Abstract
ROS1 inhibition provides impressive survival benefits in ROS1-rearranged non-small cell lung cancer (NSCLC) patients. Crizotinib is the only tyrosine kinase inhibitor (TKI) approved by both FDA and EMA for the treatment of ROS1-positive lung cancer. In addition, several TKI have been tested with preliminary proofs of success in this oncogene-driven disease, either in the post-crizotinib setting or as first-line targeted agents. Here we present the evidence concerning entrectinib, an ALK/ROS1/NTRK inhibitor developed across different tumor types harboring rearrangements in these genes, in the context of ROS1-driven NSCLC. Of interest, in August 2019 entrectinib was granted by FDA accelerated approval for the treatment of ROS1-rearranged NSCLC, as well as of NTRK-driven solid tumors.
Keywords: lung cancer, ROS1, tyrosine kinase inhibitors, entrectinib
Introduction
Molecular anticancer agents are determinant in providing survival benefits in patients affected by oncogene-driven malignant diseases. Non-small cell lung cancer (NSCLC) represents the most relevant example in precision cancer medicine, accounting to the multitude of molecular targets, responsible for tumor initiation and growth, suitable of direct inhibition with kinase inhibitors. Of note, the spectrum of both targets (eg EGFR/BRAF/MET/HER2 mutations, ALK/ROS1/RET/NTRK rearrangements, HER2/MET amplifications) and corresponding kinase inhibitors is in constant expansion. Even if the proportion of patients harboring each specific molecular alteration appears limited among the total NSCLC cases, the global epidemiology of this tumor type, regarding both incidence and mortality worldwide,1 makes their absolute number of definite relevancy.
ROS1 rearrangements are present in 1–2% of NSCLC.2 Currently, ROS1 molecular diagnosis relies on tumor analysis.3 Nevertheless, even though the detection of gene fusions in liquid biopsies is still challenging,4 next generation sequencing (NGS) of plasmatic circulating tumor DNA (ctDNA) has been recently proven a valid option to detect molecular alterations suitable of targeted treatments in NSCLC, including ROS1 rearrangements.5 The positive predictive value of ctDNA, its concordance with tumor biopsy analyses, as well as the favorable turnaround time and the achievement of a complete genotyping sustain the clinical implementation of this valuable tool, thus fostering ROS1 positivity recognition.
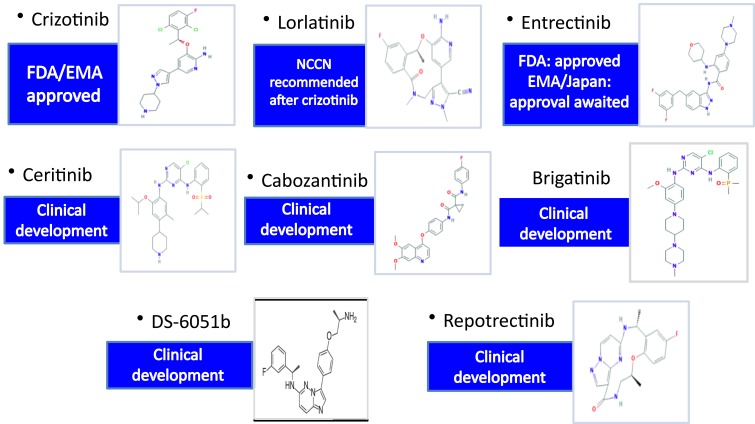
The favorable outcomes of ROS1-positive NSCLC patients receiving specific tyrosine kinase inhibitors (TKI) may be inferred by the recent update of the dedicated expansion cohort within PROFILE 1001 phase I trial of crizotinib in advanced malignancies.6,7 After a median follow-up (mFU) of more than five years, among the 53 ROS1-positive NSCLC patients median progression-free survival (mPFS) of 19.3 months [95% confidence interval (CI) 15.2–39.1] and median overall survival (mOS) of 51.4 months [95% CI, 29.3–not reached (NR)] were observed.7 Still taking into account the peculiar sensitivity of ROS1-driven diseases to pemetrexed-based chemotherapy,8,9 the subsequent availability of additional ROS1-TKI is supposed to contribute to the impressive OS results, although the treatments received after crizotinib failure were not explicited.7 Dealing with advanced tumors, disease progression as a consequence of resistance to targeted agents eventually occurs in virtually every treated patient and further treatment options are needed. Besides crizotinib (the only drug approved by both FDA and EMA for ROS1-driven NSCLC), additional TKI have shown activity and efficacy in ROS1-rearranged lung cancer: ceritinib, cabozantinib, entrectinib, lorlatinib, brigatinib, DS-6051b and repotrectinib (Figure 1).10–19 According to NCCN guidelines, lorlatinib is the only ROS1-TKI approved after crizotinib failure,20 based on available clinical trial data.14,15
Figure 1.
ROS1 inhibitors approved and in clinical development. Chemical structures are depicted.
