Abstract
Objectives
The current study, using prospective data over 25 years (1991–2015), concurrently investigates patterns of body mass index (BMI) and affective symptom trajectories in middle-aged mothers and the socioeconomic antecedents and disease outcomes of these patterns.
Method
Growth mixture modeling was used to identify latent classes of conjoint health risk trajectories (BMI, depressive symptoms, and anxiety symptoms) from 1991 to 2001. For each latent class, we identified mean trajectories of each health risk. Then, analyses were conducted identifying how these conjoint health risk classes were associated with respondents’ socioeconomic background profiles in 1991 and subsequent chronic health problems in 2015.
Results
Socioeconomic background profiles were significantly associated with initially high-risk trajectories. There was a statistically significant association between membership in certain classes of conjoint trajectories and physical health outcomes in later years. Consistent patterns of association with changes in different health outcomes including onset of diseases were observed when classes of conjoint risk trajectories are examined.
Discussion
The identification of members of various conjoint risk trajectory groups provides a potentially useful prognostic tool for early preventive intervention efforts, treatment, and policy formation. Such interventions should promote and develop resiliency factors, thereby aiding in the redirection of middle-aged women’s adverse risk trajectories.
Keywords: Comorbidity, Mental health, Middle years, Physical health
Middle-aged men and women are exposed to multiple risk factors for chronic diseases. Consistently high body mass index (BMI) trajectories are associated with numerous diseases including asthma, arthritis, hypertension, diabetes, heart disease, chronic bronchitis or emphysema, and reduced self-rated overall health during the middle years (Wang et al., 2016) as well as with increased hospital visits and hospitalization (Elrashidi et al., 2016; Steppuhn, Langen, Keil, & Scheidt-Nave, 2014). Additionally, research has shown that consistently high and increasing depressive and anxiety symptom trajectories predict the onset of metabolic and cardiovascular diseases in adult and later years (Rugulies, 2002; Wickrama, Kwag, Lorenz, Conger, & Surjadi, 2010; Wickrama, O’Neal, & Lorenz, 2017) as well as disability and premature mortality in later years (Murphy et al., 2016). More importantly, research suggests that the co-occurrence of weight problems and elevated affective symptoms, which show increasing average trajectories during the middle years (Clarke, O’Malley, Johnston, & Schulenberg, 2009), is a major risk factor for disease (Faulconbridge, Wadden, Berkowitz, Pulcini, & Treadwell, 2011; Ladwig, Marten-Mittag, Löwel, Döring, & Koenig, 2003; Ladwig, Marten-Mittag, Löwel, Döring, & Wichmann, 2006). Furthermore, some research shows that the association between mental health and weight problems becomes stronger over the adult life course (Kivimäki et al., 2009).
Cumulative disadvantage theory contends that early social and economic disadvantages influence long-term outcomes through the accumulation and compounding of disadvantages or risk factors over the life course, thereby increasing health disparity in later life (Dannefer, 2003; O’Rand, 1996). Life course theory also proposes several processes related to the cumulative influence of early disadvantage (Elder, 1998). Applying cumulative disadvantage theory together with tenants from life course theory for early-adult socioeconomic disadvantage (the current study focuses on disadvantages in early midlife) and later-life health outcomes (postmidlife), we posit that health disparity resulting from early socioeconomic disadvantages may operate through several risk mechanisms. We examine independent health risks operating through these mechanisms, as well as dynamic interactions among them.
First, variations in early socioeconomic disadvantage may launch health risk trajectories with differing initial levels (severity) as a result of varying psychophysiological responses. These risk trajectories (e.g., BMI, depressive and anxiety symptoms) with different initial severity levels may exert independent influences on health outcomes in later years. Second, if these health risks are associated with each other and co-occur (i.e., comorbidity or rank order comorbidity), they may produce a synergistic health effect (a level-level interaction) in addition to their unique health effects. Third, health risks may compound over time and produce parallel escalating trajectories (i.e., comorbidity in the longitudinal context or temporal comorbidity) (Mumford, Liu, Hair, & Yu, 2013). This longitudinal codevelopment among risks may produce a powerful synergistic health effect over the life course (a change-change interaction). We argue that these qualitatively different health processes can be examined by investigating patterns of conjoint health risk trajectories, as differences in these patterns may reflect differences in previously discussed health processes. We expect that these processes—which are influenced by early socioeconomic disadvantage—would cumulatively contribute to an array of chronic physical health problems in later years.
To date, relatively little is known about the patterning of co-occurring, or conjoint, trajectories of BMI and affective symptoms in middle years and their health consequences and socioeconomic antecedents. Consistent with the notion of “timing and sequence of events” in life course perspective (Elder & Giele, 2009), previous studies suggest that midlife is a sensitive developmental period that is dense in life events (or nonevents) and circumstances related to multiple roles involving work (e.g., promotions or lack thereof), aging parents (parental care), children (educations and occupational attainment/failures), and marriage (marital disruptions, divorce). These events may accelerate the compounding of health risks and contribute to adverse risk trajectories over time. Further, the incidence of chronic disease and physical impairment increases notably during the middle years (Lorenz, Wickrama, Conger, & Elder, 2006; Martikainen, Stansfeld, Hemingway, & Marmot, 1999; Ryff, Singer, & Palmersheim, 2004; Siegler, 1997). Thus, midlife is an influential period in the life course for health outcomes in later years. It is therefore important to investigate and understand the cumulative health risk associated with premidlife socioeconomic disadvantage.
The investigation of health outcomes for rural middle-aged mothers is particularly important for several reasons. First, rural middle-aged mothers may be more vulnerable to midlife events because, in general, parental and marital roles are very salient to their personal identity (Wickrama, Conger, Lorenz, & Matthews, 1995). Second, middle-aged women experience changes in bodily (e.g., hormonal) systems, which have consequences for emotional health (Dennerstein & Soares, 2008) and BMI trajectories in the middle years (Clarke et al., 2009). Thus, it is important to study rural mothers as a subpopulation to understand their unique health processes over the middle years.
Using prospective data collected from middle-aged women over a period of 25 years (1991–2015) who were parents of early adolescents in 1991, this study examines concurrent trajectories of BMI, depressive symptoms and anxiety symptoms (affective symptoms) over their middle years (42–52 years on average). The socioeconomic antecedents of these trajectories during pre- and early middle years (40 years or less) are also examined as well as their physical health outcomes in late-middle and older years (65 years on average).
Co-occurrence of BMI and Affective Symptoms Trajectories
Previous studies have found clusters of individuals that show a co-occurrence, or comorbidity, of weight problems and mental health problems (Kivimäki et al., 2009; Ladwig et al., 2003). These studies suggest several psychological, behavioral, and biological mechanisms for this concurrent association. For instance, mental health problems can increase individuals’ risk of weight problems (Kivimäki et al., 2009), and behavioral mechanisms may be responsible for this directional association (e.g., excessive eating and lack of exercise). However, people with a high BMI are also at an increased risk of depression and anxiety (Farmer et al., 2008; Roberts, Deleger, Strawbridge, & Kaplan, 2003), and psychological mechanisms have primarily been identified as culprits for this directional association (e.g., obesity gets stigmatized and leads to increased levels of depressive and anxiety symptoms). Still other studies have revealed a bidirectional relationship between high BMI and mental health problems (Atlantis & Baker, 2008). This association is likely attributed to biological mechanisms (e.g., secretion of hormones through increased hypothalamic and neuropeptide levels, and regulation of neurological reward systems; Maxwell & Cole, 2009). Furthermore, some researchers contend that the bidirectional association between weight problems and affective symptoms is at least partly due to a cognitive process involving body image, body dissatisfaction, and feelings of self-worthlessness (Rawana, Morgan, Nguyen, & Craig, 2010). We expect that these multiple mechanisms operate in middle-aged mothers over an extended period of time creating a bidirectional relationship between BMI and affective symptoms trajectories.
