; p = 0.005). The distribution of other demographic, acculturation, and health access variables were not significantly different between groups.
Table 1.
Characteristics of Intervention and Control Group Participants: CRC Screening Program (n=925).
| Variable | Intervention Group (n=470) No. (%) | Control Group (n=455) No. (%) | P1 |
|---|---|---|---|
| Age (mean years) | 62.28±9.94 | 62.93±9.27 | 0.361 |
| Gender | 0.158 | ||
| Male | 197 (42.5) | 171 (37.8) | |
| Female | 267 (57.5) | 281 (62.2) | |
| Marital status | 0.404 | ||
| Married | 378 (81.5) | 351 (79.2) | |
| Not Married | 86 (18.5) | 92 (20.8) | |
| Education | 0.104 | ||
| Below high school | 55 (12.1) | 71 (16.2) | |
| High school graduate | 150 (32.9) | 153 (34.9) | |
| Some college or higher | 251 (55.0) | 215 (49.0) | |
| Annual household income | 0.050 | ||
| Less than $20,000 | 157 (36.9) | 139 (36.2) | |
| $20,000 - $40,000 | 178 (41.9) | 137 (35.7) | |
| Greater than $40,000 | 90 (21.2) | 108 (28.1) | |
| Employment | 0.736 | ||
| Employed | 257 (56.2) | 251 (57.4) | |
| Unemployed/Retired/Homemaker | 200 (43.8) | 186 (42.6) | |
| Year living in US | <0.001 | ||
| Less than 10 yrs | 90 (12.2) | 104 (15.5) | |
| Between 10 and 20 yrs | 145 (19.7) | 178 (26.6) | |
| More than 20 years | 501 (68.1) | 388 (57.9) | |
| Ability to speak English | 0.296 | ||
| Not at all | 43 (9.3) | 54 (12.1) | |
| Not well | 299 (64.7) | 289 (64.8) | |
| Well/Very well | 120 (26.0) | 103 (23.1) | |
| Health insurance status | 0.005 | ||
| No | 248 (53.9) | 199 (44.5) | |
| Yes | 212 (46.1) | 248 (55.5) | |
| Regular physician status | 0.411 | ||
| No | 191 (42.7) | 171 (40.0) | |
| Yes | 256 (57.3) | 257 (60.0) | |
| Barriers to screening | |||
| Do not know what it is | 0.035 | ||
| Unchecked | 393 (84.0) | 356 (78.4) | |
| Checked | 75 (16.0) | 98 (21.6) | |
| Do not know where to get it | 1.000 | ||
| Unchecked | 442 (94.4) | 429 (94.5) | |
| Checked | 26 (5.6) | 25 (5.5) | |
| Cannot afford | 0.012 | ||
| Unchecked | 335 (71.6) | 358 (78.9) | |
| Checked | 133 (28.4) | 96 (21.1) | |
| Do not have time | 0.339 | ||
| Unchecked | 413 (88.2) | 410 (90.3) | |
| Checked | 55 (11.8) | 44 (9.7) | |
| Transportation difficulty | 0.579 | ||
| Unchecked | 460 (98.3) | 449 (98.9) | |
| Checked | 8 (1.7) | 5 (1.1) | |
| Language difficulty | 0.698 | ||
| Unchecked | 453 (96.8) | 442 (97.4) | |
| Checked | 15 (3.2) | 12 (2.6) | |
| Afraid of pain | 0.243 | ||
| Unchecked | 439 (93.8) | 434 (95.6) | |
| Checked | 29 (6.2) | 20 (4.4) | |
| Feel healthy | 0.001 | ||
| Unchecked | 361 (77.1) | 389 (85.7) | |
| Checked | 107 (22.9) | 65 (14.3) | |
1 P-values based on Rao-Scott chi-square test excluding missing values. Rao-Scott chi-square test used to account for design effects of clustering at the site level.