Similarly to what observed in EGFR- and ALK-positive diseases, the novel TKI can contribute to the prolongation of disease control (turning out to be a surrogate of OS) in two alternative ways. First, their administration is active (ie, overcomes resistance) after the first-generation TKI (crizotinib in the case of ROS1-positve NSCLC) and generates improvements in efficacy outcomes (PFS, OS). Otherwise, new TKI may be administered upfront (ie, substituting crizotinib) if they are deemed to guarantee a more prolonged control of the disease compared to a sequential strategy.21 In addition to activity and efficacy estimations of each TKI in the two depicted scenarios, toxicity spectra of TKI should be taken into account, as dealing with chronic treatments.
In this context, the present review aims to recapitulate all the available evidence concerning entrectinib for the treatment of ROS1-positive NSCLC. Of note, FDA has recently granted entrectinib (600 mg daily, oral intake) an accelerated approval in this precise setting, as well as for the treatment of NTRK fusion–positive solid tumors.22 In addition, entrectinib has received the Priority Medicines (PRIME) designation by EMA, whereas in Japan it is approved for NTRK-rearranged solid tumors and under regulatory review for the treatment of ROS1-positive NSCLC.23
Preclinical proofs of entrectinib activity in ROS1-positive NSCLC models
Entrectinib (ROZLYTREK, RDX-101. Genentech Inc.) has been developed through the chemical optimization of an ALK-TKI utilized as a tool compound for preclinical studies.24 Sharing similarities in their tyrosine kinase domain amino-acidic sequences, ALK, ROS1 and TRKA/B/C emerged as suitable entrectinib targets.25 Indeed, the half maximal inhibitory concentration (IC50) against purified ALK, ROS1 and TRKs enzymes were 12, 7 and 1–5 nM, respectively.24 Albeit experiments on human-derived tumor cells were performed in ALK- and TRK-driven models only, the activity of entrectinib was tested on engineered ROS1-dependent Ba/F3 cells models, in which the drug confirmed an IC50 of 5 nM.24,26 Overlapping results were observed in ALK- and TRK-positive models, whereas ABL- and RET-dependent cells were characterized by IC50 in the μM range, thus considered resistant and testifying entrectinib selectivity.24,26 The compound showed highest potency in ROS1 inhibition compared to crizotinib (IC50 180 nM) even in short-term immunoblot analyses, still in the lack of an extensive study on the intracellular signaling (ie, MEK/ERK, PI3K/mTOR, JAK/STAT pathways), yet performed with success in ALK- and TRK-positive models.26
In in vitro and in vivo models, entrectinib showed also favorable pharmacokinetic profiles, in terms of absorption, distribution, metabolism, and excretion (ADME) properties, translating into high oral bioavailability, low clearance, satisfactory volume of distribution and half-life estimations.24 In this sense, complete regression of mice tumors derived by subcutaneous injection of ROS1-dependent Ba/F3 was obtained with entrectinib administration (60 mg/kg orally twice daily for 10 consecutive days), similarly to what observed in ALK- and TRK-positive animals.26
In these first entrectinib studies, researchers addressed two of the main questions regarding overcoming resistance to crizotinib in ALK- and ROS1-rearranged NSCLC.
First, ALK mutations in the kinase domain, known to confer crizotinib resistance, were expressed in Ba/F3 models for dose-response assays. If entrectinib retained activity against ALKC1156Y and ALKL1196M mutants (IC50 of 29 and 67 nM, respectively), inhibition of cellular growth in ALKG1202R and ALKG1269A was obtained at concentrations compatible with drug resistance (897 and 390 nM, respectively).26 No specific evidence of entrectinib activity against ROS1 mutants had been provided in this study. Nevertheless, the similarity in the spectrum of resistance mutations between ALK and ROS1 suggested that the compound may not inhibit ROS1G2032R (the most commonly emerging at progression on crizotinib and the less prone to be reverted towards sensitivity by next-generation drugs).27 Indeed, Katayama and colleagues have recently provided an extensive study on the differential activity of ROS1 inhibitors against specific ROS1 mutants.28 In particular, while retaining activity at nanomolar concentrations in ROS1L1951R, ROS1L2026M (corresponding to ALKL1196M) and ROS1D2033N (corresponding to ALKD1203N) models, entrectinib was not able to inhibit cell growth and signaling in cells harboring ROS1G2032R (corresponding to ALKG1202R). In this study, activity against ROS1G2032R was maintained only by DS-6051b.
