ABSTRACT
HPV is involved in cervical, anal, penile, vulvar and oropharyngeal cancers, as well as genital warts. It is important to investigate knowledge and attitudes among university students, considering in this age a shift in healthcare decision-making from parents to students themselves. The aim of this study was to estimate knowledge and perception of HPV in terms of potential shame for HPV-related conditions, trust in vaccine efficacy and worry for potential side effects.
The study involved students (18–25 years old) from the Universities of Padua and Verona, Italy. Socio-demographic and behavioural characteristics were collected with a questionnaire (n = 9988).
Female gender and older age were positively associated with higher knowledge. The adjusted logistic regression showed an association between the set of perceptions investigated and the vaccination status, while a direct connection with knowledge was not found. However, another adjusted linear regression showed that a good set of perceptions could be partially explained by a high level of knowledge. Perceptions seem to fill an intermediate position between the knowledge and the decision to get vaccinated. The potential shame deriving from asking for HPV-vaccination was not identified as a relevant barrier. Having received information from healthcare workers, family and school showed to be positively associated with the adhesion to the vaccination policy.
This study identifies university students as a possible target for HPV vaccination and pinpoints specific areas that might be targeted as first to encourage vaccine uptake. Primary prevention together with screening programmes remains essential in further reducing the burden of HPV-related diseases.
KEYWORDS: HPV, risk perception, vaccine, knowledge
Introduction
Human Papillomavirus (HPV) infection is the most common sexually transmitted infection, responsible for a large number of pathologies in both women and men. Over 200 HPV types have been identified and classified in high risk (HR) and low risk (LR) types on the basis of their potential to induce cancerous lesions.1 Globally, the prevalence of HPV infection in women has been estimated around 11.7%, with the highest rates in Sub-Saharan Africa (24.0%).2
About 70–90% of HPV infections are asymptomatic and resolve spontaneously within 1–2 years, but persistent infections with HR types may progress to invasive cancer. HPV-16 and HPV-18 are responsible for more than 70% of all cases of cervical, vaginal and anal cancers worldwide and they account for about 30–40% of cancers of the vulva, penis and oropharynx.3 Nevertheless, non-oncogenic HPV types (mostly types 6 and 11) are extensively involved in the aetiology of genital warts which, however, massively impact on the quality of life.4
According with the World Health Organization (WHO), vaccination against HPV is an essential strategy in preventing cervical cancer.5 Globally, as of 2017, 71 countries had introduced HPV vaccination for girls, and 11 countries also for boys.6 In Italy, since 2007, HPV vaccination has been offered free of charge to all girls in the age of 12 and in 6 out of 21 Italian regions also to older age group and HIV-positive individuals between 2007 and 2010. Since 2015 some regions started to offer HPV vaccine also to boys in the age of 12 and in 2018 a gender-neutral strategy was implemented in all Italian regions.7 Moreover, HPV immunization also for unvaccinated females aged more than 12 (in particular to 25-years-old women that undergo cervical screening for the first time) and MSM is recommended.8
However, despite the national target for vaccine coverage was set at 95% within 5 years from the start of vaccine implementation in girls,9 at the end of 2017 coverage rate stood at around 69% in the first vaccinated cohort (girls born in 1997).10 As of 2011, coverage rates achieved by the catch-up programmes ranged between 44.3% and 80.0%.11
Suboptimal vaccination coverage can be partly explained by factors associated with Italian parents’ hesitancy, including concerns about the vaccine efficacy or possible serious side effects.12 Furthermore, Roberts et al. found that the proportion of individuals with an incomplete immunisation status was higher in adolescents whose parents acknowledged to be unable to openly discuss their concerns about vaccines with healthcare professionals.13
In this context, it is important to investigate knowledge and perception towards HPV and vaccination among university students, also considering that in this period of their life there may be a shift in health care decision-making from parents and guardians to the students themselves.14 Knowledge gaps and misrepresented perceptions on HPV and HPV vaccination were detected not only among college students from low-income countries, such as Pakistan,15 Malaysia16 and Nigeria,17 but also from high-income countries, including the US,18 Canada19 and Germany.20
The aim of this study was to estimate the students’ knowledge and perception about HPV infection in terms of potential shame for HPV-related conditions, trust in vaccine efficacy and worry for potential side effects of the vaccine 8 years after the implementation of the national vaccination programme in Italy.
Results
Overall, 9988 students agreed to participate in the study by completing the questionnaire (Figure 1). Socio-demographic and behavioural characteristics are shown in Table 1. Mean age of participants was 20.5 years (SD = 1.81), median age 20.0 years, ranging from 19 to 25. Just over one quarter of students sampled were HPV-vaccinated (n = 2552/9545a; 26.7%); of these, only 81 (3.2%) were men. This included 88% who had received all three doses, 9% who received one or two doses and 3% who booked an appointment to receive the first dose.
Figure 1.
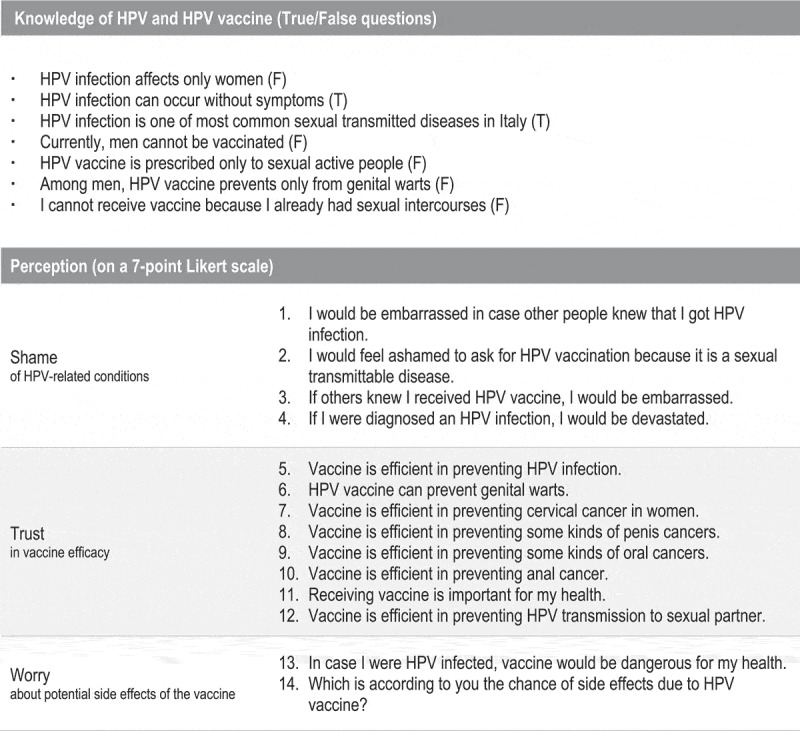
Sentences assessing students’ knowledge and perception of HPV and vaccine-related conditions. T = true; F = false.
