Abstract
Background and Aims:
Confirmation of endotracheal tube (ETT) position is necessary to ensure proper ventilation. The present study was conducted with the aim to compare the efficacy of three ultrasonographic (USG) techniques in terms of time taken for confirmation of ETT position. The time taken by each USG technique was also compared with that for auscultation and capnography. The ability of the three USG techniques to identify tracheal placement of ETT was evaluated in all patients.
Material and Methods:
Ninety adult American Society of Anesthesiologists (ASA) I/II patients requiring general anaesthesia with tracheal intubation were randomised into three groups (n = 30 each) depending upon the initial USG transducer position used to confirm tracheal placement of ETT: group T (tracheal), group P (pleural) and group D (diaphragm). The time taken for confirmation of tracheal placement of ETT by USG, auscultation and capnography was recorded for each of the groups. Subsequently, USG confirmation of ETT placement was performed with the other two USG techniques in all patients.
Results:
The time taken for USG in group T was significantly less (3.8 ± 0.9 s) compared to group P (12.1 ± 1.6 s) and group D (13.8 ± 1.7 s); P < 0.001. USG was significantly faster than both auscultation and capnography in group T (P < 0.001), whereas in group P and group D, USG took longer time compared to auscultation (P = 0.014 and P < 0.001, respectively) but lesser time than capnography (P < 0.001 in both groups).
Conclusion:
USG is a rapid technique for identification of ETT placement. All the three USG techniques are reliable in identifying the tracheal placement of ETT.
Keywords: Auscultation, capnography, tracheal intubation, ultrasonography
Introduction
Tracheal intubation is one of the essential medical procedures. Unrecognised or accidental endobronchial intubation results in hypoventilation and collapse of the non-ventilated lung, barotrauma or pneumothorax in the ventilated lung.[1] Unrecognised oesophageal intubation can lead to severe morbidity like hypoxic brain damage.[2,3] Therefore, verification of correct positioning of endotracheal tube (ETT) is essential to avoid serious consequences.
Various methods have been described to identify the correct position of ETT viz., intubation under direct vision,[4] inspection of chest wall movements, auscultation of bilateral breath sounds, monitoring of end-tidal carbon dioxide (EtCO2),[5] use of negative pressure devices, fiberoptic bronchoscopy, sonomatic confirmation of tracheal intubation (SCOTI) device and chest X-ray. Among all, though capnography is considered the gold standard[6,7] it may not be reliable under certain conditions, e.g., endobronchial intubation, poor circulatory perfusion as in cardiac arrest, severe hypotension,[8] pulmonary embolism, severe bronchospasm, poor pulmonary reserve like pleural effusion, pneumothorax and pulmonary malignancy.[8,9] Prior bag-mask ventilation leading to gastric insufflation, antacid consumption or ingestion of carbonated beverages also may lead to false positive results with capnography.[8] The American College of Emergency Physicians 2005 guidelines recommend that some additional method of confirmation must be performed after placement and before securing the ETT.[3]
Ultrasound is a relatively new technique for ETT confirmation. It is non-invasive, portable and serves as a real-time diagnostic tool with rapid and accurate results. Additionally, there is no interference due to ambient environmental noise.[10] The ultrasonographic (USG) images are not affected by low pulmonary blood flow.[6]
Three USG methods have been described in the literature for confirmation of ETT position viz., direct visualisation of ETT during intubation (tracheal USG),[2,5,6,8] sliding lung sign (visceral-parietal pleural interface or VPPI)[9,10,11,12,13] and bilateral diaphragmatic dome movement.[4,14,15] Tracheal USG technique can detect oesophageal intubation even before initiating ventilation, thereby preventing unnecessary insufflation of stomach and its associated complications.[5,6] Lung sliding sign and bilateral diaphragm dome movement methods can additionally detect endobronchial intubation by visualising pleural and hemidiaphragm movements bilaterally, respectively[9,14] and can thus prevent inadvertent endobronchial intubation which may be missed by conventional methods material.