Second, brain disease dissemination is extremely frequent in ALK- and ROS1-positive NSCLC at diagnosis and during the disease course, owing both to the peculiar cellular tropism and to the limited crizotinib activity in central nervous system (CNS) localizations.29–31 The intracranial injection of an ALK-rearranged cell line (NCI-H2228) in mice led to the development of macroscopic CNS lesions and entrectinib was therefore administered at the dose previously used against subcutaneous tumors and at its double, given an estimated cerebrospinal fluid (CSF)/plasma concentration ratio of 50%.26 Albeit the “standard” dose already performed better that crizotinib, the most significant results in terms of disease control and OS were observed at the dose of 120 mg/kg twice daily. As the suboptimal intracranial activity of crizotinib is ascribed to pharmacokinetics issues (low CSF concentration), these results provided the first evidence for entrectinib brain penetration ability. Of note, no relevant toxicity in animals treated with different entrectinib doses for a period of 14 days had been observed up to the dose of 240 mg/kg daily.
If no report of the molecular mechanism underpinning entrectinib resistance in ROS1-positive NSCLC patients exists, recent evidence has been provided using preclinical models. Exposing HCC78 cell line (harboring SLC34A2-ROS1 fusion) to increasing doses of entrectinib, resistant clones were obtained with a KRAS mutation G12C detected by next-generation sequencing.32 KRAS mutation was accompanied by KRAS and FGF3 amplification and overexpression in two different resistant clones. Of note, these cells were cross-resistant to other ROS1 inhibitors such as crizotinib, ceritinib and lorlatinib, whereas the combination of entrectinib with the MEK inhibitor selumetinib revealed synergistic effect against resistant clones.32
Clinical evidence of entrectinib activity and efficacy in ROS1-rearranged NSCLC patients
The clinical development of entrectinib focused on specific oncogene targets since its early phases. ALKA-327-001 (EudraCT 2012-000148-88, phase I), STARTRK-1 (NCT02097810, phase I), STARTRK-2 (NCT02568267, basket phase II) enrolled exclusively patients suffering from advanced tumors harboring ALK, ROS1 or NTRK1/2/3 rearrangements. The recommended phase II dose of 600 mg daily emerged from dose-escalation cohorts.13
With specific regards to entrectinib profile in the setting of ROS1-postive NSCLC, interesting insights may be driven mainly from the manuscript by Drilon and collaborators, focusing on the two phase I studies,13 and from the recent presentation by Barlesi and colleagues at the 2019 ELCC (European Lung Cancer Congress), that gather data from the three mentioned trials.33 In addition, further preliminary results were presented at 2017 and 2018 World Conference on Lung Cancer (WCLC)34,35 and may have been incorporated in the more recent report by Barlesi and coauthors, including a longer follow-up. Up to this latter update, 53 ROS1-positive NSCLC patients received entrectinib as the upfront TKI (efficacy population), the majority having received no (n=17, 32%) or one (n=23, 43%) previous lines of systemic treatment, with a minimum follow-up of 12 months. Objective response rate (ORR) and duration of response (DoR) were the two primary endpoints. According to a blinded independent central review, ORR was observed in 41 cases (77.4%, 95% CI 63.8–87.7), whereas mPFS and mDoR were respectively estimated, after a mFU of 15.5 month (12 months minimum), at 19 (95% CI 12.2–36.6) and 24.6 months (95% CI 11.4–34.8). mOS, even in its lower 95% CI bound, was not estimable (NE), with only nine events (17%).33
Of note, a relevant number of patients (n=23, 43%) presented CNS involvement before treatment initiation. In this population, whereas activity measures were overlapping to the global one (ORR 74%, 95% CI 51.6–89.8), mPFS (13.6 months, 95% CI 4.5–NE) and mDoR (12.6 months, 95% CI 6.5–NE) were reduced. These data, together with intacranial RR of 55% (11 out of 20 evaluable patients), mPFS of 7.7 months (3.81–9.3) mDoR of 12.9 months (5.6–NE), vouch for entrectinib activity and efficacy against CNS lesions.33 Nevertheless, the inferior survival outcomes observed in patients with prior CNS involvement suggest that brain disease progression is likely frequent. The lack of information regarding the type of brain imaging screening and timeline of follow-up (putting as a remarkable reference ALEX trial comparing alectinib versus crizotinib in first-line ALK-positive NSCLC),36 the incidence of brain progression in patients without baseline CNS metastases and the limited patient number preclude a complete evaluation of entrectinib CNS potency.
