Abstract
HIV/AIDS prevalence rates in South Africa are among the highest in the world. The key to reducing transmission is the dissemination of accurate knowledge. Here, we investigate the accuracy of HIV/AIDS knowledge among youth affected by the disease. Data from the Fourth South African National HIV, Behaviour and Health Survey (2012) are used and a weighted sample of 4 095 447 youth (15-24 years old) who have known or cared for someone with HIV/AIDS are analyzed. Results show that more than one-third (40.37%) of youth in South Africa are affected by the disease. One-quarter of the affected youth have 75% accurate knowledge of the virus, while only 10% have 100% accurate knowledge. Rural place of residence (odds ratio [OR] = 0.61) and looking for work (OR = 0.39) are less likely to have accurate knowledge. Youth without disabilities (OR = 2.46), in cohabiting (OR = 1.69), and in dating (OR = 1.70) relationships are more likely to have accurate knowledge. In conclusion, in order to reduce HIV incidence and combat HIV myths, efforts to improve the accuracy of HIV knowledge among youth affected by the disease are needed. There should be more community-based campaigns to target unemployed youth in the country.
Keywords: HIV/AIDS knowledge, youth, South Africa, logistic regression
What do we already know about this topic?
Youth do not have comprehensive HIV knowledge.
How does your research contribute to the field?
This study identifies which knowledge is largely unknown among youth affected by HIV.
What are your research's implications toward theory, practice, or policy?
Through identification of the exact knowledge youth affected by the disease are lacking, programmes in South Africa can make efforts to improve interventions and knowledge- based outreach.
Introduction
Accurate knowledge of HIV/AIDS is pivotal to prevent further transmission of the disease. HIV knowledge is the correct information regarding modes of transmission, high-risk behaviors, and prevention and care strategies.1 The need for reliable, valid, and accurate tools for testing HIV knowledge has led to the development many different questionnaire scales over the years.2–4 These tools are conceptualized to evaluate the extent to which knowledge exists by age-group, sex, and other subpopulations in a number of different countries.5–7 These tools have also been adopted and adapted in various surveys, including population-based household and sexual behavior surveys.8,9
A number of studies have identified the determinants of HIV knowledge.10–13 One study found that women with more education and who are wealthy are more likely to know about HIV protective behaviors, including consistent condom use, and are less likely to have misconceptions about modes of transmission.11 Education, in particular the ability to read, makes written information, including pamphlets, billboards, newspaper articles, and health briefs and policy documents, easier to comprehend. Education also makes it possible to critically evaluate information that is disseminated and decide what correct and incorrect knowledge is. Another study of young, urban women in Kenya found that older youth (20-24 years old), having been for at least 1 HIV test in their lifetime and knowing someone, or knowing someone who died from AIDS increases the likelihood of comprehensive HIV knowledge.12 Older youth are more likely to have completed secondary education compared to adolescents (15-19 years old). For this reason, more education could translate into being able to comprehend more information regarding the disease. In addition, HIV-testing facilities offer trained consultation and support. Therefore, persons who have tested have access to a trained consultant or nurse to whom they may pose questions about the disease. Finally, knowing someone with the disease allows for dialogue and conversation regarding modes of transmission and protective behaviors between 2 or more individuals, one of whom would be speaking from experience.
Among youth in South Africa, the dissemination of accurate knowledge has been hindered by the perpetuation of AIDS myths and misinformation.14–16 Of notable importance is the impact false information has on sexual violence in the country, with 1 study reporting that 9.4% of adolescent boys, who believed that rape is a cure for HIV, demonstrated sexual violence toward a female partner.17 And with current youth HIV prevalence rates in the population being as high as 7.1%, there is need to reassess the accuracy of HIV knowledge among youth in the country.18
Further, while youth tend to have some or incomplete knowledge about HIV and how it is transmitted, evidence suggests that youth affected by the virus, that is knowing someone with HIV/AIDS in their households and/or communities, have better knowledge than youth who are not affected.19,20 However, even among youth affected by the disease, knowledge is not 100% accurate, yet these youth can play an important role as peer educators in preventing the spread of the disease within their households and communities, provided that they have the most accurate (100%) knowledge of HIV and AIDS. Therefore, the primary purpose of this study is to identify the factors associated with HIV knowledge accuracy among youth affected by the disease in South Africa.
