Abstract
Effective approaches to promoting pre-exposure prophylaxis (PrEP) and linkage to PrEP care among those who may benefit the most from PrEP has proven to be a major challenge. We designed and pilot tested a strengths-based case management (SBCM) intervention for PrEP linkage. Adults interested in PrEP and meeting criteria (n = 61) were randomized to passive referral (control) or active SBCM (treatment). Outcomes measured were completion of provider visit, initiation of PrEP, and time to initiation of PrEP. Overall, 34% initiated PrEP by 12 weeks: 9 (29%) in the control group and 12 (40%) in the treatment group. The mean time to PrEP initiation was 13.1 weeks (95% confidence interval, 12.0-14.2) with no difference between groups (P = .382). There was a 21% difference in achieving a provider visit between the treatment and control groups (53.3% versus 32.3%) by 12 weeks (P = .096). Participants encountered financial, logistical, social, and provider-related barriers to PrEP access. Strengths-based case management–based patient navigation is a promising strategy for assisting PrEP seekers in obtaining a medical provider visit and initiating PrEP.
Keywords: pre-exposure prophylaxis, HIV prevention, access to care, navigation
Introduction
Although pre-exposure prophylaxis (PrEP) with oral tenofovir/emtricitabine (TDF/FTC) can reduce the risk of new HIV infections by more than 90% when taken daily, disparities exist in PrEP access and delivery.1-3 South Florida includes the 3 metropolitan areas with the highest rates of new HIV infections in the United States,4 but suboptimal levels of PrEP prescribing have been observed in this region compared to other areas of the United States.5
Among participants in a demonstration project that provided PrEP free of charge in a research environment,5 those located in Miami and minority participants, particularly young black and Hispanic men who have sex with men (MSM), were unlikely to utilize PrEP beyond completion of a demonstration project study compared to white, non-Hispanic/Latino MSM, and those in San Francisco.6 Despite previous experience with PrEP and expressed high interest in continuing PrEP, study participants reported pessimism about accessing PrEP on their own.6 Potential PrEP candidates report perceptions of high cost, difficulty identifying a PrEP provider, discomfort communicating sexual risk to a provider, lack of accessible medical care, and fear of community and provider stigma regarding HIV and sexual behavior as barriers to PrEP linkage.7-9
Strengths-based case management (SBCM) is a model of community-based case management that focuses on a participant’s own abilities/strengths and assets, recognizes and supports goal setting, and encourages use of the community as a resource for support.10 Strengths-based case management is the only intervention that has shown, in a randomized controlled trial, effectiveness in linking newly HIV-positive individuals to their initial HIV care visit.11 The individualized approach of SBCM is well suited to racially, economically, and ethnically diverse populations such as those found in Miami-Dade County. Varied challenges to linkage to care including financial concerns, complexities of immigration status, stigma, and provider access may be addressed through SBCM.8,12,13 The SBCM approach, in which the individual’s abilities and assets are recognized and supported by a patient navigator, while also identifying sources of support and resources in the community and encouraging engagement, may effectively counter frequently observed despondent attitudes regarding linkage to prevention care and encourage positive engagement in the process.5,14
What Do We Already Know about This Topic?
Pre-exposure prophylaxis (PrEP) is an effective HIV prevention strategy when taken as directed by people who are at increased risk of HIV infection. For many people who could benefit from PrEP, linkage to a prescribing provider is a major barrier to receiving PrEP. These barriers disproportionately impact people who are socioeconomically disadvantaged. Strengths-based case management has been effective in facilitating linkage to HIV treatment in other studies but has not been tested for PrEP linkage.
How Does Your Research Contribute to the Field?
New strategies for linking people to PrEP care more effectively are needed. This study finds that use of a strengths-based case management approach for PrEP linkage is promising. Delineation of the barriers encountered by PrEP seekers in this study also contributes to our understanding of the factors that influence PrEP access.
What Are Your Research’s Implications toward Theory, Practice, or Policy?
This study provides support for further investigation of a strengths-based case management approach to PrEP linkage. Further, we describe structural, logistical, provider-related, and social barriers to PrEP care that are important to consider in development of policies and practice aimed at broadening PrEP implementation in diverse populations.
The objective of this study was to test and evaluate the efficacy of an adaptation of the evidence-based antiretroviral treatment access study,11 using a brief, SBCM intervention to facilitate linkage to PrEP/HIV prevention care in a majority of low-income, urban, nonwhite sample population. Specifically, we aimed to assess the percentage of participants who started PrEP, as well as time to PrEP initiation. To the best of our knowledge, no previous research has evaluated the impact of an SBCM intervention on linkage to PrEP care. Additionally, descriptive data regarding barriers faced by participants and interventions required by navigators to overcome these barriers were obtained to inform future patient navigation interventions and public health interventions involving patient navigators.
