The majority of soft contact lens wearers perceive themselves as being compliant with contact lens wear and hygiene, but it has been reported that most wearers practice some degree of non-compliance when it comes to replacing, cleaning, storing, or sleeping in their lenses.[1, 2] Non-compliance with habits including lens replacement and overnight wear can lead to complications that range from minor and self-limiting inflammation to vision threatening microbial keratitis.[3–7] It is important, therefore, to understand the magnitude of non-compliance in contact lens wearers so eye care providers can better educate participants and address reasons for non-compliance.
Lens replacement schedules vary depending on lens material, brand, and other parameters. For most commercially produced lenses, the manufacturer recommends a replacement schedule. It has been shown that more frequent contact lens replacement results in reduced rates of contact lens complications.[8–13] Contact lens wearers, however, commonly wear their lenses for longer intervals than suggested by the manufacturer and/or their eye care provider.[14, 15] Furthermore, it has been reported that eye care providers frequently prescribe lens replacement schedules that vary from those suggested by the manufacturer.[14, 15]
Overnight wear is another contact lens practice that has been reported to increase the risk of contact lens-associated ocular health complications.[5, 16–20] Some lens materials and brands are approved for overnight wear, but extended or continuous contact lens wear is intended to occur with approval from an eye care provider – not at the wearer’s discretion. Similar to lens replacement, contact lens wearers often practice overnight contact lens wear that conflicts with the wear schedule indicated by their eye care provider.[21]
Aside from daily disposable or continuous wear modalities, a contact lens has almost as much interaction with the case it is stored in as the eye it is worn on. Frequency of contact lens case replacement and case hygiene also influence risk for contact lens-associated health complications.[4, 16, 17] It has been reported that cases older than six months increase the risk of a corneal inflammatory event,[16] and poor contact lens case hygiene is a risk factor for microbial keratitis.[4, 17] The case, however, is the contact lens accessory that receives the least cleaning attention and is most likely to be contaminated (compared to the contact lens and contact lens solution).[22, 23]
Understanding how contact lens wearers use and misuse their contact lenses allows eye care providers to deliver targeted education that could help prevent contact lens-related ocular health complications. This study surveyed a sample of soft contact lens-wearing adults in a public setting in order to determine lens replacement, overnight wear, and contact lens case replacement habits.
Methods
This prospective, cross-sectional survey study recruited adult (ages 18 years and older) soft contact lens wearers at the Center for Science and Industry (COSI), a public science museum, in Columbus, Ohio, U.S.A. The study followed the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of the Ohio State University. COSI visitors were asked if they were current soft contact lens wearers, had the purpose of the study explained to them, and asked if they would like to participate. Participation was voluntary, anonymous, and took approximately five minutes. Because the survey collected no personal identifying health information, verbal informed consent was appropriate for this study and was obtained from each participant before the survey. COSI visitors who agreed to participate in the study were asked questions about their contact lens brand, replacement habits, overnight wear habits, and contact lens case hygiene. Survey responses were collected over an approximate three-month time period in 2017.
Each participant was asked to report the brand name of their contact lenses. It has been suggested that contact lens wearers have poor recall of their contact lens brand.[24] Picture identification improves accuracy of brand recall.[24] Therefore, a list of contact lens brands with a picture of each brand’s current packaging was provided to improve recall accuracy. If a participant’s brand was not listed, it was manually entered into the survey software. If a participant was unsure of what brand they were wearing, they had the option to choose “I don’t know.” Study data were collected and managed on an iPad using Research Electronic Data Capture (REDCap) tools hosted at the Ohio State University.[25] REDCap is a service supported by Grant UL1TR001070 from the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences of the National Institutes of Health.
The survey asked participants to report how often they typically replace their contact lenses and how often their eye care provider instructed them to replace their contact lenses. These responses were used to determine a participant’s compliance with their eye care provider’s prescription as well as determine how often each replacement type was being prescribed according to the manufacturer’s recommended replacement schedule (MRS). If a participant reported being compliant with the replacement schedule that was prescribed by their eye care provider (defined as replacing their contact lens as often or more often than they reported their eye care provider prescribed), they were considered to be compliant with replacement (regardless of if the eye care provider prescribed lens replacement as suggested by the manufacturer or if the participant knew what lens they were wearing).
