Abstract
Objectives:
This study aimed to assess urban adolescents’ knowledge of and attitudes about emergency contraception (EC) and to assess the intention to use EC in particular hypothetical situations. We hypothesized that knowledge about EC would be limited, but that adolescents would support using EC in certain situations.
Methods:
A cross-sectional survey of English-speaking, 14- to 19-year-old adolescent girls presenting for care at 2 urban pediatric emergency departments. The survey was based on previous research with this target population and the constructs of the theory of planned behavior.
Results:
We enrolled 223 adolescents; 56% reported a history of sexual activity. Sixty-four percent stated that they had heard of EC. Participants with a history of sexual activity were more likely to have heard of EC compared with those without (odds ratio, 2.6; 95% confidence interval, 1.4–4.7), as were those 17 years and older (odds ratio, 2.3; 95% confidence interval, 1.2–4.3). The majority of participants were concerned about potential short-term and long-term adverse effects (86% and 78%, respectively); many participants were concerned about the cost of EC (45%) and about being able to get to a doctor for a prescription (45%). Participants supported using EC in the following situations: rape (88%), the condom breaks (82%), or no birth control was used (76%). Fewer supported using EC in the following situations: missed 1 oral contraceptive pill (51%) or first sexual experience (57%).
Conclusions:
Participants indicated that although they would support EC use in several situations, they have concerns about EC use and access. Awareness of these factors and potential influences of EC use can guide providers toward effective counseling and interventions aimed to increase adolescents’ use of EC in appropriate settings.
Keywords: emergency contraception, adolescents, pregnancy
Unintended teenage pregnancy is a major public health issue. In 2009, although the birth rate for young women ages 15 through 19 years was the lowest ever recorded, there were still more than 410,000 births to adolescent girls.1 Furthermore, the United States has by far the highest teenage pregnancy rate of any industrialized nation.2 An estimated 80% of teenage pregnancies are unintended3; despite this, a significant proportion of ‘teenagers report using no contraception during their first sexual intercourse.4 Similarly, according to the Youth Risk Behavior Survey, of the 34% of high school students who report being currently sexually active, only 61% and 20% reported using condoms or oral contraceptives, respectively, during their most recent sexual intercourse.5 Concern over adolescent pregnancy was highlighted in the US Department of Health and Human Services’ Healthy People goals for 2010 and recently again for 2020,6 based on the knowledge that teenage pregnancy is associated with a higher risk of poor outcomes such as low birth weight, prematurity, and intrauterine growth retardation.7,8 In addition, adolescent pregnancy places a heavy social and economic burden on mothers, fathers, babies, and society.9–12
The emergency contraception pill (EC) is one option available for pregnancy prevention. Although EC is widely used in other countries, many women in the United States, particularly adolescents, are unaware of this pregnancy prevention option. In addition to a lack of knowledge about EC,13–16 studies suggest that additional barriers to its use exist, such as social and familial disapproval, negative attitudes of health care providers that may impact accessibility, and concerns about adverse effects.17–19 Although several national medical organizations have called for increased access to EC for adolescents20–22 and the Food and Drug Administration recommended that age restrictions for behind-the-counter access to EC be lifted, the director of the US Department of Health and Human Services recently ruled to continue limiting over-the-counter access of EC.23 Given this recent development, it is now more critical than ever to determine which access concerns, barriers, and specific knowledge gaps should be targeted when designing a strategy to reduce unintended teenage pregnancy.
