A 15-minute intervention in PC can benefit adolescents with more severe alcohol and marijuana use 1 year later compared with UC.
Abstract
BACKGROUND AND OBJECTIVES:
The primary care (PC) setting provides an opportunity to address adolescent alcohol and marijuana use. We examined moderators of effectiveness for a PC brief motivational intervention on adolescents’ alcohol and marijuana use and consequences 1 year later.
METHODS:
We conducted a randomized controlled trial in 4 PC clinics from April 2013 to November 2015 and followed adolescents using Web-based surveys. We examined whether demographic factors and severity of use moderated 12-month outcomes. Adolescents aged 12 through 18 were screened by using the National Institute on Alcohol Abuse and Alcoholism Screening Guide. Those identified as at risk were randomly assigned to the intervention (CHAT) or to usual care (UC).
RESULTS:
The sample (n = 294) was 58% female, 66% Hispanic, 17% African American, 12% white, and 5% multiethnic or of other race with an average age of 16 years. After controlling for baseline values of outcomes, teens in CHAT who reported more negative consequences from drinking or had an alcohol use disorder at baseline reported less alcohol use, heavy drinking, and consequences 1 year later compared with teens in UC. Similarly, teens in CHAT with more negative consequences from marijuana use at baseline reported less marijuana use 1 year later compared with teens in UC; however, teens in CHAT who reported fewer marijuana consequences at baseline reported greater marijuana use 1 year later compared with teens in UC.
CONCLUSIONS:
A brief intervention can be efficacious over the long-term for adolescents who report problems from alcohol and marijuana use. Findings emphasize the importance of both screening and intervention in at-risk adolescents in PC.
What’s Known on the Subject:
Adolescents with alcohol and marijuana use problems do not typically access services to change their use. Brief interventions in primary care can reach many at-risk teens and have been shown to reduce both use and consequences.
What This Study Adds:
This study examined moderators of intervention effectiveness for alcohol and marijuana use. Teens receiving brief interventions in primary care with greater severity of use (eg, numerous consequences) were more likely to reduce use and consequences 1 year later compared with those in usual care.
In 2016, only 11% of US adolescents aged 12 to 17 with a substance use disorder received treatment.1 Untreated substance use disorders are associated with high-risk behaviors (eg, driving under the influence) and substantial negative consequences, including premature mortality.2 Substance use is a leading contributor to the global burden of disease among youth3; thus, it is crucial to increase early-intervention services to identify and counsel adolescents before more serious problems occur.
The primary care (PC) setting offers a unique opportunity to identify adolescents at risk for substance use.4 Most adolescents receive medical preventive services5 at well-child checkups, with ∼80% of US adolescents receiving an annual checkup.6 These visits consist of interactions to promote health, offering teachable moments when adolescents may be more receptive to information intended to reduce risk behaviors.7
Screening and brief intervention for substance use still occurs infrequently in PC8,9; however, evidence increasingly supports the efficacy of these services. Studies have found positive short-term effects of brief intervention in PC and the emergency department (ED)10–13; however, evidence is mixed for long-term outcomes.14 One randomized trial in PC compared a brief in-person intervention to a computerized intervention for adolescents ages 12 to 18 who reported marijuana use and for those who did not. No intervention effects were found 1 year later on alcohol or marijuana use for teens who reported using marijuana.12 For nonusing teens, although prevalence of use did not differ at each time point, the cumulative prevalence over 12 months was significantly lower for intervention teens compared with control teens.5
Some ED studies have tried to elucidate characteristics of adolescents who are more likely to benefit from brief interventions. Findings have focused on alcohol use and suggest that adolescents with more severe problems, higher self-efficacy to not drink, and an alcohol-related injury as the source of the ED visit tend to benefit more from brief ED interventions.15,16
It is unknown whether moderators of alcohol-focused interventions translate to marijuana-focused interventions among adolescents. The literature has established that adolescents view marijuana as being safer than alcohol and having fewer consequences,17 and therefore, different factors may moderate marijuana outcomes versus alcohol outcomes.18 In our original randomized controlled trial (RCT), we recruited almost 300 at-risk adolescents (eg, screened and reported alcohol use) aged 12 through 18 attending a PC appointment. Teens who received a 15-minute in-person brief intervention in PC reported significantly fewer alcohol-and-marijuana–related consequences 1 year later compared with adolescents receiving usual care (UC); we did not find effects for alcohol or marijuana use.4 The current study is a secondary analysis that adds to the original RCT findings and addresses gaps in this literature by examining demographic and alcohol-and-marijuana–related baseline moderators on 12-month alcohol and marijuana outcomes. We hope to determine which teens may benefit the most from brief PC interventions in the long-term to inform PC providers how to best use limited resources.
Methods
Study procedures are described elsewhere.4 Briefly, participants were recruited from 4 PC clinics in Los Angeles and Pittsburgh providing care for ethnically and racially diverse and underserved youth; all adolescents (12–18 years of age) attending an appointment during the study period (April 2013–November 2015) were invited to participate. Procedures were approved by the institutional review board and clinics. Adolescents were screened by using the National Institute on Alcohol Abuse and Alcoholism Screening Guide (NIAAA-SG); we obtained either youth consent (if age 18) or parental consent and youth assent (if age <18). Adolescents who screened in as at risk (see the measures) were randomly assigned to the intervention (CHAT) or to enhanced UC. Adolescents completed Web surveys after screening and at the time of random assignment (baseline) and at 3, 6, and 12 months (postbaseline). Adolescents were paid $25 (baseline), $40 (3 months), $50 (6 months), and $75 (12 months).
