Abstract
In Vietnam where alcohol use is culturally normative and little treatment is available, persons living with HIV (PLWH) who consume alcohol at unhealthy levels are at greatly increased risk for negative health outcomes. We describe the first systematic adaptation of 2 evidence-based alcohol interventions for use in Vietnam: a combined motivational enhancement therapy/cognitive behavioral therapy and a brief alcohol intervention. Using the situated information, motivation and behavioral skills model, and systematic procedures for tailoring evidence-based treatments, we identified core intervention content to be preserved and key characteristics to be tailored for relevance to the clinical setting. We describe the use of in-depth interviews with antiretroviral treatment clients and providers, expert input, and counselor training procedures to develop tailored manuals for counselors and clients. Adapting evidence-based alcohol treatments for global settings is facilitated by the use of a model of behavior change and systematic procedures to operationalize the approach.
Keywords: HIV, alcohol use, Vietnam, cultural adaptation, alcohol intervention
What Do We Already Know About This Topic?
Alcohol interventions are effective for people living with HIV.
How Does Your Research Contribute to the Field?
First alcohol intervention to be tested in Vietnam and information about how to intervention structure and content for Vietnamese setting.
What Are Your Research’s Implications Toward Theory, Practice, or Policy?
We provide a road map for cultural adaptation of evidence-based alcohol interventions for low-resource setting.
Introduction
Hazardous or at-risk alcohol use is a significant health concern for people living with HIV (PLWH) because of its association with transmission risk behaviors, suboptimal initiation of and adherence to antiretroviral treatment (ART), accelerated progression of liver disease, and decreased viral suppression.1-4 Hazardous use or at-risk use is defined as exceeding daily or weekly drinking limits.5 Even in countries such as Vietnam where the HIV epidemic has been driven largely by intravenous drug use,6,7 alcohol remains a critical barrier to HIV prevention and care.8 In a countrywide sample of clinics providing HIV care, a standardized screening tool classified 30.0% of PLWH as at-risk drinkers and these patients were about twice as likely to be ART nonadherent.9 Furthermore, even as PLWH have reduced injection drug use, hazardous drinking has increased.10
Alcohol use by PLWH is normative and culturally acceptable in Vietnam.11 Currently, Vietnam ranks 94th of 191 countries in per capita alcohol consumption.12 Unlike many countries that have stable or declining use, Vietnam’s alcohol use has nearly doubled from the survey period 2003 to 2005 and 2008 to 2010.12 In a recent national survey, 40% of men and 3% of women consumed alcohol at levels that are considered harmful to their health.13 This surge in alcohol use is partly attributable to the opening of Vietnam’s economy in the 1990s that rapidly expanded wealth and urbanization and increased production of commercial alcohol products.11,14
Even before economic expansion, alcohol use had been highly normative in Vietnam.2,12,15 Cultural practices typically involve drinking alcohol, particularly for men.12,15 At business and social gatherings, drinking is expected and integral to social exchange.11,16 Alcohol is widely available, frequently consumed at each meal, and relatively inexpensive owing to the ease and low cost of home-brewed production, especially in rural areas.15 Home brew is largely unregulated or not enforced with very limited controls on the quantity or alcohol by volume obtained.2,12 There is also very limited access to treatment programs for alcohol use disorders (AUDs)2 and a lack of general information about and access to alcohol-related care.16-18 Effective strategies to reduce hazardous alcohol use are thus strongly needed in Vietnam to improve health outcomes, particularly among PLWH.
In highly resourced settings, evidence-based treatments for at-risk alcohol use include multisession motivational enhancement therapy (MET),19-21 cognitive behavioral therapy (CBT),18,22 and brief alcohol intervention (BI).23 Motivational enhancement therapy uses normative-based feedback and decisional balance to prompt intrinsic motivation for behavior change and to build a plan for change, whereas CBT teaches problem-solving and coping skills to reduce alcohol consumption. Brief alcohol intervention typically combines some elements of both these interventions in a 1- to 2-session format.23,24 A recent systematic review concluded that alcohol interventions in HIV clinical settings have been efficacious in reducing hazardous alcohol use, transmission risk behaviors, and suboptimal adherence that contributes to poor health outcomes.25 Although many of these interventions were implemented in low-resource international settings, few specifically addressed if cultural adaptation occurred. As MET, CBT, and BI were developed in high-income countries and are increasingly exported for alcohol treatment, it is critical to understand how they have been adapted for use in other cultural settings.25,26 This is particularly critical as it appears that cultural adaptation may increase the efficacy of AUD interventions,26,27 increase ART access and adherence,28,29 and improve overall health outcomes.30 Furthermore, there is an extensive evidence base on adaptation methods to ensure that the process is highly systematic.30-33 Common to each method is the identification of core elements and key characteristics. Core elements are the theoretical and empirical mechanisms of change that presumably underlie intervention efficacy.30 Key characteristics are language, beliefs, knowledge, values, norms, and context that help ensure that intervention activities and delivery methods are tailored and relevant to the target population.31-33
This article describes the theoretical approach and systematic procedures we used to select, modify, and test evidence-based alcohol interventions for PLWH. We applied the widely used situated information, motivation, and behavioral skills (sIMB) model, developed to understand determinants of HIV risk and preventive behaviors, as our overarching model for intervention content selection and modification. The sIMB model asserts that accurate information about a health behavior, motivating attitudes/beliefs regarding the positive and negative consequences of a health behavior, and self-efficacy combine to enable behavior change.34 The sIMB appreciates that these components are “situated” in the context and culture in which a health behavior occurs.35 We used a 3-phased cultural adaptation process for HIV interventions that included assessment, preparation, and implementation.30-33 The sIMB model informed content and contextual tailoring and the cultural adaptation process structured the methodological approach to answer our research questions: What sIMB components are core elements to be preserved and what sIMB components are key characteristics to be modified to produce a culturally relevant alcohol intervention? These cultural adaptations occurred in preparation for a 3-arm randomized clinical trial comparing the adapted alcohol interventions with usual care among PLWH in Vietnam. To our knowledge, this is one of the first systematic adaptations of 2 evidence-based alcohol reduction interventions in a lower resource setting.
