Abstract
The World Health Organization recommended removing all CD4 requirements for initiation of antiretroviral therapy (ART) in resource-limited settings. We examined the pre-ART period to identify and assess factors associated with outcomes of pre-ART care. Four modes of transition out of pre-ART care were considered. Beta estimates from the competing risks Cox models were used to investigate whether the effects of covariates differed by mode of transition. Median CD4 counts at entry showed no meaningful change over time. Advanced disease progression and presence of opportunistic infections were significant predictors of pre-ART mortality. Men were more likely to die before initiating ART, transfer to another facility, or be lost to follow-up than were women. Removing CD4 thresholds is not likely to substantially reduce program mortality prior to ART initiation unless and until patients enroll earlier in disease progression. Care programs should focus on diagnosis and treatment of opportunistic infections to reduce pre-ART mortality.
Keywords: HIV, pre-ART period, treatment guidelines, opportunistic infections, competing risks analysis
Introduction
Since antiretroviral therapy (ART) became widely available to patients in developing countries, public health programs have had to balance clinical science with resource constraints. In 2006, the World Health Organization (WHO) was recommending treatment only for people living with HIV (PLHIV) with CD4 counts lower than 200cells/mm3 or with a WHO clinical stage of III or IV.1 After 3 years, the threshold was raised to 3502 and to 500 in 2013.3 On September 30, 2015, the WHO recommended the removal of all CD4 restrictions to treatment initiation for PLHIV in resource-limited settings.4
Clinical eligibility criteria have historically been the sole threshold to starting treatment. There is little evidence that people are presenting for care substantially earlier in disease progression than they were a decade ago5,6; therefore, the new guidelines may not have a great impact on the timing of ART initiation for most PLHIV in resource-limited settings. Without effective changes in program practices in the pre-ART period—the time between enrollment for care and initiation of ART—we can expect that many of the same factors that limit the successful initiation of ART observed previously will persist even under the new treatment guidelines.
Many countries may lack resources to implement the 2015 recommendations immediately. Until they are able, programs should identify and assess factors associated with transition from pre-ART care, in addition to presenting CD4 count, and whether these factors can be targeted to reduce transition from pre-ART care for reasons other than initiating treatment. It is during this period that patients gain ART readiness—diagnosis and treatment of opportunistic infections and acquisition of treatment literacy and support mechanisms for lifelong adherence to treatment. This period is arguably the most neglected phase of the HIV continuum of care.
While most literature from international HIV programs focused on treatment outcomes—the period after ART is initiated—there is a growing body of literature on outcomes during the pre-ART period. Several studies have reported higher program loss, lower ART initiation, and/or higher pre-ART mortality among men than among women,7-13 while others have found no difference by sex.14-16 Analyses of the effect of patient’s age at enrollment have also found mixed results, with some studies reporting greater attrition prior to ART initiation among younger patients,10,11,13,15 and other studies finding no age differences.7-9,12,14 The impact of disease progression at enrollment (CD4 count and WHO stage) is difficult to compare across studies because of differences in selection criteria.
The objective of this study was to identify factors associated with transition from pre-ART care and determine whether those factors differ by mode of transition. The present study adds to the evidence base with analysis of patient records from AIDSRelief, a large-scale care and treatment program funded under the President’s Emergency Plan for AIDS Relief (PEPFAR).
Methods
Data Source
We conducted a retrospective cohort study of all adults enrolled in all HIV care and treatment facilities supported by AIDSRelief in Kenya (33 sites) and Tanzania (78 sites). Records were obtained from approximately 140 000 people receiving care and treatment in Kenya and approximately 142 352 people receiving care and treatment in Tanzania between August 1, 2004, and September 30, 2011.17 During the study observation period, the national treatment eligibility threshold in both countries was CD4 <200 cells/mm3 in the absence of other signs of advanced HIV disease. Data were collected in each facility during routine clinical visits. The data were extracted from each clinical database, all identifying patient information was removed, and patients and clinics were assigned randomly generated identification numbers. The key linking patient names to identification numbers was destroyed. Use of the deidentified data for this study was approved by the ethics committee of the Kenya Medical Research Institute and the Tanzania National Medical Research Institute IRB.
