ABSTRACT
Background. Improving human papilloma virus (HPV) vaccination coverage in the US will require healthcare providers to recommend the vaccine more effectively. To inform quality improvement efforts, we systematically reviewed studies of dental provider communication about HPV vaccination.
Methods. We searched MEDLINE, CINAHL, ScienceDirect, PsycINFO and JSTOR in August 2018 to identify studies of dental provider knowledge, perceived role and communication about HPV, HPV vaccination and HPV-associated oropharyngeal cancer (HPV-OPC).
Results. We identified 10 qualitative and quantitative studies. Results of the primarily descriptive studies showed that although there were some deficiencies in knowledge about HPV-related outcomes and its effect on the male population, most providers understand HPV as a sexually transmitted infection and know the HPV vaccine is available, yet many are not discussing the HPV-OPC link or recommending vaccination. Providers were less often to recommend HPV vaccination if they were uncomfortable discussing sex, perceived parents as hesitant, or believed patients to be low risk. Studies reported mixed results on providers’ perceived role in expanded HPV vaccination and HPV-OPC education, but indicated support for the role of professional organizations in promoting awareness.
Conclusion. Interventions are needed to help dental providers perceive their role to deliver effective recommendations within the complex communication environment surrounding HPV vaccination and HPV-OPC education.
KEYWORDS: dental professionals, human papilloma virus, human papilloma vaccine, human papilloma virus knowledge, perceived roles, systematic review, oropharyngeal cancer, oropharyngeal cancer protection, oropharyngeal cancer education
Introduction
Human Papillomavirus (HPV) is the most common sexually transmitted infection (STI) in the US.1 It is associated with a subset of cancers of the oral cavity (OC) and oropharynx (OPC).2 Historically, the primary etiological agents for the development of oral cancer were long-term exposure to tobacco and alcohol, alone or in combination. However, high-risk human papilloma virus (HR-HPV) infections are now additionally recognized as an important etiologic agent in the development of these types of cancer.1,3 Current data indicate that HPV is associated with approximately 70% of newly diagnosed OPCs in the US.4,5 HPV-associated OPC is four times more common in males than females, and it occurs earlier in life (40 to 59 years old) than other oral cavity cancers.6,7 It is estimated that the prevalence of HPV-associated OPC will surpass that of HPV-associated cervical cancers by the year 2020.8
The HPV vaccine is a primary prevention method related to HPV and cancer.9 Vaccination against HPV has proven to be effective in protecting against HPV, particularly oncogenic types 16 and 18, which are associated with 80.1% of all HPV-associated cancers and 86.4% of HPV-associated OPC.10,11 Although the vaccine is not currently approved for the prevention of OPC, the Advisory Committee on Immunization Practices (ACIP) of the Centers for Disease Control and Prevention (CDC) recommends routine vaccination of children prior to 15 years of age, preferably between 11 and 12 years of age, that is administered in two doses roughly 6 to 12 months apart. Teens and adults age 15–26 who start the series later are recommended to have three doses to protect against cancer causing HPV infection.12
While the existing vaccines that have been used have a high level of efficacy, the overall vaccination rate of adolescents in the US remains relatively low with 48.6 of adolescents being up-to date (UTD) in 2017.13 UTD is defined as having completed either the 2-dose or 3-dose HPV vaccination regimens.13 More females (53.1%) than males (44.3%) were UTD in 2017.13 Adolescents living below the poverty level had a higher percentage of completion of either regimen (53.7%) than those at or above the poverty level (46.7%), and adolescents living in a non-Metropolitan Statistical Area (MSA) had a lower rate of compliance in comparison to those in a MSA principal city (42.4 % versus 52.4).13
Dental providers are the primary group of healthcare providers who assess the condition of the oral cavity,14 and they should be key players for recommending vaccination against HPV and discussing HPV-OPC. One study indicated that of the 26.0% of children and 24.1% of adults who did not have contact with a general healthcare provider in 2008, a sizeable proportion (34.7% of these children and 23.1% of these adults) did visit a dental practice that year. Taken together, these individuals are estimated to represent 19.5 million people.15 However, the profession has historically limited its role to secondary prevention of HPV-OPC through oral and head and neck examinations.16
Recent American Dental Association (ADA) and American Academy of Pediatric Dentistry (AAPD) guidelines are suggesting an expanded role for dental professionals in HPV vaccination and HPV-OPC protection, stating that they should “strongly and clearly recommend HPV vaccination to all age-eligible patients” and should “educate themselves and their patients about the relationship between HPV and oropharyngeal cancer”.17,18 Given the evolving role of dental providers in recommending HPV vaccination and educating about HPV-OPC, there is a need to assess their current knowledge of HPV and HPV-OPC, their perception of their roles in HPV disease prevention, their willingness to discuss HPV vaccination and HPV-OPC and their actual behaviors in HPV-OPC protection. This study systematically analyzed research studies that have assessed these variables as they relate to dental providers. The goal was to compare and contrast thematic findings to identify direction for future research aimed at integrating dental providers in HPV vaccination discussion and protection of HPV-associated OPC.