Barriers of screening were generally similar in distribution between the intervention and control groups, with the exception of three variables. Participants in the intervention group were more likely than those in the control group to endorse ‘not being able to afford it’ (28.4% vs. 22.9%; p = 0.012), and ‘feeling healthy’ (22.9% vs. 14.3%; p =0.001) as the reason of not having had screening. However, less participants (16.0%) of the intervention group reported ‘not knowing what screening is’ compared to those in the control group (21.6%; p = 0.035) (Table 1).
Screening rates by methods and sites
As shown in Table 2-1, CRC screening behaviors were significantly different between intervention and control groups. In the intervention group, a total of 277 out of 400 participants (69.3%) were screened for CRC at 12 months, compared to 61 out of 382 (16.0%) in the control group (χ2 (1) = 226.04, p<0.001). In the intervention group, the majority (66.8%) screened by FIT, and minority screened by colonoscopy (2.0%) and sigmoidoscopy (0.3%). In contrast, in the control group a minority (1.8%) screened by FIT, and the majority screened by colonoscopy (11.5%) and sigmoidoscopy (5.8%).
TABLE 2-1.
CRC Screening Rates at 12 Months Follow-up by Screening Methods
| Outcome | Intervention Group (n=400) No. (%) | Control Group (n=382) No. (%) | P |
|---|---|---|---|
| Screened for CRC | 277 (69.3) | 61 (16.0) | < 0.001 |
| Type of Screening | |||
| FIT | 267(66.8) | 7 (1.8) | < 0.001 |
| Colonoscopy | 8 (2.0) | 44 (11.5) | < 0.001 |
| Sigmoidoscopy | 1 (0.3) | 22 (5.8) | < 0.001 |
P-values based on chi-square test of Fisher’s exact test excluding missing values.
As shown in Table 2-2, out of the 15 paired church sites in the study, the majority (n = 12) had screening rates significantly higher by intervention group than by control group: the screening rates in the intervention group ranged from 60.0% to 93.8%, while corresponding control group screening rates ranged from 0% to 38.9%. However, at 3 church pairs (5th, 8th, and 14th), screening rates were not significantly different between the two treatment groups, with substantially low level of screening rates (33.3% – 45.8%) compared to other sites in the intervention group. Compared to the intervention participants from the other church sites, those from the 5th, 8th, and 14th church pairs were more likely to have college or higher education (73.8% vs. 51.2%; p = 0.005), be employed (73.8 % vs. 55.7%; p = 0.01), have greater than $40,000 annual income (49.1% vs. 15.9%; p < 0.001), and have health insurance coverage (56.5% vs. 42.9%; p = 0.048).
TABLE 2-2.
CRC Screening Rates at 12 Months Follow-up by Community Sites
| Intervention (n=400) | Control (n=382) | P | |||
|---|---|---|---|---|---|
| Pair | N | Test rate (%) | N | Test rate (%) | |
| 1 | 33/41 | 80.5 | 2/20 | 10.0 | <0.001 |
| 2 | 22/36 | 61.1 | 3/17 | 17.6 | 0.004 |
| 3 | 30/37 | 81.1 | 7/35 | 20.0 | <0.001 |
| 4 | 16/31 | 51.6 | 0/21 | 0.00 | <0.001 |
| 5 | 5/15 | 33.3 | 10/47 | 21.3 | 0.489 |
| 6 | 15/16 | 93.8 | 4/30 | 13.3 | <0.001 |
| 7 | 13/20 | 65.0 | 1/31 | 3.2 | <0.001 |
| 8 | 11/24 | 45.8 | 10/37 | 27.0 | 0.171 |
| 9 | 21/28 | 75.0 | 0/20 | 0.0 | <0.001 |
| 10 | 30/34 | 88.2 | 7/18 | 38.9 | 0.001 |
| 11 | 18/21 | 85.7 | 4/17 | 23.5 | <0.001 |
| 12 | 18/22 | 81.8 | 4/36 | 11.1 | <0.001 |
| 13 | 22/31 | 71.0 | 3/14 | 21.4 | 0.003 |
| 14 | 11/24 | 45.8 | 6/18 | 33.3 | 0.530 |
| 15 | 12/20 | 60.0 | 0/21 | 0.0 | <0.001 |
P-values based on chi-square test of Fisher’s exact test excluding missing values.