Heterogeneity in Risk Trajectories
Social and developmental perspectives, as well as empirical research, suggest that individual trajectories for socioeconomic and health attributes may not follow the same pattern of growth/decline; rather, such trajectories are inherently heterogeneous over the life course (House, Lantz, & Herd, 2005). That is, individuals are stratified, or clustered, in terms of both socioeconomic and health attributes (unobserved heterogeneity) due to underlying social processes. In separate studies, past empirical research has identified heterogeneous groups of BMI trajectories (Kivimäki et al., 2009) and heterogeneous groups of depressive symptom trajectories (Wickrama, Wickrama, & Lott, 2009; Wickrama & Wickrama, 2010). Because the development of BMI and affective symptoms trajectories are expected to be concurrent, or parallel, we expect a simultaneous examination of BMI and affective symptoms trajectories to identify heterogeneous groups with unique patterns. We predict that a person-centered investigation of these conjoint trajectories over a long period of time will reveal these heterogeneous patterns, including different risk trajectory patterns such as comorbid levels of affective symptoms and BMI (i.e., rank-order comorbidity) and parallel changes in BMI and affective symptoms over time (i.e., temporal comorbidity).
Synergistic Health Risk of BMI and Affective Symptoms Trajectories
Research suggests that BMI reflects the degree of inflammation and dysregulation in neuroendocrine systems with high BMI ultimately leading to the onset of metabolic and cardiovascular diseases for many individuals (Dyer, Stamler, Garside, & Greenland, 2004; Glei, Goldman, Chuang, & Weinstein, 2007; Wang & Nakayama, 2010). Also, research has shown that elevated levels of affective symptoms, particularly depressive symptoms, influence the onset of chronic diseases such as cardiovascular diseases. This association is mediated by physiological responses within the body, including inflammation, dysfunction within the neuroendocrine and autonomic nervous systems, and platelet activity in addition to health risk behaviors (Huffman, Celano, Beach, Motiwala, & Januzzi, 2013).
Recent research suggests that, along with their independent health risks, high BMI and mental health problems combine to influence chronic physical health problems (Ladwig et al., 2006). That is, the health risk of obesity may not be equally distributed among individuals with varying levels of depressive symptoms because there is a synergistic health effect between obesity and depression (equivalently, health risk of depression may not be equally distributed among obese individuals) (Roberts et al., 2003). This may result in differential disease risks associated with heterogeneous patterns (groups) of concurrent BMI and affective symptoms trajectories.
Applying stress process theory (Pearlin, Schieman, Fazio, & Meersman, 2005) within a life course perspective, we expect that stressful life experiences (e.g., family economic problems) experienced by mothers in their early middle years may initiate previously discussed biological and cognitive mechanisms that result in elevated and/or parallel trajectories of BMI and affective symptoms over the middle years. Indeed, consistent with the “historical timing” concept from the life course perspective (Elder, 1998), mid-western women in the present study belong to the baby-boom cohort and, as a result, have faced chronic family economic problems and stressful events stemming from the “farm crisis” of the 1980s. This includes chronically low prices of agricultural products, unemployment, low income, indebtedness, as well as displacement from their communities (Lorenz, Elder, Bao, Wickrama, & Conger, 2000) in their early middle years.
Socioeconomic Antecedents: Income, Assets, and Family Economic Problems
The health impacts of low income, economic problems and difficulty making ends meet are well documented for chronic diseases and physical impairment (Ahnquist, Fredlund, & Wamala, 2007; Lorenz et al., 2000; McDonough & Berglund, 2003; Wickrama et al., 2010). As argued previously, we expect that this association is at least partially explained by the patterning of BMI and affective symptom trajectories. These health risk trajectories have been shown to be shaped by stressful events (Dugravot et al., 2010; Mumford et al., 2013). However, most previous studies have conceptualized and analyzed health risks and outcomes in static terms rather than as a progression over time (McDonough & Berglund, 2003). Little is known about the influence of stressful socioeconomic circumstances in the early middle years on the progression of multiple health risks over the middle years leading to chronic health problems in later age.
Thus, hypotheses of the current study include:
(a) Heterogeneity exists in conjoint trajectories of BMI, depressive, and anxiety symptoms over the middle years.
(b) Health is socially stratified; that is, socioeconomic stress profiles are associated with conjoint trajectory classes of BMI and affective symptoms.
(c) These risk classes are associated with multiple health outcomes in the later years.
Method
Participants and Procedures
The data used to evaluate these hypotheses are from the Family Transition Project (FTP), the Midlife Transitions Project (MTP) and the Later Adulthood Study (LAS). Together, these projects are a 27-year panel study of rural families from a cluster of eight counties in north-central Iowa that closely mirror the economic diversity of the rural Midwest. The FTP represents an extension of two earlier studies: The Iowa Youth and Family Project (IYFP) (Conger & Elder, 1994) and the Iowa Single Parent Project (ISPP) (Simons, 1996). The IYFP began in 1989 as a study of rural couples with children, at least one of whom was a seventh grader in 1989. The ISPP was integrated into the IYFP 2 years later by adding 102 recently divorced mothers with children, at least one of whom was a ninth grader in 1991. The total sample in 1991 was 522 families. Families meeting the selection criteria were enumerated through contacts with public and private schools and then randomly selected and recruited into the study, with 78% of the married couples and 99% of the single mothers agreeing to participate (Conger & Elder, 1994; Simons, 1996). Parents from the FTP participated in the MTP in 2001 and LAS in 2015. The 349 mothers in the current study are those who participated in 1991, 1992, 1994, 2001, and 2015 data collections (71% of the 522).
In 1991, respondent mothers were in their early middle years; their average age was 40 years with a range from 31 to 55 years. The median age of their youngest child was 12. In 1989, the average number of years of education was 13.54 years. Because there are very few minorities in the rural area studied, all participating families were White.
Measures
Socioeconomic antecedents
Gross family income
Because the original research focused on the farm crisis, respondents were asked to report detailed information about their income and assets in 1991 (Conger & Elder, 1994). Incomes from wages, self-employment including farming, dividends, rents and other sources (both husband and wives) were summed to create a measure of gross family income in 1991.
Total family assets
Respondents’ reports of values of all family assets including farm assets, houses, vehicles, equipment, equities, savings, retirement accounts, and other reported assets were summed to create a measure of the total family assets in 1991.
Family economic problems
The list of economic problems was adapted from Dohrenwend, Krasnoff, Askenasy, & Dohrenwend (1978) to capture families’ economic circumstances in 1991. Mothers’ “yes” responses to each of the 27 items were summed to indicate the number of economic problems experienced by the family during the previous year (1 = yes, 0 = no). The list of economic problems included items such as “borrowed money to help pay bills,” “sold possessions or cashed in life insurance,” and “changed food shopping or eating habits to save money.”