Study Sample
To be eligible for inclusion in the analysis, patients must have been HIV-infected and be at least 15 years of age at the time of enrollment into care.
Statistical Analysis
The outcome variable for this study was transition from pre-ART care by mode of transition. We classified patient transition from pre-ART care into 4 mutually exclusive categories: started ART (irrespective of treatment outcome), died before ART initiation, lost to follow-up (LTFU; no contact with the facility for 6 months), or transferred to another facility. Mode of transition was actively ascertained during the routine provision of care. Patients whose status could not be ascertained were classified as LTFU. Patients who had not experienced one of the transition events at the end of the observation period were classified as remained in care and censored at the end of follow-up.
Baseline covariates that were investigated for their relationship with mode of transition included sex, age at enrollment, CD4 count at enrollment, presence of tuberculosis at enrollment, presence of cryptococcal disease at enrollment, presence of Pneumocystis jiroveci pneumonia (PCP) at enrollment, presence of other active opportunistic infections, and year of enrollment in care.
Age was categorized into 5 groups: 15 to 25, 26 to 35, 36 to 45, 46 to 55, and older than 55. Baseline CD4 count was classified into 5 standard clinically relevant categories: 0 to 50, 51 to 100, 101 to 200, 201 to 350, and >350 or missing. Year of enrollment in care took a value from 2004 to 2011. All other variables were treated as dichotomous.
Data were first investigated using univariate analysis to describe the frequency and distribution of the outcome and covariates. Data were then analyzed for bivariate associations with the outcomes to determine crude associations. To investigate whether the effects of the covariates are the same or differ by mode of transition from pre-ART care, we conducted a competing risks analysis using life table methods and Cox models. We fit Cox models with type of transition as the outcome of interest and compared the covariate estimates. To test the null hypothesis that all β estimates are equal across all types of transition, we summed the −2 log likelihood statistics for all 4 transition types and subtracted it from the −2 log likelihood statistic from a combined data set, where each patient based on his or her mode of transition has a specific transition event and is censored for the other 3 types. We then created a likelihood ratio chi-square statistic. To determine whether the β-estimates differ across modes of transition, we constructed Wald chi-square statistics for each pairwise comparison. Cause-specific hazard ratios for each mode of transition are presented. All data were analyzed using SAS 9.4 (Cary, North Carolina).
Results
Between August 1, 2004, and September 30, 2011, 101 821 patients and 123 070 patients aged 15 or older were enrolled in the Kenya and Tanzania AIDSRelief-supported clinics, respectively. After excluding patients with previous ART experience and a small number of patients subsequently found to be HIV negative, there were records from 77 626 ART-naive patients in Kenya and 117 385 ART-naive patients in Tanzania for analysis (see supplemental Figure 1).
In both countries, one-third of the enrolled patients were men (Kenya 32% and Tanzania 33%; Table 1). Men on average were older than women at enrollment (Kenya: 39.7 versus 34.6 years; Tanzania: 40.2 versus 35.1), had a lower mean CD4 count (Kenya 364 versus 285, Tanzania 293 versus 235), and had a higher proportion of recorded opportunistic infections (Kenya 31% versus 24%, Tanzania 12% versus 10%).
Table 1.
Baseline Characteristics of Study Sample by Country.
