Abstract
Objectives:
To assess the effectiveness of a high resolution ultrasound for temporomandibular joint (TMJ) evaluation in comparison to MRI in patients with TMJ disorders.
Methods:
Our study comprised 50 patients (35 female and 15 male) with a mean age of 30.61. Clinical examination was performed. Bilateral imaging of TMJ was conducted by using a high-resolution ultrasound and 1.5 Tesla MR. Diagnostic accuracy of ultrasound was assessed for disc displacement and joint effusion in comparison to MRI. Sensitivity (Se), specificity (Sp), positive predictive value (PPV), negative predictive value (NPV), and accuracy (Ac) were calculated for ultrasound. Measurements were compared by Bland & Altman and intraclass correlation coefficient (ICC). Significance level was set at p < 0.05.
Results:
Most frequent complaints were noise 42 (84%) and 34 (68%) pain. For disc position assessment with ultrasound for both sides and closed-open mouth, sensitivity, specificity, PPV, NPV and accuracy ranged between, 0.88 – 1, 0.60 – 0.87, 0.70 – 0.97, 0.75 – 1, and 0.84 – 0.98, respectively. For the diagnosis of effusion with ultrasound for both sides, sensitivity, specificity, PPV, NPV and accuracy ranged between 0.65 – 0.81, 0.91 – 1, 0.96 – 1, 0.45 – 0.46 and 0.72 – 0.84, respectively. ICC values calculated for intraobserver agreement for right and left TMJ for all measurements were found to be statistically significant (p < 0.001). ICC values ranged between 0.964 and 0.995 suggesting excellent correlation among ultrasound and MRI. In general, for ultrasound measurements we found a mean difference ranging between −0.182 and +0.130 mm in comparison to MRI.
Conclusion:
Ultrasound can be suggested as an adjunct to common imaging modalities in the assessment of TMJ.
Keywords: ultrasound, temporomandibular joint, MRI
Introduction
The temporomandibular joint (TMJ) is a composite ginglymus-arthrodial joint that is composed of the condyle, glenoid fossa, articular tubercle, articular disc, retrodiscal tissue, synovial membrane, and joint capsule. Temporomandibular joint disorders (TMD) do not only affect TMJ but also the masticatory muscles and other components of the stomatognatic system.1 Pringle et al., were the first to report and define TMD in 1918.2 Although the aetiology of TMD is not fully understood yet, presence of trauma, degenerative disease, inflammation, para-functional habits, postural condition, occlusal microtrauma, orthodontic disorders, systemic predisposition, sleep disorders, and deleterious psychosocial alterations were all proposed as risk factors.3
A common form of TMD is the internal derangement that manifests as displacement of the disc as a result of instability between condyle, temporal bone and articular disc components. Anterior disc displacement is more frequently discovered in comparison to posterior, medial and lateral displacements. Internal derangements may also be divided into three different subgroups as follows: (1) disc displacement with reduction, (2) disc displacement without reduction, (3) disc displacement without reduction and limited mouth opening.4,5 TMJ effusion, the excessive accumulation of fluid in and around TMJ, is an inflammatory response that occurs as a result of internal derangement, trauma, arthritis, and inflammatory changes related to rheumatoid diseases. Osteoarthritis is characterized by degenerative changes of TMJ structures, and irregularities of the condyle.6–8 TMD affects 28% of the world population6 and may present clinical signs such as; TMJ pain, articular noises, and restricted jaw function.7,8 Restricted jaw opening and joint pain have a negative effect on the patients’ quality of life, therefore, accurate diagnosis of TMD is essential in order to render an appropriate treatment plan.9
In conjunction with medical history and clinical examination, MRI, arthrography, and CBCT are the techniques which are preferred for TMJ imaging in order to make accurate diagnosis. Arthrography is an invasive method that may be complicated by pain and allergic reactions. MRI is a powerful and versatile imaging modality utilized in various medical fields. Three-dimensional (3D) MRI assessment of morphology and function without ionizing radiation attracted attention in dental applications during 1980s.10,11 MRI is accepted as the reference standard for the diagnostic imaging of TMJ disorders related to articular disc structure and position along with changes in soft tissues and synovial fluid, however; low availability, long time requirement, and high cost preclude its routine use. In addition, MR is contraindicated for patients with claustrophobia, pacemaker and metal prosthesis.9–12 The ability to provide high-resolution and accurate multiplanar reformatted images with a lower dose than multidetector CT (MDCT) made CBCT the imaging modality of choice for assessing osseous components of the TMJ. Reformatted CBCT images provide useful information for the diagnosis of a variety of TMJ related entities, including subchondral cyst, flattening and sclerosis of condylar structures, osteophyte formation and idiopathic condylar resorption. However, patient is subjected to ionizing radiation and visualization of TMJ soft tissue structures and the articular disc is not possible with CBCT.13–15
In response to the high demand for a technique that could provide real time images at a low cost and without ionizing radiation, a group of scientists proposed ultrasound imaging as an alternative technique in the beginning of 1990s.16 In diagnostic ultrasound, high frequency sound waves are transmitted into the body by use of a transducer and echoes from tissue interface are detected and displayed on a screen. Sound waves are emitted from the ultrasound transducer via piezoelectric crystals. TMJ ultrasonography may be considered as an onsite, comfortable, easy to use, fast and low cost technique.17,18 With ultrasound, immediate assessment of condylar translation, disc position, and articular effusion is possible.19–21 Our objective was therefore to assess the effectiveness of a high resolution ultrasound for the diagnosis of disc position and effusion, in comparison to MRI, in patients who referred to our clinic with TMJ complaints. In addition, patient history and clinical examination findings were critically analyzed.
Methods and materials
Ethical approval was obtained from Ankara University, Faculty of Dentistry, Ethics Committee (36290600/72-14/1). Our study comprised 50 patients (35 female and 15 male) admitted to Dentomaxillofacial Radiology Department between January 2017 and June 2017 with complaints of TMJ and who met certain criteria as follows: (1) Patients with pain and/or noise in TMJ region, limited mouth opening, and/or tinnitus. (2) Patients diagnosed with TMD during clinical and radiological examination (MRI, ultrasound and/or CBCT). (3) Patients, whose, TMJs could be visualized by use of ultrasound probe. Besides, patients who received previous trauma to TMJ region, who had orthognathic surgery, who were under active orthodontic treatment and patients with syndromes effecting dentomaxillofacial region were not included in the present research.
Clinical evaluation and diagnostic imaging
Clinical evaluation was performed and recorded by one researcher (oral and maxillofacial radiologist) with 10 years of clinical experience in TMJ patients, who also blindly and separately assessed the diagnostic images with the two techniques obtained later. In case of uncertainty, consensus was reached by consulting another experienced researcher (oral and maxillofacial radiologist). A specific calibration session prior to data collection was conducted on a patient with TMD who was not included in the study. An informed consent was obtained from each patient. During patient history taking and clinical examination, difficulty when opening jaw in the morning, pain during jaw opening and closing, pain in the ear and cheek region, tinnitus, clenching, prior referral to a dentist due to TMJ complaint, prior use of night guards along with pain in the muscles (lateral pterygoid muscle, medial pterygoid muscle, and masseter muscle) were all assessed. Thereafter, bilateral imaging of TMJ by using ultrasound was conducted and TMJs were assessed for each patient. Bilateral TMJ MRI of the patients were also obtained and reported for each patient. Diagnostic accuracy of ultrasound was assessed for disc displacement and joint effusion along with measurement accuracy of various TMJ related structures in comparison to MRI.
