ABSTRACT
The human papillomavirus virus (HPV) vaccine is effective at preventing various cancers, but coverage falls short of targets that are needed for community protection. Here, we use the RE-AIM implementation framework (Reach, Effectiveness, Adoption, Implementation, Maintenance) to understand how text, email, and electronic health record (EHR) reminders and social media campaigns can be used as part of policy and practice interventions to increase HPV vaccination. These technology-based interventions could be used together and mainstreamed into clinical and system-based practice to have the greatest impact. Of the interventions explored, text-based, email-based, and EHR reminders have the most evidence behind them to support their effectiveness. While there are several studies of promotion of the HPV vaccine on social media, more studies are needed to demonstrate their effects and better methods are needed to be able to attribute results to these interventions.
KEYWORDS: HPV, technology, vaccine, text message, email, EHR, social media, RE-AIM, digital
Introduction
Human papillomavirus virus (HPV) vaccination has great potential to decrease the burden of not only cervical cancer but a number of associated oncologic diseases, such as oropharyngeal cancer and other anogenital cancers of the vulva, vagina, penis, and anus. Yet, both in the U.S. and abroad, HPV vaccination rates fall below the coverage needed to enact their full prevention potential.1,2 Furthermore, disparities in vaccination coverage exist geographically and are also driven by socioeconomic factors.1
In recent years, technology has been highlighted as an impactful tool for improving vaccination rates for many diseases, including HPV.3 However, an important next step is to identify not only where technology could be effective but also what is needed for its implementation into sustainable practice. In this commentary, we use an implementation framework to explore how technology-based interventions can be used to improve HPV vaccination rates, with a greater focus on the United States (U.S.), where the majority of studies to date have taken place.
Evaluation using RE-AIM
For nearly 20 years, the RE-AIM model has been applied through multiple stages of evaluative research.4 The theory is made up of five components: Reach (number, proportion, and representativeness of the people who would be able to or want to participate in an intervention); Effectiveness (impact a given intervention has on outcomes including negative effects); Adoption (number, proportion, and representativeness of the organizations and settings who are willing to adopt it); Implementation (fidelity and consistency to the intervention’s protocol); and Maintenance (long-term effects of a program on the individual level and institutionalization of the intervention at the organizational level)(Figure 1).4,5 The RE-AIM framework can be used to understand how technology can be utilized to increase HPV vaccine coverage by identifying at what stage of the implementation process various digital technologies are currently. It can also be used to highlight areas where either more research may be needed or processes put into place to move from research to implementation.
Figure 1.
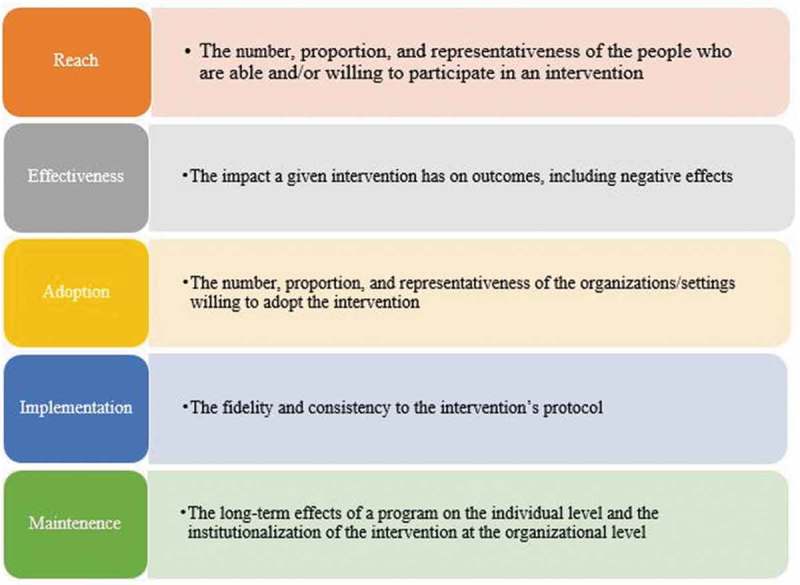
RE-AIM framework.5
RE-AIM component 1: REACH
Text message, email, and app-based reminders
Increasing cell phone access and health technology use presents unique opportunities to employ different methods of reminder-recalls than traditional forms. In the U.S., 95% of adults own a cellphone with high levels of ownership among diverse populations differing by race/ethnicity, education, income, age, and community type.6 Rates are nearly 100% among 30–49 year olds, the age of many parents of adolescents. Cell phone ownership rates are also high globally and will reach an estimated 4.68 billion cell phone users worldwide by 2019.7 Smartphone use is also increasing with 77% of U.S. adults owning a smartphone.6 However, in the U.S., disparities exist as there are moderately lower rates of smartphone ownership for those living in rural areas, with the lowest income strata, with less than a high school education, and/or in older age groups.6 In terms of communication uses, most cell phone owners use text messaging. In one survey, a reported 97% of smartphone owners used text messaging at least once in the past week.8 Email use is also high, with >90% of internet users under the age of 65 in the U.S. using email.9 Almost 90% of smartphone users access email on their phone,8 and more than half of adults with cell phones have also downloaded a health-related app.10 Text messages are also useful across populations with various levels of literacy since each text message can only be 160 characters, which facilitates the use of a minimal number of short, simple words. While text messages that are longer can be split into two or more messages, care must be taken to make sure that split happens in a place that is not confusing to the recipient. In addition, depending on the service, recipients may pay per message received.
Electronic health records
The Health Information Technology for Economic and Clinical Health (HITECH) Act of 2009 was implemented in the U.S. to foster an electronic health information infrastructure and to spearhead the use of electronic health record (EHR) systems for providers.11 Though uptake was initially slow, EHR utilization has become mainstream in health systems across the country. By 2016, more than 60% of the outpatient U.S. physicians achieved meaningful use of an accredited EHR, and more than 95% of the hospitals eligible for the incentive program achieved meaningful use.12 Many eligible professionals also report electronically to immunization information systems (IIS) often directly from their EHR as a part of meaningful use criteria,13 which improves efficiency and timeliness of reporting.14 IIS are population-based registries that consolidate vaccination information across a city or state. All 50 states have an IIS, as do some major cities and territories.15 In addition, some IIS now have bidirectional exchange of vaccine information, allowing vaccines administered elsewhere to be available within the EHR allowing more complete vaccination information.16 Most countries do not currently have IIS; implementation is highly variable for those that have one.17 Australia has a specific HPV vaccine registry.18
Though this article primarily focuses on the evaluation of EHR implementation in the U.S., it is by no means the only country making investments in these sorts of information technologies. In the mid-1990s, Israel became the first country in the world to introduce health information exchange systems and currently, nearly 100% of its primary care physicians use EHR systems.19,20 In Europe, 19 countries have begun development on EHR systems; notable EHR systems have also been studied in Canada, New Zealand, and South Korea, with some implementation initiatives pre-dating that of the U.S.20 The acceptance and nascent implementation of EHR have also begun in developing countries, with notable efforts in highly populated countries such as India, Bangladesh, and China.21–23 The potential health information technology has to improve efficiency, reduce costs, and increase access in health-care systems has incentivized and spurred countries worldwide to develop integrated EHR systems.24
Social media
There were almost 3.2 billion social media users worldwide in 2018, and social media usage continues to grow with an annual increase of 13% worldwide between 2017 and 2018.25 Facebook and YouTube are also the most widely used platforms worldwide with around 2.3 billion Facebook users and 1.9 billion YouTube users.26 Social media use is ubiquitous among U.S. adults with approximately 70% of adults reporting using at least one social media site.27 The most commonly used social media sites in the U.S. are YouTube, used by 73% of adults, followed by Facebook which is used by 68% of adults.27 Social media usage is even higher in younger age groups. Almost 90% of U.S. adults aged 18 to 29 report using one or more types of social media; similar to the overall adult population, young adults most frequently use YouTube and Facebook.28 However, in the youngest adults aged 18–24, there is high uptake of multiple social media sites including YouTube (94%), Facebook (80%), Snapchat (78%), Instagram (71%), and Twitter (45%).28
Adults in the U.S. also frequently use the internet to seek out health information. More than 70% of U.S. adults said that they have gone online for health information with 80% starting with a search engine and 1% turning to a social network as the first resource.29 Given their widespread use, these technologies all have great potential to be used by health-care professionals as a delivery method for health promotion messages.
RE-AIM component 2: EFFECTIVENESS
Text message, email, and app-based reminders
Recommendations encouraging the use of vaccination reminders and recall messages to notify families when vaccines are due or overdue are widespread.30–35 The U.S. Task Force on Community Preventive Services found strong evidence that such reminders improve vaccination rates35 and recently calculated that reminder-recalls result in a median 6 percentage point increase (interquartile interval: 3–13 percentage points; 14 studies) in vaccination rates with client reminder and recall interventions used alone.36 Similarly, a meta-analysis of over 50 studies with more than 138,000 combined participants found that reminders (telephone and autodialer calls, letters, postcards, text messages) were associated with an increased relative rate of vaccine uptake of 1.28 (95% CI 1.23–1.35).37
However, traditional reminder formats, such as via mail or by phone call, have historically had a more limited effect on vaccination uptake in adolescent, low-income, and rural populations in the U.S. as compared to reminders that employ more advanced technology.38–43 These blunted effects could be due to mailings not reaching low-income patients who may move frequently. Potential message recipients may also react negatively or ignore intrusive, impersonal automated phone calls.