The survey asked participants how often they slept overnight (occasional napping was not assessed in this survey) in their lenses and how often their eye care provider had prescribed overnight wear. If a participant reported overnight wear that matched their eye care provider’s recommendation or slept in their lenses less than that recommendation, they were considered to be compliant with overnight wear. These classifications were implemented to ensure that reported results reflected what the participant recalled being educated on by their eye care provider. Finally, participants who reported using a contact lens case were asked how old their current case was and how often they believed the case should be replaced.
Statistical analyses were performed using IBM SPSS Statistics (Version 24). Univariate analyses (chi-square tests and t-tests) were performed to determine how contact lens compliance (contact lens replacement, overnight wear compliance) were related to various participant factors that have been reported to influence ocular health in contact lens wearers.[26] When univariate analyses revealed that participant factors significantly influenced a compliance factor, multivariate binary logistic regression was performed to determine how these same participant factors, when analyzed together, impacted that particular compliance factor. Regression analyses met basic assumptions of binary logistic regression (binary dependent variable, independent observations, little/no multicolinearity among independent variables, relatively large sample size). Frequency of contact lens case replacement was compared to various participant factors using t-tests and one-way ANOVA. A p-value of <0.05 was the level of significance used to make conclusions in this study.
Results
At study completion, 307 COSI visitors participated in the survey. Survey data from ten were not analyzed because these participants did not know what brand of contact lenses they were wearing and/or they did not answer all of the questions used in analyses. Therefore, data from 297 participants were analyzed. The mean age of this study population was 34.4 ± 10.4 years (18 to 67), and 76.4% (n = 227) of participants were female. The mean years of reported contact lens wear for the entire sample was 16.2 ± 8.8 years (0.25 to 49). Non-compliance with prescribed lens replacement was reported in 38.7% (n = 115) of participants and 23.9% (n = 71) of the sample reported non-compliance with prescribed overnight wear.
When comparing the participant-reported contact lens brand to MRS in the overall sample, two-week replacement modalities were reported by 45.5% (n = 135), monthly replacement lenses were reported by 34.3% (n = 102), and daily replacement brands were reported by 20.2% (n = 60). Prevalence of daily disposable and planned-replacement modalities agree with reported prescribing trends in the United States at the time of the survey (2017).[27, 28] Table 1 shows univariate and multivariate analyses comparing age, gender, years of contact lens wear, replacement modality, and overnight wear compliance in participants who were compliant and not compliant with what they reported as their prescribed replacement schedules.
Table 1:
Univariate and multivariate analyses of lens replacement compliance compared to age, gender, years of contact lens wear, manufacture’s recommended replacement schedule (MRS), and overnight wear compliance in participants (n = 297) who were compliant (C) and noncompliant (NC) with their reported prescribed lens replacement schedules. MRS is listed as daily replacement (DR), monthly replacement (MR) and two-week replacement (2WR). Some overall percentages do not sum to 100% due to rounding.
| Lens Replacement Compliance (38.7% non-compliance, n = 115) |
||||
|---|---|---|---|---|
|
Age (years) |
Univariate | Multivariate | ||
| C | 35.2 ± 11.6 | p = 0.1a t = 1.8 |
p = 0.02 OR = 0.96 95% Cl: 0.92–0.99 |
|
| NC | 33.2 ± 8.1 | |||
| Gender | C | 74.7% female | p = 0.4 X2 = 0.8 |
p = 0.9 OR = 0.96 95% Cl: 0.52–1.76 |
| NC | 79.1% female | |||
| Years of Contact Lens Wear | C | 15.8 ± 9.7 | p = 0.4a t = −0.9 |
p = 0.02 OR = 1.05 95% Cl: 1.007–1.1 |
| NC | 16.7 ± 7.2 | |||
| MRS | C | 29.1% DR 34.6% MR 36.2% 2WR |
p < 0.0001b X2 = 27.3 |
p < 0.0001c |
| NC | 6.1% DR 33.9% MR 60.0% 2WR |
|||
| Overnight Wear Compliance | C | 81.3% compliant with ON wear |
p = 0.008 X2 = 7.1 |
p = 0.02 OR = 0.49 95% Cl: 0.27–0.88 |
| NC | 67.8% compliant with ON wear | |||
Levene’s Test for Equality of Variances revealed that equal variances could not be assumed (p < 0.05), so p and t-values reported in these cells are for independent t-tests when equal variances are not assumed.