Table 1.
Knowledge and perception of HPV-related and vaccine-related conditions by socio-demographic and behavioural characteristics of the study population.
| Level of perceptions |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Level of knowledge |
Shame |
Trust |
Fear |
||||||||
| n | % | Mean | ANOVA | Mean | ANOVA | Mean | ANOVA | Mean | ANOVA | ||
| Gender | F | 6019 | 60.3 | 5.86 | p < .001 | 3.28 | p < .001 | 4.89 | p < .001 | 3.34 | p = .035 |
| M | 3969 | 39.7 | 5.67 | 3.56 | 4.81 | 3.40 | |||||
| Age | 18–19 y | 3816 | 38.2 | 5.77 | p < .001 | 3.46 | p < .001 | 4.87 | p < .001 | 3.40 | p < .001 |
| 20–21 y | 3196 | 32.0 | 5.74 | 3.41 | 4.83 | 3.41 | |||||
| 22–23 y | 2211 | 22.1 | 5.82 | 3.31 | 4.84 | 3.28 | |||||
| 24–25 y | 765 | 7.7 | 5.96 | 3.21 | 4.97 | 3.25 | |||||
| Degree course attended (grouped by main areas) | 1 Health-care professions | 2239 | 23.1 | 5.84 | p < .001 | 3.36 | p < .001 | 4.89 | p < .001 | 3.29 | p < .001 |
| 2 Sciences | 1899 | 19.6 | 5.71 | 3.46 | 4.82 | 3.41 | |||||
| 3 Humanities | 1575 | 16.2 | 5.78 | 3.38 | 4.80 | 3.48 | |||||
| 4 Engineering | 1472 | 15.2 | 5.62 | 3.60 | 4.71 | 3.55 | |||||
| 5 Law and Economics | 607 | 6.3 | 5.69 | 3.47 | 4.83 | 3.46 | |||||
| 6 Psychology | 932 | 9.6 | 5.84 | 3.28 | 4.81 | 3.45 | |||||
| 7 Medicine and Dentistry | 978 | 10.1 | 6.10 | 3.07 | 5.23 | 2.84 | |||||
| N. of sexual partners within last 24 months | 0 | 767 | 9.9 | 5.74 | p < .001 | 3.52 | p < .001 | 4.80 | p < .001 | 3.38 | p = .004 |
| 1 | 4593 | 59.4 | 5.84 | 3.33 | 4.90 | 3.34 | |||||
| 2 | 1212 | 15.7 | 5.84 | 3.36 | 4.91 | 3.30 | |||||
| 3+ | 1161 | 15.0 | 5.78 | 3.35 | 4.86 | 3.36 | |||||
| Age at first intercourse | 14 y or less | 419 | 5.5 | 5.82 | p < .001 | 3.20 | p < .001 | 4.85 | p = .001 | 3.41 | p = .033 |
| 15–16 y | 2516 | 33.0 | 5.83 | 3.28 | 4.86 | 3.35 | |||||
| 17–18 y | 3498 | 45.9 | 5.79 | 3.38 | 4.88 | 3.34 | |||||
| 19 y or more | 1196 | 15.7 | 5.84 | 3.41 | 4.89 | 3.31 | |||||
| Sexual orientation | Heterosexual | 9329 | 94.7 | 5.79 | p = .007 | 3.39 | p = .001 | 4.86 | p = .193 | 3.36 | p = .342 |
| Homosexual | 177 | 1.8 | 5.83 | 3.45 | 4.81 | 3.28 | |||||
| Other | 341 | 3.5 | 5.87 | 3.20 | 4.83 | 3.37 | |||||
| Use of birth pill | Yes | 1786 | 31.0 | 5.93 | p < .001 | 3.16 | p < .001 | 4.95 | p < .001 | 3.29 | p = .008 |
| No | 3983 | 69.0 | 5.85 | 3.32 | 4.87 | 3.36 | |||||
| Smoking habit | Non-smoker | 6927 | 71.3 | 5.80 | p = .001 | 3.42 | p < .001 | 4.88 | p < .001 | 3.35 | p = .095 |
| Current or ex-smoker | 2785 | 28.7 | 5.76 | 3.30 | 4.81 | 3.41 | |||||
| Personal or close people’s experience of genital warts | Yes | 840 | 8.5 | 5.88 | p < .001 | 3.25 | p < .001 | 4.89 | p = .029 | 3.32 | p = .127 |
| No | 9061 | 91.5 | 5.78 | 3.40 | 4.86 | 3.37 | |||||
| HPV vaccination status | Vaccinated | 2552 | 26.7 | 5.91 | p < .001 | 3.15 | p < .001 | 5.01 | p < .001 | 3.09 | p < .001 |
| Non-vaccinated | 6993 | 73.3 | 5.77 | 3.47 | 4.81 | 3.46 | |||||
Note: numbers may not add up to the total number due to missing data from questionnaire
As regards knowledge of HPV and HPV-vaccine, 65% of participants correctly answered to 6 or more questions out of 7 and 90% of the sample correctly answered to 5 or more. In Figure 2, mean values of agreement to proposed sentences are shown one at a time, according to the Likert scale adopted.