Methods
Setting
The national HIV prevalence in Vietnam is 0.34%; however, the HIV prevalence among people who inject drugs (PWID) is 21%.36 Thai Nguyen is the ninth largest province in Vietnam with a 2010 population census of 330 000 and an economy based in green tea and steel export. Similar to country estimates, the HIV epidemic in Thai Nguyen is predominately concentrated PWID, as one study found an HIV prevalence of 33% among PWID.36,37 In 2016, Thai Nguyen had an estimated 2026 drug users and 6 methadone maintenance treatment clinics serving more than 800 patients.38 All ART clinics are government run and our target study population was patients from 7 of these clinics with the highest patient volume. Of the patients attending these clinics, 70% are currently on ART, while the remaining 30% were not yet eligible for ART. The majority of patients were PWID and male.
Participants
In the assessment phase, we conducted the first round of in-depth interviews (IDIs) to obtain individual- and cultural-level information about alcohol use. Three ART providers were approached and 3 agreed to be interviewed by research staff to discuss their observations about alcohol use among ART patients. We also asked the providers to refer patients whom they knew consumed alcohol. If a provider identified alcohol use by a patient, the provider would briefly describe the study. The provider was not required to determine whether or not use was hazardous. Interested patients were then referred to the study recruiter for more study information, consent, and determination of eligibility. Patients were eligible if they were able to provide consent and screened as positive for “hazardous drinking” by a score of ≥8 on the Alcohol Use Disorders Identification Test.39,40 Finally, research staff chose a convenience sample of owners and workers at karaoke bars and restaurants to be interviewed. These venues were chosen because they were socioeconomically representative of venues ART clinic patients frequented. In the preparation phase, we conducted a second round of IDI and focus groups (FGs) for intervention testing with a new group of ART patients who were positive for hazardous drinking and enrolled in ART care. All participants were ≥18 years of age and provided oral informed consent at study entry. Each participant was assigned a unique study number which was placed on the verbal consent form. The staff conducting oral consent marked “yes” on the verbal consent form if the participant agreed to participate in the study or marked “no” if the participant did not agree to participate in the study. This study was approved by the Office of Human Research Ethics Institutional Review Board (IRB) at the University of North Carolina at Chapel Hill (approval number 14-0225) and the IRB for Biomedical Research of the Thai Nguyen Centers for Disease Control in Thai Nguyen Vietnam.
Procedures
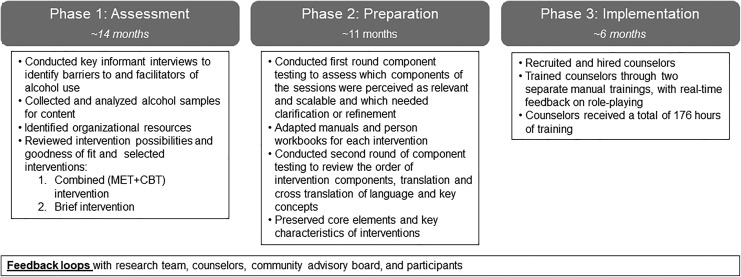
The sIMB model was used as an overarching framework to select interventions and then intervention elements. The process for systematically adapting evidence-based alcohol interventions involved a 3-phase approach following the recommendations for cultural adaptation with PLWH.31-33 Figure 1 summarizes this process. Phase 1 reviewed and selected alcohol interventions and conducted IDIs to gather information for adaptation; phase 2 integrated these data on key characteristics with intervention core elements, and phase 3 provided in vivo testing with PLWH and counselors to make final modifications.
Figure 1.
Procedures for systematic adaptation of 2 evidence-based alcohol interventions for PLWH. PLWH indicates persons living with HIV.
