Abstract
Sleep is exceedingly important for our physical, physiological, psychological, and social health. Currently, few Koreans get the recommended daily amount of sleep. Stress can also have a major impact on our physiological, neurological, and mental health. In this study, we explored the correlation between sleep duration and perceived stress. The study used data from the Community Health Survey (CHS), 2017, which included 133,444 responses from Koreans. Sleeping time and stress were measured by self-diagnosis. The relationship between sleeping time and stress was analyzed using the chi-square test and multivariable regression. Both men and women felt the most stress when they slept for an average of 6 h a day. The results of the subgroup analysis showed that even when they sleep for the same time, younger people felt more stressed than older people. In the group that slept for an average of 6 h a day, women were the most stressed. We observed a correlation between sleeping time and stress in Korean adults. We found that about 16.7% of Koreans were sleeping for less than 5 h. This is less than the 7–9 h of sleep recommended by the National Sleep Foundation (NSF). In addition, stress was found to increase when sleep was insufficient. In particular, it was also observed that young people who slept for less than 8 h felt stressed more easily.
Keywords: community health survey, sleep duration, stress, national sleep foundation
1. Introduction
Sleep has recently become a popular topic of research among academics. The results of this study show how sleep habits can affect physical, physiological, psychological, and social aspects [1,2,3]. Sleep duration seems particular important: excessively short or long sleep, compared to adequate amounts of sleep, is associated with a higher risk of mortality [4,5,6,7]{Kripke DF, 2002 #1}. In addition, sleep duration is also associated with the onset of various diseases such as depression, hypertension, diabetes, and obesity [8,9,10,11,12]. Both short and excessively long sleep duration (>10 h) appear to be associated with a risk of chronic disease [12,13]. According to a survey conducted by Gallup Korea in 2017, the average sleep duration in South Korea is about 6.5 h [14]. A survey by Statistics Korea, on the other hand, found an average sleep duration among Koreans of 7.7 h. These surveys suggested that many Koreans are not getting the recommended daily amount of 7–9 h of sleep suggested by the National Sleep Foundation (NSF). These averages are also substantially less than the average sleep duration of Organization for Economic Co-Operation and Development (OECD) countries, which is 8.3 h. However, only about 22.8% of Koreans reported being aware that they were not getting enough sleep [15].
Stress can be defined as a physiological reaction to protect our body from external stimuli. It can manifest as a state of physiological arousal and can have profound negative effects, particularly anxiety [16,17]. The autonomic nervous system and hypothalamic-pituitary-adrenal (HPA) axis are the two major bodily systems that govern stress [18,19]. Several experts have categorized stress into “good stress” and “bad stress,” or eustress and distress, respectively [20,21]. Both types of stress can directly or indirectly influence health. One study found a link between psychosocial stress and heart disease [22], while other studies have found that stress can affect the brain [23]. In the same survey that investigated sleep, 54.4% of the respondents felt generally stressed in their daily lives. This finding suggested that numerous people were exposed to stress. Interestingly, that same survey evaluated the prevalence of smoking and drinking and how stress related to attempts to quit these problematic behaviors. Among the respondents who smoked, 47.3% of them reported trying to quit smoking; however, over half of these respondents (52.6%) found that it was difficult to stop smoking because of stress. A similar finding was obtained for alcohol consumption; among those who tried to quit drinking or who tried to drink less, 34.7% said it was too difficult to do so because of stress. These findings suggest that stress can directly affect health, as well as indirectly influence it through the promotion of adverse health-related behavior. There are a number of studies on the correlation between sleep time and mental health worldwide. However, since the study of the relationship between sleep time and stress in Korea is very limited, we conducted this study to see if the same results would be obtained from Koreans.
2. Materials and Methods
2.1. Data Collection and Study Participants
For this study, we used data from the 2017 Community Health Survey, a cross-sectional, nationwide survey conducted by the Korea Centers for Disease Control and Prevention (KCDC). The total number of participants in this survey was 228,381. For this study, we excluded all individuals who did not respond to the question on stress (n = 104). We also excluded participants who did not respond to questions on age (n = 2452), marital status (n = 251), household income (n = 2006), occupational characteristics (n = 81,297), educational level (n = 106), region (n = 8364), smoking (n = 4), alcohol consumption (n = 4), depression (n = 18), suicidal ideation (n = 11), subjective health status (n = 6), physical activity (n = 53), unmet medical needs (n = 4), subjective body recognition (n = 16), and life satisfaction (n = 241). Thus, we analyzed the data of 133,444 participants (71,708 males and 61,736 females) as a representative sample.
2.2. Variables
Our variable of interest was sleep time. The CHS asked “How much sleep do you have per day?”. The questionnaire was designed to make a response in hours and minutes. We classified these as ≤ 8, 7, 6, and <5 h for analysis.