Methods
To assess the impact of the SBCM intervention on successful linkage to a PrEP-competent provider and PrEP uptake, this study recruited individuals at risk for HIV infection by the following criteria: (1) were eligible for PrEP based on the Centers for Disease Control and Prevention (CDC; 2014) clinical practice recommendations for PrEP use15 and (2) had not previously accessed PrEP in a nonresearch setting. Study flyers were distributed inside outpatient clinics that belonged to a large public hospital in the Miami Metropolitan area and community-based organizations where PrEP was not offered on-site. Also, a message beginning “Interested in PrEP? Not sure how to get it?” was broadcasted locally through GRINDR, a social networking smartphone application. Our recruitment strategy aimed to enroll participants from diverse racial, ethnic, and sexual orientation-based backgrounds in South Florida with previously encountered challenges to PrEP linkage.12 The recruitment period was from January 26, 2016, to October 20, 2016.
Prospective participants were currently uninfected with HIV by self-report. They were 18 years of age or older, able to meet the project interviewer/patient navigator at the research site, able to give informed consent, willing to provide personal contact information and to be contacted by phone, and appropriate for consideration of PrEP based on criteria from the CDC Clinical Practice Guidelines.16 Those candidates meeting study inclusion criteria were then asked to provide informed consent and a Health Insurance Portability and Accountability Act authorization to obtain medical records from their provider regarding visits, HIV test results, and PrEP prescriptions. All participants were informed that they would be responsible for the cost associated with the provider visit and associated HIV testing per the health center’s policies.
All study procedures and informed consent documents were approved by the University of Miami Human Subject Research Office Institutional Review Board (approval number 20150121). All patients provided written informed consent prior to enrollment in the study.
Following study enrollment, participants completed an interviewer-administered baseline survey (see description of assessments, below). Participants were then immediately randomized to receive either the intervention condition (patient navigator individualized assessment and follow-up using SBCM) or the control condition (enhanced standard of care including a PrEP Starter Package). Randomization occurred by computer-generated block randomization with randomly selected block sizes. Randomization was stratified by 2 subgroups: one for MSM and transgender women and one for heterosexual men and women. Cards with study group assignment were placed in sealed, signed envelopes by the data manager (who did not interact with participants during the study). The sequentially numbered envelope was opened following the completion of the baseline study.
Intervention
Our SBCM intervention focused on participant’s abilities, strengths, and community support and engagement for enacting desired change. The 5 principles of SBCM include: (1) encourage identification and the use of strengths, abilities, and assets; (2) recognize and support participant control over goal setting and the search for needed resources; (3) establish an effective working relationship; (4) view the community as a resource and identify sources of support; and (5) conduct case management as active, community-based activities.10,12,17 This pilot intervention addressed these principles systematically using the following activities subsequent to the baseline assessment and during the first visit with the patient navigator: building the relationship; emphasizing personal strengths; learning to make contact. All SBCM intervention arm participants had 1 in-person session with the patient navigator lasting 45 to 60 minutes to develop these elements (either directly following the screening, informed consent, and enrollment procedures or at a scheduled follow-up appointment). Participants had the option to attend 4 additional follow-up visits and/or phone/text message contact to revisit personal strengths, reevaluate available resources, and focus on the remaining SBCM elements of reviewing progress and completing the work. Each of these activities were aligned with specific objectives and are described in the intervention manual.
Enhanced Standard of Care
Control condition participants were provided with a package of information on HIV prevention strategies including (1) a list of PrEP providers in the area as well as HIV testing sites and sexually transmitted infection clinics, (2) recommendations regarding initiating discussion with the provider regarding PrEP, and (3) information regarding available patient assistance and co-pay assistance programs for PrEP. Patient navigators were trained to provide up-to-date information on available programs supporting PrEP access, for example, Medicaid and patient assistance programs for medication cost and co-pay assistance to ensure the availability of resources for linkage in both arms.
Patient Navigation
Trained study staff functioned as navigators for the study. Following assessment, navigators provided information regarding PrEP, discussed available resources in the community for prevention services with participants, and supported and motivated the participant’s efforts to engage in HIV prevention strategies inclusive of PrEP. Patient navigators collected semistructured study notes for each treatment arm participant encounter on barriers and facilitators to PrEP uptake. Navigators also discussed strategies to overcome barriers. As part of the SBCM protocol, barriers confronted (eg, difficulties scheduling appointment, communicating with provider, paying for visit, etc) were assessed at each encounter and documented in these study notes.