Screening rates among disadvantaged individuals
Difference in CRC screening rates between intervention and control groups were heightened when examined among disadvantaged individuals only (Table 3). Specifically, among the participants who had an education of high school level or below, annual household income of less than $40,000, were unemployed, could not speak English, and had no health insurance or access to a regular physician, the average rates of screening were consistently over 70% in the intervention group. However, the screening rates in the control group among the disadvantaged individuals were generally lower than the overall screening rates in the control group except for the unemployed participants. The difference in screening rates between the two groups were even higher among those who faced barriers to screening such as not knowing what CRC screening is (69.4% vs. 7.8%), not knowing where to get it (81% vs. 10%), not being able to afford it (70.6% vs. 6.3%), having a language difficulty (80% vs. 11.1%) and feeling healthy (71.4% v. 9.3).
TABLE 3.
CRC Screening Results 12 Months Follow-up Only Among Disadvantaged Individuals
| Variable | Intervention n (%) | Control n (%) | p-value |
|---|---|---|---|
| High school or below (n = 365) | 132/175 (75.4) | 29/190 (15.3) | <0.001 |
| Income < $40,000 (n=516) | 211/287 (73.5) | 37/229 (16.2) | <0.001 |
| Unemployed (n=310) | 117/161 (72.7) | 31/149 (20.8) | <0.001 |
| English- not well/not at all (n = 580) | 207/292 (70.9) | 39/288 (13.5) | <0.001 |
| No health insurance (n = 390) | 154/215 (71.6) | 14/175 (8.0) | <0.001 |
| No regular physician (n=310) | 114/162 (70.4) | 12/148 (8.1) | <0.001 |
| Barriers to screening | |||
| Do not know what it is (n=139) | 43/62 (69.4) | 6/77 (7.8) | <0.001 |
| Do not know where to get it (n=41) | 17/21 (81.0) | 2/20 (10.0) | <0.001 |
| Cannot afford (n=199) | 84/119 (70.6) | 5/80 (6.3) | <0.001 |
| Do not have time (n=89) | 29/49 (59.2) | 2/40 (5.0) | <0.001 |
| Language difficulty (n=24) | 12/15 (80.0) | 1/9 (11.1) | =0.001 |
| Afraid of pain (n=44) | 17/25 (68.0) | 3/19 (15.8) | =0.001 |
| Feel healthy (n=144) | 64/90 (71.1) | 5/54 (9.3) | <0.001 |
Factors associated with FIT and colonoscopy
As shown in Table 4, controlling for intervention effect, several predictors were significantly associated with screening by FIT. Males were twice as likely to have screened by FIT (OR = 2.02, 95% CI 1.17–3.49, p = 0.012). Individuals who have high school education (OR = 2.69, 95% CI 1.44–5.03) and those who had an annual income of $20,000–$40,000 (OR = 2.01, 95% CI 1.02–3.95, p=0.046) were more likely to be screened by FIT than those with college or higher education and those with greater than $40,000 income. Compared to individuals with health insurance, those without health insurance were 2.5 times as likely to screen by FIT (OR = 2.54, 95% CI 1.20–5.37, p=0.017). On the other hand, English inefficiency was significantly (OR = 0.45, 95% CI 0.20–0.99, p=0.031) and having no health insurance was marginally significantly (OR = 0.34, 95% CI 0.10–1.18, p=0.081) associated with decreased odds of screening by colonoscopy/sigmoidoscopy.
TABLE 4.
