Abstract
Erosive pustular dermatosis of the scalp is a rare chronic inflammatory disorder defined. It usually affects elderly people and is characterized by extensive pustular lesions, erosions, and crusts located on the scalp. The pathogenesis of this disease is not completely understood, but a known predisposing factor is skin trauma. Autoimmune disorders including rheumatoid arthritis, autoimmune hepatitis, Hashimoto thyroiditis, and Takayasu aortitis are associated diseases reported. The clinical examination reveals erythema, erosions, crusts, follicular pustules, and in advanced stages, scarring alopecia. A scalp biopsy is recommended but not specific, founding epidermal atrophy, focal erosions, and a mixed inflammatory infiltrate consisting of neutrophils, lymphocytes, and plasma cells. Bacterial cultures, fungal and viral stains are not necessary and are usually negative. . Topical high-potency corticosteroids, retinoids, calcipotriol, dapsone, and topical tacrolimus are reported treatments, while photodynamic therapy has been effective in some patients, but has induced the disease in others. All the findings are suggestive but not specific, so it is an excluding diagnosis. The combination of predisposing factors is very important for a correct diagnosis, such as elderly age, sun-damaged skin, presence of androgenetic alopecia, together with clinical manifestations, non-specific histology and laboratory investigations negative for other disease. In our opinion, this scalp disease is a challenge for the dermatologist. We review all the literature to better define the possible solutions in case of suspected erosive pustular dermatosis of the scalp.
Keywords: scalp erosions, cicatricial alopecia, scarring alopecia, trichoscopy, scalp trauma
Introduction
Erosive pustular dermatosis of the scalp (EPDS) is a rare inflammatory condition of the scalp characterized by one or more areas of alopecia with erosions, thick yellow or yellow-brown crusts, superficial ulceration, and pustules that develop over several months or even years, leading to atrophic skin and scarring alopecia. It occurs most commonly in the elderly with bald and sun-damaged scalp, with a history of trauma to the scalp. Types of trauma reported before onset of EPDS are multiple: mechanical traumas, physical therapies, herpes zoster of the scalp, and topical drugs. Histologically, EPDS shows a non-specific inflammatory reaction with atrophic epidermis and chronic inflammation, starting with a spongiotic pustular superficial reaction in the early stage and following with a mixed inflammatory infiltrate of neutrophils, lymphocytes, and plasma cells until giant cells in the late stages. Bacterial and mycologic cultures are negative because the pustules are sterile. The clinical presentation of EPDS mimics different diseases, such as scalp infections, bullous diseases, and scarring alopecia. Treatment modalities include topical and systemic corticosteroids, tacrolimus, and calcipotriol. EPDS might require long-term management.
The most important challenges of EPDS are differential diagnosis, trichoscopy, histopathology, treatment, and follow-up.
In spite of the multiple challenges, solutions are possible and we propose in this review a guideline to manage the course of EPDS starting from the differential diagnosis, to aid clinical practice, to help the recognition of this non-specific inflammatory hair disease, whilst proving insight into the current understanding, management, and treatment of EPDS.
Text
EPDS is a rare inflammatory disease with a chronic course and the need of long-term management. Because of its rarity, the true incidence and prevalence of EPDS are unknown. Internationally, a female propensity is observed, with an estimated female to male preponderance of 2:1.1 EPDS predominantly affects elderly people with aging of onset at 60–70 years.2 A history of trauma to the scalp before the onset of the disease is common as well as severe androgenetic alopecia and scalp chronic actinic damage, but a few cases of EPDS in children have been reported.3 Usually, these rare cases have been linked to prolonged labor and caput succedaneum or surgical procedures.4
EPDS is considered as an underappreciated mimicker of different skin disorders of the scalp; the clinical picture can easily be mistaken for an infection, inflammation, or neoplastic reaction. It was first described as an inflammatory dermatosis in the late 1970s by Burton and Pye et al.5,6 Lesions can be solitary or multiple, some of them confluent. Sterile pustules, superficial erosions, and round or oval crusted lesions on atrophic skin, resulting in cicatricial alopecia, characterize the typical clinical presentation (Figure 1). The most affected area of the scalp is the vertex.2 The scalp lesion is not painful, nor does it itch.
Figure 1.

Typical clinical aspect of EPDS with superficial erosions and crusted lesions on atrophic skin.
Abbreviation: EPDS, erosive pustular dermatosis of the scalp.