We approached 3309 adolescents. Of these, 27% were ineligible because of age, lack of English language proficiency, being present for an appointment other than their own, or cognitive impairment; 18.5% refused to participate, mostly because of time constraints or the teen being at the clinic for family planning (eg, to obtain birth control) and not wanting their parent(s) to know. This yielded a sample of 1803 adolescents who enrolled or provided consent to contact. Of these, 230 did not complete the baseline assessment within the field period or had unreliable contact information, leaving 1573 adolescents to be screened by using the NIAAA-SG (Fig 1). Of these, 294 were identified as at risk by using the NIAAA-SG and were randomly assigned to either CHAT (N = 153) or UC (N = 141). Randomization began with a 1:1 ratio (CHAT:UC) and was implemented by assigning entire days (block randomization) within each clinic to either CHAT or UC. This allocation was adjusted by using a random-number generator19 over the course of the study to ensure sufficient sample size in each condition given that the number of visits per day fluctuated over time. Initial sample size targets were based on achieving adequate power to detect small-to-medium effects.4
FIGURE 1.
Consort diagram. (Reprinted with permission from D’Amico EJ, Parast L, Shadel WG, Meredith LS, Seelam R, Stein BD. Brief motivational interviewing intervention to reduce alcohol and marijuana use for at-risk adolescents in primary care. J Consult Clin Psychol. 2018;86(9):775–786.)
Intervention
CHAT is a 15- to 20-minute brief intervention using motivational interviewing (MI)20 delivered by trained MI facilitators to assess motivation for change, provide normative information for alcohol and other drug (AOD) use, and discuss whether teens might want to make changes in their behavior.4,21 CHAT was delivered immediately after the baseline survey, and fidelity was high throughout the study.4
To ensure each adolescent received AOD information during their PC appointment, adolescents randomly assigned to UC were given a brochure developed by the project team, which included information on effects of AOD use, how to prepare for risky situations, and a list of resources.
NIAAA-SG
Adolescents were identified as at risk by using the NIAAA-SG,22 which has been validated for use with adolescents across several studies and performs well for alcohol-related outcomes.23–25 Two screening questions were asked in a different order depending on age: “In the past year, on how many days have you had more than a few sips of beer, wine, or any drink containing alcohol?” and “Do any of your friends drink alcohol?” Youth aged 12 to 14 were first asked about friends’ drinking and then self-drinking as a less threatening way to gauge use, whereas youth aged 15 and older (and 14-year-olds in high school) were first asked about self-drinking and then friends’ drinking. On the basis of the NIAAA-SG, adolescents were categorized as no risk, lower risk, moderate risk, and highest risk. For this study, adolescents were considered at risk if they were categorized as either moderate or highest risk. For example, youth aged 12 to 15 were categorized as moderate risk if they reported 1 to 5 days of use; adolescents who were 16 years old were categorized as moderate risk if they reported 6 to 11 days of use (see the Supplemental Information for all determinations).22
Outcomes
We examined prespecified outcomes from the original RCT,4 including drinking, heavy drinking, negative alcohol consequences, marijuana use, heavy marijuana use, negative marijuana consequences, perceived peer use (alcohol and marijuana), time spent around peers who use (alcohol and marijuana), and resistance self-efficacy (RSE) (alcohol and marijuana). This study focuses on 12-month outcomes.
Alcohol use, heavy alcohol use, and marijuana use were assessed by using well-established measures26,27 asking, “During the past [time frame], how many times did you try or use [at least 1 full drink of alcohol] [drink 5 or more drinks] [marijuana]?” At baseline, the time frame was the past year; at 12-month follow-up, the time frame was the past 3 months. The 6-point frequency response scale (0 = “never”; 5 = “more than 20 times”) was rescaled to a pseudocontinuous variable ranging from 0 to 20 by using the midpoint of any range as the new value (eg, 3–10 times was recoded as 6.5 times). We rescaled responses for several reasons. First, the NIAAA Web site supports this midpoint rescaling and states within the Estimating Alcohol Consumption section, “If the frequency categories include a range of frequencies, the midpoint of these values is used (eg, ‘2–3 times a month’ is converted to 2.5 times per month or 30 times per year).”28 Second, this approach matches the rescaling performed for the main RCT article. Finally, this rescaled approach makes the intervention effect estimate clinically interpretable in terms of the number of times an adolescent tried or used the substance in the past 3 months. Teens also reported their maximum quantity of alcohol consumed in the past 30 days, which was capped at 15 drinks. We assessed heavy marijuana use by asking, “On days you use marijuana, how many times do you use it?” Response options ranged from “I don’t use marijuana at all” to “3 or more times.” Responses ranged from 0 to 3.
Negative consequences experienced were measured by using well-established measures for adolescents.23 Adolescents rated how often they experienced a particular negative consequence from drinking alcohol or using marijuana in the past year (baseline) or past 3 months (12 month follow up) on a scale from “never” to “20 or more times.” There were 6 consequences related to drinking alcohol (eg, “doing something I regretted because of drinking”) and 4 consequences related to using marijuana (eg, “had trouble concentrating because of marijuana use”). Items were rescaled to a pseudocontinuous variable ranging from 0 to 20 by using the midpoint of any range as the new value and then summed to create a total score indicating the number of negative consequences experienced (alcohol α = 0.89; marijuana α = 0.88 at 12 months).
Peer influence was assessed with 2 items of perceived peer use (eg, how many in a group of 100 teens drink alcohol and/or use marijuana at least once per month from 0 to 100)29 and 2 items about time spent around peers who use alcohol or marijuana (scored as “never” = 0, “hardly ever” = 1, “sometimes” = 2, and “often” = 3).10
RSE30 for alcohol and marijuana was defined as the average of 4 items rated from “I would definitely use” to “I would definitely not use” on the basis of different situations (eg, if the teen’s best friend were using or the teen was bored at party). RSE ranged from 1 to 4; higher scores indicated greater RSE (alcohol α = 0.92; marijuana α = 0.97 at 12 months).