Assessment and Study Flow
Assessments at baseline, 6-, and 12-week follow-up consisted of an interviewer-administered questionnaire conducted in either English or Spanish, by participant preference. Measures were aligned with the SBCM model. The length of the baseline assessment was 30 to 45 minutes. Measures included sociodemographics, experiences with PrEP and/or nonoccupational postexposure prophylaxis, risk perception, risk behaviors, current prevention strategies, experiences with providers and clinics on HIV prevention care, perceived barriers and facilitators to obtaining PrEP, knowledge, beliefs, and attitudes towards PrEP, adherence self-efficacy, health literacy and numeracy, depression, quality of life, and social support.
The primary outcome of completion of a visit with a PrEP provider was defined by participant self-report. The PrEP initiation was defined as participant self-reported receipt of a PrEP prescription and initiation of PrEP. Outcome measures were queried at 6 and 12 weeks and by brief time-matched check-ins at weeks 4 and 10 to ensure accurate recording of events occurring between follow-up assessments. Time was scaled in weeks. If a participant initiated PrEP within the 12-week observation period, the event was coded as 1; if there was no PrEP initiation within the observation period, this was coded as 0; and participants lost to follow-up were censored and assigned a time of 16 weeks to ensure that every participant is counted in the analysis.
Data Analysis
To address the primary study hypotheses that SBCM would increase the proportion of participants who complete a physician visit for discussion of PrEP and start PrEP medication, χ2 analysis was conducted for each time point an assessment was delivered to a participant. Participant’s reports of having made an appointment to see a provider about PrEP and initiating PrEP within 12 weeks were yes–no scales asked at 4, 6, 8, and 12 weeks; if the participant was lost to follow-up, they were assigned a no response. To assess time to obtaining PrEP, a Kaplan-Meier time-to-event analysis was utilized. Time was scaled in weeks. If a participant initiated PrEP within the 12-week observation period, the event was coded as 1; if there was no PrEP initiation within the observation period, this was coded as 0; and participants lost to follow-up were censored and assigned a time of 16 weeks. Censoring considers all participants by assigning a value to each participant ensuring that every participant is counted in the analysis. The Mantel-Cox log-rank test was used to compare the survival distributions of participants in the control and treatment groups. Statistical analysis was conducted in R (RStudio version 1.0.153, 2009-2017; RStudio, Inc, Boston, MA, USA), using packages Survival and Mosaic.18
A sample size of 61 participants gave stable estimates of rates in each group and had over 80% power in uncovering absolute risk differences of 25% to 30% between groups. Subgroups (race, ethnicity, gender, sexual orientation, sexual behavior) were combined for the primary analysis, and differences by subgroup presented descriptively with an emphasis on effect size rather than hypothesis testing. We estimated that 75% of study participants randomized to the intervention arm would achieve linkage.
Barriers and facilitators to PrEP uptake were examined using both descriptive analysis of the repeated survey data and qualitative assessment of the study notes prepared by patient navigators. Barriers were categorized as “logistical,” “financial,” “provider related,” or “social.” Solutions offered by patient navigators to attempt to overcome each barrier were recorded. Success obtaining PrEP medication was recorded by the type of barrier encountered. The effort and extent of patient navigator contact with participants (number of hours of active case management and number of encounters) was also calculated and described.
Results
Study staff assessed 110 individuals for eligibility and interest by telephone and subsequently recruited 61 individuals at risk of HIV infection (33 MSM/transgender women (TGW) and 28 heterosexual men and women). Baseline demographic characteristics for participants enrolled in the study are summarized by randomization group in Table 1. Of the 61 individuals enrolled in the study, the majority were male (84%), most of which (64%) self-identified as MSM; 1 (3.3%) participant identified as a TGW. Most participants identified race/ethnicity as Hispanic/Latino (43%) or Black/African American (34%). Among respondents, 64% had previously heard of PrEP, 44% had less than a high school education, 80.3% reported an income of <US$40 000 a year, and 44% of all participants did not have health insurance at baseline.
Table 1.
Baseline Demographics for Treatment and Control Groups.