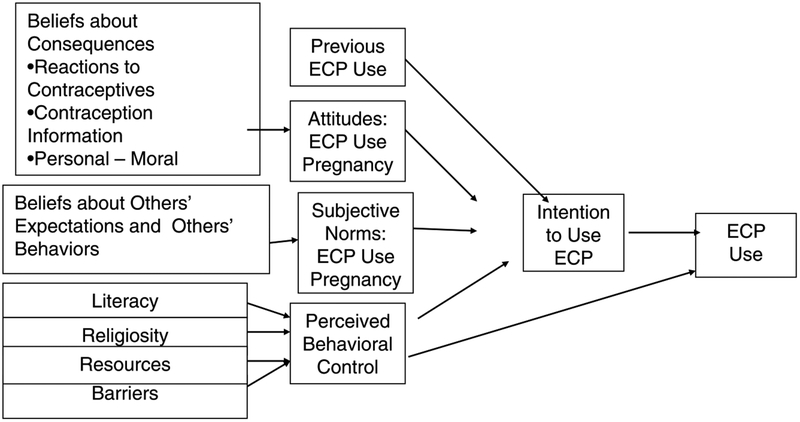
The theory of planned behavior (TPB)24 is a conceptual framework that can be used to understand the decision-making processes of adolescents and can be useful to understand intentions to use EC. The theory states that personal and social beliefs and values determine personal attitudes and perceived social expectations (“subjective norms”) and that various additional factors can influence perceived behavior control. These attitudes, subjective norms, and perceived behavior control in turn influence behavioral intention, which then influences actual behavior. (Fig. 1) By assessing these specific constructs, we can obtain information about specific areas for interventions aimed at increasing intention to perform a behavior. The TPB is a comprehensive model that has been assessed and validated for understanding a variety of health conditions including rule following in homeless youth, promotion of physical activity, and healthy eating.25–28 In addition, the TPB has also been used to understand sexual risk behaviors in adolescents.29–31
FIGURE 1.
Modified TPB, Adapted to model EC use.
The emergency department (ED) is an important site to reach adolescents at risk for pregnancy. Adolescents use the ED more frequently than adults and often seek care for nonurgent complaints32; in addition, adolescents with higher levels of risk behaviors such as substance use and depression are more likely to use the ED as their primary source of care.33 A significant proportion of teenagers may be at risk of pregnancy at the time of their ED visit; a study conducted at 2 urban EDs found that between 10% and 47% of sexually active 15- to 18-year-olds reported that they used no form of contraception and were not trying to become pregnant,34 and a more recent study found that 14% of sexually active adolescents reported unprotected intercourse within the 5 days preceding the ED visit.35 Therefore, we chose to focus on a population of adolescents seeking care in the ED. This study builds on our previous work, in a larger, more diverse sample of female adolescents; we used the framework of the TPB to assess urban adolescents’ knowledge of and attitudes about EC and to assess intention to use EC in particular hypothetical situations to identify areas of concern to be addressed in future interventions. Based on our previous work, we hypothesized that within the constructs of the TPB, attitudes would be affected by limited knowledge, that opinions of mothers and boyfriends would play an important role in intention to use EC, and that barriers such as cost and confidentiality would limit access to EC. In addition, we hypothesized that adolescents would support using EC in certain situations.
METHODS
Study Design and Setting
We conducted a cross-sectional survey with adolescent girls seeking care in 2 urban, children’s hospital EDs. Hospital 1 [name deleted for blinding], located in the Northeastern United States, cares for approximately 90,000 patients each year, and hospital 2, located in the Midwest, cares for almost 70,000 patients each year. The majority of patients at hospital 1 are black (65%), with the remainder being primarily white (23%). The racial/ethnic breakdown at hospital 2 is 40% black, 33% non-Hispanic white, and 20% Hispanic white. The majority of patients at both hospitals are on Medicaid (57% hospital 1, 69% hospital 2), with the remainder reporting private insurance (39% and 21%, respectively) and self-pay (4% and 9%, respectively). The study protocol and consent procedures were approved by the institutional review boards at both institutions.
Study Population
Subjects were included at hospital 1 if they were adolescent girls between the ages of 15 and 19 years (inclusive), if they resided in 1 of 11 zip codes surrounding the hospital, and if they were black and English speaking, as self-identified to the ED registrar at the time of presentation to the ED. These criteria directly mirrored the inclusion criteria of previous work by the authors in this area, in which in-depth interviews were conducted to explore adolescents’ attitudes and beliefs about pregnancy prevention and EC. For that exploratory work, these inclusion criteria were selected to reflect a somewhat culturally homogenous population, given the potentially diverse range of opinions related to teen pregnancy and emergency contraception use.17 Because this project was developed as a direct result of that work, we continued to use the same inclusion criteria. However, to increase the diversity of responses for this study, we added an additional site, and slightly broader inclusion criteria were used at hospital 2: participants as young as 14 years old were included and there were no geographic or racial/ethnic limitations for inclusion. Participants were excluded at both institutions if they were identified by the patient care team as too acutely ill to participate or if they had significant developmental delay that would make completing the questionnaire difficult. Participants were not compensated for participation.