Of note, the total number of ROS1-positive patients who received at least one dose of entrectinib and were included in the safety analysis (see next section) accounted to 134. Albeit similar proportions of previously untreated/pretreated patients were included in efficacy and safety populations, it cannot be retraced how many patients had previously received crizotinib or another ROS1 inhibitor. The only information on TKI-pretreated patients derives from the previous publication by Drilon and colleagues.13 None out of the six patients who had previously received crizotinib experienced disease response. No specific resistance mechanisms responsible for crizotinib resistance (ie, ROS1 acquired mutations), as well as CNS disease status, were reported for this small population apparently refractory to crizotinib. This observation makes compelling to envisage the potential utility of entrectinib after crizotinib specifically in the presence of CNS progression or acquired secondary ROS1 mutations. Entrectinib has been showed by in vitro studies to retain activity against some ROS1 mutants, but it is ineffective on ROS1G2032R,28 the most relevant in the clinical setting of post-crizotinib resistance (see Section 2).31
Entrectinib toxicity spectrum
Since its early development, entrectinib appeared a manageable drug.13 The good safety profile was confirmed with a longer follow-up and a wider population. If considering all the patients regardless of tumor type and molecular alteration who received at least one entrectinib dose (n=355), gathering ALKA-327-001, STARTRK-1, STARTRK-2 and the phase I/Ib STARTRK-NG trials, grade 1/2, 3 and 4 adverse events (AEs) occurred in 61%, 28% and 3% of the cases, respectively.33 No grade 5 AEs were reported, while dose reductions and treatment discontinuation were respectively required in 27% and 4% of the patients. Similar proportions were registered in the ROS1-positive NSCLC safety population (n=134). Considering toxicities observed at least in 10% of the patients, 42% reported dysgeusia, whereas fatigue, weight increase, diarrhea, constipation and dizziness occurred in proportions between 20% and 30%. Of note, almost all the reported AEs were of grade 1/2. Three and 10 patients experienced grade ≥3 diarrhea and weight increase, respectively, whereas other severe toxicities occurred sporadically.33
Entrectinib in the context of ROS1 inhibition in NSCLC
ROS1 targeting in NSCLC has significantly progressed in the last few years and crizotinib has to be considered as the reference treatment, harboring the widest body of supporting evidence and representing the only ROS1 inhibitor approved by both FDA and EMA thus far. Despite its significant results about activity and efficacy, resistance to crizotinib occurs virtually in every patient and novel treatment strategies are needed. With regard to non-targeted agents, pemetrexed-based chemotherapy still carries a meaningful role in ROS1-positive NSCLC patients.8,9 Concerning immunotherapy contribution, the limited number of reported cases exposed to PD-1/PD-L1 inhibitors precludes definitive conclusions. Nevertheless, responsiveness of ROS1-dependent diseases to these agents seems to recapitulate the scarce cases observed in EGFR- and ALK-driven NSCLC.37 Further evidence is needed to establish a potential role of anti-angiogenic treatment in synergizing with chemo-immunotherapy, as seen for EGFR-mutated lung cancers.38
Similarly to what observed in the other oncogene-addicted references, the development of additional specific inhibitors, in the present case beyond crizotinib, is crucial. By date, six drugs have shown anti-ROS1 clinical activity: ceritinib, cabozantinib, entrectinib, lorlatinib, brigatinib, DS-6051b and repotrectinib (Figure 1). According to NCCN guidelines, lorlatinib is the only ROS1 inhibitor recommended in the post-crizotinib setting thus far.20 In order to be more proficient than crizotinib, these inhibitors should be more potent against the target and its mutants emerging as resistance mechanisms, retain a good brain activity accounting to crizotinib suboptimal one and the frequent CNS involvement of ROS1-positive disease.30,31 In addition, dealing with chronic treatments, drug specificity is required to avoid off-target activity engendering toxicities. These novel inhibitors may provide survival effects beyond crizotinib in two major scenarios: performing better than the reference treatment if given upfront, or being active and efficient once tumors escape on crizotinib. If ever both strategies were successful, a debate on which should be adopted will be of interest in the setting of ROS1-positive NSCLC, flanking EGFR- and ALK-driven diseases one.21
Given the relative rarity of ROS1-rearranged NSCLC, that can be defined as a rare molecular subclass of a common tumor, is it difficult to envisage head-to-head comparisons between different ROS1 inhibitors, as seen for EGFR- and ALK-positive lung tumors. Albeit always challenging and risky due to methodological issues, indirect comparisons between different trials and experiences may serve as a surrogate to define the potential role of each drug.
As approached in Section 3, the data regarding entrectinib administration in the post-crizotinib setting are extremely scarce (only six patients reported) and not encouraging, as no response was observed. Of note, similar results were obtained in ceritinib phase II trial, as the two patients enrolled after crizotinib resistance experienced further progression on ceritinib.10 In addition, Sun and colleagues reported four cases out of four in which primary ceritinib resistance after crizotinib progression was managed by cabozantinib administration.12 Responses to cabozantinib, lorlatinib, DS-6051b and repotrectinib were indeed observed, with a special mention to the last drug, retaining significant activity against brain disease and, even more remarkably, against the recalcitrant ROS1G2032R mutation.11,12,14,15,17,19 The evidence concerning the activity of each mentioned ROS1-TKI against specific ROS1 mutants will be likely extended, given the current documentation of resistance mutations from ctDNA in ROS1-positive NSCLC patients,39,40 similar to EGFR-mutated and ALK-rearranged ones.41,42 The large-scale availability of such analyses, bypassing the practical issues of tumor biopsies, would allow the systemic capture of resistance mechanisms to ROS1 inhibitors and pave the way for the following correlations with drug activity.