Methods
We searched five databases (MEDLINE, CINAHL, ScienceDirect, PsycINFO and JSTOR) in August 2018 to identify studies related to dental providers’ knowledge about HPV and HPV-OPC, their perceptions and behaviors regarding HPV vaccination education and their self-perceived role in HPV and HPV-OPC protection. Additional thematic findings regarding sources of HPV information that emerged from the selected papers are also discussed. We included JSTOR as a database to expand to health communication journals that might include communication about the outcome variables. Searches by database varied slightly, but consisted of a combination of three main domains: HPV-related search terms (e.g. HPV, Papillomavirus), relevant cancer types (e.g. oral, oropharyngeal) and provider type (e.g. dentist, hygienist, dental provider/practitioner/professional, oral health provider/practitioner/professional). Additionally, we searched for possible studies by checking reference lists of papers included in our review.
We reviewed studies for inclusion using a two-step process. First, one author (KW) reviewed paper titles and abstracts to identify relevant studies, and another (RJ) checked the study determinations for eligibility. Second, we conducted full-text reviews of identified studies. Studies for inclusion were decided by two-author agreement based upon meeting the pre-defined criteria of being a study about the assessment of dental providers’ HPV knowledge, HPV-OPC knowledge, perceptions of role in HPV/HPV-OPC protection, and thoughts or actual behavior in discussing HPV vaccination/HPV-OPC with patients.
Once the studies were confirmed by both authors, the data were coded by one author (KW) for a comparison and contrast of themes and findings related to the study variables. The other authors (RJ, JD, MN, SS) also coded one section each of the themed sections. At each step, authors resolved questions and disagreements in coding through discussion.
Inclusion criteria for eligible studies were that the data had to derive from a US sample, report quantitative or qualitative findings related to dental providers’ knowledge of HPV or HPV-OPC or perceptions or actual behaviors of providers about HPV and HPV-OPC roles and protective behaviors. We operationally defined a dental provider to include dentists and dental hygienists. We defined HPV perceptions of and roles for HPV and HPV protection as thought processes about education or discussion about HPV, HPV-OPC or HPV vaccination. Behaviors were similarly defined as conducting an actual HPV, HPV-OPC or HPV vaccination discussion. Excluded studies were those that reported on knowledge of OC/OPC without the HPV context, those that tested the validity of an instrument without findings, interventions and inquiries that did not assess dental provider knowledge or perceptions about roles and discussion (e.g. assessed parents’ or patients’ perceptions of oral providers).
We limited our review to studies with US samples to provide context for the unique practices, policies and dental environments in the US. In comparison to other Organisation for Economic Co-operation and Development (OECD) countries, US oral healthcare services are primarily funded by the private sector.19 Indeed, in 2011, public funding for dental services in the US accounted for only 9.3% of all expenditures on oral health care.20 This makes dental disease in the US costly, and accordingly, there are less dental consultations in the US than many other OECD countries.21 Additionally, dental hygienists, dental assistants, dental laboratory technicians and dentists are recognized in practice in the US.20 Thirty-five US states have policies that allow dental hygienists in community-based settings to provide preventive oral health services without the direct supervision of a dentist.20 These factors influence unique settings for providing HPV vaccination education in the US.
Results
The search yielded 3,585 unduplicated articles, of which 10 met the authors’ eligibility criteria and were included in this review (See Figure 1 for PRISMA diagram). Six studies were quantitative, primarily of survey methodology; 3 were qualitative focus groups and 1 used a mixed methodology design. Five articles assessed both practicing dentists and dental hygienists, 3 practicing dentists only, 1 practicing hygienists only and 1 graduate dental education program directors (See Table 1). Only one study included an intervention. Five studies utilized a theoretical framework to drive study questions.22–26 The majority of articles (6) were interested in outcome variables as they related to general patients, 1 of patients and parents, 1 of female patients, and 2 of adolescents.
Figure 1.
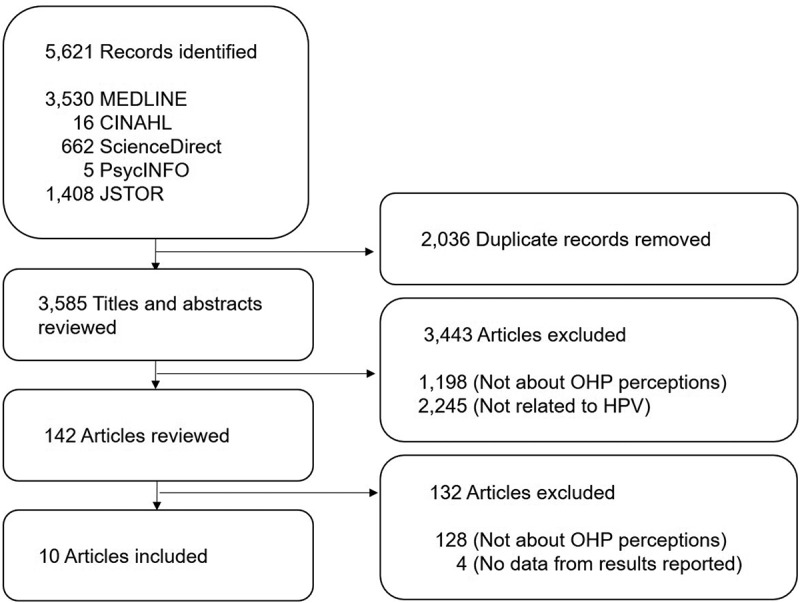
Flow diagram of included and excluded articles.
