Abstract
Objective:
To conduct a cross-sectional assessment of the adoption of Total Worker Health® (TWH) policies and practices by business size and evaluate extent and alignment of their safety and health.
Methods:
We conducted an analysis of 382 businesses that completed the Health Links™ Assessment. We measured organizational adoption of TWH across six benchmarks: organizational supports, workplace assessments, health policies and programs, safety, engagement, and evaluation.
Results:
Benchmark scores were significantly associated with business size. Larger businesses were more likely to score higher across each benchmark.
Conclusions:
Small businesses are implementing TWH in a variety of ways and the level of implementation differs by business size. Practical interventions as well as dissemination and implementation research should take business size into account to ensure TWH is both effective and sustainable in meeting the needs of employees.
Keywords: Total Worker Health®, Small Business, Workplace Health, Occupational Safety, Organizational Behavior
INTRODUCTION
Globally, the majority of workplaces employ fewer than 50 employees.1 In the US, small businesses with fewer than 250 employees make up 99% of private firms, employing 56.8 million workers.1 A substantial body of research demonstrates the benefits of occupational health and safety (OHS) programs and of health promotion programs in large businesses, including improving safety and health behaviors, lowering costs to workers and employers, and ultimately preventing work-related injury and illness. However, there has been little research specifically examining how small employers address worker health, safety, and well-being or identifying differences based on business size. 2, 3
Workers employed by small businesses bear a greater burden of occupational fatalities, illnesses, and injuries.4 They also suffer higher than average rates of chronic health conditions and unhealthy behaviors. 5,6,7,8,9 Thus, based on the burden, need, and potential impact, small businesses warrant closer examination to assess how they can better address safety, health and well-being.
The National Institute for Occupational Safety and Health’s (NIOSH) Total Worker Health® (TWH) approach is defined as policies, programs, and practices that integrate protection from work-related safety and health hazards with promotion of injury and illness prevention efforts to advance worker well-being.10 While research on TWH approaches hold promise for establishing new ways of meeting the needs of workers in small businesses, most TWH intervention studies to date have been conducted in large businesses, with little evidence to support the generalization of results to the small business setting. 5, 7, 11 Our understanding of the current practices in small businesses and of the barriers to adoption, effectiveness, and sustainability of TWH programs remain extremely limited.11, 12, 13
The emerging TWH intervention literature is still sparse, especially as it relates to small business. TWH researchers have documented that small businesses, especially those with less than 50 employees, generally do not offer the same level of either integrated or even siloed health protection, health promotion, and health-impacting employee benefits found in larger organizations.2,14,15 Research confirms low adherence to traditional occupational safety and health best practices by small businesses as well as a low degree of adoption of TWH practices.16 However, a recent review by Anger and colleagues found only 17 published intervention efficacy studies that examined integrated interventions that addressed traditional occupational safety and/or health (OSH) and wellness and/or well-being.2 None of the 17 studies were conducted in businesses with less than 500 employees, underscoring the gap in our understanding of how to improve TWH in small business. In addition, when TWH approaches have been investigated, the number of small businesses studied has been small, concentrated in single industries, and designed to test selected, individual elements of TWH policies and programs, raising concerns about generalizability. To our knowledge, there have been no studies that have looked at comprehensive policies and strategies for TWH in small businesses across multiple industries and comparing multiple organizations.
Study Purpose
In order to identify potential opportunities to improve OSH solutions in small businesses, the current study characterizes current TWH practices across multiple industrial sectors and across the spectrum of organization sizes. We hypothesized that larger businesses offer TWH programming than do smaller enterprises. In considering TWH integration, we hypothesized that businesses that address workplace safety would be more likely to also address health promotion, regardless of business size.
METHODS
Health Links™
In July 2013, Health Links™ was launched in Colorado as a non-profit, academic, community-based program focused on engaging businesses of all sizes to help them build a culture of health, safety, and well-being.7,11 Researchers from the Center for Health, Work, & Environment based at the Colorado School of Public Health designed and implemented Health Links to 1) assess organizations’ efforts to support health and safety, 2) advise on actionable goals in one-on-one advising sessions, 3) connect like-minded businesses with one another and to local resources, and 4) certify employers as Certified Healthy Businesses. We implemented the program at the community level by partnering with chambers of commerce, economic development groups, and local public health agencies (LPHAs), as well as through direct outreach to the business community in Colorado. Outreach and recruitment were largely targeted at reaching small and mid-sized employers. Figure 1. Shows the channel partners for program implementation.
FIGURE 1.
The Health Links dissemination model to reach, educate and assess TWH in small businesses, representing the types of groups share information.
The program was designed by conducting both focus groups and key informant interviews with business leaders, small business owners, employees, chambers of commerce, payers, brokers, offices of economic development, marketing and advertising consultants, public health officials, experts in occupational health and safety, occupational medicine, health promotion practitioners, and other stakeholders. We determined that the intervention must: 1) be based on best available evidence, 2) accommodate the needs of many different types of businesses and workforces, 3) be feasible for small businesses to access and adopt, meaning inexpensive and not resource/time intensive, 4) be scalable to large numbers of businesses, 5) apply basic principles of organizational change management, and 6) generate metrics so that the program could be evaluated in five domains of the RE-AIM model: reach, efficacy, adoption, implementation and maintenance of the intervention.17
We developed a business-facing website to ensure that the assessment, key messaging, customized feedback, and resources were easy to access, simple to understand, and useful for the target audience.18 Focus groups with employers and small business leaders were conducted to gather feedback to help inform the content presented on the website and optimize user experience. The final website included basic information on TWH and a main call to action to complete the assessment. The website also included a portal where users could view their assessment and report card that was generated based on algorithms using responses from the assessment. Users were connected to a resource center that provided downloadable materials relevant to the identified priority areas for improvement and a geo-coded map to direct them to local resources.
The Health Links Assessment was developed based on key principles distilled from the CDC Worksite Health ScoreCard, 19 the NIOSH Total Worker Health® approach, 20 and the WHO Healthy Workplace Framework.21 It was designed to collect data in six key areas including organizational supports, workplace assessment, health policies and programs, safety policies and programs, engagement, and evaluation. For example, a sample item under organization supports asks, “In the last 12 months, what resources have you dedicated to workplace health and safety efforts?” A sample item under health policies and programs asks, “Do you provide free or subsidized clinical screening for depression, substance abuse, or other mental health concerns?” Organizations that completed the online assessment received a report card summarizing their results across each benchmark and providing them with a set of recommendations. Businesses could also access an online Resource Center that provided a centralized database of tools including online materials for implementing TWH, relevant to each recommendation. The Resource Center also connected businesses to other organizations that had completed the Health Links Assessment in their region and a map of local resources including recreation centers, OSH providers, and healthcare services. Businesses were offered up to two on-site advising sessions conducted by Health Links community advisors. Advising sessions focused on reviewing results from the assessment, goal setting, and designing an action plan aimed at helping the business implement changes that addressed gaps and priority areas. Community advisors were recruited through local public health agencies and business groups and represented individuals with health education, safety, and wellness backgrounds. They were trained on the Health Links benchmarks and advising process, business consulting practices, and the TWH paradigm. Advisors were compensated as contractors for conducting outreach in their communities, recruiting businesses, and conducting in-person advising sessions. During advising sessions, advisors were trained to validate responses from the assessment prior to developing an action plan that was customized based on the priorities of the business and their employees’ needs for health and safety. The action plan provided three goals, action steps, and evidence-based resources to implement each step including connection to local health and safety service providers.