Making ends meet
Mothers indicated how constrained they felt by current economic conditions (1 = strongly disagree, 5 = strongly agree). Respondents were prompted with items such as “Our income never seems to catch up with our expenses.” They were also asked to describe whether they had “no difficulty at all” (1) to “a great deal of difficulty” (5) in paying bill over the past year and at the end of each month if they had “more than enough money left over” (1) to “not enough to make ends meet” (4). The internal consistency of this measure was .82.
Divorced/separated
Respondents’ reports about their marital status in 1991 were used to create a dichotomous variable distinguishing mothers who were divorced/separated (1) from those who were married (2).
Educational level
Respondents’ years of education in 1991 was used to assess their education level.
Health risks
Depressive symptoms
Nine items from the Symptom Checklist (SCL-90-R) (Derogatis & Melisaratos, 1983) were used to capture self-reported ratings of depressive symptoms from the previous week for women during the years of 1991, 1994, and 2001. Sample items include, “thoughts of ending your life,” “feelings of worthlessness,” and “feeling hopeless about the future.” These items were scored on a 5-point Likert scale from 1 = not at all to 5 = extremely. A mean score was computed with higher scores indicating more depressive symptoms. The internal consistencies were more than .90 for 1991, 1994, and 2001.
Anxiety symptoms
In 1991, 1994, and 2001, women indicated how much discomfort they experienced from ten anxiety symptoms in the preceding week using the SCL-90-R (Derogatis & Melisaratos, 1983). Responses were given on a 5-point Likert scale from 1 = not at all to 5 = extremely. Sample items include, “nervousness or shakiness inside,” “feeling tense or keyed up,” and “feeling fearful.” For each time point, a mean score was computed with higher values indicating more anxiety symptoms. The internal consistencies were more than .80 for 1991, 1994, and 2001.
BMI
Respondents reported their height and weight in 1991, 1994, and 2001. From these responses, their BMI values, the ratio of weight to height squared ([lbs*703]/inches2), were calculated and used to assess their degree of being overweight.
Physical health outcomes
Poor global health
Self-assessment of poor global health was obtained in 2015 using two items. The first question asked participants to indicate the following on a scale from 1 = excellent to 5 = poor: “How would you rate your overall physical health?” The second item asked participants to indicate the following on a scale from 1 = much better to 5 = much worse: “Compared to 1 year ago, how would you rate your physical health in general now?” We computed the mean of these two items, with higher scores representing poorer physical health. A similar illness measure from 1991 was used to capture the change in poor global health from 1991 to 2015.
Physical diseases
In 2015, respondents indicated if they had suffered from any symptoms or diseases (diagnosed by a physician) in the previous two years using a list of 48 physical health ailments. Sample items include: “diabetes,” “cancer,” “arthritis,” “stroke,” “high cholesterol,” “high blood pressure,” and “peptic ulcer.” Items were coded as 1 = yes and 0 = no. A sum score was computed representing the total number of symptoms or diseases the individual experienced from the 48 listed conditions (Lorenz et al., 2006). Respondents reporting 8 or more illnesses were assigned a value of 8 to reduce the skewness of this variable (16 and 17 respondents reported more than eight diseases in 2001 and 2015, respectively). A similar illness measure from 2001 was used to capture the change in disease count from 2001 to 2015.
CVD counts after 2001
In 2015, respondents reported timing (year) of cardiovascular disease (CVD) onset (including high blood pressure, irregular heartbeats, chest pain, hardening of the arteries, blood clot in the lung, blood clot in the vessels, heart failure, stroke, and heart attack). We summed the number of these CVDs with an onset after 2001.
Physical impairment
In 2015, the degree of physical impairment was measured by the 10-item physical impairment scale of the Rand Health Science Program in Health Survey 1.0 (1986). Respondents were asked to indicate their physical impairment on a 3-point scale ranging from 1 = no, not limited at all to 3 = yes, limited a lot. The scale captures impairment for vigorous (e.g., running or lifting heavy objects) and moderate activities (e.g., moving a table, pushing a vacuum cleaner, lifting or carrying groceries). Responses were averaged to create a measure of overall physical impairment. Cronbach’s α for physical impairment was .89. A similar physical impairment measure from 2001 was used calculate the change in physical impairment from 2001 to 2015.
Bodily pain
In 2015, the degree of bodily pain was assessed by 2 items from the Rand Health Science Program in Health Survey 1.0 (1986). On a 6-point scale ranging from 1 = none to 6 = very severe, respondents indicated how much bodily pain they experienced in the four preceding weeks. Also, on a 5-point scale ranging from 1 = not at all to 5 = extremely, respondents indicated “How much did pain interfere with your normal work (including both work outside the home and housework)?” Responses were standardized and averaged to create a measure of bodily pain. The correlation between the two items was .74. A similar bodily pain measure from 2001 was used calculate the change in bodily pain from 2001 to 2015.
Statistical Analyses
Using Mplus software (version 7.4; Muthén & Muthén, 1998–2015), we first examined the change in BMI, depressive symptoms, and anxiety symptoms in middle-aged women by estimating latent growth curves (LGCs) over 10 years (from 1991 to 2001) with initial levels and slopes as latent constructs. Models estimating linear trajectories provided a better fit with the data than quadratic trajectories.
Growth mixture modeling (GMM; Muthén, Khoo, Francis, & Boscardin, 2003; Wickrama, Lee, O’Neal, & Lorenz, 2016) was used to identify latent classes (LC) of conjoint health risk trajectories. In this modeling approach, first, univariate growth curves for BMI, depressive and affective symptoms are estimated with a correlated initial level and slope in each growth curve but uncorrelated growth parameters across different growth curves. Growth factors of the three growth curves (levels and slopes) are used as indicators of latent classes that reflect different patterns of concurrent trajectories. This classification approach for trajectory classes is a data-driven, person-centered method (Wickrama et al., 2013).
The trajectory class of individuals is inferred from the data based on class membership probabilities (posterior probability) of each individual (Muthén et al., 2003). Each individual is assigned to the class with the highest posterior probability. Posterior probability is the probability of an individual who has a specific pattern of growth factors belonging to a certain class. In a single-trajectory growth mixture modeling (e.g., linear BMI trajectory) these indicators are the initial level and slope of the specific attribute (examples of possible patterns include low-level with increasing-change and high-level with decreasing-change, and so on). Individual posterior probabilities are not affected by matrices of observed indicators, but by their observed qualitative patterns.
When estimating conjoint trajectories (e.g., BMI, depressive and anxiety symptom trajectories), the individual growth patterns are determined by the patterning of both of the growth factors (level and slope) for all three constructs; that is, the patterning of the initial levels and slopes for trajectories of BMI, depressive symptoms and anxiety symptoms. Because, in the current study, there are six growth parameters of three linear trajectories, there can be numerous patterns among them. Akaike Information Criterion (AIC) statistics and entropy values are used assess the model fit (Jackson, Sher, & Schulenberg, 2005; Olino, Klein, Lewinsohn, Rodhe, & Seeley, 2010; Wickrama, Mancini, Kwag, & Kwon, 2013). This approach gives consideration to the patterning of growth parameters for multiple health risks (severity levels, and deteriorations or recovery) simultaneously when identifying LCs. Because these conjoint LCs capture comorbidity between BMI and affective symptoms in a longitudinal context, these LCs may more accurately reflect the cumulative disadvantage of early socioeconomic disadvantage (e.g., family economic problems) and subsequent health problems compared to LCs of a specific health risk.