| Characteristic | Kenya (n = 77 626), n (%) | Tanzania (n = 117 385), n (%) |
|---|---|---|
| Year of enrollment | ||
| 2004 (5 months) | 732 (0.9) | 249 (0.2) |
| 2005 | 3397 (4.4) | 6101 (5.2) |
| 2006 | 4543 (5.9) | 12 750 (10.9) |
| 2007 | 8178 (10.5) | 19 620 (16.7) |
| 2008 | 18 201 (23.4) | 22 386 (19.1) |
| 2009 | 17 291 (22.3) | 23 671 (20.2) |
| 2010 | 16 427 (21.2) | 19 857 (16.9) |
| 2011 (9 months) | 8857 (11.4) | 12 751 (10.9) |
| Gender | ||
| Male | 24 881 (32.1) | 38 337 (32.7) |
| Female | 52 745 (67.9) | 79 045 (67.3) |
| Age, years | ||
| Median (IQR) | 34.6 (28.3, 42.5) | 35.3 (29.2, 42.5) |
| 15-25 | 12 887 (16.6) | 16 140 (13.7) |
| 26-35 | 29 995 (38.6) | 46 132 (39.3) |
| 36-45 | 20 875 (26.9) | 34 047 (29.0) |
| 46-55 | 9734 (12.5) | 14 662 (12.5) |
| 55+ | 4135 (5.3) | 6404 (5.5) |
| CD4 count, mm3 | ||
| Median (IQR) | 286 (131, 481) | 205 (83, 391) |
| ≤50 | 5711 (7.4) | 11 248 (9.6) |
| 51-100 | 4899 (6.3) | 8279 (7.1) |
| 101-200 | 9285 (12.0) | 13 492 (11.5) |
| 201-350 | 12 161 (15.7) | 14 326 (12.2) |
| >350 | 22 222 (28.6) | 19 646 (16.7) |
| Missing | 23 348 (30.1) | 50 394 (42.9) |
| Opportunistic infections | ||
| Tuberculosis | ||
| Yes | 11 086 (14.3) | 737 (0.6) |
| No | 66 540 (85.7) | 11 6648 (99.4) |
| Cryptococcal disease | ||
| Yes | 386 (0.5) | 37 (0.1) |
| No | 77 240 (99.5) | 117 348 (99.9) |
| Pneumocystis jiroveci pneumonia | ||
| Yes | 2752 (3.5) | 399 (0.3) |
| No | 74 874 (96.5) | 116 986 (99.7) |
| Othera | ||
| Yes | 20 545 (26.5) | 12 920 (11.0) |
| No | 57 081 (73.5) | 104 465 (89.0) |
| Facility location | ||
| Urban | 7966 (10.3) | 90 769 (77.3) |
| Peri-urban | 20 466 (26.4) | 5768 (4.9) |
| Rural | 49 194 (63.4) | 20 848 (17.8) |
| Facility type | ||
| Primary | 12 574 (16.2) | 18 661 (15.9) |
| Secondary | 65 052 (83.8) | 88 977 (75.8) |
| Tertiary | 0 (0.0) | 9747 (8.3) |
Abbreviations: IQR, interquartile range; WHO, World Health Organization.
aAll opportunistic infections used for WHO disease staging other than tuberculosis, cryptococcal disease, and Pneumocystis jiroveci pneumonia.
Program enrollment peaked in 2008/2009. Examination of CD4 counts at entry shows no clinically meaningful change over the period 2008 to 2011 (Table 2).
Table 2.
Median CD4 Count and Interquartile Range (IQR) at Enrollment From 2008 to 2011.
| 2008 | 2009 | 2010 | 2011 | |
|---|---|---|---|---|
| Kenya | ||||
| Median CD4 | 262 | 277 | 277 | 285 |
| (IQR) | (119-451) | (129-466) | (132-461) | (137-476) |
| % Missing | 36 | 20 | 17 | 17 |
| Tanzania | ||||
| Median CD4 | 214 | 235 | 224 | 213 |
| (IQR) | (86-410) | (98-429) | (86-409) | (82-395) |
| % Missing | 35 | 37 | 50 | 48 |
Mode of Transition
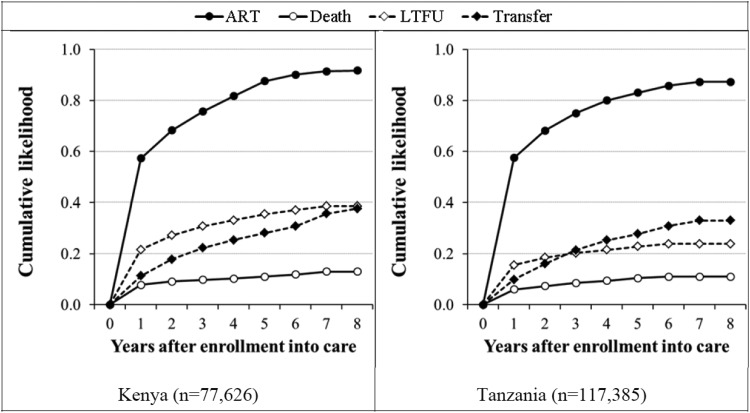
In both countries, the greatest probability for transition from pre-ART care for any reason occurred in the first year after a patient’s enrollment. Initiation of ART was the predominant mode of transition (Figure 1). After the first year, the probability of death as a competing risk for all other modes of attrition remained relatively flat.
