Abstract
Introduction
Electronic consultation (eConsult)—provider-to-provider electronic asynchronous exchanges of patient health information at a distance—is emerging as a potential tool to improve the interface between primary care providers and specialists. Despite growing evidence that eConsult has clinical benefits, it is not widely adopted. We investigated factors influencing the adoption and implementation of eConsult services.
Methods
We applied established methods to guide the review, and the recently published Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for scoping reviews to report our findings. We searched five electronic databases and the grey literature for relevant studies. Two reviewers independently screened titles and full texts to identify studies that reported barriers to and/or facilitators of eConsult (asynchronous (store-and-forward) use of telemedicine to exchange patient health information between two providers (primary and secondary) at a distance using secure infrastructure). We extracted data on study characteristics and key barriers and facilitators were analysed thematically and classified using the Quadruple Aim framework taxonomy. No date or language restrictions were applied.
Results
Among the 2579 publications retrieved, 130 studies met eligibility for the review. We identified and summarised key barriers to and facilitators of eConsult adoption and implementation across four domains: provider, patient, healthcare system and cost. Key barriers were increased workload for providers, privacy concerns and insufficient reimbursement for providers. Main facilitators were remote residence location, timely responses from specialists, utilisation of referral coordinators, addressing medicolegal concerns and incentives for providers to use eConsult.
Conclusion
There are multiple barriers to and facilitators of eConsult adoption across the domains of Quadruple Aim framework. Our findings will inform the development of practice tools to support the wider adoption and scalability of eConsult implementation.
Keywords: health services research, review
Key questions.
What is already known?
Although a growing empirical evidence support the potential positive impact of electronic consultation (eConsult), its adoption and wide scale implementation remains limited.
The barriers to and facilitators of eConsult implementation from a global perspective have not been studied.
What are the new findings?
This work has provided insights into the barriers and facilitators associated with eConsult implementation from the perspective of the healthcare provider, patient, healthcare system and cost.
The key barriers identified included concerns for increased workload, privacy issues and absence of a reimbursement model by providers in some jurisdictions.
The main facilitators identified were remote residence location, timely responses from specialists, integration of non-physician practitioners, circumvention of medicolegal obstacles and provision of incentives for providers to use eConsult.
What do the new findings imply?
The findings are useful for the development of policies towards guiding eConsult implementation across countries and regions.
Introduction
Access to specialist care is associated with improved outcomes, reduced mortality, use of appropriate medications and greater adherence to guidelines.1 2 Conversely, generalist care produces greater value at the population level by achieving a similar quality of care at lower cost.3 4 Therefore, an effective, efficient partnership between the two levels of care would seem important5 and has long been the focus of attention for primary care reforms.3 6 7 Such reforms are especially needed in enhancing healthcare delivery, where referrals to specialist care face increasing pressure due to growing demands and provider shortages.8 9 In a systematic review investigating interventions affecting the nexus between primary and specialist care, interventions aimed at changing the process of care were found to be most effective.10 Within this category, two types of interventions—specialist consultation before referral and electronic referrals—demonstrated the strongest positive effects.10 Electronic consultation (eConsult) is defined as a provider-to-provider asynchronous exchange of patient information using a secure electronic platform.11 Although the use of eConsult has been linked to an increase in access to specialist care and improved communication between providers, it has not been widely implemented across settings.
Designing new interventions that may inadvertently disrupt healthcare delivery is challenging.12 Furthermore, there is a lack of sustained implementation of new programme, especially in health information technology.13 14 Therefore, when designing and implementing a complex health system delivery tool like eConsult, it is imperative to identify the factors that could favour and hinder its wider adoption and scale up.15 However, little evidence exists about these factors and how they influence eConsult adoption and implementation.16 In a systematic review, Vimalananda and colleagues identified implementation studies as one of key deficiencies in the current eConsult literature.15 The aim of this scoping review was to systematically identify barriers to and facilitators of eConsult implementation across the globe. Results will be used to inform policy targeted to those responsible for implementing eConsult programme by using the experiences of early adopters, and highlighting the factors that must be considered and tailored to their local contexts.
The question that we sought to answer was: ‘What is known about the barriers to and facilitators of the wider implementation of electronic consultation to enhance access to specialist care?’ Using preidentified themes and selected published literature on barriers and facilitators as a guide,16 17 we synthesised information on the factors influencing eConsult implementation and categorised these factors at multiple stakeholder levels.
Methods
Study design
We chose to perform a scoping review to answer our research question given the broad nature of the topic and the need to map key concepts and identify gaps in the literature. This is particularly salient when studying a topic such as eConsult, which is a complex intervention in an emerging field18 with working concepts that are just evolving.19 Moreover, a scoping review is appropriate when the literature includes a variety of study designs (quantitative, qualitative and mixed methods).20 21 Therefore, a scoping review was determined to be the optimal methodology to address our study question.22
Our review was guided by the method first described by Arksey and O’Malley23 with modifications based on Levac et al’s recommendations.24 We followed the recently published extension to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses reporting guidelines for scoping reviews developed by Tricco and colleagues.25
Protocol
Details on the methods are published elsewhere.26 In brief, we reported our approach and explained any deviation from the published protocol in the following sections:
Eligibility criteria
Using a priori developed selection criteria,26 we included studies reporting on barriers to and facilitators of eConsult implementation using a common definition of eConsult identified during our preliminary search. eConsult was defined as an asynchronous (store-and-forward) use of telemedicine to exchange patient health information between two providers (primary and secondary) at a distance using secure infrastructure. This definition excludes synchronous methods of telemedicine (eg, video-conferencing) and the use of less secure methods (eg, email). Furthermore, we excluded studies reporting only on image-based eConsult programme (eg, teledermatology) as they are more widely adopted in medical specialties that rely extensively on image-based data.27 All study designs were considered including experimental (randomised controlled trials (RCTs)), observational (quantities, qualitative and mixed methods) and reviews (systematic, non-systematic). We applied no language, source of data or publication date restrictions.
Information sources and search strategy
An experienced information specialist (RF) developed and executed the literature search strategies for the selected databases and other data sources, which were peer-reviewed by a second medical librarian (TL). Studies were identified by conducting comprehensive searches of several bibliographic databases (Ovid MEDLINE, Ovid Embase, Wiley Cochrane Library, CINAHL via EBSCOhost and Ovid PsycINFO) from inception until search date (7 December 2017). We also searched ProQuest Dissertations & Theses Global,28 and included relevant grey literature by searching the Conference Proceedings Citation Index and screening the first five pages (n=100 results in total) from a Google search. Finally, through backward citation chaining29 we reviewed the reference lists of included studies for relevant studies not identified from our initial search until saturation was achieved.
Data items and data abstraction process
Two reviewers (MAO, LB) independently screened all identified citations for potential inclusion. In the initial screening of titles and abstracts, potentially relevant papers were identified separately based on the inclusion and exclusion criteria, the two-screened lists were compiled and then full-text papers were obtained. When agreement on a citation could not be reached between the two reviewers, a third reviewer (AKB) was consulted for resolution. We obtained a kappa statistic of 0.66 (95% CI 0.50 to 0.83) for full-text inclusion. Data were extracted from eligible studies using a data extraction tool previously piloted on five papers. Abstracted data items included study characteristics, study design and key barriers and facilitators at patient, provider and health system levels. We also categorised the design of each eConsult system based on two main approaches identified in the literature: (1) standalone web-based platforms that can be accessed via the internet30 and (2) platforms integrated with existing electronic medical record (EMR) systems.31 All data were extracted into Microsoft Excel V.2016.
