Abstract
A Community Health System Strengthening model, which mobilizes communities by applying quality improvement, was used in 39 communities around 3 health centers in Gaza Province, Mozambique, to increase identification of pregnant women and support them to attend antenatal care (ANC). This article describes the process and results. Community group representatives formed a community improvement team to spread messages about the importance of ANC, identify pregnant women, link them to the facility, and follow up. Between March 2014 and February 2015, teams identified 2020 pregnant women. Antenatal care attendance increased at all 3 centers. One health center did an additional chart review and found that postintervention, women were enrolling in care earlier in pregnancy. There were no changes in HIV testing or treatment initiation for HIV-positive women. Community-led improvement initiatives play an important role in connecting pregnant women with services to receive testing and treatment to promote optimal health and prevent HIV transmission.
Keywords: community, prevention of mother-to-child transmission of HIV (PMTCT), quality improvement, antenatal care, linkages to care
Background
HIV prevalence among women of reproductive age (15-49 years) in Mozambique was 13.1% based on a 2009 study, and mother-to-child transmission (MTCT) accounted for 5% of all HIV transmission.1 United Nations Programme on HIV and AIDS reports that between 2009 and 2015 in Mozambique, coverage of antiretroviral therapy for HIV-positive pregnant women increased from 34% to 95% and the rate of MTCT decreased from 11% to 3%.2 Although this reflects a strong commitment of the Government of Mozambique and progress toward reaching the goal of elimination of MTCT (EMTCT), many barriers still existed. Antenatal care (ANC) attendance rates were low, with only half of the pregnant women attending all the recommended 4 ANC visits.3 In Mozambique, pregnant women—especially those in economically insecure communities—may keep their pregnancy a secret to avoid being the target of witchcraft spurred by envy; by extension, they delay seeking ANC services.4-6 Late entry into and low attendance of ANC, in addition to unknown HIV status at delivery, made it difficult for providers to follow clinical protocols for eliminating the transmission of HIV from mother to child. Strong community-level engagement that encourages individual health-seeking behaviors for ANC and HIV services is critical to the larger goals of keeping women and their infants in optimal health and keeping the infants HIV negative.7,8
What Do We Already Know about This Topic?
Community engagement has been shown to improve antenatal care attendance for pregnant women.
How Does Your Research Contribute to the Field?
This case study demonstrates how a quality improvement approach combined with community engagement can contribute to early ANC attendance among pregnant women so that they can get the care they need, including HIV services if they are found to be positive.
What Are Your Research’s Implications toward Theory, Practice, or Policy?
This case study demonstrates that in practice, the Community Health Systems Strengthening model can be included in EMTCT programming to expand demand and access to ANC.
Community-level support for EMTCT services in Mozambique is provided by community health volunteers known as activistas, who identify pregnant women and disseminate health messaging about ANC and HIV. However, there were not enough activistas to reach all women and households on a regular basis. Heavy workloads and lack of transportation prevented the maternal and child health (MCH) nurses at facilities from conducting community outreach visits. The Partnership for HIV-Free Survival (PHFS) was a 6-country initiative in sub-Saharan Africa, funded by the President’s Emergency Plan for AIDS Relief. In Mozambique, the PHFS conducted several activities at different levels of the health system to improve access to HIV prevention and care services, with the larger goal of reducing MTCT. As part of PHFS, in late 2013, under the auspices of the Ministry of Health of Mozambique (MISAU) and the United States Agency for International Development (USAID), the USAID Applying Science to Strengthen and Improve Systems (ASSIST) Project introduced a community-based quality improvement (QI) approach to improve ANC service uptake in 39 bairros (communities) in Gaza Province. The community-led QI approach aimed to find ways that the larger community could supplement and enhance the work of activistas and health-care providers. Given the limited period of available funding, the activity was implemented as a demonstration project to show the potential for applying community-based QI methods to increase the number of women attending ANC.
The specific goal of the PHFS community demonstration project was to apply QI principles to increase community awareness, improve community–facility linkages, and increase access to ANC and HIV services for pregnant women. The specific improvement aims for this project were to:
Increase the number of pregnant women identified by community group members,
Increase the percentage of pregnant women who accessed ANC services,
Increase the percentage of pregnant women tested for HIV, and
Increase the percentage of HIV-positive pregnant women who initiated treatment.