Data from three versions of the Health Links assessment were used for this study of 385 businesses. Two assessments were administered to 284 businesses from July 2013 – September 2016. One assessment included a total of 34 questions and was offered to businesses with less than 50 employees. The second assessment consisted of 38 questions and was offered to businesses of any size. In 2016, based on feedback from users and program evaluation, it was decided to create a single assessment and revise some questions. A total of 29 items from the original two assessments were used in the current version of the assessment. The final version consists of 35 questions and was completed by an additional 101 businesses between October 2016 and September 2017. The Colorado Institutional Review Board reviewed this project and determined it was not human subjects research.
Business Recruitment
Businesses were recruited through statewide and local marketing, media, and outreach. As shown in Figure 1, we developed a marketing and communications strategy aimed at forming strategic partnerships with trusted intermediary groups including chambers of commerce, economic development groups, and local public health departments. These partners disseminated information about the Health Links Assessment tool and the value of advising and certification to their members through email blasts, conferences, speaking engagements, and local news stories. The Colorado Small Business Development Center Network (SBDC) featured Health Links as a signature program and “wellness consulting” arm on its website to advertise the assessment and advising as a community resource for small businesses. In April 2015, the Colorado Governor’s Council for Healthy and Active Lifestyles began awarding an annual Governor’s Award for Worksite Wellness using Health Links certification as the eligibility criteria. Businesses were also recruited through direct and community outreach. Health Links advisors conducted outreach by attending local networking events, following up with attendees, and establishing key relationships with local coalitions and business groups. Businesses were also recruited from Oregon, Florida and California as part of separate pilots in partnership with local public health agencies and state-based workers’ compensation insurers.
In order to gain a better understanding of how finer size gradations of small businesses were implementing health and safety policies, we subclassified the businesses into four groups according to size, based on quartiles of the sample’s distribution. We formed those groups prior to conducting the analysis. For purposes of this paper, we will refer to these subgroups as microbusinesses (2–10 employees), small businesses (11–50 employees), medium-sized (51–200 employees), or large businesses (>200 employees). A single representative from each business completed the assessment online.
Measures
The assessment collected self-reported information from each organization about business demographics, leadership commitment, health promotion and safety policies and activities, communication strategies, employee reach, organizational motivation, incentives, employee benefits (healthcare, workers’ compensation, paid leave), and evaluation measures. Assessments were completed by business executives (n=145, 38%), human resource (HR) professionals (n=85, 22%), health and safety professionals (n=64, 17%), and other (n=84, 22%). These categories were defined using the BLS standard occupation classification (SOC) codes.22 Professionals in the “other” category included administrators, educators, executive assistants, and employee representatives for health and safety.
The assessment, introduced in October 2016, scored businesses across six benchmarks and recognized them at one of four levels: Kick-Start, Certified Healthy Business, Certified Healthy Business Partner or Certified Healthy Business Leader. The benchmarks measured 1) organizational support, 2) workplace assessment, 3) health policies and programs, 4) safety policies and programs, 5) engagement, and 6) evaluation. The benchmark scores were summed to create a total score, with a maximum possible score of 100. We categorized these benchmarks into two core areas for our analysis: 1) systems measures, and 2) health and safety measures (Table 1).
TABLE 1.
Measures and Scoring from Health Links Assessment. Total Possible Score = 100 pts.
|
Systems Measures (68 pts.) |
|
|
Workplace Health Measures (16 pts.) |
|
|
Workplace Safety Measures (16 pts.) |
|
|
Motivation for Health and Safety (0 pts.) |
Statistical Analysis
Analysis was performed in two parts. The first analysis was conducted among all 382 businesses using assessment responses to individual questions that were common to the two original assessments (n = 281) and the October 2016 updated assessment (n =101). Chi-square test was used to test the association between the four business size groups and their responses to the assessment measures.
The second part of our analysis utilized data from the updated assessment for 101 companies, comparing business performance on the six benchmarks described above. This group included seven microbusinesses, 23 small businesses, 30 medium sized businesses, and 41 large businesses. The total score and sub-scores for each of the benchmarks were coded for each business and were compared between the four sizes groups by ANOVA. Tukey’s Studentized Range (HSD) Test was used to test for multiple comparisons. We conducted Levene’s test for equality of variances for the benchmark scores in each businesses group. We performed Pearson correlation to assess the relationships between workplace health and safety scores.
Because a single individual from each organization completed the assessment, a sensitivity analysis was performed to determine the impact that the position of this individual had on the assessment responses. We grouped each business by the position of the individual who completed their assessment into business executive, HR professionals, health and safety professionals, and other (response group). A Chi-square test was used to determine if the proportion of each response group completing the assessment differed by business size. The sample was then stratified by size of business and Chi-square tests were used to assess if responses differed between response groups within each business size category. The primary analyses were then re-run, stratifying on response group, and compared to the original analysis. The results from this analysis are provided in the Supplemental tables.
All data analyses were performed in SAS version 9.4 (SAS Institute, Inc., Cary, NC).23
RESULTS
Demographics
The Health Links Assessment was completed by 385 businesses between July 2013 and September 2017. Three businesses did not meet inclusion criteria because they did not report business size, resulting in a total sample of 382 businesses. The range of full-time employees for large businesses was 50–27,166 (median: 417). Of those meeting inclusion criteria, 282 (74%) had fewer than 200 employees. Businesses in Colorado represented a majority of the sample, 345 (90%), with 23 (6%) in Oregon, 14 (4%) in Florida. Most participating businesses were in healthcare and social assistance (24%), services (21%), or public administration (19%) industries (Table 1). The distribution of businesses size was fairly consistent across industry. Businesses in the cohort included 197 (55%) urban, 138 (38%) rural, and 24 (7%) frontier. Rural regions contained a higher percentage of smaller businesses. In Colorado, participating companies came from 32 of 64 counties. In Oregon, participating companies came from 12 of 36 counties. Data were available for a single county in Florida. Organizations reported that 75% of their employees were full time, 19% part-time, and 5% contract. Fifty-five percent were female.
Systems Measures
When examined overall, the larger businesses demonstrated a more comprehensive approach to health and safety compared to smaller businesses (Table 3). We observed a consistent pattern in almost all survey responses, by business size category. More systematic approaches, including policies and programs aimed at supporting employee health and safety, were in place in larger businesses compared to smaller businesses.
TABLE 3.
Business Systems Supporting Workplace Health and Safety by Business Size (2013-2017).