Figure 1.
Initiation of antiretroviral therapy, death, loss to follow-up, and transfers among patients in Kenya and Tanzania.* * indicates the competing risk life table curves have been inverted for ease of interpretation.
With 2 countries, 4 modes of transition, and 8 predictor variables, some with multiple levels, there are 168 opportunities to obtain statistically significant adjusted hazard rates (aHR) as well as 126 comparisons of predictor effects on mode of transition per country. For completeness, all aHR results are presented in Tables 3 and 4. In the text subsequently, we focus on those findings that we believe have the most programmatic relevance.
Table 3.
Competing Risks Cause Specific Adjusted Hazard Ratios (aHR) for Mode of Transition from Pre-ART Care in Kenya.a
| Characteristic | Started ART | Died | Lost to Follow-Up | Transferred |
|---|---|---|---|---|
| aHR (95% CI) | aHR (95% CI) | aHR (95% CI) | aHR (95% CI) | |
| Sex | ||||
| Female | 1.0 | 1.0 | 1.0 | 1.0 |
| Male | 1.00 (0.99-1.01) | 1.54 (1.49-1.59) | 1.24 (1.22-1.27) | 1.22 (1.18-1.25) |
| Age in years | ||||
| 15-25 | 1.0 | 1.0 | 1.0 | 1.0 |
| 26-35 | 1.17 (1.15-1.18) | 1.11 (1.06-1.17) | 0.66 (0.65-0.68) | 0.73 (0.71-0.75) |
| 36-45 | 1.29 (1.27-1.31) | 1.11 (1.05-1.17) | 0.54 (0.53-0.56) | 0.60 (0.58-0.62) |
| 46-55 | 1.29 (1.26-1.31) | 1.19 (1.11-1.26) | 0.51 (0.49-0.53) | 0.60 (0.57-0.62) |
| >55 | 1.28 (1.25-1.31) | 1.76 (1.64-1.88) | 0.54 (0.52-0.57) | 0.56 (0.52-0.59) |
| CD4 count/mm3 | ||||
| ≤50 | 1.0 | 1.0 | 1.0 | 1.0 |
| 51-100 | 0.99 (0.97-1.01) | 0.58 (0.55-0.62) | 0.85 (0.79-0.91) | 0.94 (0.85-1.03) |
| 101-200 | 0.97 (0.95-0.99) | 0.32 (0.30-0.34) | 0.85 (0.81-0.90) | 0.86 (0.80-0.93) |
| 201-350 | 0.69 (0.67-0.70) | 0.17 (0.16-0.18) | 0.83 (0.79-0.88) | 0.85 (0.79-0.91) |
| > 350 | 0.12 (0.12-0.12) | 0.09 (0.08-0.10) | 0.76 (0.72-0.80) | 0.80 (0.75-0.86) |
| Missing | 0.31 (0.30-0.31) | 0.46 (0.44-0.48) | 1.58 (1.51-1.65) | 1.36 (1.27-1.45) |
| Opportunistic infections | ||||
| Tuberculosis | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.21 (1.19-1.23) | 0.80 (0.76-0.85) | 0.96 (0.92-0.99) | 0.90 (0.85-0.96) |
| Cryptococcal disease | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.06 (1.00-1.13) | 1.69 (1.48-1.94) | 0.87 (0.74-1.02) | 0.79 (0.61-1.02) |
| PCP | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.79 (0.77-0.81) | 1.41 (1.31-1.52) | 1.03 (0.97-1.09) | 1.12 (1.03-1.21) |
| Other | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.13 (1.12-1.15) | 1.60 (1.53-1.67) | 0.94 (0.91-0.96) | 0.93 (0.89-0.97) |
| Enrollment year | ||||
| 2004 | 0.14 (0.13-0.15) | 2.84 (2.55-3.16) | 4.95 (4.62-5.31) | 0.57 (0.51-0.65) |
| 2005 | 0.17 (0.16-0.18) | 1.95 (1.81-2.10) | 4.18 (3.97-4.40) | 0.50 (0.47-0.53) |
| 2006 | 0.23 (0.22-0.24) | 1.91 (1.76-2.05) | 4.15 (3.95-4.36) | 0.53 (0.50-0.56) |
| 2007 | 0.42 (0.41-0.43) | 1.08 (1.00-1.17) | 3.03 (2.89-3.18) | 0.62 (0.59-0.65) |
| 2008 | 0.75 (0.73-0.76) | 0.89 (0.83-0.95) | 1.99 (1.89-2.08) | 0.75 (0.72-0.78) |
| 2009 | 0.89 (0.87-0.90) | 0.99 (0.92-1.06) | 1.64 (1.57-1.73) | 0.80 (0.76-0.83) |
| 2010 | 1.04 (1.02-1.06) | 0.95 (0.87-1.02) | 1.37 (1.31-1.44) | 0.81 (0.78-0.85) |
| 2011 | 1.0 | 1.0 | 1.0 | 1.0 |
Abbreviations: aHR, Adjusted Hazard Ratios; ART, antiretroviral therapy; CI, confidence interval; PCP, Pneumocystis jiroveci pneumonia.