Text message vaccine reminders have several characteristics that make them an attractive technology for vaccine reminders. First, the widespread use of text messaging makes them a prime candidate for reaching diverse populations. Text messages also act as a cue to action; they have the potential to draw more attention than mailed reminders, and they are often perceived as less intrusive than a phone call.44 In addition, they remain on a person’s phone as a persistent reminder making them particularly useful for interventions with a clear, desired behavioral outcome. Text messaging is scalable yet able to be personalized. It allows interaction with thousands of patients simultaneously, thereby enabling an impact not only on an individual patient’s health but also on the health of the public through increasing population-level vaccination coverage. Yet, text messages allow personalization based on individual characteristics such as age, gender, language, and desired content. Text message reminders are a flexible platform that can be used either for simple prompts or reminders that inform a patient or family when a vaccine is needed, or for more complex interactions including the embedding of educational information and interactive responses. Finally, text messages are delivered outside the office setting, which is important for reaching patients not accessing care regularly. As such, text messaging is becoming a more common method for disseminating reminder messages.
As for its specific applicability for increasing HPV vaccine uptake, text messaging has been shown to be successful amongst various populations. In a number of studies, both practice-based, IIS, or health authority generated text reminders have helped promote HPV vaccination series completion for adolescents.45–53 While HPV vaccine text message reminders have clear impact in the adolescent population, they have generally had mixed success in older targeted groups.54–56 Few, if any, studies assessing effectiveness of text message vaccine reminders for HPV vaccine outside the U.S. have been published. Text message vaccine reminders have been used for pediatric vaccination studies in some low-middle-income countries57-63 which is promising for adolescent vaccines as well.
Email vaccine reminders have also had demonstrated effects for HPV vaccination as part of studies in which families can select their modality of choice.49,51 Reminders linked to a personal health record or patient portal have also begun to be used in a limited way clinically. Likewise, the interest in the use of mobile apps is also growing, and descriptive studies of their use have been published.64–66 Interventions documenting their effectiveness for HPV or other adolescent vaccinations have not yet published.
Electronic health records
Many studies have shown that provider recommendation proves to be one of the most strongly associated factors in receipt of vaccinations including the HPV vaccine.67–80 This pattern holds true among minority populations despite greater reported mistrust in the health-care system.81,82 EHR vaccination prompts are an ideal method to cue provider vaccine recommendations to parents and adolescents and help promote vaccine uptake. According to the Task Force on Community Preventive services, provider reminder/recall interventions are strongly supported by scientific evidence in improving vaccination rates.35 Many physicians, at least in the U.S., report that they do not always recommend the HPV vaccine during office visits. In a study of pediatricians, family medicine physicians, and OB/GYNs, only 34% reported recommending the HPV vaccine at least 75% of the time to young adolescent patients aged 11–12.83 Without reminder or prompting, providers may inadvertently fail to speak with adolescents and their parents about the HPV vaccine resulting in the adolescents leaving unvaccinated. Regular use of EHR vaccine prompts in primary care settings should prove to decrease missed vaccination opportunities and increase receipt of the HPV vaccine.
Several studies have shown that implementation of EHR-based tools improves vaccine uptake in the U.S.84–90 Effectiveness studies on HPV vaccination and EHR reminders outside the U.S. have not yet been published. Though there are limited studies examining the impact of EHR on HPV vaccine uptake, most studies do show improvement.87,89,90 Fiks et al. conducted a randomized control trial that, in part, examined the impact of EHR vaccination reminder alerts during office visits on the receipt of the HPV vaccine.87 The intervention was measured alongside other strategies such as patient phone calls and provider training, so its individual contribution cannot be isolated. However still, the overall intervention led to an 8% increase in the initiation of the HPV vaccination as compared to the control arm.87 Ruffin et al. used a retrospective cohort study design to compare the uptake of the HPV vaccine in five academic community-based family health practices with EHR prompts versus the uptake in four academic community-based family practices which did not have vaccine-alert systems.89 More vaccine-eligible female patients aged 9–18-y-old initiated the HPV vaccine series in the health system with EHR vaccine prompts, and the EHR reminder systems also contributed to more timely completion of the vaccine series. The benefits of EHR prompts on HPV vaccine receipt were also observed in young male populations as well. Adolescent males are less likely than their female counterparts to receive the HPV vaccine, but there are evidence EHR systems that can help decrease this disparity.90 Using National Ambulatory Medical Care Survey data spanning from 2007 to 2012, Bae et al. were able to demonstrate that EHR reminders were associated with an overall HPV vaccine rate increase, with a particularly steep increase in the adolescent male population.90 However, not all studies of EHR vaccine prompts found improvement in vaccine uptake. Szilagyi et al. found no significant difference in adolescent immunization rates in 22 practices when comparing EHR-prompt intervention groups to control groups.91
Social media
Social media can be an effective, low-cost way of disseminating health information and motivating health behavior change.92 In promoting the HPV vaccine on social media, one must consider two distinct audiences: both the parents of adolescent children and the adolescents and young adults themselves. In some U.S. states, such as California, Pennsylvania, and New York, adolescents can confidentially consent to HPV vaccination themselves as a part of comprehensive preventive care for sexually transmitted infections.93–95 However, in other states and countries, parents must also provide consent for their child to receive the HPV vaccine, so messaging should target both groups so that a joint decision can be made about vaccination.96
Several groups have used social media as a platform to disseminate information about HPV and the HPV vaccine.95,97–103 One of the most widespread campaigns to date is the #ProtectOurFuture campaign sponsored by Ireland’s Health Service Executive (HSE), its national health program.100 The campaign aimed to combat declining HPV vaccine uptake in 2016–2017 when the rate of HPV vaccination uptake fell to 50% from 90% in 2014–2015.104 The campaign used a combination of personal stories and facts distributed through Facebook, Twitter, and YouTube targeting parents and their daughters.100 The campaign reached 1 million Facebook users with 8.7 million impressions, and lead to an increase in Tweets including the terms HSE and HPV from 500,000 in 2016 to 3.2 million in 2017.100 The campaign also had measurable impact on HPV initiation increasing from an estimated 50% in 2016–2017 to 62% in 2017–2018 countrywide.104 Denmark similarly developed a Facebook page and YouTube videos promoting HPV vaccination after HPV vaccine initiation fell to 42% for the 2004 birth cohort from a high of 92% for the 1993–2000 birth cohorts after increased public concern media coverage in the country.105 Denmark’s campaign entitled “Stop HPV – Stop Cervical Cancer” was launched in spring 2017 and is a series of videos on YouTube targeting parents of adolescent girls.102 Although results cannot solely be attributed to the social media campaign, HPV vaccine uptake doubled in 2017.106 Italy also developed a website and social media presence on Facebook, Twitter, and YouTube called “VaccinarSi” – a site with comprehensive information about vaccines to combat widespread antivaccination information in the country.103 The site has been visited more than 1 million times, but study of the effects of the campaign has not yet been studied.103 The U.S. Centers for Disease Control (CDC) have also targeted parents of adolescents through ads on websites and social media platforms such as YouTube to CDC webpages and videos about the HPV vaccine leading to 153 million impressions and 137,000 clicks on ads that redirected users to a website about HPV.107 The CDC also has a YouTube channel with several videos about HPV and the HPV vaccine, although many of these videos are targeted at physicians’ recommendation of the HPV vaccine with only a few videos targeting parents or teenagers directly.108 Results from these campaigns have yet to be published.
Others have developed social media campaigns to improve HPV vaccine uptake on a smaller scale with some effects on knowledge but limited to no effect on vaccination. Mohanty et al. employed Facebook ads for sharing HPV-related health messages and directly targeted adolescents in Philadelphia.95 They found that messages that included short-term consequences of HPV, such as genital warts, resulted in significantly higher views and likes than advertisements that included long-term outcomes, such as cancer. Through this, they were able to demonstrate that adolescents may desire information campaigns focused on immediate risks. Other groups have demonstrated the effectiveness of this loss-framing in HPV intention to vaccinate studies.99,109 By focusing on acute risks of HPV, loss-framing can increase individuals’ perceived susceptibility and severity of the disease.99 While the results of the HPV Facebook ad campaign conducted by Mohanty et al. led to only a small increase in uptake of the vaccine of those who were targeted, they were able to reach over 150,000 adolescents and engaged more than 2,000 adolescents in the campaign demonstrating a broad reach. However, the true study impact on HPV vaccine uptake was difficult to measure as they were limited to city health clinic setting for their study results.95 Ortiz et al. developed a Facebook-centered social media campaign targeting around 100 adolescents with messages about HPV and other health topics via group pages and the adolescent’s news feeds.97 The content and framework of the 3-month campaign incorporated input from adolescents who participated in focus groups and youth advisory board meetings. Though their intervention did increase knowledge in intervention versus control groups, it did not lead to increased HPV vaccination rates. Lyson et al. used Twitter to host a 5-day-long social media campaign for more than 750 adolescents that featured messages about HPV.98 Results showed only a slightly increased awareness about HPV, and there was no change in HPV-related knowledge or increase in HPV vaccine uptake. However, they had recruited a group of individuals who already had high baseline knowledge, awareness, and positive health behaviors relating to HPV therefore not leaving much room for improvement.98
While most of the social media campaigns described did lead to increased knowledge of HPV and the HPV vaccine, few were able to demonstrate increased vaccine uptake.95,104 This is partly due to issues of confidentiality; participants in social media campaigns can remain anonymous, and even those who do identify themselves cannot be linked to their vaccine information records without explicit consent. It may also be hard to know if the intended population saw the intervention. In addition, even when vaccine uptake was improved as was the case in Ireland’s #ProtectOurFuture campaign, the social media campaign was used in combination with other educational efforts, so it is difficult to attribute their results solely to the social media intervention. Therefore, further research is needed on how to better quantify and analyze the effectiveness of social media campaigns on HPV vaccine uptake.