These aims represent the first steps in connecting pregnant women with skilled providers and facility-level care early in pregnancy.
A review by Lassi et al suggested that community interventions for maternal and newborn care can reduce maternal morbidity and improve newborn outcomes,9 while another review by Hurst et al showed that demand-side interventions, including community interventions, can increase service use.10 Chibwesha et al showed that earlier initiation of pregnant women on ART reduced the risk of MTCT in Zambia.11 Therefore, the theory of change for this activity hypothesized that if pregnant women can be brought into care early and are supported by their families and communities to regularly attend ANC, then there will be increased opportunities for health workers to provide comprehensive care to pregnant women, including the prevention of HIV transmission to their child, which would, in turn, lead to lower transmission rates.12
This article presents a case study on the approach, implementation, and results of community-led QI to identify more pregnant women in the community and encourage them to receive ANC at facilities. The case study draws on project reports, self-reported data from the communities and facilities, and discussions conducted with health facility nurse coaches, bairro committee members, activistas, and community groups for the purposes of project documentation.13
Methodology
In this article, we describe the application of QI in a community setting and the accomplishments gained from that process. Quality improvement methods have been successfully adapted to community settings to improve maternal and newborn health.14-16 This intervention applied the Community Health System Strengthening model, in which an adapted QI intervention is managed by a community improvement team (CIT) composed of community groups, community health workers, facility staff, and local government officials for the purposes of identifying ways that community group members can support the community’s health goals and the local cadre of community health workers.14,17 As described in detail below, the CITs apply a QI process of setting or adopting an aim, analyzing the situation to identify problems in the process, developing change ideas that would potentially address those problems, testing small, measurable changes through plan-do-study-act cycles,18 and reviewing data regularly to determine progress toward the aim. Teams then decide whether to adopt, adapt, or discard a given change based on whether or not it resulted in improvement. Applying the Community Health System Strengthening model has been shown to improve health messaging, case identification, linkages with the formal health sector, and follow-up.14 The CIT is usually supported by coaches at the health facility and the district health management team.
Site Selection
Licilo, Chissano, and Incaia health centers and their associated catchment areas of 15, 11, and 13 bairros, respectively, in Bilene District, Gaza Province, were selected by the Ministry of Health and the ASSIST team based on high rates of HIV prevalence and low coverage of EMTCT services. HIV prevalence in Gaza was as high as 29.9% for women and 16.8% for men in 2009.1 These 3 districts allowed for easy and low-cost access from Maputo. No other EMTCT or MCH projects were taking place in these 3 health centers at the time the activity took place.
Implementation
In late 2013, the ASSIST team supported Bilene District Health Office staff to orient community leaders in the bairros surrounding the Licilo, Chissano, and Incaia health centers on the objectives for the activity and the proposed approach. Following the orientation, the community leaders held discussions with the wider community about the objectives of the activity and their roles in selecting representatives to send to the initial training. Applying Science to Strengthen and Improve System and the District Health Office led a training in February 2014 for health facility staff and selected community representatives on QI, engaging community groups, and developing a data and communication process between the community and facility.