Study Protocol and Measurements
Trained research assistants (RAs) identified potentially eligible patients through the computerized ED tracking boards, which log information about all patient visits in real time. Once a potential participant was identified, an RA determined whether the patient met inclusion criteria; if so, verbal consent was obtained from the patient. We requested and were granted a waiver of parental consent because the study involved only participation in a confidential survey, which did not alter the course of the patients’ care, and a waiver of written consent because an informed consent document would be the only link between the participant and the study data.
The RA completed a verbal fixed-choice survey with each participant. During survey administration, only the participant and the RA were in the patient’s ED room. The survey was developed by the authors, based on literature review and expert opinion, and was pilot tested on 10 subjects before beginning study enrollment to insure readability and comprehension. The survey consisted of several sections: first, demographic data (including age, school enrollment, primary care provider, visits to a gynecologist, and sexual history) were collected. For example, to assess sexual history, the participants were asked, “Have you ever had sex with anyone, by which we mean have you ever had sexual intercourse?” Next, participants answered 4 questions designed to assess their knowledge about EC. All participants were then read a short paragraph with factual information about EC to insure a baseline level of knowledge for all of the participants. Then, they were asked questions to assess their attitudes and beliefs about EC. These questions were based on the results of previous work by the authors,17 in which in-depth interviews were conducted with a similar population on the same topic, and included constructs from the TPB (attitudes, perceived behavioral control, and subjective norms). Of note, knowledge is often included within the construct of attitudes when using the TPB because attitudes are shaped by knowledge. These questions used a Likert-type response scale. For example, participants were asked, “The morning pill is good because you only need to take it once [strongly agree, agree, neutral, disagree, strongly disagree]”; “If you were going to take the morning after pill, how worried would you be about short-term adverse effects—in other words, things that might happen to your body around the time that you take the medicine? [very worried, somewhat worried, not at all]; and “How would your mother feel if you told her you wanted to get the morning after pill? [strongly approve, somewhat approve, neutral, somewhat disapprove, strongly disapprove].” Finally, participants answered questions to assess their potential intention to use EC in general and given specific scenarios, with fixed-choice responses of yes, no, maybe, and not sure for each scenario. For example, participants were asked, “would you consider using EC if you were taking birth control pills but missed one?” “… if it was the first time you had sex?” At the end of the participant’s ED visit, the RA collected chief complaint from the medical record.
Data Analysis
Data were entered into a Microsoft Access database (Redmond, WA). Demographic characteristics were summarized by standard descriptive statistics (eg, means and SDs for normally distributed continuous variables such as age and percentages for categorical variables such as type of primary care provider). Differences in means between continuous variables were determined using the t test, and differences in categorical variables were determined using the χ2 test. In addition, descriptive summaries for questions from each domain of the TPB (knowledge/attitudes, subjective norms, and perceived behavioral control) were determined. For these analyses, answers from the Likert-type responses were collapsed into 2 categories (for example, very supportive/somewhat supportive and would not care/somewhat upset/very upset). For each question, the neutral response choice was grouped with the 2 negative response choices because we were interested in clearly assessing positive attitudes toward EC and made the a priori decision that patients with opinions that were not clearly positive would be grouped with those with negative opinions. Comparisons of specific question responses between dichotomized subgroups were performed using the χ2 test. Participants were stratified into 2 age groups for these comparisons: 14 through 16 years (“younger”) and 17 through 19 years (“older”). Stata 9.2 (Stat Corp, College Station, TX) was used for these analyses.