Table 1.
Characteristics of included studies.
| Author, Year | Study Design | Sex | N | Sample Population |
|---|---|---|---|---|
| Daley, 201125 | Qualitative, focus groups | F, M | 38 | Florida-based dentists (n = 17) and dental hygienists (n = 21) |
| Shepperd, 201328 | Cross-sectional, online survey | F, M | 929 | Florida dentists randomly selected from three regions based on the Agency for Health Care Administration’s regional boundary lines |
| Daley, 201422 | Cross-sectional, online survey | F, M | 210 | Florida-based dentists |
| Hosking, 201727 | Cross-sectional, in-person survey | F, M | 64 | Attendees from the American Academy of Pediatric Dentistry (AAPD) annual meeting for graduate and associate program directors |
| Thompson, 201719 | Qualitative, focus groups | F | 48 | National sample of dental hygienists recruited via email |
| Daley, 201826 | Cross-sectional, in-person survey | F, M | 182 | Dentists (n = 36) and dental hygienists (n = 146) recruited from regional dental conference |
| Kline, 201823 | Mixed methods: qualitative focus groups and quantitative in-person surveys | F, M | 284 | Dentists (n = 70) recruited from regional conference in Southeastern US and dental hygienists recruited from national conference (n = 214) |
| Naleway, 201824 | Cross-sectional, online survey | F, M | 234 | Dentists (n = 79), dental hygienists (n = 62), and dental assistants (n = 93) from the Kaiser Permanente Northwest health system in Oregon and Washington |
| Shukla, 201820 | Cross-sectional, online survey | F, M | 89 | Dentists and dental hygienists that attended HPV educational lectures in New England |
| Vázquez-Otero, 201821 | Qualitative, focus groups | F, M | 33 | Dentists attending a regional conference |
Subscript numerals after author name represent number in reference section for full author information
Knowledge
Studies about dental providers’ HPV-related knowledge were categorized into topics about general HPV, HPV vaccinations, and the link between HPV and OPC. Most studies analyzed specific measures without an overall appraisal of the three HPV knowledge topics. Findings regarding specific measures on the self-reported HPV knowledge topics were varied. For instance, while some studies reported that dental providers’ knowledge about HPV vaccine guidelines was good,27 other studies reported specific HPV vaccine-related topics that were not well understood.22,28
Studies that discussed general HPV knowledge reported that most providers have an understanding of HPV as a sexually transmitted infection22,24,29 with oral sex as a possible mode of transmission.22 They were also able to correctly identify that HPV infection can result in abnormal pap smear findings and may lead to the development of cervical cancer.29 Deficiencies existed regarding knowledge of the incidence and prevalence of HPV and knowledge that HPV affects men as well as women.24,29 Other reported deficiencies in knowledge were associated with HPV outcomes,29 including the curability of HPV,29 HPV symptoms24 and modes of transmission.24 Findings reported that dental hygienists showed good knowledge of how HPV infection occurs and the typical location of OPC lesions related to HPV, but reported a lack of knowledge in describing the appearance of the lesions.22 Among dentists, a mixed response was reported in their ability to correctly identify the different strains of HPV that can lead to OPC.24 Overall HPV knowledge among dentists and dental hygienists was reported to be similar.29
Studies demonstrated that most providers knew there is a vaccine available for HPV.22,24,27,29 Two studies demonstrated gaps in providers’ knowledge about HPV vaccines.22,24 Specific knowledge deficits included a lack of awareness concerning improvements in the current HPV vaccine protection against an increasing number of target HPV strains,24 HPV vaccination recommendations by age group, gender or reimbursement method, names of marketed HPV vaccines24 and the availability of the vaccine for men.22Additionally, some dental providers also incorrectly reported that the HPV vaccine is being removed from the market, that the HPV vaccine has been linked to birth defects and that the vaccine only offers protection against low-risk HPV.24
Studies assessing providers’ knowledge of the HPV-OPC link found that baseline knowledge about the link was low in an earlier study28 but has improved over the years.22,24 In more recent studies, the data indicate most providers have a better understanding of the association between HPV and oral cancer and know that there are increased rates of OPC among young people.22,24,30 However, 53.1% of dental graduate directors still incorrectly believed that the risk of HPV-OPC is higher for females.30
Discussion of HPV and HPV-OPC
Prevailing evidence suggested suboptimal communication by the dental provider about HPV vaccination with their patients.22,24,25,29,30 The lack of discussion between provider and patient was not found to be significantly different when comparing dentists and dental hygienists.29 However, many studies found that providers recognized that they should or want to discuss HPV vaccination with their patients,22,24,26–28,30 yet there was widespread perception that discussing HPV is challenging,22,24–27,30 whether discussing it with older or younger patients.22,24
Studies identified several factors that providers believed challenged discussion of HPV-related information with patients. Discomfort communicating with patients about HPV was linked to the degree of social pressure that could be encountered in the communities the providers served.28,31 Low self-efficacy for communicating effectively was also reported as a challenge.27,31 Some providers questioned their role in vaccine promotion, as they felt they should defer to other providers such as primary care physicians or gynecologists when discussing the sexual health nature of HPV infection.25 In two studies, providers reported variability in the likelihood to counsel different patient populations.22,24 Providers reported greater challenges in discussing information about oral cancer with older adults and young children.22,24 However, groups that were perceived as high risk (e.g. people living with HIV) were identified as easier to counsel because they were perceived to be more invested in obtaining the information.22 Practice-related factors that were considered as barriers to HPV communication and interaction included a concern for patient privacy,22,24,26 leadership dynamics within the practice,22 age of the provider22,30 and time constraints.25–27