The etiology of EPDS is also poorly understood. Actinic damage and epidermal atrophy are thought to be a predisposing factor (Figure 2). Numerous other factors have been associated with the onset of condition, including various topical medications, infections, surgical procedures, or topical agents; it is, however, unknown if they play a direct role in the pathogenesis. There have also been reports of EPDS arising after topical treatment with ingenol mebutate7 or after photodynamic therapy (PDT).8 Perhaps the most common precipitating factor is mechanical trauma, but cessation of the trauma does not result in clearing of the EPDS. The median time between the triggering event and the onset of the first signs of EPDS is generally 6 months.2
Figure 2.
Actinic damage and epidermal atrophy can predispose to EPDS.
Abbreviation: EPDS, erosive pustular dermatosis of the scalp.
Bacteriologic and mycologic workups have negative results, and histopathologic evaluation findings are non-specific, but it is recently proposed to include it in the neutrophilic dermatosis due to its similarity to neutrophilic superficial folliculitis.9
Many autoimmune disorders are associated to EPDS, such as rheumatoid arthritis, autoimmune hepatitis, Hashimoto thyroiditis, and Takayasu aortitis.10–12 Impaired immunity and microcirculation may play a role in the pathogenesis of this disease.13 Recently, a new definition termed as “immunosenescence” has been used to describe the decline of immune system in fidelity and efficiency with aging; this may result in increased susceptibility to pathological conditions related to inflammation or autoreactivity.14 The hair follicle is a site of immune privilege, where factors such as loss of normal epidermal barrier and ultraviolet damage may induce a reaction of immune dysregulation. In EPDS, alopecia is secondary to chronic inflammation with subsequent destruction of the hair follicle, in particular, follicular stem cells.15 For this reason, the mainstay of treatment of EPDS is based on drugs that induce an immunosuppression, such as the local steroids or immunomodulating agents.
At the end, four elements contribute to the development of EPDS: an initial trauma to the scalp, inherent skin atrophy from aging combined with actinic damage concentrated in the area of the scalp prone to androgenetic alopecia, resulting in a prolonged and altered immune response, leading to consequent scarring and permanent hair loss.
For the correct diagnosis to be established and thus adequate treatment to be initiated, it is crucial that both clinicians and dermatopathologists be familiar with this condition. EPDS diagnosis is based on a combination of pertinent findings divulged from history, examination, trichoscopy, and histopathology.
Clinical features
Although the etiopathogenesis of EPDS remains unclear, its classification is split between a chronic, inflammatory dermatosis and an immunologic dysfunction,13 and a common predisposing condition seems to be the cutaneous atrophy typical of elderly, eventually worsen by chronic photo-damage, and local trauma, including surgery or contact dermatitis. So, clinical history is very important in case of suspected EPDS.
Physical examination of scalp reveals multiple erythematous large, erosive, and crusted patches with overlying and surrounding pustules and serum exudate involving the bald areas of the scalp with a predominance of the vertex (Figure 3). Excessive granulation tissue may cover the erosion.16 Affected areas undergo a continuous cycle of healing and recurrence, resulting in atrophic skin with new areas of pustules and erosions, in the center or in the borders of the initial lesion.
Figure 3.
A severe case of EPDS large, erosive, and crusted patches with overlying and surrounding pustules and serum exudate involving the bald areas of the scalp at the vertex.
Abbreviation: EPDS, erosive pustular dermatosis of the scalp.
EPDS clinical presentation can often be mistaken for different hair scalp diseases, starting from infections to inflammatory condition, until scalp skin cancer. Disorders to be considered in the differential diagnosis for EPDS include bacterial and fungal infections, in which a mycological investigation would be sufficient to differentiate. Differential diagnosis with skin epithelial tumors needs a biopsy, especially needed in all treatment-refractory patients with EPDS. Indeed, patients with EPDS should be monitored for possible development of these or other cutaneous malignancies. Finally, the autoimmune disease pemphigus foliaceus can be ruled out with a Tzanck smear test or histopathology.17 Immunofluorescence study is also mandatory to rule out pemphigous group.