| Program component | Micro 2-10 (N=78) |
Small 11-50 (N=133) |
Medium 51-200 (N=71) |
Large >200 (N=100) |
Total (N=382) |
Chi-squared p-value |
|---|---|---|---|---|---|---|
| Organizational Supports | ||||||
| Companywide Communications | 40 (51%) | 84 (63%) | 46 (65%) | 80 (80%) | 250 (65%) | <0.001 |
| Offer Health insurance coverage to its employees | 44 (56%) | 111 (83%) | 68 (96%) | 98 (99%) | 321 (84%) | <0.001 |
| Have worker’s compensation insurance coverage | 54 (69%) | 124 (93%) | 69 (97%) | 98 (99%) | 345 (91%) | <0.001 |
| Wellness champions | ||||||
| Senior executive (CEO, CFO, COO) | 40 (51%) | 59 (44%) | 38 (54%) | 49 (49%) | 186 (49%) | 0.599 |
| Manager | 25 (32%) | 69 (52%) | 43 (61%) | 72 (72%) | 209 (55%) | <0.001 |
| Employee | 27 (35%) | 67 (50%) | 46 (65%) | 76 (76%) | 216 (57%) | <0.001 |
| Workplace Assessment | ||||||
| Employee survey | 12 (15%) | 43 (32%) | 38 (54%) | 73 (73%) | 166 (43%) | <0.001 |
| Health risk assessment (HRA) | 13 (17%) | 33 (25%) | 30 (42%) | 81 (81%) | 157 (41%) | <0.001 |
| Physical worksite assessment | 12 (15%) | 38 (29%) | 16 (23%) | 44 (44%) | 110 (29%) | <0.001 |
| Causes of job absence | 8 (10%) | 18 (14%) | 11 (15%) | 30 (30%) | 67 (18%) | 0.002 |
| Disability claims & costs | 8 (10%) | 24 (18%) | 18 (25%) | 45 (45%) | 95 (25%) | <0.001 |
| Health care claims & costs | 9 (12%) | 31 (23%) | 30 (42%) | 79 (79%) | 149 (39%) | <0.001 |
| Workers’ compensation claims & costs | 6 (8%) | 36 (27%) | 22 (31%) | 48 (48%) | 112 (29%) | <0.001 |
| Engagement | ||||||
| Consider ethnicity, language, reading levels, age, gender or diversity of employees* | 27 (47%) | 61 (60%) | 53 (79%) | 78 (87%) | 219 (69%) | <0.001 |
| Include off-site employees’ wellness** | 17 (25%) | 41 (34%) | 34 (51%) | 65 (72%) | 157 (46%) | <0.001 |
| Incentive | ||||||
| Awards | 8 (10%) | 36 (27%) | 37 (52%) | 61 (61%) | 142 (37%) | <0.001 |
| Cash | 6 (8%) | 30 (23%) | 31 (44%) | 62 (62%) | 129 (34%) | <0.001 |
| Health insurance premiums discount | 14 (18%) | 32 (24%) | 16 (23%) | 41 (41%) | 103 (27%) | 0.002 |
| Contributions or discounts for health activities, gear, equipment | 9 (12%) | 23 (17%) | 21 (30%) | 37 (37%) | 90 (24%) | <0.001 |
| Impact | ||||||
| Health and safety program has positive impact on | ||||||
| Productivity | 24 (31%) | 53 (40%) | 36 (51%) | 55 (55%) | 168 (44%) | 0.005 |
| Employee job satisfaction | 29 (37%) | 71 (53%) | 42 (59%) | 61 (61%) | 203 (53%) | 0.009 |
| Health insurance claims & costs | 26 (33%) | 64 (48%) | 43 (61%) | 60 (60%) | 193 (51%) | 0.001 |
| Workers’ compensation claims & costs | 16 (21%) | 34 (26%) | 34 (48%) | 46 (46%) | 130 (34%) | <0.001 |
65 businesses indicated they did not have to tailor their programs, sample size was 317 for this question.
41 businesses indicated that they did not have off-site employees, sample size was 341 for this question
Organizational Supports
Overall, businesses in each size category reported senior management and employee participation in planning and programming for health and safety. Microbusinesses were less likely to provide health care insurance, whereas 277 (over 80%) of small, medium and large businesses provided some form of health care coverage to employees and in some cases, dependents (Table 3). In each instance, we observed significant greater numbers of organizational supports by business size increment. Larger businesses were more likely to report dedicated support for communications that emphasized workplace safety and health when compared to smaller businesses. They were also more likely to offer health insurance, workers’ compensation coverage, and have designated wellness champions representing senior executives, managers, and employees. Larger businesses were also more likely to report that managers and employees, not the senior executives, were the program champions for health and safety.
Workplace Assessments
The majority of businesses had made some effort to conduct some form of workplace assessment. Among all participating businesses, the most common way of conducting a workplace assessment was by an employee needs and interest survey (43%). For example, only 13 (17%) of the microbusinesses had conducted health risk assessments and only 12 (15%) of them had conducted an employee needs survey. As business size increased, attention to establishing employee needs increased as well as the methods for collecting data. The majority of large businesses reported that they had conducted and examined employee needs surveys (73%), health risk assessments (HRAs) (81%), and/or used health claim and cost data (79%) to determine the needs and interests of their employees (Table 2).
TABLE 2.
Characteristics of Health Links Participating Organizations by Business Size (2013-2017).
| Micro 2-10 (N=78) N (%) |
Small 11-50 (N=133) N (%) |
Medium 51-200 (N=71) N (%) |
Large >200 (N=100) N (%) |
Total (N=382) N (%) |
|
|---|---|---|---|---|---|
| Industry Sector | |||||
| Accommodation and Food Services | 0 (0%) | 3 (2%) | 1 (1%) | 3 (3%) | 7 (2%) |
| Agriculture, Forestry, Fishing and Hunting | 1 (1%) | 0 (0%) | 1 (1%) | 3 (3%) | 5 (1%) |
| Arts, Entertainment and Recreation | 0 (0%) | 0 (0%) | 0 (0%) | 2 (2%) | 2 (1%) |
| Construction | 2 (3%) | 7 (5%) | 4 (6%) | 4 (4%) | 17 (4%) |
| Educational Services | 1 (1%) | 5 (4%) | 1 (1%) | 4 (4%) | 11 (3%) |
| Finance and Insurance | 4 (5%) | 9 (7%) | 0 (0%) | 6 (6%) | 19 (5%) |
| Healthcare and Social Assistance | 23 (29%) | 32 (24%) | 15 (21%) | 22 (22%) | 92 (24%) |
| Information | 1 (1%) | 1 (1%) | 0 (0%) | 0 (0%) | 2 (1%) |
| Manufacturing | 0 (0%) | 2 (2%) | 6 (8%) | 1 (1%) | 9 (2%) |
| Mining, Oil and Gas Extraction | 0 (0%) | 1 (1%) | 0 (0%) | 0 (0%) | 1 (0%) |
| Public Administration | 12 (15%) | 25 (19%) | 10 (14%) | 26 (26%) | 73 (19%) |
| Real Estate, Rental and Leasing | 1 (1%) | 1 (1%) | 1 (1%) | 2 (2%) | 5 (1%) |
| Retail/ Wholesale Trade | 3 (4%) | 3 (2%) | 8 (11%) | 1 (1%) | 15 (4%) |
| Services | 24 (31%) | 29 (22%) | 12 (17%) | 15 (15%) | 80 (21%) |
| Transportation, Warehousing and Utilities | 0 (0%) | 2 (2%) | 3 (4%) | 4 (4%) | 9 (2%) |
| Other | 6 (8%) | 13 (10%) | 9 (13%) | 7 (7%) | 35 (9%) |
| Business Location* | |||||
| Urban | 35 (45%) | 62 (48%) | 45 (64%) | 70 (72%) | 212 (57%) |
| Rural | 36 (47%) | 57 (44%) | 20 (29%) | 25 (26%) | 138 (37%) |
| Frontier | 6 (8%) | 11 (8%) | 5 (7%) | 2 (2%) | 24 (6%) |
| Employment Type | |||||
| Full time | 336 (70%) | 2764 (76%) | 5765 (84%) | 126293 (75%) | 135158 (75%) |
| Part time | 77 (16%) | 612 (17%) | 796 (12%) | 33275 (20%) | 34760 (19%) |
| Contract | 70 (14%) | 249 (7%) | 344 (5%) | 9080 (5%) | 9743 (5%) |
| Employee Sex | |||||
| Male | 185 (38%) | 1595 (44%) | 3621 (53%) | 75810 (45%) | 81211 (45%) |
| Female | 298 (62%) | 2058 (56%) | 3207 (47%) | 92706 (55%) | 98269 (55%) |
8 businesses did not indicate their business location, sample size was 374 for this piece of information
Engagement
Most of the large businesses (87%) tailored existing health and safety education and program materials based on the backgrounds of employees such as literacy levels, languages, and education (Table 2). Microbusinesses were much less likely to include offsite employees in their health and safety programs compared to large businesses (25% vs. 72%, p <0.001). More than 60% of the large businesses reported that they offered incentives in the form of awards or cash to increase employee participation. Small and microbusinesses were much less likely to offer incentives.