an = 77 626.
Table 4.
Competing Risks Cause Specific Adjusted Hazard Ratios for Mode of Transition From pre-ART Care in Tanzania.a
| Characteristic | Started ART, aHR (95% CI) | Died, aHR (95% CI) | Lost to follow-up, aHR (95% CI) | Transferred, aHR (95% CI) |
|---|---|---|---|---|
| Sex | ||||
| Female | 1.0 | 1.0 | 1.0 | 1.0 |
| Male | 1.01 (1.00-1.03) | 1.49 (1.40-1.58) | 1.14 (1.10-1.19) | 1.15 (1.09-1.20) |
| Age in years | ||||
| 15-25 | 1.0 | 1.0 | 1.0 | 1.0 |
| 26-35 | 0.73 (0.70-0.76) | 0.67 (0.58-0.78) | 1.42 (1.30-1.54) | 1.01 (0.92-1.12) |
| 36-45 | 0.91 (0.88-0.94) | 0.83 (0.75-0.92) | 1.11 (1.03-1.19) | 0.90 (0.83-0.97) |
| 46-55 | 1.04 (1.01-1.07) | 0.84 (0.75-0.93) | 0.92 (0.85-0.99) | 0.85 (0.79-0.93) |
| > 55 | 1.08 (1.05-1.12) | 0.85 (0.76-0.96) | 0.82 (0.76-0.90) | 0.83 (0.75-0.91) |
| CD4 count/mm3 | ||||
| ≤ 50 | 1.0 | 1.0 | 1.0 | 1.0 |
| 51-100 | 0.90 (0.88-0.93) | 0.62 (0.53-0.72) | 0.94 (0.82-1.07) | 0.98 (0.84-1.15) |
| 101-200 | 0.89 (0.86-0.91) | 0.40 (0.35-0.47) | 0.76 (0.67-0.86) | 0.86 (0.75-0.99) |
| 201-350 | 0.39 (0.38-0.40) | 0.32 (0.27-0.37) | 1.04 (0.94-1.16) | 1.07 (0.95-1.21) |
| > 350 | 0.10 (0.09-0.10) | 0.22 (0.19-0.25) | 1.18 (1.07-1.30) | 1.17 (1.05-1.31) |
| Missing | 0.24 (0.24-0.25) | 0.99 (0.90-1.09) | 2.55 (2.34-2.79) | 1.51 (1.36-1.68) |
| Opportunistic Infections | ||||
| Tuberculosis | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.72 (0.65-0.80) | 0.95 (0.72-1.26) | 1.06 (0.89-1.26) | 1.15 (0.90-1.46) |
| Cryptococcal disease | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 2.08 (1.42-3.05) | 3.40 (1.61-7.15) | 0.20 (0.03-1.45) | 0.50 (0.07-3.53) |
| PCP | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.75 (1.55-1.97) | 1.24 (0.86-1.80) | 0.46 (0.32-0.65) | 0.94 (0.63-1.40) |
| Other | ||||
| No | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.94 (0.92-0.96) | 1.36 (1.25-1.48) | 1.16 (1.10-1.22) | 1.10 (1.02-1.17) |
| Enrollment year | ||||
| 2004 | 1.30 (1.10-1.55) | 3.08 (2.01-4.70) | 3.27 (2.12-5.05) | 1.48 (0.91-2.41) |
| 2005 | 1.02 (0.98-1.07) | 2.22 (1.90-2.59) | 9.66 (8.94-10.98) | 1.74 (1.52-1.99) |
| 2006 | 0.90 (0.87-0.94) | 2.25 (1.97-2.57) | 9.86 (8.73-11.13) | 1.81 (1.62-2.03) |
| 2007 | 0.88 (0.85-0.91) | 1.71 (1.50-1.95) | 6.70 (5.94-7.56) | 1.67 (1.50-1.86) |
| 2008 | 0.95 (0.92-0.99) | 1.47 (1.28-1.68) | 3.30 (2.91-3.73) | 1.95 (1.76-2.17) |
| 2009 | 0.95 (0.92-0.98) | 1.26 (1.10-1.44) | 2.35 (2.07-2.67) | 1.75 (1.57-1.94) |
| 2010 | 0.99 (0.96-1.03) | 0.90 (0.77-1.04) | 1.82 (1.59-2.08) | 1.20 (1.07-1.35) |
| 2011 | 1.0 | 1.0 | 1.0 | 1.0 |
Abbreviations: aHR, adjusted hazard ratios; ART, antiretroviral therapy; CI, confidence interval; PCP, Pneumocystis jiroveci pneumonia.
an = 117 385.
Associations between year of enrollment and mode of transition