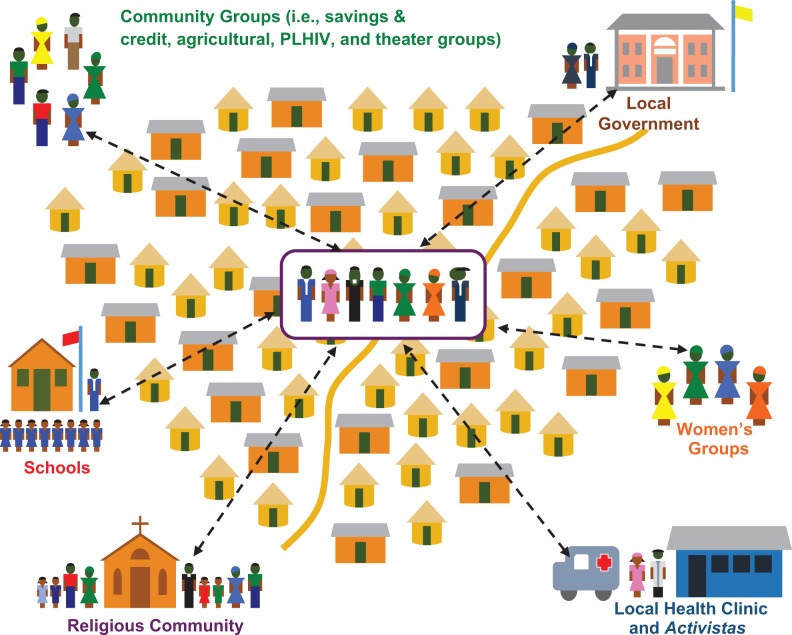
The participating community representatives then met with community leaders to further explain the importance of pregnant women enrolling early in ANC, introduce the improvement aims, and what was needed from the leaders and community group members to improve care. They worked together to develop a list of active community groups, oriented these groups to the activity, and asked them to designate a representative to the CIT (or “bairro committees”). Community groups which joined the CIT included local governing structures, school parents’ associations, agricultural groups, savings and loans groups, religious groups, and street theater and other performing groups (see Figure 1). In total, 39 bairros set up CITs to support the activistas in health messaging, data collection, and follow-up.
Figure 1.
Forming a community improvement team (CIT).
Each participating community group agreed to dedicate 30 minutes at their regular meetings to discuss health topics, especially the importance of early ANC. This facilitated the rapid spread of health messages to a large audience from the health-care worker to the CIT and from the CIT to their respective community groups, finally reaching households. Likewise, they set up a data collection system in which the members of the community group would bring information, such as who was pregnant in their households, and then pass it on to the CIT representative who, in turn, informed the MCH nurse from the facility who monitors whether the women have come for ANC.
Community improvement teams met monthly to discuss how the community groups could assist and support the health-care workers and activistas to encourage early ANC. Each CIT reviewed simple measures, such as the number of pregnant women identified and how many of them went to their first ANC visit. They also identified and tested strategies for encouraging attendance at ANC.
Community improvement teams generally met monthly and a community advisor from the project would frequently attend to provide support and facilitation (every month to 8 weeks). Maternal and child health nurses from the health centers were trained as coaches with the responsibility of helping CITs through the improvement process. As the nurses’ workload precluded participation in multiple CIT meetings each month, a health committee (high-level improvement team) was created at each health center which included the nurse coach, activistas, and representatives from each of the CITs so that delegates could participate and communicate back to the health center.
The health committee also met monthly with support from the ASSIST community advisor to review progress toward the improvement aims by comparing the number of pregnant women identified by the community to the number who attended ANC at the facility. In addition, the nurse would answer questions and provide health information, which could be shared with the wider community through the improvement team members and community group structure. The health committee members also discussed possible ways that community groups could support and promote the health of pregnant women, which would be brought back to the CITs to discuss and test.
District leaders, nurse coaches, and the community advisor convened learning sessions in May and August 2014. Learning sessions were workshops in which improvement teams could share their experiences and results, learn about the successes and failures of other CITs, reinforce key health messages, and discuss any challenges. The first learning session focused on mobilizing communities, encouraging participation from community groups, and setting up improvement teams in new health facility catchment areas. The second learning session focused on building QI skills, such as using data and learning rapid cycle problem-solving (plan–do–study–act cycles). In March 2015, a final meeting was convened to gather learning on how best to organize a community system to support pregnant women.
Data Collection
Four indicators were developed to monitor progress toward achieving the improvement aims as shown in Table 1.
Table 1.
Primary Indicators Followed by the PHFS Community Teams in Gaza Province.
| Indicator | Definition | Source |
|---|---|---|
| Number of pregnant women identified by all community groups each month | Num: # of pregnant women identified by all community groups each month | Community group and bairro committee records |
| Percentage of identified pregnant women receiving ANC | Num: # of pregnant women, identified by community groups, who attended ANC Den: # of pregnant women identified each month by community group |
Community group and bairro committee records and health center records |
| Percentage of pregnant women receiving ANC who were tested for HIV each month | Num: # of pregnant women tested for HIV each month Den: # of all pregnant women receiving care at the facility attending ANC each month |
Health center records |
| Percentage of pregnant women who were found to be HIV positive put on treatment each month | Num: # of pregnant women who tested positive for HIV who were put on treatment each month Den: # of all pregnant women receiving care at the facility who tested positive for HIV each month |
Health center records |
Abbreviations: ANC, antenatal care; PHFS, Partnership for HIV-Free Survival; Num, numerator; Den, denominator.
