Abstract
Background: Identifying problem drinkers and providing brief intervention (BI) for those who screen positive are required within all level I trauma centers. While parent–adolescent relationships impact adolescent alcohol use, parenting skills are rarely included in adolescent alcohol BIs within pediatric trauma centers.
Introduction: The primary objective of this study was to examine the feasibility and acceptability of an electronic parenting skills intervention for parents of injured adolescents who report alcohol or drug use.
Materials and Methods: Across three pediatric level I trauma centers, admitted trauma patients 12–17 years of age, screening positive for alcohol or drug use, were consented along with one parent. Adolescent–parent dyads were enrolled and assigned to the intervention (Parenting Wisely web-based modules coupled with text messaging) or standard care conditions using a 2:1 allocation ratio. Teens completed 3- and 6-month follow-up surveys; parents completed 3-month follow-up surveys.
Results: Thirty-seven dyads were enrolled into the study. Only one-third of parents accessed the web-based Parenting Wisely after baseline. All parents completed the text message program. At 3-month follow-up, 78% of parents endorsed that they would recommend the program to others. There were no significant differences in adolescent substance use or parenting behaviors between groups at follow-up.
Discussion: A texting component is well received, but web-based components may be underutilized. Larger studies are necessary to determine if an electronic skills intervention has an effect on parenting skills and adolescent substance use.
Conclusions: This study demonstrated accessibility and feasibility of an e-parenting intervention with more utilization of text components than web-based.
Keywords: SBIRT, parenting skills, adolescent alcohol
Background
According to a 2016 report, 191,000 adolescents 12–17 years of age are current heavy alcohol users and an estimated 488,000 adolescents report past-year use.1 Youth who report drinking before the legal age are significantly more likely to unintentionally injure themselves or others after drinking.2 Ehrlich et al. have illustrated that injured adolescents admitted to pediatric trauma centers are considered a high-risk population with ∼30% of these injured adolescents screening positive for alcohol misuse.3 This correlation between underage drinking and injuries provides an opportunity to intervene with adolescents who report alcohol misuse at trauma centers. The American College of Surgeons Committee on Trauma recommends that all trauma centers have the ability to identify patients who are problem drinkers and requires that all level I trauma centers have a system to provide patients who screen positive with a brief intervention (BI).4 Although increased monitoring, communication, and positive parent–adolescent relationships may delay alcohol initiation and decrease alcohol use,5 our previous work found that parenting skills are rarely included in alcohol BIs within pediatric trauma centers.6 Just as an adolescent's admission to a trauma center is an opportune time to identify alcohol and other drug (AOD) use and deliver a BI during a teachable moment,7 it also represents an ideal time to initiate a parenting skills intervention.
To date, there is no research on the feasibility and acceptability of an AOD use-centered parenting skills intervention in pediatric trauma centers. While some studies have examined the efficacy of computer-delivered interventions with adolescents for their AOD use,8,9 few consider the role that parents play in adolescent AOD use trajectories. A recent systematic review of 42 studies has shown that parenting interventions outside of the pediatric trauma center are effective for preventing and decreasing adolescent tobacco, alcohol, and illicit substance use over the short and long term.10 Among these studies, there was strong evidence supporting the use of computer-based interventions for alcohol use prevention.10 Parenting Wisely is a self-administered, highly interactive, multimedia online parenting program teaching parenting skills. A 2010 study that included 116 Australian parents using Parenting Wisely showed a substantial increase in parental knowledge and reduction in child problem behavior; these gains were maintained at 3-month follow-up.11
In addition to a computer-based intervention, reinforcement of parenting messages may be useful. Almost all American adults have a text messaging-capable phone, and most actively use text messaging.12 Interventions that include text messaging have been shown to be feasible,13–18 demonstrated short-term behavior change for various preventive health topics,13 and been accepted by parents.19,20 Nonetheless, no studies to date have utilized text messages with parenting skills to decrease teen AOD use.