In order to examine the associations between early socioeconomic disadvantage and conjoint health risk classes, we compared profiles detailing variations in relevant background characteristics and subsequent chronic health problems (i.e., disease, physical impairment and pain) using multivariate analysis of variance in SPSS software. We used univariate and multivariate F tests to examine mean differences across latent classes. We also identified mean trajectories of each health risk (BMI, depressive symptoms, and anxiety symptoms) within each latent class.
We analyzed differences in socioeconomic antecedents and health outcomes using both MANOVA and a three-step approach with the “Auxiliary” command in Mplus. The results are essentially the same except for small differences in p values. This may be attributed to the highly stable classification of LCs as reflected by entropy statistics (more than .90) (Asparouhov & Muthén, 2014). Because the Mplus analysis with the “Auxiliary” command provides only the univariate statistics (reporting differences for each outcome separately), we present the MANOVA results with univariate and multivariate statistics.
Results
Analyses for each univariate growth curve and mixture models for each health risk trajectory (i.e., BMI, depressive symptoms, and anxiety symptoms) were estimated separately. All three health risks were fit with linear growth trajectories with three measurement occasions over a 10-year period from 1991 to 2001 (Table 1).
Table 1.
Risk-Specific Univariate Growth Curve Results
| Initial level | Slope | χ2 | CFI | TLI | |||
|---|---|---|---|---|---|---|---|
| Mean | Variance | Mean | Variance | ||||
| Depressive symptoms | 1.50* | 0.22* | 0.00 | 0.03* | 18.91 (1) | 0.93 | 0.80 |
| Anxiety symptoms | 1.26* | 0.11* | 0.00 | 0.01* | 4.71 (1) | 0.99 | 0.96 |
| Body mass index | 26.35* | 30.22* | 0.71* | 0.13* | 1.32 (1) | 1.00 | 0.99 |
Note: N = 349; CFI = comparative fit index, TLI = Tucker-Lewis index; *p < .05, two-tailed test.
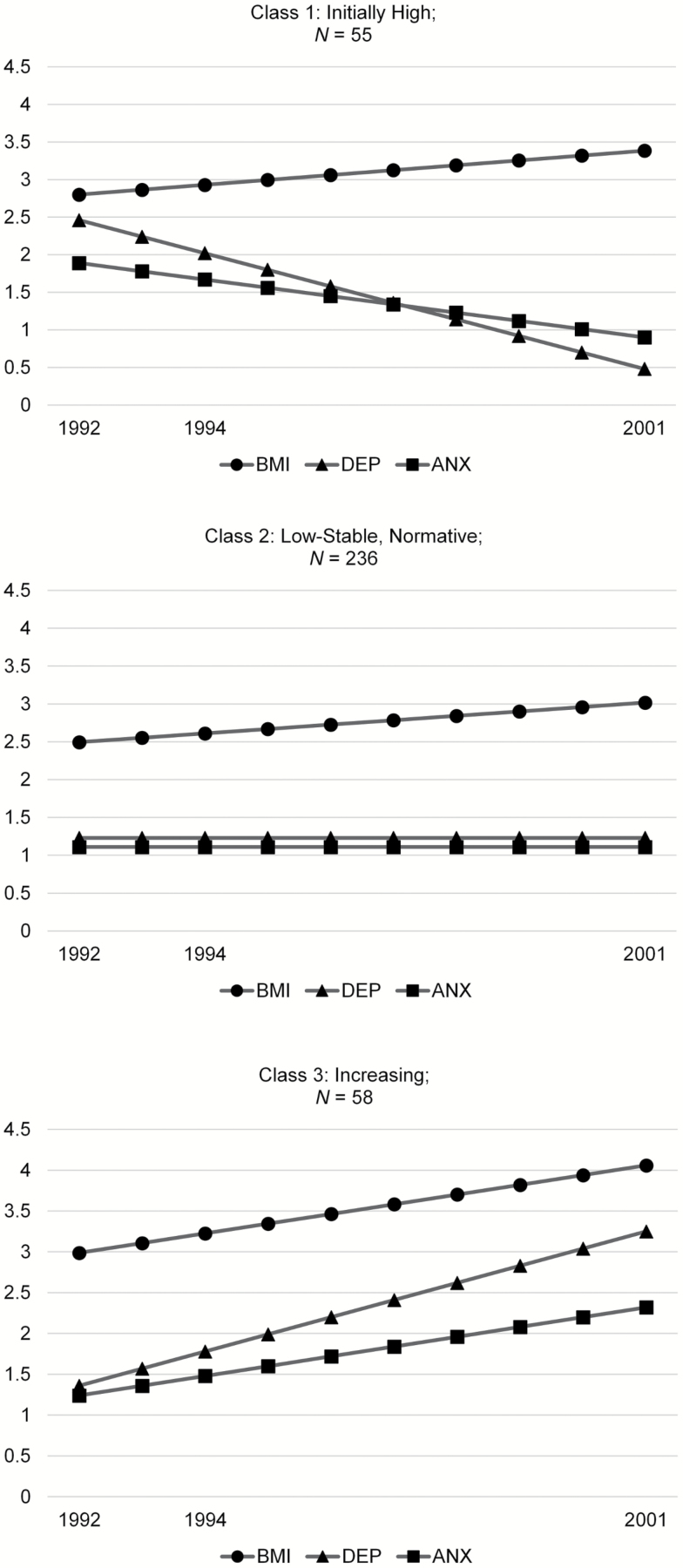
GMM was utilized to develop an acceptable model with three latent classes for the conjoint health risks trajectories (Table 2). In this model, Class 1 (N = 55) was generally comprised of women with the highest mean initial levels for all three symptoms along with a moderately increasing BMI and decreasing depressive and anxiety symptoms (initially high class), Class 2 (N = 236) was a group with relatively low and stable responses across all three symptoms (low and stable class, hereafter referred as the normative class), and members of Class 3 (N = 58) had moderately high initial levels for all three symptoms and these symptoms generally increased in adulthood (increasing class) (Figure 1). That is, this class had both higher average initial levels and rate of changes in all three risk trajectories compared to the normative Class 2.
Table 2.
Model Fit Statistics for Alternative Models with 2, 3, and 4 Latent Classes
| Conjoint trajectories model | |||
|---|---|---|---|
| 2 | 3 | 4 | |
| AIC | 5,852 | 5,704 | - |
| Entropy | 0.91 | 0.90 | |
| Class 1 N (%) | 46 (13) | 55 (16) | |
| Class 2 N (%) | 303 (87) | 236 (68) | |
| Class 3 N (%) | 58 (17) | ||
| Class 4 N (%) | |||
Note: AIC = Akaike Information Criterion; Model with 4 latent classes did not converge.
Figure 1.
Risk factor trajectories for conjoint latent classes. ANX = Anxiety symptoms; DEP = Depressive symptoms. BMI values shown are divided by 10.
