Abstract
Objective
This study examines relationships between municipal age structure and two types of self-rated health: general (SRH) and comparison with similar-aged peers (C-SRH).
Methods
Using a national sample of almost 5,000 Japanese older adults over two decades, we employ hierarchical growth curve models to estimate health trajectories. For municipal age structure, we consider both the relative prevalence of elderly adults in the local population and the pace of aging over time.
Results
Living in the oldest municipalities was generally associated with worse health, particularly between the ages of 70 and 80 years. For SRH, the speed of municipal population aging was also independently associated with worse health. For C-SRH, worse health in older areas was partially explained by less favorable economic conditions in those municipalities. Results also suggest that higher levels of employment and social integration among older adults living in the oldest municipalities operate in the opposite direction. That is, these attributes partially “protect” individuals from other factors that contribute to worse health.
Discussion
Relative differences in municipal age structure and the pace of population aging are largely unexplored and potentially important correlates of older adult health. This line of research is increasingly salient in a world with substantial and growing regional variation in population aging.
Keywords: Health trajectories, Japan, Population aging, Self-rated health
We live in “an aging world,” but age structure and the pace of population aging vary considerably within countries. For example, although Japan is the oldest country in the world, with 27% of its population aged 65-plus in 2015 (a figure that is projected to rise to almost 40% by 2050), this measure of population aging ranges from approximately 13% to 60% across municipalities (National Institute of Population and Social Security Research, 2017). This is important, since an area’s age structure may be associated with social cohesion and the availability of resources—both of which likely influence older-adult health and well-being (Cagney, 2006). Local-area age structure may thus be a marker of places that either facilitate or hinder “healthy aging” and identifying such places is a well-publicized goal of policy-makers and researchers (United Nations Population Fund, 2012)
Unfortunately, studies that examine relationships between local age structure and older-adult health are limited and provide mixed results. While some studies found “older” age structures (as measured by the percentage of 65-plus) to be associated with better health outcomes (Browning, Wallace, Feinberg, & Cagney, 2006; Kubzansky et al., 2005; Subramanian, Kubzansky, Berkman, Fay, & Kawachi, 2006); others found no relationship (Hybels et al., 2006; Wight, Cummings, Karlamangla, & Aneshensel, 2009). As a group (“prior studies linking age structure to older adult health”), this research generally shares three limitations that we attempt to address in this paper. One, age structure was not the primary theoretical or empirical focus of these studies. Instead, these studies typically included age structure as just one of many local characteristics that could explain relationships between older adult health and place. Two, these studies relied on cross-sectional data. As a result, they were unable to consider changes in either the local age structure or individual health over time. Three, these studies focused on select cities in the United States. This is important because (a) it precludes understanding of regional variation and (b) the United States has a relatively young population when compared to most other high-income countries (He, Goodkind, & Kowal, 2016).
Background
Age Structure and Health
There are reasons to believe that residential age structure can provide both compositional and contextual explanations of “why place matters” for understanding variation in older adult health outcomes (Cagney, 2006). Compositional explanations generally refer to the geographic concentration of individual-level correlates of health (Macintyre, Ellaway, & Cummins, 2002; Subramanian et al., 2006). For example, a study of Japanese older adults found that respondents living in older areas were more likely to be employed (Vogelsang & Raymo, 2014). Since employment is associated with health, this compositional “effect” contributes to health variation between relatively older and younger areas.
Contextual explanations, on the other hand, focus on ways in which the environment (e.g., social, cultural, physical) differentially impacts health outcomes. For example, places experiencing extreme population aging may face various structural challenges (e.g., limited availability of resources, economic stagnation, depopulation) that influence older-adult health (Matanle, Rausch, & Shrinking Regions Research Group, 2011). It is important to note that these compositional and contextual designations are not mutually exclusive, and are likely interrelated (Macintyre et al., 2002). For instance, a place that has strong social cohesion (a contextual characteristic) may help older adults report more friends and become more involved in social activities (composition) than they would otherwise.
Prior studies linking age structure to older adult health operationalized age structure using cross-sectional census data. While the limitations of cross-sectional data are well documented (Singer & Willett, 2003), the dynamic qualities of population age structure (Cagney, 2006) present unique methodological concerns in this line of research. In particular, local population age structure can be characterized not only by whether it is older or younger than other places at any particular point in time, but also by the degree to which it is changing. Individual health outcomes may thus be associated with relative (cross-sectional) differences in age structure as well as with differences in the pace of population aging (longitudinal). This distinction is critical when interpreting results of previous research identifying relationships between individual health and age structure. Cross-sectional data cannot tell us whether a one percent difference in the proportion elderly adults between places has the same relationship with health as a one percent difference change in the proportion elderly adults within places over time. When estimating possible relationships between age structure and health, the use of longitudinal data is also better suited to assess whether: (a) health disparities between older and younger places grow or diminish across older ages or (b) the pace and direction of later-life health change differs by age structure (Yao & Robert, 2008).
Self-Rated Health
Self-rated health (SRH) is the most widely used health survey measure in medical and social science research (Garbarski, 2016). Part of its appeal is that answers to this deceptively simple question are correlated with multiple dimensions of current and future health—including morbidity, functional health, perceived health, and mortality (Jylhä, 2009). One possible concern with using SRH to estimate older-adult health trajectories, however, is that individuals may change their evaluative criteria as they age (“response shift”); leading to SRH responses that are not comparable over time (Garbarski, 2016). These changes are likely due to a combination of normalizing morbidity, lowering personal health expectations, and viewing reference groups more negatively (Galenkamp, Huisman, Braam, & Deeg, 2012; Henchoz, Cavalli, & Girardin, 2008). In other words, while SRH tends to decline during older ages, its speed of decrease is likely mitigated by a weakened SRH-morbidity link.
