ABSTRACT
Primary prevention of human papillomavirus (HPV) through vaccination is a high priority in Canada’s cancer prevention efforts. All Canadian provinces and territories have introduced publicly funded, school-based vaccination programs against HPV, but vaccine uptake remains suboptimal in some jurisdictions. We conducted a descriptive qualitative study to better understand the determinants of low HPV vaccine uptake and identify strategies to enhance vaccine acceptance using the socio-ecological model. In Quebec, interviews and focus groups were held in 2015–2016 with 70 key informants including immunization managers, school nurses, school principals, teachers and parents of Grade 4 students (9 years of age).
Our findings showed that HPV vaccine uptake was dependent on many interrelated factors at the individual and interpersonal level (e.g. knowledge and attitudes of the different players involved in the vaccination system), at the community level (e.g. social group values and norms, media coverage around the HPV vaccine), at the organizational level (e.g. allocated resources, information provision, consent process, immunization setting and environment) and at the policy level (e.g. changes in provincial HPV vaccine program). We are using the data collection and interpretation tools and approaches developed by our team and used in Quebec to expand our study to four other provinces (British Columbia, Alberta, Ontario and Nova Scotia). We are conducting environmental scans, semi-structured interviews and a survey to better understand the determinants of low HPV vaccine uptake and identify strategies to enhance vaccine acceptance. Having an in-depth understanding of the determinants of HPV vaccination in school settings is critical in order to identify root causes of the suboptimal vaccine uptake and to develop tailored interventions to address these on both supply- and demand-side issues.
KEYWORDS: HPV vaccine, determinants, school-based immunization programs, immunization managers, interviews, socio-ecological model
Introduction
HPV vaccination programs in Canada
Primary prevention of human papillomavirus (HPV) through vaccination is a high priority in Canada’s cancer prevention efforts. Approximately 75% of Canadians will be infected with HPV during their lifetime; and though most infections resolve on their own, a minority of infections will lead to cervical, oral, anal, penile, and vaginal cancers.1 Fortunately, vaccines that target oncogenic strains of HPV have been developed and recommended in Canada for females (since 2007) and males (since 2010).2 In Canada, health care, and hence immunization, is the responsibility of the provincial/territorial governments. Most of the Canadian population lives in the provinces of Ontario (38.3%), Quebec (23.2%), British Columbia (13.2%), and Alberta (11.6%).3 From 2007 to 2010, all Canadian provinces and territories implemented publicly funded, school-based vaccination programs for females. Public health funding decisions are made at a provincial level and, therefore, the implementation of immunization programs reflect jurisdictional considerations that frequently result in different schedules and dosing. More recently, all provinces and territories have expanded the school-based HPV vaccination programs to also include males. The Canadian Immunization Committee (CIC) recommended HPV vaccination coverage targets of 80% and 90% of eligible students within two and five years of program introduction, respectively.1 However, since the introduction of HPV vaccination programs, coverage has been well below public health goals in several provinces and territories. Furthermore, there are important disparities in HPV vaccine coverage between and in some cases within jurisdictions in Canada. For example, a review conducted by Shapiro and al. in 2016 showed that HPV vaccine coverage (series completion) for females varied between 47% in Northwest Territories and 94% in Newfoundland and Labrador.4 Results of an ecological study conducted in 4 provinces revealed that, in Quebec, regional HPV vaccine coverage was lower in areas with higher proportions of socially deprived individuals, immigrants and/or native English speakers but did not reveal such inequalities in Ontario, Manitoba and British Columbia.5
The low uptake of HPV vaccination is a challenge that is limiting progress in HPV – and cancer – prevention.2 This is particularly concerning when looking at equity. No matter where a young person lives in Canada, there should be equitable opportunity for access to HPV vaccine. Suboptimal vaccine uptake since the implementation of programs is often assumed to be caused by a lack of acceptance or vaccine hesitancy issues among parents. Indeed, access to the vaccine is not expected to be a major issue since HPV vaccines are delivered free of charge to students in schools, and school-based vaccination programs are known to be an effective strategy to reach target populations.6 In Canada, other school-based programs have achieved higher vaccine coverage (e.g., meningococcal or hepatitis B vaccines).7–9 For instance, in Quebec, for the 2017–2018 school year, the uptake for the hepatitis B vaccine, which is administered at the same time as the HPV vaccine, was 84% compared to 75% for HPV. 10 However, where, when, to whom and by whom the program is delivered in schools can affect access and equity of opportunity for uptake.