Figure 2.
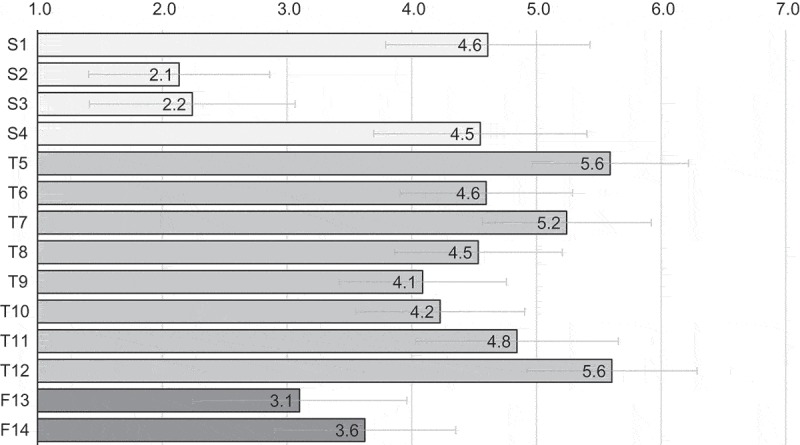
Perception. Level of agreement with each proposed item (see Figure 1 for the description of items). Mean value for each item is reported at the end of the bar. S = shame; T = trust; F = fear.
An adjusted linear regression to assess the effect of socio-demographic and behavioural characteristics on the levels of knowledge and different types perceptions regarding the emotions of shame, trust and fear towards HPV infection and vaccination was conducted. Findings are shown in Table 2. Overall, significant associations of knowledge with female gender (B: 0.14; 95%CI: 0.09 to 0.20), age (B: 0.03; 95%CI: 0.02 to 0.05), lack of a sexual partner (B: −0.13; 95%CI: −0.25 to −0.05), smoking habit (B: −0.05; 95%CI: −0.10 to −0.00), personal or close people’s experience of genital warts (B: 0.11; 95%CI: 0.03 to 0.20) and vaccination status (B: 0.19; 95%CI: 0.06 to 0.18) were found.
Table 2.
Effect of the socio-demographic and behavioural characteristics on the level of knowledge and perception of HPV-related and vaccine-related conditions.
| Level of perceptions |
|||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Level of knowledge |
Shame |
Trust |
Fear |
||||||||||
| 95% CI |
95% CI |
95% CI |
95% CI |
||||||||||
| reference | Beta-coefficient | Lower | Upper | Beta-coefficient | Lower | Upper | Beta-coefficient | Lower | Upper | Beta-coefficient | Lower | Upper | |
| Gender | (male) | ||||||||||||
| Female | .14 | .09 | .20 | −.16 | −.22 | −.10 | −.03 | −.08 | .01 | .12 | .05 | .20 | |
| Age | .03 | .02 | .05 | −.06 | −.07 | −.04 | .02 | .00 | .03 | −.06 | −.08 | −.04 | |
| N. of sexual partners within last 24 months | (1 or 2 partners) | ||||||||||||
| 0 | −.13 | −.25 | −.05 | .05 | −.08 | .18 | −.12 | −.23 | −.02 | .02 | −.14 | .19 | |
| 3 or more | −.03 | −.10 | .03 | .02 | −.05 | .09 | −.00 | −.06 | −05 | .05 | −.04 | .14 | |
| Age at first intercourse | (15–18 y) | ||||||||||||
| 14 y or less | −.00 | −.10 | .10 | −.11 | −.21 | .03 | −.04 | −.13 | .05 | .05 | −.09 | .19 | |
| 19 y or more | −.00 | −.07 | .07 | .11 | .03 | .17 | .00 | −.05 | .06 | .00 | −.08 | .10 | |
| Sexual orientation | (heterosexual) | ||||||||||||
| Other | .05 | −.04 | .15 | −.10 | −.21 | .05 | −.06 | −.15 | .02 | −.02 | −.16 | .11 | |
| Smoking habit | (non-smoker) | ||||||||||||
| Current or ex-smoker | −.05 | −.10 | −.00 | −.08 | −.14 | −.03 | −.06 | −.10 | −.01 | .06 | −.01 | .13 | |
| Personal or close people’s experience of genital warts | (no) | ||||||||||||
| Yes | .11 | .03 | .20 | −.07 | −.15 | .02 | .03 | −.04 | .10 | −.03 | −.14 | .08 | |
| HPV vaccination status | (non-vaccinated) | ||||||||||||
| Vaccinated | .19 | .06 | .18 | −.29 | −.35 | −.22 | .22 | .17 | .28 | −.50 | −.58 | −.42 | |
Adjusted linear regression.
CI = confidence interval.
The aim of the logistic regression analysis was to identify a significant association between knowledge/perceptions and the vaccination status, while controlling for age, gender, age at first intercourse, number of sexual partners smoking habit, sexual orientation, personal or close people’s experience of genital warts. The effect of these potential confounders is not shown in the table. Out of the whole study population, 6325 (63.3%) participants were included. Approximately 81% of vaccination statuses were predicted by the model described. The level of shame (OR: 0.77; 95%CI: 0.72 to 0.83), trust (OR: 1.40; 95%CI: 1.29 to 1.52) and fear (OR: 0.77; 95%CI: 0.73 to 0.81) significantly predicted the outcome, while no significant association was found with the level of knowledge (OR: 1.03; 95%CI: 0.96 to 1.19).
