Abstract
Purpose
To characterize functional complaints of new low-vision rehabilitation patients.
Design
Prospective observational study.
Participants
The Low Vision Rehabilitation Outcomes Study recruited 819 patients between 2008 and 2011 from 28 clinical centers in the United States.
Methods
New patients referred for low-vision rehabilitation were asked, “What are your chief complaints about your vision?” before their appointment. Full patient statements were transcribed as free text. Two methods assessed whether statements indicated difficulty in each of 13 functional categories: (1) assessment by 2 masked clinicians reading the statement, and (2) a computerized search of the text for specific words or word fragments. Logistic regression models were used to predict the influence of age, gender, and visual acuity on the likelihood of reporting a complaint in each functional category.
Main Outcome Measures
Prevalence and risk factors for patient concerns within various functional categories.
Results
Reading was the most common functional complaint (66.4% of patients). Other functional difficulties expressed by at least 10% of patients included driving (27.8%), using visual assistive equipment (17.5%), mobility (16.3%), performing in-home activities (15.1%), lighting and glare (11.7%), and facial recognition and social interactions (10.3%). Good agreement was noted between the masked clinician graders and the computerized algorithm for categorization of functional complaints (median κ of 0.84 across the 13 categories). Multivariate logistic regression models demonstrated that the likelihood of reading difficulties increased mildly with age (odds ratio, 1.4 per 10-year increment in age; 95% confidence interval, 1.3–1.6), but did not differ with visual acuity (P = 0.09). Additionally, men were more likely to report driving difficulties and difficulties related to lighting, whereas women were more likely to report difficulty with either in-home activities or facial recognition or social interaction (P<0.05 for all). Mobility concerns, defined as walking difficulty and out-of-home activities, showed no relationship to gender, age, or visual acuity.
Conclusions
Reading was the most commonly reported difficulty, regardless of the patient’s diagnosis. Neither visual acuity nor gender were predictive of reading concerns, although, age showed a small effect. Addressing reading rehabilitation should be a cornerstone of low-vision therapy.
Patients seeking low-vision rehabilitation (LVR) have chronic visual impairments that limit their ability to participate in daily activities. These patients have a broad range of vision-mediated functional limitations, lower quality of life, and decreased independence.1–8 Depending on the visual acuity (VA) criteria used (≤20/70 or <20/40), studies estimate that 1.5 or 3.5 million Americans older than 40 years of age, respectively, have low vision.9,10 The prevalence of vision impairment is even greater in patients older than 65 years of age. Given the predicted growth of this age group, LVR will become an even more essential part of routine ophthalmic care.11
Low-vision rehabilitation is individualized for each patient’s functional goals12; yet to date, there is little detail on the prevalence of different functional concerns in patients seeking outpatient low-vision services. Recognition of common rehabilitative needs will provide researchers and clinicians direction in the development and planning of LVR outcome measurements and rehabilitation strategies necessary to address the growing demand of the visually impaired population. Targeted and effective rehabilitation therapies can enable patients with chronic visual impairment to improve activities of daily living and overall quality of life.13
The Low Vision Rehabilitation Outcomes Study14 was designed to characterize typical patients seeking LVR in the United States and offers a unique opportunity to identify the rehabilitation priorities in these patients. In this prospective observational study, new low-vision patients seeking treatment at 1 of 28 clinical centers in the United States provided a complaint statement regarding their reason for seeking low-vision services. We categorized the difficulties voiced in these complaint statements, thus defining the primary functional categories in which patients seeking LVR services expected improvement in their daily function.
Methods
The study protocol was approved by The Johns Hopkins Institutional Review Board and adhered to the Declaration of Helsinki. When required, each study site obtained separate institutional review board approval. All participants signed a contact authorization and were contacted by the coordinating center at The Johns Hopkins University. Research assistants described the study and obtained oral consent on the telephone.
Subjects
Low Vision Rehabilitation Outcomes Study participants were recruited into this prospective, observational study from 1 of 28 clinical centers across the United States. Eight hundred nineteen participants were identified from new patients scheduling a low-vision appointment between April 25, 2008, and May 2, 2011. Eligible patients were older than 18 years of age, able to communicate in English over the telephone, and had not received low-vision services in the previous 3 years. Complaint statements were transcribed by research assistants from 535 women (66.4%) and 271 men (33.6%). Median participant age was 77 years, ranging from 18 to 110 years (standard deviation, 16.1 years). The mean VA in this sample was 0.68 logarithm of the minimum angle of resolution (logMAR) units (Snellen equivalent, 20/96), with a standard deviation of 0.50 logMAR. Median VA was 0.60 logMAR (Snellen equivalent, 20/80), with the interquartile range extending from 0.4 to 1.0 logMAR (95% confidence interval [CI], 0.64–0.72). The primary ocular diagnosis was commensurate with macular disease in the eye with the better habitual VA in 55% of the patients. No VA, visual field, or diagnosis exclusions were used because the goal was to capture a typical distribution of patients seeking LVR services.14
Categorization of Functional Complaints
Patients completed a phone interview before their initial low-vision assessment appointment and were administered several questionnaires, including an intake survey. This intake survey comprised 1 open-ended question about functional concerns followed by standardized check-box questions detailing ocular, medical, physical, psychological, and social history.14 For the open-ended question, patients were asked, “What are your chief complaints about your vision?” Interviewers transcribed patients’ statements as free text. Patients were encouraged to describe functional difficulties resulting from their vision.