In the upfront setting, evidence thus far available regarding activity and efficacy of the different inhibitors are resumed in Table 1. Whereas OS data are still immature to drive any conclusion, it seems that entrectinib performs quite similarly to other anti-ROS1 agents. Still with regard to patients who had not received crizotinib before, the signals of drug activity and efficacy in the case of CNS metastases at baseline are gathered in Table 2. Of note, the specific intracranial activity and efficacy have been reported for entrectinib only (see Section 3).33 Indirect comparisons may be indeed performed only with regard to “global” ORR and PFS in patients with CNS disease at baseline; whereas activities seem overlapping between the inhibitors, PFS appears slightly longer with entrectinib compared to crizotinib (mPFS 13.6 versus 10.2 months, respectively).
Table 1.
Activity and efficacy of ROS1 inhibitors in ROS1-TKI naïve NSCLC patients in clinical trials
| Inhibitor reference | Patients n | mFU months (95% CI) |
ORR (95% CI) |
mPFS months (95% CI) | mDoR months (95% CI) | mOS months (95% CI) |
|---|---|---|---|---|---|---|
| Crizotinib Shaw Ann Oncol 20197 |
53 | 62.6 | 72% (58–83) | 19.3 (15.2–39.1) | 24.7 (15.2–45.3) | 51.4 (29.3–NR) |
| Crizotinib Wu J Clin Oncol 201843 |
127 | 21.4 (20.1–23.0) | 71.7% (63.0–79.3) | 15.9 (12.9–24.0) | 19.7 (14.1– NR) | 32.5 (32.5– NR) |
| Crizotinib Michels J Thorac Oncol 201944 |
34 | 20.6 | 70% (51–85) | 20.0 (10.1–NR) | 19.0 (9.1–NR) | NR (17.1– NR) |
| Crizotinib Landi Clin Cancer Res 201945 |
26 | 21 (19.0–24.5) | 65% (44–82) | 22.8 (15.2‒30.3) | 21.4 (12.7–30.1) | NR |
| Ceritinib Lim J Clin Oncol 201710 |
30 | 14.0 (IQR 9.0–19.0) | 67% (48–81) | 19.3 (1–37) | 21 (17–25) | 24 (5–43)* |
| Lorlatinib Ou WCLC 201815 |
13 | 19.5 (16.6–24.8) | 61.5% (31.6–86.1) | 21.0 (4.2–26.7) | 19.6 (4.0–25.3) | NA |
| Entrectinib Barlesi ELCC 201933 |
53 | 15.5 | 77.4% (63.8–87.7) | 19 (12.2–36.6) | 24.6 (11.4–34.8) | NE (NE–NE) |
| Repotrectinib Cho ASCO 201919 |
11 | 16.4 | 82% (48–98) | NA | NR (5.6–17.7+) | NA |
Note: *Considering the entire population (n=32, including two patients previously treated with crizotinib).
Abbreviations: n, Number; mFU, Median follow-up; 95% CI, 95% confidence interval; ORR, Objective response rate; mPFS, Median progression-free survival; mDoR, Median duration of response; mOS, median overall survival; NR, not reached; NA, Not available; NE, Not estimable.
Table 2.
Activity and efficacy of ROS1 inhibitors in ROS1-TKI naïve NSCLC patients with brain metastases
| Inhibitor reference | Patients n |
mFU months (95% CI) | ORR (95% CI) |
mPFS months (95% CI) |
mDoR months (95% CI) |
mOS months (95% CI) |
|---|---|---|---|---|---|---|
| Crizotinib Wu J Clin Oncol 201831 |
23 | 21.4 (20.1–23.0) | 73.9% (51.6–89.8) | 10.2 (5.6–13.1) | NA | NA |
| Michels J Thorac Oncol 201944 |
6 | 20.6 | 66.7 (22.3–95.7) | 9.4 (1.7–NR) | NA | NR (1.7–NR) |
| Crizotinib Landi Clin Cancer Res 201945 |
6 | 21 (19.0–24.5) | 33.3% | NA | NA | NA |
| Ceritinib Lim J Clin Oncol 201710 |
8* | 14.0 (IQR 9.0–19.0) | 25% (7–59) | NA | NA | NA |
| Lorlatinib Ou WCLC 201815 |
6 | NA | 66.7% (22.3–95.7) | NA | NA | NA |
| Entrectinib Barlesi ELCC 201933 |
23 | 15.5 | 77.4% (63.8–87.7) | 13.6 (4.5–NE) | 12.6 (6.5–NE) | NE (NE-NE) |
| Repotrectinib Cho ASCO 201919 |
3 | 16.4 | 100% (29–100) | NA | NA | NA |
Note: *Considering the entire population (n=32, including two patients previously treated with crizotinib).
Abbreviations: n, Number; mFU, Median follow-up; 95% CI, 95% confidence interval; ORR, Objective response rate; mPFS, Median progression-free survival; mDoR, Median duration of response; mOS, median overall survival; NA, Not available; NE, Not estimable.