Ultrasonography
Ultrasound imaging was performed by using a high-resolution (5–14 MHz) ACUSON S 2000 ultrasound machine (Siemens, Munich, Germany) with a “hockey stick” transducer when patients were in supine position by one researcher (oral and maxillofacial radiologist with 10 years of experience in TMJ patients). Considering our pilot studies, hockey stick probe was preferred due to TMJ image quality difference between hockey stick probe and linear probe. Figure 1 shows images obtained by using both probes. Ultrasound image obtained by using hockey stick probe clearly demonstrates all TMJ-related structures. In case of uncertainty, a consensus was reached after consulting another researcher with more experience (oral and maxillofacial radiologist with 15 years of experience). Transducer was placed extraorally on left TMJ and first positioned transversally and then longitudinally in closed and open mouth positions and images were obtained. The same procedure was also repeated for the right TMJ. When obtaining closed mouth ultrasound images, transducer was placed transversally and positioned parallel to the zygomatic arc and Frankfurt plane and perpendicular to ramus. When obtaining open mouth ultrasound images, transducer was positioned transversally with a 60°−70° angle to the Frankfurt plane. The operator constantly adjusted the position of the transducer during condylar translation from closed mouth position to open mouth position for better visibility of the disc. Real-time movement was utilized for the assessment of disc displacement whereas static images were utilized for conducting ultrasound measurements. Ultrasound images of condyle and articular eminence appeared as two different hyperechoic lines whereas articular disc appeared as hypoechoic thin band between these two lines. However, disc also appeared as isoechoic (regions that produce ultrasound echoes equal to those of neighbouring tissues) in some cases. Besides, joint capsule, pterygoid muscle and retrodiscal tissues all appeared as isoechoic. Figure 2 shows ultrasound image of left TMJ with normal disc position in closed mouth position of a male patient. (A) Positioning of “hockey stick” probe in transversal plane; (B) anatomical landmarks observed in transversal plane; (C) positioning of “hockey stick” probe in longitudinal plane; and (D) anatomical landmarks observed in transversal plane. With ultrasound, assessment and measurement of specific structures were conducted as follows:
Figure 1.
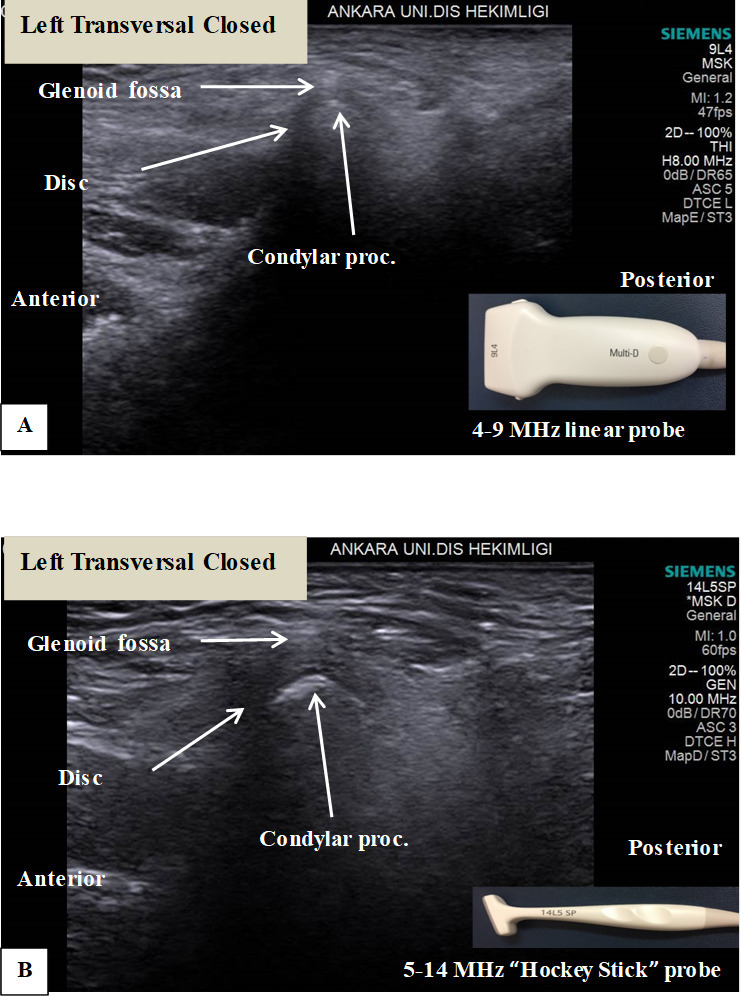
Ultrasound images obtained by using both probes from the same patient’s left closed TMJ in transversal position. (A) Ultrasound image obtained by using linear probe; (B) ultrasound image obtained by using hockey stick probe. Ultrasound image obtained by using hockey stick probe clearly demonstrates all TMJ related structures. TMJ, temporomandibular joint.
Figure 2.
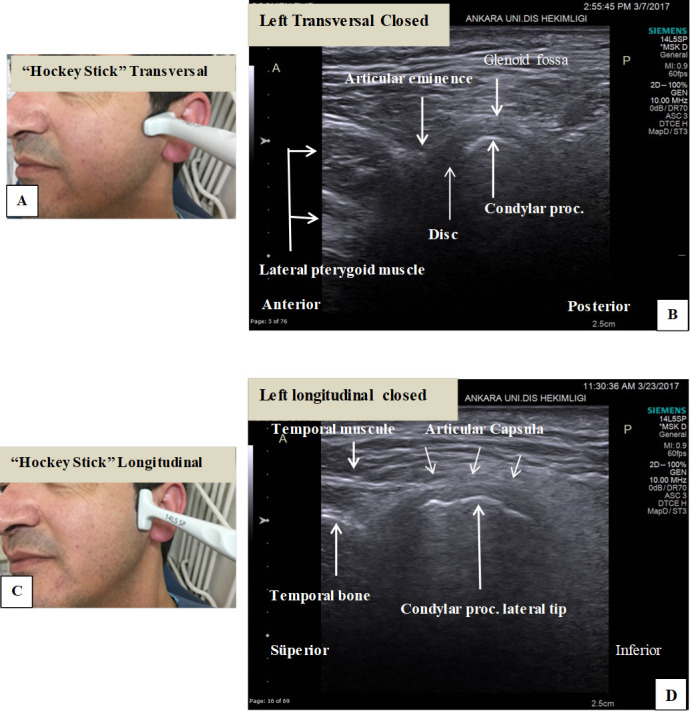
Ultrasound imaging of left TMJ with normal disc position in closed mouth position of a male patient. (A) Positioning of “hockey stick” probe in transversal plane; (B) Anatomical landmarks observed in transversal plane; (C) Positioning of “hockey stick” probe in longitudinal plane; and (D) Anatomical landmarks observed in longitudinal plane. TMJ, temporomandibular joint
(1) Articular disc position was assessed in transversal plane in both closed and open mouth situation. For open mouth ultrasound images, articular disc was considered as normal if it was located superior to condyle, whereas anterior disc displacement was considered if the disc was positioned anterior to mandibular condyle. For closed mouth ultrasound images, articular disc was considered as normal if it was located between condyle and articular eminence, whereas anterior disc displacement was considered if the disc was positioned anterior to mandibular condyle and inferior to articular eminence. Figures 3–5 show, TMJ images (ultrasound and MRI) of patients with normal disc position, anterior disc displacement with reduction, and anterior disc displacement without reduction, respectively.
Figure 3.