Risk of bias assessment or quality appraisal
Following guidance on scoping review conduct, we did not perform a risk of bias assessment or quality appraisal for included articles.21 24 25
Synthesis of results
We used the four domains of the Quadruple Aim evaluation framework to synthesise and report identified barriers and facilitators into tables and figures.32 33 This framework for optimising health system performance has been used previously to evaluate eConsult; however, this is the first time it has been used to evaluate eConsult implementation.32 34 The four components of the Quadruple Aim framework—provider, patient, population health and cost—are intended to be pursued simultaneously to improve healthcare. We adopted this framework in our review with a few modifications. We subdivided the provider perspective into the primary care provider (PCPs) and specialist perspectives; this division was helpful in our evaluation, as different factors influence the two providers’ use of health information technology.35 Also, we substituted healthcare system for population health, which is less clearly defined in the eConsult literature.
Two reviewers independently evaluated the included studies for any determinants of eConsult implementation. We analysed and presented the data qualitatively using both deductive (preidentified themes) and inductive (newly identified themes) approaches.36 We coded textual data from included papers individually using a broad-based coding scheme (MO) and documented common themes across papers textually (thematic analysis) and numerically (descriptive frequency). We used selected quotes—as a first (participants own words) and second (researchers’ interpretations) order constructs37—from the literature in reporting the results and we summarised all identified barriers and facilitators in the online supplementary file.
bmjgh-2019-001629supp001.pdf (520.1KB, pdf)
Consultation exercise
Prior to commencing the review, we conducted a focus group study to capture the perceived barriers to and facilitators of eConsult by patients, policy makers and PCPs.17 We used emerging themes from the focus group study to guide the analysis of this scoping review of the literature. Furthermore, we sent the results of this review to eConsult users and decision makers for feedback. This review was conducted from September 2017 to December 2018.
Patient and public involvement statement
Patients and the public were not involved at this stage of the project.
Results
Study selection
A total of 2579 unique citations were identified and assessed for eligibility. Of these, 130 (123 primary studies and 7 reviews) met the inclusion criteria (figure 1).
Figure 1.
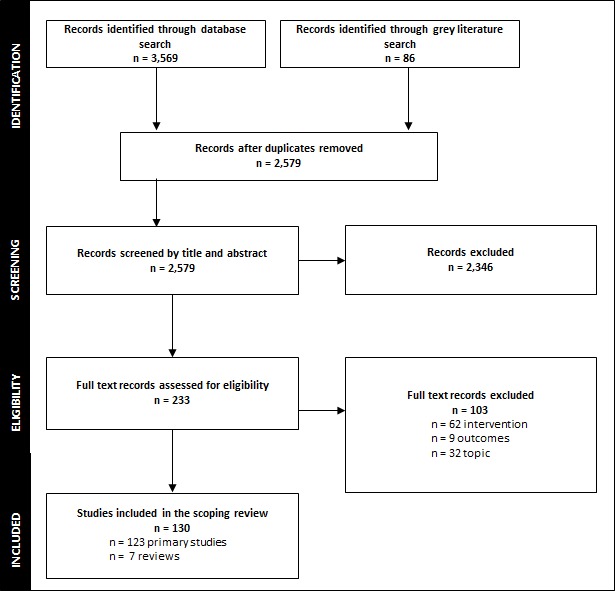
Flow chart for study search and decision process. n, number of studies.
Study characteristics
Most identified studies were published in the last 10 years (online supplementary eFigure 1) and included eConsult programme from eight countries: Finland, Ireland, Canada, Spain, Brazil, the UK, The Netherlands and USA (online supplementary eFigure 1). Observational designs were commonly used to report eConsult programme, and these included surveys,11 38–50 focus groups/interviews16 17 48 51–56 and mixed methods.57–59 We also identified three RCTs,60–62 three systematic reviews15 63 64 and four narrative reviews.65–68 Characteristics of the included studies summarised in online supplementary eTable 1.
eConsult programme
The 123 primary studies included in our review covered 30 unique eConsult programme: 18 based in the USA, 3 in the UK, and 2 in Canada, Brazil, Finland, Spain, and 1 programme in the Netherlands and Ireland (online supplementary eTable 1). The reported eConsult platforms were mainly EMR-based (n=10) and web-based (n=13) systems. Although we identified two studies reporting a process similar to eConsult in Finland in the early 1990s, the contemporary eConsult design was implemented in the early 2000s and was further developed in the 2010s in large-scale programme in Ontario and the USA. In addition, we identified three non-civilian eConsult programmes in the USA that provide access to specialist care for military personnel and their families.47 69–72
eConsult terminology
In the reviewed studies, eConsult/e-Consult was the term most commonly used to describe this use of telemedicine (online supplementary eFigure 2). eConsult/e-Consult first appeared in the literature as ‘ENT consult’ in 2003 in an article by Baum et al 73; in 2009, Stoves et al 74 used the term ‘electronic consultation’ and Angstman et al 75 used ‘e-Consult’, which has become the standard term. Other less frequent terms identified include teleconsultation, asynchronous care and electronic referral/eReferral (online supplementary eFigure 2).
Barriers to eConsult
Identified barriers to eConsult are presented in table 1. We also show the distribution of these factors among the Quadruple Aim taxonomy domains of providers (figure 2), patients (figure 3), the healthcare system (figure 4) and costs (figure 5). Further details on identified barriers can be accessed through the online supplementary file.
Table 1.
Barriers to eConsult implementation using the quadruple aim framework
| Provider perspective | Patient perspective | Healthcare system | Cost | |
| PCP | Specialist | |||
| Increased workload and workflow disruptions* ✗ It was a lot easier and quicker for me to write a consultation on…paper…Now I’m having to go through a longer process with a few more hurdles in it 54 |
Increased workload * ✗ Specialists also experienced greater workload in the form of pre-consultative exchange and virtual management, which also served as a barrier to implementation 16 |
Some patients preference to see specialists face-to-face ✗ It’s important to see the specialist to feel more secure.59 |
eConsult system design challenges* ✗ To find an application able to integrate seamlessly with diverse systems is often challenging 82 |
Insufficient remuneration for providers* ✗ A key barrier to widespread adoption of preconsultation exchange is the development of reimbursement models 77 |
| Technical challenges to use eConsult* ✗ When I added a follow up question it never seems to go through and the consult disappeared. I had to request a new consult with my follow up question.76 |
Concerns with liability ✗ Another challenge unique to electronic consultation and integrated eCR [eConsult] systems but not referral systems was specialist concern about liability 78 |
Perceived decrease in accessibility to specialist care* ✗ And if I feel like my doctor is brushing off that information, is not communicating other symptoms 48 |
Lack of resources* ✗ Health systems or practices initiating telehealth programs need to provide a base investment in the technology and then provide an ongoing and available infrastructure 67 |
Provider payment structure (salaried physicians vs fee-for-service models) ✗ And might only be cost-effective in a non -fee-for-service model such as one found in the VHA [Veterans Health Administration] 83 |
| Loss of specialist contact ✗ PCP concerns included…unable to select the specific consultant 15 |
Loss of patient contact ✗ A minority of them prefer not to use VCs [virtual consults] because of…discomfort with an impersonal process 79 |
Concerns about safety/ appropriateness of eConsult ✗ I asked someone [a specialist] and he told me to give you this. If something happens to you, it’s not my responsibility because the other doctor prescribed it 48 |
Variation in licensure requirements across provinces/states ✗ In fact, licensure requirements also differ from state to state, and this introduces a significant possible variation in practice 67 |
|
| Unfamiliarity with using eConsult service ✗ The preparation…what kinds of tests have to be done.53 |
Challenges with the quality/content of eConsult ✗ Referrals that lack a clear consultative question and relevant clinical data often render a specialist unable to make a clear diagnosis or a fully developed management plan 80 |
Privacy concerns* ✗ Concerns over privacy remain a barrier to the adoption of electronic platforms or innovations among health care providers 59 |
||
| Insufficient remuneration to use eConsult ✗ Lack of reimbursement for PCP to submit the consultation request electronically 44 |
Challenges with the use of technology ✗ However, until a more slim-line IT system is developed reducing the number of steps involved in completing an eC (electronic consultation), …it appears to be beneficial for all parties except secondary care 81 |
|||
| Challenges related to patient follow-up ✗ Concern about how and when to communicate with patients regarding a consultant’s recommendations 55 |
Insufficient remuneration to use eConsult ✗ Concerns included… the need for adequate protected time and credit 15 |
|||
| Receiving timely responses from specialists ✗ PCPs were not satisfied with the depth of the answer that was provided 76 |
||||
✗Selected quotes supporting the theme from the literature.