RE-AIM component 3: ADOPTION
Text message, email, and app-based reminders
The main facilitators and barriers to text message vaccine reminders lie in the willingness of parents and providers to use them. The majority of families has unlimited text messaging plans,110,111 reducing concerns about costs to patients/consumers of text-messaging interventions. Parents overall seem open to the use of text message reminders, although some parents remain unwilling. The majority of parents in the U.S. is also open to having text messages delivered directly to their adolescent child about the HPV vaccine.112,113 Little has been published on parents’ interest in mobile apps or personal health records. However, the greatest effects for adolescent vaccinations may be for interventions where parents can choose their reminder type.49,51 Preferences may also differ by population. In one study assessing parental preference for vaccine reminders, being a younger parent was associated with preferring text message vaccine reminders, and being a suburban parent was associated with preferring e-mail reminders. In addition, those who were younger and suburban were most likely to be interested in general use of a personal health record.113 Research into attitudes towards text message adolescent vaccine reminders outside the U.S. still needs to be assessed.
Electronic health records
Introduction of new EHR systems can be burdensome due to the need for additional provider training, cost, and information technology support needed for implementation and acceptability. However, without careful consideration given to these aspects, EHR adoption can fail even though the quality of the system is high. Ludwick and Doucette conducted a seven-country systematic review of the adoption of EHR systems and found that providers with reservations about the overall effectiveness of EHR systems are more willing to adopt when provided “leadership training, project management, and product training services” to help facilitate the transition to a new system.114
In settings where there have been demonstrated benefits to EHR use, preference has grown as providers are now more familiar with the benefits such a system provides. Several EHR systems currently on the market automatically incorporate a health maintenance section which alerts providers on vaccines which are due.115 A U.S.-based study conducted by Humiston et al. showed that although half of the practices in the research networks of the study examined did not currently use EHR prompts, it was one of the most commonly chosen strategies providers wished to implement to increase adolescent immunization rates in the primary care setting.116
Social media
Wider adoption of the use of social media to promote HPV vaccination may be needed by organizations at multiple levels. More advocacy through social media may be needed from international organizations such as the World Health Organization (WHO) and other international public health entities. To date, the WHO only has three videos on YouTube relating to HPV or cervical cancer on their channel.117 The WHO has numerous posts on Facebook about vaccines and the outbreak of vaccine-preventable illnesses frequently using the hashtag #vaccineswork, but these posts and infographics often do not have links to vaccine information or the WHO website which may be helpful.118 Similarly, WHO uses Instagram to provide short posts and infographics about vaccines, but do not often link to resources for further information.119 Vaccine-hesitant parents often cite a desire for more information about vaccines as a reason for hesitancy,120 so links to additional resources should be built into social media posts.
As discussed above, several countries including Ireland, Denmark, Italy, and the U.S. have developed vaccination information campaigns using social media sites.100,102,103,107,108 These country-level campaigns can tailor vaccine information to address country-specific gaps in knowledge, false beliefs, and other information. Similarly, campaigns could be drilled down to even more local levels such as individual cities or local health systems, with vaccine information delivered through social media by local-level health systems. In this way, provider recommendation could be augmented by a social media component with references to evidence-based health information. For example, Glanz et al. developed a randomized control trial to test a social media component which provided a forum to disseminate vaccine information and allow pregnant women to ask questions to providers at a health system in Colorado.121 Compared to general care and vaccine counseling in the office, the social media intervention did lead to improved pediatric vaccination rates,121 and this model could be adapted to provide information about the HPV vaccine to both parents and adolescents.
Several studies have shown that parents trust their child’s doctor the most for vaccine information67-80 and trust government vaccine experts or officials much less.78 This suggests that some parents may not be interested in viewing or participating in social media campaigns sponsored by government or public health entities. Providers themselves could share culturally competent, tailored information over social media sites which would more likely resonate with their patients.122 Several groups have made guides and toolkits for providers to use social media to spread information both about HPV and health information in general to help address these barriers.123–127 However, barriers for providers include lack of skills and inefficiency as well as time constraints.128
RE-AIM component 4: IMPLEMENTATION
Text message, email, and app-based reminders
The implementation of text message, email, or apps depends in part on the stability of the modality, the fidelity of receipt, and the ease of implementing a system. For any of these modalities, the key is collecting up-to-date cell phone numbers or emails and signing up families for text message reminders or email. Of note, cell phone numbers appear to be more stable than home address or home phone numbers in the U.S.;72 even when families move, they typically keep the same cell phone number. Reminders linked to a patient portal can also be used by practices whose EHR supports a portal, thereby aiding in implementation. While app-based reminders may be helpful, they are likely most helpful when linked to the patient’s medical record such that families are reminded about vaccine or care that their specific adolescent needs.
There are two main types of implementation of text message or email reminder/recall. The first is centralized through an IIS or a public health entity. The second is practice-based messages. Each have their pros and cons. While centralized recalls may be more cost effective since can be implemented for large populations as well as take the burden off the individual sites, they may lack the personal connection of the practice. On the practice level, reminder/recall may be more costly and time-consuming for the practice to implement. However, as more traditional phone reminder services offer text messaging or possibly email, implementation will be easier, and cost will be reduced. Some IIS, like the CIR in New York City (NYC), allow providers to send the text messages themselves for free from the CIR website.129 Other public health entities in the U.S. and abroad could consider doing the same.
Electronic health records
EHR prompts have been shown to improve HPV vaccine uptake, however there are concerns about alert fatigue. During a 36-week period, Embi and Leonard recorded response patterns for 178 physicians who were randomized to receive clinical trial alerts and found that response rates alerts followed a significant downward trend with time, falling 2.7% every 2 weeks.130 Provider alert fatigue could also lead to diminishing returns for EHR’s benefit for HPV vaccination uptake.
Though there is evidence that active interaction with EHR reminders may decrease with time, findings from a study conducted by Dixon et al. demonstrate the passive benefits of EHR clinical decision support (CDS) reminders that go beyond provider perception.131 During an EHR CDS intervention, providers randomized to receive the alerts were interviewed about whether they saw the alerts and whether they responded to the prompts. Most providers recalled seeing the alerts but reported that the reminder did not impact their behavior in recommending vaccines. Despite this perception, the intervention arm did experience a significant increase in HPV vaccination coverage, demonstrating that the CDS prompts work though providers feel may feel that they do not.132 Many EHRs do offer vaccine decision support supporting ease of implementation.
Social media
Social media campaigns promoting the HPV vaccine should focus on communicating clear, concise, and factually correct information to large numbers of individuals at a low cost. The campaigns should be targeted, and the messaging could be tailored to the audience with particular emphasis on appealing to the various areas of the Health Belief Model (susceptibility, severity, benefits, barriers, cues to action, and self-efficacy) which has been applied effectively to interventions aimed to improve health behaviors.133 For example, the Mohanty study used a campaign through Facebook advertisements and posts which targeted adolescent girls and boys directly and addressed each element of the Health Belief Model. Risks of HPV were presented which address the susceptibility and severity of disease and the benefits of the HPV vaccine.95 It is important that images used in social media campaigns such as these represent the diverse populations who are affected by HPV so they better understand their susceptibility.134 Additional posts aimed to improve cues to action and self-efficacy. They included information about the availability of the vaccine at local health centers at no cost and information about the laws that allow minors to consent to the vaccine themselves. Larger campaigns could be designed in this way not only by local health authorities, but also international public health organizations such as the WHO, ministries of health, and other large public health organizations which can pool resources and broaden access.
Anti-vaccination campaigns have threatened successful HPV vaccination campaigns in many countries.135 Web 2.0 (which includes social media and other user-generated content online) is a major facilitator of anti-vaccination information with themes of concerns about vaccine safety and effectiveness, alternative medicine, civil liberties, conspiracy theories, and misinformation136 often by using tactics such as skewing scientific evidence, shifting hypotheses, censoring dissent, and attacking critics.137 Posts on social media are uncensored, and misinformation stands side-by-side with factually correct posts receiving equal weight. Vaccine information found on Facebook, for example, is highly polarized and creates “echo chambers” where individuals are generally exposed to information either for or against vaccines with little crossover.138 Even more concerning is a recent study about false news articles on Twitter demonstrated that false information spread significantly farther, faster, deeper, and more broadly than truthful information.139 Exposure to anti-vaccination information has also been shown to reduce intention to vaccinate.104,105,140,141 One effective strategy for HPV vaccine social media campaigns could be to target individuals who are particularly vulnerable to finding and using unreliable and misleading information142 or targeting those communities that are found to be most vaccine hesitant.143
The analysis of sentiment towards vaccines on social media can be used to understand attitudes about the HPV vaccine, identify themes in the pro-vaccine and anti-vaccine communities, measure spikes in anti-vaccination sentiment, and develop interventions to address negative perceptions about vaccines, among other uses. Several groups have evaluated the tone and content of HPV messaging on social media,144–157 and this information can be used to map central concepts of antivaccine information found on social media. Kang et al. analyzed articles shared on Twitter about vaccine information and developed semantic networks, which are images that represent concepts and their interrelatedness in order to display clusters of content that was favorable towards vaccines versus against them.144 The group found that negative vaccine sentiment tended to focus on distrust and skepticism of institutions that promote vaccines and vaccine research and that positive articles promoted trust in vaccinations and scientific evidence.144 Analysis of Tweets can also be used to map digital antivaccination “communities” as well as identify those who are most at risk of exposure to negative vaccine sentiment.150 In addition, Dunn et al. analyzed differential exposure to Tweets based on geographic location and found that HPV vaccine uptake was lower in states where higher levels of misinformation, conspiracy theories, and safety concerns were more common.155
Addressing vaccine hesitancy is complicated, and best practices on using social media to this end are not well defined. One proposed way to reduce vaccine hesitancy is to respond to vocal vaccine deniers in a public forum which can be applied to interactions on social media platforms; the intention is not to change the belief of the refuser but to engage the audience of onlookers who may have questions about vaccines.158 In this way, one can identify the technique being used by the vaccine denier to spread misinformation and respond to the concerns with evidence-based information. While correcting misinformation may be helpful in some cases, one study, not on social media, demonstrated that correcting misinformation can actually be counterproductive and can reduce intention to vaccinate in the most vaccine-hesitant parents.159 Another way to reduce exposure to antivaccination information on social media would be to moderate content, remove false information, and prevent its spread. Content moderation is currently being discussed by platforms such as Facebook, YouTube, and Pinterest.160–162 More research is needed to study initiatives that reduce vaccine hesitancy in a coordinated manner given the complex landscape of information available to parents and patients on social media.