Free-text complaint statements were categorized by 2 methods. First, 2 clinicians (J.G. and T.C.) specializing in LVR reviewed each participant’s statement independently and coded each complaint statement using any number of the 13 functional categories characterized in Table 1. All disagreements in categorization between the 2 reviewers were discussed, and a final decision was determined for each patient’s complaint statement by consensus. Second, a computerized algorithm was used to search participants’ transcribed statements using a set of standardized query terms created by a third clinician (P.R.) independent from the other graders (Table 1). This computerized coding by search terms was conducted to corroborate objectively the coding dictated by the 2 low-vision specialists. Finally, the functional codes were analyzed against patients’ primary ocular diseases as defined by the ninth edition of the International Classification of Diseases (ICD-9).
Table 1.
Categorization of Functional Complaints of a Low-Vision Population
| Complaint | Definition | Automated Search Keywords |
|---|---|---|
| Diagnosis | The patient restates their diagnosis or medical condition, or referenced their disease | glauc,* macula,* hemianopsia, amd, retin,* stargardt, choroid,* cataract* |
| Reading | Difficulty reading any type of material | read, print |
| Television | Difficulty viewing television | television, tv |
| Driving | Complains driving difficulty or cessation, or if family or doctor concern present | driv,* road, drove |
| Facial recognition and social interactions | Complains identifying faces and expressions, especially if inhibitory to social interactions | face, kids, people, son, daughter, facial, church |
| Hobby | Discretionary activities that are nonessential for independence or daily function | golf, music, sew,* art, bold (shot pool), piano, stitch, baseball, crossword, bowling, tennis, hobb,* bingo, boat, hunt, paint, garden, craft, needle, crochet, puzzle |
| Light | Difficulty with lighting (glare, sensitivity, or night blindness) that restricts function | glare, dim, dark, night, light, photosen* |
| Employment and school | Visual complaints that impact patient’s ability to work or function in school | school, blackboard, job, courses, employ, occupation, work |
| Assistive device | Complaints regarding visual assistive equipment, excluding eyeglasses | polarize, sunglass, magnif,* cctv (closed-circuit television), binocular |
| Technology | Complaints about difficulty using technology | computer, type and typing, mouse, palm pilot, kindle |
| In-home activities | Difficulty with daily activities inside the home | writ,* cook, mail, * phone, ingredients, recipes, clothes, packag,* clean, paperwork, bill,* check, yard, microwave, bath, label, oven, eat* |
| Out-of-home activities | Difficulty with daily activities requiring the patients to leave their home | getting around, getting places, shop, transportation, go out, going out, travel, leave* home, store, grocery, supermarket |
| Walking | Complaints regarding trouble walking | bump, curb, run into, step, walk, navigat,* balance, trip, fall, fell, stair, ground, moving around, o&m(orientation and mobility), terrain, maneuvering |
Indicates wildcard letters for the key word search; allows multiple permutations of the word.
Statistical Analysis
Complaint frequencies for each functional category from the clinician and automated search-generated results were calculated and κ statistic was used to test the concordance in the categorization of these results. Chi-square analyses were used to compare results across genders. Multivariate logistic regression models were used to assess the relevance of age, gender, and VA with regard to the likelihood of expressing complaints in each functional category (using the adjudicated grader analysis). Analyses were conducted in Stata software version 12 (Stata Corp, College Station, TX).
Results
The agreement between clinician graders regarding whether or not a complaint was present within each functional category was high, and κ values were greater than 0.75 for all functional categories except out-of-home activities (κ = 0.45). For most functional categories, the consensus opinion of the 2 low vision specialists and the computerized search algorithm demonstrated high agreement regarding whether a complaint within the category was present (κ > 0.7 for 10 of 13 functional categories). Slightly lower agreement was found between the grader consensus and computerized search when assessing the presence or absence of lighting complaints (κ = 0.56), difficulty with outside activities (κ = 0.59), and difficulty with in-home activities (κ = 0.63; Table 2).
Table 2.