*Preidentified theme (deductive).
PCP, primary care provider.
Figure 2.
Provider perspective on barriers to and facilitators of eConsult implementation. n, number of studies; PCP, primary care provider.
Figure 3.
Patient perspective on barriers to and facilitators of eConsult implementation. n, number of studies.
Figure 4.

Healthcare system-related barriers to and facilitators of eConsult implementation. n, number of studies.
Figure 5.
Cost-related barriers to and facilitators of eConsult implementation. n, number of studies.
Providers’ perspective on barriers
We identified a number of barriers related to PCPs’ adoption of eConsult, including behaviour change and the resultant increased workload and workflow disruptions, technical challenges, loss of ‘immediate contact’ and/or access to specific specialists, unfamiliarity with using eConsult services, lack of financial incentives to use eConsult, challenges with patient follow-up and delayed responses from specialists (figure 2).
✗“Resistance to change, particularly to changes in PCP work flow, emerged prominently during our interviews”16 (p. 6).
✗“It was a lot easier and quicker for me to write a consultation on…paper…Now I’m having to go through a longer process with a few more hurdles in it. Just mechanically if we have any problems with the computer…”54 (p. 1341).
✗“When I added a follow up question it never seems to go through and the consult disappeared. I had to request a new consult with my follow up question”76 (p. 401).
✗“PCP concerns included…unable to select the specific consultant”15 (p. 327).
✗“The preparation…what kinds of tests have to be done”53 (p. 9).
✗“Lack of reimbursement for PCP to submit the consultation request electronically”44 (p. 4).
✗“The shortcomings of referral systems with exchanges between PCPs and consultants include… loss of patients to follow up”77 (p. 174).
✗“PCPs were not satisfied with the depth of the answer that was provided. Some providers were looking for more detail, whereas others felt their questions were not adequately addressed”76 (p. 398).
From the specialists’ perspective, key barriers included increased workload, concerns with liability, loss of patient contact, challenges with the quality/content of eConsult, use of technology and insufficient remuneration for specialists in some jurisdictions (figure 2).
✗ “Specialists also experienced greater workload in the form of pre-consultative exchange and virtual management, which also served as a barrier to implementation”16 (p. 6).
✗“Another challenge unique to electronic consultation and integrated eCR [eConsult] systems but not referral systems was specialist concern about liability”78 (p. 6).
✗“A minority of them prefer not to use VCs [virtual consults] because of…discomfort with an impersonal process”79 (p. 17).
✗ “Referrals that lack a clear consultative question and relevant clinical data often render a specialist unable to make a clear diagnosis or a fully developed management plan”80 (p. 519).
✗“However, until a more slim-line IT system is developed reducing the number of steps involved in completing an eC [electronic consultation]…it appears to be beneficial for all parties except secondary care”81 (p. A239).
Patients’ perspective on barriers
For patients, more facilitators for eConsult than barriers were identified. We identified three central themes: Some patient’s preference for face-to-face contact with specialists, perceptions that eConsult systematically limits accessibility to specialist care, and concerns about the safety and/or appropriateness of eConsult (figure 3).
✗“It’s important to see the specialist to feel more secure”59 (p. 327).
✗“And if I feel like my doctor is brushing off that information, is not communicating other symptoms…you know, these are the only four symptoms that matter and so I’m just going to give those to the specialist, at that point I might feel like wow, there’s more information that’s not getting through”48 (pp. 10–11).
✗“I asked someone [a specialist] and he told me to give you this. If something happens to you, it’s not my responsibility because the other doctor prescribed it”48 (p. 9).
Healthcare system-related barriers
Implementation barriers related to the healthcare system included variation in licensure requirements across jurisdictions, privacy concerns and provision of requisite infrastructure and resources (figure 4).
✗“To find an application able to integrate seamlessly with diverse systems is often challenging”82 (p. 984).
✗“Health systems or practices initiating telehealth programs need to provide a base investment in the technology and then provide an ongoing and available infrastructure”67 (p. 18).
✗“In fact, licensure requirements also differ from state to state, and this introduces a significant possible variation in practice”67 (p. 19).
✗“Concerns over privacy remain a barrier to the adoption of electronic platforms or innovations among health care providers”59 (p. 3).
Cost-related barriers
Cost-related barriers included a lack of reimbursement for providers in some jurisdictions, and the absence of provider-specific payment structures (salaried physicians vs fee-for-service models) (figure 5).
✗“A key barrier to widespread adoption of preconsultation exchange is the development of reimbursement models”77 (p. 174).
✗“might only be cost-effective in a non fee-for-service model such as one found in the VHA (Veterans Health Administration)”83 (p. e244).
Facilitators to eConsult
Key facilitators of eConsult implementation are summarised in table 2. We also show the distribution of these factors among the four domains of the Quadruple Aim taxonomy: providers (figure 2), patients (figure 3), healthcare system (figure 4) and costs (figure 5). Further details on identified facilitators can be accessed via the online supplementary file.
Table 2.
Facilitators to eConsult implementation using the quadruple aim framework
| Provider perspective | Patient perspective | Healthcare system | Cost | |
| PCP | Specialist | |||
| PCPs receiving timely response from specialist* ✓ A very helpful service, giving timely help and input to the front-line generalist.41 |
Improved communication with PCPs ✓ I think it helps in the interaction with the health care provider. They tell you what information they have, you evaluate it and then if you need further information, you tell them “This is what you need.” 30 |
Remote residence location* ✓ I live in a more remote location…A lot of the specialists probably aren’t going to be here, so [eConsult can] save me a trip to Ottawa.52 |
Increase provider knowledge capacity and confidence ✓ This information could be used to inform the planning of continuing medical education (CME) and professional development events for PCPs. 38 |
Developing payment models and incentives for providers to use eConsult ✓ Its success at San Francisco General Hospital depended on …and on financial incentives that were not completely wedded to clinic productivity.66 |
| Building capacity and knowledge* ✓ Thank you to Dr. X for the excellent advice. This will also help me manage patients with similar profiles in the future.76 |
Educational opportunities* ✓ (eConsult) also provides education. If you take the time to write out the thinking, then they don’t have to ask you the question again because you just taught them. So it helps them be a better physician and it also will cut down on the questions.86 |
Timely access to specialist care ✓ If I wanted to see them [the specialist] face-to-face it would have taken possibly months.52 |
eConsult platform choice ✓ Innovators may be tempted to develop a service as an extension of a specific EMR program or vendor, since harnessing an existing platform can reduce the upfront time and costs associated with development. However, greater flexibility will support wider adoption, allowing the service to reach a broader segment of the population. 68 |
Potential cost savings for insurance payers to use eConsult ✓ Referral to specialty departments dramatically affects the annual cost of medical care for a group of insured patients. 75 |
| Improved referral efficiency* ✓ Satisfaction with the e-consult was high among nephrologists; in the majority of cases thought that the e-consult was efficient.87 |
Potential cost savings ✓ From a patient perspective, fewer office visits translates to less time taken off work and reduced transportation costs.88 |
eConsult ease of use ✓ The workflow of the e-consultation system must fit as seamlessly as possible into the physician’s usual workflow to ensure participation. It is important to minimize system usage time.82 |
Potential cost savings for society ✓ Cost savings for eConsult from the societal perspective attributable to patient avoided costs, as patients whose PCPs had originally considered a referral but ultimately chose not to refer them avoided the travel costs and lost wages/ productivity.91 |
|
| Reduced time commitments required for eConsult ✓ Reassuringly, the average self-reported time it took specialists to complete an eConsult was 11.2 min, which is shorter than it would take to complete an in-person consult.107 |
Acceptance of eConsult ✓ Acceptance is vital to the success of any healthcare innovation, and patients’ perspectives on new and innovative services must be thoroughly established. 68 |
Improved access to specialist care* ✓ The benefits include improved access to specialty care for those practicing in remote communities.67 |
Potential cost savings for the healthcare system ✓ Please continue with e-consult services as it will save on health [dollars] in the long run and will assist in improvement of patient care.76 |
|
| Ability to expedite face-to-face consultation if needed ✓ If we have any reservations or the patient has any reservations, we see them(face-to-face).53 |
Use of case manager to triage consultations ✓ Use of referral case managers to improve efficiency.51 |
|||
| Security measures ✓ We reviewed our e-consult process with risk management lawyers and we were able to reassure providers that this system would not place them at undue legal risk.89 |
||||
| Improved quality of care/ ‘safety net’ effect* ✓ [In] 4% of cases PCPs were not planning on sending the patient for a traditional face-to-face referral… however, the eConsultant recommended one due to the potential high-acuity nature or complexity of the problem. 38 |
||||
| Organisational commitment to implementation ✓Obtaining buy-in from health system leadership is essential to lay the necessary ground work. 90 |
||||
| Clarifying providers’ duty of care/role ✓ eConsults from a medical legal perspective are considered along the same lines as a “curbside consult” in that the specialist provider does assume a duty of care once the case is reviewed. 38 |
||||
| End user engagement/ consultation ✓ Disseminate the benefits. (using actual data) of E-Consults for patients and for workflow to participating providers. 56 |
||||
| Providing ongoing support/training ✓In contrast, a high-volume site participant noted that training was crucial. 58 |
||||
| Piloting eConsult ✓I think the reason why they’ve jumped onto the bandwagon is because they probably saw how efficient it was with GI.54 |
||||
✓Selected quotes supporting the theme from the literature.