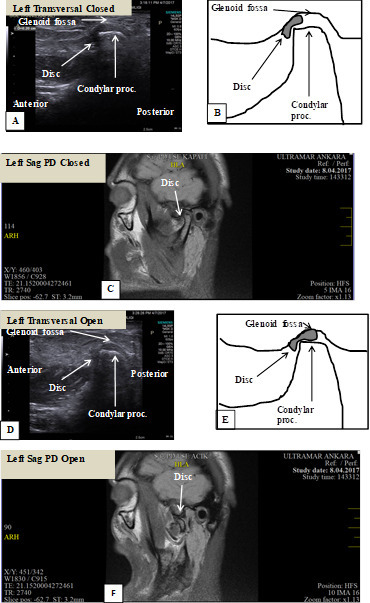
A 26-year-old male patient referred with the complaints of clicking and pain during mouth opening in left TMJ. Disc is in normal position in left TMJ. (A) Closed mouth ultrasound (transducer placed transversally) image; (B) schematic drawing of closed mouth ultrasound (transducer placed transversally) image; (C) closed mouth MRI (sagittal plane) image of the patient showing left TMJ with normal disc position; (D) open mouth ultrasound (transducer placed transversally) image; (E) schematic drawing of open mouth ultrasound (transducer placed transversally) image; (F) open mouth MRI (sagittal plane) image of the patient showing left TMJ with normal disc position. TMJ, temporomandibular joint.
Figure 4.
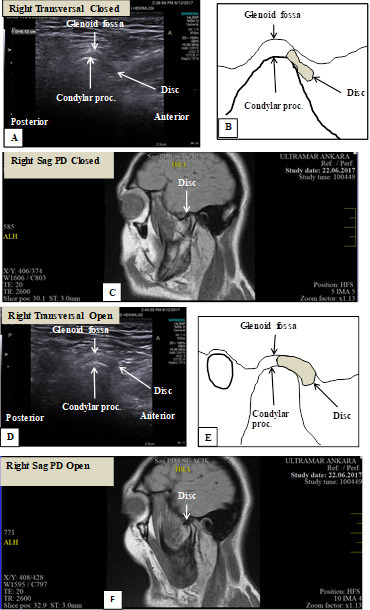
A 21-year-old female patient referred with limited mouth opening and clicking during mouth opening in right TMJ. (A) Closed mouth ultrasound (transducer placed transversally) image with disc in anterior position; (B) schematic drawing of closed mouth ultrasound (transducer placed transversally) image with disc in anterior position; (C) closed mouth MRI (sagittal plane) image of the patient showing right TMJ with anteriorly positioned disc; (D) closed mouth ultrasound (transducer placed transversally) image with disc in normal position; (E) schematic drawing of open mouth ultrasound (transducer placed transversally) image with disc in normal position; (F) open mouth MRI (sagittal plane) image of the patient showing right TMJ with anterior disc displacement with reduction. TMJ, temporomandibular joint.
Figure 5.
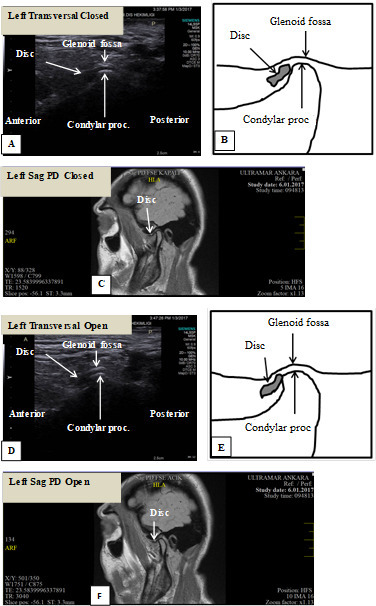
A 26-year-old female patient referred with complaints of limited mouth opening and pain in left TMJ. Condylar flattening and degenerative changes are observed. (A) Closed mouth ultrasound (transducer placed transversally) image with disc in anterior position; (B) schematic drawing of closed mouth ultrasound (transducer placed transversally) image with disc in anterior position; (C) closed mouth MRI (sagittal plane) image of the patient showing left TMJ with anteriorly positioned disc; (D) open mouth ultrasound (transducer placed transversally) image with disc in anterior position; (E) schematic drawing of open mouth ultrasound (transducer placed transversally) image with disc in anterior position; and (F) open mouth MRI (sagittal plane) image of the patient showing left TMJ with anterior disc displacement without reduction. TMJ, temporomandibular joint.
(2) Both in transversal and longitudinal transducer positions synovial fluid increase in TMJ space was assessed. In transversal position, for closed mouth measurement, distance between mandibular condyle and glenoid fossa was measured at three points twice and the highest value was recorded, whereas, for open mouth measurement, distance between posterior articular eminence and mandibular condyle was measured at three points twice and the highest value was recorded. Prior to our study, ultrasound imaging was conducted on 15 patients (who were not included in the present study) with available MR images with effusion in TMJ. Our pilot ultrasound measurements from those patients were in accordance with a previous study.22 Therefore, measurements higher than 1.76 mm were considered as an increase in synovial fluid thickness leading to TMJ effusion.22 In longitudinal position, in both closed and open mouth positions, distance between TMJ capsule and lateral pole of mandibular condyle was measured at three points twice and the highest value was recorded, thereby; the effect of synovial fluid increase in the space between capsule and mandibular condyle was determined.
Magnetic resonance imaging
MRI were obtained by utilizing General Electric HDI 1.5 Tesla machine (GE, Milwaukee, WI). In both closed and open mouth positions T1W (T1 weighted) images which demonstrates differences in the T1 relaxation times of tissues, Multiple Echo Recombined Gradient Echo that offers high resolution and Proton Density (PD) series images of bilateral TMJs were obtained with sagittal and coronal oblique reconstructions. Disc position and effusion were evaluated from 3 mm thickness slices by an oral and maxillofacial radiology specialist independently in a separate session. With MRI, articular disc is visualized as biconcave shaped with low signal intensity. Mandibular condyle, bone marrow are seen as homogenous high signal at T1W and PD-weighted images, whereas, as medium signal intensity at T2 weighted images. Bone marrow edema is seen as low intensity signal at T1W and PD-weighted images, whereas, as high signal intensity at T2 weighted images. Sclerosis and fibrosis of TMJ are seen as low signal intensity at T1W, PD-weighted and T2 weighted images. Osteonecrosis is observed as heterogenic signal intensity.23 Figures 3–5 show TMJ images (ultrasound and MRI) of patients with normal disc position, anterior disc displacement with reduction, and anterior disc displacement without reduction, respectively.
Following gold standard measurements were also obtained from MRI images by using proprietary software in the MRI scanner software: (1) At mouth closed position, distance between glenoid fossa and mandibular condyle were measured at three points twice and the highest value was recorded on sagittal oblique planes (transversal). (2) At open mouth position, distance between articular eminence and mandibular condyle was measured at three points twice and the highest value was recorded on sagittal oblique planes (transversal). (3) At both closed and open mouth positions distance between joint capsule and lateral end of mandibular condyle was measured at three points twice and the highest value was recorded on coronal oblique planes (longitudinal). “Measure distance” tool was selected and distances were measured by clicking the mouse and enhancement tools (density and contrast adjustment and zoom function) were used when deemed necessary. Figure 6 shows MRI and ultrasound images of a patient with joint effusion in left TMJ. Finally, following responses were recorded twice by the researcher within 1 week interval. For the disc position: displacement with reduction, displacement without reduction or normal disc position. For joint effusion: a yes or no response.
Figure 6.