In summary, ROS1 inhibition represents a current crowded space in development in NSCLC. Besides crizotinib, approved by both FDA and EMA, and entrectinib, having recently been granted accelerated approval by FDA, several promising drugs are showing activity and efficacy. Focusing on entrectinib, no signs of activity in the post-crizotinib setting have been reported (still in a very limited number of patients). With regard to the population that have not previously received any TKI, the long-term survivor outcomes observed with crizotinib require other trials to be reported with longer follow-up. Nevertheless, for entrectinib and for other additional TKI with anti-ROS1 activity, the prolonged benefit observed with crizotinib in ROS1-positive NSCLC appears hard to beat.
Disclosure
The authors of this work report they have no conflicts of interest to disclose.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi: 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Bergethon K, Shaw AT, Ou S-HI, et al. ROS1 rearrangements define a unique molecular class of lung cancers. J Clin Oncol. 2012;30(8):863–870. doi: 10.1200/JCO.2011.35.6345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rossi G, Jocollé G, Conti A, et al. Detection of ROS1 rearrangement in non-small cell lung cancer: current and future perspectives. Lung Cancer (Auckl). 2017;8:45–55. doi: 10.2147/LCTT.S120172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Supplee JG, Milan MSD, Lim LP, et al. Sensitivity of next-generation sequencing assays detecting oncogenic fusions in plasma cell-free DNA. Lung Cancer. 2019;134:96–99. doi: 10.1016/j.lungcan.2019.06.004 [DOI] [PubMed] [Google Scholar]
- 5.Leighl NB, Page RD, Raymond VM, et al. Clinical utility of comprehensive cell-free DNA analysis to identify genomic biomarkers in patients with newly diagnosed metastatic non–small cell lung cancer. Clin Cancer Res. 2019;25(15):4691–4700. doi: 10.1158/1078-0432.CCR-19-0624 [DOI] [PubMed] [Google Scholar]
- 6.Shaw AT, Ou S-HI, Bang Y-J, et al. Crizotinib in ROS1-rearranged non-small-cell lung cancer. N Engl J Med. 2014;371(21):1963–1971. doi: 10.1056/NEJMoa1406766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaw AT, Riely GJ, Bang Y-J, et al. Crizotinib in ROS1-rearranged advanced non-small-cell lung cancer (NSCLC): updated results, including overall survival, from PROFILE 1001. Ann Oncol. 2019. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liang Y, Wakelee HA, Neal JW. Relationship of driver oncogenes to long-term pemetrexed response in non-small-cell lung cancer. Clin Lung Cancer. 2015;16(5):366–373. doi: 10.1016/j.cllc.2014.12.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen YF, Hsieh MS, Wu SG, et al. Efficacy of pemetrexed-based chemotherapy in patients with ROS1 fusion-positive lung adenocarcinoma compared with in patients harboring other driver mutations in East Asian populations. J Thorac Oncol. 2016;11(7):1140–1152. doi: 10.1016/j.jtho.2016.03.022 [DOI] [PubMed] [Google Scholar]
- 10.Lim SM, Kim HR, Lee JS, et al. Open-label, multicenter, phase II study of ceritinib in patients with non-small-cell lung cancer harboring ROS1 rearrangement. J Clin Oncol. 2017;35(23):2613–2618. doi: 10.1200/JCO.2016.71.3701 [DOI] [PubMed] [Google Scholar]
- 11.Drilon A, Somwar R, Wagner JP, et al. A novel crizotinib-resistant solvent-front mutation responsive to cabozantinib therapy in a patient with ROS1-rearranged lung cancer. Clin Cancer Res. 2015;22(10):2351–2358. doi: 10.1158/1078-0432.CCR-15-2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sun TY, Niu X, Chakraborty A, et al. Lengthy progression-free survival and intracranial activity of cabozantinib in patients with crizotinib and ceritinib-resistant ROS1-positive non–small cell lung cancer. J Thorac Oncol. 2019;14(2):e21–e24. doi: 10.1016/j.jtho.2018.08.2030 [DOI] [PubMed] [Google Scholar]
- 13.Drilon A, Siena S, Ou SHI, et al. Safety and antitumor activity of the multitargeted pan-TRK, ROS1, and ALK inhibitor entrectinib: combined results from two phase I trials (ALKA-372-001 and STARTRK-1). Cancer Discov. 2017;7(4):400–409. doi: 10.1158/2159-8290.CD-16-1237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shaw AT, Felip E, Bauer TM, et al. Lorlatinib in non-small-cell lung cancer with ALK or ROS1 rearrangement: an international, multicentre, open-label, single-arm first-in-man phase 1 trial. Lancet Oncol. 2017;18(12):1590–1599. doi: 10.1016/S1470-2045(17)30072-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ou S, Shaw A, Riely G, et al. OA02.03 Clinical Activity of lorlatinib in patients with ROS1+ advanced non-small cell lung cancer: phase 2 study cohort EXP-6. J Thorac Oncol. 2018;13(suppl_10):S322–S323. doi: 10.1016/j.jtho.2018.08.241 [DOI] [Google Scholar]