| Control, N = 31 | Treatment, N = 30 | ||||
|---|---|---|---|---|---|
| Count, N | Column % | Count, N | Column % | ||
| Age, mean (SE) | 40.6 | 2.28 | 40.2 | 2.29 | |
| Race/ethnicity | Hispanic | 16 | 51.6% | 10 | 33.3% |
| Black/African American | 10 | 32.3% | 11 | 36.7% | |
| White Non-Hispanic | 4 | 12.9% | 3 | 10.0% | |
| Other; multiple | 1 | 3.2% | 6 | 20.0% | |
| Gender (self-described) | Male | 26 | 83.9% | 25I | 83.3% |
| Female | 5 | 16.1% | 4 | 13.3% | |
| Transgender woman | 0 | 0.0% | 1 | 3.3% | |
| Educational level completed | <High school | 2 | 6.5% | 7 | 23.3% |
| HS graduate | 9 | 29.0% | 7 | 23.3% | |
| Some college | 12 | 38.7% | 7 | 23.3% | |
| College graduate | 8 | 25.8% | 7 | 23.3% | |
| Postgraduate | 0 | 0.0% | 2 | 6.7% | |
| Sexual orientation | Gay or queer | 13 | 41.9% | 13 | 43.3% |
| Bisexual | 3 | 9.7% | 4 | 13.3% | |
| Straight | 13 | 41.9% | 12 | 40.0% | |
| Other | 2 | 6.5% | 1 | 3.3% | |
| Previously heard of PrEP | 21 | 67.7% | 18 | 60.0% | |
| Income | US$0-10 980 | 9 | 29.0% | 131 | 43.3% |
| US$10 981-19 999 | 8 | 25.8% | 6 | 20.0% | |
| US$20 000-39 999 | 10 | 32.3% | 3 | 10.0% | |
| US$40 000-59 000 | 3 | 9.7% | 3 | 10.0% | |
| US$60 000-99 999 | 0 | 0.0% | 5 | 16.7% | |
| US$100 000 or more | 0 | 0.0% | 0 | 0.0% | |
| Insurance coverage | 15 | 48.4% | 19 | 63.3% | |
| Alcohol use (90 days) | Daily | 1 | 3.2% | 2 | 6.7% |
| 5-6 times/week | 1 | 3.2% | 0 | 0.0% | |
| 3-4 times/week | 2 | 6.5% | 4 | 13.3% | |
| 1-2 times/week | 10 | 32.3% | 6 | 20.0% | |
| 2-3 times/month | 4 | 12.9% | 3 | 10.0% | |
| Once a month | 6 | 19.4% | 3 | 10.0% | |
| None | |||||
| 7 | 22.6% | 12 | 40.0% | ||
| Injection drug use (90 days) | 1 | 3.2% | 1 | 3.3% | |
Abbreviations: PrEP, pre-exposure prophylaxis; SE, standard error.
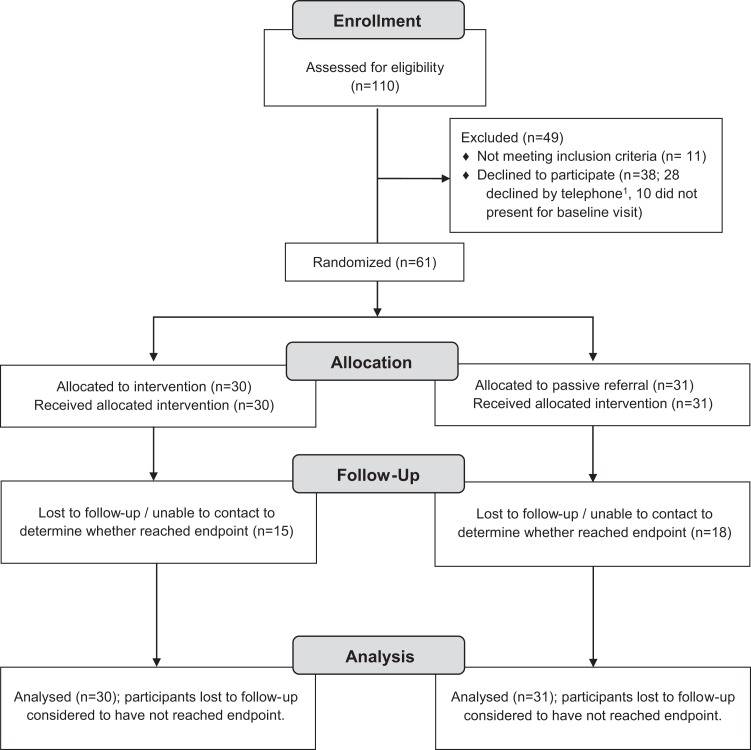
As the first step of the intervention was delivered immediately after randomization, all participants randomized to receive the intervention received at least 1 in-person intervention session and all participants randomized to receive the control intervention also received this intervention at the baseline visit. Of those who were randomized to receive the intervention, a median of 2 in-person visits (range: 1-5, p25 = 1, p75 = 3) and a median of 3 phone or text sessions (range: 0-10, p25 = 1, p75 = 5) were delivered during the intervention period. Of those randomized to receive the study intervention, 15 (50%) of 30 were lost to follow-up before staff could determine whether the primary end point was reached. Of those randomized to receive the control intervention, 18 (58.1%) of 31 were lost to follow-up (see Figure 1). All individuals who were randomized were included in the analysis; those who were lost to follow-up were assumed to have not reached the study end points.
Figure 1.
CONSORT 2010 flow diagram.