Both countries showed declines in the hazard ratios for pre-ART mortality and LTFU, over the period 2004 to 2011. In Kenya, earlier years were associated with a decreased hazard for starting ART. In Tanzania, year was not meaningfully associated with the hazard of starting ART.
Associations between clinical status at enrollment and mode of transition
In both countries, the risk of pre-ART mortality decreased with increasing CD4 count at enrollment. Patients with an entry level of CD4 <50 cells/mm3 were 6 times more likely to die in the pre-ART phase than patients with CD4 >200 cells/mm3 in Kenya (12% versus 2%) and more than twice as likely to die in Tanzania (5% versus 2%). Patients with enrollment CD4 counts above the prevailing eligibility threshold of 200 cells/mm3 were least likely to initiate ART during the observation period. In Kenya, 40% of patients entering care with CD4 >350 cells/ mm3 were still in pre-ART care at the end of the observation period as were 51% of those patients in Tanzania. In Tanzania, but not in Kenya, patients with CD4 counts >350 cells/mm3 had higher hazards for LTFU compared to patients with enrollment CD4 counts ≤50 cells/mm3. Enrollment CD4 count estimates of effect were significantly different across all modes of transition from pre-ART care except when comparing LTFU to transfer.
Associations between sex and mode of transition
In both countries, men were more likely than women to die and to be lost to follow-up. Men and women were equally likely to initiate ART within the observation period. The effect of male sex was more strongly associated with death and LTFU compared to starting ART.
Associations between age and mode of transition
In Kenya, but not in Tanzania, all age groups were less likely to be LTFU compared to patients aged 15 to 25. However, in general, the effects of age-group were highly variable across modes of transition and between countries.
Discussion
This study demonstrated that most patients transition from pre-ART care through the initiation of ART. Additionally, the study demonstrated that being male, CD4 count at enrollment, and the presence of OIs (such as candidiasis, wasting, Kaposi’s sacrcoma, herpes zoster, and other OIs associated with advanced HIV infection excluding TB, PCP, and cryptococcal disease) at enrollment each have a significant impact on transition due to mortality and LTFU. While previous studies7-16 used some form of competing risk analysis to assess the impact of patient-level covariates on pre-ART outcomes, only half7,9,12-14 included survival analysis and of these, only one14 compared ART initiation with death and LTFU. The present study improves on these previous designs by including cause-specific hazard ratios, so meaningful differences in the effect of covariates on one mode of transition over another were not ignored.