Although SRH implies a neutral or “global” reference, its vague wording allows respondents to select from a wide variety of social and temporal comparisons when making this assessment (Jylhä, 2009). To address this concern, alternatively worded SRH questions explicitly define reference groups, such as a comparison to age-peers (C-SRH). One important distinction between SRH and C-SRH is that research suggests older adults are more optimistic about their C-SRH; in part because this measure is less tied to functional ability (Vuorisalmi, Lintonen, & Jylhä, 2006). In other words, when compared to SRH, C-SRH evaluations are more likely to be influenced by psycho-social processes (Sargent-Cox, Anstey, & Luszcz, 2008). Employing both SRH and C-SRH in studies linking age structure to health may help in understanding how population aging shapes both individuals’ self-perceptions and their social comparisons.
Population Aging in Japan
As the world’s oldest population, Japan is a valuable setting in which to investigate relationships between age structure and older adult health. Despite unprecedented aging at the national level, there is pronounced regional variation in age structure across Japan. For example, while Tokyo prefecture is relatively young (23% of its residents are 65-and-over), some villages and small towns already have an elderly-majority (National Institute of Population and Social Security Research, 2017). In addition, rapid population aging and “very old” age structures, originally confined to rural areas, can now be seen in many larger towns and regional cities in Japan (Muramatsu & Akiyama, 2011).
Residential stability among older Japanese may help to mitigate some of the methodological problems that plague the health and place literature, such as multiple moves and accounting for the period of exposure to particular environments. Studies of migration at older ages provide little information on Japan (Bradley & Longino, 2009), but available data indicate that residential mobility among older Japanese is substantially lower than that of their American counterparts. Not only do older Japanese move at about half the rate of American older adults, but also approximately half of Japanese movers remain within the same municipality (He & Schachter, 2003; National Institute of Population and Social Security Research, 2017).
Methods
Data
We use the first seven waves of data from the National Survey of the Japanese Elderly (NSJE); a longitudinal study of noninstitutionalized men and women aged 60 and over in Japan. The first wave (n = 2,200), conducted in 1987, was a two-stage national probability sample, comprised of 198 primary sampling units stratified by geographic region and population size (Liang & Maeda, 2006). A subsequent study found this first wave to be broadly representative of the Japanese population in that year and patterns of nonresponse were comparable to similar U.S. surveys (Jay, Liang, Liu, & Sugisawa, 1993). Follow-up surveys were conducted at 3-year intervals (4 years between Waves 6 and 7). Supplemental samples of younger respondents were added at Waves 2 (ages 60–63; n = 404) and 4 (ages 60–66; n = 976); with a third supplement (aged 70-plus; n = 1,657) added at Wave 5. Follow-up response rates across all waves—calculated as a percentage of those asked to participate—ranged from 75% to 93%. In total, 4,999 individuals responded to at least one survey; completing a total of 16,957 surveys across the seven waves.
Municipalities and Age Structure
Respondents’ place of residence is coded at the municipality-level—the smallest government level in Japan—representing designated villages, towns, smaller cities, and wards within larger cities. Since a number of federally-promoted municipal merges were implemented during the study period, we place respondents in the largest (and typically most recent) municipal boundaries. NSJE respondents lived in 307 different municipalities across the seven waves; with populations ranging from 4,011 to 1,164,898 (median 124,892). The proportion of adults aged 65-plus in these municipalities ranged from 5.3% to 26.4% in 1987; and from 12.6% to 49.5% in 2006. Prior studies linking age structure to older adult health typically operationalized age structure as a continuous variable, with little theoretical or empirical justification. While intuitive and similar to other widely-used used census measures (e.g., percent living in poverty), this approach could be problematic if relationships between age structure and health are not linear (Moorman, Stokes, & Morelock, 2016).
We employ two distinct measures of age structure; both based upon the proportion of a municipality’s population that is aged 65-plus. The first of these is a categorical classification of relative baseline age structure. Given the lack of prior research examining nonlinear associations, we considered a wide range of classifications. These included (a) groups with equal numbers of respondents (e.g., tertiles, quartiles, deciles), and (b) groups defined by cut-points used by the United Nations (Kinsella & He, 2009) and a prior study of Japanese older adults (Vogelsang & Raymo, 2014) (i.e., 7%–14%–21% and 10%–15%–20%). We then conducted our analyses using each of these alternative classification schemes. Based upon model fit statistics from these analyses, we chose the most parsimonious grouping: a three-category measure based on quintiles representing “Younger” (quintiles 1 and 2), “Intermediate” aging (quintiles 3 and 4), and “Older” (quintile 5) municipalities. For example, when using deciles, we found that point estimates for deciles 9 and 10 (i.e., quintile 5) were essentially equal; but statistically different from all other deciles. Interestingly, employing cut-points of <10%, 10–15%, and >15% of the population aged 65-plus would have resulted in three categories virtually identical to those presented in this manuscript. Only 189 respondents lived in two or more different municipalities during the survey period; half of whom moved to a municipality in the same age structure category.
The second measure of age structure represents a municipality’s pace of aging; calculated by subtracting the percent 65-plus at wave t-1 from that of wave t. For this variable, a municipality’s percentage of older adults was determined using the Japanese census (Wave 2), interpolation between censuses (Waves 1 and 3), or population estimates from the Statistics Bureau of Japan (Waves 4 through 7).