RE-AIM component 5: MAINTENANCE
Text message, email, and app-based reminders
Most text message and other interventions have been as stand-alone studies. The key to maintenance will be integrating these technologies into the usual practice in clinical settings in the U.S. the way that auto-dialer or mailed reminders have previously. Many companies that had previously used auto-dialer reminders now offer text messaging as do some EHR systems – this will be key to its long-term use.
Electronic health records
As a part of HITECH’s meaningful use program, billions of dollars have been distributed to physicians across America to incentivize the adoption and implementation of EHR systems in order to improve health-care outcomes.163 However, many providers feel that EHR systems may reduce productivity and lack key data sharing and interoperability features.163 Even so, as discussed earlier, EHR vaccination reminder use in health centers has been associated with an increase in HPV vaccination uptake in multiple observed settings. Also, providers have been shown to prefer EHR use when framed in terms of its utility as a clinical decision aid.116 As we focus on EHR’s role in improving rates of HPV vaccine receipt, increased functionality and CDS could be emphasized as a selling point for providers and as an aspect of informing policy and would be an important aspect of maintenance.
Social media
The key to maintenance will be investing in social media divisions at public health and governmental organizations who maintain and disseminate factual, up-to-date information about the HPV vaccine. International public health organizations such as the World Health Organization could lead the charge in promoting accurate information about the safety and efficacy of vaccines through social media outlets. These organizations should also take an active role in moderating the vaccine debate. They can use tools to monitor for spikes in antivaccination discourse on social media and launch campaigns through social media and provide commentary on widely viewed antivaccination posts with links back to evidence-based information about the HPV vaccine and other vaccines in general. Country health ministries should continue to promote information about HPV vaccination as discussed above in the cases of Ireland, Denmark, and the U.S. However, more countries must join the charge as antivaccination movements are present worldwide, and countries can develop culturally competent and relevant messaging for their citizens. Providers and health organizations should also be given tools and time to Tweet, blog, or disseminate information via various social media sites. Finally, training and social media guides or Toolkits would be helpful to providers and public health entities who would like to engage via social media but lack sufficient training.
New arenas – more research
Using the RE-AIM framework, one can begin to see at what stage various digital technologies that can be utilized to increase HPV vaccine coverage currently are (Figure 2) as well as what next steps may be. The effectiveness of at least text message reminders and EHR alerts has been established. Therefore, the next steps are for wider spread adoption, implementation, and maintenance in the U.S. Next steps in increasing use of mobile and other media for reminder-recalls could be to facilitate the enrollment of patients and families and for organizations to send the reminders. This would likely be best through linking with EHRs whose immunization data are synchronized with its local IIS. In that way, organizations can seamlessly identify those who are not up to date for vaccination, using the most complete data possible, and send families reminders in their preferred form. This should be paired with immunization Clinical Decision Support (CDS), such that providers do not miss opportunities to vaccinate when patients present for a visit, both for well and acute care. Outside the U.S., more research may be needed to assess the interest in and effectiveness of HPV reminders.
Figure 2.

RE-AIM framework applied to health information technology approaches to improving HPV vaccination uptake.
For social media, the next steps could be to develop better measures to evaluate the impact of these campaigns and conduct more rigorous studies such as randomized control trials. Once measurable effects of these social media campaigns on vaccination have been demonstrated, resources could be pooled, distinct messaging could be developed for various groups including adolescents, their parents, and physicians who recommend the vaccine to their patients, and interventions could be scaled up to reach large groups. Better evidence of the efficacy of social media could also motivate providers and organizations to continue to use these platforms. Additional training may also be needed for doctors, public health entities, and health-care organizations to effectively use social media.
In addition, the greatest impact may be realized if these technology-based interventions are combined rather than used individually. For example, in a potentially ideal scenario, an adolescent patient or their parent was informed of his or her risk and the severity of HPV by a post on Facebook or video on YouTube. The family then scheduled an appointment where the clinician was prompted to give the HPV vaccine by an EHR prompt. Then, 6 months later, that patient was reminded via text message, email, or app to return to the clinic for the second dose of the HPV vaccine and the patient has completed the vaccine series.
These digital technologies will continue to advance, and new technologies and uses of older ones will likely emerge holding great promise. Overall, in the coming years, integration of these technologies could become the mainstays of interventions to promote vaccination.
Disclosure of potential conflicts of interest
The authors have no conflicts of interest to disclose.
References
- 1.Walker TY, Elam-Evans LD, Yankey D, Markowitz LE, Williams CL, Mbaeyi SA, Fredua B, Stokley S.. National, regional, state, and selected local area vaccination coverage among adolescents aged 13-17 Years – United States, 2017. MMWR Morb Mortal Wkly Rep. 2018;67:909–17. doi: 10.15585/mmwr.mm6733a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, de Sanjosé S, Castellsagué X. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. The Lancet Global Health. 2016;4:e453–63. doi: 10.1016/S2214-109X(16)30099-7. [DOI] [PubMed] [Google Scholar]
- 3.Francis DB, Cates JR, Wagner KPG, Zola T, Fitter JE, Coyne-Beasley T. Communication technologies to improve HPV vaccination initiation and completion: a systematic review. Patient Educ Couns. 2017;100:1280–86. doi: 10.1016/j.pec.2017.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Gaglio B, Shoup JA, Glasgow RE. The RE-AIM framework: a systematic review of use over time. Am J Public Health. 2013;103:e38–46. doi: 10.2105/AJPH.2013.301299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89:1322–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pew Research Center Mobile Fact Sheet. [Accessed 2018 December9]http://www.pewinternet.org/fact-sheet/mobile/.
- 7.Statista Number of mobile phone users worldwide from 2013 to 2019 (in billions). [Accessed 2018 December28]. https://www.statista.com/statistics/274774/forecast-of-mobile-phone-users-worldwide/.
- 8.Pew Research Center U.S. smartphone use in 2015. Accessed on 2018 December9].http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/.
- 9.Statista Percentage of internet users in the United States who use e-mail as of November 2017, by age group. Accessed 2018 December9]. https://www.statista.com/statistics/271501/us-email-usage-reach-by-age/.
- 10.Krebs P, Duncan DT. Health app use among US mobile phone owner a national survey. Jmir mHealth And uHealth. 2015;3:e101. doi: 10.2196/mhealth.3949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thomas B. Hitech act driving EHR implementation and standards. Internal Auditing. 2011;26:19–22. [Google Scholar]
- 12.Office of the National Coordinator for Health Information Technology. Non-federal Acute Care Hospital Electronic Health Record Adoption [Accessed 2018 December18]. www.dashboard.healthit.gov/quickstats/pages/FIG-Hospital-EHR-Adoption.php.
- 13.Office of the National Coordinator for Health Information Technology. Electronic Reporting to Immunization Information Services (IIS) by Stage of Meaningful Use Accessed on 2018 December23]. https://dashboard.healthit.gov/quickstats/pages/medicare-eps-immunization-registry-reporting-stage-one-and-two.php.
- 14.Merrill J, Phillips A, Keeling J, Kaushal R, Senathirajah Y. Effects of automated immunization registry reporting via an electronic health record deployed in community practice settings. Appl Clin Inform. 2013;4:267–75. doi: 10.4338/ACI-2013-02-CR-0009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Contacts for IIS Immunization Records [Accessed 2018 December23]. https://www.cdc.gov/vaccines/programs/iis/contacts-locate-records.html.
- 16.Stockwell MS, Natarajan K, Ramakrishnan R, Holleran S, Forney K, Aponte A, Vawdrey DK. Immunization data exchange with electronic health records. Pediatrics. 2016;137:e20154335. doi: 10.1542/peds.2015-4335. [DOI] [PubMed] [Google Scholar]
- 17.Tozzi AE, Gesualdo F, D‘Ambrosio A, Pandolfi E, Agricola E, Lopalco P. Can digital tools be used for improving immunization programs? Frontiers in Public Health. 2016;4:36. doi: 10.3389/fpubh.2016.00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The National Human Papillomavirus (HPV) Vaccination Program Register [Accessed 2019 March2]. http://www.hpvregister.org.au/.