Frequency of Complaints in Low-Vision Patients by Automated Search versus Manual Grading*
| Type of Complaints† | Manual (%) | Keyword (%) | κ Value‡ (95% Confidence Interval) |
|---|---|---|---|
| Reading | 66.4 | 66.7 | 0.94 (0.91–0.97) |
| Driving | 27.8 | 28.8 | 0.95 (0.92–0.97) |
| Assistive device | 17.5 | 15.4 | 0.91 (0.87–0.95) |
| Diagnosis | 15.8 | 8.3 | 0.63 (0.55–0.71) |
| In-home activities | 15.1 | 16.7 | 0.63 (0.56–0.70) |
| Light related | 11.7 | 16.4 | 0.75 (0.68–0.81) |
| No complaints categorized | 11.2 | 12.5 | 0.80 (0.74–0.87) |
| Facial recognition and | 10.3 | 12.7 | 0.86 (0.80–0.91) |
| social interactions | |||
| Walking | 9.7 | 9.4 | 0.84 (0.78–0.91) |
| Hobby | 7.6 | 8.8 | 0.71 (0.62–0.8) |
| Out-of-home activities | 6.6 | 7.2 | 0.59 (0.48–0.70) |
| Technology | 5.7 | 5.7 | 0.97 (0.95–1.0) |
| Television | 5.6 | 7.3 | 0.86 (0.79–0.93) |
| Employment and school | 3.9 | 6.2 | 0.56 (0.43–0.69) |
The automated search was conducted by using keyword search terms created by a clinician independent of the 2 low-vision rehabilitation clinicians who performed manual categorization.
Each patient’s statement may be categorized under multiple complaint categories.
Reflects agreement between for the categorization determined by the computerized key word search versus the adjudicated patient statements.
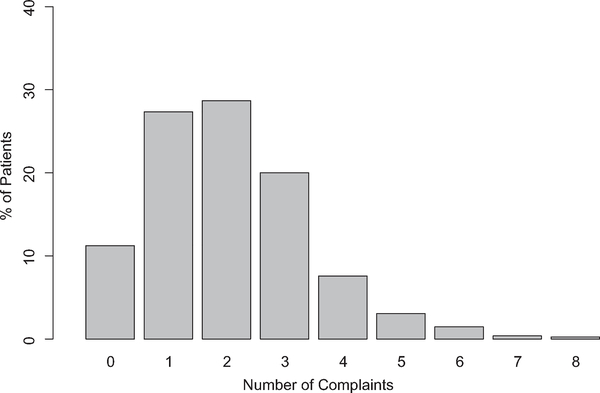
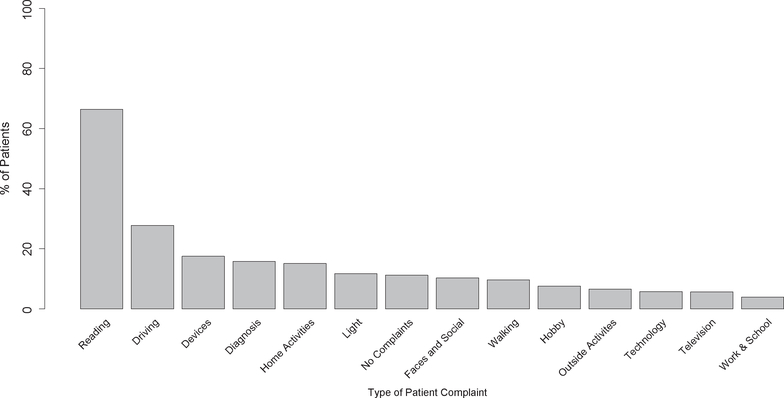
Participant statements could have complaints in 0, 1, or more than 1 functional category, and 11.2% (92/819) of patient statements did not describe a functional complaint. One functional complaint was identified in 27.4% of statements, 2 functional complaints were identified in 28.7% statements, 3 functional complaints were identified in 20% of statements, and 4 or more complaints were identified in 12.7% of patient statements (Fig 1). Overall, reading was the most frequent complaint and was reported by 544 (66.4%) of 819 patients (Fig 2). Driving concerns (228 patients; 27.8%) and the use of assistive devices (143 patients; 17.5%) were the next most commonly reported complaints. Other complaints reported by at least 10% of patients included difficulty with in-home activities (124 patients; 15.1%), lighting-related activities (96 patients; 11.7%), and recognizing faces or interacting socially (84 patients; 10.3%). Categories with less than 10% of patients included difficulties with walking, performing hobbies, using technology, watching television, doing out-of-home activities, and working- or school-related activities. Mobility-related complaints, defined as a complaint with either walking or out-of-home activities, were voiced by 133 patients (16.3%).
Figure 1.
Bar graph showing the number of functional complaints per individual in a national sample of patients seeking low-vision treatment. Data taken from 819 new low-vision patients seeking treatment at 1 of 28 clinical centers.
Figure 2.