RESULTS
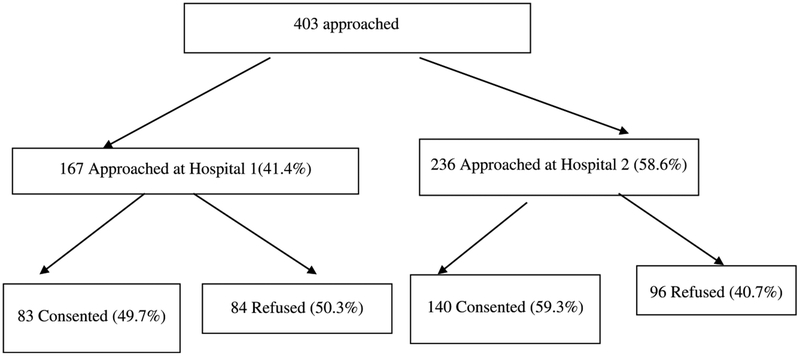
Participant enrollment began at hospital 1 in June 2008 and was completed in April 2009; enrollment at hospital 2 began in June 2009 and was completed in November 2009. A total of 403 adolescents were approached for enrollment; 223 (55.5%) consented for enrollment, 83 (37.2% of the total) at hospital 1 and 140 (62.8% of the total) at hospital 2. Refusal rates were similar at both institutions (50% at hospital 1, 40% at hospital 2) (Fig. 2). Demographic data of the study population, overall and by site of enrollment, are presented in Table 1. The majority (58%) of participants were younger than 17 years (n = 129). Demographic data (race/ethnicity and age) were collected for 90% of those who refused; those who refused were similar in these categories to those who consented. Most of those who refused reported “I do not have time” or “I do not feel like it” as the reason for refusal; for 22%, the parent refused participation on behalf of the patient. Just more than half (55.6%) of the participants reported a history of sexual activity, and 8% reported a history of one pregnancy; of these, 44% resulted in a live birth, 44% in an abortion, and 12% in a miscarriage. No participant reported being pregnant more than once. Approximately one fifth of the total sample (20.2%) reported that they were at risk for pregnancy in the next 6 months, including 4.5% who intended to become sexually active, because of actual or likely inconsistent contraception use. The patients’ chief complaints for the ED visit at both sites were extremely varied; abdominal pain was the most common complaint (15.7%), followed by injuries (9.9%), sore throat (5.8%), and respiratory distress (4.5%).
FIGURE 2.
Approached and, consented/enrolled.
TABLE 1.
Characteristics of the Study Population (n = 223)
| Overall (n = 223) | Hospital 1 (n = 83) (37.2) | Hospital 2 (n = 140) (62.8) | |
|---|---|---|---|
| Age, mean SD, y* | 16.1 (1.3) | 16.7 (1.1) | 15.8 (1.3) |
| n (%) | n (%) | n (%) | |
| Enrolled in school | 215 (96.4) | 81 (97.6) | 134 (95.7) |
| Race/ethnicity* | |||
| Black | 155 (69.5) | 83 (100) | 72 (51.4) |
| White | 45 (20.2) | 0 | 45 (32.1) |
| Hispanic/Latina | 12 (5.4) | 0 | 12 (8.6) |
| Mixed race | 10 (4.5) | 0 | 10 (7.1) |
| Asian | 1 (0.04) | 0 | 1 (0.1) |
| In care of a gynecologist | 49 (22.0) | 24 (28.9) | 25 (17.9) |
| History of sexual activity | 124 (55.6) | 53 (63.9) | 71 (50.7) |
| History of pregnancy* | 18 (8.0) | 14 (16.9) | 4 (2.9) |
P < 0.05.
With respect to specific knowledge of EC, 63.7% of participants stated “yes” to the question, “Have you ever heard of the morning after pill?”; just more than one quarter of participants (26.0%) reported they knew someone who had used it. Eight percent reported they personally had used EC in the past; of these 18 participants, 7 also had a history of pregnancy, including 4 with children. Participants with a history of sexual activity were more likely to have heard of EC compared with those without a history of sexual activity (odds ratio [OR], 2.6; 95% confidence interval [CI], 1.4–4.7), as were older participants (OR, 2.3; 95% CI, 1.2–4.3); in addition, the older participants were more likely to report having used EC in the past (OR, 4.0; 95% CI, 1.3–14.7). When asked about the correct timing of EC use through a multiple-choice question, only 7 participants (3.1%) knew that EC could be effective within 5 days of unprotected intercourse; an additional 12.1% believed that EC must be used within 3 days of unprotected intercourse (the correct timing as per the package insert). More than one quarter (27.4%) thought it must be used within 1 day, and almost half (42.2%) answered “do not know.”
Attitudes About EC
The majority of participants were concerned about potential short-term adverse effects (86.1%) and potential long-term adverse effects (78.3%) of using EC. In addition, the majority (81.6%) of participants was concerned that EC would not be effective if taken to prevent pregnancy. These attitudes did not differ significantly between those with and without a history or sexual activity or between the 2 age groups. Just more than half (52.6%) of participants agreed with the statement, “EC works faster than birth control pills.” Participants who were sexually active were significantly more likely to have this perception than those who were not (OR, 2.3; 95% CI, 1.3–4.1); there was no difference between the younger- and older-age groups.
Perceived Behavioral Control
Many participants were concerned about the cost of EC (44.8%) and about being able to get to a doctor for a prescription (44.8%). These results did not differ significantly between those who were sexually active and those who were not or between the younger- and older-age groups.