On extensive literature search, it was found that these three USG methods have never been compared with each other. Therefore, the present study was conducted with the primary objective to evaluate the three USG techniques for their efficacy to detect the tracheal position of ETT in terms of time taken for confirmation of ETT position. The secondary objective of the study was to compare the time taken by USG technique with time taken for auscultation and capnography. As an ancillary observation, ability of USG technique to identify tracheal placement of ETT in all patients and the feasibility of USG to detect accidental oesophageal intubation, if it occurred, was also studied.
Material and Methods
An approval of the procedures followed in this prospective, randomised, observational study was obtained from the institutional ethics committee-human research and were in accordance with the Helsinki Declaration of 1975, as revised in 2000. The protocol of the study was registered prospectively with www.ctri.nic.in. A written informed consent was obtained from all the participants. Ninety American Society of Anesthesiologists (ASA) I or II patients between 18–60 years of age with Mallampati Class I or II airway scheduled to undergo elective surgical procedures requiring general anaesthesia (GA) with endotracheal intubation were included. Pregnant patients, those at risk of pulmonary aspiration or having neck swellings, cervical spine disease, pleural effusion, pneumothorax, intercostal drain in situ and body mass index (BMI) ≥35 kg/m2 were excluded.
In the pre-operative room, USG scanning was performed with the SonoRite™ USG scanner. A 9.0 MHz linear transducer was used to identify the trachea initially in the longitudinal orientation and then in transverse orientation. Antero-lateral chest wall between 4th and 6th intercostal space was scanned bilaterally with 9.0 MHz linear transducer in mid-clavicular line, anterior axillary line and mid-axillary line. A 7.5 MHz linear transducer placed in the sub-xiphoid/subcostal region was used to identify the diaphragm. Skin markings were done at the site of best visualisation of trachea, VPPI and diaphragmatic domes in all the participants.
In the operating room, monitoring in the form of lead II electrocardiography, pulse oximetry, non-invasive blood pressure and side-stream capnography was started. Using a computer-generated random number table, patients were assigned to one of the three groups: group T (tracheal), group P (pleural) or group D (diaphragm) based on the ultrasound technique which was to be timed for identifying endotracheal intubation in addition to auscultation and capnography in all the patients. General anaesthesia was induced with fentanyl 2 μg/kg, propofol 2–3 mg/kg and vecuronium 0.1 mg/kg IV. An ETT of appropriate size was used for tracheal intubation.
Time taken from introduction of ETT to confirmation of placement was recorded with the USG technique (as per group allocation), auscultation and capnography. Four investigators were involved in the conduct of the study. The first investigator performed the intubation, attached the breathing circuit, initiated ventilations and announced the appearance of six regular EtCO2 waveforms on capnography. The second investigator announced the confirmation of placement of ETT with auscultation at the epigastrium and both lung apices. The third investigator wore head phones to prevent overhearing of any verbal communication between other investigators, performed the USG and announced ETT confirmation by USG technique (visualisation of ‘comet tail sign’ in group T, 'sliding lung sign’ on bilateral lung fields in Group P and ‘movement of both the domes of the diaphragm’ with positive pressure ventilation in group D). The capnograph screen was kept out of his sight to avoid any kind of observational bias. The fourth investigator recorded all the timings as announced by the first three investigators with a stopwatch.
Once the time taken for the USG technique, auscultation and capnography was complete, the other two positions of USG transducer were explored for visualisation of the signs of tracheal intubation, though timings were noted for only the first USG technique as per randomisation. Rest of the technique of anaesthesia was as per the standard protocol.
Since there was no previous published literature comparing the three USG techniques for their efficacy in terms of the time taken for confirmation of tracheal position of ETT in patients undergoing elective surgical procedures, this study was carried out as a pilot study with 30 patients in each group. Descriptive tables were generated. The time taken for confirmation of tracheal placement of ETT was reported as mean ± standard deviation (SD). The quantitative variables were compared using one-way analysis of variance (ANOVA) followed by post-hoc Tukey's test. A P value <0.05 was considered significant. Statistical analysis was carried out using the SPSS version 20.