*Preidentified theme (deductive).
PCP, primary care provider.
Providers’ perspective on facilitators
From PCPs’ perspective, facilitators included efficiency (eg, timely responses from specialists) and enhanced capacity for chronic disease care by increasing access to new knowledge and resources (figure 2).
✓“A very helpful service, giving timely help and input to the front-line generalist”41 (p. 354).
✓“My patient was surprised about the technology and how quickly a response was obtained”84 (p. 1036).
✓“Thank you to Dr. X for the excellent advice. This will also help me manage patients with similar profiles in the future”76 (p. 400).
✓“Identifying the most common questions and content being asked via the eConsult service will allow for more informed continuing medical education programme for PCPs”85 (p. 1).
From specialists’ perspective, the use of eConsult facilitated communication with PCPs, provided educational opportunities for PCPs and improved referral efficiency. Other facilitators included reduced time commitments from specialists, and the ability to expedite face-to-face consultation, if needed (figure 2).
✓“I think it helps in the interaction with the healthcare provider. They tell you what information they have, you evaluate it and then if you need further information, you tell them ‘This is what you need”30 (p. 9).
✓“(eConsult) also provides education. If you take the time to write out the thinking, then they don’t have to ask you the question again because you just taught them. So it helps them be a better physician and it also will cut down on the questions”86 (p. 5).
✓“In the majority of cases, nephrologists and PCPs (99% and 96%, respectively) thought that the e-consult was efficient”87 (p. 821).
✓“It’s always quicker to read someone’s findings rather than to go ahead and do the full exam yourself. I probably would spend anywhere from 30 to 45 min with a new patient. What I reported as having spent on e-consultation was much less than that. Nothing more than 20 min”30 (p. e5).
✓“If we have any reservations or the patient has any reservations, we see them [face-to face]”53 (p. 10).
Patients’ perspective on facilitators
The main facilitator from patients’ perspective was remote residence location; other factors included timely access to specialist advice, cost savings, and acceptance of eConsult as a convenient model of care (figure 3).
✓“I live in a more remote location…A lot of the specialists probably aren’t going to be here, so (eConsult can) save me a trip to Ottawa”52 (p. 95).
✓“From a patient perspective, fewer office visits translates to less time taken off work and reduced transportation costs”88 (p. 1149).
✓“The service allowed a significant proportion of patients to avoid traditional consultations leading to the potential of cost savings”85 (p. 42).
✓“Acceptance is vital to the success of any healthcare innovation, and patients’ perspectives on new and innovative services must be thoroughly established”59 (p. 9).
Healthcare system-related facilitators
Facilitators identified at the healthcare system level include increased efficiency (ie, enhanced access and rapid triage of patients) for both referring PCPs and specialists, opportunities to use other care providers (eg, case managers) and medicolegal elements (figure 4).
✓“The benefits include improved access to specialty care for those practicing in remote communities”67 (p. 20).
✓“Use of referral case managers to improve efficiency”51 (p. 78).
✓“We reviewed our e-consult process with risk management lawyers and we were able to reassure providers that this system would not place them at undue legal risk”89 (p. 554).
✓“(In) 4% of cases PCPs were not planning on sending the patient for a traditional face-to-face referral…however, the eConsultant recommended one due to the potential high-acuity nature or complexity of the problem”38 (p. 425).
✓“Obtaining buy-in from health system leadership is essential to lay the necessary ground work”90 (p. 387).
✓“eConsults from a medical legal perspective are considered along the same lines as a ‘curbside consult’ in that the specialist provider does assume a duty of care once the case is reviewed”38 (p. 422).
✓“Disseminate the benefits (using actual data) of E-Consults for patients and for workflow to participating providers”56 (p. S437).
✓“In contrast, a high-volume site participant noted that training was crucial”58 (p. 5)
✓“I think the reason why they’ve jumped onto the bandwagon is because they probably saw how efficient it was with GI”54 (p. 1343).
Cost-related facilitators
The primary cost-related facilitator of eConsult implementation was the development of payment models and incentives for providers to use the system. Other facilitators include potential cost savings for society, insurance payers and the healthcare system (figure 5).
✓“Its success at San Francisco General Hospital depended on…financial incentives that were not completely wedded to clinic productivity”66 (p. 971).
✓“Referral to specialty departments dramatically affects the annual cost of medical care for a group of insured patients”75 (p. 256).
✓“Cost savings for eConsult from the societal perspective attributable to patient avoided costs, as patients whose PCPs had originally considered a referral but ultimately chose not to refer them avoided the travel costs and lost wages/productivity”91 (p. 5).
✓“Please continue with e-consult services as it will save on health (dollars) in the long run and will assist in improvement of patient care”76 (p. 399).
Discussion
This scoping review reveals insights into the barriers and facilitators associated with eConsult adoption as reported in the current literature. We leveraged the Quadruple Aim framework taxonomy33 to categorise findings into the four domains of provider, patient, healthcare system and cost. The key barriers identified were providers’ perceptions of increased workload, privacy concerns and the absence of a reimbursement model for providers in some jurisdictions. Key facilitators were remote residence location, timely responses from specialists, integration of non-physician practitioners (eg, case managers, referral coordinators, nurse practitioners), circumvention of medicolegal obstacles and provision of incentives for providers to use eConsult (eg, fee-for-service or other funding models).
To our knowledge, this is the first scoping review aimed at identifying barriers and facilitators associated with eConsult adoption and implementation at a multinational level. A previous study by Tuot and colleagues identified a number of facilitators, including engaged leadership, provider incentives, user-friendly technology and integration with EMRs, as well as barriers, including provider resistance, lack of reimbursement, liability concerns and lack of integration with EMRs.16 They examined a select number of organisations in the USA that had recently implemented eConsult.