Health and Other Measures
We examined relationships between age structure and two types of self-assessed health (SRH and C-SRH). In the NSJE, SRH was determined by asking “On the whole, how would you rate your health at the present time?”—“excellent,” “very good,” “good,” “fair,” or “poor.” We dichotomized SRH into “fair/poor” (16.9%) versus all other responses, reflecting the concentration of negative health outcomes associated with these two categories (Idler & Kasl, 1995; Jylhä, 2009); and guidance suggesting this common treatment (Salomon, Nordhagen, Oza, & Murray, 2009). Although both respondent-provided SRH and proxy-provided SRH are independently associated with health outcomes (Ayalon & Covinsky, 2009), these measures are not equivalent and should not be used interchangeably (Vuorisalmi, Sarkeala, Hervonen, & Jylhä, 2012). Therefore, we excluded data from proxy respondents in this study (9.1% of person-waves). SRH was missing in 67 person-waves (0.4%), resulting in a sample size of 16,890.
C-SRH was based on the question “Compared to other people of your age, do you think your health is ‘better,’ ‘about the same,’ or ‘worse’?” To facilitate comparison with SRH, we also dichotomized C-SRH: “worse” (12.7%) versus other responses. Answers to this question were missing in 429 (2.5%) person-waves—resulting in a sample of 16,528. For NSJE respondents who reported unfavorable health for either of these measures (n = 3,243), 17% reported worse C-SRH, 35% reported fair/poor SRH and 48% reported both.
Our models also include age, sex, marital status, work status, education, and income; since these compositional characteristics are likely related to both health and age structure (Subramanian et al., 2006; Vogelsang & Raymo, 2014). Income represents the total income of the respondent and his or her spouse (average exchange rate across the survey years was approximately ¥120 = $1). We also included a dummy variable to identify the year that respondents first participated in the survey.
Recent research suggests that differences in social-connectedness are one way that living in relatively older or younger areas may be associated with health (Moorman et al., 2016). Because of this, we employ a social integration index utilizing all related NSJE questions that were asked consistently across waves. We created this index by dichotomizing categorical and quantitative responses to represent “high” and “low” social activity; and then summing the scores (range 0–6) (Kirst, Lazgare, Zhang, & O’Campo, 2015; Verhaeghe & Tampubolon, 2012). These items were: “has at least two close friends whom you can confide in (52%),” “meets friends, neighbors, or (nonchild) relatives more than once a month” (55%), “talks with friends, neighbors or (nonchild) relatives more than once a week” (33%), “belongs to a social club or group” (65%), “never feels isolated” (79%), and “has children and sees them at least once a month (59%).”
In addition to these compositional characteristics, we used census measures to characterize two kinds of social conditions (i.e., context) at the municipal level (Diez Roux & Mair, 2010). The first, municipality per capita taxable income, represents local economic circumstances. This variable was calculated by taking the natural log of year- and municipality-specific total annual taxable income (in million yen) divided by the total municipal population. The vast majority of “health and place” studies focuses on, or controls for, economic conditions (e.g., inequality, structural disadvantage) (Entwisle, 2007). As such, including this measure allows us to assess whether observed relationships between age structure and health are simply proxies for relationships between the local economy and health.
We also utilize a municipality’s gross migration rate as a measure of residential stability. We chose this measure since there is evidence that places with a greater proportion of older adults have less residential turnover (Cagney, 2006; Wight, Cummings, Karlamangla, & Aneshensel, 2010); which may facilitate health-improving social cohesion and social integration (Kawachi & Berkman, 2000). We calculated this measure by dividing the mean annual number of residents moving in or out of a municipality in a given year by the mean population in the same year. Income data were obtained from the Japanese Statistical Abstract of Municipalities; while the migration figures were from the Japanese Basic Resident Registry.
Analytic Strategy
The goals of this paper are to (a) assess the extent to which local area age structure is associated with two types of subjective health trajectories across older ages in Japan and (b) examine individual (compositional) and municipal (contextual) characteristics that might account for relationships observed in (a). To accomplish this, we estimated a sequence of three multilevel growth curve models (Rabe-Hesketh & Skrondal, 2012) using Stata 14.1 (StataCorp, 2015). These models nested observations (Level 1) within respondents (Level 2); and operationalized time using respondents’ age. The use of age-based growth curve models allows us to estimate interpersonal differences in health trajectories between municipal age-structure categories; including the direction and pace of health change. By including two random effects (intercept and slope), these models also allow us to account for unobserved heterogeneity and dependence among multiple observations of the same individual (Rabe-Hesketh & Skrondal, 2012). Independent variables that can differ by survey wave (e.g., work status, municipal pace of aging) are included in the Level 1 equation; while those that are fixed for individuals (e.g., education, baseline municipal age structure) are included in the Level 2 equation.
The first model (M1) is a baseline model that assesses whether health trajectories differ by municipal age structure. The second model (M2) includes all individual-level correlates of health. This model establishes the extent to which population composition explains or suppresses any relationships between municipal population aging and individual health trajectories estimated in M1. The third model (M3) tests whether relationships identified in M2 are explained by two municipal-level measures of context (economic well-being and residential stability). In estimating these SRH and C-SRH trajectories, we tested numerous specifications of time (age); including linear, quadratic and cubic functional forms. We present results from the most parsimonious model specifications, after considering both goodness of fit statistics (likelihood-ratio tests, AIC comparisons) and statistically significant coefficients. For SRH, we found a significant interaction between age structure and both the linear and quadratic measures of time. For C-SRH, we found no significant interaction between age structure and time. However, model fit statistics indicated that time should be estimated using a quadratic specification.
Results
Table 1 presents descriptive statistics. It also indicates whether these statistics differ significantly by age structure; using younger municipalities as the reference category. For example, those living in older municipalities were significantly more likely to report fair/poor SRH (19.0%) and worse C-SRH (14.4%) than those in younger places (16.0% and 11.4%, respectively). There were also significant relationships between age structure and the following individual-level characteristics: marriage, employment, low SES, and social integration (all of which were more prevalent/higher in older areas). In addition, older places were characterized by greater residential stability and lower per capita income when compared to younger municipalities.
Table 1.