Results
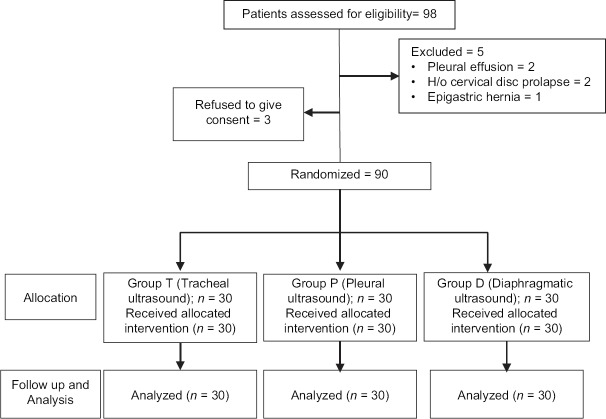
A total of 98 patients were assessed for eligibility. Three of them refused to give consent and five were excluded as per defined exclusion criteria. Ninety patients were randomised and analysed with 30 patients per group [Figure 1]. The demographic profile is shown in Table 1. All the three groups were statistically similar in terms of mean age, height and gender distribution. The weight and BMI of patients in group D was significantly less than that of group T.
Figure 1.
CONSORT flow diagram
Table 1.
Demographic profile
| Group T (n=30) | Group P (n=30) | Group D (n=30) | P | |
|---|---|---|---|---|
| Age (years)* | 34.3±12.4 | 34.6±17.9 | 35.2±12.5 | 0.961 |
| Weight (kg)* | 60.7±9.5 | 58.2±8.3 | 54.5±7.2 | 0.015 |
| Height (m)* | 1.6±0.1 | 1.6±0.1 | 1.6±0.1 | 0.505 |
| BMI (kg/m2)* | 24.1±3.1 | 22.9±2.3 | 22.0±2.5 | 0.011 |
| Gender (M:F)† | 15:15 | 17:13 | 17:13 | 0.836 |
T=Tracheal; P=Pleural; D: Diaphragm; BMI=Body mass index; *Values are expressed as mean±SD; †Values are expressed as ratio; M=Male; F=Female
Table 2 shows the time taken for confirmation of placement of ETT by USG, auscultation and capnography. The mean time for confirmation with USG was significantly less in group T compared to groups P and D (P < 0.001), whereas time taken for auscultation and capnography was comparable in all the three groups (P = 0.207 and P = 0.827, respectively).
Table 2.
Time for confirmation of placement of endotracheal tube
| Method | Group T (n=30) | Group P (n=30) | Group D (n=30) | P |
|---|---|---|---|---|
| USG confirmation | 3.8±0.9 | 12.1±1.6 | 13.8±1.7 | <0.001 |
| Auscultation | 9.8±1.8 | 10.6±2.3 | 10.5±1.7 | 0.207 |
| Capnography | 22.3±0.9 | 22.3±1.8 | 22.1±1.5 | 0.827 |
| P | <0.001 | <0.001 | <0.001 |
T=Tracheal; P=Pleural; D=Diaphragm; *Values are expressed as mean±SD in seconds, USG=Ultrasonographic, P<0.05 is significant
On intra-group comparisons [Table 2], tracheal USG was significantly faster than both auscultation and capnography (P < 0.001), whereas pleural and diaphragmatic USG took more time than auscultation (P = 0.014 and P < 0.001, respectively), but less time than capnography (P < 0.001 for both groups). Capnography took significantly longer time than auscultation in all the three groups (P < 0.001).