Univariate individual comparisons of each MRS group showed that DR wearers were more likely to be compliant with replacement than 2WR ( X2 = 27.1, p < 0.0001) and MR wearers (X2 = 13.1, p < 0.0001). MR wearers were more likely to be compliant with replacement than 2WR wearers (X2 = 3.9, p = 0.049).
Multivariate individual comparisons of each MRS groups showed that DR wearers were more likely to be compliant with lens replacement than 2WR wearers (OR = 6.8, 95% CI: 2.81 – 16.20, p <0.0001) and MR (OR = 4.40, 95% CI: 1.78 – 10.88, p = 0.001). There was no statistical difference in compliance with multivariate comparison of MR and 2WR wearers (OR = 0.70, 95% CI: 0.38 – 1.12, p = 0.1).
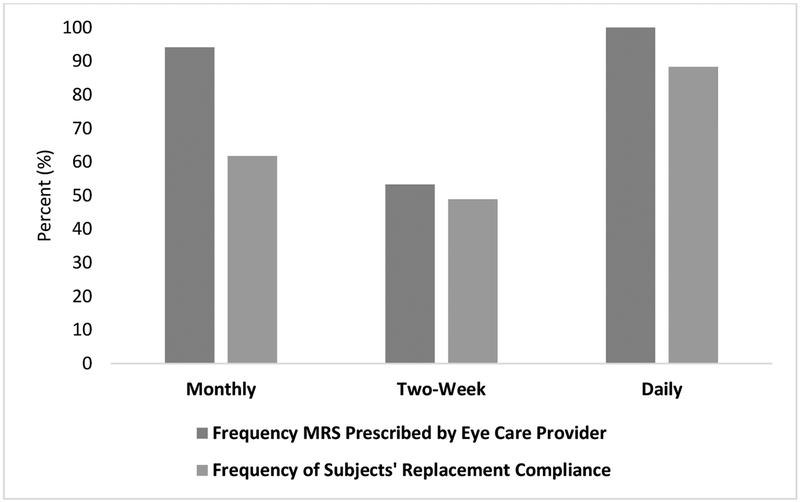
Overall, 23.2% (n = 69) of prescribed replacement schedules (as reported by the participant) did not match MRS. MRS affected if a lens was prescribed according to the suggested MRS (X2 = 76.9, p < 0.0001). Participants wearing a two-week MRS lens were less likely to have that lens prescribed according to MRS (53.3% prescribed as two-week replacement, n = 72) compared to monthly (94.1% prescribed as monthly replacement, n = 96, X2 = 46.8, p < 0.0001) and daily lens wearers (100% prescribed as daily replacement, n = 60, X2 = 41.4, p < 0.0001). Participants wearing daily replacement and monthly replacement MRS modalities were equally as likely to have their lenses prescribed according to MRS (X2 = 3.7, p = 0.06). Figure 1 shows the frequency each replacement modality was prescribed according to the MRS and how often participants in each replacement modality were compliant with what they reported as their prescribed replacement schedule.
Figure 1:
Frequency each lens modality was prescribed (as reported by the participant) according to the manufacturer’s recommended replacement schedule (MRS)(94.1% monthly, 53.3% two-week, 100.0% daily), and the frequency participants in each MRS reported compliance with their prescribed replacement schedule (61.8% monthly, 48.9% two-week, 88.3% daily)(n = 297).
Table 2 shows univariate and multivariate analyses comparing age, gender, years of contact lens wear, replacement modality, and lens replacement compliance in participants who were compliant and not compliant with their prescribed overnight wear schedules. Of the participants who reported sleeping in their lenses every night (n = 47), 34.0% (n = 16) reported that they were prescribed that way, 19.1% (n = 9) said they were prescribed to be slept in up to six nights in a row, and 46.8% (n = 22) said their lenses were prescribed to never be slept in.
Table 2:
Univariate and multivariate analyses of overnight wear compliance compared to age, gender, years of contact lens wear, manufacturer’s recommended replacement schedule (MRS), and lens replacement compliance in participants (n = 297) who were compliant (C) and noncompliant (NC) with their reported prescribed lens replacement schedules. MRS is listed as daily replacement (DR), monthly replacement (MR) and two-week replacement (2WR).