The ASSIST community advisor supported CITs to collect data and would review the data and clarify indicators during support visits. The ANC indicator was the most challenging for teams to understand, but the advisor worked with CITs to clarify a definition (Table 1). The data on HIV testing and treatment were collected by the health facility nurse, who would report on the overall achievement for the community and not discuss individual names. No external validation of the data was conducted beyond review by the community advisor.
Ethical Approval and Informed Consent
Ethical approval or informed consent was not required. The information in this article is derived from project reports, self-reported data from the communities and facilities, and discussions conducted with health facility and community staff and volunteers for the purposes of project documentation. No individual-level patient data are presented.
Results
Barriers to Care
Table 2 describes barriers to care that pregnant women experience, taken from discussions with community groups and improvement teams during initial start-up and implementation.
Table 2.
Community and Health System Barriers to Care.
| Community Barriers | Health System Barriers |
|---|---|
|
|
Abbreviation: ANC, antenatal care.
Changes Made to Improve Care
Community improvement teams developed new processes and developed changes to improve community-level support for early ANC (see Table 3).
Table 3.
Changes at the Community Level to Improve Identification of Women and Attendance at Early ANC.
| Community Group Structure/Mission | Pregnancy Identification | ANC Attendance |
|---|---|---|
| Community groups added time to discuss health issues at their regular meetings Community groups collected information on pregnant women in their network Process designed for data collection on pregnant women identified by community groups and for sharing with CIT and health facilities Process designed for regular joint review of performance on ANC attendance and HIV testing by health facilities, CIT, and community groups |
Encouraged women, their partners, and mothers-in-law to self-identify when pregnant by talking to the designated community group or improvement team representative Introduced a referral form from the community group for pregnant women to take to the health facility; team members or activistas would follow-up and encourage ANC attendance Created skits and songs to perform on market days to encourage early ANC; collected names of pregnant women (voluntary) and encouraged them one-on-one to attend ANC (theater group in Licilo) |
Assigned a specific person, such as a community group member, improvement team member, or activista to visit the woman and provide her with information on the importance of ANC Assigned someone to talk to the mother-in-law as many husbands worked in South African mines, leaving the mother-in-law in charge of care-seeking decisions Targeted ANC messages at older women (mothers-in-law) and men (husbands) |
Abbreviations: ANC, antenatal care; CIT, community improvement team.
The combined membership of all the participating community groups represented a significant proportion of the households; they were more easily able to identify pregnant women than the activista alone. However, several challenges remained. Due to stigma, improvement team members did not directly discuss the need for HIV testing but discussed other topics for why ANC was important such as bed nets, anemia, or testing for other diseases. Another challenge was how to get health messages to husbands working in South African mines.
