Abstract
Current guidelines suggest that HIV-infected patients should receive chemoprophylaxis against Pneumocystis jirovecii pneumonia (PJP) if they have a cluster determinant 4 (CD4) count <200 cells/mm3 or oropharyngeal candidiasis. Persons with CD4 percentage (CD4%) below 14% should also be considered for prophylaxis. Discordance between CD4 count and CD4% occurs in 16% to 25% of HIV-infected patients. Provider compliance with current PJP prophylaxis guidelines when such discordance is present was assessed. Electronic medical records of 429 HIV-infected individuals who had CD4 count and CD4% measured at our clinic were reviewed. CD4 count and percentage discordance was seen in 57 (13%) of 429. Patients with CD4 count >200 but CD4% <14 were significantly less likely to be prescribed PJP prophylaxis compared with those who had CD4 count <200 and CD4% >14 (29% versus 86%; odds ratio = 0.064, 95% confidence interval: 0.0168-0.2436; P < .0001). We emphasize monitoring both the absolute CD4 count and percentage to appropriately guide PJP primary and secondary prophylaxis.
Keywords: CD4 count, CD4 %, Pneumocystis jirovecii pneumonia, prophylaxis
Background
The absolute count of human helper T lymphocytes that express cluster determinant 4 (CD4) count is pivotal in the management of HIV infection and in determining immune function and serving as an indicator of when to start prophylaxis against opportunistic infections. Current guidelines1 suggest that HIV-infected patients should receive chemoprophylaxis against Pneumocystis jirovecii pneumonia (PJP) if they have a CD4 count of less than 200 cells/mm3 or a history of oropharyngeal candidiasis. Guidelines also recommend that persons with a CD4 percentage (CD4%) below 14% should also be considered for prophylaxis.1-3 Physicians are often faced with a discordant CD4 count/CD4% pair. Previous studies of discordant CD4 count and CD4% have focused on how it predicts disease progression in HIV and how it influences outcomes on antiretroviral therapy (ART),4 but no study has evaluated how such discordance affects provider compliance with current guidelines on PJP prophylaxis. This study was conducted to assess provider compliance with current PJP prophylaxis guidelines when discordance between CD4 count and CD4% is present.
Methods
This study was a retrospective chart review of the electronic medical records of HIV-infected patients receiving care at Harlem Hospital’s Infectious Diseases (ID) Clinic. Over 1000 HIV-infected patients receive HIV primary care in the hospital’s ID clinic. Patient information from all visits is stored in an electronic database (Discoverer Plus). Records of HIV-infected patients who had absolute CD4 count and CD4% measured at the ID clinic during the study period July 2010 to April 2011 were reviewed. Patients with a CD4 count >200 but a CD4% <14 and conversely a CD4 count <200 but CD4% >14 were defined to have a CD4 discordance. Discordance A (Dis-A) included patients with CD4 count >200 and CD4% <14 and discordance B (Dis-B) included patients with CD4 count <200 but CD4% >14.
We reviewed whether patients with CD4 discordance were on PJP prophylaxis 6 months prior and 6 months after their CD4 count/CD4% pair in question was measured. Any form of PJP prophylaxis including trimethoprim–sulfamethoxazole (TMP-SMX), atovaquone, dapsone, and pentamidine was considered. Development of PJP, hospital admissions for respiratory illness other than PJP (eg, bronchitis and pneumonia), viral load, and ART were also assessed.
Odds ratios were calculated and χ2 or Fisher exact test were used to assess associations for categorical variables. Statistical analyses were executed with SAS version 9.2 (SAS Institute, Inc).
Results
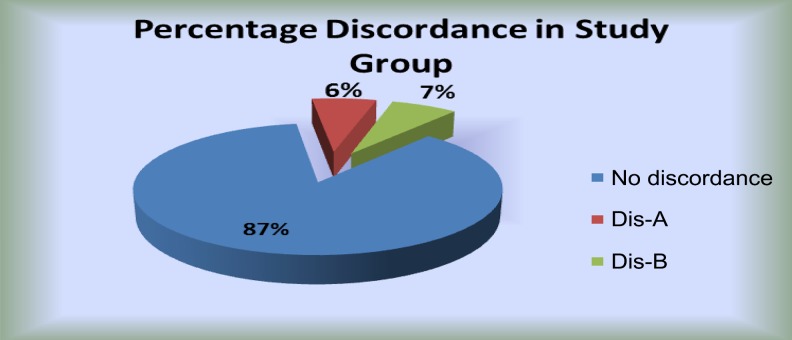
A total of 429 HIV-infected patients had absolute CD4 count and CD4% measured at the ID clinic during the study period; 53% were male, 81% were black (non-Hispanic), 15% Hispanic, and 2% white (see Table 1). Absolute CD4 count and percentage discordance was seen in 57 (13%) of 429; 28 (6.5%) of 429 had Dis-A and 29 (6.7%) of 429 had Dis-B (Figure 1).