In the first phase, assessment, we (1) evaluated the goodness of fit of 3 alcohol interventions using the sIMB framework and examined each intervention to parse the interventions into core elements as to whether they were I, M, or B. This selection of elements was based on theoretical and empirically established mechanisms of behavior change for these alcohol interventions.41-43
(2) We then identified key characteristics that would need exploration through IDI with target populations and stakeholders.31-33 The topics were selected because they “situated” the information, motivation, and behavioral skills (IMB). For example, alcohol refusal skills are a “core” skill, but how refusal is enacted depends on how locally credible the verbal and nonverbal body language is. In-depth interviews were used to provide information on that topic to help teach and role model effective refusal skills. The topics explored included drinking motives; social norms and acceptability of drinking; drinking practices and drinking refusal; knowledge of alcohol-related harms, especially related to HIV disease; and reasons and methods for reducing or quitting alcohol use. These topics were organized into semistructured interview guides asking ART clients, ART providers, and bar/restaurant staff/owners to provide their observations. We included ART providers as they provided information on barriers and facilitators that alcohol poses to HIV care. We included bar and restaurant owners because they provided information on type of drinks consumed, social norms and practices regarding alcohol serving, and consumption practices and observations on refusal skills that could be observed outside the home. Both IDIs and FGs were audio-recorded and transcribed verbatim. Transcripts were analyzed in an iterative manner. Two investigators independently reviewed transcripts and developed a joint coding scheme. The research team examined these provisional codebooks and created a representative codebook. Data were organized in NVivo11. The number of interviews was determined by thematic saturation. A full description of the coding methods and results of IDI with ART clients is described elsewhere.
We also determined that in order to provide accurate personalized feedback on levels of hazardous drinking to clients (a core element of alcohol interventions), we would need to conduct a chemical analysis of commonly consumed alcoholic beverages (a key characteristic). The availability of home-brewed alcohol rendered it impossible to ascertain the amount of alcohol consumed by study participants. Thus, we collected random samples of rice wines and beer from 10 homes and Thai Nguyen karaoke bars/street cafes and transported them in <3 oz bottles for analysis at Johns Hopkins University School of Medicine. We analyzed these rice wines and beers to determine amount of alcohol by volume (ABV) that would define a “standard drink.” With this analysis, we could more accurately ascertain whether alcohol use was below or exceeded safer drinking limits as defined by National Institute on Alcohol Abuse and Alcoholism (NIAAA).5 Finally, we assessed organizational resources to understand what treatments were currently available. The second phase, preparation, was a parallel process of using a second round of IDIs and also FG to (1) test intervention session content and (2) conduct preliminary observations of counselors-in-training. We used manuals developed for Project MATCH CBT, and MET and Project TrEAT BI.18,19,23,24
Using IDI and FG, each session of the interventions was reviewed with ART clients, who had not participated in the formative phase. For example, refusal skills are a core element of CBT. We tested this element using semistructured questions to identify current refusal responses, specific sociocultural contexts where refusals are needed, expected consequences of refusals, alternatives to drinking, and person-situation-specific skills needed to implement them. Staff recorded extensive notes on ART clients’ perceptions of the utility, clarity, and acceptability of each session. A summary of these recorded responses was reviewed by the US and Vietnam teams and incorporated into the cultural adaptation of the interventions.
Focus groups testing also served as an opportunity to observe administration of interventions and begin selection and training of 2 male/female pairs of potential counselors. Their training consisted of an initial overview of theories of and techniques for behavior change in CBT and MET, review of goals and methods of each session in the counselor manual, and role-playing counseling skills. Counselors were also provided detailed directions and “scripts.” A US and Vietnam project staff member was paired with each counselor to supervise and record observations of the counselor with ART patients. Using these testing results, we adapted the interventions’ counselor manuals and personal workbooks for participants.
In a second round of intervention testing 6 months later, the adapted counselor manuals were reviewed by US and Vietnam teams and counselors-in-training for clarity, acceptability, translation and back-translation of language and key concepts, and relevance of adapted content.
In the third phase, implementation, we finalized intervention adaptation and counselor hiring and training. Over 5 days, the US team conducted in-depth intervention training. Each session was role-played by the counselors and their local supervisors who also took turns acting as client and counselor. We provided clinical feedback and made final revisions to each counselor manual. Counselors continued to review manual and role-play prior to study initiation using the script as a guide. Both sets of counselors were trained on defining a standard drink using visual aids and sample containers. Counselors were also provided information on hazardous alcohol use, HIV disease, and ethics of care.
Feedback loops and monitoring and evaluation procedures were conducted throughout all 3 phases of the adaptation. Counselor manual adaptation was an ongoing process that was conducted with research team, counselors, participants, and community advisory board (CAB). The CAB was made up of ART clients, their families, and community and health leaders within Thai Nguyen. The CAB held meetings every 6 months to answer any questions and to obtain advice on key issues related to the study.
Results
The cultural adaptation of the interventions was conducted in 3 phases over 36 months garnering information and integrating feedback obtained from ART patients, ART providers, community members, project counselors, and US and Vietnam research teams into culturally adapted counselor manuals and personal workbooks for participants.
Phase 1: Assessment
1) Using the sIMB framework, we reviewed evidence-based alcohol interventions to determine goodness of fit and identify core elements. We considered CBT, BI, and MET as potential interventions. The capacity of these interventions to address sIMB to reduce alcohol use as well as feasibility of these interventions was jointly discussed by the US and Vietnam teams. As the concept of alcohol reduction/abstinence and the methods to achieve these were highly novel in this setting, we reasoned that a broad approach which addressed information, motivation, and skill-building components34,35 would be critical to intervention efficacy. Thus, we chose a combination MET/CBT because it addressed the wider range of sIMB and has been used successfully in other alcohol reduction trials.20 We conducted the first session using MET, particularly decisional balance, to engage motivation and as a predominant interviewing style, with subsequent sessions using CBT incorporating behavioral skill building and role-playing. For the comparison arm, we chose a BI which, if efficacious, could be implemented in a resource-limited setting. The BI had components similar to the combined CBT/MET but was 2 rather than 6 sessions and sessions were briefer. We had previously tested a BI based on Project TrEAT that was efficacious in reducing alcohol use among HIV-infected women at an HIV clinic in the United States.24
The core elements of the interventions that we identified are presented in Table 1. This table shows whether core elements were information, motivation, or a behavioral skill. We also show the key characteristic that was modified to situate the core element and the data source for this information.