- 19.Peterburg Y. Israel‘s health IT industry: what does the american recovery and reinvestment act mean for Israeli Collaborative Opportunities? Israel trade commission. Sydney, Australia: Australia Milken Institute 2010. [Google Scholar]
- 20.Fragidis LL, Chatzoglou PD. Implementation of a nationwide electronic health record (EHR). Int J Health Care Qual Assur. 2018;31:116–30. doi: 10.1108/IJHCQA-09-2016-0136. [DOI] [PubMed] [Google Scholar]
- 21.Srivastava SK. Adoption of electronic health records: a roadmap for India. Healthc Inform Res. 2016;22:261–69. doi: 10.4258/hir.2016.22.4.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xiang Y. Evaluation of EHR in health care in China: utilizing fuzzy AHP in SWOT analysis In Shaozi Li, Qun Jin, Xiaohong Jiang, J.H. Park, editors. Frontier and future development of information technology in medicine and education ITME. Dordrecht (Netherlands): Springer Netherlands; 2013;2014 2715. [Google Scholar]
- 23.Hossain A, Quaresma R, Rahman H. Investigating factors influencing the physicians’ adoption of electronic health record (EHR) in healthcare system of Bangladesh: an empirical study. Int J Inf Manage. 2019;44:76–87. doi: 10.1016/j.ijinfomgt.2018.09.016. [DOI] [Google Scholar]
- 24.Stone CP. 2014. A glimpse at EHR implementation around the world: the lessons the US Can Learn The Health Institute for E-Health Policy. https://www.e-healthpolicy.org/sites/e-healthpolicy.org/files/A_Glimpse_at_EHR_Implementation_Around_the_World1_ChrisStone.pdf [Google Scholar]
- 25.Smart Insights . Global social media research summary. [Accessed 2019. Mar 1]. https://www.smartinsights.com/social-media-marketing/social-media-strategy/new-global-social-media-research/.
- 26.Statista Most popular social networks worldwide as of January 2019, ranked by number of active users (in millions). [Accessed 2019 March1]. https://www.statista.com/statistics/272014/global-social-networks-ranked-by-number-of-users/.
- 27.Pew Research Center Social media fact sheet. Available at http://www.pewinternet.org/fact-sheet/social-media/. Accessed on November26, 2018.
- 28.Pew Research Center Social Media Use in. [Accessed 2018 November19]. http://www.pewinternet.org/2018/03/01/social-media-use-in-2018.
- 29.Pew Research Center Health Online. 2013. [Accessed 2018 November20]. http://www.pewinternet.org/2013/01/15/health-online-2013/.
- 30.Centers for Disease Control and Prevention. Standards for pediatric immunization practices. Recommended by the National Vaccine Advisory Committee. MMWR Recomm Rep 1993;42:1–10 [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Recommendations of the advisory committee on immunization practices, the American academy of pediatrics, and the american academy of family physicians: use of reminder and recall by vaccination providers to increase vaccination rates. MMWR Morb Mortal Wkly Rep. 1998; 47: 715–17. [PubMed] [Google Scholar]
- 32.The National Vaccine Advisory Committee. Strategies to sustain success in childhood immunizations. JAMA 1999; 282: 363–70. [DOI] [PubMed] [Google Scholar]
- 33.National Vaccine AC. Standards for child and adolescent immunization practices. National Vaccine Advisory Committee. Pediatrics. 2003;112:958–63. [PubMed] [Google Scholar]
- 34.Middleman AB, Rosenthal SL, Rickert VI, Neinstein L, Fishbein DB, D‘Angelo L. Adolescent immunizations: a position paper of the Society for Adolescent Medicine. J Adolesc. Health. 2006;38:321–27. [DOI] [PubMed] [Google Scholar]
- 35.Briss PA, Rodewald LE, Hinman AR, Shefer AM, Strikas RA, Bernier RR, Carande-Kulis VG, Yusuf HR, Ndaiye SM, Williams SM, et al. Reviews of evidence regarding interventions to improve vaccination coverage in children, adolescents, and adults. The Task Force on Community Preventive Services. Am J Prev Med. 2000;18:97–140. [DOI] [PubMed] [Google Scholar]
- 36.Community Preventive Services Task Force. Increasing appropriate vaccination: client reminder and recall systems: Task Force finding and rationale statement 2015. [Accessed 2018 December18 https://www.thecommunityguide.org/sites/default/files/assets/Vaccination-Client-Reminders.pdf.
- 37.Jacobson Vann JC, Jacobson RM, Coyne-Beasley T, Asafu-Adjei JK, Szilagyi PG. Patient reminder and recall interventions to improve immunization rates. Cochrane Database Syst Rev. 2018(1):CD003941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.LeBaron CW, Starnes DM, Rask KJ. The impact of reminder-recall interventions on low vaccination coverage in an inner-city population. Arch Pediatr Adolesc Med. 2004;158:255–61. doi: 10.1001/archpedi.158.3.255. [DOI] [PubMed] [Google Scholar]
- 39.Irigoyen MM, Findley S, Wang D, Chen S, Chimkin F, Pena O, Mendonca E. Challenges and successes of immunization registry reminders at inner-city practices. Ambul Pediatr. 2006;6:100–04. doi: 10.1016/j.ambp.2005.10.006. [DOI] [PubMed] [Google Scholar]
- 40.Szilagyi PG, Schaffer S, Barth R, Shone LP, Humiston SG, Ambrose S, Averhoff F. Effect of telephone reminder/recall on adolescent immunization and preventive visits: results from a randomized clinical trial. Arch Pediatr Adolesc Med. 2006;160:157–63. doi: 10.1001/archpedi.160.2.157. [DOI] [PubMed] [Google Scholar]
- 41.Hambidge SJ, Davidson AJ, Phibbs SL, Chandramouli V, Zerbe G, LeBaron CW, Steiner JF. Strategies to improve immunization rates and well-child care in a disadvantaged population: a cluster randomized controlled trial. Arch Pediatr Adolesc Med. 2004;158:162–69. doi: 10.1001/archpedi.158.2.162. [DOI] [PubMed] [Google Scholar]
- 42.Daley MF, Steiner JF, Brayden RM, Xu S, Morrison S, Kempe A. Immunization registry-based recall for a new vaccine. Ambul Pediatr. 2002;2:438–43. [DOI] [PubMed] [Google Scholar]
- 43.Centers for Disease for Control Prevention. Evaluation of vaccination recall letter system for Medicaid-enrolled children aged 19-23 months–montana, 2011. MMWR Morb Mortal Wkly Rep 2012;61:811–15. [PubMed] [Google Scholar]
- 44.Kharbanda EO, Stockwell MS, Fox HW, Rickert VI. Text4Health: a qualitative evaluation of parental readiness for text message immunization reminders. Am J Public Health. 2009;99:2176–78. doi: 10.2105/AJPH.2009.161364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stockwell MS, Kharbanda EO, Martinez RA, Lara M, Vawdrey D, Natarajan K, Rickert VI. Text4Health: impact of text message reminder-recalls for pediatric and adolescent immunizations. Am J Public Health. 2012;102:e15–21. doi: 10.2105/AJPH.2011.300331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kharbanda EO, Stockwell MS, Fox HW, Andres R, Lara M, Rickert VI. Text message reminders to promote human papillomavirus vaccination. Vaccine. 2011;29:2537–41. doi: 10.1016/j.vaccine.2011.01.065. [DOI] [PubMed] [Google Scholar]
- 47.Rand CM, Vincelli P, Goldstein NP, Blumkin A, Szilagyi PG. Effects of phone and text message reminders on completion of the human papillomavirus vaccine series. J Adolesc. Health. 2017;60:113–19. doi: 10.1016/j.jadohealth.2016.09.011. [DOI] [PubMed] [Google Scholar]
- 48.O‘Leary ST, Lee M, Lockhart S, Eisert S, Furniss A, Barnard J, Eblovi D, Shmueli D, Stokley S, Dickinson LM, et al. Effectiveness and cost of bidirectional text messaging for adolescent vaccines and well care. Pediatrics. 2015;136:e1220–7. doi: 10.1542/peds.2015-1089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kempe A, O‘Leary ST, Shoup JA, Stokley S, Lockhart S, Furniss A, Dickinson LM, Barnard J, Daley MF. Parental choice of recall method for HPV vaccination: a pragmatic trial. Pediatrics. 2016;137:e20152857. doi: 10.1542/peds.2015-2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Aragones A, Bruno DM, Ehrenberg M, Tonda-Salcedo J, Gany FM. Parental education and text messaging reminders as effective community based tools to increase HPV vaccination rates among Mexican American children. Preventive Med Reports. 2015;2:554–58. doi: 10.1016/j.pmedr.2015.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morris J, Wang W, Wang L, Peddecord KM, Sawyer MH. Comparison of reminder methods in selected adolescents with records in an immunization registry. J Adolesc. Health. 2015;56:S27–32. doi: 10.1016/j.jadohealth.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 52.Rand CM, Brill H, Albertin C, Humiston SG, Schaffer S, Shone LP, Blumkin AK, Szilagyi PG. Effectiveness of centralized text message reminders on human papillomavirus immunization coverage for publicly insured adolescents. J Adolesc. Health. 2015;56:S17–20. doi: 10.1016/j.jadohealth.2014.10.273. [DOI] [PubMed] [Google Scholar]
- 53.Bar-Shain DS, Stager MM, Runkle AP, Leon JB, Kaelber DC. Direct messaging to parents/guardians to improve adolescent immunizations. J Adolesc. Health. 2015;56:S21–6. doi: 10.1016/j.jadohealth.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 54.Richman AR, Maddy L, Torres E, Goldberg EJ. A randomized intervention study to evaluate whether electronic messaging can increase human papillomavirus vaccine completion and knowledge among college students. J Am College Health. 2016;64:269–78. doi: 10.1080/07448481.2015.1117466. [DOI] [PubMed] [Google Scholar]
- 55.Patel A, Stern L, Unger Z, Debevec E, Roston A, Hanover R, Morfesis J. Staying on track: a cluster randomized controlled trial of automated reminders aimed at increasing human papillomavirus vaccine completion. Vaccine. 2014;32:2428–33. doi: 10.1016/j.vaccine.2014.02.095. [DOI] [PubMed] [Google Scholar]