Bar graph showing the frequency of various functional complaints among a national sample of patients seeking low-vision treatment. Data taken from 819 new low-vision patients seeking treatment at 1 of 28 clinical centers.
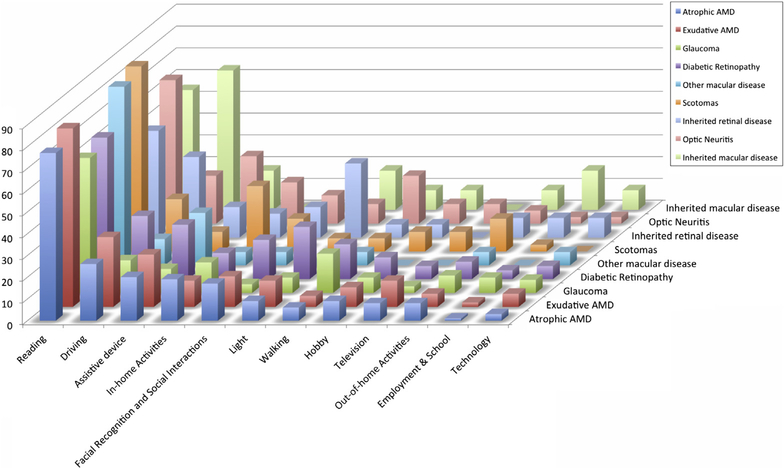
Disorder diagnoses were available in 586 of 819 patients and showed the most common primary diagnosis to be atrophic macular degeneration (ICD-9-CM code 362.51). This diagnosis was found in 25% (149/573) of patients, and 77% of these patients had reading complaints. Driving (26%) and use of assistive devices (20%) were the next most common complaints in atrophic age-related macular degeneration patients, whereas all other complaints were reported less than 20% of the time in this patient group. Similarly, in all other diagnosis categories, reading and driving were overwhelmingly the most common patient complaints (Fig 3).
Figure 3.
Bar graph showing the frequency of functional complaints by ocular disease diagnosis in a national sample of patients seeking low-vision treatment. Diagnosis defined by International Classification of Disease, Ninth Edition, coding. AMD = age-related macular degeneration.
In univariate analyses, women were more likely to report difficulty using assistive devices (19.3% vs. 13.6%; P = 0.04), performing in-home activities (18.1% vs. 9.2%; P<0.001), engaging in social activities (12.2% vs. 6.3%; P = 0.007), and walking (11.2% vs. 6.6%; P = 0.03). Men were more likely to report driving difficulty (36.2% vs. 23.6%; P<0.001) and light-related problems (14.0% vs. 10.1%; P = 0.01; Table 3). The prevalence of reading or other functional complaints was not significantly different between men and women (all P>0.06).
Table 3.
Types of Complaints* in Low-Vision Patients by Gender
| Type of Complaint | Women (%) | Men (%) | P Value |
|---|---|---|---|
| Reading | 68.6 | 62.7 | 0.097 |
| Driving | 23.6 | 36.2 | <0.001 |
| Assistive device | 19.3 | 13.6 | 0.043 |
| In-home activities | 18.1 | 9.23 | <0.001 |
| Diagnosis | 15.9 | 14.8 | 0.68 |
| Facial recognition and social interactions | 12.2 | 6.27 | 0.007 |
| Walking | 11.2 | 6.6 | 0.03 |
| Out-of-home activities | 7.9 | 4.4 | 0.06 |
| Light | 10.1 | 14.0 | 0.10 |
| Hobby | 8.6 | 5.5 | 0.11 |
| Technology | 6.2 | 5.2 | 0.56 |
| Television | 5.8 | 5.2 | 0.71 |
| Employment and school | 3.7 | 3.2 | 0.76 |
Boldface indicates P < 0.05.
Each patient’s statement may be categorized under multiple complaint codes.
In multivariate analyses, older age was associated with a greater odds of reading complaints (odds ratio [OR], 1.4 for 10-year increment in age; 95% CI, 1.3–1.6). No significant association was found between VA or gender and the presence of a reading complaint. Men had a 1.9 times greater odds of reporting a driving complaint when compared with women (95% CI, 1.3–2.8), and younger subjects also were more likely to report driving concerns than older subjects (OR, 0.87 per 10-year increment in age; 95% CI, 0.8–1.0). Assistive device complaints were more likely in older subjects as compared with younger subjects (OR, 1.3; 95% CI, 1.1–1.5), whereas complaints about using technology (OR, 0.70 per 10-year increment in age; 95% CI, 0.6–0.9) and functioning at work or school (OR, 0.74 per 10-year increment in age; 95% CI, 0.6–0.9) were less frequent with increasing age. Men were less likely to report difficulty with facial recognition and social interactions as compared with women (OR, 0.44; 95% CI, 0.2–0.8) and also were less likely to report difficulty with in-home activities compared with women (OR, 0.39; 95% CI, 0.2–0.7). Worse VA was associated with a greater likelihood of reporting difficulty with in-home activities (OR, 1.9; 95% CI, 1.3–2.9) and television watching (OR, 1.8; 95% CI, 1.0–3.2) and a lower likelihood of light-related complaints (OR, 0.5; 95% CI, 0.3–0.9). The frequency of complaints within other functional categories did not vary significantly across age, gender, or VA (Table 4).