Introduction
The primary objective of this study was to examine the feasibility and acceptability of an electronic parenting skills intervention, referred here as e-parenting. The intervention consists of online Parenting Wisely modules coupled with text messaging for parents of injured adolescents, who reported AOD use. We also collected data on parenting behavior and assessed the feasibility of measuring the injured adolescent's report of AOD use.
Materials and Methods
Three level I pediatric trauma centers participated in the study. Each site obtained institutional IRB approval and received protocol training from the research team before beginning research activities. Sites were responsible for enrollment only; the coordinating center was responsible for data management and follow-up.
Each site performed an initial screening of adolescents admitted to the inpatient trauma service (including orthopedics, neurosurgery, and burn units), for the following inclusion criteria: adolescent 12–17 years of age; medically stable; screen positive for alcohol and/or drug use by the CRAFFT21 (mnemonic acronym of first letters of key words in the six alcohol/drug use screening questions) or biochemical test; English speaking; and parent with a text-capable cell phone. The CRAFFT is an AOD use screening tool that asks about past-year alcohol, marijuana, and other drug use, as well as six risk behavior questions related to assess high-risk use.21 We excluded dyads where the adolescent was determined by the clinical team to be cognitively or emotionally unable to participate, suspected to be a victim of child abuse, under state protective custody, being evaluated following a suicide attempt, and being treated for an alcohol or drug dependency before admission, or those currently incarcerated. Research staff approached eligible parent–adolescent dyads and obtained parental consent from one parent and adolescent assent.
Consented adolescents–parent dyads were enrolled and assigned to either intervention or standard care conditions using a 2:1 allocation ratio. We randomized more dyads to the experimental condition to maximize our experience conducting the e-parenting intervention. Those assigned to the standard care condition received standard clinical care from their specific institution, which included an alcohol and/or drug BI for the adolescent by clinical staff, but without the e-parenting intervention. Those assigned to the e-parenting intervention received institutional standard care, the Parenting Wisely program, and accompanying text messages.
Parenting Wisely
Parenting Wisely is an interactive web-based parenting program consisting of video scenarios, skills practice, interactive quizzes, and a parent forum. The program covers topics such as alcohol and drugs, school and homework problems, delinquency and other problem behaviors, and family conflict. The e-parenting intervention group was provided online access to the Parenting Wisely program for 12 weeks with one module (Finding Drugs, ∼20 min) completed in the hospital at the time of consent. Parents were encouraged by research staff at enrollment to complete at least three additional modules after their adolescents' hospitalization. Parents were also informed about the online Parenting Wisely forum where parents could post questions that would be answered by a Parenting Wisely psychologist.
Text Messages
The e-parenting group also received twice-weekly parenting skills text messages for 12 weeks, which was programmed and implemented by an external vendor. The first week text message was a welcome message and the last week (week 12) was a thank you message for completing the program. After the first week, the program delivered twice-weekly text messages for 10 weeks tailored to specific parenting skills, including communication, monitoring/supervision, conflict resolution, and self-talk. Each week, parents were asked by text which topic they would like to learn more about (First Text Example: “Which topic would be helpful this wk? Reply A to learn about talking to your teen. B = keeping track of your teen. C = handling arguments. D = helping yourself.”). Based on the topic they chose, parents would receive a text 2 days later on the topic they chose (Second Text Example: “A PROMPT is a little reminder to nudge your teen toward a desired behavior without confrontation” http://tinyurl.com/PWPrompt.”) The second text of that week contained information about the same identified topic, with a corresponding link. Links included video clips from appropriate Parenting Wisely modules or a direct link to the Parenting Wisely website. (Third text example: “Compliment your teen about something positive they have done this week to show you are paying attention to them. https//goo.l/EsvzBX.”) If a parent did not choose any track for the week, they would be reminded and if they still did not respond, they would automatically be pushed a predetermined topic for the week.