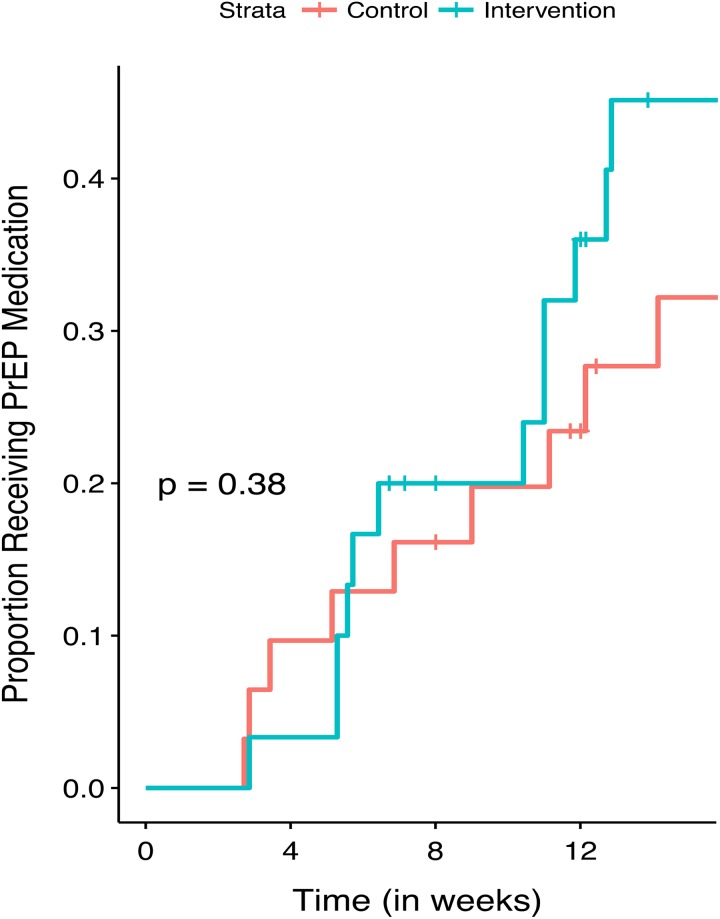
Overall, 34% of participants initiated PrEP by 12 weeks: 9 (29%) in the control group and 12 (40%) in the treatment group. The mean time to PrEP initiation overall was 13.1 weeks (95% confidence interval [CI], 12.0-14.2). In the control group, mean time to PrEP was 13.42 weeks (95% CI, 11.8-15.0), in the treatment group, mean time to PrEP was 12.76 weeks (95% CI, 11.2-14.3; P = .382). Table 2 demonstrates the proportion of participants, by randomization group, (1) seeing a provider for the purpose of discussing PrEP and (2) initiating PrEP medication within 12 weeks of the baseline assessment. The 11% difference between the treatment and control groups in the proportion of participants starting PrEP in 12 weeks was not statistically significant (P = .367). The proportion of participants in each group who obtained PrEP over time by hazard analysis was also determined (Figure 2).
Table 2.
12-week Outcomes (Saw PrEP Provider and Started PrEP) by Treatment Group.
| Outcomes | Control | Treatment | χ2, P | |
|---|---|---|---|---|
| Saw Provider ≤12 weeks | Yes | 10 (32.2%) | 16 (53.3%) | 4.84, .096 |
| No | 21 (67.7%) | 14 (46.7%) | ||
| Started PrEP ≤12 weeks | Yes | 9 (29%) | 12 (40%) | 0.812, .367 |
| No | 22 (71.0%) | 18 (60%) | ||
Abbreviation: PrEP, pre-exposure prophylaxis.
Figure 2.
Kaplan-Meier time-to-event analysis for receipt of pre-exposure prophylaxis (PrEP) medication, by study treatment group.
A 14% difference, which favored the treatment group over the control group (40% versus 25.8%), was seen in PrEP provider consultation by 6 weeks (P = .367). At the 12-week follow-up, there was a 21% difference between the treatment and control groups (53.3% versus 32.3%), again favoring the treatment group (P = .096).
Participants encountered numerous barriers during their attempts to obtain PrEP; a summary of the barriers experienced by those in the intervention condition and potential strategies offered by patient navigators to attempt to overcome them is provided in Table 3. All participants experienced at least 1 barrier, with a median of barriers in 2 of the 4 categories (range: 1-3). Logistical barriers were reported by 70.0% (21/30) participants, financial barriers by 67.7% (20/30), provider-related barriers by 50.0% (15/30), and social by 16.7% (5/30). Rates of PrEP initiation varied from 20.0% (1/5) for those experiencing social barriers to 53.3% (8/15) for those experiencing provider-related barriers.
Table 3.