Effective strategies to increase HPV vaccine uptake and acceptance are urgently needed in order for Canada to achieve its vaccination coverage goal of 90%. However, a recent literature review on educational interventions to increase HPV vaccination acceptance indicates that well-designed studies adequately powered to detect change in HPV vaccine uptake were rare and generally did not demonstrate the effectiveness of the tested intervention.11 Only with a better understanding of the underlying determinants of suboptimal and variable HPV vaccination coverage will we be able to design effective and tailored interventions.
Determinants of HPV acceptance and uptake
In the past decade, several studies have investigated the determinants of HPV vaccination uptake.12–14 Different factors have been associated with HPV vaccination acceptance, such as the importance of healthcare providers’ recommendations, perceived benefits and safety of the vaccine or vaccine-related knowledge. However, because the majority of these studies were based on social cognitive models (e.g. Health Belief Model, Theory of planned behaviour) they have measured similar constructs (e.g. perceived safety of the vaccine, perceived threat of the disease, etc.). Thus, there is limited information on the socio-contextual and organizational factors associated with suboptimal HPV vaccine uptake. In a school-based delivery program these factors may be equally or potentially more important than individual factors. Furthermore, very few studies have looked at implementation factors linked to HPV vaccination uptake in school-based programs.15 There is also a paucity of studies looking at the ethical issues of implementing school-based vaccination programs for children and adolescents (e.g., informed consent and information provision, parental vs. students consent).16,17
Using the Socio-Ecological model to better understand barriers and enabling conditions of HPV vaccine acceptance and uptake in school-based programs
Our team’s work is informed by the Socio-Ecological Model. This model assumes that an individual’s behaviours and attitudes are determined by multiple levels of influence, which interact with one another, within a complex ecological environment.18 According to the socio-ecological model, HPV vaccination decisions are shaped by a complex interaction between factors operating at different levels: individual and interpersonal (i.e. parents’ and students’ attitudes, values, knowledge, confidence, fear of pain, as well as the influence of parents’ and students’ closest social circles); organizational (i.e. delivery aspects of HPV vaccination services that can facilitate or discourage vaccination – e.g., pain mitigation efforts, vaccination settings); community and public policy (i.e. broad socio-cultural factors that create a climate in which vaccination is either encouraged or inhibited as well as national, regional and local agencies’ support for policies that promote/facilitate HPV vaccination).18,19 We selected this model because it includes factors both at the demand side (attitudes, knowledge and beliefs about HPV vaccination) and supply side (the way that school-based vaccination programs are delivered). The use of this model allows us to select which determinants to act upon in order to increase HPV vaccination uptake in school-based programs and facilitates tailoring interventions to fit specific contexts.18,19
Results and discussion
In the province of Quebec, the school-based HPV vaccination program was implemented in 2008 (Grade 4 girls only) and was extended to boys in 2016. While the HPV school-based program targets students aged 9 years-old, adolescents can consent to be vaccinated at the age of 14 and thus could receive the HPV vaccine despite their parents’ refusal during catch-up clinics in high schools.20 During the 2008/09 school-year, HPV vaccine coverage uptake was 81% for the entire province (data compiled by the ministry of Health). In 2014/15, HPV vaccine coverage uptake dropped to 74% and the lowest HPV vaccine uptake was recorded for the 2015/16 school-year with 73% of vaccine coverage (using the information from the provincial immunization registry implemented in 2015). Moreover, wide disparities exist between areas regarding HPV coverage. Since the very beginning of the school-based program, some areas in Quebec had coverage well below the provincial average, while others succeed in reaching the target coverage rate (90% or above). Interviews and focus groups were held in 2015–2016 with 70 key informants including immunization managers, school nurses, school principals, teachers and parents of Grade 4 students. Our findings showed, not surprisingly, that HPV vaccine uptake was dependent on many interrelated factors at the individual and interpersonal level, at the organizational level and at the community and policy level (Figure 1).