Table 4.
Associations in Low-Vision Patient Complaints after Adjusting for Gender, Age, and Visual Acuity
| Type of Complaint | Independent Variables: Odds Ratio (95% Confidence Interval) |
||
|---|---|---|---|
| Male Gender | Age (per 10 yrs) | VA (0.1 LogMAR Worse) | |
| Reading | 0.78 (0.5–1.1) | 1.4 (1.3 –1.6) | 1.3 (1.0–2.0) |
| Driving | 1.9 (1.3–2.8) | 0.87 (0.8 –1.0) | 0.94 (0.7–1.4) |
| Assistive device | 0.74 (0.5–1.2) | 1.3 (1.1–1.5) | 1.2 (0.8–1.8) |
| In-home activities | 0.39 (0.2–0.7) | 1.2 (1.0–1.4) | 1.2 (1.3–2.9) |
| Diagnosis | 0.93 (0.6–1.4) | 0.99 (0.9–1.1) | 0.49 (0.3–0.9) |
| Facial recognition and social interactions | 0.44 (0.2–0.8) | 1.1 (0.9–1.3) | 1.4 (0.9–2.3) |
| Walking | 0.51 (0.3–1.0) | 0.9 (0.8–1.1) | 1.6 (1.0–2.6) |
| Out-of-home activities | 0.50 (0.23–1.1) | 1.1 (0.9–1.3) | 0.62 (0.3–1.3) |
| Light | 1.9 (1.2–3.2) | 0.82 (0.7–1.0) | 0.5 (0.3–0.9) |
| Hobby | 0.64 (0.3–1.3) | 1.2 (0.9–1.4) | 0.90 (0.5–1.7) |
| Technology | 0.86 (0.4–1.9) | 0.70 (0.6–0.9) | 0.61 (0.3–1.4) |
| Television | 0.99 (0.48–2.0) | 1.2 (0.9–1.6) | 1.8 (1.0–3.2) |
| Employment and school | 0.34 (0.1–1.2) | 0.74 (0.6–0.9) | 1.4 (0.6–3.2) |
logMAR = logarithm of the minimum angle of resolution; VA = visual acuity.
Boldface indicates P < 0.05.
Discussion
Reading
The current study was the first to assess systematically the chief complaints of a large group of patients seeking outpatient LVR across the United States. We found that reading difficulty was by far the most common presenting concern, characterized in the complaint statements of two-thirds of new LVR patients. This frequency was significantly greater than the frequency observed for other categories of complaints including driving, assistive devices, and in-home activities (frequency less than 30% for all). The overwhelming prevalence of reading-related concerns found in our study supports the idea that improving reading function should be the cornerstone of LVR.
Despite the extensive literature describing a strong relationship between reading ability and VA,2,15–17 we did not find an association between VA and the presence of reading complaints in this study sample. One possible explanation for this finding is that patients have deficits other than VA loss that affect their reading ability and initiate seeking low-vision services independent of VA. For example, paracentral scotomas resulting from macular disease, visual field loss resulting from glaucoma,18 or reduced contrast sensitivity or glare with discomfort resulting from corneal disease may contribute to reading difficulty even with good VA.19,20 Thus, our study corroborates previous work suggesting that VA measurements should not be the only determining factor when identifying reading concerns or referring for low-vision services. 14,21,22
A second possible explanation for the lack of association between VA and the presence of a reading complaint is that the specific reading tasks that the patients desired to perform varied across the spectrum of VA. Indeed, the term reading covers a broad range of activities with significant variability in difficulty, including sustained continuous reading of a book, magazine, or computer versus spot reading of medicine bottles, bills, or food labels.16,19,23–26 Furthermore, previous research suggests that sustained reading tasks may be significantly more affected than spot reading tasks with certain types of visual impairment.20,27 Finally, advances in technology have increased the number of formats in which reading takes place. Today, reading takes place on computer screens, tablets, e-readers, and smart phones in addition to traditional reading sources such as hard-copy magazines, newspapers, and standard large-print books; hence, reading difficulty may vary significantly across these media. Understanding the importance of reading tasks for patients’ specific needs and the required ability to achieve these diverse tasks is essential for generating evaluative measures to address all spectrums of reading tasks and for development of customized LVR protocols aimed at rehabilitating task-specific reading activities.