Moreover, an adjusted linear regression was performed to predict each perception investigated (shame, trust and fear) based on the level of knowledge while controlling for age, gender, age at first intercourse, number of sexual partners smoking habit, sexual orientation, personal or close people’s experience of genital warts and degree course attended (results are not reported in the table). Out of 9988, 36% of cases were excluded from these analysis because of a missing value in any variable investigated. There was a significant positive relationship between knowledge and trust (B: 0.12; 95%CI: 0.10 to 0.15), while a negative relationship was detected both for fear (B: −0.13; 95%CI: −0.16 to −0.10) and shame (B: −0.10; 95%CI: −0.12 to −0.07).
Finally, Table 3 shows the association between the type of source of information on HPV and its vaccination used by the students and their mean levels of knowledge and perceptions.
Table 3.
Knowledge and perception of HPV-related and vaccine-related conditions by source of information.
| Perception |
|||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Knowledge |
Shame |
Trust |
Fear |
||||||||||||
| n | % | Mean | Difference between means | ANOVA | Mean | Difference between means | ANOVA | Mean | Difference between means | ANOVA | Mean | Difference between means | ANOVA | ||
| Healthcare workers | No | 6582 | 65.9 | 5.71 | 0.23 | p < .001 | 3.52 | −0.38 | p < .001 | 4.79 | 0.20 | p < .001 | 3.46 | −0.27 | p < .001 |
| Yes | 3406 | 34.1 | 5.94 | 3.14 | 4.99 | 3.19 | |||||||||
| Friend | No | 9061 | 90.7 | 5.78 | 0.07 | p = .029 | 3.41 | −0.23 | p < .001 | 4.85 | 0.06 | p = .031 | 3.37 | −0.06 | p = .154 |
| Yes | 927 | 9.3 | 5.85 | 3.18 | 4.91 | 3.31 | |||||||||
| Family | No | 7817 | 78.3 | 5.76 | 0.13 | p < .001 | 3.45 | −0.28 | p < .001 | 4.83 | 0.13 | p < .001 | 3.40 | −0.17 | p < .001 |
| Yes | 2171 | 21.7 | 5.89 | 3.17 | 4.96 | 3.23 | |||||||||
| TV | No | 8354 | 83.6 | 5.78 | 0.05 | p = .024 | 3.39 | 0.01 | p = .733 | 4.85 | 0.05 | p = .015 | 3.36 | 0.02 | p = .649 |
| Yes | 1634 | 16.4 | 5.83 | 3.40 | 4.90 | 3.38 | |||||||||
| Internet | No | 8813 | 88.2 | 5.76 | 0.20 | p < .001 | 3.40 | −0.09 | p = .009 | 4.85 | 0.08 | p = .002 | 3.38 | −0.14 | p < .001 |
| Yes | 1175 | 11.8 | 5.96 | 3.31 | 4.93 | 3.24 | |||||||||
| Newspaper | No | 9479 | 94.9 | 5.78 | 0.18 | p < .001 | 3.40 | −0.19 | p < .001 | 4.85 | 0.08 | p = .039 | 3.37 | −0.11 | p = .063 |
| Yes | 509 | 5.1 | 5.96 | 3.21 | 4.93 | 3.26 | |||||||||
| School | No | 7106 | 71.1 | 5.73 | 0.20 | p < .001 | 3.43 | −0.14 | p < .001 | 4.82 | 0.13 | p < .001 | 3.41 | −0.15 | p < .001 |
| Yes | 2882 | 28.9 | 5.93 | 3.29 | 4.95 | 3.26 | |||||||||
Discussion
Similarly to other recent American researches,18,21 this study pointed out that a significant proportion of university students was not vaccinated, particularly among men (only 2.2% of men were vaccinated), highlighting the existing gap of HPV vaccine coverage among university aged individuals.
Overall, students investigated showed a good level of knowledge on HPV infection and HPV vaccination, contrary to previous research which found greater gaps knowledge about HPV among college students also in high-income countries.18–20 Nevertheless, the comparison between these different studies must be done cautiously, because of the different methods performed to test knowledge levels about HPV. This high level of knowledge detected seems to be promising in the light of robust evidences about a positive association between women’s awareness on HPV and HPV vaccination uptake.22,23 However, higher knowledge is not always associated with higher vaccine uptake or, at least, its contribution does not necessary play a predominant role. In a recent meta-analysis, the contribution of knowledge has been resized in favour of other factors, such as physician’s recommendation or parents’ believes.24 Another systematic review exploring barriers and facilitators to HPV vaccination of young women in high-income countries shows how parents seem keen to retain a crucial role in decision-making on behalf of their daughters and healthcare professionals appeared to reinforce this position.25
Effect of socio-demographic and behavioural characteristics on knowledge and perception
According with the primary results of the regression analysis, females were significantly more acquainted with HPV infection and they showed a lower level of shame than males. Interestingly, concerns about possible side effects following vaccination were higher in females. This result is in line with findings from other studies18,19,26 and it should not be ignored by information campaigns designed to improve HPV awareness among young adults. Interestingly, no effect of the sexual orientation was noted for neither the knowledge nor the perception. The use of birth control pill was also associated to better outcomes both regarding knowledge and perceptions: this finding could be partially explained by a previous contact with healthcare professionals, since in Italy a medical prescription for receiving birth pill is required. Nevertheless, the study identified in the healthcare workers the source of information with the highest positive impact on all outcomes investigated (see below), in line with other and diverse contexts from Italy,27 USA28 and Asia.29 Moreover, the girls using the birth-pill could be represent a sample of selected students who are more informed than others about sexually transmitted diseases.
The age played a key role in the knowledge of HPV and perceptions. Surely, the exposition to health-related information increases with the age, in line with another Italian study on a sample of adolescents and young women aged 14–24 years as the adjusted OR was 1.14 (95%CI: 1.08 to 1.20) for every 1-year increment.30 This finding is of crucial importance, since it has to be taken into account the fact that a preventive intervention such HPV vaccination can provide a better protection if taken in a younger age.