Hypothesized Moderators
We tested prespecified hypothesized moderators of the effect of CHAT on outcomes: sex, race and/or ethnicity (non-Hispanic white, African American, Hispanic, and other or multiracial throughout all analyses), risk level (moderate risk versus highest risk), past-year substance use (alcohol or marijuana), negative consequences (alcohol or marijuana), and alcohol use disorder (AUD) or cannabis use disorder (CUD), all reported at baseline. Adolescents were classified as having an AUD or CUD if they reported 2 or more of the 11 Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for AUD or CUD4 on the Diagnostic Interview Schedule for Children Version IV31 computerized version (with DSM-5 criteria), which is valid and reliable in adolescents.32,33
Statistical Analysis
We performend an intent-to-treat analysis (ie, participants who were randomly assigned were included in the statistical analysis ans analyzed according to the group to which they were originally assigned, regardless of compliance)34 and accouned for missing data due to loss to follow-up and item missingness by using multiple imputation. Forty imputed data sets were generated by using multivariate imputation by chained equations with the MI procedure in SAS version 9.4 (SAS Institute, Inc, Cary, NC).35–37 Analyses were performed within each imputed data set, and results were pooled across data sets.38
We investigated moderators using linear regression models with 12-month outcomes. We included a CHAT indicator as the primary independent variable while controlling for the baseline values of outcome, age, sex, mother’s education, and race and/or ethnicity. Mother’s education was categorized as less than high school, high school, some college, college, or unknown. All models included an indicator for clinic site to account for clustering. The moderator was included as an independent variable along with the interaction between the moderator and the CHAT indicator. Significant moderation was identified on the basis of significance of the interaction term. All hypothesized associations and models were substance specific; for example, when examining whether the number of negative consequences at baseline moderated the effect of CHAT on substance use at 12 months, 1 regression included the outcome as alcohol use and the moderator as the number of negative consequences of alcohol, and another regression model included the outcome as marijuana use and the moderator as the number of negative consequences of marijuana. Analyses were performed with SAS version 9.4.
Results
Among the 153 adolescents assigned to CHAT, 142 received the intervention as intended, 2 refused, and 9 did not complete the intervention. Rates of follow-up at 12-months were 122 (80%) and 114 (81%) for CHAT and UC, respectively (Fig 1).4
The overall study sample was 58% female, 66% Hispanic, 17% African American, 12% white, and 5% multiethnic or of other race and had an average age of 16 years. Notably, 90% of the entire sample reported past-year alcohol use, 66% reported heavy drinking, and 77% reported marijuana use. Using DSM-5 criteria, 19% of teens met criteria for AUD, and 40% met criteria for CUD. Table 1 shows all variables by group; there were no statistically significant baseline differences between groups.
TABLE 1.
Baseline Characteristics Stratified by Group
| CHAT (n = 153) | UC (n = 141) | P | |
|---|---|---|---|
| Demographics | |||
| Age, mean (SD) | 16.16 (1.61) | 15.91 (1.61) | .19 |
| Female, n (%) | 90 (59.6) | 77 (55.4) | .55 |
| Race, n (%) | .06 | ||
| White | 19 (12.4) | 15 (10.6) | |
| Black | 31 (20.3) | 18 (12.8) | |
| Hispanic | 99 (64.7) | 96 (68.1) | |
| Multiracial/other | 4 (2.6) | 12 (8.5) | |
| Mother’s education ≥ some college | 35 (26.7) | 30 (25) | .87 |
| Behaviors, mean (SD) | |||
| Past year use, No. times, range 0–20 | |||
| Alcohol | 10.43 (7.93) | 9.46 (7.76) | .29 |
| Heavy alcohol | 5.25 (6.23) | 5.51 (7.12) | .74 |
| Marijuana | 10.02 (8.51) | 9.51 (8.31) | .60 |
| Alcohol max quantity, No. drinks, range 0–15 | 3.94 (4.19) | 3.6 (4.46) | .50 |
| On days using marijuana, No. times used, range 0–3 | 1.54 (1.15) | 1.51 (1.15) | .83 |
| Negative consequences, No. experienced, mean (SD) | |||
| Alcohol, range 0–120 | 6.59 (14.17) | 7.86 (16.57) | .48 |
| Marijuana, range 0–80 | 3.58 (10.46) | 4.63 (12.54) | .44 |
| Alcohol use disorder, n (%) | 29 (19.8) | 24 (17.3) | .57 |
| Cannabis use disorder, n (%) | 56 (38.6) | 57 (40.7) | .72 |
| Peer influence and resistance self-efficacy, mean (SD) | |||
| Perceived peer use (out of 100 peers) | |||
| Alcohol | 54.38 (26.13) | 53.76 (26.06) | .84 |
| Marijuana | 63.92 (27.37) | 65.53 (27.63) | .62 |
| Time spent around peers who use, 0 = never to 3 = often | |||
| Alcohol | 1.93 (0.96) | 1.91 (0.89) | .80 |
| Marijuana | 2.07 (0.96) | 2.16 (0.99) | .46 |
| RSE, range 1–4a | |||
| Alcohol | 2.46 (0.91) | 2.46 (0.88) | .99 |
| Marijuana | 2.55 (1.12) | 2.57 (1.13) | .91 |
| City, n (%) | .37 | ||
| Los Angeles | 100 (65.4) | 100 (70.9) | |
| Pittsburgh | 53 (34.6) | 41 (29.1) |
All calculated among nonmissing values. (Reprinted with permission from D’Amico, EJ, Parast, L, Shadel, WG, Meredith, LS, Seelam, R, Stein, BD. Brief motivational interviewing intervention to reduce alcohol and marijuana use for at-risk adolescents in primary care. J Consult Clin Psychol. 2018;86(9):775–786.)