Trachea was visualised with both longitudinal and transverse USG transducer positions in all the patients [Table 3]. Anterior wall of ETT was seen in longitudinal position of the transducer [Figure 2a] and ‘comet tail sign’ was seen in transverse position in all the patients [Figure 2b]. 'Sliding lung sign’ was best seen in the mid-clavicular window bilaterally (41.1% patients) [Table 3]. Sliding of VPPI was appreciated bilaterally in all the patients [Figure 3]. Sub-xiphoid window was used to visualise bilateral diaphragm domes in all patients [Table 3]. Figure 4 shows the domes of the diaphragm as they were visualised from the sub-xiphoid window. All the three USG techniques could identify the presence of ETT in the trachea in all patients.
Table 3.
USG transducer positions for structural visualisation
| Structure | Transducer position | Number of patients | |||
|---|---|---|---|---|---|
| Group T | Group P | Group D | Total | ||
| Trachea | Longitudinal | 30 | 30 | 30 | 90 |
| Transverse | 30 | 30 | 30 | 90 | |
| Pleura | Right mid-clavicular line | 14 | 10 | 13 | 37 |
| Right anterior-axillary line | 5 | 9 | 7 | 21 | |
| Right mid-axillary line | 11 | 11 | 10 | 32 | |
| Left mid-clavicular line | 13 | 11 | 13 | 37 | |
| Left anterior-axillary line | 4 | 8 | 4 | 16 | |
| Left mid-axillary line | 13 | 11 | 13 | 37 | |
| Diaphragm | Right sub-xiphoid window | 30 | 30 | 30 | 90 |
| Right subcostal window | 0 | 0 | 0 | 0 | |
| Left sub-xiphoid window | 30 | 30 | 30 | 90 | |
| Left subcostal window | 0 | 0 | 0 | 0 | |
Values are number of patients. USG=Ultrasonographic
Figure 2.
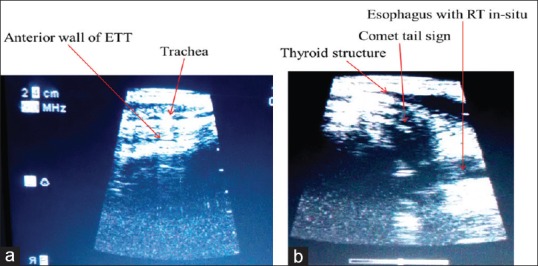
Ultrasonographic view of trachea. (a) Longitudinal orientation of transducer. (b) Transverse orientation of transducer
Figure 3.

View of the visceral-parietal pleural interface with the transducer on the mid-clavicular line
Figure 4.
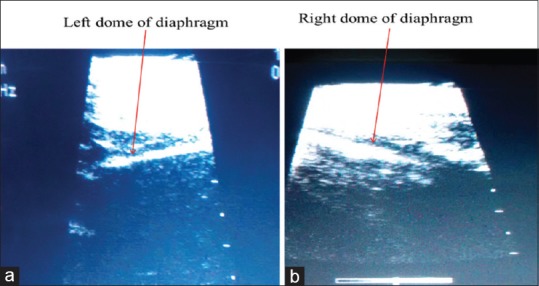
Domes of the diaphragm as visualised from the sub-xiphoid window. (a) Left dome of diaphragm. (b) Right dome of diaphragm
There was no incidence of oesophageal intubation.
Discussion
In the present study, amongst the USG techniques, tracheal USG took the least time for confirmation of ETT position followed by pleural and diaphragmatic USG. Time taken for ETT confirmation with auscultation was longer than tracheal USG but lesser than pleural and diaphragmatic USG. Capnography took maximum time for confirmation when compared to any of the three USG techniques and auscultation. The characteristic signs of tracheal intubation could be identified in all patients with all three USG techniques. There was no incidence of oesophageal intubation.
We could not locate any study which has measured the time taken for ETT confirmation with diaphragmatic position of the USG transducer. Additionally, in this study, the time taken by USG technique to detect tracheal position of ETT has been compared with that taken for by auscultation and capnography, which has not been done in previous studies.