Summary of Barriers to Obtaining PrEP, by Category.
| Barrier | Patient Navigator Solution | Number of Participants Experiencing Barrier, n = 30 | Participants Who Encountered Barrier and Started PrEP | ||
|---|---|---|---|---|---|
| Logistical barriers | Total for those experiencing at least 1 logistical barrier | 21 | 70.0% | 9/21 | 42.9% |
| Transportation difficulties | Offered resources for transportation | 14 | 46.6% | 5/14 | 35.7% |
| Unstable housing | Provided flexibility in communication and/or relayed messages from providers’ offices if needed, arranged for alternative medication delivery strategies | 10 | 33.3% | 4/10 | 40.0% |
| Difficulty navigating insurance coverage | Assisted with communication with insurance company and/or suggested alternative PrEP provider/clinic | 7 | 23.3% | 4/7 | 57% |
| Unable to complete forms without assistance | Assisted with completion of forms | 5 | 16.6% | 3/5 | 60.0% |
| Could not take time off from work | Provided participant with options for health centers with extended operating hours | 5 | 16.6% | 3/5 | 60% |
| Financial barriers | Total for those experiencing at least one financial barrier | 20 | 67.7% | 8/20 | 40% |
| Lack of medical insurance | Referred to federally qualified health centers and other centers providing PrEP care for patients regardless of ability to pay; provided information regarding patient assistance programs | 11 | 36.6% | 3/11 | 27.2% |
| Could not afford co-pay | Informed participants of available co-pay assistance programs and provided appropriate forms for enrollment | 7 | 23.3% | 5/7 | 71.4% |
| Could not afford administrative costs (eg, notary services) related to attaining PrEP | Provided participant with options regarding community resources that provided administrative services at no cost | 4 | 13.3% | 3/4 | 75% |
| Provider-related barriers | Total for those experiencing at least one provider-related barrier | 15 | 50.0% | 8/15 | 53.3% |
| Difficulty obtaining appointment for PrEP provider visit | Assisted with scheduling appointment | 9 | 30% | 7/9 | 77.7% |
| Provider not comfortable prescribing PrEP | Options for alternative PrEP provider offered | 6 | 16.7% | 4/6 | 66.6% |
| Uncomfortable speaking with a provider about PrEP | Options for alternative PrEP provider offered and/or coached participant on how to start conversation with provider about PrEP | 6 | 20% | 4/6 | 66.6% |
| Social barriers | Total for those experiencing at least one social barrier | 5 | 16.7% | 1/5 | 20.0% |
| Insured through parents or spouse—reluctant to use insurance to access PrEP due to concern about parental or spousal notification | Informed participants of low-cost health resources that offered PrEP, where insurance was unnecessary if the individual could pay out-of-pocket for services | 4 | 13.3% | 1/4 | 25.0% |
| Spouse unwilling to provide documents needed to access patient programs | Coached participant on effective communication strategies that could be used to encourage their partner’s co-operation and support for PrEP seeking | 1 | 3.3% | 0/1 | 0% |
Abbreviations: PrEP, pre-exposure prophylaxis.
Discussion
This pilot study explored the impact of providing an adapted SBCM intervention to high-risk individuals with HIV seeking PrEP in the Miami metropolitan area. In our heterogeneous group of largely racial/ethnic minority PrEP seekers, our SBCM-based patient navigation strategy resulted in a nonsignificant (P < .1) difference between the proportion of participants obtaining PrEP in the 2 study groups. Time to initiating PrEP was longer than expected in both the SBCM intervention and control groups (>12 weeks), and loss-to-follow-up was frequent. Participant adherence to PrEP among those successfully initiating PrEP medication was comparable and moderately high in both groups.
Prior studies have demonstrated that knowledge of PrEP and its efficacy does not necessarily lead to successful PrEP linkage in real-world settings. Barriers to obtaining PrEP that do not exist within the context of research studies can hinder PrEP initiation. Some of these barriers include perceptions and realities of high cost and difficulty identifying PrEP providers.5,6,19,20 While PrEP navigators are frequently employed within PrEP clinical settings, we observed that, for many individuals, there is a need for navigation and assistance with the process of identifying a PrEP provider. We also observed needs related to preparing for the visit and provision of reassurance that financial and logistical barriers can indeed be overcome. In fact, study navigators had to utilize several strategies in order to mitigate barriers, found to be common, and which preceded an initial PrEP provider visit. As an example, a register of provider contacts who were known to be PrEP competent was developed and provided to participants as necessary. Navigators also scheduled PrEP visits for participants when appropriate; for example, for participants who could not access a phone or did not feel confident in scheduling the appointment themselves. Some participants had to be informed and reminded of documentation they needed to bring with them to the appointment. Further, study navigators often explained to participants how the utilization of certain patient assistant programs could remove or at least reduce the costs associated with PrEP initiation.