Results of Community Identification of Pregnant Women
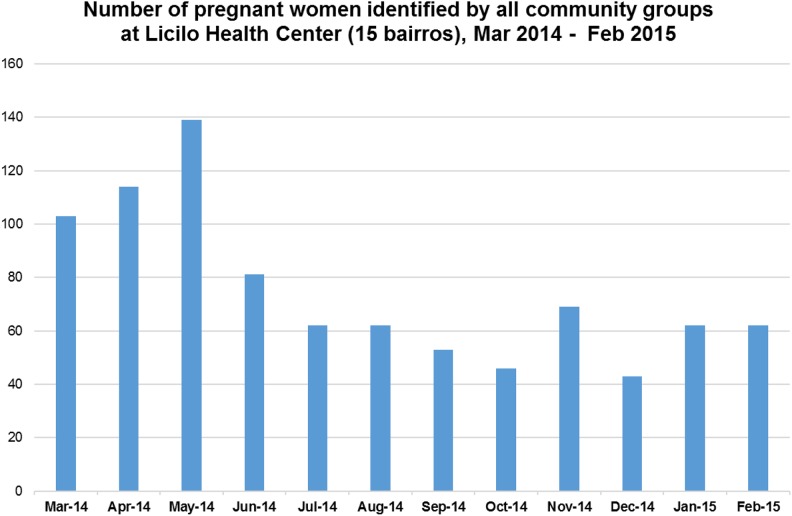
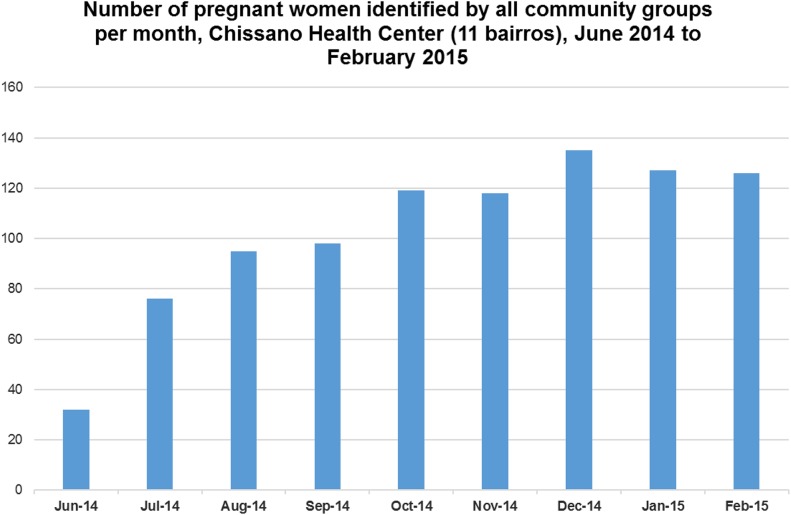
Figure 2 shows the number of pregnant women identified around Licilo Health Center. Between March 2014 and February 2015, the community groups around Licilo Health Center identified a total of 896 pregnant women. The initial high numbers reflect the pregnant women identified who were previously unknown to the health workers. After a few months, these numbers leveled off to only newly pregnant women. Figure 3 shows the number of pregnant women identified (926 in total) around Chissano Health Center. The number grew more gradually over time because of the slow initial engagement of community groups. Community groups around Incaia Health Center also took longer to became engaged, such that the identification of pregnant women increased over time, reaching 409 pregnant women by February 2015.
Figure 2.
Number of pregnant women identified by all community groups, Licilo Health Center (15 bairros).
Figure 3.
Number of pregnant women identified by community groups per month, Chissano Health Center (11 bairros).
Results of ANC Attendance
Community improvement teams were confused about how to record women who were found in one month but attended ANC in a different month, despite numerous attempts to clarify this measure by the community advisor. In the end, if a woman attended ANC, it was recorded in the month in which she was identified, even if ANC attendance had happened later. The measure did not indicate the time to linkage, but whether or not a visit had occurred at any time.
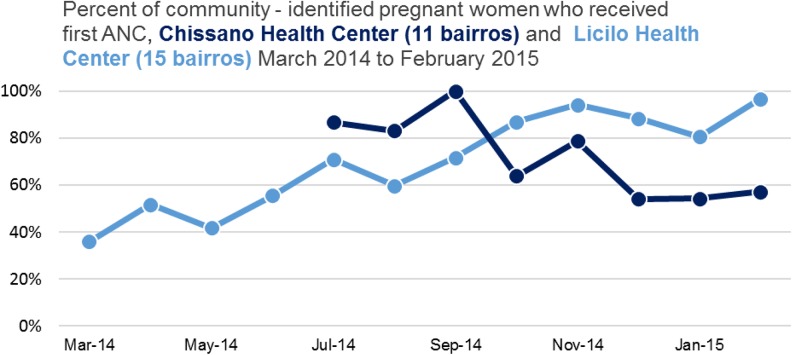
In Licilo, there was an increase from 36% in March 2014 to 97% in February 2015 in the percentage of pregnant women receiving their first ANC (see Figure 4). Over 12 months, the cumulative percentage of women who went to ANC was 64%. In contrast, data from the Chissano Health Committee showed a decreasing percentage of pregnant women receiving ANC from 87% in July 2014 to 57% in February 2015. Possible reasons for this include data collection errors at the beginning of the activity or the inability of the health center to meet demand.