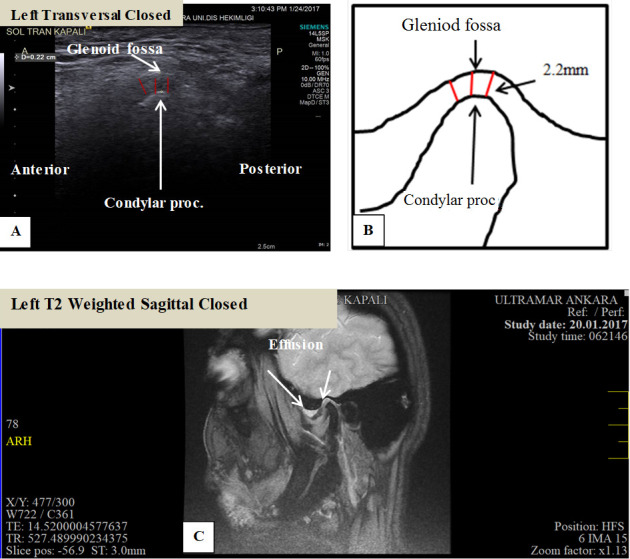
MRI and ultrasound images of left TMJ of a 55-year-old female patient with joint effusion. The patient was referred with the complaints of severe pain and limitation in mouth opening. (A) Measurement of the distance between mandibular condyle and glenoid fossa on transversal ultrasound image in left closed mouth position; (B) schematic drawing of measurement of the distance between mandibular condyle and glenoid fossa on transversal ultrasound image in left closed mouth position. Measurements higher than 1.76 mm were considered as an increase in synovial fluid thickness leading to joint effusion; (C) sagittal T2 weighted MRI image of the same patient showing joint effusion with high signal intensity anterosuperiorly.
Statistical Analysis
Descriptive statistics were given as mean, median, standard deviation, minimum and maximum values for continuous data. Percentage values were given for intermittent data. Chi square/Fisher’s Exact Test were used for the comparison of intermittent data. Sensitivity (Se), specificity (Spe), positive predictive value (PPV), negative predictive value (NPV), and accuracy (Ac) were calculated for ultrasound as compared to gold-standard MRI. Measurements obtained by using ultrasound and MRI techniques were compared and assessed by Bland & Altman and intraclass correlation coefficient (ICC). Significance level was set at p < 0.05.
Results
There was a total of 50 patients, 35 females (70%) and 15 males (30%) aged between 17 and 75 (mean 30.61 ± standard deviation 1.856; median = 26). According to patient history and clinical examination most frequent complaints were noise 42 (84%) and 34 (68%) pain during opening and closing mouth. Pain was mostly prominent in the ear region with 26 (52%) patients. Masticatory pain was observed in 36 patients (72%) and most frequently, lateral pterygoid muscle was tender to palpation with 31 patients (62%). 95.8% of the patients with limited mouth opening in the morning had muscle pain as well (p < 0.001). 42.3% of the patients (11 out of 26) had mouth splint treatment for at least 1 year approximately 1 year prior to our examination. Patient history and clinical examination findings are given in Table 1.
Table 1.
Distribution of patient history and clinical examination findings
| n | % | |
| Difficulty during jaw opening in the morning | ||
| No | 26 | 52 |
| Yes | 24 | 48 |
| Pain during jaw opening and closing | ||
| No | 16 | 32 |
| Yes | 34 | 68 |
| Pain in the ear region | ||
| No | 24 | 48 |
| Yes | 26 | 52 |
| Pain in the cheek region | ||
| No | 41 | 82 |
| Yes | 9 | 18 |
| Tinnitus | ||
| No | 8 | 16 |
| Yes | 42 | 84 |
| Clenching | ||
| No | 19 | 38 |
| Yes | 31 | 62 |
| Prior referral to a dentist with TMJ complaint | ||
| No | 24 | 48 |
| Yes | 26 | 52 |
| Prior usage of night guards | ||
| No | 39 | 78 |
| Yes | 11 | 22 |
| Pain in the muscles | ||
| No | 14 | 28 |
| Yes | 36 | 72 |
| Lateral pterygoid pain | ||
| No | 19 | 38 |
| Yes | 31 | 62 |
| Medial pterygoid pain | ||
| No | 27 | 54 |
| Yes | 23 | 46 |
| Masseter pain | ||
| No | 27 | 54 |
| Yes | 23 | 46 |
MRI assessment revealed disc displacement with reduction in 28 (56%) patients, disc displacement without reduction in 17 (34%) patients, and normal disc position in 5 (10%) patients for left TMJ and disc displacement with reduction in 29 (58%) patients, disc displacement without reduction in 16 (32%) patients, and normal disc position in 5 (10%) patients for right TMJ. The most frequent type of internal derangement was disc displacement with reduction on both sides in 21 patients (42%). Of the 17 patients who were diagnosed as disc displacement without reduction on the left side, 15 had effusion, whereas, on the right side, of the 16 patients who were diagnosed as disc displacement without reduction, 14 had effusion. Table 2 shows the distribution of disc displacement and effusion found by using MRI.
Table 2.
Distribution of disc displacement and effusion found by using MRI
| Left TMJ effusion | Disc displacement with reduction | Disc displacement without reduction | Normal disc position | Total |
| No | 7 (58.3%) |
2 (16.7%) |
3 (25%) |
12 (100%) |
| Yes | 21 (55.3%) |
15 (39.5%) |
2 (5.3%) |
38 (100%) |
| Total | 28 (56%) |
17 (34%) |
5 (100%) |
50 (100%) |
| Right TMJ effusion | Disc displacement with reduction | Disc displacement without reduction | Normal disc position | Total |
| No | 4 (57.1%) |
2 (28.6%) |
1 (14.3%) |
7 (100%) |
| Yes | 25 (58.1%9 |
14 (32.6%) |
4 (9.3%) |
43 (100%) |
| Total | 29 (58%) |
16 (32%) |
5 (10%) |
50 (100%) |
TMJ, temporomandibular joint.
Patients who had unilateral chewing habit had higher rates of anterior disc displacement (p < 0.05) and joint effusion (p < 0.05) when compared to patients who did not have unilateral chewing habit. Average mouth opening was found to be 3.94 + 1.02 cm, median 4 cm, min – max 1–5.8 cm. Number of patients with anterior disc displacement who had mouth opening smaller than 3.5 cm was higher when compared to patients who had mouth opening larger than 3.5 cm (p < 0.05). Number of patients with anterior disc displacement who had lateral pterygoid muscle pain was lower than with that of who had no lateral pterygoid muscle pain (p < 0.05). Number of patients with anterior disc displacement who had pain or limitation during lateral and protrusive movement of the jaw was higher than that of who had no pain or limitation during lateral and protrusive movement of the jaw (p < 0.05). The percentage of effusion in patients with pain during protrusion was found to be higher when compared to patients without pain during protrusion (p < 0.05).
We found a significant positive correlation between transversal and longitudinal measurements conducted by using gold standard MRI images on both sides (r = 0.768 for right TMJ and r = 0.741 for left TMJ, p = 0.000). Table 3 shows Se, Sp, PPV, NPV and Ac values found for ultrasound imaging in comparison to MRI for both left and right TMJs. For anterior disc position assessment with ultrasound for both sides and closed-open mouth, sensitivity, specificity, PPV, NPV and accuracy ranged between, 0.88–1, 0.60–0.87, 0.70–0.97, 0.75–1, and 0.84–0.98, respectively. For the diagnosis of effusion with ultrasound for both sides, sensitivity, specificity, PPV, NPV and accuracy ranged between 0.65–0.81, 0.91–1, 0.96–1, 0.45–0.46 and 0.72–0.84, respectively.
Table 3.