Perceived stress was the dependent variable in this study. To measure it, respondents responded to the following question: “How stressful do you feel in your daily life?” Their response options were “feel very much,” “feel a lot,” “feel a little bit,” “hardly feel it,” and “do not feel it at all.” For the analysis, we categorized individuals who responded with “feel very much,” “feel a lot,” and “feel a little bit” as people who usually felt stressed in their daily lives, while those who responded with “hardly feel it” and “do not feel at all” were classified as people who did not usually feel stressed.
We also measured a number of sociodemographic, economic, health-related characteristics as covariates in the analysis. The sociodemographic characteristics included sex (male, female), age (20–29, 30–39, 40–49, 50–59, ≥60 years), marital status (married, unmarried, previously married (divorced, separated, widowed)), monthly household income (high, medium, medium-high, medium-low, low), occupation characteristics (white collar, pink collar, blue collar work), educational level (elementary school or below, middle school, high school, college, university, graduate school), and region (urban, rural). The health-related behaviors included smoking status (smoker: currently smokes cigarettes every day or occasionally; non-smoker: has never smoked or who has smoked in the past but does not smoke now) and alcohol status (regular alcohol drinkers: 1–16 times per month; non-regular drinkers: <1 time per month using the drinking frequency question for 1). In addition, the following variables were corrected with other covariates: depression (feel, do not feel), suicidal ideation (think suicide, do not think suicide), subjective health level (good, not bad, bad), physical activity(seldomly, 2–3 times, more than 4 times a week), unmet medical need (experienced, not experienced), subjective body recognition (thin, normal, obese), and life satisfaction (dissatisfied, satisfied).
2.3. Statistical Analysis
The chi square test and multiple logistics regression analysis were used to analyze the data. A p-value < 0.05 was considered to indicate a statistically significant result. The chi square test was used to examine the significant difference in stress depending on the sleep duration. Multiple logistic regression analysis was used to determine odds ratios (ORs) and 95% confidence intervals (CIs). Subgroup analysis was performed according to the sleep duration and stress. Statistical analyses were performed using SAS software, version 9.4 (SAS Institute, Cary, NC, USA).
3. Results
3.1. Study Participants
Table 1 shows the general characteristics of the study participants according to whether they felt stressed or not. Of the 71,708 male respondents, 56,976 (79.5%) were classified as people who usually felt stressed and 14,732 (20.5%) were classified as people who did not; of the 61,736 female respondents, 50,439 (81.7%) and 11,297 (18.3%) were categorized as “usually feeling stressed” and “not usually feeling stressed,” respectively.
Table 1.
General characteristics of study observations (2017).
| Variables | Male | Female | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Stress | Non-Stress | p-Value | Total | Stress | Non-Stress | p-Value | ||||||||
| n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) | ||||
| Sleep time (hours) | <0.0001 | <0.0001 | |||||||||||||