Some research attempted to move beyond the challenges presented and proposed strategies for improving ability to provide counseling. The literature suggested that educational interventions could help providers feel more comfortable discussing HPV.23,26,28 Interventions were advised to be tailored to the varying stages of readiness of providers to counsel, as sources of information and barriers were reported to differ among groups according to their stage of readiness.25 Some studies reported that encouraging patients to initiate HPV vaccination discussion would also facilitate conversations with patients about HPV in general.26,28 To initiate discussion, providers underlined the role that professional associations could play in raising public awareness about HPV and its link to oral cancer.28
Relationships between discussion and knowledge
Several studies assessed relationships between providers’ knowledge of HPV-related information and discussion of such with patients. One study found that general HPV knowledge and HPV vaccine-related knowledge did not translate to readiness among dentists to discuss HPV vaccine with their female patients,25 while a study with dental hygienists found that those with lower knowledge levels were less likely to talk to their patients about HPV.29 Higher level of provider knowledge of HPV and HPV vaccination was also related to greater comfort discussing the role of multiple sexual partners with their patients and increased recommendation of the vaccine for their patients’ daughters and sons among pediatric graduate school directors.30 Although not tested for effectiveness, dental providers indicated in two studies that an increase in knowledge about HPV and OPC would enhance their ability to educate their patients on the topic28 and provide better care to their patients.23
Sources of information
Half of the studies discussed the sources of information that surround oral providers’ knowledge and discussion of HPV and HPV-associated OPC.22–26 Two studies analyzed providers’ sources of HPV and HPV-related cancer information,22,24 one analyzed providers’ use of sources to discuss HPV and HPV vaccination with patients,26 and another (an interventional toolkit) assessed the sources providers’ felt most effective for influencing patients’ attitudes and behavior toward HPV vaccination.23 A fifth study assessed the association between sources used by dentists with their stage of readiness for discussing HPV vaccination with female patients.25
Findings indicated that both dentists and dental hygienists’ self-reported using scholarly journals and continuing education courses as primary sources of HPV information.22,24 Dentists also commonly self-reported using colleagues as primary sources of information, while dental hygienists reported using oral health advocacy websites and dental hygiene continuing education courses. Less commonly reported sources of information for dental hygienists were news reports, magazines, social media, blogs, public service announcements, their personal medical providers and peers/colleagues. Dentists less commonly reported using the American Dental Association (ADA), magazines, television, friends and family and dental school.22,24 Dental hygienists who had been in practice longer felt they had not received information about HPV and HPV-related cancers in their educational training, while dentists who were recent graduates (<5 years in practice) noted dental school as a source of information.22,24 In terms of preference of materials to use for discussing the relationship between HPV and oral cancer, focus groups found that dentists and dental hygienists preferred to use written materials. Specific materials included pamphlets, posters, frequently asked questions (FAQ)-sheets, and short videos for the waiting room.26 Office conversation and pediatrician recommendation were the sources dental and dental hygienists’ felt were most influential on patients’ attitudes and opinions toward HPV vaccination (27.9% each), followed by pamphlets and other communications, including social media and family (18.6% each) and audiovisuals (7%).23 Dentists who reported using professional journals, oral health colleagues, and continuing education courses as a source of HPV vaccine-related information were significantly more likely to be in the contemplation stage of readiness to discuss the HPV vaccine with female patients than other stages of the transtheoretical model.25
Role of dental providers in HPV education
Four articles specifically considered the role of dental providers in the prevention of HPV-associated OPC.23,26,28,30 Two studies of a sample of practicing dentists and hygienists (one of focus groups and one of mixed methodology) reported different results.26,28 The first reported mixed response for and against their perceived role in discussing the HPV-OPC link and HPV vaccination, while the second found that the majority strongly agreed or agreed they had a role in HPV-OPC prevention.26,28 Both studies reported that providers felt their professional organizations and dental profession had a clear role in discussing the HPV-OPC link and vaccination with the public. One study provided additional insight into differences in perceptions of each profession’s role in HPV-OPC prevention. Hygienists reported seeing themselves as prevention specialists who educate patients, while dentists reported being more focused on secondary prevention of OPC through screening.26 Out of a sample of 64 pediatric dental graduate directors, 65.6% felt it their role to discuss HPV vaccination, while 74.6% believed it within the scope of pediatric dentistry practice to discuss sexual health and its link to OPC.30 The educational intervention aimed at improving dentists’ and hygienists’ HPV discussion and vaccination recommendation showed that 82.6% felt the intervention was successful in clarifying their role in educating patients about HPV.23
Discussion
Current ADA and AAPD recommendations regarding the dental provider’s role in addressing HPV and HPV-associated oral cancer suggest that they are positioned to evolve into leaders of a full range of HPV protective behaviors.17,18 Given their role, the significance of this review is the discovery of the paucity of studies that have assessed their perceived roles and behaviors in primary preventive techniques or knowledge of HPV and its association with OPC. While the initial article search did uncover many articles related to providers’ knowledge, perceptions and behaviors toward oral cancer prevention, few have been updated to consider the HPV link.