Figure 4.
Percentage of community-identified pregnant women who received first antenatal care (ANC), Chissano Health Center (11 bairros) and Licilo Health Center (15 bairros).
Incaia had inconsistent community-level data collection before September 2014, which made it difficult to determine a change in performance. Health facility data for all women attending ANC showed an average of 46 women per month between June and August 2014, increasing to 55 per month between September 2014 and February 2015 which implies increased attendance.
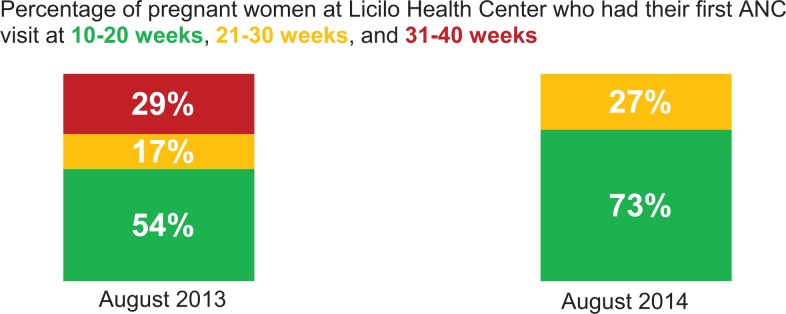
Licilo Health Center conducted an additional chart review comparing the week of gestation of pregnant women attending first ANC. The review reflected a shift to earlier first ANC attendance (Figure 5).
Figure 5.
Pregnant women attending first antenatal care (ANC) by weeks of gestation, Licilo Health Center.
Testing and Treatment
During the period of intervention for this activity, no significant change was seen in any facility in the percentage of pregnant women receiving HIV testing or initiating treatment. In all sites, the percentage of pregnant women who attended ANC and were tested for HIV was high throughout the initiative, with an average of 97% in Licilo, 93% in Chissano, and 90% in Incaia. All facilities were performing well on initiating treatment: 100% of pregnant women found to be HIV positive were initiated on treatment (74 women in Licilo, 124 in Chissano, and 43 in Incaia) between March 2014 and February 2015.
Discussion
Our results showed that, similar to other studies,10,19 engaging communities in maternal health increased demand and access to services, specifically ANC. In particular, the use of the Community Health Systems Strengthening approach, which combines community engagement and QI, was able to increase the participation of community groups in pregnancy identification and encourage more pregnant women to begin ANC. This experience showed that despite education and literacy barriers, communities can apply QI approaches and learn to use data to review performance and make changes to improve care.14
More research is needed to explain the variation between the sites. One possible reason that results from Incaia and Chissano were not as compelling as those from Licilo is because of the slower engagement of groups to participate in the CITs in those communities. The Licilo Health Center nurse and a few key community groups were interested and highly motivated and therefore served as champions to move the activity along quickly.
Community-based approaches have been shown to improve continuum of care for PMTCT.20 The 39 communities in Gaza Province achieved the aim of identifying more pregnant women, connecting them with the health-care system, and getting them enrolled in ANC, which can contribute to early testing and treatment for HIV, reducing the risk of transmission. Women receiving care earlier in pregnancy allows for HIV testing, knowledge of status, and, when positive, immediate initiation on treatment in addition to building a foundation for the provider–client relationship. The CIT could have played a larger role in HIV testing for pregnant women and their partners, but prevailing stigma prevented open discussion of the need for testing.
The Community Health Systems Strengthening approach can widen the reach of the formal health sector. Community-based health workers, in this case activistas, can be more motivated by the support and interactions they receive from communities than by their interactions with the formal health system.21 In Mozambique, activistas and community group members working together reached more households and identified pregnant women previously unknown to health-care workers. The health committee enabled community group members, activistas, and facility staff to develop working relationships and information flow which could be used for other health areas.
For future implementation of the Community Health Systems Strengthening approach, the authors recommend that community QI interventions be closely linked with a similar intervention at the local health facility. Community QI alone can create demand which the facility may be ill-equipped to manage, as may have been the case for at least one of the 3 health centers.