Perceived Impact
One question, consisting of multiple response options, assessed the perceived impact of workplace health and safety efforts on business and worker outcomes. Among large businesses, approximately half indicated that their health and safety programs have an impact on employee productivity (55%), achieving employee job satisfaction (61%), and lowering health insurance (60%) and workers’ compensation costs (46%). However, fewer than half of the microbusinesses held this view. In general, businesses of all sizes were similar in their impact metrics, with the notable exception of microbusinesses. Only 24 businesses (31%) responded that they believe health and safety efforts have a positive impact on employee productivity. A smaller number of small and microbusinesses reported a positive impact of health and safety programming on workers’ compensation claims and costs.
Workplace Health and Safety Measures
As shown in Table 4, when considered overall, large businesses were more likely to report having specific policies and programs in place for both health and safety, compared to smaller businesses. We observed statistically significant, incremental increases in the level of safety as well as the level of health promotion practices based on business size.
TABLE 4.
Business Workplace Health and Safety Policies and Programs by Business Size (2013-2017).
| Assessment Component | Micro 2-10 (N=78) |
Small 11-50 (N=133) |
Medium 51-200 (N=71) |
Large >200 (N=100) |
Total (N=382) |
Chi-squared p-value |
|---|---|---|---|---|---|---|
| Safety | ||||||
| Changed the way we work to reduce injuries | 26 (33%) | 62 (47%) | 42 (59%) | 80 (80%) | 210 (55%) | <0.001 |
| Engineering controls | 27 (35%) | 72 (54%) | 47 (66%) | 79 (79%) | 225 (59%) | <0.001 |
| Administrative controls | 34 (44%) | 69 (52%) | 45 (63%) | 84 (84%) | 232 (61%) | <0.001 |
| Provided Personal Protective Equipment | 19 (24%) | 63 (47%) | 47 (66%) | 91 (91%) | 220 (58%) | <0.001 |
| Written accident prevention plan | 10 (13%) | 54 (41%) | 32 (45%) | 68 (68%) | 164 (43%) | <0.001 |
| Conducted ergonomic assessment | 14 (18%) | 31 (23%) | 26 (37%) | 76 (76%) | 147 (38%) | <0.001 |
| Limited amount of time workers perform repetitive tasks | 14 (18%) | 21 (16%) | 16 (23%) | 31 (31%) | 82 (21%) | 0.036 |
| Modified workstations or work tasks | 14 (18%) | 41 (31%) | 40 (56%) | 67 (67%) | 162 (42%) | <0.001 |
| Plan for disaster and emergency preparedness | 30 (38%) | 86 (65%) | 52 (73%) | 93 (93%) | 261 (68%) | <0.001 |
| Health | ||||||
| Tobacco Control | 16 (21%) | 44 (33%) | 35 (49%) | 81 (81%) | 176 (46%) | <0.001 |
| Written policy | 9 (12%) | 32 (24%) | 23 (33%) | 52 (52%) | 116 (30%) | <0.001 |
| Ban tobacco use | 8 (10%) | 21 (16%) | 14 (20%) | 27 (27%) | 70 (18%) | 0.028 |
| Education | 4 (5%) | 16 (12%) | 19 (27%) | 61 (61%) | 100 (26%) | <0.001 |
| Refer employees to quit lines | 6 (8%) | 23 (17%) | 21 (30%) | 65 (65%) | 115 (30%) | <0.001 |
| Nutrition | 23 (29%) | 53 (40%) | 48 (68%) | 81(81%) | 205 (54%) | <0.001 |
| Written policy | 3 (4%) | 7 (5%) | 12 (17%) | 23 (23%) | 45 (12%) | <0.001 |
| Provide nutritional info | 11 (14%) | 30 (23%) | 25 (35%) | 54 (54%) | 120 (31%) | <0.001 |
| Healthy vending options | 9 (12%) | 23 (17%) | 30 (42%) | 51 (51%) | 113 (30%) | <0.001 |
| Provide education | 9 (12%) | 28 (21%) | 29 (41%) | 59 (59%) | 125 (33%) | <0.001 |
| Mental Health | 16 (21%) | 47 (35%) | 44 (62%) | 88 (88%) | 195 (51%) | <0.001 |
| Free or subsidized clinical screening | 3 (4%) | 14 (11%) | 16 (23%) | 47 (47%) | 80 (21%) | <0.001 |
| Self-assessment tools | 2 (3%) | 9 (7%) | 16 (23%) | 38 (38%) | 65 (17%) | <0.001 |
| Provide educational materials | 6 (8%) | 21 (16%) | 23 (32%) | 64 (64%) | 114 (30%) | <0.001 |
| Free or subsidized counseling | 8 (10%) | 20 (15%) | 23 (32%) | 64 (64%) | 115 (30%) | <0.001 |
| Physical Activity | 29 (37%) | 76 (57%) | 55 (77%) | 90 (90%) | 250 (65%) | <0.001 |
| Free or subsidized cost of off-site | 8 (10%) | 37 (28%) | 37 (52%) | 65 (65%) | 147 (38%) | <0.001 |
| Group programs | 15 (19%) | 39 (29%) | 33 (46%) | 66 (66%) | 153 (40%) | <0.001 |
| Stress Management | 23 (29%) | 57 (43%) | 46 (65%) | 89 (89%) | 215 (56%) | <0.001 |
| Stress relief therapies (yoga, message, therapists) | 13 (17%) | 24 (18%) | 23 (32%) | 57 (57%) | 117 (31%) | <0.001 |
| Financial advising | 9 (12%) | 26 (20%) | 34 (48%) | 65 (65%) | 134 (35%) | <0.001 |
| Family counseling | 6 (8%) | 19 (14%) | 26 (37%) | 62 (62%) | 113 (30%) | <0.001 |
| Disease Prevention | 15 (19%) | 38 (28%) | 36 (51%) | 79 (79%) | 168 (44%) | <0.001 |
| Provide communication and education | 5 (6%) | 24 (18%) | 15 (21%) | 60 (60%) | 104 (27%) | <0.001 |
| Provide free or subsidized health screening | 5 (6%) | 25 (19%) | 26 (37%) | 71 (71%) | 127 (33%) | <0.001 |
Safety Policies and Programs
Overall, 210 (55%) of the businesses responded that their organization had changed the way it worked to reduce injuries during the last year, especially in larger companies. Microbusinesses were significantly less likely to have established safety policies, programs and practices, compared with larger enterprises. For example, among microbusinesses, only 19 (24%) provided personal protective equipment compared to 91 (91%) of large business (p < 0.001). Only 30 (38%) of the microbusinesses had plans for disaster and emergency preparedness, compared to 93 (93%) of the large businesses (p < 0.0001). Engineering controls and emergency preparedness were both more common among the small and medium-sized businesses. Of the large businesses, 79% had implemented engineering controls, 84% had administrative controls for safety, and 91% provided personal protective equipment. Among available strategies to address safety, businesses of all sizes were least likely to report that they limit the amount of time workers performed repetitive tasks.
Health Policies and Programs
Overall, the top three areas that businesses indicated for the health policies and programs benchmark were physical activity (65%), stress management (56%), and nutrition (54%). Less than half of the 382 businesses indicated they had a disease prevention and management program. Fewer than half of businesses implemented tobacco control programs (176, 46%).