Furthermore, of the ten studies analyzed, only one encompassed an intervention that tested the impact of educational lectures on the provider.23 Additionally, only half of the studies were guided by a theoretical framework.22–26 Results indicate most studies of the topic are in the descriptive, exploratory stage, with half of them unguided by theory. Given the growing emphasis in public health on the importance of evidence-based interventions to improve population health and reduce health inequities, it is notable that theory-driven interventions were lacking.32 To inform how to best support dental providers in counseling their patients, future efforts should encompass the design and testing of interventional communication strategies for improving HPV education so that evaluation research can ultimately assess whether improved communication practices impact HPV vaccine uptake among different patient populations. Studies measuring success of HPV vaccine uptake within the larger literature are still evolving, with some studies showing that high-quality recommendations are strongly linked to vaccine uptake, and others demonstrating low success on actual behaviour.33,34 Interventions and evaluative research on the effects of dental providers’ communication efforts regarding HPV immunization behavior could not only contribute to the literature on OPC prevention, but could also improve our understanding of which features of communication interventions lead to actual change in immunization behavior.
Half of the studies in this review sought to address either the sources of information providers use to discuss HPV-related information with their patients or the sources for which they gain HVP-related knowledge.22–26 Because overall findings indicated that providers’ communication with patients about HPV and the HPV vaccination is suboptimal,22,24,25,29,30 strategies that have been used to effectively guide paediatricians in improving HPV-related discussion such as motivational interviewing 35 are recommended to improve dental providers’ ability to discuss HPV with their patients. Also, as studies in this review indicated that many providers desired passive communication to start the HPV discussion,23,26,28 it is recommended to use print materials suggested in this review and in previous studies with physicians, including fact sheets, parent education websites, HPV disease images and HPV vaccine decision aids.26,36 Implementation of technology such as short videos for waiting rooms, text messages and automated from clinics, along with print materials, could help address the provider-related barriers of discomfort 28,31 and low self-efficacy for communicating.27,31 Developing and testing these communication modes with various subgroups is important, as providers reported variability in their propensity to counsel different patient populations, which can contribute to further health disparities.22,24 In particular, providers reported greater perceived challenges discussing HPV with older and younger populations22,24 and more ease with populations at high-risk (e.g. people living with HIV).22 However, HPV as a risk factor for oral cancer has shaken the traditional understanding of the risk profile that revolved around the male, older, tobacco-smoking patient.28 As more scientific evidence of the link between HPV and oral cancers emerge,37 future research should focus on testing different print and technology channels of communication to build communication capacity among dental providers to discuss HPV vaccination and sexual health-related concerns to meet the needs of different segments of patients while keeping an eye on health equity.