Se, Sp, PPV, NPV and Ac values found for ultrasound imaging in comparison to MRI with 95% CI and min-max values for both left and right TMJs
| Sensitivity 95 % CI |
Specificity 95 % CI |
PPV 95 % CI |
NPV 95 % CI |
Accuracy values | |
| Left closed disc position | 0.978 (0.884–0.996) |
0.600 (0.231–0.882) |
0.956 (0.846–0.992) |
0.750 (0.604–0.857) |
0.940 |
| Left open disc position | 0.882 (0.657–0.967) |
0.879 (0.727–0.952) |
0.789 (0.647–0.887) |
0.935 (0.819–0.982) |
0.880 |
| Left effusion presence | 0.658 (0.499–0.768) |
0.917 0.646–0.985) |
0.961 (0.853–0.994) |
0.458 (0.319–0.604) |
0.720 |
| Right closed disc position | 1.000 (0.921–1.000) |
0.800 (0.375–0.964) |
0.978 (0.877–0.999) |
1.000 (0.911–0.998) |
0.980 |
| Right open disc position | 0.875 (0.639–0.965) |
0.823 (0.664–0.916) |
0.700 (0.552–0.817) |
0.933 (0.8156–0.981) |
0.840 |
| Right effusion presence | 0.814 (0.674–0.903) |
1.000 (0.546–1.000) |
1.000 (0.911–998) |
0.467 (0.327–0.612) |
0.840 |
Ac, accuracy; CI, confidence interval; NPV, negative predictive value; PPV, positive predictive value; Se, sensitivity; Spe, specificity.
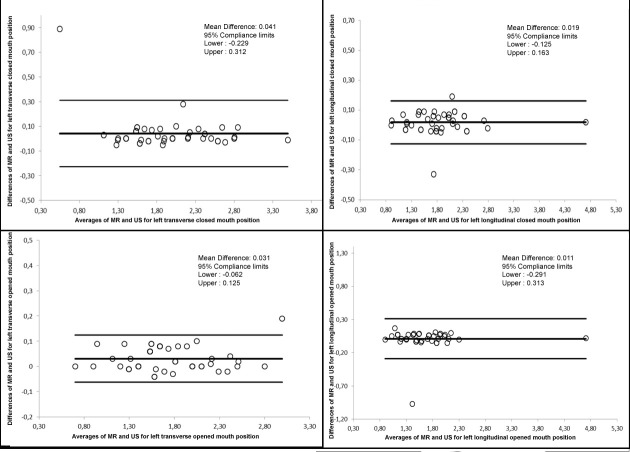
ICC values calculated for intraobserver agreement for right and left TMJ ranged between 0.096 and 0.999. For all measurements intraobserver agreement was found to be statistically significant (p < 0.001). Table 4 shows ICC values for MRI and ultrasound measurements for both left and right TMJs. ICC values ranged between 0.964 and 0.995 suggesting excellent correlation among both methods. Table 5 shows average measurement differences between MRI and ultrasound according to jaw position and transducer localization. In general, for ultrasound measurements we found a mean difference ranging between −0.182 and +0.130 mm in comparison to MRI measurements. Figure 7 shows Bland & Altman graphics of ultrasound and MRI measurement correlation according to jaw position and transducer localization on both TMJ sides.
Table 4.
ICC values for MRI and ultrasound measurements for both left and right TMJs
| Intra Class Correlation | p | 95% Confidence interval | ||
| Lower limit | Upper limit | |||
| MR left transversal closed & ultrasonography left transversal closed |
0.971 | 0.000 | 0.950 | 0.984 |
| MR left longitudinal closed & ultrasonography left longitudinal closed | 0.993 | 0.000 | 0.987 | 0.996 |
| MR left transversal open & ultrasonography left transversal open |
0.995 | 0.000 | 0.992 | 0.997 |
| MR left longitudinal open & ultrasonographies left longitudinal open | 0.964 | 0.000 | 0.938 | 0.980 |
| MR right transversal closed & ultrasonography right transversal closed |
0.988 | 0.000 | 0.979 | 0.993 |
| MR right longitudinal closed & ultrasonography right longitudinal closed | 0.993 | 0.000 | 0.987 | 0.996 |
| MR right transversal open & ultrasonography right transversal open |
0.995 | 0.000 | 0.991 | 0.997 |
| MR right longitudinal open & ultrasonography right longitudinal open | 0.991 | 0.000 | 0.984 | 0.995 |
ICC, intraclass correlation coefficient; TMJ, temporomandibular joint.
Table 5.
Average measurement differences between MRI and ultrasoundS according to jaw position and transducer localization
| Difference | Compliance limits (95%) | ||||
| N | Average | Standard deviation | Lower | Upper | |
| MR & ultrasonography left transversal closed | 50 | 0.041 | 0.134 | −0.229 | 0.312 |
| MR & ultrasonography left longitudinal closed | 50 | 0.019 | 0.071 | −0.125 | 0.163 |
| MR & ultrasonography left transversal open | 50 | 0.031 | 0.046 | −0.062 | 0.125 |
| MR & ultrasonography left longitudinal open | 50 | 0.011 | 0.150 | −0.291 | 0.313 |
| MR & ultrasonography right transversal closed | 50 | 0.032 | 0.069 | −0.106 | 0.171 |
| MR & ultrasonography right longitudinal closed | 50 | 0.016 | 0.056 | −0.096 | 0.129 |
| MR & ultrasonography right transversal open | 50 | 0.027 | 0.043 | −0.059 | 0.113 |
| MR & ultrasonography right longitudinal open | 50 | 0.026 | 0.132 | −0.079 | 0.132 |
Figure 7.
Bland & Altman graphics of ultrasound and MRI measurement correlation according to jaw position and transducer localization on both TMJ sides. TMJ, temporomandibular joint.
Discussion
Diagnosis of TMJ mainly depends on patient history and clinical examination in conjunction with various imaging techniques. The choice of an accurate and reliable imaging modality in the assessment of TMJ is clinically important in terms of diagnosis and selection of treatment approach. Thereby, patient comfort is maintained and psychologic and economic stress on the patient is relieved. Panoramic radiography, CBCT, arthrography and MRI are utilized for diagnostic assessment of TMJ.24–27Our research was designed to assess and compare ultrasound and MRI techniques for the assessment of disc position and effusion in patients with TMJ complaints along with clinical symptoms. We found high Se, Spe, Ac, PPV, and NPV for ultrasound imaging for the assessment of TMJ in terms of anterior disc position and effusion. In addition, measurements obtained from ultrasound images highly correlated with those of MRI measurements. MRI has been used in the TMJ, specifically to determine the disc position. MRI do not only shows the presence or absence of disc displacement but also associated bony changes. The TMJ disc may be stuck in a normal or displaced position and limits the normal degree of condylar translation, which results in restricted jaw opening. However, clinical significance of disc displacement is not always definite since disc displacement may also be observed in asymptomatic patients. Therefore, in the present study we assessed gold standard MR images in conjunction with patient history and clinical examination findings.28
Ultrasound is an operator—and—patient dependent imaging modality and this phenomenon should be taken into consideration when evaluating ultrasound findings. In addition, depending on the patient and tissues ultrasonic characteristics and resistance to propagation of ultrasound waves—the acoustic impedance—may vary. In particular, weight of the patient, excessive fat tissue, gender (sideburn in male patients), and patient age (decreased water concentration in elderly) may all negatively affect image quality.24–27 We found a high prevalence of TMJ disorders which can be explained by the fact that only patients with TMJ complaints were included in the present research. Obviously, it was neither ethical nor practical to obtain ultrasound and MRI from patients with no TMJ complaints as the control group. Ultrasound can be preferred as an adjunct to commonly utilized imaging modalities in the assessment of TMJ owing to its non-ionizing nature, availability, ease of usage, and real time rapid imaging at a low cost.
Another recent pilot study conducted by Katzberg et al.29 assessed disc displacement in only six patients, by using 15 MHz “hockey stick” transducer intraorally in transversal position. Due to difficulties during positioning of the transducer the condyle and subcondylar surface were visible in 10 of 10 joints (100%), and the disc in 7 of 10 joints (70%). Authors confirmed the correlation with ultrasound and MRI for disc position and configuration in the five joints with MRI findings. Although, we utilized a similar transducer in the transversal position in order to assess disc position, unlike mentioned study we preferred using extra oral approach due to difficulties which may occur as a result of application, patient cooperation and sterilization issues when using the transducer intraorally. Considering the visibility of structures we were able to observe and evaluate all TMJ structures in all patients.