Over this period, both country programs showed a steady decline in the rate of early (pre-ART) mortality. At the same time, we observed no programmatically meaningful change in median CD4 counts at enrollment. In other words, despite program maturity, patients were still delaying enrollment into care until late in HIV disease progression. A similar lack of change in entry-level CD4 counts was reported in a meta-analysis of 56 studies from sub-Saharan Africa published between 2002 and 2013.5
Patients with advanced HIV disease based on CD4 counts at enrollment were more likely to start ART and more likely to die before initiating ART compared to patients with more intact immune systems. This trend should be monitored in further observational studies to determine whether the removal of CD4 thresholds impacts rates of ART initiation, mortality, and loss to follow-up going forward. At the other end of the spectrum, patients with enrollment CD4 cell counts above the threshold for ART eligibility during the study period were less likely to have started ART and less likely to die than those with the lowest CD4 cell counts at enrollment. This finding is consistent with Monte Carlo simulations18 that predicted less than 3% excess mortality from delaying ART initiation by 52 weeks for patients enrolling for care with CD4 levels between 300 and 350 cells/mm3. The paradoxical finding that diagnosed tuberculosis was protective against early mortality in Kenya probably reflects AIDSRelief’s focus as well as the focus of the ministries of Health in both countries, on testing for and treating tuberculosis. A study conducted in South Africa10 also reported that tuberculosis treatment was associated with lower attrition in the pre-ART period.
The strength of our analysis lies in the use of 2 large observational cohorts from multiple facilities in 2 countries operating in settings typical of national HIV care and treatment programs in sub-Saharan Africa. Most of the published studies on pre-ART retention were conducted in only one6-10,15 or 2 facilities14 and with far fewer patients. Patients and providers benefited from continuous quality improvement and information use strategies that improved both patient outcomes—seen in the low rates of mortality and lost to follow-up in both countries—and the quality of patient data collected.
We also recognize the inherent limitations of using data collected originally for providing routine HIV care and treatment and not for research purposes, for example, missing data records, data entry errors, and misclassification of events such as transfer out versus LTFU. Given the attention paid to ensuring data quality, including employment of paid data entry clerks and quarterly supervision of patient records, we do not think that these errors jeopardize the robustness of the findings. Additionally, we would expect any misclassification of the mode of transition to be independent of the covariates under investigation. To estimate the potential bias from misclassification, we examined patients who were classified in the records as active when they had not had a visit within 6 months of the close of the study. We found that 0.4% of patients documented as active had been misclassified. Assuming a 99% sensitivity of classification of status, we found that the estimates of effect were stable when 1% of patients were randomly reclassified to another mode of transition.
To the extent that there may be differences in the patterns of transition from pre-ART care by facility type, the findings of this study may not be fully generalizable to other primary health-care settings. We note that facility type and location were not significantly associated with either the covariates or the modes of transition in this data set. We would expect the strong effect of male sex and the degree of immune suppression at enrollment on transition due to death and lost to follow-up to persist. Future research would benefit from the inclusion of other key information, such as duration of HIV infection at enrollment for care, viral load during the pre-ART period, information related to patient disclosure and support networks, and changes in staffing and clinic functioning, which were not available in our records.
Conclusions
Historical data are important referents in guiding development of future norms and drawing attention to persistent, unsolved problems. Together with results reported previously in the literature, this study of patient outcomes in the pre-ART period of care provides the following insights as programs implement the new treatment guidelines: (1) While removing eligibility requirements for ART is good clinical medicine, it is not likely to substantially reduce program mortality prior to ART initiation unless and until PLHIV enroll earlier in disease progression. Most of our mortality came from patients who were already eligible for ART when they first presented for care, and pre-ART mortality did not increase appreciably after the first year following registration. (2) In the short-term, care programs may benefit from a targeted focus on diagnosing and treating OIs and retention of men. As long as PLHIV continue to register for care late in disease progression, Cryptococcal disease and PCP are likely to persist as risk factors for mortality. Our paradoxical finding that diagnosed tuberculosis was protective against early mortality in Kenya may not be generalizable to other programs in higher TB burden settings. Even after controlling for clinical factors, men progressed significantly faster to both mortality and LTFU compared to women. This suggests that programs might offer special counseling and/or support at intake to men.