Subjective Norms
Most participants were not concerned that important people in their lives would disapprove of their potential use of EC. For example, only 26% of participants felt their mother would disapprove of EC use, and only 18% reported their boyfriend would disapprove of its use. However, close to half (40.8%) reported they would consider not using EC if their boyfriend had expressed interest in having a child. Although participants generally felt the people close to them would support their use of EC, many were concerned that someone they did not intend to know could find out they had taken it (46.2%). This concern was more likely to be expressed by participants who were not sexually active (OR, 2.0; 95% CI, 1.1–3.5). There was no significant difference between the younger and older participants with respect to these concerns.
Intention to Use EC
Of the 124 participants who reported being currently sexually active, 66.1% reported they would consider using EC in the future. For all participants, when presented with a series of scenarios in which a woman could consider using EC, most participants supported personal EC use in the case of rape (88.3%), if the condom had broken; (82.1%), or if no type of birth control had been used (75.7%). More than half of the participants supported personal EC use if it was their first sexual experience (57.0%) and if they were taking oral contraceptives but had missed one pill (50.7%). Again, there were not significant differences in these opinions among those with different sexual experiences or those of the different age groups.
There were no differences in attitudes, perceived behavioral control, subjective norms or intention to use EC between the 2 study sites.
DISCUSSION
Knowledge about EC among adolescents continues to be less than ideal. Multiple studies during the last 15 years have demonstrated an increase in awareness of EC in this population, with reported rates of awareness ranging from 30% to 73%.13–17,36 However, although the rate of awareness has increased through the last decade, there has been little reported change in the last several years; Aiken et al37 reported in 2005 that 73% of the adolescents surveyed were aware of EC, compared with the findings by Ahern et al14 in which 70% were aware of EC and our findings that approximately two thirds of the study population had heard of EC. Our results do suggest that some subgroups of adolescents may have higher awareness than others, however, such as those with a history of sexual activity and older adolescents.
Unfortunately, even if awareness of EC were 100%, it is likely that awareness alone is not sufficient to increase use. Several studies have found that women, including adolescents, may not choose to use EC because they feel ashamed or embarrassed, are worried about what others think, and have concerns about adverse effects.17,18,38 Our results are similar to those previously reported, including those of our qualitative work,17 although this project allowed us to better quantify the attitudes and beliefs that were previously identified through in-depth interviews with similar adolescents. We again found that our population of adolescent girls had limited knowledge of the correct timing of use for EC, believed that EC somehow works faster than oral contraceptives, had concerns about cost and adverse effects, and were concerned about access to a prescription and about confidentiality. However, despite these concerns, we also found that adolescent women report important people in their lives would support EC use if needed. Interestingly, despite the concerns identified about EC, we found that adolescents are supportive of the use of EC in many specific scenarios and many would consider using EC themselves.
This geographically diverse group of urban adolescents provides some insight into the issues that need to be addressed to increase appropriate use of EC. Our previous work with this population helped us understand, in conjunction with previously published work, what attitudes, barriers, and knowledge gaps we should explore and helped us identify which people adolescents turn to for pregnancy prevention advice and guidance. This study has further clarified specific barriers and deficits regarding EC (including concerns about potential adverse effects, privacy, access, and cost) so that we can develop interventions, which include an EC component aimed at reducing adolescent pregnancy. Providers discussing contraception options with adolescents should be aware of the range of specific concerns that adolescents may have about EC, keeping in mind that although knowledge of the method may exist, there are potentially other concerns and/or misconceptions that should be addressed. Furthermore, providers can consider involving those close to the patient (with the adolescent’s permission) and can work with the adolescent to identify a supportive adult who can aid in contraceptive decision making. Finally, as adolescents are often concerned about cost and access, providers can work toward educating their patients about options for obtaining EC if needed; this may include advance provision in appropriate circumstances.
Our study has several limitations. First, the population at 1 site was limited to a more homogeneous group. However, the addition of a second site increased the diversity of the sample, and given the similarity of our results to those published previously, we believe our findings are generalizable to other urban settings. Second, approximately 50% of patients who were eligible for the study declined participation; so our results may be affected in that those who chose to participate may have had more knowledge or stronger opinions about EC. However, those who declined were similar to those who participated in age and race/ethnicity; we did enroll a group of varying ages, chief complaints, and ethnicities, and we found a range of opinions about the different concerns related to EC.