At the bottom of each text message, the option to reply “STOP” to end the texting program was offered. If the parent replied with “STOP”, research staff would contact the parent to check in. If the parent did not want to receive further text messages, they would be considered withdrawn from the texting component, but would continue in the research project.
While in the hospital, both adolescents and parents completed web-based baseline assessments. Parents received a 3-month follow-up assessment, and adolescents received 3- and 6-month assessments. These assessments were conducted to determine if the effects of the intervention faded over time. All assessments were administered by REDCap, a secure web application for building and managing online surveys and databases.22 Individuals without computer access were able to complete the surveys through telephone. Parents and adolescents were compensated with a $25 gift card for each assessment completed. Table 1 details the assessment instruments administered at each time point.
Table 1.
Teen and Parent Assessments
| CONSTRUCT | MEASURE | BASELINE | 3 MONTH | 6 MONTH |
|---|---|---|---|---|
| Teen | ||||
| Alcohol and other drug screening (inclusion criteria) | CRAFFT | X | ||
| Demographics | Adolescent Demographic Information | X | ||
| Alcohol use (drinking days/heavy drinking days) | Adolescent Drug Questionnaire | X | X | X |
| Marijuana and other drugs | Drug Use Questionnaire | X | X | |
| Adolescent perception of parental monitoring | Parental Monitoring Questionnaire | X | X | X |
| Parent | ||||
| Demographic | Parent Demographic Information | X | ||
| Acceptability (Intervention parents only) | Consumer Satisfaction Questionnaire | X | ||
CRAFFT, mnemonic acronym of first letters of key words in the six alcohol/drug use screening questions.
Study Measures
Parents
Demographic data, including gender, age, race, and ethnicity, were administered at the baseline survey. At the 3-month follow-up, intervention parents were asked 27 questions covering four main themes about their response to the e-parenting program: (1) overall recommendation; (2) helpfulness; (3) satisfaction; and (4) ease of interface with technical aspects of the program. For a smaller subset of the intervention group, parents were asked open-ended questions about the e-parenting program. We also collected data on the frequency of parents' engagements with the different aspects of the e-parenting program (i.e., Parenting Wisely website and forum, text messaging, and web links within text messages). Questions were derived from the Consumer Satisfaction Questionnaire.23 All parents (intervention/standard care groups) were also asked about their substance use and their teen's use of substance use services; however, these measures are not reported in this article.
Adolescents
Demographic data, including gender, age, race, and ethnicity, were collected with the baseline survey. We also asked the adolescents about their AOD use, specifically (1) past 3-month use of alcohol (Yes/No); and, if alcohol was reported, questions about (2) binge alcohol use in the past 3 months (three or more drinks for females and four of more for males [Yes/No]); (3) being drunk/intoxicated due to alcohol in the past 3 months (Yes/No), and (4) single question about the past 30-day use of marijuana (Yes/No). These questions were asked at baseline, and 3- and 6-month assessment. A modified version of the Drug Use Questionnaire24 about use of substances other than alcohol or marijuana in the past 6 months (Yes/No) was administered at baseline and 6-month assessments. Adolescents were also administered the Parental Monitoring Questionnaire (PMQ)25 at baseline, and 3- and 6-month assessments. The PMQ is a 24-item questionnaire assessing adolescent perception of parental monitoring and supervising behavior. Each item has a score range 1–5 (higher scores indicating more involved parental behavior). In this study, all items were summed to provide a total PMQ score (max score = 120).
Data Analysis
Data were analyzed using SAS version 9.4 (Carey, NC). Descriptors of the sample and counts of parental responses are reported. All substance use questions asked of the teen at the three assessment time points are reported as percentages. PMQ mean scores with standard deviations are also reported, on parental behaviors as reported by the adolescent.