| Overnight Wear Compliance (23.9% non-compliance, n = 71) |
||||
|---|---|---|---|---|
|
Age (years) |
Univariate | Multivariate | ||
| C | 35.1 ± 10.4 | p = 0.053 t = 1.9 |
p = 1.0 OR = 1.001 95% Cl: 0.97–1.04 |
|
| NC | 32.3 ± 10.3 | |||
| Gender | C | 76.7% female |
p = 0.7 X2 = 0.2 |
p = 0.5 OR = 1.23 95% Cl: 0.64–2.36 |
| NC | 74.6% female |
|||
| Years of Contact Lens Wear | C | 16.9 ± 9.1 |
p = 0.008 t = 2.7 |
p = 0.02 OR = 0.95 95% Cl: 0.91–0.99 |
| NC | 13.8 ± 7.6 | |||
| MRS | C | 21.7% DR 36.3% MR 42.0% 2WR |
p = 0.1 X2 = 4.5 |
p = 0.3a |
| NC | 15.5% DR 28.2% MR 56.3% 2WR |
|||
| Lens Replacement Compliance | C | 65.4% lens replacement compliance |
p = 0.008 X2 = 7.1 |
p = 0.02 OR = 0.48 95% Cl: 0.27–0.87 |
| NC | 47.9% lens replacement compliance | |||
Multivariate individual comparisons of each MRS groups showed that there was no difference in overnight wear compliance in DR wearers compared to 2WR (OR = 1.58, 95% CI: 0.70 – 3.60, p = 0.3) and MR wearers (OR = 1.03, 95% CI: 0.43 – 2.46, p = 0.9). There was no difference in overnight wear compliance in 2WR wears compared to MR wearers (OR = 0.65, 95% CI: 0.35 – 1.23, p = 0.2).
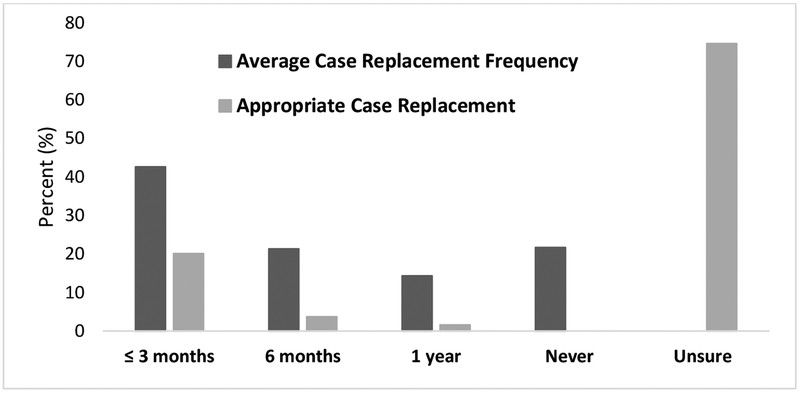
Participants were asked what they thought an appropriate contact lens case replacement schedule is and how often, on average, they actually replaced their contact lens case. If a participant reported never using a contact lens case (n = 53), they left this question blank and were not included in these analyses. Figure 2 reports the average reported frequency of contact lens case replacement and the perceived appropriate case replacement schedule. Average case replacement frequency was not associated with age (F = 0.9 p = 0.5), gender (X2 = 2.5, p = 0.5), years of contact lens wear (F = 0.5, p = 0.7), MRS (X2 = 6.1, p = 0.4), lens replacement compliance (X2 = 4.1, p = 0.3), or overnight wear compliance (X2 = 1.5, p = 0.7).
Figure 2:
The average reported frequency of contact lens case replacement and the perceived appropriate case replacement schedule reported by the sample (n = 244)
Discussion
In this population, contact lens wearers in daily replacement, or daily disposable, modalities were most compliant with prescribed lens replacement, compared to both monthly and two-week replacement modalities. In the group of wearers who were non-compliant with their prescribed replacement schedule, 60% reported wearing a 2-week replacement brand. These findings agree with previous studies which described that two-week wearers stretch replacement longer than one-month wearers,[3] and two-week wearers are less compliant with lens replacement than both monthly and daily replacement wearers.[29–31]
It has been reported that eye care providers prescribe the MRS most frequently with daily and monthly lenses.[14, 15] In our sample, a similar outcome was observed. Daily and monthly replacement wearers reported prescribed replacement schedules that matched the MRS 100% and 94% of the time, respectively, while participants in two-week modalities were prescribed two-week replacement only 53.3% of the time. In a study that surveyed eye care providers and contact lens wearers, it was reported that eye care providers in the United States and Canada prescribed two-week modalities for longer than two-week replacement 18% and 35% of the time, respectively.[14] Interestingly, the contact lens wearers in this same study reported that their eye care providers prescribed two-week modalities for longer than two week replacement for 25% and 42% of the time in the United States and Canada, respectively.[14] These findings suggest that replacement schedule recommendations may not be adequately communicated to patients, so patient-reported results may not accurately describe what eye care providers are recommending. It is important, therefore, for eye care providers to clearly communicate and instruct patients on proper lens replacement schedules.