Descriptive Statistics and Bivariate Analysis by Age Structure Categories, National Survey of Japanese Elderly Adults, Waves 1–7 (n = 16,957)
| Baseline age structure of residential municipality (% 65-plus) | Quintiles 1 and 2 (“Younger”) | Quintiles 3 and 4 (“Intermediate”) | Quintile 5 (“Older”) | Total sample |
|---|---|---|---|---|
| Fair/poor SRH (%), (SD) | 16.0 (0.4) | 16.8 (0.4) | 19.0* (0.4) | 16.9 (0.4) |
| Worse C-SRH (%), (SD) | 11.4 (0.3) | 13.1* (0.4) | 14.4* (0.4) | 12.7 (0.3) |
| % 65-plus at baseline; mean (SD) | 8.4 (1.4) | 12.5* (1.2) | 17.5* (2.8) | 11.7 (3.7) |
| Change in Municipality % 65-plus (between survey waves); mean (SD) | 1.4 (0.6) | 1.5* (0.5) | 1.7* (0.7) | 1.5 (0.6) |
| Age, mean (SD) | 72.8 (7.2) | 73.1 (7.2) | 72.8 (7.3) | 72.9 (7.2) |
| Female (%) | 58.5 | 55.1* | 56.7 | 56.8 |
| Married (%) | 60.0 | 63.1* | 65.4* | 62.3 |
| Working (%) | 22.7 | 27.0* | 32.6* | 26.4 |
| Education (%): | ||||
| No answer | 1.4 | 2.0 | 1.5 | 1.7 |
| No high school | 39.3 | 41.1* | 46.4* | 41.5 |
| Some/completed high school | 41.4 | 43.0 | 41.4 | 42.0 |
| >High school | 17.9 | 13.9* | 10.7* | 14.8 |
| Income (%): | ||||
| Did not answer | 15.6 | 15.1 | 17.0 | 15.7 |
| <¥1.2 Mil | 17.6 | 23.1* | 25.5* | 21.4 |
| ≥¥1,2 Mil-<¥3.0 Mil | 36.3 | 32.9 | 31.3* | 33.9 |
| ≥¥3.0 Mil-<¥5.0 Mil | 19.3 | 18.9 | 18.1 | 18.9 |
| ≥¥5.0 Mil | 11.2 | 10.0* | 8.1* | 10.1 |
| Social integration, mean (SD) | 3.3 (1.6) | 3.4* (1.5) | 3.7* (1.5) | 3.4 (1.6) |
| Municipal gross migration rate, mean | 11.9 | 9.0* | 7.2* | 9.8 |
| Municipal per capita income (¥), mean | 402,837.1 | 290,711.4* | 39,373.0* | 286,172.6 |
| (Natural Log) | (12.5) | (11.9)* | (10.3)* | (11.8) |
| N | 6,787 | 6,836 | 3,334 | 16,957 |
Note: SRH = Self-rated health; C-SRH=Self-rated health comparison to age-peers.
*Statistically different from the younger municipalities at p ≤ .05.
Results of the regression models are presented in Table 2 (SRH) and Table 3 (C-SRH). Estimates are displayed as the odds ratios (OR) for reporting fair/poor (SRH) or worse (C-SRH) health, conditional upon individual-level random effects. For SRH, the baseline model (M1-A) indicates that older adults living in older municipalities experienced more rapid health decline (OR = 1.08) than those living in younger areas. However, there was no evidence of fixed (intercept) SRH differences by local age structure. Results also indicated that the pace of aging at the municipality level (increase of one percentage point in the proportion of older adults between survey waves) was positively associated with reporting fair/poor SRH (OR = 1.19).
Table 2.
Odds Ratios for Reporting Fair or Poor Self-Rated Health, Conditional Upon Random Effects
| M1-A | M2-A | M3-A | ||||
|---|---|---|---|---|---|---|
| OR | (SE) | OR | (SE) | OR | (SE) | |
| Baseline Municipal Age Structure | ||||||
| “Younger” (Quintiles 1 and 2) (ref.) | 1.00 | (0.00) | 1.00 | (0.00) | 1.00 | (0.00) |
| “Intermediate” (Quintiles 3 and 4) | 1.40 | (0.36) | 1.48# | (0.36) | 1.45 | (0.36) |
| “Older” (Quintile 5) | 0.72 | (0.24) | 0.76 | (0.24) | 0.68 | (0.22) |
| Change in Municipality % 65-plus (between survey waves) | 1.19** | (0.08) | 1.20** | (0.08) | 1.18** | (0.03) |
| Age | 1.10** | (0.03) | 1.07** | (0.03) | 1.07** | (0.03) |
| Age × “Intermediate” | 0.96 | (0.03) | 0.97 | (0.03) | 0.96 | (0.03) |
| Age × “Older” | 1.08* | (0.04) | 1.11* | (0.04) | 1.11* | (0.04) |
| Age Squared | 0.99 | (0.00) | 0.99 | (0.00) | 0.99 | (0.00) |
| Age Squared × “Intermediate” | 1.00 | (0.00) | 1.00 | (0.00) | 1.00 | (0.00) |
| Age Squared × “Older” | 0.99# | (0.00) | 0.99* | (0.00) | 0.99* | (0.00) |