| 8 ≤ | 13,019 | 18.2 | 9284 | 71.3 | 3735 | 28.7 | 11,737 | 19.0 | 8925 | 76.0 | 2812 | 24.0 | |||
| 7 | 24,166 | 33.7 | 19,446 | 80.5 | 4720 | 19.5 | 20,260 | 32.8 | 16,584 | 81.9 | 3676 | 18.1 | |||
| 6 | 23,634 | 33.0 | 19,434 | 82.2 | 4200 | 17.8 | 18,596 | 30.1 | 15,702 | 84.4 | 2894 | 15.6 | |||
| <6 | 10,889 | 15.2 | 8812 | 80.9 | 2077 | 19.1 | 11,143 | 18.1 | 9228 | 82.8 | 1915 | 17.2 | |||
| Age (years) | <0.0001 | <0.0001 | |||||||||||||
| 20–29 | 5652 | 7.9 | 4844 | 85.7 | 808 | 14.3 | 6261 | 10.1 | 5711 | 91.2 | 550 | 8.8 | |||
| 30–39 | 12,252 | 17.1 | 11,002 | 89.8 | 1250 | 10.2 | 8618 | 14.0 | 7837 | 90.9 | 781 | 9.1 | |||
| 40–49 | 16,367 | 22.8 | 14,467 | 88.4 | 1900 | 11.6 | 13,663 | 22.1 | 11,932 | 87.3 | 1731 | 12.7 | |||
| 50–59 | 17,364 | 24.2 | 13,895 | 80.0 | 3469 | 20.0 | 15,099 | 24.5 | 12,464 | 82.6 | 2635 | 17.5 | |||
| ≧60 | 20,073 | 28.0 | 12,768 | 63.6 | 7305 | 36.4 | 18,095 | 29.3 | 12,495 | 69.1 | 5600 | 31.0 | |||
| Marital status | <0.0001 | <0.0001 | |||||||||||||
| Married | 55,338 | 77.2 | 43,350 | 78.3 | 11,988 | 21.7 | 41,882 | 67.8 | 34,525 | 82.4 | 7357 | 17.6 | |||
| Once married (divorced, separated, bereavement) | 4649 | 6.5 | 3541 | 76.2 | 1108 | 23.8 | 11,143 | 18.1 | 7989 | 71.7 | 3154 | 28.3 | |||
| Unmarried | 11,721 | 16.4 | 10,085 | 86.0 | 1636 | 14.0 | 8,711 | 14.1 | 7925 | 91.0 | 786 | 9.0 | |||
| Household income | <0.0001 | <0.0001 | |||||||||||||
| Low | 17,080 | 23.8 | 11,573 | 67.8 | 5507 | 32.2 | 19,845 | 32.1 | 14,623 | 73.7 | 5222 | 26.3 | |||
| Medium-Low | 28,038 | 39.1 | 22,780 | 81.3 | 5258 | 18.8 | 19,811 | 32.1 | 16,683 | 84.2 | 3128 | 15.8 | |||
| Medium-High | 16,415 | 22.9 | 14,061 | 85.7 | 2354 | 14.3 | 13,448 | 21.8 | 11,630 | 86.5 | 1818 | 13.5 | |||
| High | 10,175 | 14.2 | 8,562 | 84.2 | 1613 | 15.9 | 8632 | 14.0 | 7503 | 86.9 | 1129 | 13.1 | |||
| Occupational characteristics | <0.0001 | <0.0001 | |||||||||||||
| White collar | 21,508 | 30.0 | 18,659 | 86.8 | 2849 | 13.3 | 19,845 | 32.1 | 17,655 | 89.0 | 2190 | 11.0 | |||
| Pink collar | 9560 | 13.3 | 8050 | 84.2 | 1510 | 15.8 | 16,906 | 27.4 | 14,308 | 84.6 | 2598 | 15.4 | |||
| Blue collar | 40,640 | 56.7 | 30,267 | 74.5 | 10,373 | 25.5 | 24,985 | 40.5 | 18,476 | 74.0 | 6509 | 26.1 | |||
| Educational level | <0.0001 | <0.0001 | |||||||||||||
| Elementary school or less | 8379 | 11.7 | 5090 | 60.8 | 3289 | 39.3 | 15,190 | 24.6 | 10,457 | 68.8 | 4733 | 31.2 | |||
| Middle school | 7830 | 10.9 | 5440 | 69.5 | 2390 | 30.5 | 6880 | 11.1 | 5417 | 78.7 | 1463 | 21.3 | |||
| High school | 23,681 | 33.0 | 19,093 | 80.6 | 4588 | 19.4 | 17,834 | 28.9 | 15,181 | 85.1 | 2653 | 14.9 | |||
| College | 9251 | 12.9 | 8029 | 86.8 | 1222 | 13.2 | 7578 | 12.3 | 6740 | 88.9 | 838 | 11.1 | |||
| University | 18,896 | 26.4 | 16,282 | 86.2 | 2614 | 13.8 | 12,223 | 19.8 | 10,860 | 88.9 | 1363 | 11.2 | |||
| Graduate school | 3671 | 5.1 | 3042 | 82.9 | 629 | 17.1 | 2031 | 3.3 | 1784 | 87.8 | 247 | 12.2 | |||
| Region | <0.0001 | <0.0001 | |||||||||||||
| Urban | 17,661 | 24.6 | 14,909 | 84.4 | 2752 | 15.6 | 14,579 | 23.6 | 12,676 | 87.0 | 1903 | 13.1 | |||
| Rural | 54,047 | 75.4 | 42,067 | 77.8 | 11,980 | 22.2 | 47,157 | 76.4 | 37,763 | 80.1 | 9394 | 19.9 | |||
| Smoking | <0.0001 | <0.0001 | |||||||||||||
| Yes | 27,856 | 38.9 | 23,338 | 83.8 | 4518 | 16.2 | 1886 | 3.1 | 1650 | 87.5 | 236 | 12.5 | |||