Our sample of contact lens wearers reported that their two-week MRS lenses were prescribed for longer than the MRS almost half of the time, but it is possible that the prescribed replacement was forgotten by the wearer or not communicated clearly by the eye care provider. Regardless of the reason, it is notable that monthly and daily wearers showed nearly complete agreement with the MRS. These findings may suggest that monthly and daily modalities are more likely to result in lens replacement and lens prescribing that complies with MRS for both the wearer and the prescriber.
While MRS affected lens replacement compliance and reported replacement schedule MRS adherence, it did not affect overnight wear compliance. In participants who reported sleeping overnight in their lenses against the prescription of their eye care provider, two-week, monthly, and daily replacement lens wearers were equally likely to sleep in their lenses. Of participants who were non-compliant with overnight wear, about 15% were in a daily replacement modality. This outcome, initially, may be surprising especially considering that daily lenses are intended to be disposed of and replaced daily. Despite having good lens replacement compliance,[3, 29] daily wearers have been reported to have general overnight wear noncompliance.[32] While this survey asked specifically about overnight sleeping in contact lenses, it is possible that participants reported other sleeping episodes, such as napping, when reporting overnight wear. Regardless, considering the increased prevalence of daily replacement prescribing[33, 34] and the fact that our the prevalence of daily replacement wearers in our sample match prescribing trends at the time of the survey (2017), these results should encourage eye care providers to educate all soft lens wearers – even those wearing daily disposable modalities – on appropriate sleeping habits.
Although certain factors appeared to influence lens replacement and overnight wear compliance in this soft contact lens wearing group, lens case replacement was not similarly associated with factors like age, gender, or years of contact lens wear, or MRS. Importantly, contact lens case replacement frequency was not associated with compliance in lens replacement or overnight wear, suggesting that even compliant contact lens wearers are not aware of proper contact lens case replacement. In fact, over 70% of the participants who used a contact lens case were unsure of when the appropriate replacement should be. It is possible that no associations were found between case replacement and demographic factors because there was so much uncertainly about proper lens case care in the sample. The frequency of case replacement in this sample was similar to that reported by Dumbleton et al. in 2011.[3] While suggested case replacement varies, the American Optometric Association recommends that contact lens cases be replaced every three months[35], and The Association of Optometrists and most contact lens solution manufacturers suggest the case be replaced with every new bottle of solution.[36–38]
Unlike other studies that have investigated contact lens compliance,[3, 15, 29, 32] this study was performed in a public setting and not in conjunction with the participants’ eye care providers. Other authors have postulated that participants may respond more candidly when not recruited by their eye care provider and/or in the clinical space where they receive eye care.[39] It is possible that, if this survey were administered to a clinic population that receives regular eye care, the results would be different. Future studies could investigate this hypothesis.
Factors like lens brand, prescribed replacement, and prescribed overnight wear were analyzed based on participant recall alone. Investigators were not able to verify if the lens types and prescribed practices reported by each participant were actually what were instructed by their eye care providers. It is possible, then, that inaccurate participant recall played some part in confounding the results. For instance, it is possible that participants erroneously recalled prescribed lens practices like replacement schedule and/or overnight wear. Even in this instance, the participants were still reporting what they remembered as being instructed. Whether that was correct or not, it represents the effectiveness of the patient education provided by the eye care provider.
In conclusion, this study of a soft contact lens wearing population examined habits associated with lens replacement, overnight wear, and contact lens case replacement. Daily disposable contact lens wearers were most likely to be compliant with lens replacement, but all replacement modalities reported similar compliance with prescribed overnight wear. As well, participants who were non-compliant with prescribed contact lens replacement were more likely to be non-compliant with overnight wear. Contact lens case replacement was not associated with any demographic factor or compliance in lens replacement or overnight wear, suggesting that the general population is poorly educated on contact lens case hygiene. The results of this study indicate that, regardless of lens type or modality, eye care providers should provide clear communication and education about appropriate contact lens habits – especially overnight wear and contact lens case replacement - when fitting and prescribing contact lenses.