Bradlmaier et al.30 assessed TMJs of 48 patients for the presence or absence of disc displacement by placing 12 MHz linear transducer longitudinally. For closed mouth position, they found Se 0.93, Spe 0.77, Ac 0.87, PPV 0.86 and NPV 0.88, whereas, for open mouth position they found Se 0.63, Spe 0.89, Ac 0.80, PPV 0.74 and NPV 0.85. In the present clinical research, in order to assess TMJ disc position we placed the transducer in transversal position since we had a better vision of the condyle and articular eminence when transducer was placed parallel to the zygomatic arch in comparison to longitudinal positioning which was parallel to the ramus. On both sides, we determined disc displacement on the basis of disc position according to condyle. Also, transversal positioning of the 4–15 MHz “hokey stick” transducer enabled better visualization and localization of disc during mouth opening. The operator constantly adjusted the position of the transducer during condylar translation from closed mouth position to open mouth position for better visibility of the disc. Higher Se, Spe, PPV, NPV, and Ac values found in the present study when compared to previous studies17,30 in which authors placed linear transducer in a longitudinal position validate the use of our methodological approach.
Emshoff et al.31 assessed TMJs of 29 patients for the presence of disc displacement, by placing 12 MHz linear transducer both in transversal and longitudinal positions. Analogous to our findings, for closed mouth position, they found Ac 0.91, PPV 0.97 and NPV 0.81, whereas, for open mouth position, they found Ac 0.93, PPV 0.88 and NPV 0.97. In fact, in general, previous studies revealed lower accuracy values when compared to ours. Bonafé et al.32 assessed TMJs of 40 patients for the presence of disc displacement, by placing 5–12 MHz linear transducer both in transversal and longitudinal directions. For closed mouth position, they found Se 0.22, Spe 0.96, PPV 0.81 and NPV 0.64, whereas, for open mouth position they found Se 0, Spe 0.98, PPV 0 and NPV 0.91. Abdel Razek et al.33 assessed TMJs of 22 patients for anterior and lateral-medial disc displacement, by placing 12 MHz linear transducer both in transversal and longitudinal directions. For anterior disc displacement, they found Se 0.79, Spe 0.72, Ac 0.77, PPV 0.88 and NPV 0.57, whereas, for lateral-medial disc displacement they found Se 0.75, Spe 0.63, Ac 0.66, PPV 0.42 and NPV 0.87. In the present study, we did not focus on the direction of disc displacement since it was almost impossible to detect medial or lateral displacement with ultrasound and most of our patients showed anterior disc displacement with or without reduction. Therefore, comparison of the findings obtained from anterior and mediolateral disc displacement was out of our scope. In addition, previous ultrasound studies conducted on knee joint34,35 revealed that ultrasound was a safe non-invasive imaging modality that could be used for the diagnosis of different disorders involving the knee joint. The advantages of ultrasound included low cost, portability, real-time assessment, and facilitated side-by-side-comparisons.34,35 Authors, also found excellent interobserver agreement for most diagnostic tasks related to knee joint with ultrasound.35 Main difference between TMJ and knee joint assessment with ultrasound probe is that when assessing TMJ, unlike knee joint, the operator is only able to approach from lateral aspect of the TMJ. This can be considered as a major limitation of TMJ assessment with ultrasound in comparison to other parts of musculoskeletal system.
Tognini et al.36 assessed TMJs of 41 patients for the presence of disc displacement, by placing 8–20 MHz linear transducer both in transversal and longitudinal directions and they found Se 0.65, Spe 0.80, Ac 0.73, PPV 0.77 and NPV 0.70. Landes et al.37 assessed TMJs of 33 patients for the presence of disc displacement by placing 8–12.5 MHz linear transducer transversally. For closed mouth position, they found Se 0.63, Spe 0.47, Ac 0.55, PPV 0.50 and NPV 0.61, whereas, for open mouth position they found Se 0.43, Spe 0.78, Ac 0.73, PPV 0.42 and NPV 0.85. We found more accurate results in the assessment of disc displacement when compared to mentioned studies.36,37 Apart from using a high resolution hockey stick transducer in a transversal position for assessing disc position, it is possible that observer performance, study design, and patient selection might all cause discrepancies between different study findings and ours regarding disc displacement assessment.
TMJ effusion may occur as a result of internal derangement, trauma, arthritis, or inflammatory changes related to rheumatoid diseases.38 Several studies proved ultrasound to be effective in the evaluation of effusion in large joints, however; studies regarding small joints like TMJ are sparse.39 Joint effusion causes enlargement of joint capsule and observed as anechoic or hypoechoic in ultrasound images40,41Manfredini et al.42 assessed 69 patients by using 8–20 MHz linear transducer longitudinally and transversally for the detection of effusion. For the measurement of the distance between articular capsule and condyle, values higher than 1.95 mm and 2.15 mm were considered as effusion. For the threshold value of 1.95 mm, PPV was 0.83, NPV was 0.26 and sensitivity was high and for the threshold value of 2.15 mm, PPV was 0.71, NPV was 0.11 and specificity was high. In the present study, for the diagnosis of effusion with ultrasound for both sides, sensitivity, specificity, PPV, NPV and accuracy ranged between 0.65–0.81, 0.91–1, 0.96–1, 0.45–0.46 and 0.72–0.84, respectively. Higher values found in our study might be attributable to threshold value which was taken as 1.76 mm. In a previous study conducted by Assaf et al,22 measurements higher than 1.76 mm were considered as an increase in synovial fluid thickness leading to joint effusion.22 While Assaf et al,22 assessed joint effusion both as “sonographically visible joint effusion in the joint in current inflammatory activity” and “specific measurements higher than the threshold value” it was not possible to visualize joint effusion in the present study. Therefore, we diagnosed effusion on the basis of specific measurements conducted on ultrasound and assessment of gold standard MR images. In addition, the threshold value of 1.76 mm reported by Assaf et al,22 was found to be clinically realistic by our team.
Bas et al.43 in their study assessed 91 patients by placing 10 MHz linear transducer longitudinally and transversally and investigated the relationship between effusion and pain. Authors accepted 1.66 mm as the threshold value for effusion and scored pain level according to visual analogue scale (VAS). However, unlike our study, authors did not compare ultrasound and MRI for the evaluation of effusion. For measurements lower than 1.65 mm VAS was found to be 2.2, whereas, for measurements higher than 1.65 mm VAS was 3.75 suggesting that there was a positive correlation between pain scores and ultrasound capsule thickness measurements (R2 = 0.137; R2 = 0.370). We also found that the percentage of effusion in patients with pain during protrusion was higher when compared to patients without pain during protrusion.
In a previous pilot study conducted by Jank et al.10 by using 2D and 3D ultrasound imaging, TMJ disc displacement, condylar degeneration, and effusion were assessed in closed and open mouth positions in 100 patients. However, unlike the present study, authors did not give detailed information regarding the frequency and position of the transducer and the method used to assess different variables. For disc displacement assessment in closed mouth position, high resolution ultrasound device revealed, 0.92, 0.92, 0.92, 0.96 and 0.84, Sey, Spe, Ac rate, PPV and NPV, whereas, in open mouth position, 0.86, 0.91, 0.90, 0.86 and 0.92, Se, Spe, Ac rate, PPV and NPV, respectively. Authors also found, 0.81, 1, 0.95, 0.93, and 0.93 for Se, Spe, Ac rate, PPV and NPV, respectively, for the diagnosis of effusion with ultrasound. Higher rates obtained in the mentioned study might be related to transducer and technique used, study design, patient characteristics and experience of operator. It is possible that a 3D ultrasound system that was chosen for the mentioned study could enhance observer performance in TMJ evaluation. Assessment of the 3D visualization properties of ultrasound and fusion of ultrasound images with other image modalities in the dentomaxillofacial region may be the subject of further research.