Trichoscopy
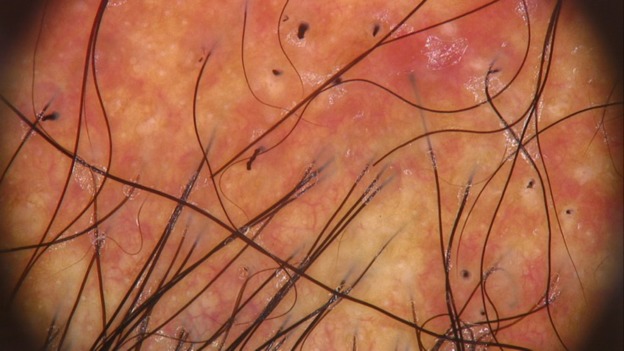
Trichoscopic examination shows different patterns that are non-specific of EPDS, such as follicular keratotic plugging, milky red areas, white patches, hair shaft tortuosity, tapering hair, and absence of follicular openings (Figure 4). In regard to the trichoscopic findings, follicular keratotic plugging and absence of follicular openings are common in scarring alopecia.18 Milky red areas and white patches are thought to reflect inflammation and scarring of the scalp. Tapering hair and hair shaft shape changes are related to hair cycle changes.
Figure 4.
Trichoscopy picture showing absence of follicular openings, hemorrhagic crusts, and hair shaft tortuosity.
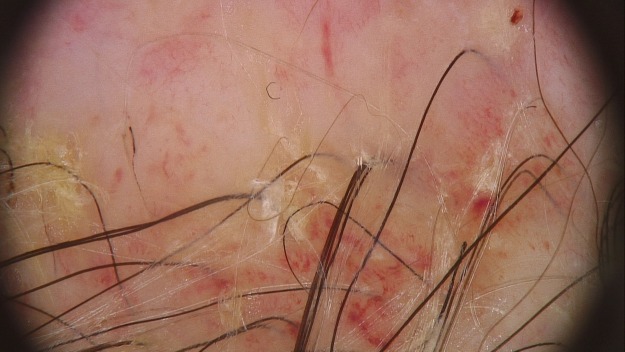
With trichoscopy, it is possible to classify two different phases of EPDS: active phase and a chronic phase.2 The active phase is characterized by perifollicular serous, black-yellow crusts, patchy brown-gray skin hyperpigmentation, tortuous and curved hair shaft like pili torti, several hair shafts broken a few millimeters above the scalp and finally hair tufting with no more than four hairs emerging from the same unit (Figure 5). The trichoscopic findings of most cases of chronic EPDS reveal marked atrophic skin, lack of follicular ostia, and follicular yellow thick exudate (Figure 6). The most specific feature of EPDS is the anagen bulb visible thought the atrophic skin.19 Another important trichoscopic aspect is the presence of prominent telangiectasias, especially after detachment of the crusts.15 The visualization of enlarged dermal vessels has also been described.2 A recent article pointed out a unique dermoscopic pattern typical of the hypergranulation variant of EPDS consisting of different types of vessels: linearly stretched and dilated, telangiectatic and polymorphous on focus vessels, confluent vessels, milky red and white areas (Figure 7).18
Figure 5.
Active phase of the disease with red and milky areas, absence of follicular opening, and several hair shafts broken.
Figure 6.
Trichoscopy of chronic EPDS where there is evident marked atrophic skin, lack of follicular ostia, and follicular yellow thick exudate.
Abbreviation: EPDS, erosive pustular dermatosis of the scalp.
Figure 7.
The hypergranulation variant of EPDS showing different types of vessels at trichoscopy.
Abbreviation: EPDS, erosive pustular dermatosis of the scalp.
Histopathology
EPDS might be underrecognized on pathology, because of the lack of specific and pathognomonic histopathological findings.20,21 A large deep biopsy is crucial for confirming/ruling out any other scalp diseases that might be mimicking EPDS and should be followed by histologic and immunofluorescent (IF) examination.17
Non-specific histologic findings of EPDS seen in early stages of the condition show sterile pustules, epidermal changes including hypertrophy or atrophy, prominent dermal edema with telangiectasia, and erosions. Density of hair follicles is generally normal with increased ratio of catagen to anagen follicles. In addition, early findings can include a polymorphous dermal inflammatory infiltrate composed of neutrophils, lymphocytes, plasma cells, and even foreign body giant cells (Figure 8). Although neutrophils, plasma cells, and giant cells are commonly seen in EPDS, these findings should not be considered pathognomonic because of their prevalence in many other conditions. Hematoxylin–eosin stain can also be used to rule out cutaneous malignancies, such as SCC and basal cell carcinoma, and neutrophilic dermatoses, such as pyoderma gangrenous. Direct IF and special stains should be used to rule out autoimmune blistering conditions such as pemphigus, and PAS stain to exclude a fungal infection.2,22
Figure 8.