- 16.Hegde A, Hong DS, Behrang A, et al. Activity of brigatinib in crizotinib and ceritinib-resistant ROS1-rearranged non–small-cell lung cancer. JCO Precis Oncol. 2019;3:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fujiwara Y, Takeda M, Yamamoto N, et al. Safety and pharmacokinetics of DS-6051b in Japanese patients with non-small cell lung cancer harboring ROS1 fusions: a phase I study. Oncotarget. 2018;9(34):23729–23737. doi: 10.18632/oncotarget.25263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drilon A, Ou S-HI, Cho BC, et al. Repotrectinib (TPX-0005) is a next generation ROS1/TRK/ALK inhibitor that potently inhibits ROS1/TRK/ALK solvent front mutations. Cancer Discov. 2018;8(10):1227–1236. doi: 10.1158/2159-8290.CD-18-0484 [DOI] [PubMed] [Google Scholar]
- 19.Cho BC, Drilon A, Doebele R, et al. Safety and preliminary clinical activity of repotrectinib in patients with advanced ROS1 fusion-positive non-small cell lung cancer (TRIDENT-1 study). J Clin Oncol. 2019;37(15_suppl):9011. [Google Scholar]
- 20.National Comprehensive Cancer Network. NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Non-Small Cell Lung Cancer (version 2.2019). Available from: https://www.nccn.org/professionals/physician_gls/recently_updated.aspx. Accessed September 3, 2019. [Google Scholar]
- 21.Recondo G, Facchinetti F, Olaussen KA, Besse B, Friboulet L. Making the first move in EGFR-driven or ALK-driven NSCLC: first-generation or next-generation TKI? Nat Rev Clin Oncol. 2018;15(11):694–708. doi: 10.1038/s41571-018-0081-4 [DOI] [PubMed] [Google Scholar]
- 22.FDA. FDA approves entrectinib for NTRK solid tumors and ROS-1 NSCLC Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-entrectinib-ntrk-solid-tumors-and-ros-1-nsclc. Accessed August 28, 2019
- 23.ESMO. Japan Becomes the First Country to Approve Entrectinib Available from: https://www.esmo.org/Oncology-News/Japan-Becomes-the-First-Country-to-Approve-Entrectinib. Accessed August 28, 2019.
- 24.Menichincheri M, Ardini E, Magnaghi P, et al. Discovery of entrectinib: a new 3-aminoindazole as a potent anaplastic lymphoma kinase (ALK), c-ros oncogene 1 kinase (ROS1), and pan-tropomyosin receptor kinases (pan-TRKs) inhibitor. J Med Chem. 2016;59(7):3392–3408. doi: 10.1021/acs.jmedchem.6b00064 [DOI] [PubMed] [Google Scholar]
- 25.Awad MM, Katayama R, McTigue M, et al. Acquired resistance to crizotinib from a mutation in CD74-ROS1. N Engl J Med. 2013;368(25):2395–2401. doi: 10.1056/NEJMoa1215530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ardini E, Menichincheri M, Banfi P, et al. Entrectinib, a pan-TRK, ROS1, and ALK inhibitor with activity in multiple molecularly defined cancer indications. Mol Cancer Ther. 2016;15(4):628–639. doi: 10.1158/1535-7163.MCT-15-0758 [DOI] [PubMed] [Google Scholar]
- 27.Facchinetti F, Loriot Y, Kuo MS, et al. Crizotinib-resistant ROS1 mutations reveal a predictive kinase inhibitor sensitivity model for ROS1- and ALK-rearranged lung cancers. Clin Cancer Res. 2016;22(24):5983–5991. doi: 10.1158/1078-0432.CCR-16-0917 [DOI] [PubMed] [Google Scholar]
- 28.Katayama R, Gong B, Togashi N, et al. The new-generation selective ROS1/NTRK inhibitor DS-6051b overcomes crizotinib resistant ROS1- G2032R mutation in preclinical models. Nat Commun. 2019;10(1):3604. doi: 10.1038/s41467-019-11496-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Peters S, Camidge DR, Shaw AT, et al. Alectinib versus crizotinib in untreated ALK-positive non–small-cell lung cancer. N Engl J Med. 2017;377(9):829–838. doi: 10.1056/NEJMoa1704795 [DOI] [PubMed] [Google Scholar]