| Education | ||||||
| Did not answer | 1.27 | (0.37) | 1.28 | (0.33) | ||
| No HS | 1.00 | (0.00) | 1.00 | (0.00) | ||
| Some/completed HS | 0.94 | (0.09) | 0.95 | (0.09) | ||
| >High School | 0.83 | (0.12) | 0.85 | (0.13) | ||
| Income | ||||||
| (Did not answer) | 1.00 | (0.09) | 1.00 | (0.09) | ||
| <¥1.2 Mil | 1.07 | (0.09) | 1.07 | (0.09) | ||
| ≥¥1,2 Mil-<¥3.0 Mil | 1.00 | (0.00) | 1.00 | (0.00) | ||
| ≥¥3.0 Mil-<¥5.0 Mil | 0.87 | (0.08) | 0.87 | (0.08) | ||
| ≥¥5.0 Mil | 0.74* | (0.10) | 0.75* | (0.10) | ||
| Female | 1.03 | (0.10) | 1.03 | (0.10) | ||
| Working (ref. = not working) | 0.33*** | (0.03) | 0.33*** | (0.03) | ||
| Married (ref. = not married) | 1.00 | (0.09) | 1.00 | (0.09) | ||
| Social integration | 0.71*** | (0.02) | 0.71*** | (0.03) | ||
| Municipal Gross Migration Rate | 1.01 | (0.01) | ||||
| Municipal (Log) Per Capita Income (¥) | 0.93* | (0.03) | ||||
| Entry Cohort (ref: Wave 1) | ||||||
| Wave 2 | 0.73# | (0.13) | 0.87 | (0.15) | 0.87 | (0.15) |
| Wave 4 | 0.58*** | (0.08) | 0.74* | (0.11) | 0.74* | (0.11) |
| Wave 5 | 0.90 | (0.10) | 0.97 | (0.10) | 0.97 | (0.10) |
| Random Effect (SD): Intercept | 2.11 | (0.07) | 1.92 | (0.06) | 1.92 | (0.06) |
| Random Effect (SD): Slope | 0.03 | (0.00) | 0.03 | (0.00) | 0.03 | (0.00) |
| Akaike information criterion | 13,621 | 13,167 | 13,167 | |||
| Log Likelihood | −6,797 | −6,558 | −6,556 | |||
| N | 16,890 | 16,890 | 16,890 | |||
Note:
*p ≤ .05; **p ≤ .01; ***p ≤ .001; #p ≤ .10.
Table 3.
Odds Ratios for Reporting Worse Health than Age-Peers, Conditional Upon Random Effects
| M1-B | M2-B | M3-B | ||||
|---|---|---|---|---|---|---|
| OR | (SE) | OR | (SE) | OR | (SE) | |
| Baseline Municipal Age Structure | ||||||
| “Younger” (Quintiles 1 and 2) (ref.) | 1.00 | (0.00) | 1.00 | (0.00) | 1.00 | (0.00) |
| “Intermediate” (Quintiles 3 and 4) | 1.30* | (0.15) | 1.35** | (0.15) | 1.27* | (0.15) |
| “Older” (Quintile 5) | 1.50** | (0.21) | 1.77*** | (0.24) | 1.40* | (0.24) |
| Change in Municipality % 65-plus (between survey waves) | 1.08 | (0.08) | 1.10 | (0.08) | 1.08 | (0.08) |
| Age | 1.08** | (0.02) | 1.05** | (0.02) | 1.05** | (0.02) |
| Age Squared | 0.99* | (0.00) | 0.99*** | (0.00) | 0.99*** | (0.00) |
| Education | ||||||
| (Did not answer) | 1.58 | (0.52) | 1.58 | (0.53) | ||
| No HS | 1.00 | (0.00) | 1.00 | (0.00) | ||
| Some/Completed HS | 0.92 | (0.11) | 0.93 | (0.11) | ||
| >High School | 0.63** | (0.11) | 0.66** | (0.12) | ||
| Income | ||||||
| (Did not answer) | 0.93 | (0.10) | 0.93 | (0.10) | ||
| <¥1.2 Mil | 1.13 | (0.11) | 1.11 | (0.11) | ||
| ≥¥1,2 Mil-<¥3.0 Mil | 1.00 | (0.00) | 1.00 | (0.00) | ||
| ≥¥3.0 Mil-<¥5.0 Mil | 0.75** | (0.08) | 0.75** | (0.08) | ||
| ≥¥5.0 Mil | 0.61** | (0.10) | 0.62** | (0.10) | ||
| Female | 1.16 | (0.13) | 1.16 | (0.13) | ||
| Working (ref. = not working) | 0.28*** | (0.03) | 0.27*** | (0.03) | ||
| Married (ref. = not married) | 1.11 | (0.11) | 1.11 | (0.12) | ||
| Social Integration | 0.65*** | (0.02) | 0.65*** | (0.02) | ||
| Municipal Gross Migration Rate | 1.00 | (0.01) | ||||
| Municipal (Log) Per Capita Income (¥) | 0.89** | (0.04) | ||||
| Entry Cohort (ref: Wave 1) | ||||||
| Wave 2 | 0.82 | (0.16) | 1.04 | (0.20) | 1.04 | (0.20) |
| Wave 4 | 0.63*** | (0.10) | 0.91 | (0.15) | 0.90 | (0.15) |
| Wave 5 | 0.84 | (0.10) | 0.96 | (0.12) | 0.96 | (0.12) |
| Random Effect (SD): Intercept | 2.45 | (0.08) | 2.15 | (0.08) | 2.14 | (0.08) |
| Random Effect (SD): Slope | 0.03 | (0.00) | 0.03 | (0.00) | 0.03 | (0.00) |
| AIC | 11,115 | 10,522 | 10,518 | |||
| Log Likelihood | −5,509 | −5,240 | −5,236 | |||
| N | 16,528 | 16,528 | 16,528 | |||
Note: *p ≤ .05; **p ≤ .01; ***p ≤ .001.