Evaluating Socioeconomic Antecedents (1991 or before)
Panel A in Table 3 shows the socioeconomic antecedent profiles for each of the three conjoint trajectory classes. Compared to women in the normative class (Class 2; low and stable), those in Class 1 (initially high) reported significantly higher mean levels of family economic problems and difficulty making ends meet. On average, they also reported the fewer assets and less family income in 1991 compared to Class 2. Similarly, the increasing class (Class 3) also reported more difficulty making ends meet compared to Class 2 (low and stable). Class differences in other socioeconomic antecedents were not statistically significant. These results suggest that socioeconomic disadvantage and associated stressful socioeconomic experiences in the early and premidlife play a role in “sorting” respondents into different health risk trajectory classes.
Table 3.
Socioeconomic Antecedent and Physical Health Profiles
| Panel A. Socioeconomic Antecedent Profiles (1991 or before), reference group is Class 2 (normative group with low and stable values) | ||||
|---|---|---|---|---|
| Class 1 | Class 3 | |||
| Initially High | Increasing | Univariate F | ||
| Gross Family Income (1991 in $1000s) | −2.82** | −2.01 | 2.44* | |
| Family Assets (1991 in $1000s) | −71.00** | −27.00 | 2.41* | |
| Family Economic Problems | 3.01* | 2.23 | 6.18** | |
| Making Ends Meet | 0.46* | 0.15* | 4.70* | |
| Divorce/Separated (1991) | 0.07 | 0.04 | 1.90 | |
| Education (1991) | 0.12 | −0.15 | 2.00 | |
| Multivariate F (12, 360) = 7.38** | ||||
| Panel B. Physical Health Profiles in 2015, reference group is Class 2 (normative group with low and stable values) | ||||
|---|---|---|---|---|
| Class 1 | Class 3 | |||
| Initially high | Increasing | Univariate F | ||
| Global Poor Health 2015 | 0.23* | 0.64* | 17.68** | |
| Disease Count 2015 | 2.50* | 1.87* | 12.23** | |
| CVD Onsets since 2001 | 0.05 | 0.07** | 2.00* | |
| Physical Impairment 2015 | 0.20* | 0.46* | 17.30** | |
| Bodily Pain 2015 | 0.05* | 0.26* | 9.87** | |
| Multivariate F (10, 360) = 5.80** | ||||
| Panel C. Change in Health for Each Class | ||||
|---|---|---|---|---|
| Class 1 | Class 2 | Class 3 | ||
| Initially high | Low and stable | Increasing | Univariate F | |
| Change in Disease Count (1991–2015) | 0.29* | 0.76^ | 2.19 | 6.09** |
| Change in Disease Count (2001–2015) | 1.36++ | 0.87^^ | 1.42 | 2.10* |
| Change in Global Poor Health | 0.11* | 0.22^ | 0.40 | 2.40 |
| Change in Bodily Pain | 0.03 | 0.00 | 0.01 | 0.90 |
| Change in physical impairment (2001–2015) | 0.77 | 0.55^^ | 1.48 | 3.40* |
| Multivariate F (12, 360) = 3.40* | ||||
Note: N = 349; class comparison p < .05 if +1 vs 2, *1 vs 3, ^2 vs 3; p < .01 if ++1 vs 2, ** 1 vs 3, ^^2 vs 3; for F tests, *p < .05, **p < .01; two-tailed tests presented.
Evaluating Physical Health Profiles in Later Adulthood (2015)
Panel B in Table 3 presents the latent class mean levels of health problems in 2015. The low and stable normative class (Class 2) generally reported significantly better health later in life, as assessed by all five health outcomes, compared to the increasing class (Class 3). That is, the average member of the low and stable class had better global health, fewer diseases, less onset of CVD since 2001, less reported physical impairment and less reported pain in 2015 when compared to members of the increasing class (Class 3).
The high initial level class (Class 1) also experienced significantly poorer health outcomes compared to those of normative class (Class 2). More specifically, compared to the normative Class 2, Class 1 generally reported significantly poorer health later in life, as assessed by several health outcomes. The average member of Class 1 reported poorer global health, a higher number of diseases, more physical impairment and more bodily pain in 2015 when compared to members of the normative class (Class 1). Despite the decline in affective symptoms, high severity levels of BMI and affective symptoms appear to exert a persistent influence on health outcomes in later years. With regard to the difference between Class 1 and Class 3, on average, members of Class 1 also reported better global health in 2015 compared to the increasing class (Class 3) (results not shown).
Evaluating Changes in Physical Health in Later Adulthood (1991–2015)
Panel C in Table 3 presents results for change in reports of poor global health, disease counts, bodily pain and physical impairment from 2001 to 2105 and from 1991 to 2015 (only for disease counts). Members of the normative low and stable class (Class 2) averaged a smaller increase in disease count and poor global health from 2001 to 2015 compared to the increasing class (Class 3). Compared to Class 3, Class 1 (initially high) also had a lower mean increase in disease count and their report of poor global health between 2001 and 2015. However, Class 1 (initially high) had a higher mean increase in disease counts and reported poor global health despite declines in affective symptoms compared to the normative class (Class 2). It seems that initial stressful socioeconomic experiences had persistent influences on their health outcomes that were not erased by improving affective symptoms.
Members of the increasing class (Class 3) had a steeper average increase in both reported poor global health and number of diseases from 2001 to 2015 compared to both the low and stable and initially high classes. It seems that both the levels and changes in risk trajectories cumulatively contributed to adverse health outcomes in later years. To provide a descriptive illustration, the average member of the increasing class (Class 3) reported approximately two more illnesses in 2015 than she reported in 1991, compared to a mean increase of less than one disease for both of the other classes. Because the increasing class (Class 3) did not start out with as many physical complaints or mental health risk indicators in 1991, these results suggest that they were catching up with others over time—as if their observed resilience for health risk behaviors in mid-life was only temporary. Thus, they are a particularly interesting group for more intensive study because they are a group that is mostly likely to be overlooked at midlife because their risk level appears lower during midlife.
Discussion
Research shows that both BMI and affective symptoms generally increase during the middle years, particularly for women, putting them at higher risk for chronic health problems (Clarke et al., 2009; Harris, Perreira, & Lee, 2009). Yet, previous research has rarely explored the different types of comorbidities and corresponding processes with synergistic health effects of BMI and affective symptoms over time. Thus, the present study investigated the patterning of conjoint trajectories of BMI and affective symptoms in middle-aged women, which may correspond to these different health processes. The present study also identified the physical health consequences of these trajectories and their socioeconomic antecedents. With a data set spanning 25 years, the current study followed women over an extended period of time from their early middle years to later years. This extended period of time was necessary for an examination of the potential compounding health risk and the materialization of health outcomes. Further, the extended follow-up period allowed for conducting analyses with the correct temporal ordering of constructs when estimating conjoint trajectories (10 years follow-up) and subsequent chronic health problems (after 15 years). The results of a mixture analysis distinguished patterning, or heterogeneous classes, of these conjoint risk trajectories showed there were statistically significant associations between membership in certain conjoint trajectories classes and physical health outcomes in later life. These results provide evidence for independent as well as synergistic health effects stemming from the co-occurrence of multiple health risks.
The results revealed three prominent classes with different patterns of risk trajectories. The largest class (Class 2), labeled the normative class, was characterized by the lowest initial levels and lowest increases (chronically low) of BMI and affective symptoms over the middle years. Members of this class also exhibited the lowest mean scores for socioeconomic disadvantage in 1991. As evidenced by the least physical health problems in later years, this class, on average, reported fewer physical health problems in their later years compared to the other two classes.