Given that the review uncovered areas of deficiencies in HPV, HPV-OPC and HPV vaccination knowledge among providers, the same fact sheets and Q&A sheets that lay out HPV information for patients might also improve provider knowledge, and thus their self-efficacy for educating their patients. Most notable in this review was the lack of knowledge that HPV affects men and that the HPV vaccine is recommended for men,22,24,29 which is pertinent, as the incidence of HPV-related OPC is increasing among men.8 Deficiencies were also reported regarding knowledge about HPV outcomes, such as its curability, symptoms and transmission.22,24,29 Providers also demonstrated a gap in knowledge about HPV vaccine recommendations (for age, sex and insurance coverage) and the HPV types covered by the vaccine.24 While most providers knew that HPV is linked to OPC, there is still room for improving such knowledge, especially as it impacts young men.22,24,30 The importance of improving provider knowledge for HPV discussion was indicated in the study with graduate directors that showed that a higher level of knowledge of HPV and HPV vaccination was related to greater comfort discussing the role of multiple sexual partners as a risk factor for HPV and OPC and greater likelihood of encouraging parents to vaccinate their daughters.30
The literature has also discussed other mechanisms in addition to communication for improving provider HPV knowledge.25 Some of the approaches recommended in the literature are the integration of HPV-related information into dental hygiene curricula and the inclusion of HPV topics in national as well as state and regional boards.22 Inclusion of HPV-related information into curricula is suggested by evidence in this review that indicates providers who were out of school longer were less likely to report their school/education as a source of HPV information.22,24 As findings from this review indicated that both dentists and dental hygienists self-reported using scholarly journals and continuing education courses as primary sources of HPV information,22,24 incorporating HPV topics in professional meetings and lectures for continuing education requirements should also be considered. In addition to didactics, skill building workshops that allow hands-on training to improve OPC screening techniques can play an essential role in furthering the goal of creating a skilled dental provider workforce in HPV screening and vaccination.28
Only four studies specifically inquired of dental providers’ perception of their role in HPV-associated OPC protective efforts,23,26,28,30 and two of the studies reported mixed feelings that providers have a role in HPV prevention efforts, while more firmly believing in the professions’ role in encouraging awareness.26,28 Given the current ADA and AAPD policies recommending that dental providers expand their role to include HPV vaccination, assessment of their acceptance and implementation is necessary. Although there is no direct benefit linking the HPV vaccine to HPV-OPC,38 their policies encouraging oral healthcare providers to educate patients, parents, and guardians on the serious health consequences of OPC and its relationship to HPV and counsel regarding the HPV vaccine,17,18 are in response to the recognition that HPV vaccination is a way to help prevent infection of the types of HPV associated with oropharyngeal cancer.38 One study in the review indicated that dental hygienists might be the ready champion for promoting HPV primary prevention efforts in the dental setting, as they identified themselves as “prevention specialists” who have an important role in educating patients, and often have more patient contact time than dentists.22
This systematic review has its limitations. Limitations include the review’s reliance on studies that primarily use cross-sectional designs, convenience samples, and self-reported measures of providers’ knowledge and perceptions of HPV and HPV-protective discussions. We also recognize the small number of articles from which to draw conclusions. Last, although our primary focus was on what dental providers know and perceive about their role in HPV-OPC protection, we recognize that related literatures regarding others’ perceptions, namely patients and physicians, are also relevant to a more complete understanding of the factors associated with integrating dental providers more expansively into their roles in HPV vaccination and HPV-OPC protection. The emphasis on providers’ belief in the role of professional organizations for improving HPV-OPC and HPV vaccination awareness reported in the review can also be leveraged for improving overall knowledge.23
Conclusion
To our knowledge, this is the first systematic review examining the studies (or lack thereof) of dental providers’ knowledge, behavior and perceptions toward their role in HPV vaccination and HPV-OPC education. While there is a paucity of studies on the subject, patterns of themes emerged that indicate a hesitancy to discuss HPV and HPV vaccination with patients and a need for more education about HPV and HPV-OPC, especially among older providers, with passive communication materials needed to facilitate discussion. Theory driven research is needed to continue descriptive studies, with development of messages and strategic interventions to improve and evaluate dental providers’ knowledge, and HPV-protective perceptions and behaviors an ultimate goal.