We did find that reading complaints became slightly more significant with older age (Table 4). Additionally, complaints regarding visual assistive equipment also increased slightly with age, although the small magnitude of these findings suggests they have limited clinical significance. Similar to previous reports,28 we did not find any associations between gender and the likelihood of reporting reading concerns, nor did we find that ocular diagnosis significantly impacted the chief complaint of patients. Rather, our findings show that reading is consistently the most common complaint among all patients seeking LVR services.
Driving
Driving difficulty was the second most common complaint and was reported in more than one quarter (28%) of low-vision patients. The severity of VA loss was not predictive of having a driving complaint, which may reflect the increased prevalence of driving cessation with worse VA.29–31 As VA declines and cessation of driving occurs, adjustment to becoming a nondriver may reduce the importance of driving as a concern, explaining our observed findings. Additionally, the relationship between VA and driving complaints may be minimized because of effective changes in driving practices that occur in low vision populations. It is estimated that one quarter to one third of patients seeking low-vision services drive and that most of these patients self-restrict their driving practices.14,31,32 Driving in familiar environments and fewer miles per week limit the need to perform more difficult behind-the-wheel tasks that require better VA, such as reading road signs, maps, and GPS devices.31 As a result of more limited driving demands and modifications in driving behavior, many patients may feel that their driving activities are manageable and not a concern that needs to be addressed.
Our findings showed that younger individuals seeking LVR were more likely to report driving complaints. This is consistent with the everyday demands of family, work, or school responsibilities requiring transportation. The median age of our sample was 77 years, and with increasing age comes the associated physical, cognitive, and psychological comorbidities that can contribute to driving cessation regardless of vision loss.33 Gender also was found to be a strong predictor of driving complaints. This effect may occur because men continue to drive despite having visual concerns, and women discontinue driving earlier.33–37 Based on these findings, it is important to query younger male patients with any level of visual impairment about their driving concerns and practices to limit risks to public safety.
Mobility
Mobility-related complaints, described as walking and out-of-home activities, were a concern in 16.3% of the sample. The concern was more evident in females; however, after adjusting for age and VA, gender was not predictive of having a mobility-related complaint. The prevalence of mobility concerns may be even greater in patients with visual impairment because other activity categories (i.e., in-home activities, hobbies) also may involve walking. Mild visual impairment and reduced physical ability notably increase the risk of falls both in and out of the home, decrease independence, and reduced quality of life. 14,33,38 Considering that the prevalence of mobility-related concerns in people with peripheral vision loss is greater than those with central loss8,38,39 and that most patients in our sample had macular disease with central visual impairment,14 our potential undersampling of diseases causing peripheral visual field loss may underestimate the impact of mobility concerns in LVR patients. It is noteworthy that the prevalence of complaints related to walking was greatest when the primary diagnosis was categorized as glaucoma, diabetic retinopathy, or optic neuritis—all of which are commonly associated with peripheral visual field loss.
The classifications of patient complaints into functional categories show good agreement between the 2 clinicians and between the clinicians and key word searches. The ability to classify functional complaints of low-vision patients consistently is essential because LVR evaluation and treatment is guided by key domains (e.g., reading, mobility) of valued activities. Complaint categorization typically is guided by clinician interview, visual function question-naires,40 or the use of item banks.41 The changes in functional ability within these domains often are used as the primary outcome measures in LVR, and our study showed that clinical categorization of complaints voiced by patients is consistent with objective computerized methods to categorize complaints.
Our assessments of reading and other functional complaints were free form, so we could not report detailed information about patients’ functional ability. Additionally, complaint statements do not specify particular subtasks, for example, reading books versus computer reading versus reading medicine bottles. Different reading tasks may be affected at different stages of vision loss, perhaps explaining the lack of relationship between VA and reading complaints in the current study, whereas an extensive literature describes a strong association between visual acuity and reading ability.16,19,33,42 Our large sample size with geographic diversity provided generalizability to our characterization of the typical patient seeking low-vision services in the United States, although different findings may be found in other countries.
The predominance of reading complaints in low-vision patients and high reading demands as part of everyday activities in the United States necessitate careful consideration in attending to patient concerns regardless of their level of VA or gender. Patients seeking outpatient LVR may have multiple concerns that require discussion and evaluation because of the potential health (e.g., falls) and public safety consequences (e.g., driving). Development of new technology and approaches to reading rehabilitation should remain a directive in ongoing research to address the reading demands of patients with vision loss.
Supplementary Material
Acknowledgments
Supported by the National Institutes of Health, Bethesda, MD (grant nos.: EY018595, EY012045, and EY018696); Reader’s Digest Partners for Sight, Mt. Kisco, NY; Foundation for Research to Prevent Blindness; and the Doris Duke Charitable Foundation, New York, NY. The funding organizations had no role in the design or conduct of this research.