| No | 43,852 | 61.2 | 33,638 | 76.7 | 10,214 | 23.3 | 59,850 | 97.0 | 48,789 | 81.5 | 11,061 | 18.5 | |||
| Alcohol consumption | <0.0001 | <0.0001 | |||||||||||||
| Yes | 59,557 | 83.1 | 48,423 | 81.3 | 11,134 | 18.7 | 41,129 | 66.6 | 35,063 | 85.3 | 6066 | 14.8 | |||
| No | 12,151 | 17.0 | 8553 | 70.4 | 3598 | 29.6 | 20,607 | 33.4 | 15,376 | 74.6 | 5231 | 25.4 | |||
| Depression | <0.0001 | <0.0001 | |||||||||||||
| Yes | 2461 | 3.4 | 2344 | 95.3 | 117 | 4.8 | 3910 | 6.3 | 3727 | 95.3 | 183 | 4.7 | |||
| No | 69,247 | 96.6 | 54,632 | 78.9 | 14,615 | 21.1 | 57,826 | 93.7 | 46,712 | 80.8 | 11,114 | 19.2 | |||
| Suicidal ideation | <0.0001 | <0.0001 | |||||||||||||
| Yes | 3185 | 4.4 | 2961 | 93.0 | 224 | 7.0 | 4602 | 7.5 | 4345 | 94.4 | 257 | 5.6 | |||
| No | 68,523 | 95.6 | 54,015 | 78.8 | 14,508 | 21.2 | 57,134 | 92.6 | 46,094 | 80.7 | 11,040 | 19.3 | |||
| Subjective health status | <0.0001 | <0.0001 | |||||||||||||
| Good | 32,342 | 45.1 | 24,642 | 76.2 | 7700 | 23.8 | 22,778 | 36.9 | 17,921 | 78.7 | 4857 | 21.3 | |||
| Not bad | 31,061 | 43.3 | 25,823 | 83.1 | 5238 | 16.9 | 28,618 | 46.4 | 24,180 | 84.5 | 4438 | 15.5 | |||
| Bad | 8305 | 11.6 | 6511 | 78.4 | 1794 | 21.6 | 10,340 | 16.8 | 8338 | 80.6 | 2002 | 19.4 | |||
| Physical activity | <0.0001 | <0.0001 | |||||||||||||
| Seldomly | 52,802 | 73.6 | 41,582 | 78.8 | 11,220 | 21.3 | 51,309 | 83.1 | 41,862 | 81.6 | 9447 | 18.4 | |||
| 2–3 times | 11,070 | 15.4 | 9193 | 83.0 | 1877 | 17.0 | 6182 | 10.0 | 5193 | 84.0 | 989 | 16.0 | |||
| More than 4 times a week | 7836 | 10.9 | 6201 | 79.1 | 1635 | 20.9 | 4245 | 6.9 | 3384 | 79.7 | 861 | 20.3 | |||
| Unmet medical need | <0.0001 | <0.0001 | |||||||||||||
| Yes | 6494 | 9.1 | 5807 | 89.4 | 687 | 10.6 | 8121 | 13.2 | 7327 | 90.2 | 794 | 9.8 | |||
| No | 65,214 | 90.9 | 51,169 | 78.5 | 14,045 | 21.5 | 53,615 | 86.9 | 43,112 | 80.4 | 10,503 | 19.6 | |||
| Subjective body recognition | <0.0001 | <0.0001 | |||||||||||||
| Thin | 13,126 | 18.3 | 10,415 | 79.4 | 2711 | 20.7 | 8580 | 13.9 | 6799 | 79.2 | 1781 | 20.8 | |||
| Normal | 32,814 | 45.8 | 25,262 | 77.0 | 7552 | 23.0 | 27,385 | 44.4 | 22,023 | 80.4 | 5362 | 19.6 | |||
| Obese | 25,768 | 35.9 | 21,299 | 82.7 | 4469 | 17.3 | 25,771 | 41.7 | 21,617 | 83.9 | 4154 | 16.1 | |||
| Life satisfaction | <0.0001 | <0.0001 | |||||||||||||
| Dissatisfaction | 15,804 | 22.0 | 13,566 | 85.8 | 2238 | 14.2 | 15,132 | 24.5 | 13,393 | 88.5 | 1739 | 11.5 | |||
| Satisfaction | 55,904 | 78.0 | 43,410 | 77.7 | 12,494 | 22.4 | 46,604 | 75.5 | 37,046 | 79.5 | 9558 | 20.5 | |||
| Total | 71,708 | 100 | 56,976 | 79.5 | 14,732 | 20.5 | 61,736 | 100 | 50,439 | 81.7 | 11,297 | 18.3 | |||
Among males, 9284 (71.3%) of the 13,019 individuals who slept for more than 8 h per day reported feeling stressed. Of the 24,166 participants who slept for 7 h, 19,446 (80.5%) reported feeling stressed. Of the 23,634 participants who slept for 6 h, 19,434 (82.2%) reported feeling stressed. Finally, among the 10,889 males who slept less than 6 h per day, 8812 (80.9%) indicated that they were feeling stressed. As for females, 8925 (76.0%) of the 11,737 who reported sleeping for more than 8 h usually felt stressed. Of the 20,260 females who slept for 7 h per day, 16,584 (81.9%) mentioned feeling stressed. In addition, 18,596 (84.4%) of the 18,596 females who slept for 6 h reported feeling stressed. Finally, among the 11,143 females who slept less than 6 h, 9228 (82.8%) reported feeling stressed.