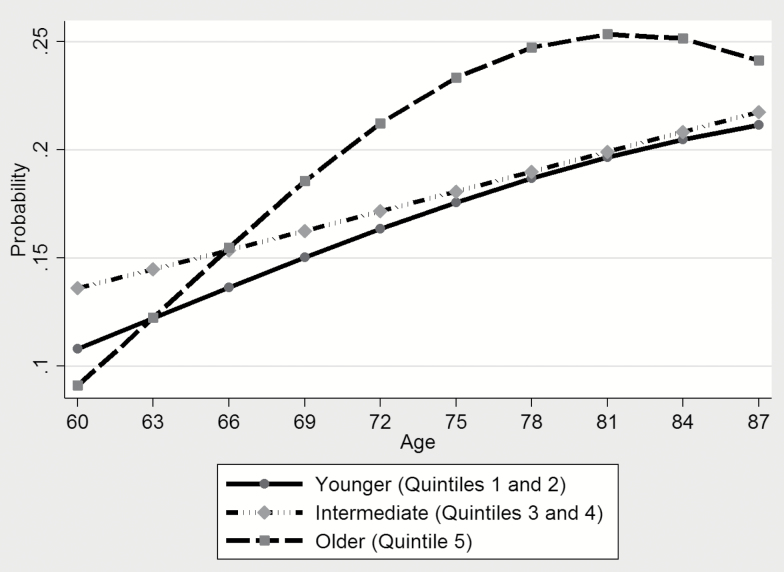
After including individual-level covariates (composition) in M2-A, the more rapid health decline associated with living in older areas (compared to those living in younger places) became more pronounced (OR = 1.11). This reflects higher average levels of social integration and employment (partially offset by lower income) suppressing some of the health “disadvantage” associated with living in Japan’s older areas in M1-A. Introducing municipal-level measures of net migration and per capita income (context) in M3-A did little to change these relationships. In other words, even though more favorable municipal-level economic conditions were associated with better SRH (OR = 0.93), inclusion of this contextual variable did not alter the estimated relationships between age structure and health. Further, model fit statistics preferred M2-A over M3-A (LR test χ2 = 4.0 [p = .14]). Figure 1 displays the estimated marginal trajectories from M2-A, by age structure categories, evaluated at the mean values of all other independent variables. This figure illustrates that the higher probability of reporting fair/poor SRH among those living in older municipalities (when compared to younger areas) is primarily observed between ages 70 and 80.
Figure 1.
Predictive Marginal Probability of Reporting Fair or Poor Self-Rated Health; by Baseline Age Structure Categories (based upon Model 2-A, Table 2).
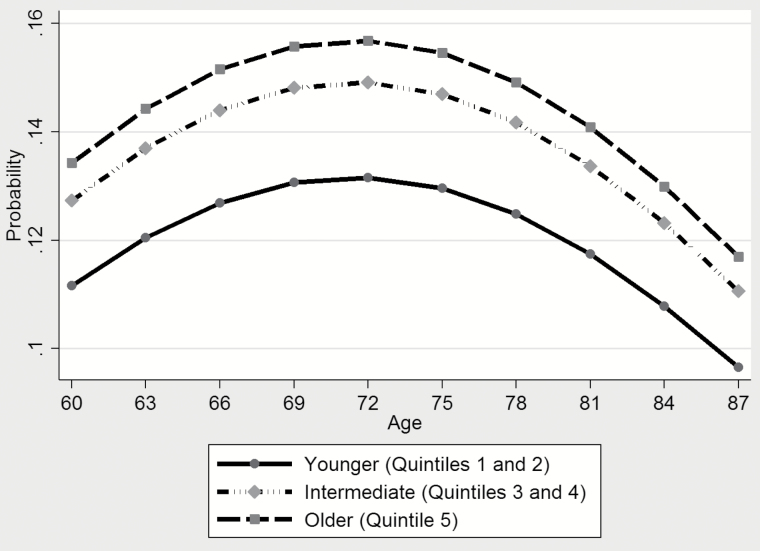
For C-SRH (Table 3), M1-B revealed that the relative odds of reporting worse health are greater in the intermediate and older municipalities (OR = 1.30 and OR = 1.50, respectively), when compared to those living in younger places. These associations became even stronger after the inclusion of individual-level characteristics in M2-B (OR = 1.35 and OR = 1.77, respectively)—suggesting that, similar to SRH, differences in population composition act to mitigate the relationship between older age structures and worse health at the individual level. Unlike SRH, however, there was no evidence in either M1-B or M2-B of a relationship between the pace of municipality population aging and C-SRH. In M3-B, including regional characteristics (context) suggest that almost half of the relationship between older age structures and C-SRH identified in M2-B is attributable to regional economic circumstances (OR = 1.40; compared to OR = 1.77 in M2-B). Model fit statistics preferred M3-B over M2-B (LR test χ2 = 9.7 [p = .01]) and a graphical representation of results from this model is provided in Figure 2.
Figure 2.
Predictive Marginal Probability of Reporting Worse Health than Age-Peers; by Baseline Age Structure Categories (based upon Model 3-B, Table 3).
Sensitivity Analyses
We performed multiple sensitivity tests in order to assess the robustness of our results. First, we estimated an additional set of models that considered how our results may be sensitive to nonrandom attrition due to mortality (n = 1,979) and nonresponse (11.4% of person-waves). In this set of models, we employed inverse probability weights that were calculated using a predicated probability of attrition based upon individual-level characteristics. Results of these analyses were virtually identical to those presented in this paper; reflecting the fact that survey attrition and the mean age of attrition did not differ significantly across age structure categories.
Our second supplemental analysis considered the NSJE’s use of irregular survey supplements; particularly the large additional sample of individuals aged 70-plus in Wave 5. We estimated an additional set of models using survey weights in Waves 5 through 7 that ensured a consistent age distribution prior to and subsequent to this supplement. Results from these models were essentially the same as those presented in the paper; with one exception: the association between SRH and the pace of municipal population aging was attenuated (from OR = 1.20 to OR = 1.13 in M2-A). This was attributable to the fact that this association was weaker among the survey’s younger respondents (aged 60–72)—the same group that was more heavily weighted in the supplementary analysis.