Highlights: A Study of Contact Lens Compliance in a Non-Clinical Setting.
Daily replacement contact lens wearers are more likely to be compliant with lens replacement, but all replacement modalities reported similar compliance with prescribed overnight wear.
Contact lens wearers who are non-compliant with prescribed contact lens replacement are more likely to be non-compliant with overnight wear.
Contact lens case replacement was not associated with lens replacement or overnight wear compliance.
Regardless of lens type or modality, eye care providers should provide clear communication and education about appropriate contact lens habits – especially overnight wear and contact lens case replacement - when fitting and prescribing contact lenses.
Funding:
This research received support from the National Eye Institute of the National Institutes of Health (T35 EY007151).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest: None
References
- 1.Robertson DM and Cavanagh HD, Non-compliance with contact lens wear and care practices: a comparative analysis. Optom Vis Sci, 2011. 88(12): p. 1402–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bui TH, et al. , Patient compliance during contact lens wear: perceptions, awareness, and behavior. Eye Contact Lens, 2010. 36(6): p. 334–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dumbleton KA, et al. , The relationship between compliance with lens replacement and contact lens-related problems in silicone hydrogel wearers. Cont Lens Anterior Eye, 2011. 34(5): p. 216–22. [DOI] [PubMed] [Google Scholar]
- 4.Stapleton F, et al. , Risk factors and causative organisms in microbial keratitis in daily disposable contact lens wear. PLoS One, 2017. 12(8): p. e0181343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stapleton F, et al. , Risk factors for moderate and severe microbial keratitis in daily wear contact lens users. Ophthalmology, 2012. 119(8): p. 1516–21. [DOI] [PubMed] [Google Scholar]
- 6.Chalmers RL, et al. , Risk factors for contact lens complications in US clinical practices. Optom Vis Sci, 2010. 87(10): p. 725–35. [DOI] [PubMed] [Google Scholar]
- 7.Chalmers RL, et al. , Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci, 2011. 52(9): p. 6690–6. [DOI] [PubMed] [Google Scholar]
- 8.Muhafiz E, et al. , Evaluation of the ocular surface in different contact lens replacement schedules. Cornea, 2019. Volume ePublished Ahead of Print (January 24). [DOI] [PubMed] [Google Scholar]
- 9.Hickson-Curran S, et al. , The use of daily disposable lenses in problematic reusable contact lens wearers. Cont Lens Anterior Eye, 2014. 37(4): p. 285–91. [DOI] [PubMed] [Google Scholar]
- 10.Nilsson SE and Montan PG, The annualized incidence of contact lens induced keratitis in Sweden and its relation to lens type and wear schedule: results of a 3-month prospective study. CLAO J, 1994. 20(4): p. 225–30. [DOI] [PubMed] [Google Scholar]
- 11.Poggio EC and Abelson MB, Complications and symptoms with disposable daily wear contact lenses and conventional soft daily wear contact lenses. CLAO J, 1993. 19(2): p. 95–102. [PubMed] [Google Scholar]
- 12.Solomon OD, et al. , A 3-year prospective study of the clinical performance of daily disposable contact lenses compared with frequent replacement and conventional daily wear contact lenses. CLAO J, 1996. 22(4): p. 250–7. [PubMed] [Google Scholar]
- 13.Suchecki JK, Ehlers WH, and Donshik PC, A comparison of contact lens-related complications in various daily wear modalities. CLAO J, 2000. 26(4): p. 204–13. [PubMed] [Google Scholar]
- 14.Dumbleton K, et al. , Compliance with contact lens replacement in Canada and the United States. Optom Vis Sci, 2010. 87(2): p. 131–9. [DOI] [PubMed] [Google Scholar]
- 15.Dumbleton K, et al. , Patient and practitioner compliance with silicone hydrogel and daily disposable lens replacement in the United States. Eye Contact Lens, 2009. 35(4): p. 164–71. [DOI] [PubMed] [Google Scholar]
- 16.Richdale K, et al. , Case-Control Pilot Study of Soft Contact Lens Wearers With Corneal Infiltrative Events and Healthy Controls. Invest Ophthalmol Vis Sci, 2016. 57(1): p. 47–55. [DOI] [PubMed] [Google Scholar]