Results
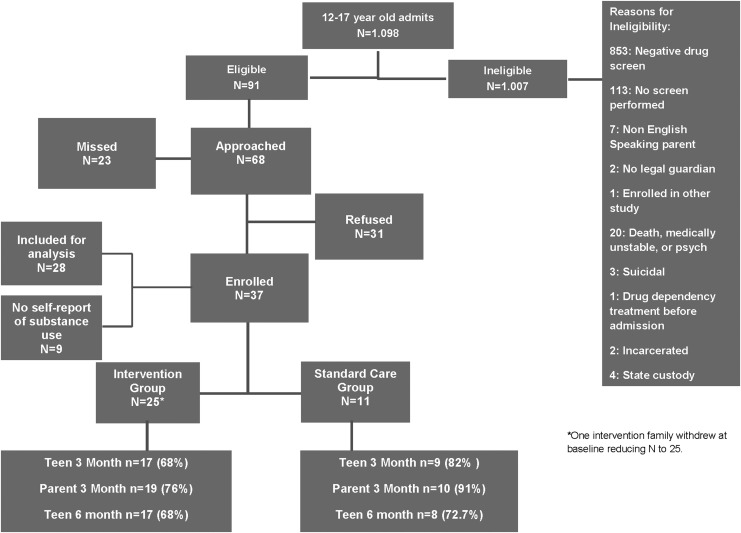
Of the 1,089 adolescent (12–17 year old) trauma admissions across the three institutions, 91 patients were identified as eligible for the study; 68 (75%) parent–teen dyads were approached and 37 dyads (54%) were enrolled. One dyad withdrew participation before completing baseline activities. Of the remaining 36 dyads, 25 randomized to intervention and 11 to standard care completed baseline activities (see Consort diagram, Fig. 1). The majority of the enrolled parents were female (86%) and mothers (83%); the most frequent relationship status reported was married (56%). In the past year, 55% of the parents reported having binged on alcohol at least once, 33% had used tobacco, 11% had used illicit drugs, and 22% had used prescription medications not as prescribed.
Fig. 1.
e-Parenting recruitment, allocation, and retention.
The majority of teens were male (78%) with a mean age of 15.6 years. Sixty-eight percent of teens identified as non-Hispanic; and 62% as white. There were no significant differences between the two intervention groups on these parent and adolescent demographic characteristics. Detailed demographic characteristics are presented in Table 2.
Table 2.
Teen and Parent Demographic Information
| VARIABLE | STANDARD CARE: TEEN (N = 9) | e-PARENTING: TEEN (N = 28) | STANDARD CARE: PARENT (N = 9) | e-PARENTING: PARENT (N = 27)a |
|---|---|---|---|---|
| Age (mean) | 15.1 | 15.8 | 42.3 | 42.9 |
| Gender (N, %) | Male n = 8 (89) | Male n = 21 (75) | Male n = 1 (11) | Male n = 4 (15) |
| Female n = 1 (11) | Female n = 7 (25) | Female n = 8 (89) | Female n = 23 (85) | |
| Hispanic (N, %) | Yes n = 3 (33) | Yes n = 9 (32) | Yes n = 3 (33) | Yes n = 6 (22) |
| No n = 6 (67) | No n = 19 (68) | No n = 6 (67) | No n = 21 (78) | |
| Race (N, %) | White n = 5 (56) | White n = 18 (64) | White n = 6 (67) | White n = 21 (78) |
| Black n = 1 (11) | Black n = 1 (4) | Black n = 1 (11) | Black n = 0 (0) | |
| More than one race n = 2 (22) | More than one race n = 3 (11) | More than one race n = 0 (0) | More than one race n = 2 (7) | |
| Other race n = 1 (11) | Other race n = 5 (18) | Other race n = 2 (22) | Other race n = 3 (11) | |
| I don't know n = 0 (0) | I don't know n = 1 (4) | I don't know n = 0 (0) | I don't know n = 1 (4) |
One parent did not complete baseline survey.
Only one-third of parents (n = 7) accessed the Parenting Wisely website after completing the required module, with only four parents (18%) completing an additional module. No parents utilized the Parenting Wisely online forum. All intervention parents received text messages for the entire 3-month period; no one elected to stop participation. Nearly two-thirds of parents (n = 13) selected a text-message parenting theme for at least 1 week or an average of four times throughout the cycle.