From the patient’s perspective, surprisingly we identified more facilitators for eConsult than barriers. Few studies directly evaluated patient’s perspectives. In one study,89 it was reported that over 90% of patients surveyed were highly satisfied with their eConsult experiences, and in another study the majority of patients (86.6%) stated that eConsult was “useful in their situation.”52 In other studies, PCPs’ perceptions were used as a proxy to evaluate patient satisfaction. In several studies, the majority of providers rated eConsult as ‘very good’ to ‘excellent’ service for their patients.11 39 41 43 76 92 93 The perspective of PCPs is also important, as one study of patient engagement in eConsult found that most patients expressed minimal desire to directly engage with eConsult and preferred their PCPs to take on that role.48
Concerns about increased workload are key barriers from the perspective of care providers. The apparent benefits of using eConsult may not be realised if it creates an additional burden on clinicians. However, several studies showed specialists’ self-reported time spent responding to e-consult requests was less than 10 min on average, much less than a face-to-face consult which e-consult often replaces the need for.38 39 42 93–96 For PCPs, the time commitment is less clear; one study reported that a consultation takes an average of 10 min to be completed by both PCPs and specialists.97 PCPs’ involvement with eConsult includes many tasks beyond initiating and responding to consultation, such as conducting extra tests and communicating consultation outcomes to patients. Findings that quantify PCPs’ workload in relation to eConsult will be useful in engaging PCPs. Similar to patients, some of providers’ barriers can be addressed through targeted interventions such as academic detailing, audit and feedback,98 and by soliciting input from PCPs82 when eConsult tools are in the development stage. Using clinician champions to advocate for eConsult among their peers also is an effective way to overcome barriers to use by providers.82
Recent studies published after the completion of our review are consistent with our findings.99 100 In a qualitative study evaluating 40 PCPs’ perspectives on eConsult in the USA, the authors reported themes aligned with our findings.100 During interviews, PCPs identified several facilitators, including timely specialist input and the ability to broaden their scope of practice, and a barrier in the form of increased workload as more specialist shift care to PCPs.100 Interestingly, the authors described how this barrier differs between discretionary systems (eConsult as an add-on service to traditional referral pathways) and mandatory systems (all referrals go through eConsult). They found that compared with mandatory eConsult, discretionary eConsult is associated with more positive perceptions with regard to workload, but is less used by PCPs.100 Based on their findings, the authors developed a tool to guide decision-making for programme seeking to implement eConsult.100 The findings of our scoping review can be used to develop similar tools to facilitate the adoption of eConsult beyond the USA.
One of our key findings is that none of the identified facilitators were unique to specific programme, except for the platform choice and provider reimbursement model. For example, the Veterans Affairs eConsult101 102 programme reported a shared EMR platform as a prerequisite for successful eConsult implementation, while the Ontario eConsult advocated for a standalone web-based system.64 82 While both approaches are acceptable, other factors (eg, patient and provider perceptions of eConsult and the provision of incentives to use eConsult) influenced implementation. It also appears that the existence of a compensation model for providers time rather than a specific payment structure, such as fee-for-service or salary, is a key facilitator for eConsult adoption.83
Of note, some of the factors identified were more common with the implementation of other health information technologies. For instance, a systematic review on EMR identified privacy and security concerns, ease of use, costs and workload as the most frequently reported factors influencing implementation of EMR.103 This highlights the overlap across healthcare delivery technology platforms. Thus, a more in-depth exploration of these interrelated factors and their impact on the use of health information technology is warranted.
The use of eConsult in clinical practice is a relatively recent development and our findings provide new information to decision makers to guide implementation across a spectrum covering perspectives from several stakeholders that included patients, care providers and relevant costs. We have identified significant heterogeneity between studies evaluating eConsult implementation from various settings; the recently published framework proposed by Tuot and colleagues19 is useful for the design of future studies using the recommended approach to allow for comparison of data in a more meaningful way.
The implications of our findings are that the design of eConsult systems requires careful consideration of factors that hinder or favour implementation. However, it is important to recognise the driving force and goals of eConsult implementation in priority setting. For instance, if eConsult is adopted at the healthcare system level to improve access to specialist care in response to patient’s frustration, then the highest priority might be to address specialist providers to get their buy-in to the programme. Alternatively, if eConsult is being driven by specialists who want to increase access to care without having their clinics overwhelmed, then perhaps the barriers and facilitators at the PCPs level are where to start. Ideally, champions at all stakeholder levels would drive service implementation and success.
We used a rigorous and transparent method to review the literature but the findings are very broad. Scoping reviews are broad by nature, with limited or no focus on a specific research question and/or hypothesis; typically, the goal is to address broad and complex questions as our study.104 Another common limitation with this kind of reviews is the lack of comprehensiveness in the search for relevant literature. We mitigated this by conducting the search in a stepwise fashion following the recommended guidelines, using several databases, searching the grey literature and manually searching the reference lists of included studies.
Despite these efforts, we could not find any study in low-income and middle-income countries that met our inclusion criteria. We recognised the efforts of philanthropic non-governmental organisations such as Médecins Sans Frontières providing telemedicine service in developing countries with several challenges such as technical (eg, internet connectivity), operational (eg, high turnover rates of field users) and cultural (eg, trust between health professionals from different countries) reported.105 Addressing eConsult implementation factors in low resource settings, where a relatively lower prevalence of specialists practice, is of growing importance and might make eConsult especially attractive. Further limitations of this work include the limited number of published works on health economic evaluations on the development and implementation of eConsult. This is a relatively new and emerging field and a subject of several ongoing studies across multiple settings.91 93 106
Conclusions
Even though it is well documented that eConsult improves access to care, particularly by reducing wait times, adoption rates remain low, even in high-income countries with well-established health systems (eHealth infrastructure). The design of eConsult systems requires a careful consideration of all factors that hinder or favour implementation. In this study, we identified common barriers to and facilitators of eConsult implementation to improve access to specialist care. Our findings provide new information to guide the implementation and scale up eConsult programme worldwide, regardless of setting.
Acknowledgments
Authors like to thank Tara Landry (Medical Librarian, Montreal General Hospital Library, McGill University) for her help with the search strategy.
Footnotes
Handling editor: Soumyadeep Bhaumik
Contributors: The authors followed the International Committee of Medical Journal Editors authorship guidelines. AKB and MAO had the original idea for this study. MAO and AKB wrote the first draft of the manuscript. All authors contributed to the study development and reviewed the manuscript for intellectual content. All authors approved the final submitted version of the manuscript.
Funding: This work was funded by Northern Alberta Renal Program/AMGEN Inc Supported Care Innovation Grant and the Interdisciplinary Chronic Disease Collaboration (ICDC). The ICDC is funded through an Alberta Innovates Collaborative Research & Innovation Opportunity Team Grant. It was also supported by the Alberta Strategy for Patient-Oriented Research (SPOR) SUPPORT Unit Knowledge Translation Platform, which is funded by Alberta Innovates and the Canadian Institutes of Health Research. BB has been supported by the Kidney Health Translational Research Chair of the Division of Nephrology, Department of Medicine, at the Faculty of Medicine and Dentistry, University of Alberta.
Disclaimer: The authors were responsible for data management, analysis and interpretation, as well as manuscript preparation, review and approval, and the decision to submit the manuscript for publication. The funder has no role in these activities.
Competing interests: No, there are no competing interests for any author.
Patient consent for publication: Not required.