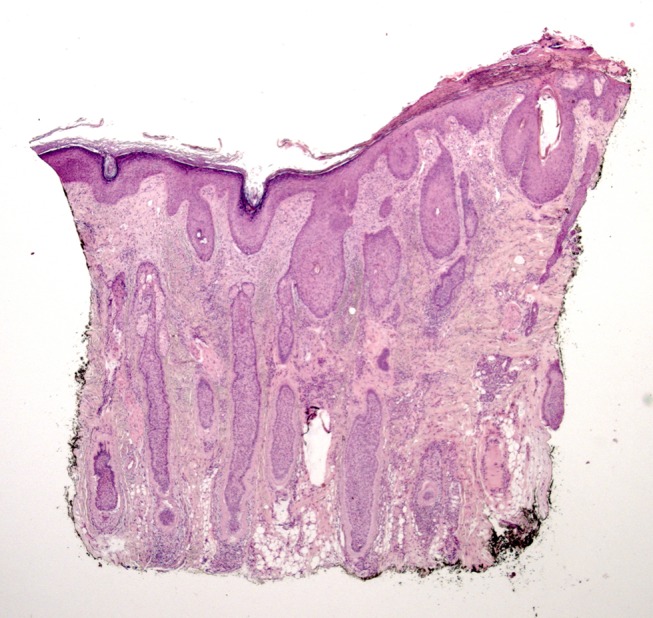
Early stage of erosive pustular dermatosis of the scalp: pathology shows laminated orthokeratosis and psoriasiform hyperplasia at the epidermis; slight mixed inflammatory infiltrate mainly consisting of neutrophils, lymphocytes, and plasmocytes, and mild fibrosis at the papillary dermis; hair follicular density is normal, with terminal, miniaturized anagen follicles and an increased number of catagen follicles.
Treatment
Because of the rarity and unknown etiology of EPDS, there is no established treatment recommendation, but the topical therapies are the most and first line used. Therapy focuses on reducing inflammation, healing erosions, and halting the progression of scarring alopecia, with treatment started as early as possible to minimize permanent hair loss. EPDS is a chronic recurring disease requiring extended therapy, ranging from weeks to months.
Possible treatments include systemic or topical corticosteroids, topical tacrolimus, oral or topical retinoids, topical calcipotriol, PDT, dapsone gel, silicone gel, and oral zinc sulfate. Corticosteroids, tacrolimus, and wound dressings appear to be more effective and are considered first-line treatments to promote re-epithelialization.15 High-potency topical corticosteroids are the most frequently used treatment and are established as effective and safe with almost a complete resolution after 1–2 months.2 However, some disadvantages of topical steroids include the risk of skin atrophy and EPDS relapse after drug withdrawal. If no improvement is observed after the first 2 months, discontinuation of steroids is advisable. Topical tacrolimus 0.1% alone may be attempted in this case or can be used proactively to prevent relapses. If topical corticosteroids fail to resolve the lesions, due to the inability to penetrate hyperkeratosis crusts, a possible treatment option is curettage followed by aminolevulinic acid PDT.23 This therapeutic opportunity is controversial because this compound of PDT increases lipophilic property and longer incubation period may contribute to toxicity and trigger EPDS.24 This direct healing promotes improved outcomes and delivers a positive quality of life to an otherwise recalcitrant and refractory disease. Refractory erosive pustular dermatosis may benefit from topical calcipotriol, short courses of systemic steroids, doxycycline, isotretinoin, acitretin, or dapsone.12–15
Recently in the literature, a treatment algorithm for EPDS to follow on the basis of the response of the traditional therapy has been described.25 This algorithm focuses on a practical approach of the treatment in the different stages of EPDS.
Follow-up
EPDS is an uncommon condition that is reported after local injuries. This condition has a slowly progressive and sometimes relapsing course. Because of the waxing and waning course of the condition, the earlier the treatment is provided, the greater the response with minimal risk of recurrence.12
Most patients show an undulating clinical course with intermittent improvement yet no healing despite topical anti-inflammatory treatment; in some individuals, the lesions heal in scarring with cicatricial alopecia. Beside the rarity of the observation, long-term follow-up for the development of cutaneous malignancy or possible relapses is advisable.
Conclusion
EPDS is clinically characterized by an erythematous skin erosion with thick crusts and pustules with alopecia. Recurrent erosions, crusts, and pustules over time result in scarring and subsequent alopecia, telangiectasia, and atrophy of the skin. The hyperkeratotic lesions are not painful and pruritus is rare.