Linking community-level interventions with improved health outcomes remains a challenge for researchers.22 Additional research is needed on the effects that CITs’ efforts have on the whole continuum of care and outcomes. For example, pregnant HIV-positive women are more frequently lost to follow-up than other HIV-positive adults,23 and loss to follow-up increases in the period before delivery and postpartum.24 Communities have the potential to influence attitudes and care-seeking behaviors, as well as developing interventions which can support mothers and families to stay in care, which could be a future focus of implementation and research.
More implementation time is needed to determine the sustainability of the approach in addition to the impact that it could have on retention in care. Areas for future research include the cost-effectiveness of the approach, sustainability of the approach following the end of the activity, and connection of community work to outcomes.
Limitations
Low levels of education, literacy, and numeracy skills created difficulties in data collection and analysis. Illiterate CIT members found creative solutions for recording data, such as engaging school children to write down information. The community advisor found simple ways to explain the data, including comparing numbers rather than using percentages. Initial data were not reliable, and it took several months of working with CITs to get consistent information. The early unreliable or unverifiable data were excluded from the data presented here.
Conclusions
The application of a QI approach in 39 communities in Gaza Province resulted in an increase in identification of pregnant women and early entry into ANC, which are critical first steps to timely EMTCT care. The intervention showed that communities can influence and support care-seeking and access to ANC. In addition, despite education and literacy barriers, this case shows that QI can be applied at the community level to improve care.
Acknowledgments
The authors would like to acknowledge the work and efforts of the 240 community groups in Gaza Province who volunteered their time and efforts to help connect pregnant women with care. The authors would like to thank the nurse coaches, Nélia Mugadui, Chissano Health Center, and Berta Aníbal Chambe, Incaia Health Center, who supported and guided these community groups. Finally, the authors would like to thank the leaders of Bilene District, including Fanuel Baloi, District Health Director; Fernando Matule, District Medical Chief; Virginia Nguila, Local Chief of the Administrative Post of Chissano; and Angelina Macamo, Violeta Chambule, and Maria Herculano Macave, the Locality Chiefs for Chissano, Chicotane, and Licilo, respectively. The authors would also like to acknowledge the contributions and support from former URC employees in Mozambique, Luke Dausse and Mario Bambo, and in the United States, Anisa Ismail. The authors would like to thank Dionisio Matos, Katherine Raleigh, and Timothy Quick from USAID for their technical direction. Finally, the authors would like to thank Amy Stern of URC for her overall direction and guidance of the PHFS activities under ASSIST. The development of this manuscript was made possible by the support of the American people through USAID.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for the activities in Mozambique came from the President’s Emergency Plan for AIDS Relief and the USAID-supported Partnership for HIV-Free Survival initiative.
References
- 1. Health MMo. Mozambique National Survey on Prevalence, Behavioral Risks and Information about HIV and AIDS (INSIDA 2009) Key Findings. Maputo, Mozambique: Instituto Nacional de Saúde (INS) of the Ministry of Health; 2009. [Google Scholar]
- 2. United Nations Programme on HIV and AIDS. UNAIDS Global Plan Country Factsheet Mozambique. http://www.unaids.org/sites/default/files/media/documents/UNAIDS_GlobalplanCountryfactsheet_mozambique_en.pdf. Published 8 June 2016 Accessed April 16, 2019.
- 3. World Health Organization. Mozambique HIV country profile. 2016; https://www.who.int/hiv/data/Country_profile_Mozambique.pdf?.ua=1. Accessed April 16, 2019.