- 56.Berenson AB, Rahman M, Hirth JM, Rupp RE, Sarpong KO. A human papillomavirus vaccination program for low-income postpartum women. Am J Obstet Gynecol. 2016;215:318:e1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Bangure D, Chirundu D, Gombe N, Marufu T, Mandozana G, Tshimanga M, Takundwa L. Effectiveness of short message services reminder on childhood immunization programme in Kadoma, Zimbabwe – a randomized controlled trial, 2013. BMC Public Health. 2015;15:137. doi: 10.1186/s12889-015-1470-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Gibson DG, Ochieng B, Kagucia EW, Were J, Hayford K, Moulton LH, Levine OS, Odhiambo F, O’Brien KL, Feikin DR. Mobile phone-delivered reminders and incentives to improve childhood immunisation coverage and timeliness in Kenya (M-SIMU): a cluster randomised controlled trial. The Lancet Global Health. 2017;5:e428–e38. doi: 10.1016/S2214-109X(17)30072-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Haji A, Lowther S, Ngan‘Ga Z, Gura Z, Tabu C, Sandhu H, Arvelo W. Reducing routine vaccination dropout rates: evaluating two interventions in three Kenyan districts, 2014. BMC Public Health. 2016;16:152. doi: 10.1186/s12889-016-2823-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Domek GJ, Contreras-Roldan IL, O‘Leary ST, Bull S, Furniss A, Kempe A, Asturias EJ. SMS text message reminders to improve infant vaccination coverage in Guatemala: A pilot randomized controlled trial. Vaccine. 2016;34:2437–43. doi: 10.1016/j.vaccine.2016.03.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Uddin MJ, Shamsuzzaman M, Horng L, Labrique A, Vasudevan L, Zeller K, Chowdhury M, Larson CP, Bishai D, Alam N. Use of mobile phones for improving vaccination coverage among children living in rural hard-to-reach areas and urban streets of Bangladesh. Vaccine. 2016;34:276–83. doi: 10.1016/j.vaccine.2015.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kazi AM, Ali M, Zubair K, Kalimuddin H, Kazi AN, Iqbal SP, Collet J-P, Ali SA. Effect of mobile phone text message reminders on routine immunization uptake in Pakistan: randomized controlled trial. JMIR Public Health Surveill. 2018;4:e20. doi: 10.2196/publichealth.7026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Eze GU, Adeleye OO. Enhancing routine immunization performance using innovative technology in an urban area of Nigeria. West Afr J Med. 2015;34:3–10. [PubMed] [Google Scholar]
- 64.Bednarczyk RA, Frew PM, Salmon DA, Whitney E, Omer SB. ReadyVax: a new mobile vaccine information app. Hum Vaccin Immunother. 2017;13:1149–54. doi: 10.1080/21645515.2016.1263779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fadda M, Galimberti E, Fiordelli M, Romano L, Zanetti A, Schulz PJ. Effectiveness of a smartphone app to increase parents‘ knowledge and empowerment in the MMR vaccination decision: a randomized controlled trial. Hum Vaccin Immunother. 2017;13:2512–21. doi: 10.1080/21645515.2017.1360456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Fadda M, Galimberti E, Fiordelli M, Schulz PJ. Evaluation of a mobile phone-based intervention to increase parents‘ knowledge about the measles-mumps-rubella vaccination and their psychological empowerment: mixed-method approach. Jmir mHealth And uHealth. 2018;6:e59. doi: 10.2196/mhealth.8263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lu PJ, Yankey D, Fredua B, O‘Halloran AC, Williams C, Markowitz LE, Reagan-Steiner S. Association of provider recommendation and human papillomavirus vaccination initiation among male adolescents aged 13-17 Years-United States. J Pediatr. 2018. doi: 10.1016/j.jpeds.2017.12.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Fenton AT, Eun TJ, Clark JA, Perkins RB. Indicated or elective? The association of providers‘ words with HPV vaccine receipt. Hum Vaccin Immunother. 2018;14:2503–09. doi: 10.1080/21645515.2018.1480237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gilkey MB, Calo WA, Moss JL, Shah PD, Marciniak MW, Brewer NT. Provider communication and HPV vaccination: the impact of recommendation quality. Vaccine. 2016;34:1187–92. doi: 10.1016/j.vaccine.2016.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rahman M, Laz TH, McGrath CJ, Berenson AB. Provider recommendation mediates the relationship between parental human papillomavirus (HPV) vaccine awareness and HPV vaccine initiation and completion among 13- to 17-year-old U.S. adolescent children. Clin Pediatr (Phila). 2015;54:371–75. doi: 10.1177/0009922814551135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Newman PA, Logie CH, Lacombe-Duncan A, Baiden P, Tepjan S, Rubincam C, Doukas N, Asey F. Parents‘ uptake of human papillomavirus vaccines for their children: a systematic review and meta-analysis of observational studies. BMJ Open. 2018;8:e019206. doi: 10.1136/bmjopen-2017-019206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Clark SJ, Butchart A, Kennedy A, Dombkowski KJ. Parents‘ experiences with and preferences for immunization reminder/recall technologies. Pediatrics. 2011;128:e1100–5. doi: 10.1542/peds.2011-0270. [DOI] [PubMed] [Google Scholar]
- 73.Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168:76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Perkins RB, Clark JA, Apte G, Vercruysse JL, Sumner JJ, Wall-Haas CL, Rosenquist AW, Pierre-Joseph N. Missed opportunities for HPV vaccination in adolescent girls: a qualitative study. Pediatrics. 2014;134:e666–74. doi: 10.1542/peds.2014-0442. [DOI] [PubMed] [Google Scholar]
- 75.Kahn JA, Rosenthal SL, Jin Y, Huang B, Namakydoust A, Zimet GD. Rates of human papillomavirus vaccination, attitudes about vaccination, and human papillomavirus prevalence in young women. Obstet Gynecol. 2008;111:1103–10. doi: 10.1097/AOG.0b013e31817051fa. [DOI] [PubMed] [Google Scholar]
- 76.Caskey R, Lindau ST, Alexander GC. Knowledge and early adoption of the HPV vaccine among girls and young women: results of a national survey. J Adolesc. Health. 2009;45:453–62. doi: 10.1016/j.jadohealth.2009.04.021. [DOI] [PubMed] [Google Scholar]
- 77.Dempsey AF, Abraham LM, Dalton V, Ruffin M. Understanding the reasons why mothers do or do not have their adolescent daughters vaccinated against human papillomavirus. Ann Epidemiol. 2009;19:531–38. doi: 10.1016/j.annepidem.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Freed GL, Clark SJ, Butchart AT, Singer DC, Davis MM. Sources and perceived credibility of vaccine-safety information for parents. Pediatrics. 2011;127(Suppl 1):S107–12. doi: 10.1542/peds.2010-1722P. [DOI] [PubMed] [Google Scholar]
- 79.Kennedy A, Basket M, Sheedy K. Vaccine attitudes, concerns, and information sources reported by parents of young children: results from the 2009 HealthStyles survey. Pediatrics. 2011;127(Suppl 1):S92–9. doi: 10.1542/peds.2010-1722N. [DOI] [PubMed] [Google Scholar]
- 80.Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34:6700–06. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 81.Fu LY, Zimet GD, Latkin CA, Joseph JG. Associations of trust and healthcare provider advice with HPV vaccine acceptance among African American parents. Vaccine. 2017;35:802–07. doi: 10.1016/j.vaccine.2016.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Scarinci IC, Garces-Palacio IC, Partridge EE. An examination of acceptability of HPV vaccination among African American women and Latina immigrants. J Womens Health. 2007;16:1224–33. doi: 10.1089/jwh.2006.0175. [DOI] [PubMed] [Google Scholar]
- 83.Vadaparampil ST, Kahn JA, Salmon D, Lee JH, Quinn GP, Roetzheim R, Bruder K, Malo TL, Proveaux T, Zhao X, et al. Missed clinical opportunities: provider recommendations for HPV vaccination for 11-12 year old girls are limited. Vaccine. 2011;29:8634–41. doi: 10.1016/j.vaccine.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Shojania KG, Jennings A, Mayhew A, Ramsay CR, Eccles MP, Grimshaw J. The effects of on-screen, point of care computer reminders on processes and outcomes of care. Cochrane Database Syst Rev. 2009;3;CD001096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Castillo EM, Chan TC, Tolia VM, Trumm NA, Powell RA, Brennan JJ, Kreshak AA. Effect of a computerized alert on emergency department hepatitis a vaccination in homeless patients during a large regional outbreak. J Emerg Med. 2018;55:764–68. doi: 10.1016/j.jemermed.2018.09.004. [DOI] [PubMed] [Google Scholar]
- 86.Fiks AG, Hunter KF, Localio AR, Grundmeier RW, Bryant-Stephens T, Luberti AA, Bell LM, Alessandrini EA. Impact of electronic health record-based alerts on influenza vaccination for children with asthma. Pediatrics. 2009;124:159–69. doi: 10.1542/peds.2008-2823. [DOI] [PubMed] [Google Scholar]
- 87.Fiks AG, Grundmeier RW, Mayne S, Song L, Feemster K, Karavite D, Hughes CC, Massey J, Keren R, Bell LM, et al. Effectiveness of decision support for families, clinicians, or both on HPV vaccine receipt. Pediatrics. 2013;131:1114–24. doi: 10.1542/peds.2012-3122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Stockwell MS, Catallozzi M, Camargo S, Ramakrishnan R, Holleran S, Findley SE, Kukafka R, Hofstetter AM, Fernandez N, Vawdrey DK. Registry-linked electronic influenza vaccine provider reminders: a cluster-crossover trial. Pediatrics. 2015;135:e75–82. doi: 10.1542/peds.2014-2616. [DOI] [PubMed] [Google Scholar]
- 89.Ruffin MT, Plegue MA, Rockwell PG, Young AP, Patel DA, Yeazel MW. Impact of an electronic health record (EHR) reminder on human papillomavirus (HPV) vaccine initiation and timely completion. J Am Board Fam Med. 2015;28:324–33. doi: 10.3122/jabfm.2015.03.140082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bae J, Ford EW, Wu S, Huerta T. Electronic reminder‘s role in promoting human papillomavirus vaccine use. Am J Managed Care. 2017;23:E353-+. [PubMed] [Google Scholar]
- 91.Szilagyi PG, Serwint JR, Humiston SG, Rand CM, Schaffer S, Vincelli P, Dhepyasuwan N, Blumkin A, Albertin C, Curtis CR. Effect of provider prompts on adolescent immunization rates: a randomized trial. Acad Pediatr. 2015;15:149–57. doi: 10.1016/j.acap.2014.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Korda H, Itani Z. Harnessing social media for health promotion and behavior change. Health Promot Pract. 2013;14:15–23. doi: 10.1177/1524839911405850. [DOI] [PubMed] [Google Scholar]
- 93.Atkins. Assembly Bill No. 499. In: Legislature CS, ed., 2011.