The absence of a sexual partner negatively affected knowledge and trust compared with people with a more stable presence of a sexual partner. This finding may raise questions about the communication strategy adopted. In our context, information on the transmissibility of HPV may not have received enough attention. For example, in other countries like Australia and in the Anglosphere in general, only in the recent years the vaccine has started to be referred as the HPV vaccine, rather than the cervical cancer vaccine, in order to extend to male population as well the perception of benefitting from this vaccine.31
Students who smoke showed a lower level of knowledge, next to a lower shame. This could be explained by the fact that people following a healthier lifestyle may have a stronger interest in HPV issues as well. Smokers seem to have less concerns about implications from HPV infection, but at the same time a lower trust in a preventive vaccine.
A previous contact with information on HPV, having likely occurred in vaccinated participants and those having a past experience with genital warts, was also significantly associated with higher knowledge, consistently with results from Koshiol et al. showing that women who reported treatment for genital warts, are more likely to have heard of HPV (OR: 2.4; 95%CI: 1.4 to 4.2) and to receive accurate information about HPV, such as HPV causes cancer (OR: 2.7, 95%CI: 1.8 to 4.3).32
A more detailed comment on single questions may be worth, because of the nuances within each area investigated. Questions regarding shame towards HPV-related conditions (sentence 1 to 4) revealed a consistent difference: embarrass arising from the possibility of being diagnosed with HPV infection and subsequent devastation were only slightly over the cut-off value of 4 but in any case more than two times higher than shame deriving from asking for HPV-vaccination or from disclosing to other their possible HPV vaccinated-status (around 2/7 points). Overall trust in vaccine efficacy (sentence 5–12) was high. In all cases, the level of agreement is above 4/7 points. More in detail, vaccine was perceived to be more efficient in preventing HPV infection, cervical cancer rather than all other kinds of HPV-related cancers (some kinds of penis, oral and anal cancers) and genital warts. The awareness of the vaccine as a tool to prevent transmission to the sexual partner was also quite high. Agreement with both sentences concerning fear for possible vaccine side effects (sentence 13 and 14) stood below 4/7 points. The vaccine was not perceived as a dangerous for health in case of the administration after an HPV infection would have occurred. In particular, the results did not identify relevant barriers in HPV vaccine uptake in the shame deriving from asking for HPV-vaccination or from disclosing to other their possible HPV vaccinated-status. As opposite, an American study18 revealed that among college students the strongest concerns about the vaccine were related to family and friends finding out if the students were to get vaccinated.
Relationship between knowledge, perception and vaccination status
In this study, the status of being vaccinated against HPV was associated to a significantly higher average level of knowledge (as well as a substantially better pattern in terms of shame, trust and fear), but the level of knowledge, surprisingly, did not show to be a predictor for the HPV vaccination status, rising an important issue as regards the decision behind the choice whether receiving the vaccine or not. However, the same logistic regression brought to light a strong association between perceptions and the vaccination status. At first sight, the rationale behind this decision seems to lie on an emotional basis, rather than on a well-informed appraisal. However, according to results of the study, this good set of perceptions could be explained at least partially by the high level of knowledge. As confirmed shown in the adjusted linear regression, increases in the level of knowledge successfully reduce the feeling of shame for HPV-related conditions and enhance trust in the protection offered by the vaccine.
In this scenario, perceptions seem to fill an intermediate position between the knowledge and the decision to receive the vaccine. However, the knowledge remains a primum movens which is worth to be targeted in health promotion and communicable disease prevention.
The role of different sources of information
Having received information from healthcare workers showed to have a relevant and positive effect on knowledge, shame, trust and fear compared with all other sources of information used to get acquainted and documented on HPV and HPV vaccine. Similar studies already pointed at healthcare providers as a reliable source of information able to improve vaccine uptake33 and knowledge also in males.34 A recent systematic review35 showed that one of the major facilitators of HPV vaccination among adolescents is the recommendation of a physician or other healthcare workers.
However, the same review also identified parental acceptance and peer encouragement as important facilitators. Rosen et al.36 found that female adolescents who received information on HPV infection from their mothers had not only higher knowledge, but also a better perception on HPV vaccines. This evidence is in line with our study, reporting a determinant role of family members and friends in reducing the perceived shame.
Information acquired at school contributed to knowledge similarly to what healthcare workers did, but did not seem to be as much efficient in reducing shame and fear and enhance trust in vaccine. These findings raise a reasonable doubt on the accuracy of information conveyed.
Strength and limitations
This study has several limitations. First, participation in this study was on a completely free and voluntary basis. Because of the study settings, we were not aware of the number of students who decided not to take part in the study in each classroom by not returning the questionnaire, or by verbally refusing in advance to receive the questionnaire. Thus, we were not able to estimate the answering rate. On this basis, we could neither exclude a potential selection bias nor predict the direction of this bias.
This was not a multi-centre study. The study population included university students from several faculties. These results may not be inferred to the same aged Italian population because of undeniable effects of the educational level on HPV awareness and perception and not even to the entire Italian college students due to the convenience sample used.
Not all participants accurately completed questionnaires in every single required fields, leaving a slightly different denominator for each computation due to missing values.
Females in the age group 18–19-year-old were exposed to free-to-charge HPV-vaccination offered within the framework of the national vaccination programme. This may affect HPV awareness and overall knowledge in this group by being overexposed compared to older students and male students, despite efforts to try to control for this confounder.
It is not possible to exclude the presence of a social desirability bias, by providing answers perceived as ‘correct’ in the social setting, especially as regards the trust in vaccination. However, the anonymous nature of the survey and the self-administration modality should have contribute to reduce this bias, at least partially. Similarity, the effect of a recall bias cannot be excluded as well, in particular with regards to recall of information about the vaccination status. As reported in other studies,37 this bias could substantially affects the accuracy of this information, however the nature of the sample and the level of knowledge showed may limit the magnitude of the influence of this bias.
In spite of these limitations, the very large sample size – approximately ten thousand participants involved – is a strength worth mentioning of our study.