Methods
Study Design
This is a cross-sectional study using the Fourth South African National HIV, Behaviour and Health Survey, 2012 (http://www.hsrc.ac.za/en/researchdata/).
Survey and Sample
The 2012 survey is the fourth in the series of national household HIV surveys conducted by a consortium of scientists led by the Human Sciences Research Council.21 The data pertain to the HIV status, demographic, socioeconomic, and behavioral characteristics of the sample.21 In the 2012 survey, over 38 000 people of all ages were interviewed.21 The number of youth who participated in the survey is (unweighted) 8221. For this study, a weighted sample of youth affected by HIV was determined through positive responses (yes) to any of the following questions “What has made you take the problem of HIV/AIDS more seriously?”, with response options of “knowing or talking to someone with HIV/AIDS”; “Caring for a person with HIV/AIDS”; “Knowing someone who has died of AIDS.” A weighted total sample of 4 095 447 youth affected by HIV/AIDS was identified. The percentage of youth affected by HIV/AIDS is 40.37%.
Variable Definitions
Dependent Variable
The dependent variable in this study is “accuracy of HIV knowledge” which is defined as having correct knowledge of all (100%) questions from the survey. Correct answers to each of the questions have been determined from similar studies that have used the same questions.12,22 Using 8 questions on HIV knowledge, a variable showing the percentage of correct answers was created. The survey asked a number of questions on HIV knowledge, attitudes, perceptions and behaviors (KAPB).21 There were only 8 questions pertaining to knowledge specifically, the rest were measurements of attitudes, perceptions, and behaviors and had been adopted from a United Nations Programme on HIV and AIDS recommended source.23 This study specifically focuses on the knowledge aspect of the KAPB regarding HIV and AIDS. The reason why knowledge is isolated as an outcome of this study is because knowledge can shape attitudes, perceptions, and even behaviors, particularly among youth.24 Knowledge therefore is a key initial component to shaping KAPB among youth affected by the disease. The questions are: (1) “Can AIDS be cured?”; (2) “Can a person reduce their risk of HIV by having fewer sexual partners?”; (3) “Can a healthy-looking person have HIV?”; (4) “Can HIV be transmitted from a mother to her unborn baby?”; (5) “Can the risk of HIV transmission be reduced by having sex with only one uninfected partner who has no other partners?”; (6) “Can a person get HIV by sharing food with someone who is infected?”; (7) “Can a person reduce the risk of getting HIV by using a condom every time he/she has sex?”; and (8)”Can medical male circumcision reduce the risk of HIV infection in males?”.
Independent Variables
The predictor variables for the study include age (15-19 and 20-24 years old); sex (male or female); race (African, colored, white, Indian or Asian or other); place of residence (urban or rural); self-reported disability status (yes or no); employment status (employed, not looking for work, student, looking for work, unable to work); education status (in school, not in school—completed grade 12 or not in school for another reason); marital status (married, cohabiting, dating and not living together, single or other); and source of HIV knowledge (peers or family, religious institution or community and AIDS organization, clinic or hospital). For the last variable, 11 categories of sources of information were grouped into the 3 variable responses.
Statistical Analysis
Frequency and percentage distributions are used to show the characteristics of the sample. Cross-tabulations are done to show the distribution of the sample by independent variables, and statistical significance (P values) is shown. An adjusted binary logistic regression model was fitted at a 95% level of significance to identify the likelihood of accurate (100%) HIV knowledge by respondents’ characteristics. Accurate knowledge (1) in the model is measured as correct responses to all 8 questions while, 0 to 7 correct answers is considered inaccurate knowledge (0). All tests were done using STATA version 13.