Table 1.
Summary Examples of Program Adaptations to MET/CBT and BI.
| IMB Component | Core Elements of Original Interventions | Key Characteristics That Situate Core Elements | Data Source | Adaptation Examples |
|---|---|---|---|---|
| M | MET: Nonjudgmental, empathic approach | Cultural mores to respect authority may increase perceived pressure for socially desirable responding | IDI-PLWH;EI | Use MET style for both interventions to increase comfort in discussing alcohol use and its consequences |
| M | MET, BI: Decisional balance: Reasons for drinking | Pressure in work and social situations to drink; medicinal use of alcohol; alcohol to improve celebration and reduce anxiety and depression | IDI-PLWH; IDI-B | Manual content added to specifically explore the range of reasons for drinking with clients such as weddings and funerals, and health/vigor. Concept of “decisional balance” was familiar |
| M | MET, BI: Decisional balance: Reasons to cut down or quit drinking | Identified relevant reasons to quit—importance of family, respect in community; health of the body, especially the liver, financial reasons are not motivating as alcohol is home brewed; decisional balance | IDI-PLWH; IDI-B; EI | Manual content added to specifically include range of reasons to quit for physical and mental health and overall social/occupational functioning, such as liver health, reducing motorbike accidents, ability to work, preserving the reputation of the family. Information about alcohol harms provided to counter misinformation in MI style |
| I | MET, BI: Personalized feedback: Alcohol use | Concept of drinking limits and ABV was novel in this setting; limited knowledge of effects of alcohol on health | EI | Information given on at-risk drinking based on ABV analysis of local wines/beers |
| I | MET, BI: Personalized feedback: Effect of alcohol on HIV | Risk factor: Limited information on harmful effects of alcohol and on HIV | IDI-PLWH; EI | Clients wanted but had limited knowledge of adverse effects of alcohol on HIV progression, transmission risk behaviors, drug use, and adherence. Information and correction of inaccurate information provided throughout sessions |
| M | MET, CBT, BI: Goal setting | Optional and flexible goal setting, various choices for reducing alcohol, for example, by setting and pattern | IDI-PLWH; EI | Optional and flexible goal setting, various choices for reducing alcohol, for example, by site and pattern: Reducing use at home first by a set amount, then reducing at social gatherings |
| B | CBT, BI: Managing risky situations/triggers | Social and business settings are high pressure to drink; rude to refuse alcohol no matter what the time of day it is offered | IDI-PLWH; EI | Developed the Vietnamese acronym, “Chờ đợi, Tự vấn và Làm việc khác” which translates as Wait, Self-talk, and Do Something Else. Delay: “I am very thirsty because of the heat, I will have water first.” Debate: Consider the consequences to reputation, family. Do something else: It is expected that home brew alcohol drink is brought to a social gathering. Clients can bring their own low alcohol content brew to drink. Clients can go to karaoke, play badminton, garden, visit a café or tea shop, talk to supportive friend, drink nonalcoholic beverages |
| B | CBT: Role-playing | Concept of role-playing was novel | EI | Counselors were trained in role-plays, what to observe about body language, and how to provide constructive feedback. Counselors then taught the concept, rationale, and modeled both client and counselor to the clients. |
| B | CBT: Refusal skills | Saying “no” is not acceptable; providing certain reasons can seem like lying, which is also unacceptable; liver concerns were highly acceptable reason to refuse | IDI-PLWH; EI | Role-plays used to develop refusal scripts that were credible and acceptable in clients setting and to develop convincing body language; health reasons, navigating on motorbike, work for men and women and children for women were common reasons for refusing |
| B | CBT: Managing negative thoughts, power of positive thinking | Thoughts as a source of feelings and actions was a novel concept; notion of positive thinking was familiar | IDI-PLWH; EI | Used daily-life examples of how negative thoughts drive feelings. For example, different beliefs about why a neighbor does not greet us and how those different beliefs subsequently affect feelings and behaviors. Manual focused on thoughts behind depressive feelings that motivate drinking and reset for developing habits of positive thinking |
Abbreviations: ABV, alcohol by volume; B, behavioral skills; BI, brief alcohol intervention; CBT, cognitive behavioral therapy; EI, expert input on the intervention; I, information; IDI-ALC, in-depth interview with ART clients on alcohol use practices; IDI-B, in-depth interview with bar owners; IDI-CL, in-depth interview with ART clinic clients on the intervention; IDI-PLWH, in-depth interview with persons living with HIV; M, motivation; MET, motivational enhancement therapy; PLWH, persons living with HIV.