Figure 1.
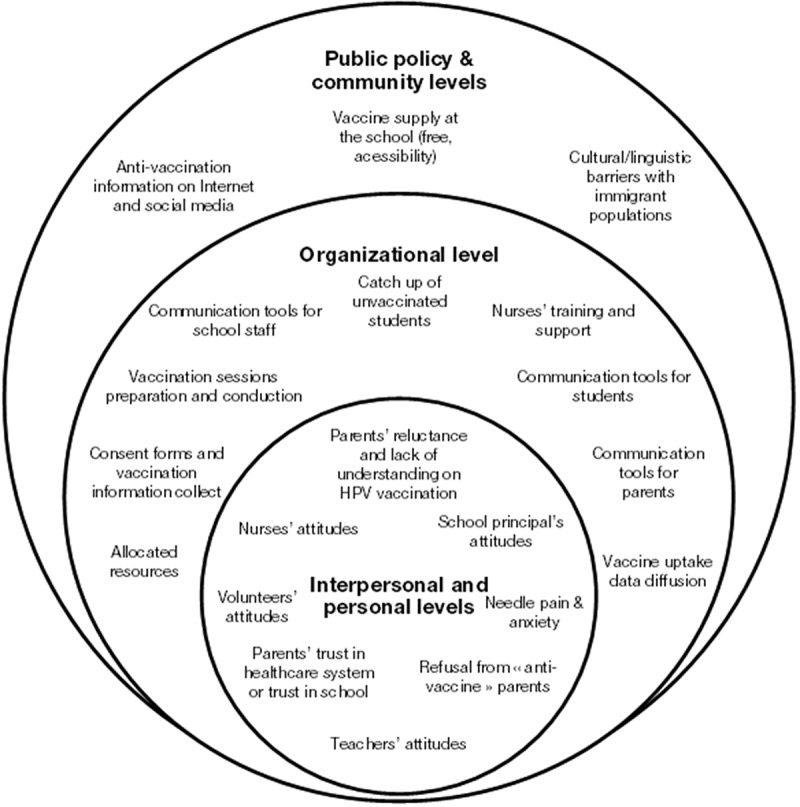
Factors associated with HPV vaccine acceptance and uptake in Quebec school-based vaccination programs based on the socio-ecological model.
At the individual and interpersonal level, the most frequently invoked barrier was parents’ lack of knowledge and negative attitudes toward the HPV vaccine. Many nurses and managers indicated that the information disseminated to parents to aid in decision-making was insufficient or inadequate (too complicated for some, too simple for others). Some nurses and managers also noted that parents’ vaccine acceptance issues were linked to specific characteristics of the HPV vaccine (e.g., the fact that the vaccine protects against a sexually transmitted infection, that it is administered to children, and that it is still perceived as a “new” vaccine). Some teachers mentioned not feeling comfortable talking about the vaccine, to promote its use or to answer students’ questions, while some school principals questioned the relevance of offering this vaccine in a school setting (e.g. perception of no direct benefits for the school clientele in comparison to other “air-borne contagious” diseases such as measles). As HPV is a vaccine against a sexually transmitted virus, some parents indicated being uncomfortable discussing sexuality with their child, especially at 9 or 10 years of age.