Ethics: Approval by a research ethics board was not required as only published and publicly available data with no identifiable patient records were reviewed.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Dr Osman and Dr Bello had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- 1. Jong P, Gong Y, Liu PP, et al. . Care and outcomes of patients newly hospitalized for heart failure in the community treated by cardiologists compared with other specialists. Circulation 2003;108:184–91. 10.1161/01.CIR.0000080290.39027.48 [DOI] [PubMed] [Google Scholar]
- 2. Jungers P, Massy ZA, Nguyen‐Khoa T, et al. . Longer duration of predialysis nephrological care is associated with improved long‐term survival of dialysis patients. Nephrol Dial Transplant 2001;16:2357–64. 10.1093/ndt/16.12.2357 [DOI] [PubMed] [Google Scholar]
- 3. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q 2005;83:457–502. 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Harrold LR, Field TS, Gurwitz JH. Knowledge, patterns of care, and outcomes of care for generalists and specialists. J Gen Intern Med 1999;14:499–511. 10.1046/j.1525-1497.1999.08168.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Smetana GW, Landon BE, Bindman AB, et al. . A comparison of outcomes resulting from generalist vs specialist care for a single discrete medical condition: a systematic review and methodologic critique. Arch Intern Med 2007;167:10–20. 10.1001/archinte.167.1.10 [DOI] [PubMed] [Google Scholar]
- 6. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA 2002;288:1775–9. 10.1001/jama.288.14.1775 [DOI] [PubMed] [Google Scholar]
- 7. van Weel C, Carelli F, Gerada C. Reforming primary care: innovation or destruction? Br J Gen Pract 2012;62:43–4. 10.3399/bjgp12X616463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Information CIfH How Canada compares: results from the Commonwealth fund 2015 international health policy survey of older adults. Ottawa, ON: CIHI, 2016. [Google Scholar]
- 9. Martin D, Miller AP, Quesnel-Vallée A, et al. . Canada's universal health-care system: achieving its potential. The Lancet 2018;391:1718–35. 10.1016/S0140-6736(18)30181-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Blank L, Baxter S, Woods HB, et al. . Referral interventions from primary to specialist care: a systematic review of international evidence. Br J Gen Pract 2014;64:e765–74. 10.3399/bjgp14X682837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemed J E Health 2013;19:733–8. 10.1089/tmj.2013.0007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Campbell NC, Murray E, Darbyshire J, et al. . Designing and evaluating complex interventions to improve health care. BMJ 2007;334:455–9. 10.1136/bmj.39108.379965.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Cresswell K, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: an interpretative review. Int J Med Inform 2013;82:e73–86. 10.1016/j.ijmedinf.2012.10.007 [DOI] [PubMed] [Google Scholar]
- 14. Greenhalgh T, Shaw S, Wherton J, et al. . Real-World implementation of video outpatient consultations at macro, meso, and micro levels: mixed-method study. J Med Internet Res 2018;20:e150 10.2196/jmir.9897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vimalananda VG, Gupte G, Seraj SM, et al. . Electronic consultations (e-consults) to improve access to specialty care: a systematic review and narrative synthesis. J Telemed Telecare 2015;21:323–30. 10.1177/1357633X15582108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Tuot DS, Leeds K, Murphy EJ, et al. . Facilitators and barriers to implementing electronic referral and/or consultation systems: a qualitative study of 16 health organizations. BMC Health Serv Res 2015;15:568 10.1186/s12913-015-1233-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bello AK, Molzahn AE, Girard LP, et al. . Patient and provider perspectives on the design and implementation of an electronic consultation system for kidney care delivery in Canada: a focus group study. BMJ Open 2017;7:e014784 10.1136/bmjopen-2016-014784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Anderson S, Allen P, Peckham S, et al. . Asking the right questions: Scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res Policy Syst 2008;6 10.1186/1478-4505-6-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tuot DS, Liddy C, Vimalananda VG, et al. . Evaluating diverse electronic consultation programs with a common framework. BMC Health Serv Res 2018;18:814 10.1186/s12913-018-3626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Brien SE, Lorenzetti DL, Lewis S, et al. . Overview of a formal scoping review on health system report cards. Implementation Sci 2010;5 10.1186/1748-5908-5-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Peters MDJ, Godfrey CM, Khalil H, et al. . Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc 2015;13:141–6. 10.1097/XEB.0000000000000050 [DOI] [PubMed] [Google Scholar]
- 22. Chang S, Reviews S. Scoping reviews and systematic reviews: is it an either/or question? Ann Intern Med 2018;169:502 10.7326/M18-2205 [DOI] [PubMed] [Google Scholar]
- 23. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 24. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Tricco AC, Lillie E, Zarin W, et al. . PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 26. Osman MA, Schick-Makaroff K, Thompson S, et al. . Barriers and facilitators for implementation of electronic consultations (eConsult) to enhance specialist access to care: a scoping review protocol. BMJ Open 2018;8:e022733 10.1136/bmjopen-2018-022733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wilson LS, Maeder AJ. Recent directions in telemedicine: review of trends in research and practice. Healthc Inform Res 2015;21:213–22. 10.4258/hir.2015.21.4.213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. ProQuest Dissertations & Theses Global Theses database. Ann Arbor, Michigan: ProqQuest. Available: https://www.proquest.com/products-services/pqdtglobal.html [Accessed May 7th 2018].
- 29. Athukorala K, Hoggan E, Lehtiö A, et al. . Information-seeking behaviors of computer scientists: challenges for electronic literature search tools. Proc Am Soc Info Sci Tech 2013;50:1–11. 10.1002/meet.14505001041 [DOI] [Google Scholar]
- 30. Liddy C, Rowan MS, Afkham A, et al. . Building access to specialist care through e-consultation. Open Med 2013;7:e1–8. [PMC free article] [PubMed] [Google Scholar]
- 31. Zuchowski JL, Rose DE, Hamilton AB, et al. . Challenges in referral communication between vha primary care and specialty care. J Gen Intern Med 2015;30:305–11. 10.1007/s11606-014-3100-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Liddy C, Drosinis P, Keely E. Electronic consultation systems: worldwide prevalence and their impact on patient care-a systematic review. Fam Pract 2016;33:274–85. 10.1093/fampra/cmw024 [DOI] [PubMed] [Google Scholar]
- 33. Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med 2014;12:573–6. 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Young MJ, Pham J. Improving the electronic nexus between generalists and specialists: a public health imperative? Paper presented at: Healthc, 2016. [DOI] [PubMed] [Google Scholar]
- 35. Redd TK, Doberne JW, Lattin D, et al. . Variability in electronic health record usage and perceptions among specialty vs. primary care physicians. Paper presented at: AMIA Annu Symp Proc, 2015. [PMC free article] [PubMed] [Google Scholar]
- 36. Elo S, Kyngäs H. The qualitative content analysis process. J Adv Nurs 2008;62:107–15. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- 37. Atkins S, Lewin S, Smith H, et al. . Conducting a meta-ethnography of qualitative literature: lessons learnt. BMC Med Res Methodol 2008;8:21 10.1186/1471-2288-8-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Fogel A, Khamisa K, Afkham A, et al. . Ask the eConsultant: improving access to haematology expertise using an asynchronous eConsult system. J Telemed Telecare 2017;23:421–7. 10.1177/1357633X16644095 [DOI] [PubMed] [Google Scholar]