3.2. Factors that Predict Perceived Stress
Table 2 shows the results of the logistic regression analysis with sleep duration and stress as the main independent and dependent variables, respectively. Both males and females showed increased odds of feeling stressed when the slept for less than 8 h per day. Specifically, males who slept for 7 h, 6 h, and less than 6 h had 1.38 (95% CI: 1.31–1.45), 1.42 (95% CI: 1.35–1.45), and 1.39 (95% CI: 1.30–1.48) times the odds of feeling stressed as did males who slept for 8 h or more, respectively. A similar trend was found among females: those who slept for 7 h, 6 h, and less than 6 h per day had 1.40 (95% CI: 1.32–1.48), 1.69 (95% CI: 1.59–1.80), and 1.33 times (CI: 1.52-1.75) the odds of feeling stressed as did females who slept for 8 h or more. A number of other variables were associated with stress, including age, occupational characteristics, education level, depression, suicidal ideation, unmet need medical, and life satisfaction. Thus, we performed a subgroup analysis with these variables.
Table 2.
Logistic regression analysis of the association between stress and sleep duration.
| Variables | Male | Female | ||||||
|---|---|---|---|---|---|---|---|---|
| Adj.OR | 95% CI | Adj.OR | 95% CI | |||||
| Sleep time (hours) | ||||||||
| 8 ≤ | 1.00 | – | – | 1.00 | – | – | ||
| 7 | 1.38 | (1.31 | – | 1.45) | 1.40 | (1.32 | – | 1.48) |
| 6 | 1.42 | (1.35 | – | 1.50) | 1.69 | (1.59 | – | 1.80) |
| < 6 | 1.39 | (1.30 | – | 1.48) | 1.63 | (1.52 | – | 1.75) |
| Age (years) | ||||||||
| 20–29 | 3.04 | (2.71 | – | 3.41) | 2.99 | (2.58 | – | 3.47) |
| 30–39 | 3.69 | (3.39 | – | 4.02) | 3.01 | (2.69 | – | 3.36) |
| 40–49 | 3.09 | (2.89 | – | 3.32) | 2.12 | (1.94 | – | 2.32) |
| 50–59 | 1.74 | (1.65 | – | 1.84) | 1.59 | (1.49 | – | 1.71) |
| ≧ 60 | 1.00 | – | – | 1.00 | – | – | ||
| Marital status | ||||||||
| Married | 1.20 | (1.11 | – | 1.30) | 1.00 | (0.89 | – | 1.12) |
| Once married (divorced, separated, bereavement) | 1.04 | (0.93 | – | 1.15) | 0.67 | (0.59 | – | 0.75) |
| Unmarried | 1.00 | – | – | 1.00 | – | – | ||
| Household income | ||||||||
| Low | 0.73 | (0.68 | – | 0.79) | 0.88 | (0.81 | – | 0.96) |
| Medium–Low | 0.94 | (0.88 | – | 1.01) | 1.04 | (0.96 | – | 1.13) |
| Medium–High | 1.10 | (1.02 | – | 1.18) | 0.99 | (0.91 | – | 1.07) |
| High | 1.00 | – | – | 1.00 | – | – | ||
| Occupational characteristics | ||||||||
| White collar | 1.44 | (1.35 | – | 1.52) | 1.45 | (1.34 | – | 1.58) |
| Pink collar | 1.28 | (1.20 | – | 1.37) | 1.34 | (1.27 | – | 1.43) |
| Blue collar | 1.00 | – | – | 1.00 | – | – | ||
| Educational level | ||||||||
| Elementary school or less | 1.00 | – | – | 1.00 | – | – | ||
| Middle school | 1.29 | (1.20 | – | 1.38) | 1.35 | (1.25 | – | 1.45) |
| High school | 1.45 | (1.36 | – | 1.55) | 1.44 | (1.33 | – | 1.56) |