A recently published systemic review and meta-analysis44 recommend ultrasound imaging be used for the assessment of suspected disc displacement in selected cases to supplement clinical examination and that combined static and dynamic examinations using high-resolution ultrasound may be utilized for gaining this information. However, in the presence of clinical signs or symptoms, ultrasound imaging is only advised after sufficient training and calibration of operating and interpretation. This recommendation is based on evidence that ultrasound is an operator and patient dependent modality and, therefore; variations among different cases should be minimized. For routine clinical practice, a standardized protocol for the diagnostic use of ultrasound in conjunction with certain reference standards for different disease processes may help effective use of ultrasound in TMJ patients.44
Up until now, medical radiologists acted as observers in most of the previous studies comparing diagnostic effectiveness of TMJ pathology with ultrasound and MRI. In our notion, considering the fact that as dentomaxillofacial radiologists are dentists and have detailed information regarding TMJ anatomy, pathology, and occlusion, TMJ reporting and assessment with ultrasound and MRI should be conducted by them. In the present research, all images obtained from 50 patients were evaluated by one researcher twice. In case of uncertainty, consensus was reached by consulting another experienced researcher. In order to assess interobserver agreement and increase the impact of the research’ we belıeve that performıng a study with more patients and observers would be more contributive to the literature. Our further research will also focus on ultrasound assessment of muscular disorders and changes in muscles that is an important component of TMJ, which may occur as a result of TMD and vice versa.
Conclusion
In consideration to high Se, Spe, Ac, PPV, and NPV found for the assessment of anterior disc position and effusion along with highly accurate measurements, ultrasound can be suggested as an adjunct to common imaging modalities in the assessment of TMJ for oral and maxillofacial radiologists due to its advantages such as; non-ionizing radiation, availability, ease of usage, and providing real-time rapid images at a low cost.
Footnotes
Acknowledgment: Authors are grateful to Nazmiye Kurşun for her statistical assistance.
REFERENCES
- 1.Fonseca RJ, Marciani RD, Turvey TA, Heir GM. Assessing temporomandibular disorders : (edsOral and maxillofacial surgery. Elsevier: The British Institute of Radiology.; 2009. [Google Scholar]
- 2.Pringle JH. Displacement of the mandibular meniscus and its treatment. Br J Surg 1918; 6: 385–9. doi: 10.1002/bjs.1800062307 [DOI] [Google Scholar]
- 3.Okeson JP. Etiology of functional disturbances in the masticatory system : Okeson J. P, Management of Temporomandibular Disorders and Occlusion. 4th edn Mosby: The British Institute of Radiology.; 1998. 149–79. [Google Scholar]
- 4.Al-Baghdadi M, Durham J, Araujo-Soares V, Robalino S, Errington L, Steele J. TMJ disc displacement without reduction management: a systematic review. J Dent Res 2014; 93(7 Suppl): 37S–51. doi: 10.1177/0022034514528333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Whyte AM, McNamara D, Rosenberg I, Whyte AW. Magnetic resonance imaging in the evaluation of temporomandibular joint disc displacement--a review of 144 cases. Int J Oral Maxillofac Surg 2006; 35: 696–703. doi: 10.1016/j.ijom.2005.12.005 [DOI] [PubMed] [Google Scholar]
- 6.Maizlin ZV, Nutia N, Dent PB. Displacement of temporomandibular joint disc: correlation between clinical findings and MRI characteristics. J Can Dent Assoc 2010; 76: 1–5. [PubMed] [Google Scholar]
- 7.Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 1992; 6: 301–55. [PubMed] [Google Scholar]
- 8.Peroz I, Tai S. Masticatory performance in patients with anterior disk displacement without reduction in comparison with symptom-free volunteers. Eur J Oral Sci 2002; 110: 341–4. doi: 10.1034/j.1600-0722.2002.21284.x [DOI] [PubMed] [Google Scholar]
- 9.Jung Y-W, Park S-H, On S-W, Song S-I. Correlation between clinical symptoms and magnetic resonance imaging findings in patients with temporomandibular joint internal derangement. J Korean Assoc Oral Maxillofac Surg 2015; 41: 125–32. doi: 10.5125/jkaoms.2015.41.3.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jank S, Emshoff R, Norer B, Missmann M, Nicasi A, Strobl H, et al. Diagnostic quality of dynamic high-resolution ultrasonography of the TMJ--a pilot study. Int J Oral Maxillofac Surg 2005; 34: 132–7. doi: 10.1016/j.ijom.2004.03.014 [DOI] [PubMed] [Google Scholar]
- 11.NÖ Y, Kamburoglu K. Magnetic resonance imaging in dentistry. OMICS J Radiology 2014; 3. [Google Scholar]
- 12.Elias FM, Birman EG, Matsuda CK, Oliveira IRdeS, Jorge WA. Ultrasonographic findings in normal temporomandibular joints. Braz Oral Res 2006; 20: 25–32. doi: 10.1590/S1806-83242006000100006 [DOI] [PubMed] [Google Scholar]
- 13.Peck CC, Goulet J-P, Lobbezoo F, Schıffman EL, Alstergren P, Anderson GC, et al. Expanding the taxonomy of the diagnostic criteria for temporomandibular disorders. J Oral Rehabil 2014; 41: 2–23. doi: 10.1111/joor.12132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barghan S, Tetradis S, Mallya S. Application of cone beam computed tomography for assessment of the temporomandibular joints. Aust Dent J 2012; 57 Suppl 1(Suppl 1): 109–18. doi: 10.1111/j.1834-7819.2011.01663.x [DOI] [PubMed] [Google Scholar]
- 15.Alkhader M, Ohbayashi N, Tetsumura A, Nakamura S, Okochi K, Momin MA, et al. Diagnostic performance of magnetic resonance imaging for detecting osseous abnormalities of the temporomandibular joint and its correlation with cone beam computed tomography. Dentomaxillofac Radiol 2010; 39: 270–6. doi: 10.1259/dmfr/25151578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evirgen Şehrazat, Kamburoğlu K, . Review on the applications of ultrasonography in dentomaxillofacial region. World J Radiol 2016; 8: 50–8. doi: 10.4329/wjr.v8.i1.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jank S, Rudisch A, Bodner G, Brandlmaier I, Gerhard S, Emshoff R. High-resolution ultrasonography of the TMJ: helpful diagnostic approach for patients with TMJ disorders ? J Craniomaxillofac Surg 2001; 29: 366–71. doi: 10.1054/jcms.2001.0252 [DOI] [PubMed] [Google Scholar]
- 18.Pereira LJ, Gavião MBD, Bonjardim LR, Castelo PM. Ultrasound and tomographic evaluation of temporomandibular joints in adolescents with and without signs and symptoms of temporomandibular disorders: a pilot study. Dentomaxillofac Radiol 2007; 36: 402–8. doi: 10.1259/dmfr/16641858 [DOI] [PubMed] [Google Scholar]