In the study by Thomas et al. conducted on 100 patients requiring emergency intubation, USG with tracheal transducer position took 8.27 ± 1.54 s to detect ETT position.[16] In another study by Chou et al., the mean time was 14.8 ± 18.7 s and the median time was 9 s. Quantitative waveform capnography took more time with the maximum time difference between USG and capnography being 60 s.[6] Werner et al. demonstrated that tracheal intubation could be easily differentiated from oesophageal intubation by tracheal USG before ventilation was initiated.[5] In our study we could identify tracheal intubation with USG transducer over the trachea before connecting the breathing circuit to ETT and the mean time taken was 3.8 ± 0.9 s. The tracheal USG technique timings of our study were considerably faster than those of Chou et al.,[6] but were in close agreement to that of Muslu et al.,[17] where the correct positioning could be verified within 3 s. Similar to Chou et al.,[6] capnography took the maximum time for confirmation in our study as well.
Pfeiffer et al. conducted a study on 25 patients and found that bilateral lung USG to visualise VPPI took a median time of 40 s [interquartile range (IQR): 35–48 s] which was as fast as auscultation [median time 42 s (IQR: 37–47 s)] and faster than auscultation and EtCO2 measurement for six breaths combined [48 s (45–53 s)].[11] Marciniak et al.,[18] in their study, described the characteristic changes in the paediatric airway for identification of tracheal position of ETT. They could confirm the position of ETT by visualisation of bilateral 'sliding lung sign’, however, they did not record the timing for this. We found that confirmation of ETT with pleural 'sliding lung sign’ took 12.1 ± 1.6 s, auscultation took 10.6 ± 2.3 s and capnography required 22.3 ± 1.8 s.
There is no previous study which has measured the time taken for ETT confirmation with diaphragmatic position of the USG transducer. We found that bilateral diaphragmatic USG took 13.8 ± 1.7 s. The comparatively longer time taken by the diaphragmatic USG technique may be because diaphragm is a deep structure in the abdomen and its visualisation with USG may be difficult and hence, more time consuming.
It is also of note that the time recording for each of these three techniques was started from the same time point, i.e., introduction of ETT in the oral cavity. Whereas the ETT can be viewed during real-time passage with tracheal position of USG transducer, visualisation of VPPI and bilateral diaphragmatic domes requires that the intubation procedure is complete, breathing circuit is attached and signs of tracheal intubation are identified bilaterally. These also contribute to the longer time taken for VPPI and diaphragmatic methods.
Capnography technique took longest time because the side-stream capnography, used in our study, has an associated rise time depending upon various factors like rotation of the chopper wheel, rate of gas aspiration, volume of aspiration tubing and water traps and dynamic response of infrared filters and other electronics.[19]
Drescher et al.[2] have advocated the use of longitudinal transducer orientation over the trachea during the time of intubation. According to them, the transverse orientation of the transducer was better for the visualisation of oesophageal intubation. In accordance with the same, the longitudinal transducer orientation was used for real-time visualisation during the passage of ETT. The transducer was later placed just above the suprasternal notch transversely as described by various other researchers.[3,6,17,18]’Comet tail sign’ [Figure 2b] was identified in all patients in the present study. In their study on a cadaver model, Ma et al. found a sensitivity of 97.1% and specificity of 100%.[20] We could identify all the intubations as tracheal with 100% accuracy.
Tracheal USG, though very fast, can identify the presence of ETT in the airway with great accuracy but it cannot differentiate endotracheal from endobronchial intubation as the carina is difficult to visualise. In a previous study, Marciniak et al. performed pleural USG to visualise bilateral VPPI after tracheal imaging to verify the endotracheal position of ETT.[18] Oesophageal intubation has been described as an anechoic circle that appears posterior to the thyroid tissue adjacent to the trachea as ETT enters the oesophagus[5] or as a ‘double track sign’.[6] There was no case of oesophageal intubation in our study. In the present study, oesophagus was identified in all the cases as a collapsed cauliflower like round structure lying lateral to the trachea with the transducer positioned transversely at the suprasternal notch.