| College | 1.56 | (1.42 | – | 1.72) | 1.51 | (1.35 | – | 1.69) |
| University | 1.52 | (1.40 | – | 1.65) | 1.48 | (1.33 | – | 1.65) |
| Graduate school | 1.26 | (1.12 | – | 1.42) | 1.46 | (1.23 | – | 1.72) |
| Region | ||||||||
| Urban | 1.13 | (1.08 | – | 1.19) | 1.15 | (1.09 | – | 1.22) |
| Rural | 1.00 | – | – | 1.00 | – | – | ||
| Smoking | ||||||||
| Yes | 1.15 | (1.10 | – | 1.20) | 1.02 | (0.87 | – | 1.18) |
| No | 1.00 | – | – | 1.00 | – | – | ||
| Alcohol consumption | ||||||||
| Yes | 1.20 | (1.14 | – | 1.26) | 1.30 | (1.24 | – | 1.37) |
| No | 1.00 | – | – | 1.00 | – | – | ||
| Depression | ||||||||
| Yes | 3.11 | (2.55 | – | 3.79) | 2.77 | (2.36 | – | 3.24) |
| No | 1.00 | – | – | 1.00 | – | – | ||
| Suicidal ideation | ||||||||
| Yes | 2.82 | (2.44 | – | 3.27) | 2.93 | (2.56 | – | 3.36) |
| No | 1.00 | – | – | 1.00 | – | – | ||
| Subjective health status | ||||||||
| Good | 1.00 | – | – | 1.00 | – | – | ||
| Not bad | 1.76 | (1.68 | – | 1.84) | 1.80 | (1.71 | – | 1.89) |
| Bad | 1.87 | (1.75 | – | 2.00) | 2.14 | (2.00 | – | 2.30) |
| Physical activity | ||||||||
| Seldomly | 1.00 | – | – | 1.00 | – | – | ||
| 2–3 times | 0.98 | (0.92 | – | 1.04) | 1.05 | (0.96 | – | 1.14) |
| More than 4 times a week | 1.08 | (1.00 | – | 1.17) | 1.06 | (0.95 | – | 1.19) |
| Unmet medical need | ||||||||
| Yes | 1.65 | (1.52 | – | 1.80) | 1.68 | (1.55 | – | 1.82) |
| No | 1.00 | – | – | 1.00 | – | – | ||
| Subjective body recognition | ||||||||
| Thin | 1.09 | (1.03 | – | 1.15) | 1.00 | (0.94 | – | 1.07) |
| Normal | 0.97 | (0.92 | – | 1.01) | 0.95 | (0.90 | – | 0.99) |
| Obese | 1.00 | – | – | 1.00 | – | – | ||
| Life satisfaction | ||||||||
| Dissatisfaction | 1.99 | (1.88 | – | 2.10) | 2.25 | (2.12 | – | 2.38) |
| Satisfaction | 1.00 | – | – | 1.00 | – | – | ||
3.3. Association between Sleep Duration and Stress Stratified by Age
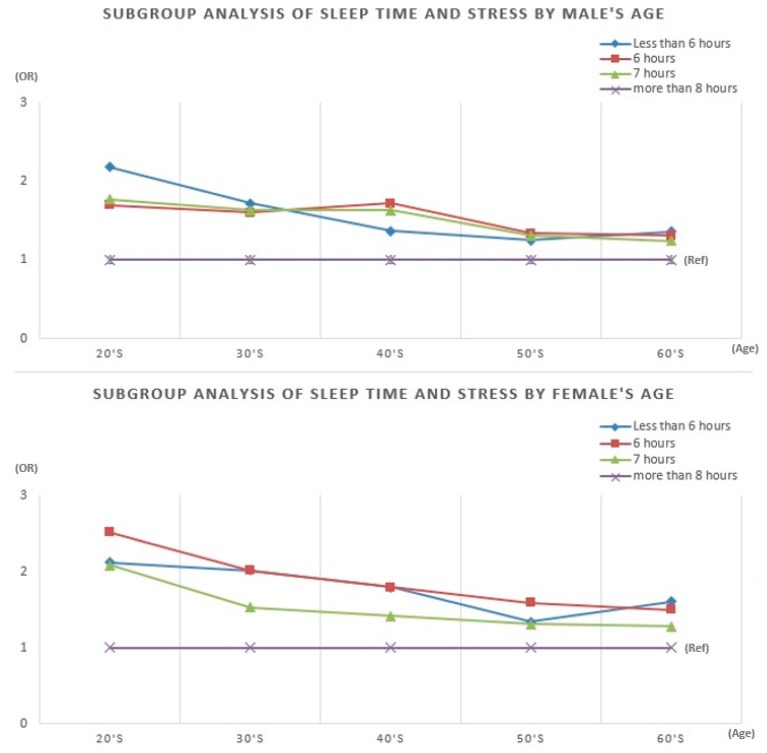
Figure 1 presents the results of the subgroup analysis by age. The results generally corresponded to those of the total sample: individuals who slept less than 8 h had higher odds of feeling stressed. We also found that, for each age group, the effect of sleep duration was stronger for females than for males. Among males in their 20s and 30s, the odds ratios were highest for those who slept less than 5 h. By contrast, among males in their 40s, the odds ratios were highest for those who reported sleeping for 6 h. The odds ratios did not differ much among those in their 50s and 60s. Among women, except for those in their 60s, the odds ratios were consistently highest for individuals who reported sleeping for 6 h. This phenomenon was somewhat different among females in their 20s and 50s, but were similar among those in their 30s, 40s, and 60s.
Figure 1.
Subgroup analysis of sleep time and stress by age.