Members of the increasing class (Class 3) averaged moderately high initial levels and in BMI and affective symptoms trajectories compared to the normative class. They also averaged the steepest increases in BMI and affective symptoms over time. This appears to be the highest health risk class, as members of this class reported the most adverse physical health outcomes in later years. As previously discussed, this cumulative health disadvantage over the middle years may be attributed to several processes. First, this class had moderately high initial levels of BMI and affective symptoms compared to normative group, which could have exerted a persistent influence on health outcomes in later years independent of the influence of longitudinal trajectories. The health effect of the initial levels of risk (severity) may be attributed to early physiological damage that manifested later in life. Early physiological damage may become stronger over time (i.e., an interaction with time) producing adverse health outcomes in later years. Second, increases in BMI and affective symptoms during the middle years may have contributed to health outcomes in later years, independent of the initial levels. That is, the steep incline in risk trajectories for this class may be associated with poorer health outcomes independent of the influence of initial moderate risk levels. Third, in addition to the additive influences of initial levels and changes, rank-order comorbidity and temporal comorbidity may have produced synergistic health influences (corresponding to level-level and change-change interactions). In summary, it appears that different growth parameters of various risks (the initial levels and change) additively and multiplicatively influenced the subsequent health outcomes of these women.
The temporal comorbidity, or the comorbidity of health risks, appears to be more powerful in the longitudinal trajectory context (i.e., parallel increases in BMI and affective symptoms for Class 3, increasing) than in the cross-sectional context (i.e., high initial BMI and affective symptoms for Class 1, initially high). This suggests that the change-change synergistic influence becomes more powerful over time; such that, people with increasing health risk trajectories are at particularly high risk for chronic health problems. Bio-behavioral studies suggest this synergistic effect may be attributed to increases in BMI and affective symptoms acting jointly on the immune system and amplifying markers of chronic inflammation, which has the effect of increasing disease risk (Ladwig et al., 2006). Furthermore, research suggests that a similar neuro-endocrine response to obesity and depression may also be attributed to this synergistic effect (Rosmond, Lapidus, Mårin, & Björntorp, 1996).
Class 1 (initially high) also reported more adverse health outcomes compared to the normative class (Class 2). Class 1 had the highest initial levels of affective symptoms out of all three classes and a moderately high initial level of BMI, as well as the highest mean value for socioeconomic adversity in 1991. Although the increase in BMI was higher for this class than the normative class, the average BMI increase for this class was lower than that experienced by the increasing class (Class 3). However, affective symptoms in this class decreased over the middle years, showing an absence of temporal comorbidity among risks. Despite decreases in affective symptoms, extremely high initial levels of affective symptoms in this class may have contributed to distal and persistent influences on health outcomes in later years, which emphasizes the unique influence of early risks largely through physiological damages incurred at the time of the stressor. This influence may include independent effects of each risk in addition to a synergistic influence from multiple high initial levels of risks. Due to the absence of temporal comorbidity within this class, the synergistic influence of different risks appears to decrease with age as indicated by a lower average increase in diseases compared to Class 3. Consistent with the life course notion of “turning points” a positive midlife event/circumstances (e.g., economic recovery), which is strongly related to mental health, could be responsible for the decline in affective symptoms trajectories, but not BMI trajectories. It is important to further investigate potential events and circumstances influencing the decline in affective symptoms for this class.
The results suggest that the patterning of conjoint trajectories was highly heterogeneous and produced qualitatively different health processes in some instances. It appears that trajectories across classes significantly differed in terms of initial levels and change. There was a lack of rank-order comorbidity in one class (Class 3) and a lack of temporal comorbidity in another (Class 1). These findings emphasize the importance of assessing the comorbidity of different health risks in a broader longitudinal context when studying their health consequences, particularly for disease onset. Further investigation focusing on the varying synergistic influences of different comorbidities of risks trajectories is needed. Particularly, longitudinal studies with longer follow-up spans should further investigate the variation in this synergistic influence over the elderly years (Kivimäki et al., 2009).
Several factors potentially limit the scope and generalizability of the results. First, the sample was comprised only of European-American, middle-aged rural women who were mothers living in rural Mid-west. As previously noted, it is important to investigate this subpopulation of middle-aged women because they possess unique characteristics which may increase their susceptibility for poor health outcomes in later years. Moreover, this cohort of rural women experienced a severe economic downturn in the form of the rural farm crisis in late 1980s. Thus, although findings enhance our understanding of health stratification processes for this subpopulation, caution should be taken when generalizing these results. Studies testing similar models with a more diverse population are needed. Future samples should not only include greater racial/ethnic diversity, but also greater variation in geographic location. Second, the present study used mostly self-report measures. Replication using more objective measures (e.g., official documents such as social welfare receipts) is needed. Third, because of the large measurement intervals and the limited availability of measures of stage-specific health-risk experiences, the present study may not fully reveal the continuity and intricacies of changes in BMI and affective symptoms trajectories. However, estimated trajectories using three measurements over ten years begin to expose how patterning of approximate trajectories relates to physical health outcomes. Finally, potential confounding variables may exist that were not considered in the present study, such as poor work and relationship quality, strained marital and parental relations, and health risk behaviors.
Despite these limitations, the findings from this study have theoretical and practical implications. Theoretically, this paper emphasizes the importance of examining and understanding both cross-sectional and temporal comorbidity of risk trajectories. That is, both the initial levels (cross-sectional) and conjoint trajectories of BMI and affective symptoms over time (temporal) have substantial health effects. Future research should further explore the way that comorbid health symptoms interact and develop across the life course, while simultaneously developing enhanced theoretical models to provide a more detailed understanding of the mechanisms responsible for these health effects. From the perspective of practical or applied implications, the identification of members of different conjoint risk trajectory groups, and the various socioeconomic antecedents and health outcomes of these groups, provides a potentially useful prognostic tool for early preventive intervention efforts, treatment, and policy formation. Such interventions should focus on promoting and developing resiliency factors, aiding in redirecting adverse risk trajectories of middle-aged women, and buffering the association between adverse risk trajectories and comorbid health outcomes.
Funding
This work is currently supported by a grant from the National Institute on Aging (AG043599, Kandauda A. S. Wickrama, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. Support for earlier years of the study also came from multiple sources, including the National Institute of Mental Health (MH00567, MH19734, MH43270, MH59355, MH62989, MH48165, MH051361); the National Institute on Drug Abuse (DA05347); the National Institute of Child Health and Human Development (HD027724, HD051746, HD047573, HD064687); the Bureau of Maternal and Child Health (MCJ-109572); and the MacArthur Foundation Research Network on Successful Adolescent Development Among Youth in High-Risk Settings.
Author Contributions
K. A. S. Wickrama planned the study, performed the statistical analysis, and wrote the paper. E. T. Klopack contributed to the data analysis and writing the paper; C. W. O’Neal, S. R. H. Beach, T. Neppl, and F. O. Lorenz contributed to editing and revising the paper; and D. Bae helped to plan the study.
Conflict of Interest
None reported.