Abbreviations and Acronyms
- CI
confidence interval
- logMAR
logarithm of the minimum angle of resolution
- LVR
low-vision rehabilitation
- OR
odds ratio
- VA
visual acuity
Footnotes
Financial Disclosure(s):
The author(s) have no proprietary or commercial interest in any materials discussed in this article.
A complete listing of the members of the Low Vision Research Network Study Group is available at www.aaojournal.org.
Supplemental material is available at www.aaojournal.org.
References
- 1.Fylan F, Morrison-Fokken A, Grunfeld EA. Focus-QoL: measuring quality of life in low vision. Int Congr Ser 2005;1282:549–53. [Google Scholar]
- 2.Massof RW, Fletcher DC. Evaluation of the NEI visual functioning questionnaire as an interval measure of visual ability in low vision. Vision Res 2001;41:397–413. [DOI] [PubMed] [Google Scholar]
- 3.Brabyn J, Schneck M, Haegerstrom-Portnoy G, Lott L. The Smith-Kettlewell Institute (SKI) longitudinal study of vision function and its impact among the elderly: an overview. Optom Vis Sci 2001;78:264–9. [DOI] [PubMed] [Google Scholar]
- 4.Cahill MT, Banks AD, Stinnett SS, Toth CA. Vision-related quality of life in patients with bilateral severe age-related macular degeneration. Ophthalmology 2005;112:152–8. [DOI] [PubMed] [Google Scholar]
- 5.Kupfer C The National Eye Institute’s low vision education program: improving quality of life. Ophthalmology 2000;107:229–30. [DOI] [PubMed] [Google Scholar]
- 6.Gormezano SR. Promoting independence through low vision rehabilitation. Optometry 2005;76:327–31. [DOI] [PubMed] [Google Scholar]
- 7.Latham K, Usherwood C. Assessing visual activities of daily living in the visually impaired. Ophthalmic Physiol Opt 2010;30:55–65. [DOI] [PubMed] [Google Scholar]
- 8.Ramulu P Glaucoma and disability: which tasks are affected, and at what stage of disease? Curr Opin Ophthalmol 2009;20:92–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Eye Diseases Prevalence Research Group. Causes and prevalence of visual impairment among adults in the United States. Arch Ophthalmol 2004;122:477–85. [DOI] [PubMed] [Google Scholar]
- 10.Massof RW. A model of the prevalence and incidence of low vision and blindness among adults in the U.S. Optom Vis Sci 2002;79:31–8. [DOI] [PubMed] [Google Scholar]
- 11.Population Projections of the United States by Age, Sex, Race, and Hispanic Origin: 1995 to 2050. U.S. Bureau of the Census, Current Population Reports, P25–1130. Washington, D.C.: U. S. Government Printing Office; 1996:7–8. Available at: http://www.census.gov/prod/1/pop/p25-1130.pdf. Accessed January 21, 2014. [Google Scholar]
- 12.Massof RW. A systems model for low vision rehabilitation. I. Basic concepts. Optom Vis Sci 1995;72:725–36. [DOI] [PubMed] [Google Scholar]
- 13.Stelmack JA, Tang XC, Reda DJ, et al. LOVIT Study Group. Outcomes of the Veterans Affairs Low Vision Intervention Trial (LOVIT). Arch Ophthalmol 2008;126:608–17. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein JE, Massof RW, Deremeik JT, et al. ; Low Vision Research Network Study Group. Baseline traits of low vision patients served by private outpatient clinical centers in the United States. Arch Ophthalmol 2012;130:1028–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Legge GE, Ahn SJ, Klitz TS, Luebker A. Psychophysics of reading—XVI. The visual span in normal and low vision. Vision Res 1997;37:1999–2010. [DOI] [PubMed] [Google Scholar]
- 16.Turco PD, Connolly J, McCabe P, Glynn RJ. Assessment of functional vision performance: a new test for low vision patients. Ophthalmic Epidemiol 1994;1:15–25. [DOI] [PubMed] [Google Scholar]
- 17.Tabrett DR, Latham K. Factors influencing self-reported vision-related activity limitation in the visually impaired. Invest Ophthalmol Vis Sci 2011;52:5293–302. [DOI] [PubMed] [Google Scholar]
- 18.Legge GE, Rubin GS, Pelli DG, Schleske MM. Psychophysics of reading: II. Low vision. Vision Res 1985;25: 253–65. [DOI] [PubMed] [Google Scholar]
- 19.West SK, Rubin GS, Munoz B, et al. ; Salisbury Eye Evaluation Project Team. Assessing functional status: correlation between performance on tasks conducted in a clinic setting and performance on the same task conducted at home. J Gerontol A Biol Sci Med Sci 1997;52:M209–17. [DOI] [PubMed] [Google Scholar]