Three-month follow-up rates were 72.2% (n = 26) and 80.6% (n = 29) for teens and parents, respectively. The teen 6-month follow-up rate was 69.4% (n = 25). Eighty-five percent of intervention parents (n = 10) completed the 3-month follow-up, with 89% of intervention parents rating the program good to excellent quality; 65% said they would recommend the e-parenting program. Over 80% of intervention parents recommended the text messages containing Parenting Wisely video clips, but only one recommended the website. Of the subset of intervention parents who provided answers to the open-ended questions (n = 3), two suggested that a mobile app version be offered. Specifically, one parent stated, “If I could have accessed more from my mobile device, phone in my case, I think I would have used it a bit more.”
At 3-month follow up, the overall recommendation of the program by intervention parents was high with 78% endorsing that they were likely to recommend the program to others. Most (63%) reported that the teen parenting advice received was helpful or very helpful. The majority (63%) were also satisfied or very satisfied with the program. Most did not find the program too complex (62%) or needing technical support to interface with the program elements (88%).
Across the types of substances used and time points that the survey was administered, there were no significant differences between adolescents in the standard care and intervention groups. At baseline assessment, 78% of the standard care group and 39% of the intervention group reported using alcohol during the past 3 months. At the 6-month assessment, alcohol use was reported by 17% of the standard care group and 53% of the intervention group. These changes were not significant (Standard Care Δ = −61%; 95% confidence interval [CI]: −100 to 0; Intervention Δ = +14%, 95% CI: −4 to 32). Among those reporting alcohol use, binge drinking (gender specific, three or more for females and four or more for males) was reported by 43% of alcohol-using adolescents in the standard care group at baseline and 64% of those in the intervention group. Binge drinking increased at the 6-month assessment in both groups, although the difference in increase was not significantly different (Standard Care Δ = +57%; 95% CI: 14–100; Intervention Δ = +16%, 95% CI: 0–33). There were no significant changes in other drug or marijuana use between the groups.
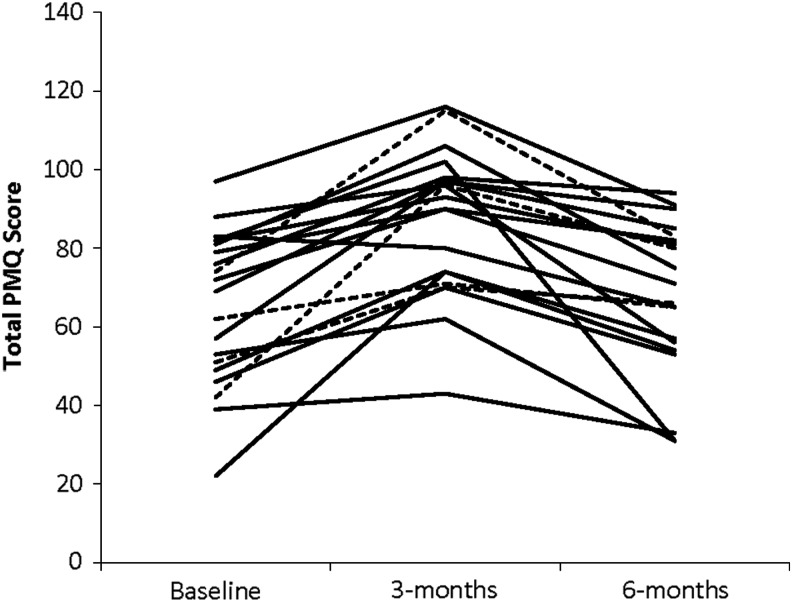
The change in PMQ scores for the subsample of adolescents who complete all three assessments (n = 20; 54%) is shown in Figure 2. Visual inspection suggests that most adolescents reported that parental monitoring and supervision increased from baseline to 3 months, but then decreased at the 6-month assessment.