4. Discussion
This study was conducted to identify the relationship between daily sleep duration and perceived stress among adults over 20 years of age. There is currently much research on the relationship between sleep duration and aspects of mental health, such as depression and suicidal thoughts. Sleep is an essential element of everyday life that is closely related to health [24,25,26]. A recent hypothesis on the effects of sleep is that the brain adapts to our ever-changing environment through synaptic strengthening during wakefulness, while sleep helps to down-regulate this synaptic strengthening. Thus, insufficient sleep can adversely affect mental health [27]. In addition to mental health, sleep is exceedingly important for our physiology. For example, during sleep, cell growth and immune function are enhanced. Melatonin is the most active hormone secreted by humans during sleep, which plays an important role in controlling biorhythm. Melatonin also oxidizes cells to detoxify active oxygen, which causes aging, and engages in antitumor activities [28]. Sleep deprivation can promote the secretion of ghrelin and reduce leptin secretion, which are both associated with obesity. Ghrelin is a hormone secreted in the stomach that increases appetite—it is often called the “fasting hormone” because its levels increase rapidly during fasting and decrease after meals. A lack of sleep is known to increase ghrelin levels by up to 30%. Leptin is a hormone that acts in opposition to ghrelin by suppressing the appetite; people show reduced secretion of leptin when they are sleep deprived [29].
The present study showed a positive correlation between sleep duration and perceived stress among Korean adults. More specifically, people who sleep less than the NSF’s recommended daily amount of 7–9 h had higher odds of stress. In addition, we found that women had higher odds of stress than men for the same sleep durations. When examining the findings by age, younger participants also tended to experience higher odds of stress when their sleep was below the recommended daily amount. People who are stressed due to a lack of sleep appear to be more likely to commit suicide [30]. We hope that our findings will help to emphasize the need for publicity, education, and institutional improvement to ensure that Koreans have adequate sleep duration.
Nevertheless, this study has some limitations. First, the cross-sectional design prevents us from inferring any causal relationships between sleep duration and stress. Second, the Community Health Survey evaluated average sleep duration per day based on the respondent’s memory. This likely led to recall bias. Third, we measured self-reported stress in this study. Experimental testing is necessary for a more accurate measurement of stress. Assessing stress levels with one question about stress may hardly reflect the actual stress levels. While it is possible to assess how stressed people feel subjectively, measurement bias or error can lead to inaccuracies in the relationship of stress to other subjective variables.
Despite these limitations, our study has several strengths. First, we used primary data suitable for Korean studies. These data are sufficient to confirm the average stress levels among Koreans because they were extracted from 133,444 questionnaires. Second, we confirmed that there is a correlation between sleep duration and stress, which suggests that publicity and education aimed at lowering stress among Koreans should focus on sleep. Furthermore, it calls for systemic environmental changes to ensure that Koreans can get enough sleep.
5. Conclusions
We have found that almost half of all Koreans get less sleep than is recommended by the NSF. According to our findings, this might suggest that Koreans are frequently stressed. Furthermore, younger people tended to have higher odds of stress when they lacked sleep. Therefore, measures should be taken to ensure that individuals in their 20s and 30s get adequate sleep.
Acknowledgments
We are grateful to the Korea Centers for Disease Control and Prevention (KCDC) that conducted the Community Health Survey which is the primary source of our study.
Author Contributions
Conceptualization, H.J.K. and J.H.J.; Formal analysis, H.J.K. and S.Y.O.; Methodology, H.J.K. and D.-W.C.; Supervision, E.-C.P.; Writing—original draft, H.J.K.; Writing—review & editing, E.-C.P.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of Interest
The authors declare that there is no conflict of interest.
References
- 1.Atkinson G., Davenne D. Relationships between sleep, physical activity and human health. Physiol. Behav. 2007;90:229–235. doi: 10.1016/j.physbeh.2006.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Freedman R.R., Sattler H.L. Physiological and psychological factors in sleep-onset insomnia. J. Abnorm. Psychol. 1982;91:380. doi: 10.1037/0021-843X.91.5.380. [DOI] [PubMed] [Google Scholar]
- 3.Molinari S., Foulkes D. Tonic and phasic events during sleep: psychological correlates and implications. Percept. Motor Skill. 1969;29:343–368. doi: 10.2466/pms.1969.29.2.343. [DOI] [PubMed] [Google Scholar]
- 4.Kripke D.F., Garfinkel L., Wingard D.L., Klauber M.R., Marler M.R. Mortality associated with sleep duration and insomnia. Rch. Gen. Psychiat. 2002;59:131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 5.Tamakoshi A., Ohno Y., JACC Study Group Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–54. [PubMed] [Google Scholar]
- 6.Patel S.R., Ayas N.T., Malhotra M.R., White D.P., Schernhammer E.S., Speizer F., Stampfer M.J., Hu F.B. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 7.Youngstedt S.D., Kripke D.F. Long sleep and mortality: rationale for sleep restriction. Sleep Med. Rev. 2004;8:159–174. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 8.Yaggi H.K., Araujo A.B., McKinlay J.B. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29:657–661. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 9.Chaput J.P., Després J.P., Bouchard C., Astrup A., Tremblay A. Sleep duration as a risk factor for the development of type 2 diabetes or impaired glucose tolerance: analyses of the Quebec Family Study. Sleep Med. 2009;10:919–924. doi: 10.1016/j.sleep.2008.09.016. [DOI] [PubMed] [Google Scholar]
- 10.Ayas N.T., White D.P., Al-Delaimy W.K., Manson J.E., Stampfer M.J., Speizer F.E., Patel S., Hu F.B. A prospective study of self-reported sleep duration and incident diabetes in women. Diabetes care. 2003;26:380–384. doi: 10.2337/diacare.26.2.380. [DOI] [PubMed] [Google Scholar]
- 11.Chaput J.P., Després J.P., Bouchard C., Tremblay A. The association between sleep duration and weight gain in adults: a 6-year prospective study from the Quebec Family Study. Sleep. 2008;31:517–523. doi: 10.1093/sleep/31.4.517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grandner M.A., Kripke D.F. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosom. Med. 2004;66:239. doi: 10.1097/01.PSY.0000107881.53228.4D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.King C.R., Knutson K.L., Rathouz P.J., Sidney S., Liu K., Lauderdale D.S. Short sleep duration and incident coronary artery calcification. Jama. 2008;300:2859–2866. doi: 10.1001/jama.2008.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gallup Korea Survey of Sleep and Dream. [(accessed on 10 September 2018)]; Available online: http://www.gallup.co.kr/gallupdb/reportContent.asp?seqNo=846.