2) Information to design the key characteristics of the interventions. For IDI, 12 bar owners/workers were approached and 3 refused participation. We interviewed 12 female and 18 male ART clients who were at-risk drinkers. The participants ranged in age from 30 to 48 years (median age = 38 years), 15 (50%) were married, and 10 (33%) were current injection drug users. We also interviewed 3 ART providers. In-depth interviews provided information on the overall information and misinformation that ART patients had about alcohol. For example, many varieties of alcohol were also consumed as anodynes for various ailments, including stress and depression. There also was limited information on the harms of alcohol in HIV. Thus, the IDI showed that alcohol use was highly prevalent and was typically part of a daily routine in business, social settings, and at home. HIV stigma was a strong motivator to drink. Antiretroviral treatment providers noted the lack of information about the harms of alcohol and challenges with assessing alcohol use patterns without objective measures of alcohol use. The primary challenges to reducing alcohol use were availability of inexpensive alcohol; perceived inability to refuse alcohol in the context of social norms; lack of knowledge about adverse effects of alcohol on HIV disease; lack of other skills for coping with negative emotions, especially related to HIV status; compensatory behaviors when reducing injection drug use; and lack of alcohol treatment programs. Overall, reducing/abstaining from alcohol was considered difficult, given how integral alcohol was to social and business gatherings. Participants cited the importance of social support from family in overcoming hazardous alcohol use, particularly because alcohol was consumed at family mealtimes. Notably, ART patients and providers identified few strategies for reducing alcohol use but expressed a desire to learn skills to manage negative feelings and refuse drinks.
Our IDI also revealed that a commonly consumed alcohol was homemade rice wine consumed as both a spirit and a medicine for a variety of ailments.11 Our chemical analysis of rice wine samples indicated that alcohol content ranged from 20% to 45% with a median ABV of 32%, which we used to calculate a standard drink. Commercial and street beers (bia) were also popular and contain approximately 3% ABV. Therefore, we were able to calculate that 2.3 shots of 32% rice wine, 1 can of beer, 0.8 bottle of beer, and 1.8 glasses of beer were each 1 standard drink.
3) Organizational resources were very limited in Vietnam. We were unable to establish the existence of alcohol treatment programs or formal support networks (eg, Alcoholics Anonymous) for AUD. Alcohol and mental health interventionists were not available, and therefore, counselors had to be fully trained and supervised. Clients with alcohol withdrawal symptoms were referred for medical evaluation and intervention before entering the trial.
Phase 2: Preparation
Intervention adaptation: Integrating key characteristic data with intervention core components
Table 1 shows the core elements of the MET/CBT and BI interventions that were preserved, to which IMB component they corresponded, the key characteristics we incorporated from that to situate the core element, the data source for the adaptation, and examples of adaptations. Intervention testing was conducted over 5 days with input from 7 ART patients paired with counselors in training and supervision by US/Vietnam intervention teams. Based on intervention testing, as well as expert input from the research team, we selected 6 of 12 possible sessions of individual MET/CBT with 3 content parallel group sessions. Session 1 was patterned on the MET manual: (1) engagement/ motivation/personalized feedback. Sessions 2 to 6 were patterned on specific chapters from the CBT manual: (2) drinking refusal skills; (3) coping with cravings or “wait, self-talk, and do something else” (Chờ đợi, tự vấn và làm việc khác); (4) understanding negative thinking and developing positive thinking; (5) developing social support; and (6) seemingly irrelevant decisions and planning for emergencies. Session 6 taught clients about the chain of “seemingly small” decisions that potentiate subsequent decisions in a chain that eventually results in hazardous drinking. For example, it may seem irrelevant to take a different route to home, until clients recognize that this detour takes them directly past a bar. As a corollary, therefore, planning for emergencies helps clients think ahead to what additional support or behavioral tools might be needed to address links in the chain and in high-risk situations for hazardous alcohol use. The BI contained the same content as the MET/CBT intervention and thus was similarly adapted. Session 1 provided information and reviewed decisional balance, personalized feedback, and goal setting, managing risky situations; session 2 reviewed goals, managing risky situations and triggers.
Phase 3: Intervention Implementation
Training and supervision
The counselors were university educated, but as counseling programs were not available in Vietnam, intensive training and supervision were required. We hired 2 female/male pairs based on qualities consonant with motivational interviewing (MI) spirit (empathy and nonjudgment), communication skills, ability to grasp behavior change concepts, conscientiousness, and professional demeanor. Counselors received a maximum of 176 hours of intervention training before study launch. While in training, counselors were also involved in the intervention adaptation to ensure the interventions were sufficiently adapted for their use. We also developed protocols for managing difficult issues such as session sleepiness, irritability, or ART nonadherence. We added peer supervision so that CBT and BI pairs worked together.