Higher values indicate greater RSE.
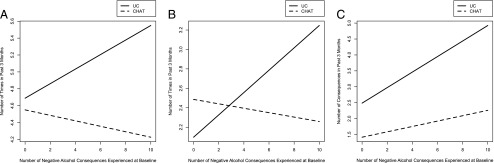
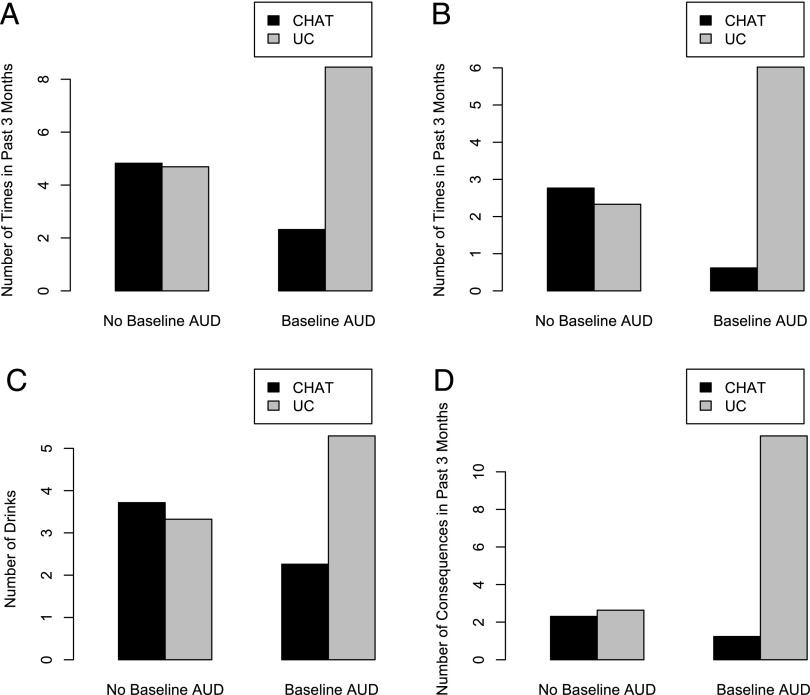
Alcohol Outcomes
Table 2 presents estimated main effects and the estimated interaction effect for alcohol analyses. For significant interactions, we created figures with the expected adjusted outcome at 12 months on the y-axis, the moderator on the x-axis, and 2 lines reflecting the interaction effect (Figs 2 and 3). There was no evidence of moderation by sex, race, baseline risk level, or alcohol use at baseline. However, the number of baseline negative consequences of alcohol moderated the effect of CHAT on alcohol use (P = .0172), heavy alcohol use (P = .0011), and the number of negative consequences of alcohol 1 year later (P = .0363). Thus, among adolescents with more alcohol consequences at baseline, teens in CHAT reported less alcohol use, heavy alcohol use, and negative consequences of alcohol at 12 months compared with similar teens in UC (Fig 2). In addition, AUD moderated the effect of CHAT on alcohol use (P = .0007), heavy alcohol use (P = .0002), maximum alcohol quantity (P = .0068), and the number of negative consequences of alcohol at 12 months (P = .0003) such that teens in CHAT with AUD reported less use and problems compared with similar teens in UC with AUD (Fig 3). No moderation effects were found for peer influence or RSE.
TABLE 2.
Moderation of CHAT Intervention: Alcohol Outcomes at 12 Months
| Hypothesized Moderators | Outcomes at 12 mo | |||||||
|---|---|---|---|---|---|---|---|---|
| Past–3 mo Alcohol Use, No. Times | Past–3 mo Heavy Alcohol Use, No. Times | Alcohol Maximum Quantity, No. Drinks | Negative Alcohol Consequences, No. Experienced | |||||
| Regression Coefficient (95% CI) | P | Regression Coefficient (95% CI) | P | Regression Coefficient (95% CI) | P | Regression Coefficient (95% CI) | P | |
| Baseline negative alcohol consequences | ||||||||
| Main effect: CHAT | −0.14 (−1.64 to 1.36) | .8562 | 0.39 (−0.84 to 1.62) | .5355 | 0.19 (−0.83 to 1.22) | .7106 | −1.07 (−3.41 to 1.27) | .3696 |
| Main effect: baseline negative alcohol consequences | 0.09 (0.01 to 0.16) | .0287 | 0.11 (0.05 to 0.18) | .0007 | 0.05 (0 to 0.1) | .0348 | 0.24 (0.14 to 0.35) | <.0001 |
| Interaction | −0.12 (−0.22 to −0.02) | .0172 | −0.14 (−0.22 to −0.06) | .0011 | −0.06 (−0.12 to 0.01) | .0905 | −0.16 (−0.31 to −0.01) | .0363 |
| Baseline AUD diagnosis | ||||||||
| Main effect: CHAT | 0.13 (−1.34 to 1.6) | .8603 | 0.44 (−0.78 to 1.66) | .4801 | 0.39 (−0.61 to 1.39) | .4439 | −0.34 (−2.63 to 1.96) | .7748 |
| Main effect: baseline AUD diagnosis | 3.77 (0.93 to 6.6) | .0094 | 3.69 (1.19 to 6.19) | .0039 | 1.97 (−0.03 to 3.97) | .0538 | 9.27 (4.74 to 13.79) | <.0001 |
| Interaction | −6.27 (−9.89 to −2.65) | .0007 | −5.84 (−8.87 to −2.81) | .0002 | −3.43 (−5.91 to −0.95) | .0068 | −10.34 (−15.97 to −4.7) | .0003 |
All results account for missing data using multiple imputation methods. Regression adjusts for baseline values of all outcomes, race and/or ethnicity, age, sex, mother’s education, and site. Detailed results for the outcomes perceived peer use of alcohol, time spent around peers who use alcohol, and alcohol RSE, and the moderators risk level at baseline, baseline alcohol use, sex, and race and/or ethnicity, are not shown. All were not significant. CI, confidence interval.