I think that parents don’t know why this vaccine is given and they have a lot of fears. We explain, explain and explain, but still people don’t understand. (School nurse)
I did not have my daughter vaccinated. […] I think the vaccine is too new and I have read about some adverse events that made me wonder. I thought that my daughter was not sexually active, so why vaccinate? She’s only in Grade 4 [i.e., aged 9 years-old], so maybe when she will be 13 or 14-years-old. So I thought she was too young. (Parent)
Our preliminary findings also showed that many system-level barriers existed at the organizational level. School-based vaccination programs’ implementation varied considerably between each area and even between different schools in the same health area. For example, most of the nurses were visiting classes to inform students about HPV vaccination, but the duration of these visits and the information provided were highly variable (i.e., some nurses only distributed the informed consent forms in classrooms while others presented information about the importance of vaccination in general and about the HPV vaccine to students). Many school nurses mentioned that obtaining informed consent from parents was often problematic. They mentioned that many parents do not read or do not understand the information. Moreover, they mentioned that there were only a couple of days between when the consent and information forms were sent to parents and when parents needed to return the signed form to the school. This short delay was also judged by parents as problematic to make an informed decision regarding their child’s vaccination (i.e., feeling of “being rushed to accept”, lack of time to call the school nurse or the family doctor to have more information about the vaccine). Language issues for parents not fluent in French or in English were also identified by nurses as an important barrier to the informed consent process.
We have some parents who don’t speak English or French, that’s not easy. When parents are able to read about the vaccine, they are more open, that is helpful. (School nurse)
Lack of resources allocated to the school-based vaccination programs was also a common challenge. The high workload of some nurses limited their involvement in education/information activities and their efforts to ensure that all informed consent forms were received. Other organizational barriers were related to logistical issues regarding organization of the vaccination days within schools (securing appropriate facilities to run an immunization clinic during school hours, lack of collaboration of school staff), accessing vaccination records of students, and running catch-up clinics for students who missed the vaccination days. Due to high staff turnover, training nurses was also problematic in some regions.
In terms of space, sometimes we are not able to find a place to vaccinate. […] We want to be part of the school life, but we are not within the school, so that’s difficult. (School nurse)
Every year it’s still a bit of a challenge for the school. We are a nuisance. Of course, they don’t say it, they are kind and everything, but you know, you go to the classrooms with all your papers, and you see the teachers who are stressed and very busy… They allow us only 5 minutes to speak to the students, you see… So we are welcomed but not welcomed at the same time… (School nurse)
At the community and the policy level, the barrier most frequently reported by parents, nurses, teachers and managers was the negative impact of misinformation from the Internet and social media that created doubts and concerns about the rationale, safety and effectiveness of the HPV vaccine.
There is a major barrier and that’s the media. There have been stories of death after HPV vaccination and this goes viral quite rapidly. We hear about these stories and right after we begin seeing vaccine refusal. (School nurse)
I looked on the Internet, I did some searches and, I don’t recall what the website was, but there was a lot of information and testimonies. That was not positive, that was not reassuring. (Parent)
The change in the provincial HPV vaccine program with the addition of vaccination of boys was perceived by key informants as both a barrier (i.e., justifying why boys were included at this point, more parents to reach) and an enabling condition (i.e., less stigma for girls, more equity).
Opportunities to enhance HPV vaccination acceptance and uptake were also identified by key informants, mostly at the individual and interpersonal level and at the organizational level. As shown in other studies, our findings reinforce the critical role of school nurses in improving HPV vaccine coverage at the organizational level.19,21–23 The involvement and dedication of school nurses in their schools and community that contribute to trust building with the public is a strength of the program. Collaboration with school staff – including support from the school principal – is also essential to ensure the smooth running of vaccination days. At the individual and interpersonal level, school nurses and managers noted the important role that teachers can have in enhancing acceptance by educating students about vaccination, by ensuring that consent forms are sent home, signed and returned, and by managing anxieties during vaccination days. Finally, many key informants noted that parents wanted to do what was best for their children and had a desire to protect their health. In that sense, different strategies to better inform parents about the effectiveness and safety of the HPV vaccine were implemented.
The teachers, many are really collaborative and supporting. Not all teachers, I would say that 80% of them are. But for those who are collaborative, that’s really helpful. When the teachers are helping with the program that makes a huge difference (School nurse).