Factors Associated with FIT and Colono/Sigmoidoscopy at 12 Month Follow-up (n=782)
| Variable | FIT | Colono/Sigmoidoscopy |
|---|---|---|
| OR (95% CI) | OR (95% CI) | |
| Intervention Group | ||
| Intervention | 151.39 (56.97, 402.26)*** | 0.10 (0.04, 0.24)*** |
| Control (Ref) | 1.00 | 1.00 |
| Age | 1.03 (0.99, 1.07) | 0.99 (0.95, 1.04) |
| Years in US | 1.05 (0.71, 1.55) | 0.84 (0.52, 1.36) |
| Gender | ||
| Male | 2.02 (1.17, 3.49)* | 1.06 (0.52, 2.15) |
| Female (Ref) | 1.00 | 1.00 |
| Marital Status | ||
| Married | 0.99 (0.48, 2.04) | 0.64 (0.29, 1.41) |
| Not married | 1.00 | 1.00 |
| Education | ||
| Below high school | 1.50 (0.55, 4.04) | 1.80 (0.61, 5.33) |
| High school graduate | 2.69 (1.44, 5.03)* | 0.92 (0.41, 2.06) |
| Some college or higher (Ref) | 1.00 | 1.00 |
| Annual household income | ||
| Less than $20,000 | 1.80 (0.78, 4.18) | 1.11 (0.38, 3.18) |
| $20,000–$40,000 | 2.01 (1.02, 3.95)* | 1.59 (0.63, 4.00) |
| Greater than $40,000 (Ref) | 1.00 | 1.00 |
| Employment | ||
| Employed | 0.934 (0.454, 1.92) | 0.61 (0.27, 1.38) |
| Unemployed/Retired (Ref) | 1.00 | 1.00 |
| Ability to speak English | ||
| Not at all | 0.587 (0.16, 2.11) | 0.66 (0.16, 2.65) |
| Not well | 0.838 (0.45, 1.56) | 0.45 (0.20, 0.99)* |
| Well/Very well (Ref) | 1.00 | 1.00 |
| Health insurance status | ||
| No | 2.54 (1.20, 5.37)* | 0.34 (0.10, 1.18)† |
| Yes (Ref) | 1.00 | 1.00 |
| Regular physician status | ||
| No | 0.80 (0.40, 1.59) | 0.80 (0.24, 2.71) |
| Yes (Ref) | 1.00 | 1.00 |
Analysis accounts for clustering at the church level
p-value < 0.1
p-value < 0.05
p-value <0.01
p-value <0.001
Regarding the barriers, controlling for the demographic covariates, ‘fear of pain’ was associated with decreased odds of screening by FIT (OR = 0.29, 95% CI 0.09–0.98, p=0.050), while ‘not feeling healthy’ was associated with increased screening by colonoscopy / sigmoidoscopy (OR = 3.47, 95% CI 1.13–10.67, p=0.031).
Screening results and follow-up care
Twenty eight out of 267 (10.2%) who completed FIT in the intervention group were screened positive. All the 28 participants with abnormal FIT results completed diagnostic colonoscopy with patient navigation assistance and physician engagement in referral and facilitation the linkages to follow up care.
DISCUSSION
This study is the first large-scale cluster randomized, multifaceted community-clinical linkage intervention trial to improve CRC screening among underserved and less acculturated Korean Americans. We found that the intervention consisting of culturally appropriate education, provision of FIT, navigation services, and physician engagement was significantly effective in increasing CRC screening, particularly among the hard-to-reach Korean Americans with limited English proficiency. Compared to the previous study that 90% of whom had public or private insurance (Tu et al., 2006), it is noteworthy that the present study achieved high screening rate among 50% participants were uninsured. The finding of the present study demonstrates the efficacy of a multilevel intervention through community-clinical linkage in this population.
Korean Americans have reported to have the lowest CRC screening rates as US general populations with a significant increase in CRC screening (Maxwell and Crespi, 2009; Maxwell et al., 2010; Hwang, 2013; Oh and Jacobsen, 2014). As the contributing factors to the CRC screening disparities in Korean Americans, large proportion of them are foreign-born, lack of health insurance, and have a lower household income, in addition to limited awareness and knowledge about CRC screening guidelines. Indeed, majority of the participants in our study who either never had CRC screening or were overdue for screening were with low income, unemployment, English inefficiency, and no health insurance. Substantial number of those who have never had CRC screening also endorsed ‘cannot afford’, ‘not knowing what it is’, and ‘feeling healthy’ as the main barriers to screening. The successful implementation and outcome of our intervention suggest that enhancing knowledge and access to CRC screening through community-clinical linkage is the effective way to improve CRC screening, particularly among the hard-to-reach underserved Korean American population who experience multiple barriers to screening.