FIGURE 2.
Number of alcohol consequences experienced at baseline as moderator. A, Alcohol use at 12 months (outcome). The moderator is the number of negative consequences experienced at baseline. B, Heavy alcohol use at 12 months (outcome). The moderator is the number of negative consequences experienced at baseline. C, Negative alcohol consequences of alcohol reported at 12 months (outcome). The moderator is the number of negative consequences experienced at baseline.
FIGURE 3.
AUD diagnosis as moderator. A, Alcohol use at 12 months (outcome). The moderator is AUD diagnosis at baseline. B, Heavy alcohol use at 12 months (outcome). The moderator is AUD diagnosis at baseline. C, Maximum alcohol quantity at 12 months (outcome). The moderator is AUD diagnosis at baseline. D, Negative alcohol consequences of alcohol reported at 12 months (outcome). The moderator is AUD diagnosis at baseline.
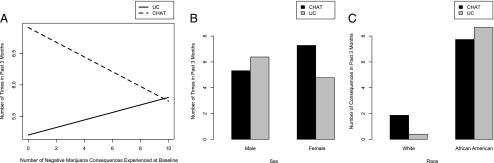
Marijuana Outcomes
Table 3 presents estimated main and interaction effects for marijuana analyses. There was no evidence of moderation by baseline risk level, marijuana use, or CUD. The number of baseline negative consequences of marijuana moderated the effect of CHAT on marijuana use at 12 months postbaseline (P = .035; Fig 4). Among teens in CHAT, the interaction effect is such that those with more marijuana consequences at baseline reported less marijuana use 1 year later compared with similar teens in UC; however, teens in CHAT who reported fewer marijuana consequences at baseline reported more marijuana use 1 year later compared with similar teens in UC (note that the axis for Fig 4A is truncated at the 95th percentile; thus, the effect for a high number of marijuana consequences is not visible in this figure). No moderation effects were found for peer influence or RSE.
TABLE 3.
Moderation of CHAT Intervention: Marijuana Outcomes at 12 Months
| Hypothesized Moderators | Outcomes at 12 mo | |||
|---|---|---|---|---|
| Past–3 mo Marijuana Use, No. Times | Negative Marijuana Consequences, No. Experienced | |||
| Regression Coefficient (95% CI) | P | Regression Coefficient (95% CI) | P | |
| Baseline negative marijuana consequences | ||||
| Main effect: CHAT | 1.71 (−0.14 to 3.56) | .0708 | −1.46 (−3.18 to 0.27) | .0978 |
| Main effect: baseline negative marijuana consequences | 0.06 (−0.07 to 0.19) | .3522 | 0.08 (−0.03 to 0.2) | .1507 |
| Interaction | −0.18 (−0.34 to −0.01) | .035 | −0.07 (−0.22 to 0.09) | .3992 |
| Sex | ||||
| Main effect: CHAT | −1.06 (−3.77 to 1.64) | .44 | −1.19 (−3.7 to 1.32) | .3529 |
| Main effect: sex | −1.61 (−4.26 to 1.04) | .2327 | 0.69 (−1.66 to 3.05) | .563 |
| Interaction | 3.57 (0.01 to 7.13) | .0495 | −0.94 (−4.24 to 2.37) | .5779 |
| Race and/or ethnicity | ||||
| Main effect: CHAT | 3.41 (−1.96 to 8.77) | .2129 | 1.46 (−3.24 to 6.17) | .5416 |
| Main effect: African American | 1.85 (−3.37 to 7.08) | .487 | 8.27 (3.54 to 12.99) | .0006 |
| Main effect: Hispanic | 1.53 (−3.21 to 6.28) | .5259 | 1.39 (−2.89 to 5.66) | .5246 |
| Main effect: multiracial or other | −0.72 (−6.79 to 5.36) | .8173 | 0.42 (−4.94 to 5.77) | .8784 |
| Interaction effect: African American | −3.63 (−10.55 to 3.28) | .3029 | −9.92 (−16.15 to −3.69) | .0018 |
| Interaction effect: Hispanic | −2.67 (−8.53 to 3.2) | .3726 | −2.39 (−7.47 to 2.69) | .3569 |
| Interaction effect: multiracial or other | −0.52 (−11.44 to 10.39) | .9248 | −0.39 (−9.4 to 8.63) | .9331 |
All results account for missing data using multiple imputation methods. Regression adjusts for baseline values of all outcomes, race and/or ethnicity, age, sex, mother’s education, and site. Detailed results for the outcomes number of times marijuana is used on days marijuana is used, perceived peer use of marijuana, time spent around peers who use marijuana, and marijuana RSE, and for the moderators risk level at baseline, baseline marijuana use, and CUD at baseline are not shown. All were not significant. CI, confidence interval.
FIGURE 4.
Marijuana outcomes and moderators. A, Marijuana use at 12 months (outcome). The moderator is the number of negative consequences experienced at baseline. B, Marijuana use at 12 months (outcome). The moderator is sex. C, Negative consequences of marijuana reported at 12 months (outcome). The moderator is race.