Conclusions
These data suggest the presence of a good framework for implementing a coordinated and comprehensive strategy to prevent HPV related diseases, as recommended by WHO, identifying in the university students a possible target for HPV vaccination. By digging deeply into perceptions, this study provides further evidence for identifying specific areas that might be targeted as first to encourage primary prevention and vaccine uptake. Alarmingly, increasing trends in HPV-related cancers – in particular anal and head and neck cancers which affect also male population – have been observed in the last decade.38 The role of primary prevention together with screening programmes is essential in controlling this increase.
In agreement with the main findings of our study, a winning strategy to overcome HPV vaccine hesitancy could be based on a correct communication style aimed not only at providing cognitive elements, but also at stimulating positive perceptions, reducing fears and shame and increasing trust on HPV vaccine efficacy. According to a recent systematic review,35 both school-based vaccination programmes and peer encouragement were identified as facilitators for HPV uptake among adolescents. These data encourage the dissemination of accurate information and positive messages to promote HPV vaccination also in the university context, trying to create positive reinforcements among university students.
Our findings may thus be useful in developing effective health education strategies and materials to raise confidence of HPV and HPV vaccines, and in turn to boost public confidence and acceptability.
Materials and methods
Sample
From October 2015 to May 2016, students were recruited from different faculties of the University of Padua and the University of Verona, Italy. Participants were recruited on a completely free and voluntary basis and they were not offered any form of compensation for their time. Participants were eligible if they identified themselves as 18–25 years of age and enrolled in one of the courses offered by the University of Padua or the University of Verona. Degree courses attended by the sample were classified in the following seven main areas: (i) health-care professions, (ii) sciences, (iii) humanities, (iv) engineering, (v) law and economics, (vi) psychology, (vii) medicine and dentistry.
Data collection
Members of the research group visited the classrooms on several given days and all students in attendance were invited to complete the questionnaire. Participants were given oral information about the purpose of the study, and reassurance of confidentiality and anonymity regarding all collected data. The questionnaire was then distributed to all participants, with consent inferred from completion of the questionnaire. Participants were asked about their socio-demographic characteristics (age, gender, nationality, area of residence), number of sexual partners in the previous 24 months, age at first sexual intercourse, sexual orientation, use of contraceptive methods (birth pill), smoking habit, personal or close people’s experience with genital warts, HPV vaccination status. The questionnaire was adapted from Schaefer et al.39 In detail, past experience with genital warts was assessed with two questions: ‘Have you ever been diagnosed with genital warts (condylomata)?’ and ‘Do you know anybody who had been diagnosed with genital warts (condylomata)?’. Participants who had answered positively to one or both these questions as regards previous personal or close people’s experiences with genital warts were coded as ‘experienced’. The HPV vaccination status was assessed by asking participants to tick a box that best described their current situation. Response options were ‘I have completed the series of three shots for the HPV vaccine, ‘I have started but not completed the series of three shots for the HPV vaccine, ‘I have scheduled an appointment with my doctor to receive the HPV vaccine’, ‘I have not received the HPV vaccine or scheduled an appointment to receive the HPV vaccine’. Participants who had received at least one dose of the HPV vaccine or had declared to have booked an appointment to receive the first dose were coded as ‘vaccinated’. Participants’ knowledge of HPV was assessed with a set of the following seven True/False questions (Figure 1). A score was calculated then for every participant: one point for each correct answer to the True/False question; zero points for each wrong or missing answer. The score ranged from 0 (no knowledge) to 7 points (maximum knowledge). Data about the sources of information were also collected by asking participants to tick a pre-labelled box: as possible sources of information we investigated a selection of persons (healthcare workers, a friend, a family member), means of communication (TV, internet and social networks, newspapers or magazines) and school education. Multiple answers were possible. As regards the perception, the three main areas of investigation of this study – given by perceived shame of potential HPV-related and vaccine-related conditions, trust in vaccine efficacy and worry for potential vaccine side effects – were assessed with 14 sentences listed in Figure 1. Questions were presented in a random order on the questionnaire. Participants were asked to grade their agreement with each sentence on a 7-point Likert scale, where 1-point means total disagreement (1 = ‘I fully disagree’) and 7-point means complete agreement (7 = ‘I fully agree’). The value of 4-point was chosen as arbitrary cut-off. The questionnaire took approximately 15 minutes to complete. A pilot survey with a small sample (n = 40) from the individuated target population was conducted. Face validity was tested by measuring the importance of items in the proposed questionnaire. Items rated with a mean value ≥ 3 on a 5-point Likert scale were maintained. Pretesting was also used to ensure that items were clearly written and interpreted correctly. According to results and issues raised by the pilot study, no questions were added or deleted and minor grammatical and lexical changes were made in the final version to improve understandability.
Data were treated with full confidentiality in accordance with Italian legislation. Written informed consent was obtained from all participants. To ensure anonymous nature of the data the informed consents were collected separately from questionnaire. This study complies with the Declaration of Helsinki and the study protocol was approved by the ethical committee of the Padua Provincial Authority (date of approval 7/30/2015).
Statistical analysis
Means and one-way between subjects analysis of variance (ANOVA) were calculated to estimate students’ knowledge of HPV and perceived shame for a potential HPV infection, trust and worry regarding HPV and vaccine related issues by socio-demographic, behavioural characteristics and means of communication used.
The effects of socio-demographic and behavioural characteristics on knowledge and perception was assessed with a linear regression analysis, adjusting for age, gender, age at first intercourse, number of sexual partners, smoking habit, sexual orientation, personal or close people’s experience of genital warts and HPV vaccination status, which were assumed as potential confounders. All variables were entered in a single step. Another adjusted linear regression was conducted to study the effect of knowledge on perception itself, while controlling for socio-demographic and behavioural characteristics.
A logistic regression model was developed to examine factors associated with vaccination status adjusting for age, gender, age at first intercourse, number of sexual partners, smoking habit, sexual orientation, personal or close people’s experience of genital warts and degree course attended.