Results
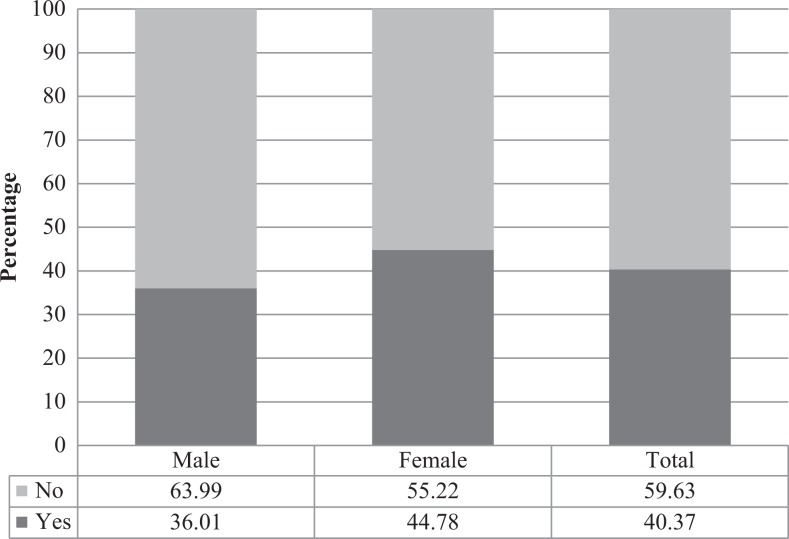
Figure 1 shows that 36.01% of male and 44.78% of female youth are affected by HIV. A total of 40.37% of all youth in the country are affected by HIV.
Figure 1.
Weighted percentage distribution of youth affected (yes) and not affected (no) by HIV by sex (weighted).
Table 1 shows that most youth (83.35%) are aware that a person with HIV can look healthy. A further 80.67% are aware that HIV cannot be transmitted by sharing food with an HIV-positive person. However, less than half of the sample (48.13%) is aware that medical male circumcision reduces the risk of HIV infection among males.
Table 1.
Ranking of Correct HIV Knowledge Questions Among Respondents Affected by HIV.
| Knowledge of HIV questions | Correct answer | Respondents N = 4 095 447 | |
|---|---|---|---|
| N | % | ||
| Can a Healthy looking person have HIV? | Yes | 3 413 468 | 83.35 |
| Can a person get HIV by sharing food with someone who is positive? | No | 3 303 759 | 80.67 |
| Can a person reduce the risk of HIV by using a condom every time he has sex? | Yes | 3 172 419 | 77.46 |
| Is there a cure for HIV? | No | 3 082 490 | 75.27 |
| Can HIV be transmitted from a mother to her unborn child? | Yes | 3 007 404 | 73.43 |
| Can the risk of HIV transmission be reduced by having sex with only one partner? | Yes | 2 831 754 | 69.14 |
| Can a person reduce the risk of HIV by having fewer sexual partners? | Yes | 2 440 196 | 59.58 |
| Can medical circumcision reduce the risk of HIV infection in males? | Yes | 1 971 046 | 48.13 |
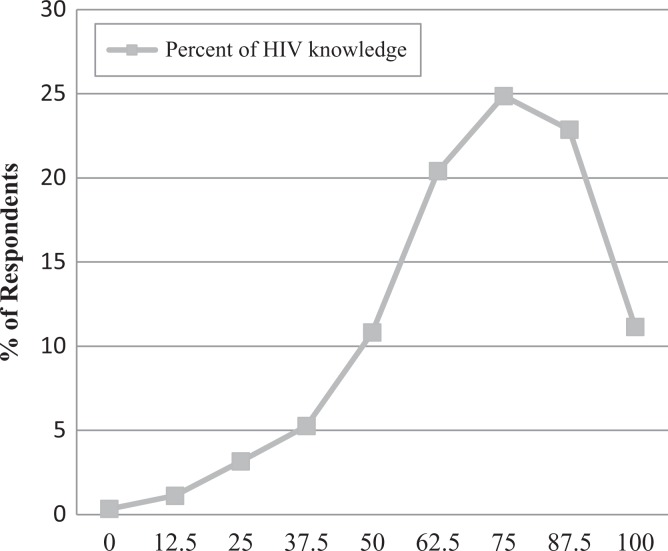
Figure 2 shows that only 11% of youth who are affected by HIV have 100% accuracy of HIV knowledge. Most youth, 25% of the sample, has 75% accurate knowledge. This is equivalent to getting 6 of the 8 questions correct.