For demographics (Fig 4), we found an interaction for sex whereby the effect of CHAT for marijuana use at 12 months was greater for male participants than female participants such that male participants in CHAT reported fewer marijuana consequences than male participants in UC, and female participants in UC reported fewer marijuana consequences than female participants in CHAT (P = .0495). We also found moderation for race whereby African American adolescents assigned to CHAT reported fewer marijuana consequences at 12 months compared with African American teens in UC, and white adolescents assigned to UC reported fewer marijuana consequences than white youth assigned to CHAT (P = .0006).
Discussion
This study examined which teens benefitted most from a 15-minute efficacious MI intervention delivered in PC.4 We assessed moderating effects of baseline factors on 1-year outcomes. For severity of problems, moderation effects were only found on behavioral outcomes. Specifically, teens who participated in CHAT with AUD and more alcohol consequences at baseline reported less drinking and fewer alcohol consequences at the 1-year follow-up compared with similar teens in UC. In addition, teens in CHAT with more marijuana consequences at baseline reported less marijuana use 1 year later than similar teens in UC. Findings suggest that adolescents with greater drinking and alcohol and/or marijuana consequences at baseline were more likely to benefit from CHAT 1 year later than those who received UC. Interestingly, we found that teens in CHAT who reported fewer marijuana consequences at baseline reported greater marijuana use at 12 months compared with teens in UC and were therefore less likely to benefit from CHAT. This is not unusual with MI interventions because the focus is on whether teens are ready to change their use. Other studies have shown, for example, that when teens feel that their marijuana use is not a problem (eg, not experiencing a lot of consequences), they are less willing to change their use,17 although they feel confident they could change use if they started experiencing more consequences.18 Thus, when teens are not yet experiencing many problems from marijuana use, it may be important for providers to build adolescents’ self-efficacy that they could change if they desire to, explore ways to recognize when marijuana-related problems are developing, and encourage use of coping strategies in risky situations in which they may use more marijuana.
For demographics, we found that male participants in CHAT reported less marijuana use compared with male participants in UC, and female participants in CHAT reported more marijuana use compared with female participants in UC. It is not clear why this difference between the sexes occurred. Further research is needed to understand how interventions may affect male and female participants uniquely.
We also found that African American adolescents in CHAT reported fewer marijuana consequences 1 year later compared with African American adolescents in UC; in contrast, white adolescents in CHAT reported more marijuana consequences than white adolescents in UC. We know from previous work that CHAT was effective among diverse populations,10 and this finding supports that, which is important because nationally representative studies indicate that these populations are less likely to seek AOD treatment.39 Thus, having a brief intervention as part of a PC appointment could help reach these populations. This effect may have also occurred because nonwhite teens tend to have greater consequences at similar levels of use40,41; thus, CHAT may have benefitted African American teens because they were having more problems from their marijuana use than white teens.
Overall, findings highlight that a brief MI intervention is an opportune way to reach teens with more severe alcohol and marijuana use in the PC setting; at-risk teens who received CHAT had less use and fewer problems than teens who received UC 1 year later. Findings have public health implications given that untreated AOD use is associated with problems into adulthood as well as risk for premature mortality.2 This study provides a preventive model of care and shows benefits for at-risk teens. Results fit with conclusions from a 2015 meta-analysis on brief alcohol interventions for adolescents, in which larger intervention effects were found for alcohol-related problems when adolescents were selected on the basis of their level of alcohol consumption,14 and extend the literature by elucidating moderating effects on marijuana outcomes.
There is often little time to screen and intervene in PC23,24; our findings have important implications for addressing adolescent AOD use in the PC setting. Previous work has indicated that brief screeners can accurately identify at-risk teens for both alcohol24,25,42–44 and marijuana use.24,44,45 Furthermore, CHAT is 1 of only 3 brief adolescent interventions tested in PC,10,12,46 and CHAT is the only brief intervention (15 minutes) to date that fits within the time frame of an adolescent’s PC appointment, targets at-risk teens, and was found to reduce both substance use and consequences in the long-term. CHAT was developed with extensive input from providers, parents, and teens,21 and the collaborative and nonjudgmental approach was well received by teens in multiple studies.4,10 Given the brevity of CHAT, it is easily learned by people with varying education levels,4 making uptake in PC settings feasible for different types of providers depending on who may be available in the clinic setting (eg, nurses, social workers, residents, and physician assistants).
Limitations include self-report, although it is important to note that teen reports of alcohol and marijuana use in this sample matched national norms.47 Furthermore, although we recruited a diverse sample over a 2.5-year period, our results may not generalize to clinics serving other populations or in other geographic areas. In addition, given the sample size, we were unable to conduct stratified analyses to further investigate mechanisms that may explain the observed moderation effects of sex and race and/or ethnicity; thus, additional research is needed in this area.
Conclusions
This brief MI intervention was particularly effective for teens reporting more problems from alcohol and marijuana use. Reaching at-risk youth is often difficult. Many adolescents see their PC providers annually,48 which is an important opportunity for providers, such as pediatricians, to talk to adolescents about their substance use and determine if they are experiencing problems due to their use. If teens are experiencing problems due to substance use, providers can implement a brief intervention, such as CHAT, to discuss the pros and cons of an adolescent’s substance use and gauge their readiness to change. In doing so, the provider gains insight into whether more intensive services are needed and what services the adolescent may be open to receiving. Thus, PC providers can potentially reach many at-risk teens who might not otherwise seek services for their use.