- 94.Amendment to Part 23 of New York Codes, Rules and Regulations (NYCRR) In: Legislature NYS, ed., 2016.
- 95.Mohanty S, Leader AE, Gibeau E, Johnson C. Using Facebook to reach adolescents for human papillomavirus (HPV) vaccination. Vaccine. 2018;36:5955–61. doi: 10.1016/j.vaccine.2018.08.060. [DOI] [PubMed] [Google Scholar]
- 96.Kabakama S, Gallagher KE, Howard N, Mounier-Jack S, Burchett HE, Griffiths UK, et al Social mobilisation, consent and acceptability: a review of human papillomavirus vaccination procedures in low and middle-income countries. BMC Public Health. 2016;16:834. doi: 10.1186/s12889-016-3517-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ortiz RR, Shafer A, Cates J, Coyne-Beasley T. Development and evaluation of a social media health intervention to improve adolescents‘ knowledge about and vaccination against the human papillomavirus. Glob Pediatr Health. 2018;5:2333794X18777918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lyson HC, Le GM, Zhang J, Rivadeneira N, Lyles C, Radcliffe K, Pasick RJ, Sawaya G, Sarkar U, Centola D. Social media as a tool to promote health awareness: results from an online cervical cancer prevention study. Journal of cancer education: the official journal of the American Association for Cancer Education, US: Spriinger. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Lee MJ, Cho J. Promoting HPV vaccination online: message design and media choice. Health Promot Pract. 2017;18:645–53. doi: 10.1177/1524839916688229. [DOI] [PubMed] [Google Scholar]
- 100.Plunkett F, Ryan M. How we used social media to increase HPV vaccination rates. [Accessed 2018 December1]. https://www.hse.ie/eng/about/who/communications/digital/blog/how-we-used-social-media-to-increase-hpv-vaccination-rates.html.
- 101.Lai CY, Wu WW, Tsai SY, Cheng SF, Lin KC, Liang SY. The effectiveness of a facebook-assisted teaching method on knowledge and attitudes about cervical cancer prevention and HPV vaccination intention among female adolescent students in Taiwan. Health Educ Behav. 2015;42:352–60. doi: 10.1177/1090198114558591. [DOI] [PubMed] [Google Scholar]
- 102.Danish Health Authority Stop HPV – stop cervical cancer. [Accessed 2019 February19]. http://www.stophpv.dk/.
- 103.Antonio Ferro AO, Siddu A, Colucci M, Anello P, Longone M, Marcon E, Castiglia P, Bonanni P, Signorelli C. Monitoring the web to support vaccine coverage: results of two years of the portal VaccinarSì. Epidemiol Prev. 2015;39:88–93. [PubMed] [Google Scholar]
- 104.Corcoran B, Clarke A, Barrett T. Rapid response to HPV vaccination crisis in Ireland. Lancet. 2018;391:2103. doi: 10.1016/S0140-6736(18)30302-7. [DOI] [PubMed] [Google Scholar]
- 105.Suppli CH, Hansen ND, Rasmussen M, Valentiner-Branth P, Krause TG, Mølbak K. Decline in HPV-vaccination uptake in Denmark – the association between HPV-related media coverage and HPV-vaccination. BMC Public Health. 2018;18:1360. doi: 10.1186/s12889-018-6268-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.World Health Organization Denmark campaign rebuilds confidence in HPV vaccination. [Accessed 2019 February11]. https://www.who.int/features/2018/hpv-vaccination-denmark/en/.
- 107.Oak Ridge Associated Universities. Assisting CDC in national HPV immunization campaign [Accessed 2019 February11]. https://www.orau.org/impact/health-communication/national-hpv-immunization-campaign.html.
- 108.Centers for Disease Control and Prevention. YouTube Channel [Accessed 2019 February11]. https://www.youtube.com/user/CDCStreamingHealth.
- 109.Lechuga J, Swain GR, Weinhardt LS. Impact of framing on intentions to vaccinate daughters against HPV: a cross-cultural perspective. Ann Behav Med. 2011;42:221–26. doi: 10.1007/s12160-011-9273-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ahlers-Schmidt CR, Chesser A, Hart T, Paschal A, Nguyen T, Wittler RR. Text messaging immunization reminders: feasibility of implementation with low-income parents. Prev Med. 2010;50:306–07. doi: 10.1016/j.ypmed.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 111.Hofstetter AM, Vargas CY, Kennedy A, Kitayama K, Stockwell MS. Parental and provider preferences and concerns regarding text message reminder/recall for early childhood vaccinations. Prev Med. 2013;57:75–80. doi: 10.1016/j.ypmed.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 112.Roberts JR, Morella K, Dawley EH, Madden CA, Jacobson RM, Pope C, Davis B, Thompson D, O’Brien ES, Darden PM. Direct-to-adolescent text messaging for vaccine reminders: what will parents permit? Vaccine. 2018;36:2788–93. doi: 10.1016/j.vaccine.2018.03.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Rand CM, Blumkin A, Vincelli P, Katsetos V, Szilagyi PG. Parent preferences for communicating with their adolescent‘s provider using new technologies. J Adolesc. Health. 2015;57:299–304. doi: 10.1016/j.jadohealth.2015.06.006. [DOI] [PubMed] [Google Scholar]
- 114.Ludwick DA, Doucette J. Adopting electronic medical records in primary care: lessons learned from health information systems implementation experience in seven countries. Int J Med Inform. 2009;78:22–31. doi: 10.1016/j.ijmedinf.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 115.Staroselsky M, Volk LA, Tsurikova R, Pizziferri L, Lippincott M, Wald J, Bates DW. Improving electronic health record (EHR) accuracy and increasing compliance with health maintenance clinical guidelines through patient access and input. Int J Med Inform. 2006;75:693–700. doi: 10.1016/j.ijmedinf.2005.10.004. [DOI] [PubMed] [Google Scholar]
- 116.Humiston SG, Serwint JR, Szilagyi PG, Vincelli PA, Dhepyasuwan N, Rand CM, Schaffer SJ, Blumkin AK, Curtis CR. Increasing adolescent immunization rates in primary care: strategies physicians use and would consider implementing. Clin Pediatr (Phila). 2013;52:710–20. doi: 10.1177/0009922813483359. [DOI] [PubMed] [Google Scholar]
- 117.World Health Organization World health organization youtube channel. [Accessed 2019 February25]. https://www.youtube.com/user/who.
- 118.World Health Organization World Health Organization Facebook Page. [Accessed 2019 February25]. https://www.facebook.com/WHO/.
- 119.World Health Organization World Health Organization Instagram Page. [Accessed 2019 February25]. https://www.instagram.com/who/.
- 120.McKee C, Bohannon K. Exploring the reasons behind parental refusal of vaccines. J Pediatr Pharmacol Ther. 2016;21:104–09. doi: 10.5863/1551-6776-21.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Glanz JM, Wagner NM, Narwaney KJ, Kraus CR, Shoup JA, Xu S, O'Leary ST, Omer SB, Geason KS, Daley MF. Web-based social media intervention to increase vaccine acceptance: a randomized controlled trial. Pediatrics. 2017;140:e20171117. doi: 10.1542/peds.2017-0685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.George DR, Rovniak LS, Kraschnewski JL. Dangers and opportunities for social media in medicine. Clin Obstet Gynecol. 2013;56:453–62. doi: 10.1097/GRF.0b013e318297dc38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.American Academy of Pedaitrics. AAP Vaccine Communication [Accessed 2018 December2]. https://www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/immunizations/HPV-Champion-Toolkit/Pages/Public-Communication.aspx.
- 124.Cervical Cancer Free Coalition. Social Media Toolkit [Accessed 2018 December2http://www.cervicalcancerfreecoalition.org/wp-content/uploads/HPVReport-Social-Media-Toolkit.pdf.
- 125.New York State Department of Health. HPV Vaccine is Cancer Prevention Toolkit [Accessed 2018 December2]. https://www.health.ny.gov/diseases/communicable/human_papillomavirus/docs/hpv_toolkit.pdf.
- 126.Centers for Disease Control and Prevention. World Immunization Week Social Media Toolkit [Accessed 2018 December2]. https://www.cdc.gov/globalhealth/socialmedia/toolkits/global-world-immunization-week.html.
- 127.Centers for Disease Control and Prevention. CDC Social Media Tools, Guidelines & Best Practices: The Health Communicator’s Social Media Toolkit [Accessed 2018 December2]. https://www.cdc.gov/socialmedia/tools/guidelines/socialmediatoolkit.html.
- 128.Antheunis ML, Tates K, Nieboer TE. Patients‘ and health professionals‘ use of social media in health care: motives, barriers and expectations. Patient Educ Couns. 2013;92:426–31. doi: 10.1016/j.pec.2013.06.020. [DOI] [PubMed] [Google Scholar]
- 129.New York Citywide Immunization Registry. Brief Text Messaging Guide [Accessed 2018 December31] http://www1.nyc.gov/assets/doh/downloads/pdf/cir/txt-messaging-guide.pdf.