- 30.Patil T, Smith DE, Bunn PA, et al. The incidence of brain metastases in stage IV ROS1-rearranged non–small cell lung cancer and rate of central nervous system progression on crizotinib. J Thorac Oncol. 2018;13(11):1717–1726. doi: 10.1016/j.jtho.2018.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gainor JF, Tseng D, Yoda S, et al. Patterns of metastatic spread and mechanisms of resistance to crizotinib in ROS1-positive non–small-cell lung cancer. JCO Precis Oncol. 2017;1:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ku BM, Bae YH, Lee KY, et al. Entrectinib resistance mechanisms in ROS1-rearranged non-small cell lung cancer. Invest New Drugs. 2019. Epub ahead of print. doi: 10.1007/s10637-019-00795-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barlesi F, Drilon A, De Braud F, et al. Entrectinib in locally advanced or metastatic ROS1 fusion-positive non-small cell lung cancer (NSCLC): integrated analysis of ALKA-372-001, STARTRK-1 and STARTRK-2. Ann Oncol. 2019;30(suppl_2):109O. doi: 10.1093/annonc/mdz063.00730357310 [DOI] [Google Scholar]
- 34.Ahn M, Cho BC, Siena S, et al. OA 14.06 Entrectinib in patients with locally advanced or metastatic ROS1 fusion-positive non-small cell lung cancer (NSCLC). J Thorac Oncol. 2017;12(11_suppl):S1783. doi: 10.1016/j.jtho.2017.09.411 [DOI] [Google Scholar]
- 35.Doebele R, Ahn M, Siena S, et al. OA02.01 Efficacy and safety of entrectinib in locally advanced or metastatic ROS1 fusion-positive non-small cell lung cancer (NSCLC). J Thorac Oncol. 2018;13(suppl_10):S321–S322. doi: 10.1016/j.jtho.2018.08.239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gadgeel S, Peters S, Mok T, et al. Alectinib versus crizotinib in treatment-naive anaplastic lymphoma kinase-positive (ALK+) non-small-cell lung cancer: CNS efficacy results from the ALEX study. Ann Oncol. 2018;29(11):2214–2222. doi: 10.1093/annonc/mdx807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mazières J, Drilon A, Lusque A, et al. Immune checkpoint inhibitors for patients with advanced lung cancer and oncogenic driver alterations: results from the IMMUNOTARGET registry. Ann Oncol. 2019. Epub ahead of print. doi: 10.1093/annonc/mdz167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Reck M, Mok TSK, Nishio M, et al. Atezolizumab plus bevacizumab and chemotherapy in non-small-cell lung cancer (IMpower150): key subgroup analyses of patients with EGFR mutations or baseline liver metastases in a randomised, open-label phase 3 trial. Lancet Respir Med. 2019;7(5):387–401. doi: 10.1016/S2213-2600(19)30084-0 [DOI] [PubMed] [Google Scholar]
- 39.Dagogo-Jack I, Rooney M, Nagy RJ, et al. Molecular analysis of plasma from patients with ROS1-positive NSCLC. J Thorac Oncol. 2019;14(15):816–824. doi: 10.1016/j.jtho.2019.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zugazagoitia J, Gómez-Rueda A, Jantus-Lewintre E, et al. Clinical utility of plasma-based digital next-generation sequencing in oncogene-driven non-small-cell lung cancer patients with tyrosine kinase inhibitor resistance. Lung Cancer. 2019;134:72–78. doi: 10.1016/j.lungcan.2019.05.032 [DOI] [PubMed] [Google Scholar]
- 41.Oxnard GR, Thress KS, Alden RS, et al. Association between plasma genotyping and outcomes of treatment with osimertinib (AZD9291) in advanced non-small-cell lung cancer. J Clin Oncol. 2016;34(28):3375–3382. doi: 10.1200/JCO.2016.66.7162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Dagogo-Jack I, Brannon AR, Ferris LA, et al. Tracking the evolution of resistance to ALK tyrosine kinase inhibitors through longitudinal analysis of circulating tumor DNA. JCO Precis Oncol. 2018;2:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wu YL, Yang JC, Kim DW, et al. Phase II study of crizotinib in East Asian patients with ROS1-positive advanced non-small-cell lung cancer. J Clin Oncol. 2018;36(14):1405–1411. doi: 10.1200/JCO.2017.75.5587 [DOI] [PubMed] [Google Scholar]
- 44.Michels S, Massutí B, Schildhaus HU, et al. Safety and efficacy of crizotinib in patients with advanced or metastatic ROS1-rearranged lung cancer (EUCROSS): a European phase II clinical trial. J Thorac Oncol. 2019;14(7):1266–1276. doi: 10.1016/j.jtho.2019.03.020 [DOI] [PubMed] [Google Scholar]
- 45.Landi L, Chiari R, Tiseo M, et al. Crizotinib in MET deregulated or ROS1 rearranged pretreated non-small-cell lung cancer (METROS): a phase II, prospective, multicentre, two-arms trial. Clin Cancer Res. 2019. Epub ahead of print. doi: 10.1158/1078-0432.CCR-19-0994 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- FDA. FDA approves entrectinib for NTRK solid tumors and ROS-1 NSCLC Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-entrectinib-ntrk-solid-tumors-and-ros-1-nsclc. Accessed August 28, 2019