- 39. Johnston DL, Murto K, Kurzawa J, et al. . Use of electronic consultation system to improve access to care in pediatric Hematology/Oncology. J Pediatr Hematol Oncol 2017;39:e367–9. 10.1097/MPH.0000000000000833 [DOI] [PubMed] [Google Scholar]
- 40. Johnston D, Murto K, Kurzawa J, et al. . Use of electronic consultation system to improve access to care in paediatric hematology/oncology. Pediatr Blood Cancer 2017;64:S27. [DOI] [PubMed] [Google Scholar]
- 41. Kohlert S, Murphy P, Tse D, et al. . Improving access to otolaryngology-head and neck surgery expert advice through eConsultations. Laryngoscope 2017;2:2. [DOI] [PubMed] [Google Scholar]
- 42. Liddy C, Drosinis P, Fogel A, et al. . Prevention of delayed referrals through the Champlain BASE eConsult service. Can Fam Physician 2017;63:e381–6. [PMC free article] [PubMed] [Google Scholar]
- 43. Liddy C, Drosinis P, Joschko J, et al. . Improving access to specialist care for an aging population. Gerontol Geriatr Med 2016;2 10.1177/2333721416677195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Poulin PA, Romanow HC, Cheng J, et al. . Offering eConsult to family physicians with patients on a pain clinic wait list: an outreach exercise. J Healthc Qual 2017;14:14. [DOI] [PubMed] [Google Scholar]
- 45. Kim Y, Chen AH, Keith E, et al. . Not perfect, but better: primary care providers' experiences with electronic referrals in a safety net health system. J Gen Intern Med 2009;24:614–9. 10.1007/s11606-009-0955-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kim-Hwang JE, Chen AH, Bell DS, et al. . Evaluating electronic referrals for specialty care at a public hospital. J Gen Intern Med 2010;25:1123–8. 10.1007/s11606-010-1402-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Malone F, Callahan CW, Chan DS, et al. . Caring for children with asthma through teleconsultation: "ECHO-Pac, The Electronic Children's Hospital of the Pacific". Telemed J E Health 2004;10:138–46. 10.1089/tmj.2004.10.138 [DOI] [PubMed] [Google Scholar]
- 48. Olayiwola JN, Knox M, Dube K, et al. . Understanding the potential for patient engagement in electronic consultation and referral systems: lessons from one safety net system. Health Serv Res 2017;20:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Liddy C, Poulin PA, Hunter Z, et al. . Patient perspectives on wait times and the impact on their life: a waiting room survey in a chronic pain clinic. Scand J Pain 2017;17:53–7. 10.1016/j.sjpain.2017.07.015 [DOI] [PubMed] [Google Scholar]
- 50. Ackerman SL, Shipman S, Moody D, et al. . Comparing patients' experiences with econsult and referral from primary to specialty care: results from a national survey. Journal of General Internal Medicine 2017;32(2 Supplement 1):S144–S145. [Google Scholar]
- 51. Fort MP, Namba LM, Dutcher S, et al. . Implementation and evaluation of the safety net specialty care program in the Denver metropolitan area. Perm 2017;21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Joschko J, Liddy C, Moroz I, et al. . Just a click away: exploring patients' perspectives on receiving care through the Champlain BASETM eConsult service. Fam Pract 2017;8:8. [DOI] [PubMed] [Google Scholar]
- 53. Rodriguez KL, Burkitt KH, Bayliss NK, et al. . Veteran, primary care provider, and specialist satisfaction with electronic consultation. JMIR Med Inform 2015;3:e5 10.2196/medinform.3725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Straus SG, Chen AH, Yee H, et al. . Implementation of an electronic referral system for outpatient specialty care. AMIA Annu Symp Proc 2011;2011:1337–46. [PMC free article] [PubMed] [Google Scholar]
- 55. Ackerman S, Intinarelli G, Gleason N, et al. . "Have you thought about sending that as an econsult?": Primary care providers' experiences with electronic consultations at an academic medical center. J Gen Intern Med 2014;29:S3. [Google Scholar]
- 56. Haverhals LM, Sayre G, Helfrich C, et al. . Identification of facilitators and barriers to implementation of e-consults using the consolidated framework for implementation research. J Gen Intern Med 2013;28:S437. [Google Scholar]
- 57. Harno KS. Telemedicine in managing demand for secondary-care services. J Telemed Telecare 1999;5:189–92. 10.1258/1357633991933611 [DOI] [PubMed] [Google Scholar]
- 58. Haverhals LM, Sayre G, Helfrich CD, et al. . E-consult implementation: lessons learned using consolidated framework for implementation research. Am J Manag Care 2015;21:e640–7. [PMC free article] [PubMed] [Google Scholar]
- 59. Keely E, Traczyk L, Liddy C. Patients' perspectives on wait times and the Referral-Consultation process while attending a tertiary diabetes and endocrinology centre: is Econsultation an acceptable option? Can J Diabetes 2015;39:325–9. 10.1016/j.jcjd.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 60. Olayiwola JN, Anderson D, Jepeal N, et al. . Electronic consultations to improve the primary Care-Specialty care interface for cardiology in the medically underserved: a cluster-randomized controlled trial. Ann Fam Med 2016;14:133–40. 10.1370/afm.1869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. van Gelder VA, Scherpbier-de Haan ND, van Berkel S, et al. . Web-Based consultation between general practitioners and nephrologists: a cluster randomized controlled trial. Fam Pract 2017;34:430–6. 10.1093/fampra/cmw131 [DOI] [PubMed] [Google Scholar]
- 62. Golberstein E, Kolvenbach S, Carruthers H, et al. . Effects of electronic psychiatric consultations on primary care provider perceptions of mental health care: survey results from a randomized evaluation. Healthc 2017;2:2. [DOI] [PubMed] [Google Scholar]
- 63. Canning S, Saloojee N, Afkham A, et al. . Impact of types of questions asked on gastroenterology econsultation outcomes. Can J Gastroenterol Hepatol Conf 2016. [Google Scholar]
- 64. Liddy C, Hogel M, Blazkho V, et al. . The current state of electronic consultation and electronic referral systems in Canada: an environmental scan. Stud Health Technol Inform 2015;209:75–83. [PubMed] [Google Scholar]
- 65. Liddy C, Moroz I, Afkham A, et al. . Evaluating the implementation of the Champlain BASE™ eConsult service in a new region of Ontario, Canada: a cross-sectional study. Healthc Policy 2017;13:79–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Chen AH, Kushel MB, Grumbach K, et al. . A safety-net system gains efficiencies through ‘eReferrals’ to specialists. Health Aff 2010;29:969–71. 10.1377/hlthaff.2010.0027 [DOI] [PubMed] [Google Scholar]
- 67. Brophy PD. Overview on the challenges and benefits of using telehealth tools in a pediatric population. Adv Chronic Kidney Dis 2017;24:17–21. 10.1053/j.ackd.2016.12.003 [DOI] [PubMed] [Google Scholar]
- 68. Keely E, Liddy C. Critical requirements and considerations for establishing and participating in an eConsultation service: lessons learned from the Champlain BASE team. Electronic Healthc Law Rev 2015;5:5–6. [Google Scholar]
- 69. Callahan CW, Malone F, Estroff D, et al. . Effectiveness of an Internet-based store-and-forward telemedicine system for pediatric subspecialty consultation. Arch Pediatr Adolesc Med 2005;159:389–93. 10.1001/archpedi.159.4.389 [DOI] [PubMed] [Google Scholar]
- 70. Lin AH, Welstead BL, Morey BL, et al. . Return on investment analysis of health experts onLine at Portsmouth: a 2-year review of the navy's newest Teleconsultation system. Mil Med 2017;182:e1696–701. 10.7205/MILMED-D-16-00259 [DOI] [PubMed] [Google Scholar]
- 71. McManus J, Salinas J, Morton M, et al. . Teleconsultation program for deployed soldiers and healthcare professionals in remote and austere environments. Prehosp Disaster Med 2008;23:210–6. 10.1017/S1049023X0006489X [DOI] [PubMed] [Google Scholar]
- 72. Lin AH, Cole JH, Chin JC, et al. . The health experts onLine at Portsmouth (HELP) system: one-year review of adult and pediatric asynchronous Telehealth consultations. SAGE Open Med 2016;4 10.1177/2050312115626433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Baum ED, Becker DG, Kennedy DW. An Internet otolaryngology referral center: a preliminary report. Am J Rhinol 2003;17:251–6. 10.1177/194589240301700501 [DOI] [PubMed] [Google Scholar]