Acknowledgments
We thank the clinics that participated and supported this project. We also thank Kirsten Becker and Jennifer Parker for overseeing the survey administrations and Michael Woodward for help with article formatting.
Glossary
- AOD
alcohol and other drug
- AUD
alcohol use disorder
- CUD
cannabis use disorder
- DSM-5
Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition
- ED
emergency department
- MI
motivational interviewing
- NIAAA
National Institute on Alcohol Abuse and Alcoholism
- NIAAA-SG
National Institute on Alcohol Abuse and Alcoholism Screening Guide
- PC
primary care
- RCT
randomized controlled trial
- RSE
resistance self-efficacy
- UC
usual care
Footnotes
Dr D’Amico conceptualized and designed the study and drafted the initial manuscript; Dr Parast oversaw the analysis plan, conducted analyses, wrote the Results section, and reviewed and revised the manuscript; Dr Osilla helped draft parts of the initial manuscript and reviewed and revised the manuscript; Ms Seelam conducted initial analyses and reviewed and revised the manuscript; Drs Meredith, Shadel, and Stein helped conceptualize the analyses for the manuscript and design the original randomized controlled trial and reviewed and revised the manuscript; and all authors approved the final manuscript as submitted.
This trial has been registered www.clinicaltrials.gov (identifier NCT01797835).
Deidentified individual participant data will not be made available.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by a grant from the National Institute on Alcohol Abuse and Alcoholism (R01AA021786; Dr D’Amico). Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.SAMHSA Results From the 2016 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality; 2016. Available at: https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2016/NSDUH-DetTabs-2016.htm#tab5-50B [Google Scholar]
- 2.Clark DB, Martin CS, Cornelius JR. Adolescent-onset substance use disorders predict young adult mortality. J Adolesc Health. 2008;42(6):637–639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gore FM, Bloem PJ, Patton GC, et al. Global burden of disease in young people aged 10-24 years: a systematic analysis. Lancet. 2011;377(9783):2093–2102 [DOI] [PubMed] [Google Scholar]
- 4.D’Amico EJ, Parast L, Shadel WG, Meredith LS, Seelam R, Stein BD. Brief motivational interviewing intervention to reduce alcohol and marijuana use for at-risk adolescents in primary care. J Consult Clin Psychol. 2018;86(9):775–786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walton MA, Resko S, Barry KL, et al. A randomized controlled trial testing the efficacy of a brief cannabis universal prevention program among adolescents in primary care. Addiction. 2014;109(5):786–797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Black LI, Nugent CN, Vahratian A. Access and utilization of selected preventive health services among adolescents aged 10-17. NCHS Data Brief. 2016;(246):1–8 [PubMed] [Google Scholar]
- 7.Lawson PJ, Flocke SA. Teachable moments for health behavior change: a concept analysis. Patient Educ Couns. 2009;76(1):25–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Meredith LS, Ewing BA, Stein BD, et al. Influence of mental health and alcohol or other drug use risk on adolescent reported care received in primary care settings. BMC Fam Pract. 2018;19(1):10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loheswaran G, Soklaridis S, Selby P, Le Foll B. Screening and treatment for alcohol, tobacco and opioid use disorders: a survey of family physicians across Ontario. PLoS One. 2015;10(4):e0124402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.D’Amico EJ, Miles JNV, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: a randomized pilot study in a primary care clinic. J Subst Abuse Treat. 2008;35(1):53–61 [DOI] [PubMed] [Google Scholar]
- 11.Spirito A, Sindelar-Manning H, Colby SM, et al. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: results of a randomized clinical trial. Arch Pediatr Adolesc Med. 2011;165(3):269–274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Walton MA, Bohnert K, Resko S, et al. Computer and therapist based brief interventions among cannabis-using adolescents presenting to primary care: one year outcomes. Drug Alcohol Depend. 2013;132(3):646–653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cunningham RM, Chermack ST, Ehrlich PF, et al. Alcohol interventions among underage drinkers in the ED: a randomized controlled trial. Pediatrics. 2015;136(4). Available at: www.pediatrics.org/cgi/content/full/136/4/e783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanner-Smith EE, Lipsey MW. Brief alcohol interventions for adolescents and young adults: a systematic review and meta-analysis. J Subst Abuse Treat. 2015;51:1–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walton MA, Goldstein AL, Chermack ST, et al. Brief alcohol intervention in the emergency department: moderators of effectiveness. J Stud Alcohol Drugs. 2008;69(4):550–560 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spirito A, Monti PM, Barnett NP, et al. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. J Pediatr. 2004;145(3):396–402 [DOI] [PubMed] [Google Scholar]
- 17.D’Amico EJ, Houck JM, Hunter SB, Miles JNV, Osilla KC, Ewing BA. Group motivational interviewing for adolescents: change talk and alcohol and marijuana outcomes. J Consult Clin Psychol. 2015;83(1):68–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Osilla KC, Ortiz JA, Miles JNV, Pedersen ER, Houck JM, D’Amico EJ. How group factors affect adolescent change talk and substance use outcomes: implications for motivational interviewing training. J Couns Psychol. 2015;62(1):79–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.R Core Team R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2013 [Google Scholar]
- 20.Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. 3rd ed. New York, NY: Guilford Press; 2012 [Google Scholar]