- 4. Chapman RR. Endangering safe motherhood in Mozambique: prenatal care as pregnancy risk. Soc Sci Med. 2003;57(2):355–374. [DOI] [PubMed] [Google Scholar]
- 5. Finlayson K, Downe S. Why do women not use antenatal services in low- and middle-income countries? A meta-synthesis of qualitative studies. PLoS Med. 2013;10(1):e1001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Munguambe K, Boene H, Vidler M, et al. Barriers and facilitators to health care seeking behaviours in pregnancy in rural communities of southern Mozambique. Reprod Health. 2016;13(suppl 1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ackerman Gulaid L, Kiragu K. Lessons learnt from promising practices in community engagement for the elimination of new HIV infections in children by 2015 and keeping their mothers alive: summary of a desk review. J Int AIDS Soc. 2012;15(suppl 2):17390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. De Schacht C, Mabunda N, Ferreira OC, et al. High HIV incidence in the postpartum period sustains vertical transmission in settings with generalized epidemics: a cohort study in Southern Mozambique. J Int AIDS Soc. 2014;17(1):18808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lassi ZS, Haider BA, Bhutta ZA. Community-based intervention packages for reducing maternal and neonatal morbidity and mortality and improving neonatal outcomes. Cochrane Database Syst Rev. 2010;(11):CD007754. [DOI] [PubMed] [Google Scholar]
- 10. Hurst TE, Semrau K, Patna M, Gawande A, Hirschhorn LR. Demand-side interventions for maternal care: evidence of more use, not better outcomes. BMC Pregnancy Childbirth. 2015;15:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chibwesha CJ, Giganti MJ, Putta N, et al. Optimal time on HAART for prevention of mother-to-child transmission of HIV. J Acquir Immune Defic Syndr. 2011;58(2):224–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Deressa W, Seme A, Asefa A, Teshome G, Enqusellassie F. Utilization of PMTCT services and associated factors among pregnant women attending antenatal clinics in Addis Ababa, Ethiopia. BMC Pregnancy Childbirth. 2014;14(1):328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Stover K TI, Stern A, Shrestha R. Partnership for HIV-Free Survival Community Demonstration Project in Gaza, Mozambique: Technical Report. Bethesda, MD: USAID ASSIST Project; 2015. [Google Scholar]
- 14. Lunsford SS, Fatta K, Stover KE, Shrestha R. Supporting close-to-community providers through a community health system approach: case examples from Ethiopia and Tanzania. Hum Resour Health. 2015;13(1):12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Horwood CM, Youngleson MS, Moses E, Stern AF, Barker PM. Using adapted quality-improvement approaches to strengthen community-based health systems and improve care in high HIV-burden sub-Saharan African countries. AIDS. 2015;29(suppl 2):S155–S164. [DOI] [PubMed] [Google Scholar]
- 16. Tesfaye S, Barry D, Gobezayehu AG, et al. Improving coverage of postnatal care in rural Ethiopia using a community-based, collaborative quality improvement approach. J Midwifery Womens Health. 2014;59(s1):S55–S64. [DOI] [PubMed] [Google Scholar]
- 17. Project HCI. Strengthening Community Health Systems to Improve Health Care at the Community Level. Bethesda, MD: Health Care Improvement Project; October 2011. [Google Scholar]
- 18. Langley GJ MR, Nolan KM, Nolan TW, Norman CL, Provost LP. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. 2nd ed San Francisco, CA: Jossey-Bass; 2009. [Google Scholar]
- 19. Morrison J, Tamang S, Mesko N, et al. Women’s health groups to improve perinatal care in rural Nepal. BMC Pregnancy Childbirth. 2005;5(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Marcos Y, Phelps BR, Bachman G. Community strategies that improve care and retention along the prevention of mother-to-child transmission of HIV cascade: a review. J Int AIDS Soc. 2012;15(suppl 2):17394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Robinson SA, Larsen DE. The relative influence of the community and health system on work performance: a case study of community health workers in Colombia. Soc Sci Med. 1990;30(10):1041–1048. [DOI] [PubMed] [Google Scholar]
- 22. Rifkin SB. Examining the links between community participation and health outcomes: a review of the literature. Health Policy Plan. 2014;29(suppl_2):ii98–ii106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tenthani L, Haas AD, Tweya H, et al. Retention in care under universal antiretroviral therapy for HIV-infected pregnant and breastfeeding women (‘Option B+’) in Malawi. AIDS. 2014;28(4):589–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rawizza HE, Chang CA, Chaplin B, et al. Loss to follow-up within the prevention of mother-to-child transmission care cascade in a large ART program in Nigeria. Curr HIV Res. 2015;13(3):201–209. [DOI] [PMC free article] [PubMed] [Google Scholar]