Parents have more trust in the program because it’s done at the school. Because it’s supported by the school, it’s supported by their child’s teacher, parents are more comfortable with the vaccination (Teacher).
School nurses are doing rounds in every classroom to talk about vaccination, this is part of the process to get parental informed consent, but it’s a way to answer questions, to speak about the vaccine. The students can bring this information back to their parents at home. We are also sending letters to parents and we put these letters on the website of the schools as well. We have pain and anxiety management strategies that nurses need to use. These are all small things, but when we do them all, it’s really helpful. It’s more than just doing the basic things to run the program (Manager in a Local Public Health Clinic).
By identifying barriers and enabling conditions of HPV vaccine acceptance and uptake, policy makers at the regional and provincial levels in Quebec benefited from our findings to implement tailored interventions to improve HPV vaccine uptake. For example, at the provincial level, a working group on improving school-based vaccination programs was created and our final report was used as the basis of the working plan.24 This working group recommended the implementation of an annual webinar on HPV vaccination for school nurses; personalised feedback on HPV vaccine coverage rates to local public health units and schools; provision of information on HPV vaccination to parents at the end of the school year prior to HPV vaccination in the next school year; standardized procedures for reminders and recalls to parents who have not returned the signed informed consent form were also implemented. These interventions were recommended as they were directly addressing barriers identified in our study.
Our project had some limitations. Participation was voluntary. Therefore health professionals, school principals, teachers and parents who were unavailable or declined to participate may have characteristics and opinions that differ from those recruited. In particular, these individuals may have been less supportive of HPV vaccination. Moreover, participants may have enhanced their responses to interview questions to provide socially desirable answers. However, we have triangulated the information provided by different key informants, we actively sought to include those with negative opinions about HPV vaccination and we achieved data saturation, which should have limited these potential biases.
Based on this successful project24, we are using the data collection and interpretation tools and approaches developed by our team and used in Quebec to expand our study to four other provinces (British Columbia, Alberta, Ontario and Nova Scotia, which, along with Quebec, comprises more than 85% of the Canadian population). We are conducting environmental scans to better understand variability in program implementation, semi-structured interviews and a survey to better understand the determinants of low HPV vaccine uptake and identify strategies to enhance vaccine acceptance. Unlike other HPV studies in Canada, our project will generate findings on: (a) the different sociocultural and logistical contexts of HPV vaccines delivery in school settings in Canada; (b) the key determinants of HPV vaccine uptake in school-based programs; and (c) barriers of HPV vaccine acceptance and uptake in students, and user-informed strategies to overcome these barriers. It is possible that the findings from these four additional provinces will differ from the findings in Quebec, but this will provide ground for comparing the major issues at play.
To conclude, there are important gender, socio-economic, ethnic, school system, and geographic disparities in HPV vaccine uptake in and between Canadian provinces. Having an in-depth understanding of the determinants of HPV vaccination in school settings is critical in order to identify the root causes of suboptimal vaccine uptake and to develop tailored interventions addressing both the supply- and the demand-side issues in order to achieve high vaccine coverage.
Materials and methods
This multi-site qualitative study took place in three areas of Quebec where the HPV vaccine uptake was the lowest since the launch of the HPV school-based vaccination program (Montreal, Laval and Laurentides areas, identified using immunization data compiled by the ministry of Health).
The sample included individuals involved in the HPV school-based vaccination program at different levels. At the macro level, key informants included regional public health professionals responsible for overseeing the implementation of the program. At the meso level, key informants were immunization managers in charge of the school-based vaccination and, at the micro level, key informants were school nurses, school principals, Grade 4 teachers and parents of Grade 4 students.