Statistical significance for all tests was set at p ≤ 0.05 (two-sided).
Data input was carried out using REDCap software platform40 and statistical analysis was performed using IBM® SPSS Statistics® version 23.
Note
443 participants did not declare their vaccine status.
Acknowledgments
We would thank Milena Sperotto for her substantial contribution in the review process.
Authors’ contribution
All authors contributed to the article and approved the final version.
SC: study conception and design, drafting of the manuscript. CB: intellectual content, drafting of the manuscript. TB: study conception, supervision. AB: data interpretation and supervision. MF statistical analyses, interpretation of data and drafting of the manuscript, DG: interpretation of data and drafting of the manuscript. SM: study conception and design, data collection. VB: study conception, design, supervision and drafting of the manuscript.
Disclosure of potential conflicts of interest
VB received grants for taking part on advisory boards and at expert meetings, and for acting as speaker and/or organizer of meetings/congresses. The other authors have no potential conflicts of interest to disclose.
References
- 1.Human papillomavirus vaccines: WHO position paper, May 2017. 92(19):241–68. WHO. Weekly Epidemiological Record, WHO. [accessed 2017. May 12]. http://www.who.int/wer/2017/wer9219/en/. [Google Scholar]
- 2.Bruni L, Diaz M, Castellsagué X, Ferrer E, Bosch FX, de Sanjosé S.. Cervical human papillomavirus prevalence in 5 continents: meta-analysis of 1 million women with normal cytological findings. J Infect Dis. 2010;202:1789–99. doi: 10.1086/657321. [DOI] [PubMed] [Google Scholar]
- 3.Muñoz N, Castellsagué X, de González AB, Gissmann L. Chapter 1: HPV in the etiology of human cancer. Vaccine. 2006;24(3):S3/1–10. doi: 10.1016/j.vaccine.2006.05.115. [DOI] [PubMed] [Google Scholar]
- 4.Cocchio S, Bertoncello C, Baldovin T, Buja A, Majori S, Baldo V. Self-reported genital warts among sexually-active university students: a cross-sectional study. BMC Infect Dis. 2018;18:41. doi: 10.1186/s12879-018-2954-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO Comprehensive cervical cancer prevention and control - a healthier future for girls and women. WHO; n.d.. [accessed 2017 November 7]. http://www.who.int/reproductivehealth/publications/cancers/9789241505147/en/. [Google Scholar]
- 6.SAGE guidance for the development of evidence-based vaccine-related recommendations ; nd [accessed 2018 February] http://www.who.int/immunization/sage/Guidelines_development_recommendations.pdf.
- 7.Italian Minister of Health (MoH) Papillomavirus, aggiornate le schedule vaccinali; nd [accessed 2018 October22] http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=1572.
- 8.Conferenza Stato-Regioni Piano nazionale prevenzione vaccinale 2017-2019 (PNPV) n.d.. http://www.trovanorme.salute.gov.it/norme/dettaglioAtto?id=58185 (accessed October22, 2018).
- 9.Intesa tra il Governo le Regioni e le province autonome di Trento e Bolzano sul documento recante “Piano Nazionale Prevenzione Vaccinale (PNPV) 2012-2014”. Intesa ai sensi dell’articolo 8, comma 6, della legge 5 giugno 2003. 131; n.d.. [accessed 2017 November 7]. http://www.statoregioni.it/Documenti/DOC_016696_264%20csr.pdf. [Google Scholar]
- 10.Italian Minister of Health (MoH) I dati nazionali al 2017 sulle coperture vaccinali per papillomavirus (HPV) n.d.. http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=3429 (accessed December4, 2018).
- 11.European Centre for Disease Prevention and Control Introduction of HPV vaccines in EU countries – an update; Stockholm: ECDC; 2012. [Google Scholar]
- 12.Napolitano F, D’Alessandro A, Angelillo IF. Investigating Italian parents’ vaccine hesitancy: A cross-sectional survey. Hum Vaccin Immunother. 2018;14:1558–65. doi: 10.1080/21645515.2018.1463943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts JR, Thompson D, Rogacki B, Hale JJ, Jacobson RM, Opel DJ, Darden PM. Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine. 2015;33:1748–55. doi: 10.1016/j.vaccine.2015.01.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ragan KR, Bednarczyk RA, Butler SM, Omer SB. Missed opportunities for catch-up human papillomavirus vaccination among university undergraduates: identifying health decision-making behaviors and uptake barriers. Vaccine. 2018;36:331–41. doi: 10.1016/j.vaccine.2017.07.041. [DOI] [PubMed] [Google Scholar]
- 15.Khan TM, Buksh MA, Rehman IU, Saleem A. Knowledge, attitudes, and perception towards human papillomavirus among university students in Pakistan. Papillomavirus Res. 2016;2:122–27. doi: 10.1016/j.pvr.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shafei MN, Zainon N, Zulkifli NF, Ibrahim MI.. Knowledge and perception on Human Papilloma Virus Infection and vaccination among medical students of a University in Malaysia. Procedia - Social and Behavioral Sciences 2014;116:2707–10. doi: 10.1016/j.sbspro.2014.01.640. [DOI] [Google Scholar]
- 17.Makwe CC, Anorlu RI, Odeyemi KA. Human papillomavirus (HPV) infection and vaccines: knowledge, attitude and perception among female students at the University of Lagos, Lagos, Nigeria. J Epidemiol Glob Health. 2012;2:199–206. doi: 10.1016/j.jegh.2012.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barnard M, George P, Perryman ML, Wolff LA. Human papillomavirus (HPV) vaccine knowledge, attitudes, and uptake in college students: implications from the precaution adoption process model. PLoS One. 2017;12:e0182266. doi: 10.1371/journal.pone.0182266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tatar O, Perez S, Naz A, Shapiro GK, Rosberger Z. Psychosocial correlates of HPV vaccine acceptability in college males: A cross-sectional exploratory study. Papillomavirus Res. 2017;4:99–107. doi: 10.1016/j.pvr.2017.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blödt S, Holmberg C, Müller-Nordhorn J, Rieckmann N. Human papillomavirus awareness, knowledge and vaccine acceptance: a survey among 18-25 year old male and female vocational school students in Berlin, Germany. Eur J Public Health. 2012;22:808–13. doi: 10.1093/eurpub/ckr188. [DOI] [PubMed] [Google Scholar]