Figure 2.
Weighted percentage distribution of accuracy of HIV knowledge (in percentages) among youth.
Table 2 shows that the majority of youth do not have 100% accurate knowledge of HIV. Among those with 100% accuracy, most are 20 to 24 (12.32%) years old, reside in urban areas (13.48%), have no disability (11.38%), are employed (17.38%), married (13.84%), and source their information from peers and family members (19.64%). By race, the African population has the lowest percentage of complete accuracy at 10.56%, with Indian/Asian youth having the highest at 40.21%. Finally, only 10.49% of youth with 100% accuracy obtain their information from an AIDS organization or clinic.
Table 2.
Weighted Percentage Distribution of Accuracy of HIV Knowledge (in Percentages) by Respondents’ Characteristics, Row Percentages.
| Characteristics | All (N = 4 095 447) | Accuracy of HIV Knowledge | |||
|---|---|---|---|---|---|
| 0% | ≤50% | >50%/ <100% | 100% | ||
| Age-groupa | |||||
| 15-19 (years) | 41.46 | 0.23 | 23.35 | 66.94 | 9.49 |
| 20-24 (years) | 58.54 | 0.42 | 18.24 | 69.01 | 12.32 |
| Sexa | |||||
| Male | 44.86 | 0.5 | 22.03 | 65.64 | 11.83 |
| Female | 0.00 | 0.22 | 19 | 70.19 | 10.59 |
| Racea | |||||
| African | 89.64 | 0.37 | 20.58 | 68.48 | 10.56 |
| White | 7.24 | 0 | 7.76 | 77.93 | 14.31 |
| Colored | 7.24 | 0.13 | 23.33 | 62.64 | 13.89 |
| Indian/Asian | 0.83 | 0.32 | 6.75 | 52.71 | 40.21 |
| Other | 0.03 | 0 | 0 | 86.83 | 13.17 |
| Place of residencea | |||||
| Urban | 58.99 | 0.07 | 15.81 | 70.63 | 13.48 |
| Rural | 41.01 | 0.74 | 26.9 | 64.58 | 7.79 |
| Disabilitya | |||||
| Yes | 1.40 | 0 | 34.69 | 63.23 | 2.08 |
| No | 98.46 | 0.35 | 20.08 | 68.18 | 11.38 |
| Unsure | 0.14 | 0 | 96.55 | 3.45 | 0 |
| Employment Statusa | |||||
| Employed | 18.09 | 0.19 | 16.26 | 66.17 | 17.38 |
| Not looking for work | 30.17 | 0.73 | 20.27 | 69.05 | 9.95 |
| Student | 46.08 | 0.22 | 21.81 | 68.70 | 9.27 |
| Looking for work | 5.20 | 0.06 | 24.31 | 70.29 | 5.35 |
| Unable to work | 0.45 | 0 | 37.99 | 52.85 | 9.16 |
| Educationa | |||||
| In school | 87.19 | 0.16 | 25.09 | 66.6 | 8.15 |
| Not in school—Completed Grade 12 | 3.34 | 0 | 20.34 | 62.45 | 17.21 |
| Not in school—other reason | 9.47 | 0 | 24.47 | 61.53 | 14 |
| Marital statusa | |||||
| Married | 3.77 | 0.08 | 6.59 | 79.48 | 13.84 |
| Cohabiting | 5.20 | 0 | 18.85 | 59.63 | 21.52 |
| Going steady | 46.34 | 0.22 | 19.51 | 68.13 | 12.14 |
| Single | 42.12 | 0.57 | 22.04 | 68.38 | 9 |
| Other | 2.57 | 0 | 27.28 | 65.26 | 7.46 |
| Source of HIV Knowledgea | |||||
| Peer/family | 9.51 | 0 | 18.57 | 61.79 | 19.64 |
| Religious/community | 4.28 | 1.02 | 26.87 | 62.77 | 9.34 |
| AIDS org / clinic | 86.21 | 0.32 | 20.18 | 69 | 10.49 |
a P values <.05.