We observed that ability to overcome barriers varied; “social” barriers, those related to the need to disclose to or depend on others for PrEP access, were most difficult to overcome. Several of study participants were insured through their parents but were unwilling to disclose their PrEP seeking for various reasons. For these individuals, options for PrEP linkage were very limited, as patient assistance programs are not available to individuals who are insured. Thus, these participants could not utilize their insurance without incurring the risk of discovery. In this instance, navigators provided contacts for low-cost health resources for which participants would have to pay out of pocket for services. Those participants who could not afford to pay (3 of 4) were unable to access PrEP. This highlights a major need for interventions that address this PrEP access “donut hole.” It also suggests there may be a potential benefit of providing PrEP navigation to at-risk individuals who may have the knowledge and some financial means, but not the complete capacity to acquire PrEP on their own.
Further, prolonged appointment delays and need for multiple appointments prior to beginning PrEP lead to discouragement and, frequently, abandonment of the process of obtaining PrEP. Shorter time to initiation of PrEP has been associated with longer term outcomes such as increased persistence in care.15 Streamlining of appointments and protocols may allow more prompt initiation of PrEP medication and improved overall engagement.
Participants reported complicated processes and prolonged wait times for an appointment with a provider, even when the patient navigator was involved, as reasons they discontinued the process. A substantial number of participants in both the control and treatment groups were lost to follow-up within the first 6 weeks of the study, and a lesser percentage completed the study without initiating PrEP. As documented by the 4-week check-in, most participants had at least attempted to schedule an appointment with a provider about getting PrEP. This finding highlights the significance of barriers to PrEP during early stages of attempting access and a need for interventions that improve linkage to PrEP providers.
Administrative delays that compromise PrEP linkage in South Florida may result in frustration and abandonment of PrEP seeking. As such, strategies that combine community patient navigation, with streamlining of scheduling requirements, such as financial assessments required at many Federally Qualified Health Centers, may be warranted. These strategies should focus on direct and timely scheduling of a provider visit and immediate PrEP initiation.
While we did not observe any HIV seroconversion events in our short time frame and small participant group study, delays of more than 3 months appointments also confer a risk of seroconversion while awaiting PrEP for individuals at increased risk of HIV. Additional strategies to improve timely and consistent linkage to PrEP providers may include tracking of referrals and timeliness of appointment outcomes and directing PrEP-seeking patients to the most effective providers
Individuals at elevated risk of HIV acquisition may require additional support in .attaining PrEP.6,21,22 The majority of this study’s sample was comprised of individuals from racial and ethnic minorities with low income in South Florida; lower than expected success in obtaining PrEP in both the control and the treatment groups suggests that persistent structural barriers are in place that require additional targeted intervention. Although our SBCM intervention was able to address some barriers among these populations, for example, assistance with completing necessary paperwork and delivering information in a lay manner to those who may be less literate, social obstacles such as need for documents from a spouse or family member or concern about disclosure of PrEP use via insurance documentation was difficult to overcome. Additionally, we observed that the indirect costs associated with PrEP linkage such as those for transportation, absence from work, and obtaining documentation were frequent but often overlooked barriers to obtaining PrEP. Facilitating these logistical arrangements may ease entry into PrEP care.
Limitations of our study include small and heterogeneous participant groups that preclude subgroup analysis. As we were only able to recruit approximately 50% of eligible participants, there is a risk that the study may overestimate the potential effectiveness of the intervention in real-world settings. In contrast, our recruitment strategies may have also enriched our study population for individuals having difficulty obtaining PrEP and therefore may paint a more pessimistic picture of PrEP linkage that does not reflect the experience of those with straightforward PrEP access not seeking the navigation assistance offered through the study. Longer than expected wait times for appointments and loss-to-follow-up prevented full assessment of the impact of the intervention; however, it is likely that those that were lost did not initiate PrEP. Nevertheless, our study participants reflect the social and economic demographics of many individuals at risk of HIV infection in the United States. The PrEP-seeking experiences described here are likely common to many others with socioeconomic challenges living in geographic areas with low structural support for PrEP.
Our pilot data suggest that barriers to PrEP access and linkage, among certain disenfranchised groups, are extensively varied and systemic. As such, these barriers proved to be somewhat difficult to overcome using this SBCM-based patient navigation intervention. The intervention may still be a promising strategy for assisting PrEP seekers in obtaining a medical provider visit and initiating PrEP. However, further research involving a more substantial study sample is needed to determine whether this multifaceted approach, combining SBCM strategies with improved structural support and provider education, is effective in facilitating PrEP linkage and access.
Footnotes
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Doblecki-Lewis has served as on a scientific advisory board for Gilead Sciences.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded by a Miami Center for AIDS Research Administrative Supplement to SDL (parent grant P30AI073961).