Similar to what we observed for safety, health policies and programs showed significant and incremental score increases based on business size. For example, more than 80% of large businesses implemented tobacco control, nutrition, mental health, physical activity and stress management programs. Seventy-nine percent of the large businesses focused on disease prevention through communication, education and providing free or subsidized screenings. Sixty-one percent of large businesses provided education on tobacco control and 65 (65%) referred employees to quit lines. Sixty-four (64%) large businesses offered free or subsidized counseling on mental health. Smaller businesses indicated they were doing less to promote healthy behaviors and prevent chronic disease. Among microbusinesses, 23 (29%) had programs addressing nutrition, 29 (37%) implemented programs to promote physical activity and 23 (29%) reported stress management programs. Few had addressed tobacco control (21%), mental health (21%) or disease prevention (19%). Among microbusiness groups, only 8 (10%) provided free or subsidized counseling for employees compared to 64 (64%) of large businesses (p < 0.001). There was also a large gap in efforts to prevent chronic disease based on business size. Seventy-one (71%) large businesses provided free or subsidized health screening to their employees to prevent chronic disease, compared to only five (6%) of microbusiness (p <0.001).
Motivation underlying organizational commitment to health and safety
As shown in Table 5, of the 101 businesses that were offered this question, 99 (98%) said they were motivated by the desire to improve the health of their employees and their employees’ families; 82 (81%) were motivated to improve employee morale; 78 (77%) were interested in enhancing productivity; 64 (63%) wanted to contain costs; 60 (59%) wanted to decrease absenteeism, and 81 (80%) wanted to improve employee retention. Among large businesses, motivations were evenly distributed. Small businesses, especially the microbusinesses, were less likely to report being motivated to have health and safety programs in order to decrease absenteeism and contain costs, compared to large businesses. The most common motivations for small and microbusinesses were to improve the health of employees and their families and to improve employee morale.
TABLE 5.
Business Motivation Underlying Organizational Commitment to Health and Safety by 1) Business Size and 2) Who Completed the Assessment.
| Business Size |
Who Completed the Assessment |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Motivation | Micro 2-10 (N=7) |
Small 11-50 (N=23) |
Medium 51-200 (N=30) |
Large >200 (N=41) |
Chi- square p-value |
Executive (N=22) |
HR (N=36) |
Health and Safety Professional (N=20) |
Other (N=23) |
Chi- square p-value |
Total (N=101) |
| Improve the health of employees and their families | 7 (100%) | 21 (91%) | 30 (100%) | 41 (100%) | 0.075 | 21 (95%) | 36 (100%) | 20 (100%) | 22 (96%) | 0.47 | 99 (98%) |
| Improve the employee morale | 5 (71%) | 16 (70%) | 26 (87%) | 35 (85%) | 0.317 | 16 (73%) | 32 (89%) | 17 (85%) | 17 (74%) | 0.33 | 82 (81%) |
| Enhance productivity | 4 (57%) | 15 (65%) | 24 (80%) | 35 (85%) | 0.16 | 14 (64%) | 31 (86%) | 17 (85%) | 16 (70%) | 0.15 | 78 (77%) |
| Contain costs | 2 (29%) | 11 (48%) | 15 (50%) | 36 (88%) | < 0.001 | 8 (36%) | 29 (81%) | 16 (80%) | 11 (48%) | 0.001 | 64 (63%) |
| Decrease absenteeism | 2 (29%) | 8 (35%) | 19 (63%) | 31 (76%) | 0.004 | 10 (45%) | 25 (69%) | 13 (65%) | 12 (52%) | 0.26 | 60 (59%) |
| Increase employee retention | 4 (57%) | 17 (74%) | 25 (83%) | 35 (85%) | 0.285 | 15 (68%) | 32 (89%) | 17 (85%) | 17 (74%) | 0.21 | 81 (80%) |
Composite Scores for Six Benchmarks
Total scores increased incrementally by business size category. The maximum achievable total score was 100. The mean total score among microbusinesses was 33 (SD: 17, Range: 11–58), among businesses with 11–50 employees the mean was 47 (SD: 14, Range: 20–69); in businesses with 51–200 employees, the mean score was 47 (SD: 13, Range: 25–71); and for the businesses > 200 employees, the mean score was 63 (SD: 16, Range: 30–88). The total scores were statistically significant associated with business size (p<0.001).
Figure 2 compares scores in each of the six benchmarks across the four businesses groups based on size. The mean scores for each of the benchmarks were statistically significant associated with business sizes: organizational support (p=0.003); workplace assessments (p <0.001); engagement (p=0.004); evaluation (p<0.001); health policies and programs (p<0.001); safety policies and programs (p<0.001). Although participating businesses of all sizes had similar scores for organizational support, we observed that businesses scored significantly better as the number of employees increased (p<0.05).
FIGURE 2.
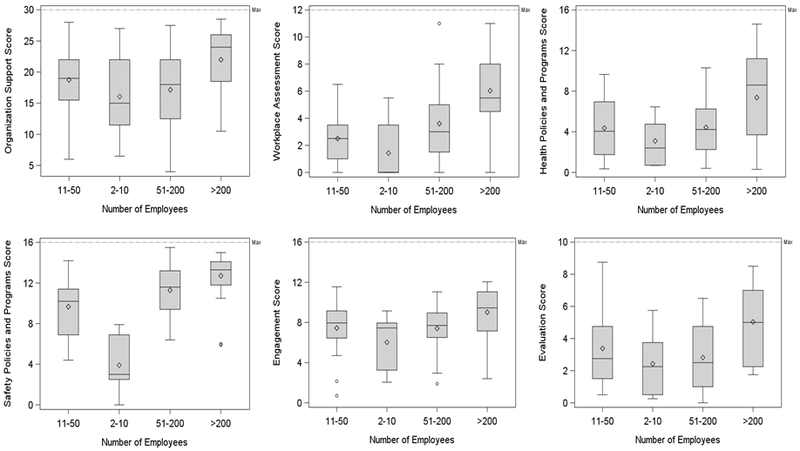
Distribution of each benchmark score by business size group.
We observed a wide range of scores, regardless of business size. The variance of scores in health promotion policies differed significantly across the four business groups (p < 0.001). There was no statistically significant difference in the degree of variance of scores for the other five benchmarks. Although large enterprises had the highest mean scores for all six benchmarks, no organization achieved a maximum score in any of the categories.
Comparison of Health and Safety Scores
We hypothesized that businesses that address workplace safety would be more likely to also address health promotion, regardless of business size. Figure 3 illustrates the correlation between safety and health promotion benchmarks for the 101 businesses. We observed a moderate correlation between these benchmarks, with higher scores of safety programs tending to be associated with higher scores in health promotion programs (r=0.45). We observed that microbusinesses’ safety and health policies and programs are well-correlated (r =0.78, p =0.04). Small businesses showed no statistically significant correlation between health and safety benchmarks (r =0.35, p=0.10). The small business group scored better for safety compared to the microbusinesses, but scored lower than large businesses in health policies and programs. We observed no correlation between health and safety policies and practices in the medium-sized business group (r =−0.001, p=0.99). This group had higher safety scores than smaller businesses but proved comparable in health policies and programs. We observed a moderate correlation between benchmarks for the large businesses overall (r = 0.57, p <0.001). Large businesses scored highest on both benchmarks, clustering into two groups: those with high scores for both benchmarks and those with strong safety scores but weaker health policies and programs scores.
FIGURE 3.