Overall, the NSJE has little missing data (Liang et al., 2002), although almost 7% of respondents were missing at least one item of the social integration index, and 17% did not answer the income question (a separate category in the main analysis, but coded as missing in this supplementary analysis). Using Stata’s multiple imputation procedure, we created five additional datasets. Results averaged across these five sets were substantively the same to those presented in Tables 2 and 3.
Discussion
This study advances the gerontological literature linking health and place in two ways. One, this is the first paper that we are aware of to find associations between older-adult health and two measures of local age structure: relative age structure differences between places, and the pace of local population aging. Two, our results suggest that relationships between age structure and self-assessed health may differ by the measure of SRH employed.
Like most studies examining “place effects” on health, we considered both composition and context (Macintyre et al., 2002) when estimating health trajectories. For example, our results indicated that the higher prevalence of employment and the greater social integration of older individuals living in relatively older places (composition) helped to partially “protect” individuals from associations between older age structures and worse health. Our finding that older adults in older areas reported greater social integration is noteworthy, since (a) individuals with lower average socioeconomic status generally have lower social capital (Kaasa & Parts, 2008; Kawachi, Takao, & Subramanian, 2013) and (b) older Japanese adults living in relatively older places are often thought to be physically and socially isolated (Matanle et al., 2011).
After considering both population composition and two measures of residential context, health trajectory differences between relatively older and younger places remained. Identifying other compositional and contextual characteristics that account for these relationships remains an important task for future research, and explanations will likely differ by the measure of health considered. SRH, for instance, has stronger associations with various “objective” health measures when compared to C-SRH (Sargent-Cox et al., 2008), and there are reasons to believe that age structure may indirectly influence some health outcomes. For example, substandard infrastructure, amenities, and services often accompany depopulation and population aging (Seaton, 2010); and these characteristics are likely tied to health at older ages. Indeed, prior research has found that elderly adults living in Japan’s oldest places report more difficulty walking a city block or shopping (Vogelsang & Raymo, 2014) and restricted transportation options continue to be a health concern for these same individuals (Murata, Kondo, Tamakoshi, Yatsuya, & Toyoshima, 2006). There is also growing recognition that both rural areas and mid-sized regional cities in Japan—the same places more likely to experience rapid population aging—are underserved by physicians and have fewer health care services (Matsumoto, Inoue, & Kajii, 2010; Shinjo & Aramaki, 2012).
Another possible explanation for more rapid SRH decline among those living in older areas pertains to the type of employment that characterizes those places—both a compositional (individual-level attribute) and contextual (e.g., cultural, historical) effect. A supplemental analysis of NSJE respondents found that 49% of those employed in older municipalities work in agriculture or fishing; compared 29% and 14% of those living in intermediate and younger age structures, respectively. Although employment is generally associated with better health, the risk of injury or the possible cumulative health effects associated with decades of physically demanding work (Amshoff & Reed, 2005) is something to be considered in subsequent research.
Unlike those of SRH, our estimated C-SRH trajectories indicate that individuals in their 70s report more-negative health than those in their 60s and 80s. This shape aligns with prior research and is likely the result of age-based response shifts (Sargent-Cox et al., 2008). These shifts, however, do not account for the “fixed” (intercept) trajectory differences between age-structure categories. Instead, these differences are likely influenced by evaluative processes that are both unique to C-SRH and associated with municipal age structure. For example, prior studies have found that C-SRH is much more likely than SRH to be influenced by social comparisons and reference groups (Sargent-Cox et al., 2008) and those in older places may compare themselves with those in younger, more vibrant places. To put it another way, older adults living in Japan’s oldest areas may not only experience inferior medical care but they may also feel as if they receive worse care. Evidence of these regional comparisons can be found in research suggesting that perceptions of relative deprivation—including a comparison to cross-country “distant others”—negatively impacts happiness and well-being (Dolan, Peasgood, & White, 2008; Kingdon & Knight, 2007). This paper, in turn, suggests that these same experiences and evaluative processes may shape subjective health.
Limitations and Conclusion
There are several limitations to this study. One, although we tested numerous specifications, we present results for just one operationalization of both baseline age structure and the pace of aging. That said, our results provide compelling evidence for considering non-linear measurement of age structure and employing longitudinal census data. In fact, supplemental analyses revealed that treating baseline age structure as a continuous variable would result in estimates implying a linear relationship between the proportion of older adults and SRH—whereas we show that those estimates are largely driven by the oldest places. Two, we did not account for self-selection into municipalities of residence; although this concern is mitigated by the relatively low rates of geographic mobility at older ages in Japan. Three, we do not have access to respondents’ residential history prior to their first response (mean age at first observation = 66), precluding us from examining how long-term exposure to particular residential contexts shapes later-life health.
Although it is well-known that the world is growing older, much less is made of age structure differences at the local level and the possible health implications for those aging in the “oldest places.” Our findings suggest that older people living in areas that are (a) already relatively old and (b) experiencing more rapid population aging may face a “double jeopardy” when it comes to the health implications of local age structure. As governments and international organizations increasingly focus on identifying attributes of age-friendly places, our findings make the case for local age structure being a part of this discussion. For instance, older adults living in relatively older places may face greater economic challenges; but these same places may promote health through greater social cohesion. This is important as we start to disentangle possible advantages and disadvantages of having large groups of older adults segregated from younger people and places.
Funding
This work was supported by a training grant from the National Institute on Aging (T32 AG000129) and by core grants to the Center for Demography and Ecology at the University of Wisconsin-Madison (P2C HD047873) and to the Center for Demography of Health and Aging at the University of Wisconsin-Madison (P30 AG017266).