Fig. 2.
Parental Monitoring Questionnaire score across time by individual participant (- - - -, control; ——, intervention).
Discussion
Due to a lack of integration of parenting skill building into pediatric trauma center-based BIs for adolescents, we created a mechanism of providing a feasible, accessible, and convenient intervention for parents of AOD-using adolescent patients. Furthermore, the intervention needed to be portable and engaging so it would continue to be used by parents after their adolescent's discharge from the hospital. Our findings demonstrated that a text message-based skill intervention for parents of alcohol- or drug-positive adolescent trauma patients may be more acceptable than a web-based program. Eighty percent of parents recommended the texting component of our program, while no parent recommended the website. Furthermore, among the subset of parents who completed the open-ended questions at follow-up, the majority stressed the importance of a brief, mobile program. It may be easier for parents to access information through interactive text messages than requiring parents to seek information on a website that requires more effort. This information is important to consider in developing future parenting interventions in this setting.
Feasibility and acceptability of this intervention were demonstrated in this study. While important determinants of adoption, it would also be necessary to demonstrate effectiveness of an e-parenting intervention within the pediatric trauma center. In this study, there were no changes in adolescent substance use or perception of parenting behaviors at 6-month follow-up. However, our small sample was not powered to detect change in these behaviors. Further study with a larger sample is necessary to determine if an e-parenting skills intervention has an effect on parenting skills and adolescent risk behaviors, such as alcohol and substance use. There did appear to be an increase in parenting behaviors at 3 months (the end of the intervention period for the experimental condition). This may suggest that an intervention that would engage parents for a longer duration might be more beneficial.
Our study findings have several limitations. Our sample was small and somewhat homogenous, and other parents of adolescents might respond differently. The sample was also not powered to detect modest changes in teen behaviors. Furthermore, only slightly more than half of qualifying dyads approached agreed to participate. Although many of these refused because of not wanting to participate in research, it is uncertain if more would accept a parenting skills program if it was offered as routine clinical care.
Our study found that it is feasible to include a parenting skills program at pediatric trauma centers and a text component would be well received, while website components might be utilized much less. Furthermore, during the intervention period, parental monitoring can increase, but it may be difficult to sustain that increase after the intervention terminates. More research is necessary to better understand the impact of an electronically delivered parenting program within the pediatric trauma center.
Acknowledgments
This study was supported through funding by National Institute of Alcohol Abuse and Alcoholism 1R21AA024185. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure Statement
No competing financial interests exist.
References
- 1. Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. SMA 17-5044, NSDUH Series H-52). Rockville, MD: Center for Behavioral Health Statistics and Quality, 2017 [Google Scholar]
- 2. Hingson RW, Zha W. Age of drinking onset, alcohol use disorders, frequent heavy drinking, and unintentionally injuring oneself and others after drinking. Pediatrics 2009;123:1477–1484 [DOI] [PubMed] [Google Scholar]
- 3. Ehrlich PF, Maio R, Drongowski R, Wagaman M, Cunningham R, Walton MA. Alcohol interventions for trauma patients are not just for adults: Justification for brief interventions for the injured adolescent at a pediatric trauma center. J Trauma 2010;69:202–210 [DOI] [PubMed] [Google Scholar]
- 4. American College of Surgeons Committee on Trauma. Resources for the optimal care of the injured patient, 2006. Available at https://acep.org/Clinical—-Practice-Management/Alcohol-Screening-in-the-Emergency-Department (last accessed May11, 2018)