- 21.Laz TH, Rahman M, Berenson AB. Human papillomavirus vaccine uptake among 18- to 26-year-old women in the United States: national health interview survey, 2010. Cancer. 2013;119:1386–92. doi: 10.1002/cncr.27894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson AR, Hashibe M, Bodson J, Gren LH, Taylor BA, Greenwood J, Jackson BR, She R, Egger MJ, Kepka D. Factors related to HPV vaccine uptake and 3-dose completion among women in a low vaccination region of the USA: an observational study. BMC Womens Health. 2016;16:41. doi: 10.1186/s12905-016-0323-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan ZCY, Chan TS, Ng KK, Wong ML. A systematic review of literature about women’s knowledge and attitudes toward human papillomavirus (HPV) vaccination. Public Health Nurs. 2012;29:481–89. doi: 10.1111/j.1525-1446.2012.01022.x. [DOI] [PubMed] [Google Scholar]
- 24.Newman PA, Logie CH, Lacombe-Duncan A, Baiden P, Tepjan S, Rubincam C, Doukas N, Asey F. Parents’ uptake of human papillomavirus vaccines for their children: a systematic review and meta-analysis of observational studies. BMJ Open. 2018;8:e019206. doi: 10.1136/bmjopen-2017-019206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:700. doi: 10.1186/1471-2458-14-700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Baer H, Allen S, Braun L. Knowledge of human papillomavirus infection among young adult men and women: implications for health education and research. J Community Health. 2000;25:67–78. doi: 10.1023/A:1005192902137. [DOI] [PubMed] [Google Scholar]
- 27.Napolitano F, Navaro M, Vezzosi L, Santagati G, Angelillo IF. Primary care pediatricians’ attitudes and practice towards HPV vaccination: A nationwide survey in Italy. PLoS One. 2018;13:e0194920. doi: 10.1371/journal.pone.0194920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nowak GJ, Cacciatore MA. Parents’ confidence in recommended childhood vaccinations: extending the assessment, expanding the context. Hum Vaccin Immunother. 2017;13:687–700. doi: 10.1080/21645515.2016.1236881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Masadeh MM, Alzoubi KH, Al-Azzam SI, Al-Agedi HS, Abu Rashid BE, Mukattash TL. Public awareness regarding children vaccination in Jordan. Hum Vaccin Immunother. 2014;10:1762–66. doi: 10.4161/hv.28608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di Giuseppe G, Abbate R, Liguori G, Albano L, Angelillo IF. Human papillomavirus and vaccination: knowledge, attitudes, and behavioural intention in adolescents and young women in Italy. Br J Cancer. 2008;99:225–29. doi: 10.1038/sj.bjc.6604454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gunasekaran B, Jayasinghe Y, Brotherton JML, Fenner Y, Moore EE, Wark JD, Fletcher A, Tabrizi SN, Garland SM. Asking about human papillomavirus vaccination and the usefulness of registry validation: a study of young women recruited using Facebook. Vaccine. 2015;33:826–31. doi: 10.1016/j.vaccine.2014.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Koshiol J, Rutten LF, Moser RP, Hesse N. Knowledge of human papillomavirus: differences by self-reported treatment for genital warts and sociodemographic characteristics. J Health Commun. 2009;14:331–45. doi: 10.1080/10810730902873067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Firenze A, Marsala MGL, Bonanno V, Maranto M, Ferrara C, Giovannelli L, Restivo V. Facilitators and barriers HPV unvaccinated girls after 5 years of program implementation. Hum Vaccin Immunother. 2015;11:240–44. doi: 10.4161/hv.36158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Napolitano F, Napolitano P, Liguori G, Angelillo IF. Human papillomavirus infection and vaccination: knowledge and attitudes among young males in Italy. Hum Vaccin Immunother. 2016;12:1504–10. doi: 10.1080/21645515.2016.1156271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Loke AY, Kwan ML, Wong Y-T, Wong AKY. The uptake of human papillomavirus vaccination and its associated factors among adolescents: a systematic review. J Prim Care Community Health. 2017;8:349–62. doi: 10.1177/2150131917742299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rosen BL, Shew ML, Zimet GD, Ding L, Mullins TLK, Kahn JA. Human papillomavirus vaccine sources of information and adolescents’ knowledge and perceptions. Glob Pediatr Health. 2017;4:2333794X17743405. doi: 10.1177/2333794X17743405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yamaguchi M, Sekine M, Kudo R, Adachi S, Ueda Y, Miyagi E, Hara M, Hanley SJB, Enomoto T. Differential misclassification between self-reported status and official HPV vaccination records in Japan: implications for evaluating vaccine safety and effectiveness. Papillomavirus Res. 2018;6:6–10. doi: 10.1016/j.pvr.2018.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Harder E, Juul KE, Jensen SM, Thomsen LT, Frederiksen K, Kjaer SK. Factors associated with non-participation in cervical cancer screening – A nationwide study of nearly half a million women in Denmark. Prev Med. 2018;111:94–100. doi: 10.1016/j.ypmed.2018.02.035. [DOI] [PubMed] [Google Scholar]
- 39.Schaefer Ziemer K, Hoffman MA. Beliefs and attitudes regarding human papillomavirus vaccination among college-age women. J Health Psychol. 2013;18:1360–70. doi: 10.1177/1359105312462432. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- SAGE guidance for the development of evidence-based vaccine-related recommendations ; nd [accessed 2018 February] http://www.who.int/immunization/sage/Guidelines_development_recommendations.pdf.