Data were collected between December 2015 and December 2016. First, interviews were conducted with key informants at the macro level. A data collection grid was developed to have an overview of the organization of school-based vaccination services in each participating area. An analysis of HPV uptake at the school level in the three areas was conducted. Schools were purposively selected in each region in order to present similar demographic characteristics (school size, teaching language, deprivation index), but having HPV vaccine coverage below and above the regional average rate. Principals, teachers and nurses working in the selected schools, as well as immunization managers responsible for the area where these particular schools were located, were invited to participate. Interviews were conducted to further assess the barriers and facilitators of HPV vaccination identified during the first interviews (macro level). Interview grids and sociodemographic questionnaires were developed, pretested and adapted for each categories of key informants. Main topics explored during these interviews were: operation and involvement in school-based vaccination programs, attitudes regarding HPV vaccination, perceived barriers and enabling conditions of the school-based program, perceived acceptability of the vaccine by the parents, suggestions to improve the HPV school-based vaccination program.
Focus groups with parents were conducted in November-December 2016. Parents were recruited in the selected schools. Parents were asked questions about their perceptions of the importance of vaccination in schools and of risk and benefits of HPV vaccine. Parents were also asked questions about the issues faced when making their decision regarding their child’s vaccination and, for those who had their child vaccinated, their perception of the vaccination process in schools.
Participation was voluntary and no incentives were given, except for parents who received a 50$ compensation for their time. All interviews were recorded and summarized or transcribed verbatim. Most participants were offered the opportunity to review the summary of their interviews for accuracy and confidentiality.18,19 Thematic content analysis was conducted using the categories of the Socio-Ecological model as main themes.
The study protocol has been approved by the Ethics Review Board of the CHU de Québec-Université Laval.
Funding Statement
This work is supported by the Quebec ministry of Health under Grant SP-00310 and the Canadian Immunization Research Network under Grant 385094.
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
References
- 1.Canadian Immunization Committee Recommendations for human papillomavirus immunization programs. [Internet] Ontario, Canada: Public Health Agency of Canada; 2014. [accessed 2016 November 2]. http://publications.gc.ca/collections/collection_2014/aspc-phac/HP40-107-2014-eng.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Canadian Immunization Committee Summary of Canadian Immunization Committee (CIC) recommendations for HPV immunization programs. CCDR. 2014;40(8):152–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Statistics Canada Census Profile, 2016 Census. 2018. [accessed 2018 November 29]. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E.
- 4.Shapiro GK, Guichon J, Kelaher M.. Canadian school-based HPV vaccine programs and policy considerations. Vaccine. 2017. October 9;35(42):5700–07. doi: 10.1016/j.vaccine.2017.07.079. [DOI] [PubMed] [Google Scholar]
- 5.Drolet M, Deeks SL, Kliewer E, Musto G, Lambert P, Brisson M. Can high overall human papillomavirus vaccination coverage hide sociodemographic inequalities? An ecological analysis in Canada. Vaccine. 2016. April 7;34(16):1874–80. doi: 10.1016/j.vaccine.2016.02.069. [DOI] [PubMed] [Google Scholar]
- 6.Regan DG, Hocking JS. Greatest effect of HPV vaccination from school-based programmes. Lancet Infect Dis. 2015;15(5):497–98. doi: 10.1016/S1473-3099(15)70078-2. [DOI] [PubMed] [Google Scholar]
- 7.Guay M, Clouatre AM, Blackburn M, Baron G, De Wals P, Roy C, Desrochers J, Milord F. Effectiveness and cost comparison of two strategies for hepatitis B vaccination of schoolchildren. Can J Public Health. 2003. Jan-Feb;94(1):64–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Markowski F, Toth E, Mercier M. Flash Vigie - Vaccination en milieu scolaire. 2017. [accessed 2018 October 10]. http://publications.msss.gouv.qc.ca/msss/fichiers/flashvigie/FlashVigie_vol12_no6.pdf.
- 9.Public Health Ontario Immunization coverage report for school pupils in Ontario, 2016-17 school year. 2018. [accessed 2018 October 10]. https://www.publichealthontario.ca/en/eRepository/immunization-coverage-report-2016-17.pdf.