- 130.Embi PJ, Leonard AC. Evaluating alert fatigue over time to EHR-based clinical trial alerts: findings from a randomized controlled study. J Am Med Inf Assoc. 2012;19:e145–8. doi: 10.1136/amiajnl-2011-000743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Dixon BE, Kasting ML, Wilson S, Kulkarni A, Zimet GD, Downs SM. Health care providers‘ perceptions of use and influence of clinical decision support reminders: qualitative study following a randomized trial to improve HPV vaccination rates. BMC Med Inform Decis Mak. 2017;17:119. doi: 10.1186/s12911-017-0521-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zimet G, Dixon BE, Xiao S, Tu W, Kulkarni A, Dugan T, Sheley M, Downs SM. Simple and elaborated clinician reminder prompts for human papillomavirus vaccination: a randomized clinical trial. Acad Pediatr. 2018;18:S66–S71. doi: 10.1016/j.acap.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 133.Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010;25:661–69. doi: 10.1080/10410236.2010.521906. [DOI] [PubMed] [Google Scholar]
- 134.Lama Y, Chen T, Dredze M, Jamison A, Quinn SC, Broniatowski DA. Discordance between human papillomavirus twitter images and disparities in human papillomavirus risk and disease in the United States: mixed-methods analysis. J Med Internet Res. 2018;20:e10244. doi: 10.2196/10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Vorsters A, Arbyn M, Baay M, Bosch X, de Sanjose S, Hanley S, Karafillakis E, Lopalco PL, Pollock KG, Yarwood J, et al. Overcoming barriers in HPV vaccination and screening programs. Papillomavirus Res. 2017;4:45–53. doi: 10.1016/j.pvr.2017.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kata A. A postmodern Pandora‘s box: anti-vaccination misinformation on the Internet. Vaccine. 2010;28:1709–16. doi: 10.1016/j.vaccine.2009.12.022. [DOI] [PubMed] [Google Scholar]
- 137.Kata A. Anti-vaccine activists, Web 2.0, and the postmodern paradigm – an overview of tactics and tropes used online by the anti-vaccination movement. Vaccine. 2012;30:3778–89. doi: 10.1016/j.vaccine.2011.11.112. [DOI] [PubMed] [Google Scholar]
- 138.Schmidt AL, Zollo F, Scala A, Betsch C, Quattrociocchi W. Polarization of the vaccination debate on Facebook. Vaccine. 2018;36:3606–12. doi: 10.1016/j.vaccine.2018.05.040. [DOI] [PubMed] [Google Scholar]
- 139.Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. 2018;359:1146–51. doi: 10.1126/science.aap9559. [DOI] [PubMed] [Google Scholar]
- 140.Margolis MA, Brewer NT, Shah PD, Calo WA, Gilkey MB. Stories about HPV vaccine in social media, traditional media, and conversations. Prev Med. 2018;118:251–56. doi: 10.1016/j.ypmed.2018.11.005. [DOI] [PubMed] [Google Scholar]
- 141.Jolley D, Douglas KM. The effects of anti-vaccine conspiracy theories on vaccination intentions. PLoS One. 2014;9:e89177. doi: 10.1371/journal.pone.0089177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Betsch C, Brewer NT, Brocard P, Davies P, Gaissmaier W, Haase N, Leask J, Renkewitz F, Renner B, Reyna VF, et al. Opportunities and challenges of Web 2.0 for vaccination decisions. Vaccine. 2012;30:3727–33. doi: 10.1016/j.vaccine.2012.02.025. [DOI] [PubMed] [Google Scholar]
- 143.Warner EL, Ding Q, Pappas LM, Henry K, Kepka D. White, affluent, educated parents are least likely to choose HPV vaccination for their children: a cross-sectional study of the National Immunization Study - teen. BMC Pediatr. 2017;17:200. doi: 10.1186/s12887-017-0969-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Kang GJ, Ewing-Nelson SR, Mackey L, Schlitt JT, Marathe A, Abbas KM, Swarup S. Semantic network analysis of vaccine sentiment in online social media. Vaccine. 2017;35:3621–38. doi: 10.1016/j.vaccine.2017.05.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Shapiro GK, Surian D, Dunn AG, Perry R, Kelaher M. Comparing human papillomavirus vaccine concerns on Twitter: a cross-sectional study of users in Australia, Canada and the UK. BMJ Open. 2017;7:e016869. doi: 10.1136/bmjopen-2017-016869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Du J, Xu J, Song H, Liu X, Tao C. Optimization on machine learning based approaches for sentiment analysis on HPV vaccines related tweets. J Biomed Semantics. 2017;8:9. doi: 10.1186/s13326-017-0120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Du J, Xu J, Song HY, Tao C. Leveraging machine learning-based approaches to assess human papillomavirus vaccination sentiment trends with Twitter data. BMC Med Inform Decis Mak. 2017;17:69. doi: 10.1186/s12911-017-0469-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Keim-Malpass J, Mitchell EM, Sun E, Kennedy C. Using twitter to understand public perceptions regarding the #HPV vaccine: opportunities for public health nurses to engage in social marketing. Public Health Nurs. 2017;34:316–23. doi: 10.1111/phn.12318. [DOI] [PubMed] [Google Scholar]
- 149.Massey PM, Leader A, Yom-Tov E, Budenz A, Fisher K, Klassen AC. Applying multiple data collection tools to quantify human papillomavirus vaccine communication on twitter. J Med Internet Res. 2016;18:e318. doi: 10.2196/jmir.6670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Surian D, Nguyen DQ, Kennedy G, Johnson M, Coiera E, Dunn AG. Characterizing twitter discussions about hpv vaccines using topic modeling and community detection. J Med Internet Res. 2016;18:e232. doi: 10.2196/jmir.6045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Basch CH, Hillyer GC, Berdnik A, Basch CE. YouTube videos related to human papillomavirus: the need for professional communication. Int J Adolesc Med Health. 2018;30:890–907. doi:10.1515/ijamh-2015-0122. [DOI] [PubMed] [Google Scholar]
- 152.Bahk CY, Cumming M, Paushter L, Madoff LC, Thomson A, Brownstein JS. Publicly available online tool facilitates real-time monitoring of vaccine conversations and sentiments. Health Aff (Millwood). 2016;35:341–47. doi: 10.1377/hlthaff.2015.1092. [DOI] [PubMed] [Google Scholar]
- 153.Zhou XJ, Coiera E, Tsafnat G, Arachi D, Ong MS, Dunn AG. Using social connection information to improve opinion mining: identifying negative sentiment about HPV vaccines on Twitter. Stud Health Technol. 2015;216:761–65. [PubMed] [Google Scholar]
- 154.Mahoney LM, Tang T, Ji K, Ulrich-Schad J. The digital distribution of public health news surrounding the human papillomavirus vaccination: a longitudinal infodemiology study. JMIR Public Health Surveill. 2015;1:e2. doi: 10.2196/publichealth.4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Dunn AG, Surian D, Leask J, Dey A, Mandl KD, Coiera E. Mapping information exposure on social media to explain differences in HPV vaccine coverage in the United States. Vaccine. 2017;35:3033–40. doi: 10.1016/j.vaccine.2017.04.060. [DOI] [PubMed] [Google Scholar]
- 156.Tangherlini TR, Roychowdhury V, Glenn B, Crespi CM, Bandari R, Wadia A, Falahi M, Ebrahimzadeh E, Bastani R. “Mommy Blogs” and the vaccination exemption narrative: results from a machine-learning approach for story aggregation on parenting social media sites. JMIR Public Health Surveill. 2016;2:e166. doi: 10.2196/publichealth.6586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Getman R, Helmi M, Roberts H, Yansane A, Cutler D, Seymour B. Vaccine hesitancy and online information: the influence of digital networks. Health Educ Behav. 2018;45:599–606. doi: 10.1177/1090198117739673. [DOI] [PubMed] [Google Scholar]
- 158.World Health Organization How to respond to vocal vaccine deniers in public. [Accessed 2019 Feb 27]. http://www.euro.who.int/__data/assets/pdf_file/0005/315761/Best-practice-guidance-respond-vocal-vaccine-deniers-public.pdf
- 159.Nyhan B, Reifler J, Richey S, Freed GL. Effective messages in vaccine promotion: a randomized trial. Pediatrics. 2014;133:e835. doi: 10.1542/peds.2013-2112. [DOI] [PubMed] [Google Scholar]
- 160.Frier S. Facebook, Facing Lawmaker Questions, Says it may remove anti-vaccine recommendations. [Accessed 2019 February27]. https://www.bloomberg.com/news/articles/2019-02-14/facebook-says-it-may-remove-anti-vaccine-recommendations.
- 161.Sands M. Is youtube right to demonetize anti-vax channels? [Accessed 2019 March1]. https://www.forbes.com/sites/masonsands/2019/02/25/is-youtube-right-to-demonetize-anti-vax-channels/#4ea84aa914ce.
- 162.Caron C. Pinterest restricts vaccine search results to curb spread of misinformation. [Accessed 2019 February25]. https://www.nytimes.com/2019/02/23/health/pinterest-vaccination-searches.html.
- 163.Mennemeyer ST, Menachemi N, Rahurkar S, Ford EW. Impact of the HITECH Act on physicians‘ adoption of electronic health records. J Am Med Inf Assoc. 2016;23:375–79. doi: 10.1093/jamia/ocv103. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Pew Research Center Mobile Fact Sheet. [Accessed 2018 December9]http://www.pewinternet.org/fact-sheet/mobile/.