- 74. Stoves J, Connolly J, Grange A, et al. . Electronic consultation as an alternative to hospital referral of selected patients with chronic kidney disease: a novel application for networked electronic health records to improve the accessibility and efficiency of health care in Bradford, UK. Quality and Safety in Health Care 2009;18:e1. [DOI] [PubMed] [Google Scholar]
- 75. Angstman KB, Rohrer JE, Adamson SC, et al. . Impact of e-consults on return visits of primary care patients. Health Care Manag 2009;28:253–7. 10.1097/HCM.0b013e3181b3efa3 [DOI] [PubMed] [Google Scholar]
- 76. Shoki A, Johnson CB, Liddy C, et al. . Using econsults to inform cardiology continuing medical education needs of primary care providers. Can J Cardiol 2015;31:S100–S101. 10.1016/j.cjca.2015.07.224 [DOI] [Google Scholar]
- 77. McGeady JB, Blaschko SD, Brajtbord JS, et al. . Electronic preconsultation as a method of quality improvement for urological referrals. Urol Pract 2014;1:172–5. 10.1016/j.urpr.2014.06.005 [DOI] [PubMed] [Google Scholar]
- 78. Keely E, Drosinis P, Afkham A, et al. . Perspectives of Champlain base specialist physicians: their motivation, experiences and recommendations for providing eConsultations to primary care providers. Stud Health Technol Inform 2015;209:38–45. [PubMed] [Google Scholar]
- 79. Angstman KB, Adamson SC, Furst JW, et al. . Provider satisfaction with virtual specialist consultations in a family medicine department. Health Care Manag 2009;28:14–18. 10.1097/HCM.0b013e318196def8 [DOI] [PubMed] [Google Scholar]
- 80. Cruz ML, Gleason N, Wang M, et al. . Transforming the endocrine consult: asynchronous provider consultations. Endocr Pract 2015;21:514–21. 10.4158/EP14297.OR [DOI] [PubMed] [Google Scholar]
- 81. Moreea S, Appleby VJ, Smith B, et al. . PTH-067 setting up a hepatology econsult service – beneficial for patients and primary care, but perhaps a hardship for secondary care? Gut 2014;63(Suppl 1):A238.2–A239. 10.1136/gutjnl-2014-307263.513 [DOI] [Google Scholar]
- 82. Liddy C, Maranger J, Afkham A, et al. . Ten steps to establishing an e-consultation service to improve access to specialist care. Telemed J E Health 2013;19:982–90. 10.1089/tmj.2013.0056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Uhlman M, Lakose S, Dietzler D, et al. . Implementation of the three E's (efficiency, education, and e-consults) to improve urology access within the Veterans health administration. Journal of Urology 2016;1:e244. [Google Scholar]
- 84. Shehata F, Posner G, Afkham A, et al. . Evaluation of an electronic consultation service in obstetrics and gynecology in Ontario. Obstet Gynecol 2016;127:1033–8. 10.1097/AOG.0000000000001431 [DOI] [PubMed] [Google Scholar]
- 85. Khamisa K, Fogel A, Liddy C, et al. . Utilization and impact of a hematology e-consultation service. Blood 2015;126:42.25918346 [Google Scholar]
- 86. Horner K, Wagner E, Tufano J. Electronic consultations between primary and specialty care clinicians: early insights. Issue Brief 2011;23:1–14. [PubMed] [Google Scholar]
- 87. Mendu ML, McMahon GM, Licurse A, et al. . Electronic consultations in nephrology: pilot implementation and evaluation. Am J Kidney Dis 2016;68:821–3. 10.1053/j.ajkd.2016.05.029 [DOI] [PubMed] [Google Scholar]
- 88. Tran CS, Liddy CE, Liu DM, et al. . eCONSULTS to endocrinologists improve access and change primary care provider behavior. Endocr Pract 2016;22:1145–50. 10.4158/E161321.OR [DOI] [PubMed] [Google Scholar]
- 89. Chittle MD, Rao SK, Jaff MR, et al. . Asynchronous vascular consultation via electronic methods: a feasibility pilot. Vasc Med 2015;20:551–6. 10.1177/1358863X15601734 [DOI] [PubMed] [Google Scholar]
- 90. Davis A, Gilchrist V, Grumbach K, et al. . Advancing the PRIMARY/SPECIALTY care interface through ECONSULTS and enhanced referrals. Ann Fam Med 2015;13:387–8. 10.1370/afm.1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Liddy C, Deri Armstrong C, Drosinis P. What are the Costs of Improving Access to Specialists through eConsultation? The Champlain BASE Experience : Global telehealth 2015: integrating technology and information for better healthcare. 209 IOS Press, 2015: 67–74. [PubMed] [Google Scholar]
- 92. Liddy C, Smyth C, Poulin PA, et al. . Improving access to chronic pain services through eConsultation: a cross-sectional study of the Champlain base eConsult service. Pain Med 2016;3:3. [DOI] [PubMed] [Google Scholar]
- 93. Liddy C, McKellips F, Armstrong CD, et al. . Improving access to specialists in remote communities: a cross-sectional study and cost analysis of the use of eConsult in Nunavut. Int J Circumpolar Health 2017;76:1323493 10.1080/22423982.2017.1323493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Gupte G, Vimalananda V, Simon SR, et al. . Disruptive innovation: implementation of electronic consultations in a Veterans Affairs health care system. JMIR Med Inform 2016;4:e6 10.2196/medinform.4801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Liddy C, Smyth C, Poulin PA, et al. . Supporting Better Access to Chronic Pain Specialists: The Champlain BASE™ eConsult Service. J Am Board Fam Med 2017;30:766–74. 10.3122/jabfm.2017.06.170170 [DOI] [PubMed] [Google Scholar]
- 96. Murthy R, Rose G, Liddy C, et al. . eConsultations to infectious disease specialists: questions asked and impact on primary care providers' behavior. Open Forum Infect Dis 2017;4:ofx030 10.1093/ofid/ofx030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Scherpbier-de Haan ND, van Gelder VA, Van Weel C, et al. . Initial implementation of a web-based consultation process for patients with chronic kidney disease. Ann Fam Med 2013;11:151–6. 10.1370/afm.1494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Linsenmeyer K, Strymish JM, Smith D, et al. . Electronic consults for improving vancomycin use. J Hosp Infect 2018;99:158–9. 10.1016/j.jhin.2017.12.002 [DOI] [PubMed] [Google Scholar]
- 99. Keely E, Williams R, Epstein G, et al. . Specialist perspectives on Ontario provincial electronic consultation services. Telemed E Health 2018. [DOI] [PubMed] [Google Scholar]
- 100. Lee MS, Ray KN, Mehrotra A, et al. . Primary care practitioners’ perceptions of electronic consult systems. JAMA Intern Med 2018;178:782 10.1001/jamainternmed.2018.0738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Kirsh S, Carey E, Aron DC, et al. . Impact of a national specialty e-consultation implementation project on access. Am J Manag Care 2015;21:e648–54. [PubMed] [Google Scholar]
- 102. Kirsh SR, Ho PM, Aron DC. Providing specialty consultant expertise to primary care: an expanding spectrum of modalities. Mayo Clin Proc 2014;89:1416–26. 10.1016/j.mayocp.2014.04.016 [DOI] [PubMed] [Google Scholar]
- 103. McGinn CA, Grenier S, Duplantie J, et al. . Comparison of user groups' perspectives of barriers and facilitators to implementing electronic health records: a systematic review. BMC Med 2011;9:46 10.1186/1741-7015-9-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Pham MT, Rajić A, Greig JD, et al. . A scoping review of scoping reviews: advancing the approach and enhancing the consistency. Res Synth Methods 2014;5:371–85. 10.1002/jrsm.1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Delaigue S, Bonnardot L, Steichen O, et al. . Seven years of telemedicine in Médecins sans Frontières demonstrate that offering direct specialist expertise in the frontline brings clinical and educational value. J Glob Health 2018;8:020414 10.7189/jogh.08.020414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Stanistreet K, Verma J, Kirvan K, et al. . Physician remuneration for remote consults: an overview of approaches across Canada. Healthc Q 2017;20:12–15. 10.12927/hcq.2017.25294 [DOI] [PubMed] [Google Scholar]
- 107. Skeith L, Mohamed M, Karovitch A, et al. . The use of eConsults to improve access to specialty care in thrombosis medicine. Thromb Res 2017;160:105–8. 10.1016/j.thromres.2017.11.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001629supp001.pdf (520.1KB, pdf)