Table 3 shows the results of the adjusted binary logistic regression model for accuracy of HIV knowledge by characteristics of the respondents. The results show that rural place of residence (odds ratio [OR] = 0.61), looking for work (OR = 0.39), and not in school for another reason (OR = 0.89) are less likely to have accurate HIV knowledge. Alternatively, not having a disability (OR = 2.46), cohabiting (OR = 1.69), and dating (OR = 1.70) are associated with higher likelihood of accurate HIV knowledge. The results show that age, sex, race, and source of knowledge are not statistically significant predictors of accuracy of HIV knowledge.
Table 3.
Logistic Regression Model of the Likelihood of Accurate HIV Knowledge by Respondent’s Characteristics, Showing Odds Ratios.
| Characteristics | Odds Ratio | P Value | 95% Confidence Interval | |
|---|---|---|---|---|
| Age-group (RC:15-19) | ||||
| 20-24 | 0.23 | .167 | 0.0280 | 1.8539 |
| Sex (RC: Male) | ||||
| Female | 1.17 | .357 | 0.8363 | 1.6422 |
| Race (RC: African) | ||||
| White | 4.43 | .158 | 0.5608 | 34.9257 |
| Colored | 1.06 | .794 | 0.6860 | 1.6372 |
| Indian/Asian | 1.67 | .375 | 0.5399 | 5.1415 |
| Place of residence (RC: Urban) | ||||
| Rural | 0.61* | .000 | 0.4923 | 0.8725 |
| Disability (RC: Yes) | ||||
| No | 2.46* | .004 | 1.9854 | 3.0104 |
| Employment status (RC: Employed) | ||||
| Not looking for work | 1.05* | .035 | 1.0302 | 3.5641 |
| Student | 0.70 | .576 | 0.2019 | 2.4329 |
| Looking for work | 0.39* | .045 | ||
| Unable to work | 1.46 | .713 | 0.1941 | 10.9718 |
| Education (RC: In School) | ||||
| Not in school—Completed Gr 12 | 1.09* | .000 | 1.0421 | 2.9326 |
| Not in school—Other reason | 0.89* | .003 | 0.5672 | 0.9236 |
| Marital status (RC: Married) | ||||
| Cohabiting | 1.69* | .026 | 1.4387 | 1.8426 |
| Dating | 1.70* | .005 | 1.5386 | 1.8924 |
| Single | 0.61 | .144 | 0.3173 | 1.1826 |
| Other | 0.35 | .011 | 0.1552 | 0.7876 |
| Source of HIV Knowledge (RC: Peers/Family) | ||||
| Religious/community | 1.77 | .365 | 0.5160 | 6.0404 |
| AIDS org / clinic | 2.13 | .043 | 1.0252 | 4.4197 |
*p-value < 0.05. RC = Reference Category.
Discussion
The aim of this article is to identify the level and factors associated with accurate HIV knowledge among youth affected by the disease. More than one-third of all youth in the country are affected by HIV/AIDS. This is plausible considering HIV infection rates in the country are high at 12.7% of the total population.25 Also, HIV disclosure is becoming less stigmatized in the country with research showing that among HIV-positive females in the Western Cape province, disclosure of status to some family, friends, and partners was common practice, and tacit exposure, seen through taking medication in front of others, was not uncommon.26 This makes it more likely that youth in the country would be aware of someone living with or who has died from the disease in their households and communities.