In conclusion, in a closed-ended, fixed-choice survey, urban, minority adolescent girls from 2 geographically distinct EDs indicated that although they would support EC use in several situations, they lack specific knowledge about EC and have concerns about EC use and access to EC. Awareness of these factors and potential influences of EC use can guide providers toward effective counseling and interventions aimed to increase adolescents’ use of EC in appropriate settings.
Acknowledgments
This project was supported by funds from the Nicolas Crognale Chair of Emergency Medicine at The Children’s Hospital of Philadelphia.
Footnotes
Disclosure: The authors declare no conflict of interest.
This study was presented at the Pediatric Academic Societies Annual Meeting, May 2010, Vancouver, Canada (poster).
REFERENCES
- 1.Centers for Disease Control and Prevention. Vital signs: teen pregnancy—United States, 1991–2009. MMWR Morb Mortal Wkly Rep. 2011;60:414–420. [PubMed] [Google Scholar]
- 2.Martin JA, Hamilton BE, Sutton PD, et al. Births: final data for 2007. Natl Vital Stat Rep. 2010;58:1–85. [PubMed] [Google Scholar]
- 3.Williams L, Morrow B, Shulman H, et al. Prams 2002 Surveillance Report. Atlanta, GA: Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 4.Abma JC, Martinez GM, Mosher WD, et al. Teenagers in the United States: sexual activity, contraceptive use, and childbearing, 2002. Vital Health Stat 23. 2004;23:1–48. [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance—United States, 2009. MMWR Morb Mortal Wkly Rep. 2010;59:20–22. [Google Scholar]
- 6.U.S. Department of Health and Human Services. Healthy People 2020: Objectives for Improving Health: Objective Topic Area 2, Adolescent Health. Washington, DC: U.S. Department of Health and Human Services; 2010. [Google Scholar]
- 7.Cunnington AJ. What’s so bad about teenage pregnancy? J Fam Plann Reprod Health Care. 2001;27:36–41. [DOI] [PubMed] [Google Scholar]
- 8.Fraser AM, Brockert JE, Ward RH. Association of young maternal age with adverse reproductive outcomes. N Engl J Med. 1995;332: 1113–1117. [DOI] [PubMed] [Google Scholar]
- 9.Kids Having Kids. A Robin Hood Foundation special report on the costs of adolescent childbearing. Maynard RA, ed. Washington DC: Urban Institute Press; 1997. [Google Scholar]
- 10.Annie E Casey Foundation. Kids Count Special Report: When Teens Have Sex: Issues and Trends. Baltimore, MD: Annie E. Casey Foundation; 1998. [Google Scholar]
- 11.Hofferth S, Reid L, Mott FL. The effects of early childbearing on schooling over time. Fam Plann Perspect. 2001;33:259–267. [PubMed] [Google Scholar]
- 12.Trussel J, Lalla AM, Doan QV, et al. Cost effectiveness of contraceptives in the United States. Contraception. 2009;79:5–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abbott J, Feldhaus KM, Houry D, et al. Emergency contraception: what do our patients know? Ann Emerg Med. 2004;43:376–381. [DOI] [PubMed] [Google Scholar]
- 14.Ahern R, Frattarelli LA, Delto J, et al. Knowledge and awareness of emergency contraception in adolescents. J Pediatr Adolesc Gynecol. 2010;23:273–278. [DOI] [PubMed] [Google Scholar]
- 15.Chuang CH, Freund KM. Emergency contraception knowledge among women in a Boston community. Contraception. 2005;71:157–160. [DOI] [PubMed] [Google Scholar]
- 16.Cohall AT, Dickerson D, Vaughan R, et al. Inner-city adolescents’ awareness of emergency contraception. J Am Med Womens Assoc. 1998;53:258–261. [PubMed] [Google Scholar]
- 17.Mollen CJ, Barg FK, Hayes KL, et al. Assessing attitudes about emergency contraception among urban, minority adolescent women: an in-depth interview study. Pediatrics. 2008;122:e395–e401. [DOI] [PubMed] [Google Scholar]
- 18.Free C, Lee RM, Ogden J. Young women’s accounts of factors influencing their use and non-use of emergency contraception: in-depth interview study. BMJ. 2002;325:1393–1397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller MK, Plantz DM, Dowd MD, et al. Pediatric emergency health care providers’ knowledge, attitudes, and experiences regarding emergency contraception. Acad Emerg Med. 2011;18:605–612. [DOI] [PubMed] [Google Scholar]
- 20.Committee on Adolescence, American Academy of Pediatrics. Emergency contraception. Pediatrics. 2005;116:1026–1035.16147972 [Google Scholar]
- 21.American College of Obstetrics and Gynecology. ACOG practice bulletin: emergency oral contraception. Int J Gynaecol Obstet. 2002;78:191–198. [DOI] [PubMed] [Google Scholar]
- 22.Gold MA, Sucato GS, Conard LA, et al. Provision of Emergency contraception to adolescents. J Adolesc Health. 2004;35:67–70. [DOI] [PubMed] [Google Scholar]
- 23.American Medical Association. HHS keeps emergency contraception behind the counter. Amednews.com. Available at: http://www.ama-assn.org/amednews/2011/12/19/gvbf1219.htm. Accessed January 20, 2012.