Community participation played a crucial role in raising awareness, facilitating motivation about cancer screening, and reducing logistical challenges among this population when clinical settings have the limitation that they can provide services only to individuals who visit the clinical settings. Offering education and low-cost FIT kits through community settings made it possible to reach the underserved Korean Americans and engage them in screening behaviors. On the other hand, physician engagement compensated the limited ability of community settings in delivery of clinical care and warranted quality services for the participants in need. This community-clinical linkage intervention seemed to be an essential component in enhancing screening behavior for hard-to-reach populations with multiple barriers to screening.
The finding that the intervention was particularly effective in promoting FIT is also consistent with the previous studies suggesting that when offered, FIT is accepted better than colonoscopy among the underserved populations (Inadomi et al., 2012; Singal et al., 2016). We did not design our study to compare FIT versus colonoscopy, but instead incorporated low-cost FIT kit provision into a multifaceted intervention that included education sessions addressing all types of CRC screening and navigation assistance to colonoscopy/sigmoidoscopy appointments, allowing the participants to select the methods of CRC screening. Despite the different options, the majority of the participants in the intervention group selected FIT, confirming the previous studies. Moreover, we found that the difference in screening rates between intervention and control groups were greater among those who were less educated, having less income, unemployed, unable to speak English, with no health insurance or a regular physician, suggesting that our intervention is more beneficial among the disadvantaged individuals. In contrary, relatively better-off participants did not seem to be as receptive to the resources offered by intervention. For instance, the three paired church sites with the lowest screening rates after intervention were attended by the participants with generally higher education, higher income, and greater health care access compared to their counterparts at the other paired church sites where the screening rates were higher. These findings highlight a promising potential of a multifaceted intervention combining FIT provision with CBPR approach for enhancing screening behavior among the most socially and economically disadvantaged members in racial minority communities.
Furthermore, we found that certain demographic characteristics and barriers to screening were associated with different modalities of CRC screening. Multivariate analysis revealed that different modalities of CRC screening seemed to appeal to different subgroups of participants. Controlling for intervention effect, FIT screening behavior was associated with high school educated, lower income, males, and those without health insurance. In contrast, colonoscopy/sigmoidoscopy screening behavior was associated with participants who have health insurance and better English proficiency. Among the barriers, ‘being afraid of pain’ was associated with increased FIT whereas, ‘not feeling healthy’ was associated with increased colonoscopy. These results indicate that the less invasive, low-cost, and more convenient FIT screening test are preferred by disadvantaged groups facing generally more barriers to screening. The more invasive but more sensitive and specific colonoscopy/sigmoidoscopy screening modality seems to be preferred among individuals who typically have health care access and have health concerns. Future work is needed to gain a deeper understanding of the factors that predetermine preference of CRC screening modality among racial minorities.
There are several limitations to this study. First, the present study had a short follow-up period which only studied one-time screening behavior at 12-month follow up. Since FIT screening warrants annual testing to be effective in CRC prevention (Singal et al., 2017), full understanding about screening behavior compliance requires a longer follow-up study to examine sustained adherence over time. In a previous long term comparative outreach study, the rates of screening decreased as low as 28% when participants were followed up for 3 years (Singal et al., 2017) compared to 1-time screening rate of 58.8% (Min, 2002). The authors of the study attributed the lower adherence rates in the FIT outreach group to the suboptimal completion of colonoscopy after a positive FIT result, in addition to the failures of completing subsequent yearly FIT screens after initial negative test results. However, given that 100% of those who had positive FIT test results in the intervention group underwent diagnostic colonoscopy with navigation assistance in our study, compared to 49.3% in the outreach study for 1-time screening (Min, 2002), our study shed the light on the potential impact of the intervention incorporating CBPR approach and navigation service to FIT provision on drawing long-term effect with improved sustained adherence to FIT. Second, despite the randomization procedures, the two groups differed on several demographic variables, including household income, health insurance status, and barriers to screening. However, participants in the control group were more likely to have higher income and health insurance, which are the factors that generally facilitate access to care. Significantly lower screening rates in the control group even with this advantage confirm the true robustness of the intervention used in the present study.