For visualisation of VPPI, mid-clavicular line gave the best views. Bilateral 'sliding lung sign’, as described by Weaver et al.,[9] was identified in all patients indicating the endotracheal position of ETT. According to them, absence of this sign on left lung indicates main stem bronchus intubation and bilateral absence signifies oesophageal intubation. In another study also, VPPI visualisation was stated to be a useful technique for identification of right endobronchial tube placement.[10] In studies done in patients requiring emergency intubations in cardiac arrest situations, this technique was found to be accurate for identification of ETT position.[13] In our study also, we could accurately confirm the endotracheal position of ETT on visualisation of bilateral VPPI with ventilation in all patients. However, as there was no case of endobronchial intubation, we did not find unilateral absence of VPPI movements.
To visualise hemidiaphragm of each side, the transducer was placed obliquely in sub-xiphoid window as described by Hsieh et al.[14] and Kerrey et al.[15] Bilateral diaphragmatic movements were visualised in all patients. Both the diaphragmatic domes moved downwards with positive pressure ventilation. Absence or paradoxical movement of diaphragm was not observed in any of our patients.
The present study has certain limitations. It was a single-centre study conducted in a controlled environment. So the results may not be reproducible in patients with difficult airways. As the sites of best visualisation using USG probe were marked pre-operatively, the results of this study may not be applicable to patients undergoing emergency intubations where there is no time to pre-visualise the underlying structures.
To conclude, if there is availability of equipment and expertise to perform and interpret its findings, USG is a rapid technique for identification of ETT placement. Real-time visualisation of tracheal tube with USG transducer placed over the trachea during intubation can be used for confirmation of ETT placement in the airway before initiating ventilation. This is very useful in trauma victims, pregnancy and patients at high risk for aspiration. Bilateral pleural and diaphragmatic USG techniques are comparable with respect to time taken for auscultation and are considerably faster than capnography for confirmation of ETT position.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Al-Qahtani AS, Messahel FM, Ouda WOA. Inadvertent endobronchial intubation: A sentinel event. Saudi J Anaesth. 2012;6:259–62. doi: 10.4103/1658-354X.101218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drescher MJ, Conard FU, Schamban NE. Identification and description of esophageal intubation using ultrasound. Acad Emerg Med. 2000;7:722–5. doi: 10.1111/j.1553-2712.2000.tb02055.x. [DOI] [PubMed] [Google Scholar]
- 3.Milling TJ, Jones M, Khan T, Tad-y D, Melniker LA, Bove J, et al. Transtracheal 2-d ultrasound for identification of esophageal intubation. J Emerg Med. 2007;32:409–14. doi: 10.1016/j.jemermed.2006.08.022. [DOI] [PubMed] [Google Scholar]
- 4.Hosseini JS, Talebian MT, Ghafari MH, Eslami V. Secondary confirmation of endotracheal tube position by diaphragm motion in right subcostal ultrasound view. Int J Crit Illn Inj Sci. 2013;3:113–7. doi: 10.4103/2229-5151.114269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Werner SL, Smith CE, Goldstein JR, Jones RA, Cydulka RK. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med. 2007;49:75–80. doi: 10.1016/j.annemergmed.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Chou H-C, Tseng W-P, Wang C-H, Ma MH-M, Wang H-P, Huang P-C, et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. 2011;82:1279–84. doi: 10.1016/j.resuscitation.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 7.Grmec S. Comparison of three different methods to confirm tracheal tube placement in emergency intubation. Intensive Care Med. 2002;28:701–4. doi: 10.1007/s00134-002-1290-x. [DOI] [PubMed] [Google Scholar]