Discussion
In Vietnam, alcohol use is highly normative and increasing with economic and urban expansion; alcohol also remains prevalent in rural areas.2,11,12 However, there are limited formal alcohol treatment programs. This resource limitation has a particular impact on PLWH owing to the deleterious effects of alcohol use across the HIV continuum.4,9,10 Herein, we described lessons learned in the first systematic adaptation of 2 evidence-based alcohol interventions. First, an overarching conceptual model was essential to organizing the adaptation process. We used the sIMB model to guide intervention selection and parse theoretical and empirical core components into information, motivation, and behavioral skills necessary to reduce hazardous alcohol use.34,35 Having identified the core components, we then used a structured, 3-phase approach to add key characteristics that situated the core elements into an appropriate, relevant cultural context.31-33
Second, gathering information on key characteristics as prescribed by evidence-based cultural adaptation methods was a lengthy but indispensable assessment process. The IDI and FG elucidated alcohol’s role in the daily Vietnam life; the values, beliefs, and cultural norms about alcohol; drinking motivations; the lack of information about and treatment resources for alcohol harms, especially for PLWH; and reasons and methods for reducing or quitting alcohol use.
Importantly, we found that PLWH had relatively little knowledge about hazardous alcohol use and its deleterious effects on HIV but were eager for information. Thus, an educational component about alcohol and HIV was incorporated into the interventions, as well as information about alcohol effects on health. This information helped increase the motivational component of the interventions: Negative effects of alcohol could be used to tip the balance of reasons toward the consideration of the negative consequences of drinking. This, in turn, is expected to motivate increased use of alcohol reduction strategies, particularly refusal skills. The culturally normative practice of, for example, drinking at lunch with the boss required relevant knowledge of factors in the decisional balance (alcohol harms), culturally acceptable ways to refuse, extensive role-playing to appear convincing and natural, and resourceful alternatives to drinking alcohol. Additionally, there was no systematic way for PLWH to understand how much alcohol they consumed over time because of the wide use of home-brewed rice wines with variable ABV. This reinforced the importance of our analysis of the ABV of rice wines and other commonly consumed drinks in Vietnam to define a “standard drink.” Once a standard drink measurement was established, we were able to provide personalized feedback on what constituted hazardous use,13 and clients were able to discern their own level of consumption. Personalized feedback is a core component of MET/CBT and BI; however, the calculation of a standard drink, a key characteristic, had to be adapted for local relevance. In the final phase, extensive training was required to implement the interventions. Our interventionists were not schooled in principles of behavior change, HIV disease, or alcohol use reduction; therefore, we found it useful to “script” interventions. This scripting, although time-consuming to generate, provided a foundation for the conduct of sessions and provided some reliability across counselors in the conduct and flow of sessions. Without sacrificing content, counselors eventually modified scripts to be delivered in their own style. It was also essential to review forward and backward translations to ensure proper meaning and tone of clinical interactions. Although the BI was less labor intensive in scripting, training, and supervision than that of the MET/CBI, it contains fewer components that build skill acquisition.
The adaptation process for this study has methodological limitations. We were unable to identify local alcohol reduction experts to assist in adapting the alcohol interventions. To compensate, we relied on input from US-based alcohol reduction experts and input from local community experts, clinicians, and clinic patients. The 2.5-year adaptation process was therefore time and resource intensive. Additionally, we did not pilot short-term efficacy of the selected alcohol reduction interventions. Rather, we sought to identify and adapt the most appropriate evidence-based interventions within the Vietnamese context. The efficacy of the interventions will be further established in an ongoing comparative effectiveness trial. Finally, the alcohol reduction interventions were not tailored by gender. Although gender differences in drinking patterns may exist within this setting, our formative IDI emphasized similar challenges in alcohol reduction for both females and males.
Conclusion
Adapting evidence-based alcohol treatments for global settings is facilitated by the use a model of behavior change and a systematic process to tailor the approach. The sIMB model can be used to delineate core intervention content that was to be preserved and identify key characteristics that were to be tailored for relevance to the clinical setting. The adaptation process required a systematic and 3-phase procedure to collect, analyze, and tailor content. The randomized controlled trial is currently underway in Vietnam comparing the relative efficacy of each intervention to usual care in reducing alcohol use and improving viral suppression. The trial will also evaluate the incremental cost-effectiveness of both interventions to provide insights into the optimal application of alcohol reduction programs. Our culturally enhanced alcohol reduction interventions, if effective, hold strong promise for reducing hazardous alcohol use and improving HIV-related outcomes among ART clinic patients in Vietnam.
Footnotes
Authors’ Note: Heidi E. Hutton and Kathryn E. Lancaster are co-first authors of this manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported in this publication was supported by the National Institute On Drug Abuse of the National Institutes of Health under Award Number R01DA037440 and by the University of North Carolina at Chapel Hill Center for AIDS Research (CFAR), an NIH funded program P30 AI050410.
ORCID iD: Heidi E. Hutton  https://orcid.org/0000-0002-0882-4456
https://orcid.org/0000-0002-0882-4456
References
- 1. Azar MM, Springer SA, Meyer JP, Altice FL. A systematic review of the impact of alcohol use disorders on HIV treatment outcomes, adherence to antiretroviral therapy and health care utilization. Drug Alcohol Depend. 2010;112(3):178–193. doi:10.1016/j.drugalcdep.2010.06.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Giang KB, Allebeck P, Spak F, Van Minh H, Dzung TV. Alcohol use and alcohol consumption-related problems in rural Vietnam: an epidemiological survey using AUDIT. Subst Use Misuse. 2008;43(3-4):481–495. doi:10.1080/10826080701208111. [DOI] [PubMed] [Google Scholar]
- 3. Hendershot CS, Stoner SA, Pantalone DW, Simoni JM. Alcohol use and antiretroviral adherence: review and meta-analysis. J Acquir Immune Defic Syndr. 2009;52(2):180–202. doi:10.1097/QAI.0b013e3181b18b6e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tran BX, Nguyen N, Ohinmaa A, et al. Prevalence and correlates of alcohol use disorders during antiretroviral treatment in injection-driven HIV epidemics in Vietnam. Drug Alcohol Depend. 2013;127(1-3):39–44. doi:10.1016/j.drugalcdep.2012.06.009. [DOI] [PubMed] [Google Scholar]
- 5. NIAAA.gov. What’s “at-risk” or “heavy” drinking? https://www.rethinkingdrinking.niaaa.nih.gov/How-much-is-too-much/Is-your-drinking-pattern-risky/Whats-At-Risk-Or-Heavy-Drinking.aspx. Accessed May 29, 2019.