A small percentage of youth affected by HIV/AIDS have, by this conceptualization, accurate knowledge of the disease. Another study using the same data, but on all youth, found that HIV knowledge has been decreasing over time, from 31.5% accurate knowledge in 2008 to 26.8% in 201218 AIDS myths and misconceptions create skepticism and make youth less likely to believe in research-based knowledge that gets disseminated.27–29
While more than two-thirds of the sample are aware that an HIV-positive person can appear healthy and know that sharing food with an HIV-positive person does not spread the disease, still less than half know that medical male circumcision can reduce the risk of infection. This could be due to the recentness of the finding and the consequent debate that surrounds the generalizability of the results. At present scholars and practitioners are moot on the issue; however, the empirical consensus is appearing to skew on the side of male circumcision being a protective factor.30–32
More positively, youth in sexually active relationships (cohabiting, dating, and married) are more likely to have accurate knowledge than single youth. This is encouraging as it suggests that sexually active youth are aware of HIV/AIDS and that knowledge can be disseminated to their partners. However, research has shown that knowledge of HIV does not always translate into practicing protective behaviors.33,34 One study found that young females who have knowledge of the disease but are in physically abusive relationships are unable to negotiate condom use with their partners.35 Another study found that while youth know that condoms prevent the transmission of HIV, they prefer not to use them.36 This literature and the result from this study suggest the need to further investigate the protective behaviors of couples who have accurate HIV knowledge.
This study contributes to the existing literature first by identifying the exact knowledge that youth are lacking. From the results, there is more that needs to be done to promote male circumcision information and practices as a viable preventative strategy. Second, the study found that youth with no employment have less knowledge than employed youth. For this reason, residential community-based programs designed to target youth who do not have places of employment should be increased. With the current unemployment rate of youth being as high as 32.4%,37 the goal should be to disseminate HIV knowledge in areas of social interactions instead of at formal places of work and schools.
The study has a few limitations. First, accuracy of HIV knowledge is based on a few questions, which do not include injecting drug use and blood transfusion modes of transmission. A survey, including these questions, should be designed to capture more comprehensive knowledge. Second, although sources of knowledge did not prove statistically significant, this study does show a more detailed study of these sources should be conducted to identify what and how much information is disseminated by different members of the youth’s networks.
In conclusion, in order for South Africa to reduce the impact of AIDS myths and misconceptions on incidence rates, efforts to increase HIV knowledge need to be made. Youth affected by the disease in their households and communities do not have 100% HIV knowledge. However, youth affected by HIV could become peer-educators and assist in disseminating knowledge in their networks and communities. And while there is no guarantee that knowledge dissemination will directly change sexual behaviors, there is the possibility that more knowledge of HIV will work indirectly to change sexual practices through dismissing AIDS myths and encouraging evidence-based safer sex habits. For this reason, youth should receive more information through public campaigns and strategies to properly protect themselves from the disease.
Footnotes
Authors’ Note: The statements made and views expressed are solely the responsibility of the authors. The authors did not need ethical approval and informed consent to use the secondary, quantitative data for this study. The data were not collected nor owned by the authors. We requested the data from the South African Human Sciences Research Council and were given fully anonymized and not privately owned data.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors would like to thank the following funding sources: Andrew W. Mellon Foundation; the Consortium for Advanced Research Training in Africa (CARTA). CARTA is jointly led by the African Population and Health Research Center and the University of the Witwatersrand and funded by the Wellcome Trust (UK) (Grant No: 087547/Z/08/Z), the Carnegie Corporation of New York (Grant No--B 8606.R02), Sida (Grant No: 54100029).