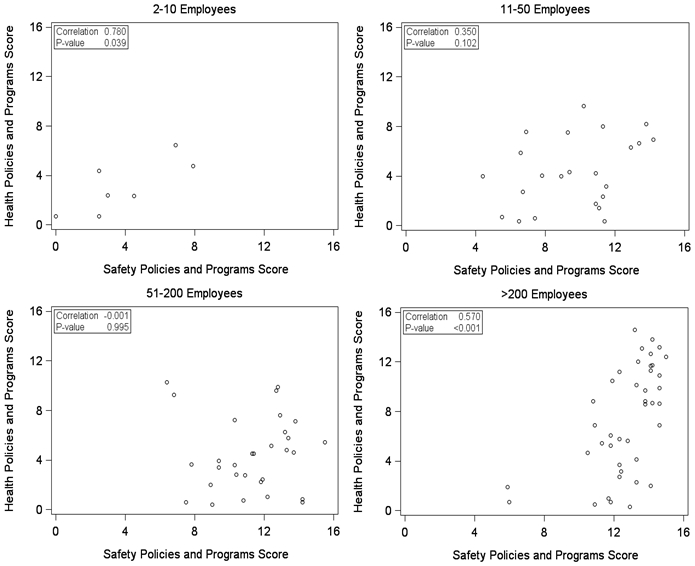
Correlation between health and safety benchmark scores by business group size.
Impact of Survey Respondent on Results
A sensitivity analysis was conducted to determine if business size was acting as a proxy for who in the organization completed the assessment. The distribution of response group was compared between business size and showed a statistically significant difference (p-value < 0.001). In microbusinesses, 43 (55%) of the assessments were completed by executives, and no assessments were completed by HR. On the other hand, most assessments from large business’ were completed by either HR (43, 43%) or health and safety professionals (35, 35%). These results are summarized in Table 6.
TABLE 6.
The Survey Respondent by Business Size (2013-2017).
| Program component |
Micro 2-10 (N=78) |
Small 11-50 (N=133) |
Medium 51-200 (N=71) |
Large >200 (N=100) |
Total (N=382) |
|---|---|---|---|---|---|
| Positions | |||||
| Executive | 43 (55%) | 49 (37%) | 13 (18%) | 12 (12%) | 117 (31%) |
| HR | 0 (0%) | 17 (13%) | 25 (35%) | 43 (43%) | 85 (22%) |
| Health and Safety Professionals | 6 (8%) | 14 (11%) | 8 (11%) | 35 (35%) | 63 (16%) |
| Others | 29 (37%) | 53 (40%) | 25 (35%) | 10 (10% ) | 117 (31%) |
Chi-square test p-value: <0.001
When stratified by business size, we observed no significant difference in the responses to the assessment between response groups. This held for all business size categories. When stratified by the response group, we found significant differences in responses between business size categories, however certain trends were no longer present. For example, the difference in responses between microbusinesses and large businesses found in the original analysis held after controlling for response group, but there was no longer a significant difference between medium and large businesses.
Of note, motivation differed between respondent groups. Executives indicated that the primary motivations were to improve health of their employees and families. However, when the assessment was completed by an HR representative, the motivations were more evenly distributed. Cost containment was a motivation for 29 (81%) businesses when an HR representative filled out the survey compared with only 8 (36%) when executives completed the assessment (p-value=0.02). These results are provided in the Supplemental tables.
DISCUSSION
This is the first study to identify significant differences in TWH adoption and approaches based on business size, revealing notably different patterns of organizational behavior even within the general classification of “small business”. Our results indicate a need for intervention research that specifically targets microbusinesses and small businesses, especially in light of the outsized health and safety risks encountered in these sectors of the economy. This study has potentially broad applicability. It is the largest of its kind to date to examine comprehensive TWH policies and practices in small businesses spanning a range of sectors across rural and urban geographical areas and in multiple states. Importantly, it offers the first systematic look at TWH behavior of microbusiness. Previous research has focused primarily on single intervention studies with small samples comprised of large businesses.
Small vs. Large.
Business size matters. Larger businesses were more likely to score higher across each Health Links benchmark, suggesting that they are taking a more systematic and comprehensive approach to addressing health promotion and safety. Although we observe that larger businesses have implemented more comprehensive health and safety strategies in their workplaces, there is significant room for improvement across the board. Our findings show that smaller businesses, especially microbusinesses, are less likely to have organizational supports, data collection methods for informing employee needs and interests, or integrated health and safety strategies. Large businesses report doing more to address chronic disease prevention including tobacco cessation, nutrition, physical activity and stress management efforts aimed at improving employee health behaviors, consistent with what has been found in other studies of large enterprises.2 Micro and small businesses are doing significantly less across all of the health promotion and safety areas we assessed. Smaller businesses also report slightly different motivations for their commitment to health and safety compared to larger enterprises, including a desire to improve employee health, morale, productivity and retention.
This study provides an intriguing insight into the way in which responsibility for TWH practices may be distributed by business size, based on who completed the Health Links assessment. Businesses with less than 50 employees had an executive complete the assessment (31%) compared to only 3% of large businesses. Large businesses were more likely to have someone from HR or in Health and Safety designated to complete the assessment. This suggests that the responsibility for health and safety is different between small and larger businesses and that the person delegated to leading and reporting TWH efforts is directed by organizational structure. Interestingly, our data suggest that with delegation comes a difference in the motivation for TWH programming, with HR managers respondents indicating a greater interest in return on investment and executive respondents reporting a greater interest in value of investment, i.e. health and safety of employees and families.
Our findings have significant implications for how researchers should design interventions if they hope to meet the diverse needs of small businesses. We agree with Cunningham et al that there are many other factors, besides employee number, that may influence adoption of occupational health and safety practices in small and medium size businesses.24 However, our data suggest that using size alone is a strong marker of level of adoption. Furthermore, our data suggest that conventional definitions of small business will fail to identify important differences in the OSH and TWH needs of these organizations. Future research should use finer size gradations to avoid missing potentially important differences in small business OSH behavior, performance, and response to interventions.
Across the board, we observed that the businesses rarely assess their workforces’ needs to determine TWH program implementation. In addition, they infrequently evaluate the effectiveness of their programs. The failure to use data to inform health and safety program decisions may place them at risk of implementing programs that may be irrelevant to the health, safety, and well-being of their employees and may waste time, money and resources. Researchers and practitioners who design interventions intended to promote health, safety and well-being should emphasize the need for data-driven decision making.
Relationship between health promotion and health protection.
Our findings show that there is generally a consistent relationship between what organizations offer for health promotion and for safety, with some noteworthy exceptions. In the full model, health promotion scores were significantly correlated with safety scores. We found that having more employees (51–200 and >200 employees) was significantly associated with increased safety. However, we also observed that large businesses fall into two categories: 1) high in health promotion and safety, and 2) high in safety but low in health promotion. Small businesses are lower in both areas and, interestingly, the microbusinesses, like a subset of large businesses, showed better correlations between safety and health promotion benchmarks. These findings suggest three conclusions. When working with larger employers, researchers, consultants, and practitioners who are introducing TWH concepts are likely to find some enterprises that have silos of health promotion and safety in their organizations, and others that have either intentionally or organically adopted a more coordinated health promotion and health protection strategy. Secondly, microbusinesses are likely to have an affinity for taking an integrated, TWH approach. We speculate that as those businesses grow, we may be able to help them continue with an integrated approach and avoid silos of health and safety, as discussed below. Third, we have the greatest opportunity to make gains in both safety and health of workers by working with micro- and small enterprises.