ORCID iD: Susanne Doblecki-Lewis, MD, MSPH  https://orcid.org/0000-0001-6535-6698
https://orcid.org/0000-0001-6535-6698
References
- 1. McCormack S, Dunn DT, Desai M, et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. Lancet. 2016;387(10013):53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Molina J-M, Capitant C, Spire B, et al. On demand PrEP with oral TDF-FTC in MSM: results of the ANRS Ipergay trial. In: Conference on Retroviruses and Opportunistic Infections 2015. [Google Scholar]
- 3. Sagaon-Teyssier L, Suzan-Monti M, Demoulin B, et al. , Uptake of PrEP and condom and sexual risk behavior among MSM during the ANRS IPERGAY trial. AIDS care. 2016;28(sup1):48–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Center for Disease Control and Prevention. Diagnoses of HIV infection and AIDS in the United States and dependent areas, 2009. HIV Surveillance Report. 2011;21:1–79. [Google Scholar]
- 5. Cohen S.E, Vittinghoff E, Bacon O, et al. High interest in pre-exposure prophylaxis among men who have sex with men at risk for HIV-infection: baseline data from the US PrEP demonstration project. J Acquir Immune Defic Syndr. 2015;68(4):439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Doblecki-Lewis S, Liu A, Feaster D, et al. Healthcare Access and PrEP Continuation in San Francisco and Miami After the US PrEP Demo Project. J Acquir Immune Defic Syndr. 2017;74(5):531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med. 2012;4(151):151ra125–151ra125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pérez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of PrEP uptake among racially/ethnically diverse young men who have sex with men: The P18 Study. AIDS Educ Prev. 2015;27(2):112–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Golub SA, Gamarel KE, Rendina HJ, Surace A, Lelutiu-Weinberger CL. From efficacy to effectiveness: facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care STDs. 2013;27(4):248–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saleebey D. The strengths perspective in social work practice: extensions and cautions. Soc Work. 1996;41(3):296–305. [PubMed] [Google Scholar]
- 11. Gardner LI, Metsch LR, Anderson-Mahoney P, et al. Efficacy of a brief case management intervention to link recently diagnosed HIV-infected persons to care. AIDS. 2005;19(4):423–431. [DOI] [PubMed] [Google Scholar]
- 12. Gardner LI, Marks G, Strathdee SA, et al. Faster entry into HIV care among HIV-infected drug users who had been in drug-use treatment programs. Drug Alcohol Depend. 2016;165:15–21. [DOI] [PubMed] [Google Scholar]
- 13. Doblecki-Lewis S, Jones D. Community federally qualified health centers as homes for HIV preexposure prophylaxis: perspectives from South Florida. J Int Assoc Provid AIDS Care. 2016;15(6):522–528. [DOI] [PubMed] [Google Scholar]
- 14. Hoots BE, Finlayson T, Nerlander L, Paz-Bailey G; National HIV Behavioral Surveillance Study Group. Willingness to take, use of, and indications for pre-exposure prophylaxis among men who have sex with men—20 US cities, 2014. Clin Infect Dis. 2016;63(5):672–677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Spinelli MA, Scott HM, Vittinghoff E, et al. A panel management and patient navigation intervention is associated with earlier PrEP initiation in a safety-net primary care health system. J Acquir Immune Defic Syndr. 2018;79(3):347–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Center for Disease Control and Prevention. (2014). Pre-Exposure Prophylaxis for the Prevention of HIV in the United States. Clinical Practice Guideline. May 14, 2014. Retrieved from http://www.cdc.gov/hiv/pdf/PrEPguidelines2014.pdf. [Google Scholar]
- 17. Koester KA, Fuller SM, Maiorana A, et al. Implementing multi-level interventions to improve HIV testing, linkage-to-and retention-in-care interventions. J Health Care Poor Underserved. 2016;27(3):1234–1251. [DOI] [PubMed] [Google Scholar]
- 18. R Core Team. R: A Language And Environment For Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing; 2017. [Google Scholar]
- 19. King HL, Keller SB, Giancola MA, et al. Pre-exposure prophylaxis accessibility research and evaluation (PrEPARE Study). AIDS Behav. 2014;18(9):1722–1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tripathi A, Ogbuanu C, Monger M, Gibson JJ, Duffus WA. Preexposure prophylaxis for HIV infection: healthcare providers’ knowledge, perception, and willingness to adopt future implementation in the southern US. South Med J. 2012;105(4):199–206. [DOI] [PubMed] [Google Scholar]
- 21. Shrestha RK, Sansom SL, Purcell DW. Assessing HIV acquisition risks among men who have sex with men in the United States of America. Rev Panam Salud Publica. 2016;40(6)474–478. [PMC free article] [PubMed] [Google Scholar]
- 22. Lieb S, Prejean J, Thompson DR, et al. HIV prevalence rates among men who have sex with men in the southern United States: population-based estimates by race/ethnicity. AIDS Behav. 2011;15(3):596–606. [DOI] [PubMed] [Google Scholar]