ORCID iD: Nicole De Wet  https://orcid.org/0000-0001-5750-2851
https://orcid.org/0000-0001-5750-2851
References
- 1. Carey MP, Schroder KE. Development and psychometric evaluation of the brief HIV knowledge questionnaire. AIDS Educ Prev. 2002;14(2):172–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carey MP, Morrison-Beedy D, Johnson BT. The HIV-knowledge questionnaire: development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS Behav. 1997;1(1):61–74. [Google Scholar]
- 3. Kalichman SC, Simbayi LC, Jooste S, et al. Development of a brief scale to measure AIDS-related stigma in South Africa. AIDS Behav. 2005;9(2):135–143. [DOI] [PubMed] [Google Scholar]
- 4. Zimet GD. Adolescent AIDS knowledge scale. Handbook of Sexuality-Related Measures. 1998;365–366. Sage. [Google Scholar]
- 5. Haile BJ, Chambers JW, Garrison JL. Correlates of HIV knowledge and testing: results of a 2003 South African survey. J Black Stud. 2007;38(2):194–208. [Google Scholar]
- 6. Pando MA, Balan I, Marone R, et al. HIV knowledge and beliefs among men who have sex with men (MSM) in Buenos Aires, Argentina. AIDS Behav. 2013;17(4):1305–1312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Talwar P, Rahman MFBA. Assessment of HIV knowledge among university students using the HIV-KQ-18 scale: a cross-sectional study. WHO South East Asia J Public Health. 2015;5(1):33–38. [Google Scholar]
- 8. Ties Boerma J, Sommerfelt AE. Demographic and health surveys (DHS: contributions and limitations. 1993. [PubMed]
- 9. Wellings K, Collumbien M, Slaymaker E, et al. Sexual behaviour in context: a global perspective. Lancet. 2006;368(9548):1706–1728. [DOI] [PubMed] [Google Scholar]
- 10. Yaya S, Bishwajit G, Danhoundo G, Shah V, Ekholuenetale M. Trends and determinants of HIV/AIDS knowledge among women in Bangladesh. BMC Public Health. 2016;16(1):812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Glick P, Randriamamonjy J, Sahn DE. Determinants of HIV knowledge and condom use among women in Madagascar: an analysis using matched household and community data. Afr Dev Rev. 2009;21(1):147–179. [Google Scholar]
- 12. Ochako R, Ulwodi D, Njagi P, Kimetu S, Onyango A. Trends and determinants of Comprehensive HIV and AIDS knowledge among urban young women in Kenya. AIDS Res Ther. 2011;8:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santos-Hövener C, Marcus U, Koschollek C, et al. Determinants of HIV, viral hepatitis and STI prevention needs among African migrants in Germany; a cross-sectional survey on knowledge, attitudes, behaviors and practices. BMC Public Health. 2015;15:753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Meel B. The myth of child rape as a cure for HIV/AIDS in Transkei. Med Sci Law. 2003;43(1):85–88. [DOI] [PubMed] [Google Scholar]
- 15. Nemutandani SM, Hendricks SJ, Mulaudzi FM. HIV/AIDS and TB knowledge and beliefs among rural traditional health practitioners in Limpopo Province, South Africa: TB, HIV/AIDS and other diseases. African Journal for Physical Health Education, Recreation and Dance. 2015;21(suppl 1):119–134. [Google Scholar]
- 16. Nyundu T, Smuts L. A different kind of AIDS: fOLK and lay theories in South African townships. Milton Park, England: Taylor & Francis; 2016. [Google Scholar]
- 17. Russell M, Cupp PK, Jewkes RK, et al. Intimate partner violence among adolescents in Cape Town, South Africa. Prev Sci. 2014;15(3):283–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zuma K, Shisana O, Rehle TM, et al. New insights into HIV epidemic in South Africa: key findings from the National HIV Prevalence, Incidence and Behaviour Survey, 2012. Afr J AIDS Res. 2016;15(1):67–75. [DOI] [PubMed] [Google Scholar]