- 17.Stapleton F, et al. , The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology, 2008. 115(10): p. 1655–62. [DOI] [PubMed] [Google Scholar]
- 18.Lim CH, et al. , Risk factors for contact lens-related microbial keratitis in Singapore. Eye (Lond), 2016. 30(3): p. 447–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chalmers RL, et al. , Risk factors for corneal infiltrates with continuous wear of contact lenses. Optom Vis Sci, 2007. 84(7): p. 573–9. [DOI] [PubMed] [Google Scholar]
- 20.Schein OD, et al. , The incidence of microbial keratitis among wearers of a 30-day silicone hydrogel extended-wear contact lens. Ophthalmology, 2005. 112(12): p. 2172–9. [DOI] [PubMed] [Google Scholar]
- 21.Jansen ME, et al. , Characterization of patients who report compliant and non-compliant overnight wear of soft contact lenses. Cont Lens Anterior Eye, 2011. 34(5): p. 229–35. [DOI] [PubMed] [Google Scholar]
- 22.Yung MS, et al. , Microbial contamination of contact lenses and lens care accessories of soft contact lens wearers (university students) in Hong Kong. Ophthalmic Physiol Opt, 2007. 27(1): p. 11–21. [DOI] [PubMed] [Google Scholar]
- 23.Rosenthal RA, et al. , A comparative study of the microbiologic effectiveness of chemical disinfectants and peroxide-neutralizer systems. CLAO J, 1995. 21(2): p. 99–110. [PubMed] [Google Scholar]
- 24.Dumbleton KA, et al. , Ability of patients to recall habitual contact lens products and enhancement of recall using photographic aids. Cont Lens Anterior Eye, 2011. 34(5): p. 236–40. [DOI] [PubMed] [Google Scholar]
- 25.Harris PA, et al. , Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 2009. 42(2): p. 377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Steele KR and Szczotka-Flynn L, Epidemiology of contact lens-induced infiltrates: an updated review. Clin Exp Optom, 2017. 100(5): p. 473–481. [DOI] [PubMed] [Google Scholar]
- 27.Morgan P, et al. , International Contact Lens Prescribing in 2016. Contact Lens Spectrum, 2017. 32(January 2017): p. 30–35. [Google Scholar]
- 28.Morgan P, et al. , International Contact Lens Prescribing in 2017. Contact Lens Spectrum, 2018. 33(January 2018): p. 28–33. [Google Scholar]
- 29.Dumbleton K, et al. , Compliance with lens replacement and the interval between eye examinations. Optom Vis Sci, 2013. 90(4): p. 351–8. [DOI] [PubMed] [Google Scholar]
- 30.Zimmerman AB, et al. , Contact Lens Corneal Inflammatory Events in a University Population. Optom Vis Sci, 2016. 93(1): p. 42–9. [DOI] [PubMed] [Google Scholar]
- 31.Yeung KK, et al. , Compliance with soft contact lens replacement schedules and associated contact lens-related ocular complications: the UCLA Contact Lens Study. Optometry, 2010. 81(11): p. 598–607. [DOI] [PubMed] [Google Scholar]
- 32.Dumbleton KA, et al. , A multi-country assessment of compliance with daily disposable contact lens wear. Cont Lens Anterior Eye, 2013. 36(6): p. 304–12. [DOI] [PubMed] [Google Scholar]
- 33.B Morgan P, et al. , International Contact Lens Prescribing in 2016. Contact Lens Spectrum, January 2018. 32: p. 30–5. [Google Scholar]
- 34.Itoi M, et al. , Trends in Contact Lens Prescribing in Japan (2003–2016). Cont Lens Anterior Eye, 2018. 41(4): p. 369–76. [DOI] [PubMed] [Google Scholar]
- 35.What You Need to Know About Contact Lens Care and Compliance. [Brochure]; Available from: http://www.aoa.org/Documents/public/AOA-contact-lens-hygiene.pdf.
- 36.Alcon Optifree PureMoist Multipurpose Solution. [Package Insert]; Available from: http://www.opti-free.com/pdfs/OFPureMoist_us_en.pdf.
- 37.AMO Revitalens OcuTec Multipurpose Solution Guidelines. Available from: http://www.amoinc.com/products/corneal/multi-purpose-solution/revitalens-ocutec-multi-purpose-disinfecting-solution.
- 38.Advice for Soft Contact Lens Wearers, A.o. Optometrists, Editor.
- 39.Bowling A, Mode of questionnaire administration can have serious effects on data quality. J Public Health (Oxf), 2005. 27(3): p. 281–91. [DOI] [PubMed] [Google Scholar]