Disclosure of potential conflicts of interest
No potential conflict of interest was reported by the authors.
References
- 1.Centers for Disease Control and Prevention HPV and oropharyngeal cancer- fact sheet-old. Atlanta (GA): United States Department of Health and Human Services; 2017. Retrieved from https://www.cdc.gov/std/hpv/stdfact-hpvandoropharyngealcancerOLD.htm. [Google Scholar]
- 2.Rutkoski H, Fowler B, Mooney R, Pappas L, Dixon BL, Pinzon LM, Winkler J, Kepka D.. Pilot test of survey to assess dental and dental hygiene student human papillomavirus-related oropharyngeal cancer knowledge, perceptions, and clinical practices. J Cancer Educ. 2017;33(4):907–914. PMID: 28091963. doi: 10.1007/s13187-017-1165-z. [DOI] [PubMed] [Google Scholar]
- 3.Mashberg A, Boffetta P, Winkelman R, Garfinkel L. Tobacco smoking, alcohol drinking, and cancer of the oral cavity and oropharynx among U.S. veterans. Cancer. 1993;72(4):1369–1375. PMID: 8339227. doi:. [DOI] [PubMed] [Google Scholar]
- 4.Stenmark MH, Shumway D, Guo C, Vainshtein J, Mierzwa M, Jagsi R, Griggs JJ, Banerjee M. Influence of human papillomavirus on the clinical presentation of oropharyngeal carcinoma in the United States. Laryngoscope. 2017;127(10):2270–2278. PMID: 28304083. doi: 10.1002/lary.26566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saraiya M, Unger ER, Thompson TD, Lynch CF, Hernandez BY, Lyu CW, Steinau M, Watson M, Wilkinson EJ, Hopenhayn C, et al. US assessment of HPV types in cancers: implications for current and 9-valent HPV vaccines. J Natl Cancer Inst. 2015;107(6):djv086 PMID: 25925419. doi: 10.1093/jnci/djv086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chaturvedi AK. Epidemiology and clinical aspects of HPV in head and neck cancers. Head Neck Pathol. 2012;6(1):S16–S24. PMID: 22782220. doi: 10.1007/s12105-012-0377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shiboski CH, Schmidt BL, Jordan RCK. Tongue and tonsil carcinoma: increasing trends in the U.S. population ages 20-44 years. Cancer. 2005;103(9):1843–1849. PMID: 15772957. doi: 10.1002/cncr.20998. [DOI] [PubMed] [Google Scholar]
- 8.Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294–4301. PMID: 21969503. doi: 10.1200/jco.2011.36.4596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Arrossi S, Temin S, Garland S, Eckert LO, Bhatla N, Castellsagué X, Alkaff SE, Felder T, Hammouda D, Konno R, et al. Primary prevention of cervical cancer: american society of clinical oncology resource-stratified guideline. J Glob Oncol. 2017;3(5):611–634. PMID: 29094100. doi: 10.1200/JGO.2016.008151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Parkin DM, Bray F. The burden of HPV-related cancers. Vaccine. 2006;24(suppl3):S11–S25. PMID: 16949997. doi: 10.1016/j.vaccine.2006.05.111. [DOI] [PubMed] [Google Scholar]
- 11.Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC, Thompson TD, Razzaghi H, Saraiya M. Human papillomavirus-associated cancers – United States, 2008-2012. MMWR Morb Mortal Wkly Rep. 2016; 65(26):661–666;PMID: 27387669 2016;():. . doi: 10.15585/mmwr.mm6526a1. [DOI] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention CDC recommends only two HPV shots for younger adolescents. Atlanta (GA): United States Department of Health and Human Services; 2016. Retrieved from https://www.cdc.gov/media/releases/2016/p1020-HPV-shots.html. [Google Scholar]
- 13.Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Mbaeyi SA, Fredua B, Stokley S. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 Years - United States. MMWR Morb Mortal Wkly Rep. 2018;67(33):909–917. PMID: 30138305. doi: 10.15585/mmwr.mm6733a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Horowitz AM, Siriphant P, Sheikh A, Child WL. Perspectives of Maryland dentists on oral cancer. J Am Dent Assoc. 2001;132(1):65–72. PMID: 11194401. doi: 10.14219/jada.archive.2001.0027. [DOI] [PubMed] [Google Scholar]
- 15.Strauss SM, Alfano MC, Shelley D, Fulmer T. Identifying unaddressed systemic health conditions at dental visits: patients who visited dental practices but not general health care providers in 2008. Am J Public Health. 2012;102(2):253–255. PMID: 22390440. doi: 10.2105/AJPH.2011.300420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.American Academy of Pediatric Dentistry Policy on human papilloma virus vaccinations. Pediatr Dent. 2017;39(6):81–82. PMID: 29179328. [PubMed] [Google Scholar]
- 17.American Dental Association Cancer prevention through HPV vaccination: An action guide for dental health care providers. Chicago (IL): National HPV Vaccination Roundtable; 2018. Retrieved from https://ebd.ada.org/~/media/ebd/files/dental-action-guide-web_ada.pdf?la=en. [Google Scholar]
- 18.American Dental Association Statement on human papillomavirus and squamous cell cancers of the oropharynx. Chicago (IL): American Dental Association ADA Council on Scientific Affairs; 2012. Retrieved from http://www.ada.org/1749.aspx. [Google Scholar]
- 19.Dental health among children. In Health at a Glance 2009 OECD Indicators. Paris, France: OECD Publishing; 2009. p. 34–35. doi: 10.1787/health_glance-2009-12-en. [DOI] [Google Scholar]