Table 1.
Demographics of study population.
| Dis A,a n (%) | Dis B,b n (%) | |
|---|---|---|
| Male | 14 (63) | 13 (45) |
| Female | 8 (37) | 16 (55) |
| African American | 14 (63) | 15 (51) |
| Hispanic | 8 (37) | 12 (41) |
| Caucasian | 0 (0) | 2 (7) |
| Total patients | 22 | 29 |
Abbreviations: CD4, cluster determinant 4; Dis, discordance.
aDis A—CD4 >200 and CD4% <14.
bDis B—CD4 <200 and CD4% >14.
Figure 1.
Percentage discordance in study group.
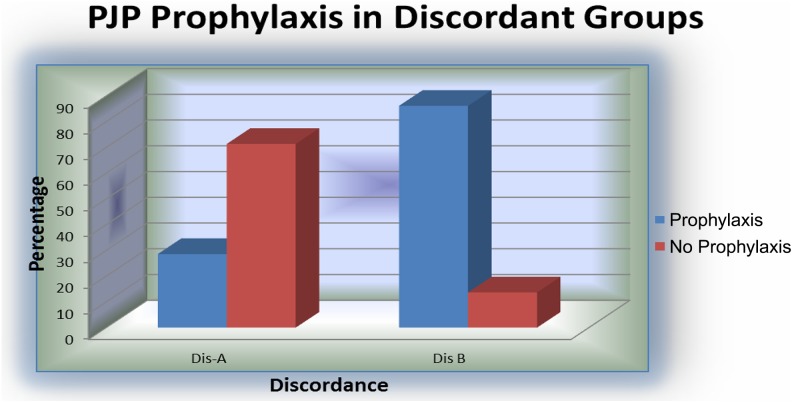
Use of PJP prophylaxis varied by the type of discordance (Figure 2). One hundred thirty-nine patients had CD4 percentage ≤14%, and 28 of these had Dis-A. Twenty (71.4%) of 28 patients with Dis-A were not on PJP prophylaxis; the 8 (28.6%) of 28 patients on PJP prophylaxis all were receiving TMP-SMX. Two hundred ninety patients had a CD4% >14, and of these, 29 had Dis-B. Only 4 (13.7%) of 29 patients with Dis-B were not on PJP prophylaxis. Of the 25 (86.2%) of 29 patients on PJP prophylaxis, 6 were receiving atovaquone and 19 TMP-SMX. Patients in the Dis-A group were significantly less likely to be on PJP prophylaxis compared to patients in the Dis-B group (P < .0001, OR = 0.064, 95% CI: 0.0168-0.2436).
Figure 2.
Pneumocystis jirovecii pneumonia prophylaxis in discordant groups.
Seventeen (60.7%) of 28 patients in the Dis-A group were prescribed ART and 16 (55.2%) of 29 patients in the Dis-B were prescribed ART. History of oral candida was comparable in both groups, including 3 (10.7%) of 28 in the Dis-A group and 3 (10.3%) of 29 in the Dis-B.
Detectable HIV viremia was present in 87.5% in the Dis A group compared to 71.4% in the Dis B group. One patient in the Dis-A group on ART with a CD4 count of 680 cells/mm3 (nadir CD4 count 289) and CD4% of 6% had been hospitalized with presumed PJP. No patient in the Dis-B group had PJP.
Three patients in the Dis-A group were admitted to the hospital for respiratory illnesses other than PJP, all of these patients were not on PJP prophylaxis. Ten patients in the Dis-B group were admitted for respiratory illnesses; 9 of these 10 patients were on PJP prophylaxis (7 on TMP-SMX and 2 on atovaquone).