- 10.Markowski F, Toth E. Flash vigie - vaccination en milieu scolaire - Vol. 13, n° 7. 2018. [accessed 2018 November 27]. http://publications.msss.gouv.qc.ca/msss/fichiers/flashvigie/FlashVigie_vol13_no7.pdf.
- 11.Fu LY, Bonhomme LA, Cooper SC, Joseph JG, Zimet GD. Educational interventions to increase HPV vaccination acceptance: a systematic review. Vaccine. 2014. April 7;32(17):1901–20. doi: 10.1016/j.vaccine.2014.01.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ogilvie G, Anderson M, Marra F, McNeil S, Pielak K, Dawar M, McIvor M, Ehlen T, Dobson S, Money D, et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. 2010;7(5):e1000270. doi: 10.1371/journal.pmed.1000270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Krawczyk A, Knauper B, Gilca V, Dube E, Perez S, Joyal-Desmarais K, Rosberger Z. Parents’ decision-making about the human papillomavirus vaccine for their daughters: I. Hum Vaccin Immunother. 2015;11(2):322–29. doi: 10.1080/21645515.2014.1004030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Smith LM, Brassard P, Kwong JC, Deeks SL, Ellis AK, Levesque LE. Factors associated with initiation and completion of the quadrivalent human papillomavirus vaccine series in an Ontario cohort of grade 8 girls. BMC Public Health. 2011;11:645. doi: 10.1186/1471-2458-11-645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cooper Robbins SC, Ward K, Skinner SR. School-based vaccination: a systematic review of process evaluations. Vaccine. 2011;29(52):9588–99. doi: 10.1016/j.vaccine.2011.10.033. [DOI] [PubMed] [Google Scholar]
- 16.Braunack-Mayer A, Skinner SR, Collins J, Tooher R, Proeve C, O’Keefe M, Burgess T, Watson M, Marshall H. Ethical challenges in school-based immunization programs for adolescents: a qualitative study. Am J Public Health. 2015;105(7):1399–403. doi: 10.2105/AJPH.2014.302280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Steenbeek A, Macdonald N, Downie J, Appleton M, Baylis F. Ill-informed consent? A content analysis of physical risk disclosure in school-based HPV vaccine programs. Public Health Nursing (Boston, Mass). 2012. Jan-Feb;29(1):71–79. doi: 10.1111/j.1525-1446.2011.00974.x. [DOI] [PubMed] [Google Scholar]
- 18.McLeroy K, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–77. [DOI] [PubMed] [Google Scholar]
- 19.Batista Ferrer H, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14(700):1–22. doi: 10.1186/1471-2458-14-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gouvernement du Québec Vaccination en milieu scolaire. 2018. [accessed 2018 November 29]. https://www.quebec.ca/sante/conseils-et-prevention/vaccination/vaccination-en-milieu-scolaire/.
- 21.Perman S, Turner S, Ramsay AIG, Baim-Lance A, Utley M, Fulop NJ. School-based vaccination programmes: a systematic review of the evidence on organisation and delivery in high income countries. BMC Public Health. 2017;17:252. doi: 10.1186/s12889-017-4168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Batista Ferrer H, Trotter CL, Hickman M, Audrey S. Barriers and facilitators to uptake of the school-based HPV vaccination programme in an ethnically diverse group of young women. J Public Health (Oxf). 2016. September;38(3):569–77. doi: 10.1093/pubmed/fdv073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Scott K, Batty ML. HPV vaccine uptake among Canadian youth and the role of the nurse practitioner. J Community Health. 2016. February;41(1):197–205. doi: 10.1007/s10900-015-0069-2. [DOI] [PubMed] [Google Scholar]
- 24.Clément P, Gagnon D, Dubé E. Stratégies de promotion de la vaccination contre les virus du papillome humain (VPH) dans le cadre du programme de vaccination scolaire: évaluation des facteurs favorables et des barrières. Québec, Canada: Institut national de santé publique du Québec; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Statistics Canada Census Profile, 2016 Census. 2018. [accessed 2018 November 29]. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E.