Clinicians are hesitant to make a diagnosis of a disease that lacks pathognomonic histologic and laboratory findings, which may leave EPDS frequently unrecognized and underreported.
The pathology of EPDS is not fully understood and remains to be elucidated. The chronic actinic damage plays a role in the etiology of EPDS. Different trigger factors have been reported. An autoimmune mechanism, based on the possible association with autoimmune disorders as well as the frequent response to steroid and anti-inflammatory treatments, has been proposed in order to explain the complexity of the onset and maintenance of this skin reaction.11 Scalp traumas on a sun-damaged atrophic scalp may begin and prolong an immunological reaction, due to an increased expression of pro-inflammatory factors. In this context, an immune-mediated reaction is maintained until steroid therapy is administered, leading to remission of clinical manifestations. The response to corticosteroids by EPDS suggests immunological dysfunction may be related to the pathomechanism, and the response to corticosteroids can aid in diagnosis.
First-line treatments include topical high-potency corticosteroids and immunomodulating topical therapy. Second-line treatments include systemic therapy or PDT. Corticosteroids have been proven to be effective in the treatment of most of these cases, but relapses after discontinuation are common. If the patient does not respond to empiric treatment, then a biopsy should be considered.
EPDS may be underdiagnosed and likely underreported because many scalp diseases can mimic its clinical manifestation even scalp atrophy with erosion in a bald area of the scalp in elderly individuals and a history of previous trauma at the same site is common of EPDS.
This review of EPDS demonstrates many aspects: how clinical acumen may appropriately diagnose the disease, how topical corticosteroids are an effective treatment for this condition, and how the follow-up is very important to avoid the possible relapses.
Author contributions
All authors contributed towards data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Patton D, Lynch PJ, Fung MA, Fazel N. Chronic atrophic erosive dermatosis of the scalp and extremities: a recharacterisation of erosive pustular dermatosis. J Am Acad Dermatol. 2007;57:421. doi: 10.1016/j.jaad.2007.04.026 [DOI] [PubMed] [Google Scholar]
- 2.Starace M, Loi C, Bruni F, et al. Erosive pustular dermatosis of the scalp: clinical, trichoscopic, and histopathologic features of 20 cases. J Am Acad Dermatol. 2017;76(6):1109–1114.e2. doi: 10.1016/j.jaad.2016.12.016 [DOI] [PubMed] [Google Scholar]
- 3.Fertig R, Maddy A, Cadore de Faris D, Simao Correa Fiho S, Rigatti M, Tosti A. Erosive pustular dermatosis of the scalp after aplasia cutis congenita in a 9-year-old patient: a 5-year follow-up. Pediatr Dermatol. 2017;34:695–696. doi: 10.1111/pde.13252 [DOI] [PubMed] [Google Scholar]
- 4.LaCour M, Allen T, Wilkerson M, Nguyen AV. A case of erosive pustular dermatosis in a pediatric patient. JAAD Case Rep. 2019;5:118–120. doi: 10.1016/j.jdcr.2018.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Burton JL. Case for diagnosis. Pustular dermatosis of the scalp. Br J Dermatol. 1977;97 Suppl:15-67-9. [DOI] [PubMed] [Google Scholar]
- 6.Burton JL, Peachey RD, Pye RJ. Erosive pustular dermatosis of the scalp–a definition. Br J Dermatol. 1988;119(3):411. doi: 10.1111/bjd.1988.119.issue-3 [DOI] [PubMed] [Google Scholar]
- 7.Rongioletti F, Chinazzo C, Javor S. Erosive pustular dermatosis of the scalp induced by ingenol mebutate. J Eur Acad Dermatol Venereol. 2016;30(11):e110–e111. doi: 10.1111/jdv.13652 [DOI] [PubMed] [Google Scholar]
- 8.Lopez V, Lopez I, Ramos V, Ricart JM. Erosive pustular dermatosis of the scalp after photodynamic therapy. Dermatol Online J. 2012;18(9):13. [PubMed] [Google Scholar]