Discussion
The absolute CD4 count is pivotal in the management of HIV infection, as a marker of immune function and a determinant of when to start prophylaxis against opportunistic infections.1 The absolute CD4 count is a product of the CD4% derived from flow cytometry and the complete white blood cell count and lymphocyte differential.5,6 A gating strategy for identifying lymphocytes using CD45 fluorescence and side-scattering characteristics is available and is the preferred method for identifying lymphocytes accurately and reproducibly.7 Unfortunately, multiple factors including but not limited to medications, chemotherapy,8 steroids,9 infections,10 smoking,11 alcohol,12 and diurnal changes13 affect the absolute CD4 count, making the CD4% a less variable indicator.14
Although CD4 count and CD4% are highly correlated, these correlations are not perfect.4,5 Discordance between CD4 count and CD4% has been well-documented in previous studies,4,15-18 occurring in 16% to 25% of HIV-infected patients.17,18 However, the clinical relevance of this discordance remains unclear.4 Unfortunately, there is no standard definition for CD4 count and CD4% discordance, but our definition (Dis-A and Dis-B above) is similar to definitions used in previous studies.15,16 In patients with HIV-1 infection, CD4 count predicts development of opportunistic illnesses and death due to AIDS.16-20 On the other hand, other studies have found CD4% as predictive of the risk of clinical progression independent of CD4 count.17,18,21 In a large study of 1020 asymptomatic HIV-infected individuals, the intrasubject coefficient of variation for CD4 count was 25% compared to 18% for the CD4%.22
In our study, we found a 13% discordance between CD4 count and CD4%. Based on our findings, it was obvious that most providers when faced with the clinical dilemma of a discordant CD4 count–CD4% pair tended to focus on the absolute CD4 count for PJP prophylaxis. One individual in the Dis-A group who was receiving ART with a CD4 count of 680 cells/mm3 and CD4% of 6% had presumed PJP based on clinical symptoms and complete recovery after treatment with TMP-SMX. He was not on PJP prophylaxis. This emphasizes the importance of PJP prophylaxis for patients with such discordance. No patient developed presumed or confirmed PJP in the Dis-B group, but contrary to our expectation, more patients in this group were admitted for respiratory infections (10/29 patients, 9/10 patients were on TMP-SMX and 3 had confirmed bacterial infections). We expected TMP-SMX at a dose of 1 double-strength tablet daily to confer protection against some common respiratory bacterial infections.23,24 Our study however is limited by the small number of patients with the CD4 count and percentage discordance and the lack of data on adherence to medications.
Some studies have suggested that primary pneumocystis prophylaxis may not be necessary for individuals who are virologically suppressed on ART with CD4 counts of 100 to 200, given the low incidence of PJP in this group.25,26 Unfortunately, only 30% of the total estimated HIV-infected population in the United States are virologically suppressed.27 Pneumocystis jirovecii pneumonia remains a major threat to HIV-infected individuals because of late HIV diagnosis and poor antiretroviral adherence.
A 1259-person study from France found that almost half of HIV-infected persons with newly diagnosed PJP had already entered HIV care, and three quarters of that group had started ART.28 Provider knowledge and vigilance in all aspects of PJP prophylaxis is necessary in preventing Pneumocystis pneumonia in HIV-infected patients.
Guidelines currently recommend that PJP prophylaxis should be discontinued in HIV-infected patients who have responded to ART with an increase in CD4 count to greater than 200 cells/mm3 for greater than 3 months.1,29-31 It is not clear when to discontinue PJP prophylaxis after starting solely based on a CD4%, but in the studies29-31 supporting the above recommendation, most patients at the time of discontinuing prophylaxis had a CD4% greater than or equal to 14%.