- 6. Ngoc LB, Hoang VH, Mulvey K, Rawson RA. Substance use disorders and HIV in Vietnam since Doi Moi (Renovation): an overview. J Food Drug Analysis. 2013;21:S42–45. doi: 10.1016/j.jfda.2013.09.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Go VF, Frangakis C, Nam LV, et al. Characteristics of high-risk HIV-positive IDUs in Vietnam: implications for future interventions. Subst use & misuse. 2011;46:381–389. doi: 10.3109/10826084.2010.505147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ministry of Health of Vietnam. Report of HIV/AIDS Prevention and Control in Vietnam. Hanoi, Vietnam; 2009. https://www.ilo.org/wcmsp5/groups/public/---ed_protect/---protrav/---ilo_aids/documents/legaldocument/wcms_174609.pdf. Accessed May 29, 2019. [Google Scholar]
- 9. Tran BX, Nguyen LT, Do CD, Nguyen QL, Maher RM. Associations between alcohol use disorders and adherence to antiretroviral treatment and quality of life amongst people living with HIV/AIDS. BMC Public Health. 2014;14:27 doi:10.1186/1471-2458-14-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Go VF, Minh NL, Frangakis C, et al. Decreased injecting is associated with increased alcohol consumption among injecting drug users in northern Vietnam. Int J Drug Policy. 2013;24(4):304–311. doi:10.1016/j.drugpo.2012.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lincoln M. Alcohol and drinking cultures in Vietnam: a review. Drug Alcohol Depend. 2016;159:1–8. doi:10.1016/j.drugalcdep.2015.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. World Health Organization. Global Status Report on Alcohol and Health 2014. Geneva, Switzerland: World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/112736/9789240692763_eng.pdf;jsessionid=20D3DF88CBE455DE43A562A8F9E3DDEA?sequence=1. Accessed May 29,2019. [Google Scholar]
- 13. Van Bui T, Blizzard CL, Luong KN, et al. Alcohol consumption in Vietnam, and the use of ‘standard drinks’ to measure alcohol intake. Alcohol Alcohol. 2016;51(2):186–195. doi:10.1093/alcalc/agv082. [DOI] [PubMed] [Google Scholar]
- 14. Ngoc LB, Thieng NT, Huong NL. The drink driving situation in Vietnam. Traffic Inj Prev. 2012;13(2):109–114. doi:10.1080/15389588.2011.636408. [DOI] [PubMed] [Google Scholar]
- 15. Luu BN, Nguyen TT, Newman IM. Traditional alcohol production and use in three provinces in Vietnam: an ethnographic exploration of health benefits and risks. BMC Public Health. 2014;14:731 doi:10.1186/1471-2458-14-731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hershow RB, Zuskov DS, Vu Tuyet Mai N, et al. “[Drinking is] Like a Rule That You Can’t Break”: perceived barriers and facilitators to reduce alcohol use and improve antiretroviral treatment adherence among people living with HIV and alcohol use disorder in Vietnam. Subst Use Misuse. 2018;53(7):1084–1092. doi:10.1080/10826084.2017.139298616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ministry of Health & General Statistic Office. National Health Survey, 2001-02. Hanoi, Vietnam: Ministry of Health & General Statistic Office; 2003. [Google Scholar]
- 18. National Commission of Social Affairs of Vietnam. Record of Workshop on Policies for Alcohol Abuse Control. Hanoi, Vietnam: Quoc hoi Viet Nam; 2003. [Google Scholar]
- 19. Miller WR, Rollnick S. Motivational Interviewing: Helping People Change. New York, NY: Guilford Press; 2012. [Google Scholar]
- 20. Parsons JT, Rosof E, Punzalan JC, Di Maria L. Integration of motivational interviewing and cognitive behavioral therapy to improve HIV medication adherence and reduce substance use among HIV-positive men and women: results of a pilot project. AIDS Patient Care STDS. 2005;19(1):31–39. doi:10.1089/apc.2005.19.31. [DOI] [PubMed] [Google Scholar]
- 21. Smedslund G, Berg RC, Hammerstrom KT, et al. Motivational interviewing for substance abuse. Cochrane Database Syst Rev. 2011;(5):CD008063 doi:10.1002/14651858.CD008063.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Magill M, Ray LA. Cognitive-behavioral treatment with adult alcohol and illicit drug users: a meta-analysis of randomized controlled trials. J Stud Alcohol Drugs. 2009;70(4):516–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fleming MF. Screening and brief intervention in primary care settings. Alcohol Res Health. 2004;28(2):57–62. [PMC free article] [PubMed] [Google Scholar]