Despite the limitations, our findings support the feasibility and efficacy of a culturally and linguistically appropriate multifaceted community-clinical linkage intervention among the most underserved members in a high-risk racial minority population. The study offers strong evidence that such an intervention approach can be a practical intervention method to effectively target hard-to-reach disadvantaged individuals who are otherwise vulnerable to CRC screening disparities. Future studies will look to investigate deeper into preference of CRC screening modality among Korean Americans and evaluate screening behavior over a longer follow-up period, as well as explore effective strategies to scale up the evidence-based community-clinical linkage intervention for broad dissemination and implementation.
Acknowledgements
This research was supported by Center to Reduce Cancer Health Disparities, National Cancer Institute, National Institutes of Health (NIH) (grant U54 CA153513 to PI: Grace X. Ma, PhD, Community Cancer Health Disparities Center. The authors wish to thank the Asian Community Health Coalition and its member community-based organizations for their collaboration and contributions. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the funding agency, NIH.
Footnotes
Conflict of interest statement
The author has declared that no competing or conflict of interests exist. The funders had no role in study design, writing of the manuscript and decision to publish.
REFERENCES
- American Cancer Society (2014). Colorectal Cancer Facts & Figures 2017–2019 (Atlanta, GA: ). [Google Scholar]
- American Cancer Society (2017). Colorectal Cancer Facts & Figures | Facts About Colon Cancer
- Center for Disease Control and Prevention (2017). Colorectal Cancer Screening Tests
- Chang ET (2003). Korean Americans
- Elmunzer BJ, Singal AG, Sussman JB, Deshpande AR, Sussman DA, Conte ML, Dwamena BA, Rogers MAM, Schoenfeld PS, Inadomi JM, et al. (2015). Comparing the effectiveness of competing tests for reducing colorectal cancer mortality: a network meta-analysis. Gastrointest. Endosc 81, 700–709.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giddings BH, Kwong SL, Parikh-Patel A, Bates JH, and Snipes KP (2012). Going against the tide: increasing incidence of colorectal cancer among Koreans, Filipinos, and South Asians in California, 1988–2007. Cancer Causes Control CCC 23, 691–702. [DOI] [PubMed] [Google Scholar]
- Gupta S, Halm EA, Rockey DC, Hammons M, Koch M, Carter E, Valdez L, Tong L, Ahn C, Kashner M, et al. (2013). Comparative effectiveness of fecal immunochemical test outreach, colonoscopy outreach, and usual care for boosting colorectal cancer screening among the underserved: a randomized clinical trial. JAMA Intern. Med 173, 1725–1732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang H (2013). Colorectal cancer screening among Asian Americans. Asian Pac. J. Cancer Prev. APJCP 14, 4025–4032. [DOI] [PubMed] [Google Scholar]
- Inadomi JM, Vijan S, Janz NK, Fagerlin A, Thomas JP, Lin YV, Muñoz R, Lau C, Somsouk M, El-Nachef N, et al. (2012). Adherence to colorectal cancer screening: a randomized clinical trial of competing strategies. Arch. Intern. Med 172, 575–582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Israel BA, Eng E, Schulz AJ, Parker EA, and Satcher D (2005). Methods in Community-Based Participatory Research for Health (San Francisco, CA: Jossey-Bass; ). [Google Scholar]
- Jo AM, Maxwell AE, Wong WK, and Bastani R (2008). Colorectal Cancer Screening among Underserved Korean Americans in Los Angeles County. J. Immigr. Minor. Health Cent. Minor. Public Health 10, 119–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juon H-S, Han W, Shin H, Kim KB, and Kim MT (2003). Predictors of older Korean Americans’ participation in colorectal cancer screening. J. Cancer Educ. Off. J. Am. Assoc. Cancer Educ 18, 37–42. [DOI] [PubMed] [Google Scholar]