- 15.Statistics Korea 2018 Social research results. [(accessed on 10 September 2018)]; Available online: http://kostat.go.kr/portal/korea/index.action.
- 16.Folkman S. Encyclopedia of Behavioral Medicine. Springer; New York, NY, USA: 2013. Stress: Appraisal and coping; pp. 1913–1915. [Google Scholar]
- 17.H S. The Stress of Life. McGraw-Hill Companies; New York, NY, USA: 1956. [Google Scholar]
- 18.Ulrich-Lai Y.M., Herman J.P. Neural regulation of endocrine and autonomic stress responses. Nat. Rev. Neurosci. 2009;10:397. doi: 10.1038/nrn2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stephens M.A.C., Wand G. Stress and the HPA axi: Role of glucocorticoids in alcohol dependence. Alcohol Res-Curr. Rev. 2012;34:468–483. [PMC free article] [PubMed] [Google Scholar]
- 20.Le F.M., Matheny J., Kolt G.S. Eustress, distress, and interpretation in occupational stress. J. Manag. Psychol. 2003;18:726–744. [Google Scholar]
- 21.Kranner I., Minibayeva F.V., Beckett R.P., Seal C.E. What is stress? Concepts, definitions and applications in seed science. New Phytol. 2010;188:655–673. doi: 10.1111/j.1469-8137.2010.03461.x. [DOI] [PubMed] [Google Scholar]
- 22.Stansfeld S.A., Marmot M.G. Stress and the Heart: Psychosocial Pathways to Coronary Heart Disease. BMJ books; Hoboken, New Jersey, USA: 2002. [Google Scholar]
- 23.De K.E.R., Joëls M., Holsboer F. Stress and the brain: from adaptation to disease. Nat. Rev. Neurosci. 2005;6:463. doi: 10.1038/nrn1683. [DOI] [PubMed] [Google Scholar]
- 24.Sabo E., Reynolds C.F., Kupfer D.J., Berman S.R. Sleep, depression, and suicide. Psychiat. Res. 1991;36:265–277. doi: 10.1016/0165-1781(91)90025-K. [DOI] [PubMed] [Google Scholar]
- 25.Tsuno N., Besset A., Ritchie K. Sleep and depression. J. Clin. Psychiat. 2005;66:1254–1269. doi: 10.4088/JCP.v66n1008. [DOI] [PubMed] [Google Scholar]
- 26.Perlman C.A., Johnson S.L., Mellman T.A. The prospective impact of sleep duration on depression and mania. Bipolar Disord. 2006;8:271–274. doi: 10.1111/j.1399-5618.2006.00330.x. [DOI] [PubMed] [Google Scholar]
- 27.Bushey D., Tononi G., Cirelli C. Sleep and synaptic homeostasis: structural evidence in Drosophila. Science. 2011;332:1576–1581. doi: 10.1126/science.1202839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Turek F.W., Gillette M.U. Melatonin, sleep, and circadian rhythms: rationale for development of specific melatonin agonists. Sleep Med. 2004;5:523–532. doi: 10.1016/j.sleep.2004.07.009. [DOI] [PubMed] [Google Scholar]
- 29.Vendrell J., Broch M., Vilarrasa N., Molina A., Gómez J.M., Gutiérrez C., Simón I., Soler J., Richart C. Resistin, adiponectin, ghrelin, leptin, and proinflammatory cytokines: relationships in obesity. Obesity. 2004;12:962–971. doi: 10.1038/oby.2004.118. [DOI] [PubMed] [Google Scholar]
- 30.Goodwin R.D., Marusic A. Association between short sleep and suicidal ideation and suicide attempt among adults in the general population. Sleep. 2008;31:1097–1101. [PMC free article] [PubMed] [Google Scholar]