- 19. Bauermeister JA, Elkington K, Brackis-Cott E, Dolezal C, Mellins CA. Sexual behavior and perceived peer norms: comparing perinatally HIV-infected and HIV-affected youth. J Youth Adolesc. 2009;38(8):1110–1122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nöstlinger C, Jonckheer T, De Belder E, et al. Families affected by HIV: parents’ and children’s characteristics and disclosure to the children. Aids Care. 2004;16(5):641–648. [DOI] [PubMed] [Google Scholar]
- 21. Shisana O, Rehle T, Simbayi L, et al. South African national HIV prevalence, incidence and behaviour survey, 2012. 2014. [DOI] [PubMed]
- 22. Rohleder P, Eide AH, Swartz L, Ranchod C, Schneider M, Schür C. Gender differences in HIV knowledge and unsafe sexual behaviours among disabled people in South Africa. Disabil Rehabil. 2012;34(7):605–610. [DOI] [PubMed] [Google Scholar]
- 23. UNICEF and Organization WH. Global AIDS response progress reporting 2013: construction of core indicators for monitoring 2011 political declaration on HI. 2013. [Google Scholar]
- 24. James S, Reddy S, Taylor M, Jinabhai CC. Young people, HIV/AIDS/STIs and sexuality in South Africa: the gap between awareness and behaviour. Acta Paediatr. 2004;93(2):264–269. [PubMed] [Google Scholar]
- 25. Statistics SA. Mid-Year Population Estimates 2016 In: Statistics South Africa, ed. Statistical release P0302. Pretoria, South Africa: Statistics South Africa; 2017. [Google Scholar]
- 26. Hunter-Adams J, Zerbe A, Philips T, et al. The dimensionality of disclosure of HIV status amongst post-partum women in Cape Town, South Africa. Afr J AIDS Res. 2017;16(2):101–107. [DOI] [PubMed] [Google Scholar]
- 27. Nattrass N. The social and symbolic power of AIDS denialism. Skeptical Inquirer. 2016. [Google Scholar]
- 28. Rubincam C. Peer educators’ responses to mistrust and confusion about HIV and AIDS science in Khayelitsha, South Africa. Cape Town, South Africa: University of Cape Town; 2014. [Google Scholar]
- 29. Sivelä J. Dangerous AIDS myths or preconceived perceptions? A critical study of the meaning and impact of myths about HIV/AIDS in South Africa. J S Afr Stud. 2016;42(6):1179–1191. [Google Scholar]
- 30. Wamai RG, Morris BJ, Bailey RC, Klausner JD, Boedicker MN. Debating male circumcision for HIV prevention: a one-sided argument does not represent a legitimate ‘controversy’analysis—Reply to de Camargo et al. Glob Public Health. 2015;10(5-6):672–678. [DOI] [PubMed] [Google Scholar]
- 31. Wamai RG, Morris BJ, Bailey RC, Klausner JD, Boedicker MN. Male circumcision for protection against HIV infection in sub-Saharan Africa: the evidence in favour justifies the implementation now in progress. Glob Public Health. 2015;10(5-6):639–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Parker R, Aggleton P, Rochel de Camargo K., Jr Circumcision and HIV prevention: Emerging debates in science, policies and programmes. Milton Park, England: Taylor & Francis; 2015. [DOI] [PubMed] [Google Scholar]
- 33. Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet. 2008;372(9639):669–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Oakley A, Fullerton D, Holland J, et al. Sexual health education interventions for young people: a methodological review. BMJ. 1995;310(6973):158–162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Minton HAM, Mittal M, Elder H, Carey MP. Relationship factors and condom use among women with a history of intimate partner violence. AIDS Behav. 2016;20(1):225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. MacPhail C, Campbell C. ‘I think condoms are good but, AAI, I hate those things’: condom use among adolescents and young people in a Southern African township. Soc Sci Med. 2001;52(11):1613–1627. [DOI] [PubMed] [Google Scholar]
- 37. Statistics SA. Quarterly labour force survey, quarter 1, 2017 In: Africa SS, ed. Statistical Release P0211. Pretoria, South Africa: Statistics South Africa; 2017. [Google Scholar]