- 20.Ramulu PY, Swenor BK, Jefferys JL, et al. Difficulty with out-loud and silent reading in glaucoma. Invest Ophthalmol Vis Sci 2013;54:666–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rubin GS, Bandeen-Roche K, Huang GH, et al. ; SEE Project Team. The association of multiple visual impairments with self-reported visual disability: SEE project. Invest Ophthalmol Vis Sci 2001;42:64–72. [PubMed] [Google Scholar]
- 22.West SK, Munoz B, Rubin GS, et al. ; SEE Project Team. Function and visual impairment in a population-based study of older adults. The SEE project. Invest Ophthalmol Vis Sci 1997;38:72–82. [PubMed] [Google Scholar]
- 23.Szlyk JP, Seiple W, Fishman GA, et al. Perceived and actual performance of daily tasks: relationship to visual function tests in individuals with retinitis pigmentosa. Ophthalmology 2001;108:65–75. [DOI] [PubMed] [Google Scholar]
- 24.Haymes SA, Johnston AW, Heyes AD. The development of the Melbourne low-vision ADL index: a measure of vision disability. Invest Ophthalmol Vis Sci 2001;42:1215–25. [PubMed] [Google Scholar]
- 25.Owsley C, Sloane M, McGwin G Jr, Ball K. Timed instrumental activities of daily living tasks: relationship to cognitive function and everyday performance assessments in older adults. Gerontology 2002;48:254–65. [DOI] [PubMed] [Google Scholar]
- 26.Dougherty BE, Martin SR, Kelly CB, et al. Development of a battery of functional tests for low vision. Optom Vis Sci 2009;86:955–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramulu PY, Swenor BK, Jefferys JL, Rubin GS. Description and validation of a test to evaluate sustained silent reading. Invest Ophthalmol Vis Sci 2013;54:673–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hazel CA, Petre KL, Armstrong RA, et al. Visual function and subjective quality of life compared in subjects with acquired macular disease. Invest Ophthalmol Vis Sci 2000;41: 1309–15. [PubMed] [Google Scholar]
- 29.Scilley K, Jackson GR, Cideciyan AV, et al. Early age-related maculopathy and self-reported visual difficulty in daily life. Ophthalmology 2002;109:1235–42. [DOI] [PubMed] [Google Scholar]
- 30.Owsley C, McGwin G Jr. Vision impairment and driving. Surv Ophthalmol 1999;43:535–50. [DOI] [PubMed] [Google Scholar]
- 31.Massof RW, Deremeik JT, Park WL, Grover LL. Self-reported importance and difficulty of driving in a low-vision clinic population. Invest Ophthalmol Vis Sci 2007;48: 4955–62. [DOI] [PubMed] [Google Scholar]
- 32.DeCarlo DK, Scilley K, Wells J, Owsley C. Driving habits and health-related quality of life in patients with age-related maculopathy. Optom Vis Sci 2003;80:207–13. [DOI] [PubMed] [Google Scholar]
- 33.Freeman EE, Munoz B, Turano KA, West SK. Measures of visual function and time to driving cessation in older adults. Optom Vis Sci 2005;82:765–73. [DOI] [PubMed] [Google Scholar]
- 34.Miljanovic B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol 2007;143:409–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Segal-Gidan F, Varma R, Salazar X, Mack WJ. Factors influencing driving status in an older Latino population. J Aging Health 2010;22:332–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Popescu ML, Boisjoly H, Schmaltz H, et al. Age-related eye disease and mobility limitations in older adults. Invest Ophthalmol Vis Sci 2011;52:7168–74. [DOI] [PubMed] [Google Scholar]
- 37.Brabyn JA, Schneck ME, Lott LA, Haegerstrom-Portnoy G. Night driving self-restriction: vision function and gender differences. Optom Vis Sci 2005;82:755–64. [DOI] [PubMed] [Google Scholar]
- 38.Willis JR, Vitale SE, Agrawal Y, Ramulu PY. Visual impairment, uncorrected refractive error, and objectively measured balance in the United States. JAMA Ophthalmol 2013;131:1049–56. [DOI] [PubMed] [Google Scholar]
- 39.Friedman DS, Freeman E, Munoz B, et al. Glaucoma and mobility performance: the Salisbury Eye Evaluation Project. Ophthalmology 2007;114:2232–7. [DOI] [PubMed] [Google Scholar]
- 40.Mangione CM, Lee PP, Pitts J, et al. ; NEI-VFQ Field Test Investigators. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). Arch Ophthalmol 1998;116:1496–504. [DOI] [PubMed] [Google Scholar]
- 41.Pesudovs K Item banking: a generational change in patient-reported outcome measurement. Optom Vis Sci 2010;87: 285–93. [DOI] [PubMed] [Google Scholar]
- 42.Massof RW, Ahmadian L, Grover LL, et al. The Activity Inventory: an adaptive visual function questionnaire. Optom Vis Sci 2007;84:763–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.