- Krist AH, Shenson D, Woolf SH, Bradley C, Liaw WR, Rothemich SF, Slonim A, Benson W, and Anderson LA (2013). Clinical and Community Delivery Systems for Preventive Care: An Integration Framework. Am. J. Prev. Med 45, 508–516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee HY, and Im H (2013). Colorectal Cancer Screening among Korean American Immigrants: Unraveling the Influence of Culture. J. Health Care Poor Underserved 24, 579–598. [DOI] [PubMed] [Google Scholar]
- Lee S-Y, and Lee EE (2013). Korean Americans’ beliefs about colorectal cancer screening. Asian Nurs. Res 7, 45–52. [DOI] [PubMed] [Google Scholar]
- Lee J, Demissie K, Lu S-E, and Rhoads GG (2007). Cancer incidence among Korean-American immigrants in the United States and native Koreans in South Korea. Cancer Control J. Moffitt Cancer Cent 14, 78–85. [DOI] [PubMed] [Google Scholar]
- Lieberman DA, De Garmo PL, Fleischer DE, Eisen GM, and Helfand M (2000). Patterns of endoscopy use in the United States. Gastroenterology 118, 619–624. [DOI] [PubMed] [Google Scholar]
- Ma GX, Shive S, Tan Y, Gao W, Rhee J, Park M, Kim J, and Toubbeh JI (2009). Community-based colorectal cancer intervention in underserved Korean Americans. Cancer Epidemiol 33, 381–386. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, and Crespi CM (2009). Trends in Colorectal Cancer Screening Utilization among Ethnic Groups in California: Are We Closing the Gap? Cancer Epidemiol. Biomark. Prev. Publ. Am. Assoc. Cancer Res. Cosponsored Am. Soc. Prev. Oncol 18, 752–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell AE, Crespi CM, Antonio CM, and Lu P (2010). Explaining disparities in colorectal cancer screening among five Asian ethnic groups: A population-based study in California. BMC Cancer 10, 214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller BA, Chu KC, Hankey BF, and Ries LAG (2008). Cancer incidence and mortality patterns among specific Asian and Pacific Islander populations in the U.S. Cancer Causes Control 19, 227–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min PG (2002). Mass migration to the United States: Classical and contemporary periods (Walnut Creek, CA: AltaMira Press; ). [Google Scholar]
- Ockene JK, Edgerton EA, Teutsch SM, Marion LN, Miller T, Genevro JL, Loveland-Cherry CJ, Fielding JE, and Briss PA (2007). Integrating Evidence-Based Clinical and Community Strategies to Improve Health. Am. J. Prev. Med 32, 244–252. [DOI] [PubMed] [Google Scholar]
- Oh KM, and Jacobsen KH (2014). Colorectal cancer screening among Korean Americans: a systematic review. J. Community Health 39, 193–200. [DOI] [PubMed] [Google Scholar]
- Persson K (2016). Integrating Clinical Care with Community Health through New Hampshire’s Million Hearts Learning Collaborative: A Population Health Case Report
- Singal AG, Gupta S, Tiro JA, Skinner CS, McCallister K, Sanders JM, Bishop WP, Agrawal D, Mayorga CA, Ahn C, et al. (2016). Outreach invitations for FIT and colonoscopy improve colorectal cancer screening rates: A randomized controlled trial in a safety-net health system. Cancer 122, 456–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singal AG, Gupta S, Skinner CS, Ahn C, Santini NO, Agrawal D, Mayorga CA, Murphy C, Tiro JA, McCallister K, et al. (2017). Effect of Colonoscopy Outreach vs Fecal Immunochemical Test Outreach on Colorectal Cancer Screening Completion: A Randomized Clinical Trial. JAMA 318, 806–815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tu S-P, Taylor V, Yasui Y, Chun A, Yip M-P, Acorda E, Li L, and Bastani R (2006). Promoting culturally appropriate colorectal cancer screening through a health educator. Cancer 107, 959–966. [DOI] [PubMed] [Google Scholar]