References
- Ahnquist J. Fredlund P. & Wamala S. P (2007). Is cumulative exposure to economic hardships more hazardous to women’s health than men’s? A 16-year follow-up study of the Swedish Survey of Living Conditions. Journal of Epidemiology and Community Health, 61, 331–336. doi:10.1136/jech.2006.049395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T., & Muthén B. O (2014). Auxiliary variables in mixture modeling: Three-step approaches using Mplus. Structural Equation Modeling, 21, 329–341. doi:10.1080/10705511.2014.915181 [Google Scholar]
- Atlantis E. & Baker M (2008). Obesity effects on depression: Systematic review of epidemiological studies. International Journal of Obesity (2005), 32, 881–891. doi:10.1038/ijo.2008.54 [DOI] [PubMed] [Google Scholar]
- Clarke P. O’Malley P. M. Johnston L. D. & Schulenberg J. E (2009). Social disparities in BMI trajectories across adulthood by gender, race/ethnicity and lifetime socio-economic position: 1986-2004. International Journal of Epidemiology, 38, 499–509. doi:10.1093/ije/dyn214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conger R., & Elder G. H (1994). Families in troubled times: Adapting to change in rural America. New York, NY: Aldine de Gruyter. [Google Scholar]
- Dannefer D. (2003). Cumulative advantage/disadvantage and the life course: Cross-fertilizing age and social science theory. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 58B, S327–S337. doi:10.1093/geronb/58.6.s327 [DOI] [PubMed] [Google Scholar]
- Dennerstein L., & Soares C. N (2008). The unique challenges of managing depression in mid-life women. World Psychiatry, 7, 137–142. doi:10.1002/j.2051–5545.2008.tb00180.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis L. R. & Melisaratos N (1983). The brief symptom inventory: An introductory report. Psychological Medicine, 13, 595–605. doi:10.1017/S0033291700048017 [PubMed] [Google Scholar]
- Dohrenwend B. S. Krasnoff L. Askenasy A. R. & Dohrenwend B. P (1978). Exemplification of a method for scaling life events: The PERI Life Events Scale. Journal of Health and Social Behavior, 19, 205–229. doi:10.2307/2136536 [PubMed] [Google Scholar]
- Dugravot A., Sabia S., Stringhini S., Kivimaki M., Westerlund H., Vahtera J.,…, Singh-Manoux A. (2010). Do socioeconomic factors shape weight and obesity trajectories over the transition from midlife to old age? Results from the French GAZEL Cohort Study. The American Journal of Clinical Nutrition, 92, 16–23. doi:10.3945/ajcn.2010.29223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyer A. R. Stamler J. Garside D. B. & Greenland P (2004). Long-term consequences of body mass index for cardiovascular mortality: The Chicago Heart Association Detection Project in Industry Study. Annals of Epidemiology, 14, 101–108. doi:10.1016/s1047-2797(03)00121-2 [DOI] [PubMed] [Google Scholar]
- Elder G. H., Jr (1998). The life course as developmental theory. Child Development, 69, 1–12. doi:10.2307/1132065 [PubMed] [Google Scholar]
- Elder G. H., & Giele J. Z (2009). The craft of life course research. New York, NY: Guilford Press. [Google Scholar]
- Elrashidi M. Y. Jacobson D. J. St Sauver J. Fan C. Lynch B. A. Rutten L. J. & Ebbert J. O (2016). Body mass index trajectories and healthcare utilization in young and middle-aged adults. Medicine, 95, e2467. doi:10.1097/md.0000000000002467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farmer A., Korszun A., Owen M. J., Craddock N., Jones L., Jones I.,…, McGuffin P. (2008). Medical disorders in people with recurrent depression. The British Journal of Psychiatry, 192, 351–355. doi:10.1192/bjp.bp.107.038380 [DOI] [PubMed] [Google Scholar]
- Faulconbridge L. F. Wadden T. A. Berkowitz R. I. Pulcini M. E. & Treadwell T (2011). Treatment of comorbid obesity and major depressive disorder: A prospective pilot study for their combined treatment. Journal of Obesity, 2011, 870385. doi:10.1155/2011/870385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glei D. A. Goldman N. Chuang Y. L. & Weinstein M (2007). Do chronic stressors lead to physiological dysregulation? Testing the theory of allostatic load. Psychosomatic Medicine, 69, 769–776. doi:10.1097/PSY.0b013e318157cba6 [DOI] [PubMed] [Google Scholar]
- Harris K. M. Perreira K. M. & Lee D (2009). Obesity in the transition to adulthood: Predictions across race/ethnicity, immigrant generation, and sex. Archives of Pediatrics & Adolescent Medicine, 163, 1022–1028. doi:10.1001/archpediatrics.2009.182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- House J. S. Lantz P. M. & Herd P (2005). Continuity and change in the social stratification of aging and health over the life course: Evidence from a nationally representative longitudinal study from 1986 to 2001/2002 (Americans’ Changing Lives Study). Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, 15–26. doi:10.1093/geronb/60.Special_Issue_2.S15 [DOI] [PubMed] [Google Scholar]
- Huffman J. C. Celano C. M. Beach S. R. Motiwala S. R. & Januzzi J. L (2013). Depression and cardiac disease: Epidemiology, mechanisms, and diagnosis. Cardiovascular Psychiatry and Neurology, 2013, 695925. doi:10.1155/2013/695925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson K. M. Sher K. J. & Schulenberg J. E (2005). Conjoint developmental trajectories of young adult alcohol and tobacco use. Journal of Abnormal Psychology, 114, 612–626. doi:10.1037/0021-843X.114.4.612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivimäki M., Lawlor D. A., Singh-Manoux A., Batty G. D., Ferrie J. E., Shipley M. J.,…, Jokela M. (2009). Common mental disorder and obesity: insight from four repeat measures over 19 years: Prospective Whitehall II cohort study. British Medical Journal, 339, b3765. doi:10.1136/bmj.b3765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ladwig K. H. Marten-Mittag B. Löwel H. Döring A. & Koenig W (2003). Influence of depressive mood on the association of CRP and obesity in 3205 middle aged healthy men. Brain, Behavior, and Immunity, 17, 268–275. doi:10.1016/S0889-1591(03)00056-4 [DOI] [PubMed] [Google Scholar]
- Ladwig K. H. Marten-Mittag B. Löwel H. Döring A. & Wichmann H. E (2006). Synergistic effects of depressed mood and obesity on long-term cardiovascular risks in 1510 obese men and women: Results from the MONICA-KORA Augsburg Cohort Study 1984-1998. International Journal of Obesity, 30, 1408–1414. doi:10.1038/sj.ijo.0803285 [DOI] [PubMed] [Google Scholar]
- Lorenz F. O., Elder G. H., Bao W.-N., Wickrama K. A. S., & Conger R. D (2000). After farming: Emotional health trajectories of farm, nonfarm, and displaced farm couples. Rural Sociology, 65, 50–71. doi:10.1111/j.1549-0831.2000.tb00342.x [Google Scholar]
- Lorenz F. O. Wickrama K. A. Conger R. D. & Elder G. H. Jr (2006). The short-term and decade-long effects of divorce on women’s midlife health. Journal of Health and Social Behavior, 47, 111–125. doi:10.1177/002214650604700202 [DOI] [PubMed] [Google Scholar]
- Martikainen P. Stansfeld S. Hemingway H. & Marmot M (1999). Determinants of socioeconomic differences in change in physical and mental functioning. Social Science & Medicine, 49, 499–507. doi:10.1016/S0277-9536(99)00135-5 [DOI] [PubMed] [Google Scholar]