- 9.Tomasini C, Michelerio A. Erosive pustular dermatosis of the scalp: a neutrophilic folliculitis within the spectrum of neutrophilic dermatosis. J Am Acad Dermatol. 2018;25. [DOI] [PubMed] [Google Scholar]
- 10.Yamamoto T, Furuse Y. Erosive pustular dermatosis of the scalp in association with rheumatoid arthritis. Int J Dermatol. 1995;34:148. doi: 10.1111/j.1365-4362.1995.tb03605.x [DOI] [PubMed] [Google Scholar]
- 11.Aoshima M, Ito T, Tokura Y. Erosive pustular dermatosis of the scalp arising concomitantly with elevation of serum matrix metalloproteinase-3 in a patient with rheumatoid arthritis. J Dermatol. 2015;42:540. doi: 10.1111/1346-8138.12815 [DOI] [PubMed] [Google Scholar]
- 12.Watanabe S, Takizawa K, Hashimoto N, et al. Pustular dermatosis of the scalp associated with autoimmune diseases. J Dermatol. 1989;16:383. [DOI] [PubMed] [Google Scholar]
- 13.Mastroianni A, Cota C, Ardigò M, Minutilli E, Berardesca E. Erosive pustular dermatosis of the scalp: a case report and review of the literature. Dermatology. 2005;211:273. doi: 10.1159/000087023 [DOI] [PubMed] [Google Scholar]
- 14.Van Exel CE, English JC 3rd. Erosive pustular dermatosis of the scalp and non scalp. J Am Acad Dermatol. 2007;57:S11–S114. doi: 10.1016/j.jaad.2006.07.009 [DOI] [PubMed] [Google Scholar]
- 15.Uva L, Aphale AN, Kehdy J, Benedetto AV. Erosive pustular dermatosis successfully treated with a novel silicone gel. Int J Dermatol. 2016;55(1):89–91. doi: 10.1111/ijd.13066 [DOI] [PubMed] [Google Scholar]
- 16.Thuraisingam T, Mirmirani P. Erosive pustular dermatosis: a manifestation of immunosenescence a report of 8 cases. Skin Appendage Disord. 2018;4(3):180–186. doi: 10.1159/000484488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilk M, Zelger BG, Hauser U, Hopfl R, Zelger B. Erosive pustular dermatosis of the scalp: reappraisal of an underrecognized entity. J Dtsch Dermatol Ges. 2018;16:15–19. [DOI] [PubMed] [Google Scholar]
- 18.Sechi A, Piraccini BM, Alessandrini A, et al. Post-traumatic erosive dermatosis of the scalp: a hypergranulated variant. Austral J Dermatol. 2019. doi: 10.1111/ajd.13099 [DOI] [PubMed] [Google Scholar]
- 19.Semkova K, Tchernev G, Wollina U. Erosive pustular dermatosis (Chronic atrophic dermatosis of the scalp and extremities). Clin Cosmet Investig Dermatol. 2013;6:177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abedini R, Kamyab Hesari K, Daneshpazhooh M, Ansari MS, Tohidinik HR, Ansari M. Validity of trichoscopy in the diagnosis of primary cicatricial alopecias. Int J Dermatol. 2016;55:1106–1114. doi: 10.1111/ijd.13145 [DOI] [PubMed] [Google Scholar]
- 21.Starace M, Patrizi A, Piraccini BM. Visualisation of hair bulbs through the scalp: a trichoscopic feature of erosive pustular dermatosis of the scalp. Int J Trichol. 2016;8:91. doi: 10.4103/0974-7753.188038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vaccaro M, Barbuzza O, Borgia F, Cannavò SP. Erosive pustular dermatosis of the scalp following topical latanoprost for androgenetic alopecia. Dermatol Ther. 2015;28(2):65–67. doi: 10.1111/dth.12197 [DOI] [PubMed] [Google Scholar]
- 23.Vaccaro M, Guarneri C, Barbuzza O, Guarneri B. Erosive pustular dermatosis of the scalp: an uncommon condition typical of elderly patients. J Am Geriatr Soc. 2008;56(4):761–762. doi: 10.1111/j.1532-5415.2008.01615.x [DOI] [PubMed] [Google Scholar]
- 24.Yang CS, Kuhn H, Cohen LM, Kroumpouzos G. Aminolevulinic acid photodynamic therapy in the treatment of erosive pustular dermatosis of the scalp: a case series. JAMA Dermatol. 2016;152:694–697. doi: 10.1001/jamadermatol.2016.2344 [DOI] [PubMed] [Google Scholar]
- 25.Yeh R, Polcz M, Wong D. Erosive pustular dermatosis of the scalp: an Australian perspective: insights to aid clinical practice. Australasian J Dermatol. 2019. doi: 10.1111/ajd.13042 [DOI] [PubMed] [Google Scholar]