- 20.Garbin Neumann D, Quiononez C.. A comparative analysis of oral health care systems in the United States, United Kingdom, France, Canada, and Brazil. NCOHR Working Papers Series. 2014;1(2):1–18. Retrieved from http://ncohr-rcrsb.ca/knowledge-sharing/working-paper-series/content/garbinneumann.pdf. [Google Scholar]
- 21.Inequalities in dentist consultations. In Health at a Glance 2009 OECD Indicators. Paris, France: OECD Publishing;2013, p. 152–153. doi: 10.1787/health_glance-2009-65-en. [DOI] [Google Scholar]
- 22.EL Thompson, EM Daley, CA Vamos, AM Horowitz, FA Catalanotto, RD DeBate, LK Merrell, SB Griner, Vazquez-Otero C, NS Kline. Health literacy approaches to improving communication between dental hygienists and patients for HPV-related oral cancer prevention. J Dent Hyg. 2017;91(4):37–45. PMID: 29118082. [PubMed] [Google Scholar]
- 23.Shukla A, Nyambose J, Vanucci R, LB Johnson, Welch K, Lind E, Villa A. Evaluating and effectiveness of human papillomavirus educational intervention among oral health professionals. J Cancer Educ. 2018;PMID: 30006799; doi: 10.1007/s13187-018-1391-z [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 24.Vázquez-Otero C, CA Vamos, EL Thompson, LK Merrell, SB Griner, NS Kline, FA Catalanotto, AR Giuliano, EM Daley. Assessing dentists’ human papillomavirus-related health literacy for oropharyngeal cancer prevention. J Am Dent Assoc. 2018;149(1):9–17. PMID: 29031503. doi: 10.1016/j.adaj.2017.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Daley E, Dodd V, DeBate R, Vamos C, Wheldon C, Kline N, Smith S, Chandler R, Dyer K, Helmy H, et al. Prevention of HPV-related oral cancer: assessing dentists’ readiness. Public Health. 2014;128(3):231–238. PMID: 24602857. doi: 10.1016/j.puhe.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kline N, Vamos C, Thompson E, Catalanotto F, Petrila J, DeBate R, Griner S, Vázquez-Otero C, Merrell L, Daley E. Are dental providers the next line of HPV-related prevention? Providers’ perceived role and needs. Papillomavirus Res. 2018;5:104–108. PMID: 29524676. doi: 10.1016/j.pvr.2018.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.AL Naleway, ML Henninger, LA Waiwaiole, DM Mosen, Leo, DJ Pihlstrom. Dental provider practices and perceptions regarding adolescent vaccination. J Public Health Dent. 2018;78(2):159–164. PMID: 29114884. doi: 10.1111/jphd.12256. [DOI] [PubMed] [Google Scholar]
- 28.Daley E, DeBate R, Dodd V, Dyer K, Fuhrmann H, Helmy H, SA Smith. Exploring awareness, attitudes, and perceived role among oral health providers regarding HPV‐related oral cancers. J Public Health Dent. 2011;71(2):136–142. PMID: 21774137. doi: 10.1111/j.1752-7325.2011.00212.x. [DOI] [PubMed] [Google Scholar]
- 29.EM Daley, EL Thompson, CA Vamos, SB Griner, Vazquez-Otero C, AL Best, NS Kline, LK Merrell. HPV-related knowledge among dentists and dental hygienists. J Cancer Educ. 2018;33(4):901–906. PMID: 28039675. doi: 10.1007/s13187-016-1156-5. [DOI] [PubMed] [Google Scholar]
- 30.YP Hosking, Cappelli D, Donly K, Redding S. HPV vaccination and the role of the pediatric dentist: survey of graduate program directors. Pediatr Dent. 2017;39(5):383–389. PMID: 29070161. [PubMed] [Google Scholar]
- 31.JA Shepperd, JL Howell, Catalanotto F, VJ Dodd, HL Logan. The decision to counsel adolescents about HPV. Am J Health Behav. 2013;37(6):755–762. PMID: 24001624. doi: 10.5993/AJHB.37.6.4. [DOI] [PubMed] [Google Scholar]
- 32.MacDonald M, Pauly B, Wong G, Schick-Makaroff K, van Roode T, HW Strosher, Kothari A, Valaitis R, Manson H, O’Briain W, et al. Supporting successful implementation of public health interventions: protocol for a realist synthesis. Syst Rev. 2016;5(54):PMID: 27055820. doi: 10.1186/s13643-016-0229-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.MB Gilkey, WA Calo, JL Moss, PD Shah, MW Marciniak, NT Brewer. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34(9):1187–1192. PMID: 26812078. doi: 10.1016/j.vaccine.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.LY Fu, LA Bonhomme, SC Cooper, JG Joseph, GD Zimet. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014;32(17):1901–1920. PMID: 24530401. doi: 10.1016/j.vaccine.2014.01.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.JE Reno, ST O’Leary, Pyrzanowski J, Lockhart S, Thomas J, AF Dempsey. Evaluation of the implementation of a multi-component intervention to improve healthcare provider communication about HPV vaccination. Acad Pediatr. 2018;PMID: 30107236; doi: 10.1016/j.acap.2018.08.004 [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 36.Slomski A. Better communication can improve HPV vaccine rates. JAMA. 2018;319(16):1649 PMID: 29710159. doi: 10.1001/jama.2018.4013. [DOI] [PubMed] [Google Scholar]
- 37.NC Chaitanya, NS Allam, Gandhi Babu DB, Waghray S, RK Badam, Lavanya R. Systematic meta-analysis on association of human papilloma virus and oral cancer. J Cancer Res Ther. 2016;12(2):969–974. PMID: 27461683. doi: 10.4103/0973-1482.179098. [DOI] [PubMed] [Google Scholar]
- 38.AR Kreimer. Prospects for prevention of HPV-driven oropharynx cancer. Oral Oncol. 2014;50(6):555–559. PMID: 23876626. doi: 10.1016/j.oraloncology.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]