- Maxwell M. A. & Cole D. A (2009). Weight change and appetite disturbance as symptoms of adolescent depression: Toward an integrative biopsychosocial model. Clinical Psychology Review, 29, 260–273. doi:10.1016/j.cpr.2009.01.007 [DOI] [PubMed] [Google Scholar]
- McDonough P. & Berglund P (2003). Histories of poverty and self-rated health trajectories. Journal of Health and Social Behavior, 44, 198–214. doi:10.2307/1519808 [PubMed] [Google Scholar]
- Mumford E. A. Liu W. Hair E. C. & Yu T. C (2013). Concurrent trajectories of BMI and mental health patterns in emerging adulthood. Social Science & Medicine (1982), 98, 1–7. doi:10.1016/j.socscimed.2013.08.036 [DOI] [PubMed] [Google Scholar]
- Murphy R. A., Hagaman A. K., Reinders I., Steeves J. A., Newman A. B., Rubin S. M.,…, Harris T. B; Health ABC Study (2016). Depressive trajectories and risk of disability and mortality in older adults: Longitudinal findings from the health, aging, and body composition study. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 71, 228–235. doi:10.1093/gerona/glv139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén B. O., Khoo S. T., Francis D., & Boscardin C (2003). Analysis of reading skills development from Kindergarten through first grade: An application of growth mixture modeling to sequential processes. In Reise S. R. & Duan N. (Eds.), Multilevel modeling: Methodological advances, issues, and applications (pp. 71–89). Mahaw, NJ: Lawrence Erlbaum Associates. [Google Scholar]
- Muthén L. K., & Muthén B. O (1998–2015). Mplus user’s guide (7th ed). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Olino T. M. Klein D. N. Lewinsohn P. M. Rohde P. & Seeley J. R (2010). Latent trajectory classes of depressive and anxiety disorders from adolescence to adulthood: Descriptions of classes and associations with risk factors. Comprehensive Psychiatry, 51, 224–235. doi:10.1016/j.comppsych.2009.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Rand A. M. (1996). The precious and the precocious: Understanding cumulative disadvantage and cumulative advantage over the life course. The Gerontologist, 36, 230–238. doi:10.1093/geront/36.2.230 [DOI] [PubMed] [Google Scholar]
- Pearlin L. I. Schieman S. Fazio E. M. & Meersman S. C (2005). Stress, health, and the life course: some conceptual perspectives. Journal of Health and Social Behavior, 46, 205–219. doi:10.1177/002214650504600206 [DOI] [PubMed] [Google Scholar]
- Rawana J. S. Morgan A. S. Nguyen H. & Craig S. G (2010). The relation between eating- and weight-related disturbances and depression in adolescence: A review. Clinical Child and Family Psychology Review, 13, 213–230. doi:10.1007/s10567-010-0072-1 [DOI] [PubMed] [Google Scholar]
- Roberts R. E. Deleger S. Strawbridge W. J. & Kaplan G. A (2003). Prospective association between obesity and depression: Evidence from the Alameda County Study. International Journal of Obesity, 27, 514–521. doi:10.1038/sj.ijo.0802204 [DOI] [PubMed] [Google Scholar]
- Rosmond R. Lapidus L. Mårin P. & Björntorp P (1996). Mental distress, obesity and body fat distribution in middle-aged men. Obesity Research, 4, 245–252. doi:10.1002/j.1550–8528.1996.tb00542.x [DOI] [PubMed] [Google Scholar]
- Rugulies R. (2002). Depression as a predictor for coronary heart disease: A review and meta-analysis. American Journal of Preventive Medicine, 23, 51–61. doi:10.1016/s0749-3797(02)00439-7 [DOI] [PubMed] [Google Scholar]
- Ryff C. D., Singer B. H., & Palmersheim K. A (2004). Social inequalities in health and well-being: The role of relational and religious protective factors. In Brim O. G., Ryff C. D., & Kessler R. C. (Eds.), How healthy are we? A national study of well-being at midlife (pp. 90–123). Chicago, IL: University of Chicago Press. [Google Scholar]
- Siegler I. C. (1997). Promoting health and minimizing stress in mid-life. In Lachman M. E. & James J. B. (Eds.), Multiple paths of mid-life development (pp. 241–256). Chicago, IL: University of Chicago Press. [Google Scholar]
- Simons R. L. (1996). The sample, data collection procedures, and measures. In Simons R. L. (Ed.), Understanding differences between divorced and intact families (pp. 21–41). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Steppuhn H. Langen U. Keil T. & Scheidt-Nave C (2014). Chronic disease co-morbidity of asthma and unscheduled asthma care among adults: Results of the national telephone health interview survey German Health Update (GEDA) 2009 and 2010. Primary Care Respiratory Journal, 23, 22–29. doi:10.4104/pcrj.2013.00107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z. & Nakayama T (2010). Inflammation, a link between obesity and cardiovascular disease. Mediators of Inflammation, 2010, 535918. doi:10.1155/2010/535918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M. Yi Y. Roebothan B. Colbourne J. Maddalena V. Wang P. P. & Sun G (2016). Body mass index trajectories among middle-aged and elderly canadians and associated health outcomes. Journal of Environmental and Public Health, 2016, 7014857. doi:10.1155/2016/7014857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama K. A. S., Conger R. D., Lorenz F. O., & Matthews L (1995). Role identity, role satisfaction, and perceived physical health. Social Psychology Quarterly, 58, 270–283. doi:10.2307/2787128 [Google Scholar]
- Wickrama K. A. S., Kwag K. H., Lorenz F. O., Conger R. D., & Surjadi F. F (2010). Dynamics of family economic hardship and the progression of health problems of husbands and wives during the middle years: A perspective from rural mid-west. Journal of Aging and Health, 22, 1132–1157. doi:10.1177/0898264310377353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama K. A. S., Lee T. K., O’Neal C. W., & Lorenz F. O (2016). Higher-order growth curves and mixture modeling with Mplus: A practical guide. New York, NY: Routledge. doi:10.4324/9781315642741 [Google Scholar]
- Wickrama K. K. Mancini J. A. Kwag K. & Kwon J (2013). Heterogeneity in multidimensional health trajectories of late old years and socioeconomic stratification: A latent trajectory class analysis. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 68, 290–297. doi:10.1093/geronb/gbs111 [DOI] [PubMed] [Google Scholar]
- Wickrama K. A. S., O’Neal C. W., & Lorenz F. O (2017). The decade-long effect of work insecurity on husbands’ and wives’ midlife health mediated by anxiety: A dyadic analysis. Journal of Occupational Health Psychology. Advance online publication. doi:10.1037/ocp0000084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickrama K. A. Wickrama T. & Lott R (2009). Heterogeneity in youth depressive symptom trajectories: Social stratification and implications for young adult physical health. The Journal of Adolescent Health, 45, 335–343. doi:10.1016/j.jadohealth.2009.04.018 [DOI] [PubMed] [Google Scholar]
- Wickrama T. & Wickrama K. A (2010). Heterogeneity in adolescent depressive symptom trajectories: Implications for young adults’ risky lifestyle. Journal of Adolescent Health, 47, 407–413. doi:10.1016/j.jadohealth.2010.02.013 [DOI] [PubMed] [Google Scholar]