- 19.Landes CA, Goral WA, Sader R, Mack MG. 3-D sonography for diagnosis of disk dislocation of the temporomandibular joint compared with MRI. Ultrasound Med Biol 2006; 32: 633–9. doi: 10.1016/j.ultrasmedbio.2006.02.1401 [DOI] [PubMed] [Google Scholar]
- 20.Emshoff R, Brandlmaier I, Bodner G, Rudisch A. Condylar erosion and disc displacement: detection with high-resolution ultrasonography. J Oral Maxillofac Surg 2003; 61: 877–81. doi: 10.1016/S0278-2391(03)00247-7 [DOI] [PubMed] [Google Scholar]
- 21.Petscavage-Thomas JM, Walker EA. Unlocking the jaw: Advanced imaging of the temporomandibular joint. AJR Am J Roentgenol 2014; 203: 1047–58. doi: 10.2214/AJR.13.12177 [DOI] [PubMed] [Google Scholar]
- 22.Assaf AT, Kahl-Nieke B, Feddersen J, Habermann CR. Is high-resolution ultrasonography suitable for the detection of temporomandibular joint involvement in children with juvenile idiopathic arthritis? Dentomaxillofac Radiol 2013; 42: 20110379. doi: 10.1259/dmfr.20110379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Larheim TA, Westesson PL, Hicks DG, Eriksson L, Brown DA. Osteonecrosis of the temporomandibular joint: correlation of magnetic resonance imaging and histology. J Oral Maxillofac Surg 1999; 57: 888–98. doi: 10.1016/S0278-2391(99)90001-0 [DOI] [PubMed] [Google Scholar]
- 24.Emshoff R, Jank S, Bertram S, Rudisch A, Bodner G. Disk displacement of the temporomandibular joint: sonography versus MR imaging. AJR Am J Roentgenol 2002; 178: 1557–62. doi: 10.2214/ajr.178.6.1781557 [DOI] [PubMed] [Google Scholar]
- 25.Vilanova JC, Barceló J, Puig J, Remollo S, Nicolau C, Bru C. Diagnostic imaging: magnetic resonance imaging, computed tomography, and ultrasound. Seminars in Ultrasound, CT and MRI 2007; 28: 184–91. doi: 10.1053/j.sult.2007.02.003 [DOI] [PubMed] [Google Scholar]
- 26.Çakır-Özkan N, Sarıkaya B, Erkorkmaz U, Aktürk Y. Ultrasonographic evaluation of disc displacement of the temporomandibular joint compared with magnetic resonance imaging. J Oral Maxillofac Surg 2010; 68: 1075–80. doi: 10.1016/j.joms.2009.08.010 [DOI] [PubMed] [Google Scholar]
- 27.Bas B, Yılmaz N, Gökce E, Akan H. Ultrasound assessment of increased capsular width in temporomandibular joint internal derangements: relationship with joint pain and magnetic resonance grading of joint effusion. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology 2011; 112: 112–7. doi: 10.1016/j.tripleo.2011.02.020 [DOI] [PubMed] [Google Scholar]
- 28.Rao VM, Liem MD, Farole A, Razek AA. Elusive "stuck" disk in the temporomandibular joint: diagnosis with MR imaging. Radiology 1993; 189: 823–7. doi: 10.1148/radiology.189.3.8234710 [DOI] [PubMed] [Google Scholar]
- 29.Katzberg RW, Conway WF, Ackerman SJ, Gonzales TS, Kheyfits V, Cronan MS. Pilot study to show the feasibility of high-resolution sagittal ultrasound imaging of the temporomandibular joint. J Oral Maxillofac Surg 2017; 75: 1151–62. doi: 10.1016/j.joms.2016.12.007 [DOI] [PubMed] [Google Scholar]
- 30.Brandlmaier I, Rudisch A, Bodner G, Bertram S, Emshoff R. Temporomandibular joint internal derangement: detection with 12.5 MHz ultrasonography. J Oral Rehabil 2003; 30: 796–801. doi: 10.1046/j.1365-2842.2003.01063.x [DOI] [PubMed] [Google Scholar]
- 31.Emshoff R, Jank S, Rudisch A, Bodner G. Are high-resolution ultrasonographic signs of disc displacement valid? J Oral Maxillofac Surg 2002; 60: 623–8. doi: 10.1053/joms.2002.33105 [DOI] [PubMed] [Google Scholar]
- 32.Dupuy-Bonafé I, Picot M-C, Maldonado IL, Lachiche V, Granier I, Bonafé A. Internal derangement of the temporomandibular joint: is there still a place for ultrasound? Oral Surg Oral Med Oral Pathol Oral Radiol 2012; 113: 832–40. doi: 10.1016/j.oooo.2011.11.017 [DOI] [PubMed] [Google Scholar]
- 33.Razek AAKA, Al Mahdy Al Belasy F, Ahmed WMS, Haggag MA. Assessment of articular disc displacement of temporomandibular joint with ultrasound. J Ultrasound 2015; 18: 159–63. doi: 10.1007/s40477-014-0133-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Razek AAKA, Fouda NS, Elmetwaley N, Elbogdady E. Sonography of the knee joint. J Ultrasound 2009; 12: 53–60. doi: 10.1016/j.jus.2009.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Razek AAKA, El-Basyouni SR. Ultrasound of knee osteoarthritis: interobserver agreement and correlation with Western Ontario and McMaster universities osteoarthritis. Clin Rheumatol 2016; 35: 997–1001. doi: 10.1007/s10067-015-2990-2 [DOI] [PubMed] [Google Scholar]
- 36.Tognini F, Manfredini D, Melchiorre D, Bosco M. Comparison of ultrasonography and magnetic resonance imaging in the evaluation of temporomandibular joint disc displacement. J Oral Rehabil 2005; 32: 248–53. doi: 10.1111/j.1365-2842.2004.01410.x [DOI] [PubMed] [Google Scholar]
- 37.Landes CA, Goral WA, Sader R, Mack MG. Three-dimensional versus two-dimensional sonography of the temporomandibular joint in comparison to MRI. Eur J Radiol 2007; 61: 235–44. doi: 10.1016/j.ejrad.2006.09.015 [DOI] [PubMed] [Google Scholar]
- 38.McNeill C. Management of temporomandibular disorders: concepts and controversies. J Prosthet Dent 1997; 77: 510–22. doi: 10.1016/S0022-3913(97)70145-8 [DOI] [PubMed] [Google Scholar]
- 39.Lange U, Piegsa M, Teichmann J, Neeck G. Ultrasonography of the glenohumeral joints--a helpful instrument in differentiation in elderly onset rheumatoid arthritis and polymyalgia rheumatica. Rheumatol Int 2000; 19: 185–9. doi: 10.1007/s002960000051 [DOI] [PubMed] [Google Scholar]
- 40.Jacobson JA, sonography M. And MR imaging. A role for both imaging methods. Radiol Clin North Am 1999; 37: 713–35. [DOI] [PubMed] [Google Scholar]
- 41.Moss SG, Schweitzer ME, Jacobson JA, Brossmann J, Lombardi JV, Dellose SM, et al. Hip joint fluid: detection and distribution at MR imaging and US with cadaveric correlation. Radiology 1998; 208: 43–8. doi: 10.1148/radiology.208.1.9646791 [DOI] [PubMed] [Google Scholar]
- 42.Manfredini D, Tognini F, Melchiorre D, Zampa V, Bosco M. Ultrasound assessment of increased capsular width as a predictor of temporomandibular joint effusion. Dentomaxillofac Radiol 2003; 32: 359–64. doi: 10.1259/dmfr/25091144 [DOI] [PubMed] [Google Scholar]
- 43.Rasmussen OC.Clinical Temporomandibular arthropathy: Radiologic and therapeutic aspects with emphasis on diagnosis. Int J Oral Surg 1983; 12: 365–97. [DOI] [PubMed] [Google Scholar]
- 44.Su N, van Wijk AJ, Visscher CM, Lobbezoo F, van der Heijden GJMG. Diagnostic value of ultrasonography for the detection of disc displacements in the temporomandibular joint: a systematic review and meta-analysis. Clin Oral Investig 2018; 22: 2599–614. doi: 10.1007/s00784-018-2359-4 [DOI] [PMC free article] [PubMed] [Google Scholar]