- 8.Li J. Capnography alone is imperfect for endotracheal tube placement confirmation during emergency intubation. J Emerg Med. 2001;20:223–9. doi: 10.1016/s0736-4679(00)00318-8. [DOI] [PubMed] [Google Scholar]
- 9.Weaver B, Lyon M, Blaivas M. Confirmation of endotracheal tube placement after intubation using the ultrasound sliding lung sign. Acad Emerg Med. 2006;13:239–44. doi: 10.1197/j.aem.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Chun R, Kirkpatrick AW, Sirois M, Sargasyn AE, Melton S, Hamilton DR, et al. Where's the tube? Evaluation of hand-held ultrasound in confirming endotracheal tube placement. Prehosp Disaster Med. 2004;19:366–9. doi: 10.1017/s1049023x00002004. [DOI] [PubMed] [Google Scholar]
- 11.Pfeiffer P, Rudolph SS, Borglum J, Isbye DL. Temporal comparison of ultrasound vs. auscultation and capnography in verification of endotracheal tube placement. Acta Anaesthesiol Scand. 2011;55:1190–5. doi: 10.1111/j.1399-6576.2011.02501.x. [DOI] [PubMed] [Google Scholar]
- 12.Breitkreutz R, Seibel A, Zechner PM. Ultrasound-guided evaluation of lung sliding for widespread use? Resuscitation. 2012;83:273–4. doi: 10.1016/j.resuscitation.2011.12.034. [DOI] [PubMed] [Google Scholar]
- 13.Sim S-S, Lien W-C, Chou H-C, Chong K-M, Liu S-H, Wang C-H, et al. Ultrasonographic lung sliding sign in confirming proper endotracheal intubation during emergency intubation. Resuscitation. 2012;83:307–12. doi: 10.1016/j.resuscitation.2011.11.010. [DOI] [PubMed] [Google Scholar]
- 14.Hsieh K-S, Lee C-L, Lin C-C, Huang T-C, Weng K-P, Lu W-H. Secondary confirmation of endotracheal tube position by ultrasound image. Crit Care Med. 2004;32:S374–7. doi: 10.1097/01.ccm.0000134354.20449.b2. [DOI] [PubMed] [Google Scholar]
- 15.Kerrey BT, Geis GL, Quinn AM, Hornung RW, Ruddy RM. A prospective comparison of diaphragmatic ultrasound and chest radiography to determine endotracheal tube position in a pediatric emergency department. Pediatrics. 2009;123:e1039–44. doi: 10.1542/peds.2008-2828. [DOI] [PubMed] [Google Scholar]
- 16.Thomas VK, Paul C, Rajeev PC, Palatty BU. Reliability of ultrasonography in confirming endotracheal tube placement in an emergency setting. Indian J Crit Care Med. 2017;21:257–61. doi: 10.4103/ijccm.IJCCM_417_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muslu B, Sert H, Kaya A, Demircioglu RI, Gözdemir M, Usta B, et al. Use of sonography for rapid identification of esophageal and tracheal intubations in adult patients. J Utrasound Med. 2011;30:671–6. doi: 10.7863/jum.2011.30.5.671. [DOI] [PubMed] [Google Scholar]
- 18.Marciniak B, Fayoux P, Hébrard A, Krivosic-Horber R, Engelhardt T, Bissonnette B. Airway management in children: Ultrasonography assessment of tracheal intubation in real time? Anesth Analg. 2009;108:461–5. doi: 10.1213/ane.0b013e31819240f5. [DOI] [PubMed] [Google Scholar]
- 19.Brunner JX, Westenskow DR. How the rise time of carbon dioxide analysers influence the accuracy of carbon dioxide measurements. Br J Anaesth. 1988;61:628–38. doi: 10.1093/bja/61.5.628. [DOI] [PubMed] [Google Scholar]
- 20.Ma G, Davis DP, Schmitt J, Vilke GM, Chan TC, Hayden SR. The sensitivity and specificity of transcricothyroid ultrasonography to confirm endotracheal tube placement in a cadaver model. J Emerg Med. 2007;32:405–7. doi: 10.1016/j.jemermed.2006.08.023. [DOI] [PubMed] [Google Scholar]