Our findings regarding the importance of size and presence of health promotion and safety echo other findings in the literature on health and safety practices. 3, 25 We found large variation in scores in the smaller businesses and weaker correlations between health promotion and safety. This may be because not all workplaces are mandated to have safety activities as a regulatory requirement of the U.S. Occupational Safety and Health Administration (OSHA). Health promotion or wellness activities remain largely voluntary for most employers. Interestingly, among the medium size businesses, we did not observe a correlation between health promotion and safety. From this group, we’ve learned that there is a range of strategies for implementing TWH. These businesses scored higher than smaller businesses for safety and workplace assessment but were similar to the smaller businesses in how they scored for organizational supports and health promotion.
Microbusinesses.
This is the first study to inventory the TWH behaviors of businesses with 2–10 employees (n=70). We learned that their approach to TWH programming differs from their larger counterparts. On average, these businesses scored lower in each of the six benchmarks, although not significantly. They indicated strong organizational supports, which reflect the commitment and unique position microbusiness leaders have to implementing TWH. Across the spectrum of health promotion practices, the participating microbusinesses addressed a number of different areas from tobacco control to stress management, but still show room for improvement when it comes to how they implement comprehensive strategies to educate workers and prevent work-related injuries and illnesses. Overall, they tend to focus on a single activity, such as providing nutritional education or group physical activity programs. Our findings suggest there is a big gap in what microbusinesses are doing for safety. This suggests that their appetite for health promotion may offer an opportunity to simultaneously introduce safety knowledge and behavior change to microbusinesses through programs like Health Links. It is also particularly noteworthy that microbusinesses fall short in the area of program evaluation. Instruction and practical tools for self-assessment of TWH programming are needed for these microbusiness employers.
Our finding of differences in TWH uptake at the microbusiness level raises many important questions for future research. Do microbusinesses face common barriers that may be overcome with better awareness and guidance? Is the agility typically associated with microbusinesses a potential asset when it comes to making decisions to adopt TWH? Because the person who is responsible for health and safety may be the owner and main decision maker in these organizations, can leadership training that targets culture change improve TWH in microenterprises?
Motivation for Health and Safety.
We observed significant differences in the motivations for implementing health and safety based on business size. Our results suggest that while all of the participating businesses are motivated to address worker health and safety, there are a variety of reasons and drivers for implementing and supporting TWH. The perceived benefits we measured showed that the larger the business, the more driven they are to invest in TWH for improving productivity and lowering health care and workers’ compensation costs. The argument could be made that smaller businesses may not be as concerned with lowering insurance premiums because they are less likely to offer these benefits, however the vast majority (81%) of our sample offered health care coverage for their employees and dependents. While there were differences between perceived benefits of implementing health and safety by business size, overall, all businesses indicate their first priority is improving the health, safety and well-being of their employees and their families. We also found that motivation differs across positions in the organization. Executives may express more altruistic reasons for investing in TWH because they are responsible for leading a vision and mission for health and safety. Human resource professionals expressed motivations related to costs and other hard outcomes, possibly because they are responsible for reporting on these factors and might be held accountable for calculating a return on investment for TWH programs. These results can be useful in crafting communication strategies to increase adoption of TWH in small businesses and with targeted messages for different stakeholders within businesses.
Dissemination.
Although it was not the central purpose of this study, our research suggests that it is feasible to attract large numbers of diverse small enterprises to adopt TWH precepts. Health Links attracted 385 businesses from a range of sectors, geographic areas, and states, proving reach and ease of adoption for businesses of all sizes. The successful uptake of Health Links has implications for practice and for research. Health Links has proven to be a successful approach to generate a study cohort, notably including hard-to-engage microbusinesses. We are capitalizing on this approach to building small business cohorts in our Small + Safe + Well Study. 7 From a practice perspective, it will be important for us to more fully evaluate why Health Links appeals to small enterprises, including the messaging, the perceived value of advising, certification, the self-assessment tool, and the access to resources. More dissemination and implementation work is warranted to understand what channels are best to use to reach small employers. Defining, messaging, and evaluating the value proposition for small businesses is crucial to adoption, implementation, impact and sustainability. Anecdotally, small employers report that they are motivated more by so-called “value of investment” (VOI) measures including improving employee health and well-being, improving productivity, lowering rates of absenteeism, and enhancing employee morale, rather than traditional return-on-investment. Future research should identify new outcomes to broaden the scope of how we define and measure VOI in small enterprise. Perceived benefits of TWH on productivity, recruitment, turnover, meaningfulness of work, and health and safety culture warrant further investigation to determine why certain interventions work and how they are implemented based on the context of the business as we described above. Future longitudinal research is also needed to assess whether interventions, such as Health Links, improve small business safety and health practices over time.
Contextual Factors.
Prevailing models of occupational safety and health and of TWH suggest that our ambitions to improve worker health, safety, and well-being should take into considering the broader context of social, organizational, and individual level influences. 7, 26 At the organizational level, there are many business characteristics that need to be considered to explain the differences our results show between TWH adoption and business size. Factors such as business structure, age and maturity of the enterprise, organization of work, wages, provision of employee benefits including health care, characteristics of the workforce including reliance on seasonal, part-time, and/or subcontract workers, management and leadership, social environment and climate of the organization, access to financial and other resources, and support in the business community including intermediary organizations, among others are likely to influence how businesses decide to implement TWH. 7, 24, 27 Unfortunately, few studies have examined these and other contextual factors affecting our understanding of TWH in small businesses.12
Opportunities for improvement in both small business safety and well-being.
Broadly speaking, we found that even well-intentioned small businesses that had volunteered to participate in Health Links fell short in organizational level adoption of safety and health promotion practices. As shown in Figure 2, safety as well as health promotion programming varied widely, even among businesses with >200 employees, although larger businesses generally did better in both arenas. Our findings point to the need to understand why smaller businesses are doing less. Previous research has identified the significant challenges small businesses face including lack of knowledge, costs, access to resources, training, and other perceived and real barriers.15, 16 Especially considering the differences we observed in microbusinesses, future research is needed to identify interventions that have reach, efficacy, adoption, implementation, and sustainability.17 Future research should be designed to identify and overcome common barriers and also leverage unique advantages these businesses have to implementing TWH. Evidence illustrates that there are leverage points in complex systems, such as an organization, where implementing even a small shift can produce large change.28 Given the level of engagement that we observed among business owners, future small business studies should leverage the influence that leadership and management have in these organizations to set goals, dedicate resources, and prioritize strategies for TWH.
Limitations.
It is important to acknowledge a number of limitations of our study. First, participating businesses chose to participate in Health Links. As such, self-selection bias is likely. If these self-selected businesses are more aware of TWH principles and practices than other small enterprises, we would speculate that the larger universe of small businesses probably do even less to address TWH than the 382 businesses described here. Since the assessment was a self-administered survey, reporting bias and response bias are likely. To mitigate these forms of bias, we validated many of the survey question responses during one-on-one in-person advising sessions conducted by trained Health Links advisors. Qualitatively, we observed that smaller businesses tended to underreport. They may be doing more than they actually took credit for on the assessment, potentially underestimating the extent of TWH adoption.
One form of information bias that should be acknowledged is that a single representative from the company fills out the Health Links assessment. The position of the person who completed the Health Links assessment varied, based on the organization’s size. Our sensitivity analyses demonstrated that the position of the person who completed the assessment is highly correlated with business size, but that business size category drove the incremental differences observed.
Nonetheless, future studies should consider potential information bias even when using a single, consistent category of company representative to complete such assessments. While the assessments were an effective tool to collect measures across multiple domains of workplace health and safety policies and programs, we still lack information on some of the contextual factors existing in organizations that we’ve discussed above. Our design was cross sectional. We don’t know the history of participating organizations’ health promotion and safety activities prior to enrollment. Longitudinal research designs are needed to understand how an organization’s past experiences with TWH adoption, and factors, such as their economic growth, impact occupational safety and health practices.