Conclusion
In this study, the use of PJP prophylaxis seemed to be determined more by the CD4 count than the CD4%. Although our study is based on a retrospective medical record review, it forms a platform for further studies to better understand the clinical relevance of CD4 count and percentage in determining PJP prophylaxis. We emphasize monitoring both the absolute CD4 count and percentage to appropriately guide PJP primary and secondary prophylaxis in accordance with current guidelines.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Masur H. Panel on Opportunistic Infections in HIV-Infected Adults and Adolescents. Guidelines for the prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from the Centers for Disease Control and Prevention, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. http://aidsinfo.nih.gov/contentfiles/lvguidelines/adult_oi.pdf. Accessed June 3, 2017. [PubMed]
- 2. Phair J, Muñoz A, Detels R, Kaslow R, Rinaldo C, Saah A. The risk of Pneumocystis carinii pneumonia among men infected with human immunodeficiency virus type 1. Multicenter aids cohort study group. N Engl J Med. 1990;322(3):161–165. [DOI] [PubMed] [Google Scholar]
- 3. Kaplan JE, Hanson DL, Navin TR, Jones JL. Risk factors for primary Pneumocystis carinii pneumonia in human immunodeficiency virus-infected adolescents and adults in the United States: reassessment of indications for chemoprophylaxis. J Infect Dis. 1998;178(4):1126–1132. [DOI] [PubMed] [Google Scholar]
- 4. Gompels M, Dunn DT, Phillips A, et al. Does discordancy between the CD4 count and CD4 percentage in HIV-positive individuals influence outcomes on highly active antiretroviral therapy? J Infect Dis. 2012;205(4):540–547. [DOI] [PubMed] [Google Scholar]
- 5. Goicoechea M, Haubrich R. CD4 lymphocyte percentage versus absolute CD4 lymphocyte count in predicting HIV disease progression: an old debate revisited. J Infect Dis. 2005;192(6):945–947. [DOI] [PubMed] [Google Scholar]
- 6. 1997 revised guidelines for performing CD4+ T-cell determinations in persons infected with human immunodeficiency virus (HIV). Centers for Disease Control and Prevention. MMWR Recomm Rep. 1997;46(RR-2):1–29. [PubMed] [Google Scholar]
- 7. Mandy FF, Nicholson JK, McDougal JS; CDC. Guidelines for performing single-platform absolute CD4+ T-cell determinations with CD45 gating for persons infected with human immunodeficiency virus. Centers for Disease Control and Prevention. MMWR Recomm Rep. 2003;52(RR-2):1–13. [PubMed] [Google Scholar]
- 8. Vedel SJ, Tholstrup D, Kolte L, et al. Limited impact of the thymus on immunological recovery during and after chemotherapy in patients with diffuse large B-cell lymphoma. Scand J Immunol. 2009;69(6):547–554. [DOI] [PubMed] [Google Scholar]
- 9. Bloemena E, Weinreich S, Schellekens PT. The influence of prednisolone on the recirculation of peripheral blood lymphocytes in vivo. Clin Exp Immunol. 1990;80(3):460–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schechter M, Harrison LH, Halsey NA, et al. Coinfection with human T-cell lymphotropic virus type I and HIV in Brazil. Impact on markers of HIV disease progression. JAMA. 1994;271(5):353–357. [PubMed] [Google Scholar]
- 11. Mili F, Flanders WD, Boring JR, Annest JL, Destefano F. The associations of race, cigarette smoking, and smoking cessation to measures of the immune system in middle-aged men. Clin Immunol Immunopathol. 1991;59(2):187–200. [DOI] [PubMed] [Google Scholar]
- 12. Pol S, Artru P, Thépot V, Berthelot P, Nalpas B. Improvement of the CD4 cell count after alcohol withdrawal in HIV-positive alcoholic patients. AIDS. 1996;10(11):1293–1294. [DOI] [PubMed] [Google Scholar]
- 13. Malone JL, Simms TE, Gray GC, Wagner KF, Burge JR, Burke DS. Sources of variability in repeated T-helper lymphocyte counts from human immunodeficiency virus type 1-infected patients: total lymphocyte count fluctuations and diurnal cycle are important. J Acquir Immune Defic Syndr. 1990;3(2):144–151. [PubMed] [Google Scholar]
- 14. Taylor JM, Fahey JL, Detels R, Giorgi JV. CD4 percentage, CD4 number, and CD4: CD8 ratio in HIV infection: which to choose and how to use. J Acquir Immune Defic Syndr. 1989;2(2):114–124. [PubMed] [Google Scholar]
- 15. Le TP, Tribble DR, Zhou SY, et al. Clinical significance of discordant CD4 count and CD4 percentage in HIV-infected individuals. AIDS. 1997;11(11):1395–1396. [PubMed] [Google Scholar]
- 16. Gebo KA, Gallant JE, Keruly JC, Moore RD. Absolute CD4 vs. CD4 percentage for predicting the risk of opportunistic illness in HIV infection. J Acquir Immune Defic Syndr. 2004;36(5):1028–1033. [DOI] [PubMed] [Google Scholar]