- 24. Chander G, Hutton HE, Lau B, Xu X, McCaul ME. Brief intervention decreases drinking frequency in HIV-infected, heavy drinking women: results of a randomized controlled trial. J Acquir Immune Defic Syndr. 2015;70(2):137–145. doi:10.1097/qai.0000000000000679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scott-Sheldon LAJ, Carey KB, Johnson BT, Carey MP. Behavioral interventions targeting alcohol use among people living with HIV/AIDS: a systematic review and meta-analysis. AIDS Behav. 2017;21(suppl 2):126–143. doi:10.1007/s10461-017-1886-327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Benegal V, Chand PK, Obot IS. Packages of care for alcohol use disorders in low- and middle-income countries. PLoS Med. 2009;6(10):e1000170 doi:10.1371/journal.pmed.1000170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Lee C S, Lopez SR, Colby SM, et al. Culturally adapted motivational interviewing for Latino heavy drinkers: results from a randomized clinical trial. J Ethn Subst Abuse. 2013;12(4):356–373. doi:10.1080/15332640.2013.836730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Manuel JK, Satre DD, Tsoh J, et al. Adapting screening, brief intervention, and referral to treatment for alcohol and drugs to culturally diverse clinical populations. J Addict Med. 2015;9(5):343–351. doi:10.1097/adm.0000000000000150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Bere T, Nyamayaro P, Magidson JF. Cultural adaptation of a cognitive-behavioural intervention to improve adherence to antiretroviral therapy among people living with HIV/AIDS in Zimbabwe: Nzira Itsva. Journal of health psychology. 2017. September;22(10):1265–1276. doi: 10.1177/1359105315626783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kekwaletswe CT, Morojele NK. Alcohol use, antiretroviral therapy adherence, and preferences regarding an alcohol-focused adherence intervention in patients with human immunodeficiency virus. Patient Prefer Adherence. 2014;8:401–413. doi:10.2147/ppa.s55547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. McKleroy VS, Galbraith JS, Cummings B, et al. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Educ Prev. 2006;18(4 suppl A):59–73. doi:10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- 32. Barrera M, Jr, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: a progress report. J Consult Clin Psychol. 2013;81(2):196–205. doi:10.1037/a0027085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wingood GM, DiClemente RJ. The ADAPT-ITT model: a novel method of adapting evidence-based HIV interventions. J Acquir Immune Defic Syndr. 2008;47(suppl 1):S40–S46. doi: 10.1097/QAI.0b013e3181605df1. [DOI] [PubMed] [Google Scholar]
- 34. Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychol Bull. 1992;111(3):455–474. [DOI] [PubMed] [Google Scholar]
- 35. Amico KR. A situated-Information Motivation Behavioral Skills Model of Care Initiation and Maintenance (sIMB-CIM): an IMB model based approach to understanding and intervening in engagement in care for chronic medical conditions. J Health Psychology. 2011;16(7):1071–1081. [DOI] [PubMed] [Google Scholar]
- 36. Vietnam Country Operational Plan. Strategic Direction Summary. 2018. https://www.pepfar.gov/documents/organization/285849.pdf. Accessed March 22, 2018.
- 37. Go VF, Frangakis C, Le Minh N, et al. Effects of an HIV peer prevention intervention on sexual and injecting risk behaviors among injecting drug users and their risk partners in Thai Nguyen, Vietnam: a randomized controlled trial. Soc Sci Med. 2013;96:154–164. doi:10.1016/j.socscimed.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. MMT Vietnam. Update on the implementation of treatment of opiate addiction with methadone (MMT) in Vietnam. 2016. http://vaac.gov.vn/mmtvietnam/vi/cap-nhat-tinh-hinh-thuc-hien-chi-tieu-dieu-tri-nghien-cac-chat-dang-thuoc-phien-bang-methadone-mmt-thang-01-nam-2016/. Accessed 2017.
- 39. Babor T, Higgins-Biddle JC, Saunders JB, Monteiro MG. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 40. Giang KB, Spak F, Dzung TV, Allebeck P. The use of AUDIT to assess level of alcohol problems in rural Vietnam. Alcohol Alcohol. 2005;40(6):578–583. doi:10.1093/alcalc/agh198 http://www.ncbi.nlm.nih.gov/pubmed/16115822. [DOI] [PubMed] [Google Scholar]
- 41. Michie S, Whittington C, Hamoudi Z, Zarnani F, Tober G, West R. Identification of behaviour change techniques to reduce excessive alcohol consumption. Addiction. 2012;107(8):1431–1440. [DOI] [PubMed] [Google Scholar]
- 42. Monti PM, Kadden RM, Rohsenow DJ, Cooney NL, Abrams D, ed. Treating Alcohol Dependence: A Coping Skills Training Guide. 2nd ed New York, NY: Guilford Press; 2002. [Google Scholar]
- 43. Zuskov DS, Hershow RB, Mai NVT, et al. Stress and stigma: alcohol consumption among female antiretroviral treatment (ART) clients with alcohol use disorders (AUDs) in Vietnam. Under Review.