Our survey instrument measures organizational level factors contributing to TWH. At this time, we do not have employee-level data on worker health and safety outcomes or perceptions of climate, although research that relates organization to individual worker level outcomes is ongoing. 7 We also do not have information regarding the ethnic, racial, socioeconomic or other forms of diversity of the workforces in participating businesses. There has been little research on this subject in the context of TWH and warrants future investigation in the small business sector.
While we did not reach all industry sectors, we have a broad representation across multiple industries compared to prior studies in the field. Although results from our cohort are more generalizable than results of studies of single worksites or single industries, future research will be needed to broaden the array of small enterprises. A number of important sectors remain underrepresented both in our cohort of businesses and in the TWH literature, including mining and extraction, agriculture, forestry, and fishing, transportation, and others well known to include a high proportion of small enterprises. We did not observe significant differences in TWH organizational behaviors across multiple sectors, however more research is needed to understand the potential interplay of industrial sector and TWH adoption.
CONCLUSIONS
In conclusion, small businesses are variably implementing TWH, and the level of implementation differs by business size. Practical interventions, as well as dissemination/implementation research should take business size into account to ensure TWH is both effective and sustainable in meeting the needs of employees. Future research is needed to understand what community, organizational, leadership, and individual factors drive the most change for improving employee health, safety, and well-being outcomes.
Supplementary Material
Acknowledgements:
The authors wish to acknowledge Pinnacol Assurance for their support of the Health Links program. Additional funding for this study was provided in part by NIOSH T42 OH009449 Mountain and Plains Education and Research Center.
Funding: Funding for this study was provided in part by the Grant or Cooperative Agreement Number, U19OH011227, funded by the Centers for Disease Control and Prevention.
Footnotes
Institution at which the work was performed
Colorado School of Public Health, University of Colorado Denver, Anschutz Medical Campus
Institution and Ethics approval and informed consent: Ethics review and exemption for our evaluation of these data was received from the Colorado Multiple Institution Review Board (COMIRB).
Disclosure (Authors): The authors declare no conflicts of interest.
Disclaimer: None
REFERENCES
- 1.SBA Office of Advocacy. United States Small Business Profile, 2016. Available at: https://www.sba.gov/sites/default/files/advocacy/United_States.pdf. Accessed August 30, 2018.
- 2.Anger WK, Elliot DL, Bodner T, et al. Effectiveness of Total Worker Health interventions. Journal of Occupational Health Psychology. 2015, 20(2), 226–247. [DOI] [PubMed] [Google Scholar]
- 3.McLellan DM, Caban-Martinez A, Nelson CC, et al. Organizational characteristics influence implementation of worksite health protection and promotion programs: Evidence from smaller businesses. J Occup Environ Med. 2015, 57(9):1009–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sinclair RC, Cunningham TR, & Schulte PA. A model for occupational safety and health intervention diffusion to small businesses. Am J Ind Med. 2013, 56(12), 1442–1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Newman LS, Stinson KE, Metcalf D, et al. Implementation of a worksite wellness program targeting small businesses: The Pinnacol Assurance Health Risk Management Study. J Occup and Environ Med. 2015; 57(1), 14–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schwatka NV, Atherly A, Dally MJ, et al. Health risk factors as predictors of workers’ compensation claim occurrence and cost. Occupational and Environmental Medicine.2016; 74(1), 14–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schwatka NV, Tenney L, Dally MJ, et al. Small business total worker health: a conceptual and methodological approach to facilitating organizational change. Occup Health Sci. 2018; 2(1), 25–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Merrill RM A small business worksite wellness model for improving health behaviors. Journal of Occupational and Environmental Medicine. 2013; 55(8), 895–900. [DOI] [PubMed] [Google Scholar]
- 9.Sorensen G, Barbeau E, Stoddard A, Hunt M, Kaphingst K, & Wallace L. Promoting behavior change among working-class, multiethnic workers: Results of the healthy directions—Small business study. American Journal of Public Health. 2005; 95(8), 1389–1395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.NIOSH. 2017. What is Total Worker Health? Available at: https://www.cdc.gov/niosh/twh/default.html. Accessed August 30, 2018
- 11.Institute of Medicine. 2014. Promising and best practices in total worker health: workshop summary. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- 12.Feltner C, Peterson K, Weber RP, et al. The effectiveness of Total Worker Health interventions: A systematic review for a National Institutes of Health Pathways to Prevention Workshop. Annals of Internal Medicine. 2016; 1–24. [DOI] [PubMed] [Google Scholar]
- 13.Bradley CJ, Grossman DC, Hubbard RA, Ortega AN, & Curry SJ. Integrated interventions for improving Total worker health: A panel report from the National Institutes of Health pathways to prevention workshop: Total worker health—What’s work got to do with it? Annals of Internal Medicine. 2016; 1–7. [DOI] [PubMed] [Google Scholar]
- 14.Pronk NP. Integrated worker health protection and promotion programs: overview and perspectives on health and economic outcomes. Journal of occupational and environmental medicine/American College of Occupational and Environmental Medicine. 2013; 55(12 0), S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McCoy K, Stinson K, Scott K, Tenney L, Newman LS. Health promotion in small business: a systematic review of factors influencing adoption and effectiveness of worksite wellness programs. J Occup Environ Med, 2014. 56(6): p. 579–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Linnan L, Bowling M, Childress J, et al. Results of the 2004 national worksite health promotion survey. American Journal of Public Health. 2008; 98(8), pp.1503–1509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Glasgow R, Vogt T, & Boles S. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. American Journal of Public Health.1999; 89(9), 1322–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Health Links Certified. (2018). Available at: https://www.healthlinkscertified.org/ Accessed August 30, 2018
- 19.Centers for Disease Control. (2015). Worksite health scorecard. Available at: http://www.cdc.gov/dhdsp/pubs/worksite_scorecard.htm. Accessed August 30, 2018
- 20.CDC - National Institute for Occupational Safety and Health. CDC - NIOSH Total Worker Health. 2018. Available at: https://www.cdc.gov/niosh/TWH/. Accessed August 30, 2018
- 21.WHO: World Health Organization, World Health Organization. WHO ∣ Healthy workplaces: a WHO global model for action. 2018. Available at: http://www.who.int/occupational_health/healthy_workplaces/en/ Accessed August 30, 2018
- 22.United States Bureau of Labor Statistics. Standard Occupational Classfication. 2018 SOC System. Available at: https://www.bls.gov/soc/2018/home.htm. Accessed August 30, 2018
- 23.SAS version 9.4. SAS Institute Inc., Cary, NC, 2013 [Google Scholar]
- 24.Cunningham TR, Sinclair R, & Schulte P Better understanding the small business construct to advance research on delivering workplace health and safety. Small Enterprise Research.2014; 21(2), 148–160. [Google Scholar]
- 25.Sinclair RC, Cunningham TR. Safety activities in small businesses. Safety Sci 2014; 64:32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burke MJ, Signal SM. Workplace safety: A multilevel, interdisciplinary perspective. Research in Personnel and Human Resources Management. 2010;29:1–47. [Google Scholar]
- 27.Harris JR, Hannon PA, Beresford SAA, Linnan LA, & McLellan DL. Health promotion in smaller workplaces in the United States. Annual Review Public Health. 2014; 35(1), 327–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Meadows D Leverage Points: Places to Intervene in a System, 1999. Available at: http://donellameadows.org/archives/leverage-points-places-to-intervene-in-a-system/. Accessed August 30, 2018
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