Supplementary Material
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. WHO. Adult ART Guidelines. 2006. [cited 2015 October 30]. http://www.who.int/hiv/pub/guidelines/artadultguidelines.pdf?ua=1. Accessed March 30, 2017.
- 2. WHO. Adult ART Guidelines. 2009. [cited 2015 October 30]. http://www.who.int/hiv/pub/arv/rapid_advice_art.pdf?ua=1. Accessed March 30, 2017.
- 3. WHO. Adult ART Guidelines. 2012. [cited 2015 October 30]. http://apps.who.int/iris/bitstream/10665/85321/1/9789241505727_eng.pdf?ua=1. Accessed March 30, 2017.
- 4. WHO. HIV treat all recommendations. 2015. [cited 2015 October 30]. http://www.who.int/mediacentre/news/releases/2015/hiv-treat-all-recommendation/en/. Accessed March 30, 2017.
- 5. Siedner MJ, Ng CK, Bassett IV, Katz IT, Bangsberg DR, Tsai AC. Trends in CD4 count at presentation to care and treatment initiation in sub-Saharan Africa, 2002-2013: a meta-analysis. Clin Infect Dis. 2015;60(7):1120–1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nash D, Tymejczyk O, Gadisa T, et al. Factors associated with initiation of antiretroviral therapy in the advanced stages of HIV infection in six Ethiopian HIV clinics, 2012 to 2013. 2016;19(1):20637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Amuron B, Namara G, Birungi J, et al. Mortality and loss-to-follow-up during the pre-treatment period in an antiretroviral therapy programme under normal health service conditions in Uganda. BMC Public Health. 2009;9:290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bassett IV, Wang B, Chetty S, et al. Loss to care and death before antiretroviral therapy in Durban, South Africa. J Acquir Immune Defic Syndr, 2009;51(2): 135–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Castelnuovo B, Musaazi J, Musomba R, RP4 Ratanshi, Kiragga AN. Quantifying retention during pre-antiretroviral treatment in a large urban clinic in Uganda. BMC Infect Dis, 2015;15:252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Clouse K, Pettifor AE, Maskew M, et al. Patient retention from HIV diagnosis through one year on antiretroviral therapy at a primary health care clinic in Johannesburg, South Africa. J Acquir Immune Defic Syndr. 2013;62(2):e39–e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Geng EH, Bwana MB, Muyindike W, et al. Failure to initiate antiretroviral therapy, loss to follow-up and mortality among HIV-infected patients during the pre-ART period in Uganda. J Acquir Immune Defic Syndr. 2013;63(2): e64–e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ingle SM, May M, Uebel K, et al. Outcomes in patients waiting for antiretroviral treatment in the Free State Province, South Africa: prospective linkage study. AIDS. 2010;24(17):2717–2725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mugisha V, Teasdale CA, Wang C, et al. Determinants of mortality and loss to follow-up among adults enrolled in HIV care services in Rwanda. PLoS One. 2014;9(1):e85774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Alvarez-Uria G, Pakam R, Midde M, Naik PK. Predictors of delayed antiretroviral therapy initiation, mortality, and loss to followup in HIV infected patients eligible for HIV treatment: data from an HIV cohort study in India. Biomed Res Int. 2013;2013:849042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Feldacker C, Johnson D, Hosseinipour M, Phiri S, Tweya H. Who starts? Factors associated with starting antiretroviral therapy among eligible patients in two, public HIV clinics in Lilongwe, Malawi. PLoS One. 2012;7(11):e50871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Noel E, Esperance M, McLaughlin M, et al. Attrition from HIV testing to antiretroviral therapy initiation among patients newly diagnosed with HIV in Haiti. J Acquir Immune Defic Syndr. 2013;62(3):e61–e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Catholic Relief Services. AIDSRelief Final Report. 2014. https://www.crs.org/sites/default/files/tools-research/aidsrelief_final_report.pdf. Accessed March 30, 2017.
- 18. Hoffmann CJ, Lewis JJ, Dowdy DW, et al. Mortality associated with delays between clinic entry and ART initiation in resource-limited settings: results of a transition-state model. J Acquir Immune Defic Syndr. 2013;63(1):105–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.