- 17. Hulgan T, Raffanti S, Kheshti A, et al. CD4 lymphocyte percentage predicts disease progression in HIV-infected patients initiating highly active antiretroviral therapy with CD4 lymphocyte counts >350 lymphocytes/mm3 . J Infect Dis. 2005;192(6):950–957. [DOI] [PubMed] [Google Scholar]
- 18. Hulgan T, Shepherd BE, Raffanti SP. Absolute count and percentage of CD4+ lymphocytes are independent predictors of disease progression in HIV-infected persons initiating highly active antiretroviral therapy. J Infect Dis. 2007;195(3):425–431. [DOI] [PubMed] [Google Scholar]
- 19. Cameron DW, Heath-Chiozzi M, Danner S, et al. Randomised placebo-controlled trial of ritonavir in advanced HIV-1 disease. The advanced HIV Disease Ritonavir Study Group. Lancet. 1998;351(9102):543–549. [DOI] [PubMed] [Google Scholar]
- 20. Hammer SM, Squires KE, Hughes MD, et al. A controlled trial of two nucleoside analogues plus indinavir in persons with human immunodeficiency virus infection and CD4 cell counts of 200 per cubic millimeter or less. AIDS Clinical Trials Group 320 Study Team. N Engl J Med. 1997;337(11):725–733. [DOI] [PubMed] [Google Scholar]
- 21. Guiguet M, Kendjo E, Carcelain G, et al. CD4+ T-cell percentage is an independent predictor of clinical progression in AIDS-free antiretroviral-naive patients with CD4+ T-cell counts >200 cells/mm3 . Antivir Ther. 2009;14(3):451–457. [DOI] [PubMed] [Google Scholar]
- 22. Hughes MD, Stein DS, Gundacker HM, Valentine FT, Phair JP, Volberding PA. Within-subject variation in CD4 lymphocyte count in asymptomatic human immunodeficiency virus infection: implications for patient monitoring. J Infect Dis. 1994;169(1):28–36. [DOI] [PubMed] [Google Scholar]
- 23. Bozzette SA, Finkelstein DM, Spector SA, et al. A randomized trial of three antipneumocystis agents in patients with advanced human immunodeficiency virus infection. NIAID AIDS Clinical Trials Group. N Engl J Med. 1995;332(11):693–699. [DOI] [PubMed] [Google Scholar]
- 24. Hardy WD, Feinberg J, Finkelstein DM, et al. A controlled trial of trimethoprim-sulfamethoxazole or aerosolized pentamidine for secondary prophylaxis of Pneumocystis carinii pneumonia in patients with the acquired immunodeficiency syndrome. AIDS Clinical Trials Group Protocol 021. N Engl J Med. 1992;327(26):1842–1848. [DOI] [PubMed] [Google Scholar]
- 25. Costiniuk CT, Fergusson DA, Doucette S, Angel JB. Discontinuation of Pneumocystis jirovecii pneumonia prophylaxis with CD4 count <200 cells/μL and virologic suppression: a systematic review. PLoS One. 2011;6(12):e28570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Opportunistic Infections Project Team of the Collaboration of Observational HIV Epidemiological Research in Europe (COHERE), Mocroft A, Reiss P, Kirk O, et al. Is it safe to discontinue primary Pneumocystis jiroveci pneumonia prophylaxis in patients with virologically suppressed HIV infection and a CD4 cell count<200 cells/microL? Clin Infect Dis. 2010;51(5):611–619. [DOI] [PubMed] [Google Scholar]
- 27. Centers for Disease Control and Prevention (CDC). Vital signs: HIV Diagnosis, Care and Treatment Among Persons Living with HIV–United States, 2011. MMWR Morb Mortal Wkly Rep. 2014; 63(47):1113–1117. http://www.ncbi.nlm.nih.gov/pubmed/25426654. [PMC free article] [PubMed] [Google Scholar]
- 28. Denis B, Guiguet M, Gregoire G, et al. Pneumocystis jirovecii pneumonia (PCP) in HIV infected patients in France in the combined antiretroviral therapy (cART) era is associated with late presentation or poor adherence. Paper presented at: 53rd Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC); 2013; Denver, CO Abstract H-1260 http://www.natap.org/2013/ICAAC/ICAAC_79.htm. Accessed June 4, 2017. [Google Scholar]
- 29. Dworkin MS, Hanson DL, Kaplan JE, Jones JL, Ward JW. Risk for preventable opportunistic infections in persons with AIDS after antiretroviral therapy increases CD4+ T lymphocyte counts above prophylaxis thresholds. J Infect Dis. 2000;182(2):611–615. [DOI] [PubMed] [Google Scholar]
- 30. Furrer H, Egger M, Opravil M, et al. Discontinuation of primary prophylaxis against Pneumocystis carinii pneumonia in HIV-1-infected adults treated with combination antiretroviral therapy. Swiss HIV Cohort Study. N Engl J Med. 1999;340(17):1301–1306. [DOI] [PubMed] [Google Scholar]
- 31. Green H, Hay P, Dunn DT, McCormack S; STOPIT Investigators. A prospective multicentre study of discontinuing prophylaxis for opportunistic infections after effective antiretroviral therapy. HIV Med. 2004;5(4):278–283. [DOI] [PubMed] [Google Scholar]