- 21.Stern SA, Meredith LS, Gholson J, Gore P, D’Amico EJ. Project CHAT: a brief motivational substance abuse intervention for teens in primary care. J Subst Abuse Treat. 2007;32(2):153–165 [DOI] [PubMed] [Google Scholar]
- 22.NIAAA Alcohol Screening and Brief Intervention for Youth: A Practitioners Guide. NIH Publication No. 11-7805. Rockville, MD: NIAAA, DHHS, and AAP; 2011 [Google Scholar]
- 23.D’Amico EJ, Parast L, Meredith LS, Ewing BA, Shadel WG, Stein BD. Screening in primary care: what is the best way to identify at-risk youth for substance use? Pediatrics. 2016;138(6):1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kelly SM, Gryczynski J, Mitchell SG, Kirk A, O’Grady KE, Schwartz RP. Validity of brief screening instrument for adolescent tobacco, alcohol, and drug use. Pediatrics. 2014;133(5):819–826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clark DB, Martin CS, Chung T, et al. Screening for underage drinking and Diagnostic and Statistical Manual of mental disorders, 5th edition alcohol use disorder in rural primary care practice. J Pediatr. 2016;173:214–200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ellickson PL, McCaffrey DF, Ghosh-Dastidar B, Longshore DL. New inroads in preventing adolescent drug use: results from a large-scale trial of project ALERT in middle schools. Am J Public Health. 2003;93(11):1830–1836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Survey Results on Drug Use, 1975-2012. Vol. I: Secondary School Students. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2013 [Google Scholar]
- 28.Dawson DA. Methodological issues in measuring alcohol use. Alcohol Res Health. 2003;27(1):18–29 [PMC free article] [PubMed] [Google Scholar]
- 29.Pedersen ER, Miles JN, Ewing BA, Shih RA, Tucker JS, D’Amico EJ. A longitudinal examination of alcohol, marijuana, and cigarette perceived norms among middle school adolescents. Drug Alcohol Depend. 2013;133(2):647–653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.D’Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, Green HDJ Jr. Preventing alcohol use with a voluntary after-school program for middle school students: results from a cluster randomized controlled trial of CHOICE. Prev Sci. 2012;13(4):415–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shaffer D, Fisher P, Lucas C, Comer J. Diagnostic Interview Schedule for Children (DISC-IV) Scoring Manual. New York, NY: NIMH DISC Editorial Board and Mark Davies; 2007 [Google Scholar]
- 32.NIMH NHANES Data Documentation National Institute of Mental Health Diagnostic Interview Schedule for Children (DISC) (YDQ): Years of Coverage: 1999–2004. Rockville, MD: NIMH; 2006. Available at: www.cdc.gov/nchs/data/nhanes/limited_access/ydq.pdf [Google Scholar]
- 33.Wasserman GA, McReynolds LS, Lucas CP, Fisher P, Santos L. The voice DISC-IV with incarcerated male youths: prevalence of disorder. J Am Acad Child Adolesc Psychiatry. 2002;41(3):314–321 [DOI] [PubMed] [Google Scholar]
- 34.Lachin JM. Statistical considerations in the intent-to-treat principle. Control Clin Trials. 2000;21(3):167–189 [DOI] [PubMed] [Google Scholar]
- 35.Azur MJ, Stuart EA, Frangakis C, Leaf PJ. Multiple imputation by chained equations: what is it and how does it work? Int J Methods Psychiatr Res. 2011;20(1):40–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.White IR, Royston P, Wood AM. Multiple imputation using chained equations: issues and guidance for practice. Stat Med. 2011;30(4):377–399 [DOI] [PubMed] [Google Scholar]
- 37.van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1–67 [Google Scholar]
- 38.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychol Methods. 2002;7(2):147–177 [PubMed] [Google Scholar]
- 39.Center for Behavioral Health Statistics and Quality 2016 National Survey on Drug Use and Health: Detailed Tables (Table 5.43B). Rockville, MD: Substance Abuse and Mental Health Services Administration; 2017 [Google Scholar]
- 40.D’Amico EJ, Tucker JS, Miles JNV, Ewing BA, Shih RA, Pedersen ER. Alcohol and marijuana use trajectories in a diverse longitudinal sample of adolescents: examining use patterns from age 11 to 17 years. Addiction. 2016;111(10):1825–1835 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dunbar MS, Tucker JS, Ewing BA, et al. Ethnic differences in cigarette use trajectories and health, psychosocial, and academic outcomes. J Adolesc Health. 2018;62(3):327–333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mitchell SG, Kelly SM, Gryczynski J, et al. The CRAFFT cut-points and DSM-5 criteria for alcohol and other drugs: a reevaluation and reexamination. Subst Abus. 2014;35(4):376–380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chung T, Colby SM, Barnett NP, Rohsenow DJ, Spirito A, Monti PM. Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. J Stud Alcohol. 2000;61(4):579–587 [DOI] [PubMed] [Google Scholar]
- 44.Parast L, Meredith LS, Stein BD, Shadel WG, D’Amico EJ. Identifying adolescents with alcohol use disorder: optimal screening using the National Institute on Alcohol Abuse and Alcoholism screening guide. Psychol Addict Behav. 2018;32(5):508–516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cummins LH, Chan KK, Burns KM, Blume AW, Larimer M, Marlatt GA. Validity of the CRAFFT in American-Indian and Alaska-Native adolescents: screening for drug and alcohol risk. J Stud Alcohol. 2003;64(5):727–732 [DOI] [PubMed] [Google Scholar]
- 46.Mason M, Light J, Campbell L, et al. Peer network counseling with urban adolescents: a randomized controlled trial with moderate substance users. J Subst Abuse Treat. 2015;58:16–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2011. Ann Arbor, MI: Institute for Social Research, The University of Michigan; 2012 [Google Scholar]
- 48.CDC, National Center for Health Statistics Summary Health Statistics: National Health Interview Survey, 2015. Vol Table C-8a Atlanta, GA: Centers for Disease Control and Prevention; 2015. Available at: https://www.cdc.gov/nchs/fastats/physician-visits.htm [Google Scholar]