- 24.Ajzen A From intentions to actions: a theory of planned behavior. In: Kuhl J, Becman J, eds. Action-Control: From Cognition to Behavior. Heidelberg, Germany: Springer; 1985:11–39. [Google Scholar]
- 25.Broadhead-Fearn D, White KM. The role of self-efficacy in predicting rule-following behaviors in shelters for homeless youth: a test of the theory of planned behavior. J Soc Psychol. 2006;146:307–325. [DOI] [PubMed] [Google Scholar]
- 26.Rah JH, Hasler CM, Painter JE, et al. Applying the theory of planned behavior to women’s behavioral attitudes on and consumption of soy products. J Nutr Educ Behav. 2004;36:238–244. [DOI] [PubMed] [Google Scholar]
- 27.Tsorbatzoudis H Evaluation of a planned behavior theory-based intervention programme to promote healthy eating. Percept Mot Skills. 2005;101:587–604. [DOI] [PubMed] [Google Scholar]
- 28.Tsorbatzoudis H Evaluation of a school-based intervention programme to promote physical activity: an application of the theory of planned behavior. Percept Mot Skills. 2005;101:787–802. [DOI] [PubMed] [Google Scholar]
- 29.Cha ES, Doswell WM, Kim KH, et al. Evaluating the theory of planned behavior to explain intention to engage in premarital sex amongst Korean college students: a questionnaire survey. Int J Nurs Stud. 2007;44:1147–1157. [DOI] [PubMed] [Google Scholar]
- 30.Hutchinson MK, Wood EB. Reconceptualizing adolescent sexual risk in a parent-based expansion of the theory of planned behavior. J Nurs Scholarsh. 2007;39:141–146. [DOI] [PubMed] [Google Scholar]
- 31.Myklestad I, Rise J. Predicting willingness to engage in unsafe sex and intention to perform sexual protective behaviors among adolescents. Health Educ Behav. 2007;34:686–699. [DOI] [PubMed] [Google Scholar]
- 32.Ziv A, Boulet JR, Slap GB. Emergency department utilization by adolescents in the United States. Pediatrics. 1998;101:987–994. [DOI] [PubMed] [Google Scholar]
- 33.Wilson KM, Klein JD. Adolescents who use the emergency department as their usual source of care. Arch Pediatr Adolesc Med. 2000;154:361–365. [DOI] [PubMed] [Google Scholar]
- 34.Todd CS, Moutvarner G, Lichenstein R. Unintended pregnancy risk in an emergency department population. Contraception. 2005;71:35–39. [DOI] [PubMed] [Google Scholar]
- 35.Fine L, Mollen CJ. A pilot study to assess pregnancy risk and need for emergency contraception in a pediatric emergency department population. Pediatr Emerg Care. 2010;26:413–416. [DOI] [PubMed] [Google Scholar]
- 36.Johnson R, Nshow M, Nye AM, et al. There’s always Plan B: adolescent knowledge, attitudes and intention to use emergency contraception. Contraception. 2010:81:128–132. [DOI] [PubMed] [Google Scholar]
- 37.Aiken AM, Gold MA, Parker AM. Changes in young women’s awareness, attitudes, and perceived barriers to using emergency contraception. J Pediatr Adolesc Gynecol. 2005;18:25–32. [DOI] [PubMed] [Google Scholar]
- 38.Karasz A, Kirchen NT, Gold M. The visit before the morning after: barriers to prescribing emergency contraception. Ann Fam Med. 2004;2:345–350. [DOI] [PMC free article] [PubMed] [Google Scholar]