- 5. Spirito A, Hernandez L, Cancilliere MK, Graves H, Knopik VS, Barnett N. Improving parenting and parent-teen communication to delay or prevent the onset of alcohol and drug use in young adolescents with emotional/behavioral disorders: A pilot trial. J Child Adolesc Subst Abuse 2015;24:308–322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Workgroup PTS. Implementation of alcohol screening, brief intervention and referral to treatment policies in pediatric trauma centers. Providence, RI: Injury Prevention Center at Rhode Island Hospital, 2012 [Google Scholar]
- 7. Longabaugh R, Woolard RE, Nirenberg TD, et al. . Evaluating the effects of a brief motivational intervention for injured drinkers in the emergency department. J Stud Alcohol 2001;62:806–816 [DOI] [PubMed] [Google Scholar]
- 8. Maio RF, Shope JT, Blow FC, et al. . A randomized controlled trial of an emergency department-based interactive computer program to prevent alcohol misuse among injured adolescents. Ann Emerg Med 2005;45:420–429 [DOI] [PubMed] [Google Scholar]
- 9. Walton MA, Chermack ST, Shope JT, et al. . Effects of a brief intervention for reducing violence and alcohol misuse among adolescents: A randomized controlled trial. JAMA 2010;304:527–535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Allen ML, Garcia-Huidobro D, Porta C, et al. . Effective parenting interventions to reduce youth substance use: A systematic review. Pediatrics 2016;138:pii: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Cefai J, Smith D, Pushak RE. Parenting wisely: Parent training via CD-ROM with an Australian sample. Child Fam Behav Ther 2010;32:17–33 [Google Scholar]
- 12. Pew Internet & American Life Project. Mobile health. 2012. Available at http://pewinternet.org/Reports/2012/Mobile-Health.aspx (last accessed May11, 2018)
- 13. Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. Am J Prev Med 2009;36:165–173 [DOI] [PubMed] [Google Scholar]
- 14. Waterlander W, Whittaker R, McRobbie H, et al. . Development of an evidence-based mHealth weight management program using a formative research process. JMIR Mhealth Uhealth 2014;2:e18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Free C, Knight R, Robertson S, et al. . Smoking cessation support delivered via mobile phone text messaging (txt2stop): A single-blind, randomised trial. Lancet 2011;378:49–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Granholm E, Ben-Zeev D, Link PC, Bradshaw KR, Holden JL. Mobile Assessment and Treatment for Schizophrenia (MATS): A pilot trial of an interactive text-messaging intervention for medication adherence, socialization, and auditory hallucinations. Schizophr Bull 2012;38:414–425 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Suffoletto B, Callaway C, Kristan J, Kraemer K, Clark DB. Text-message-based drinking assessments and brief interventions for young adults discharged from the emergency department. Alcohol Clin Exp Res 2012;36:552–560 [DOI] [PubMed] [Google Scholar]
- 18. Kool B, Smith E, Raerino K, Ameratunga S. Perceptions of adult trauma patients on the acceptability of text messaging as an aid to reduce harmful drinking behaviours. BMC Res Notes 2014;7:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kharbanda EO, Stockwell MS, Fox HW, Rickert VI. Text4Health: A qualitative evaluation of parental readiness for text message immunization reminders. Am J Public Health 2009;99:2176–2178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Militello LK, Kelly SA, Melnyk BM. Systematic review of text-messaging interventions to promote healthy behaviors in pediatric and adolescent populations: Implications for clinical practice and research. Worldviews Evid Based Nurs 2012;9:66–77 [DOI] [PubMed] [Google Scholar]
- 21. Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shaffer HJ. A new brief screen for adolescent substance abuse. Arch Pediatr Adolesc Med 1999;153:591–596 [DOI] [PubMed] [Google Scholar]
- 22. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Larsen D AC, Argreaves W, Nguyen T. Assessment of client/patient satisfaction: Development of a general scale. Eval Program Plann 1979;2:197–207 [DOI] [PubMed] [Google Scholar]
- 24. Spirito A. Reliability data on the drug use questionnaire. Providence, RI: Brown University, 2001 [Google Scholar]
- 25. Kerr M, Stattin H. What parents know, how they know it, and several forms of adolescent adjustment: Further support for a reinterpretation of monitoring. Dev Psychol 2000;36:366–380 [PubMed] [Google Scholar]