Conflict of Interest
The authors declare that they have no competing interests.
Author Contributions
E. M. Vogelsang planned the study, performed the statistical analysis, and was the primary writer of the manuscript. J. M. Raymo contributed to the writing of the manuscript and the planning of the study. J. Liang contributed to the writing of the manuscript. E. Kobayashi and T. Fukaya conducted primary data collection and coded geographic identifiers.
References
- Amshoff S. K. & Reed D. B (2005). Health, work, and safety of farmers ages 50 and older. Geriatric Nursing, 26, 304–308. doi:10.1016/j.gerinurse.2005.08.008 [DOI] [PubMed] [Google Scholar]
- Ayalon L. & Covinsky K. E (2009). Spouse-rated vs self-rated health as predictors of mortality. Archives of Internal Medicine, 169, 2156–2161. doi:10.1001/archinternmed.2009.386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley D. E., & Longino C. F (2009). Geographic mobility and aging in place. In Uhlenberg P. (Ed.), International handbook of population aging (pp. 319–339). New York: Springer. [Google Scholar]
- Browning C. R., Wallace D., Feinberg S. L., & Cagney K. A (2006). Neighborhood social processes, physical conditions, and disaster-related mortality: The case of the 1995 chicago heat wave. American Sociological Review, 71, 661–678. doi:10.1177/000312240607100407 [Google Scholar]
- Cagney K. A. (2006). Neighborhood age structure and its implications for health. Journal of Urban Health: Bulletin of the New York Academy of Medicine, 83, 827–834. doi:10.1007/s11524-006-9092-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez Roux A. V. & Mair C (2010). Neighborhoods and health. Annals of the New York Academy of Sciences, 1186, 125–145. doi:10.1111/j.1749-6632.2009.05333.x [DOI] [PubMed] [Google Scholar]
- Dolan P., Peasgood T., & White M (2008). Do we really know what makes us happy? A review of the economic literature on the factors associated with subjective well-being. Journal of Economic Psychology, 29, 94–122. doi:10.1016/j.joep.2007.09.001 [Google Scholar]
- Entwisle B. (2007). Putting people into place. Demography, 44, 687–703. [DOI] [PubMed] [Google Scholar]
- Galenkamp H. Huisman M. Braam A. W. & Deeg D. J (2012). Estimates of prospective change in self-rated health in older people were biased owing to potential recalibration response shift. Journal of Clinical Epidemiology, 65, 978–988. doi:10.1016/j.jclinepi.2012.03.010 [DOI] [PubMed] [Google Scholar]
- Garbarski D. (2016). Research in and prospects for the measurement of health using self-rated health. Public Opinion Quarterly, 80, 977–997. doi:10.1093/poq/nfw033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- He W., Goodkind D., & Kowal P (2016). An aging world: 2015 (Vol. P95/16-1). Washington, DC: U.S. Census Bureau. [Google Scholar]
- He W., & Schachter J. P (2003). Internal migration of the older population: 1995 to 2000 Census 2000 Special Reports. Washington DC: U.S. Census Bureau. [Google Scholar]
- Henchoz K., Cavalli S., & Girardin M (2008). Health perception and health status in advanced old age: A paradox of association. Journal of Aging Studies, 22, 282–290. doi:10.1016/j.jaging.2007.03.002 [Google Scholar]
- Hybels C. F., Blazer D. G., Pieper C. F., Burchett B. M., Hays J. C., Fillenbaum G. G.,…, Berkman L. F. (2006). Sociodemographic characteristics of the neighborhood and depressive symptoms in older adults: Using multilevel modeling in geriatric psychiatry. The American Journal of Geriatric Psychiatry: Official Journal of the American Association for Geriatric Psychiatry, 14, 498–506. doi:10.1097/01.JGP.0000194649.49784.29 [DOI] [PubMed] [Google Scholar]
- Idler E. L. & Kasl S. V (1995). Self-ratings of health: Do they also predict change in functional ability?The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 50, S344–S353.doi:10.1093/geronb/50b.6.s344 [DOI] [PubMed] [Google Scholar]
- Jay G. M. Liang J. Liu X. & Sugisawa H (1993). Patterns of nonresponse in a national survey of elderly Japanese. Journal of Gerontology, 48, S143–S152. [PubMed] [Google Scholar]
- Jylhä M. (2009). What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Social Science & Medicine (1982), 69, 307–316. doi:10.1016/j.socscimed.2009.05.013 [DOI] [PubMed] [Google Scholar]
- Kaasa A., & Parts E (2008). Individual-level determinants of social capital in europe differences between country groups. Acta Sociologica, 51, 145–168. doi:10.2139/ssrn.1017757 [Google Scholar]
- Kawachi I., & Berkman L (2000). Social cohesion, social capital, and health. Social Epidemiology, 174–190. doi:10.1093/med/9780195377903.003.0008 [Google Scholar]
- Kawachi I., Takao S., & Subramanian S. V (2013). Global perspectives on social capital and health. New York: Springer. doi:10.1007/978-1-4614-7464-7 [Google Scholar]
- Kingdon G. G., & Knight J (2007). Community, comparisons and subjective well-being in a divided society. Journal of Economic Behavior & Organization, 64, 69–90. doi:10.1016/j.jebo.2007.03.004 [Google Scholar]
- Kinsella K., & He W (2009). An aging world: 2008 (Vol. PF05/09-1). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Kirst M. Lazgare L. P. Zhang Y. J. & O’Campo P (2015). The effects of social capital and neighborhood characteristics on intimate partner violence: A consideration of social resources and risks. American Journal of Community Psychology, 55, 314–325. doi:10.1007/s10464-015-9716-0 [DOI] [PubMed] [Google Scholar]
- Kubzansky L. D. Subramanian S. V. Kawachi I. Fay M. E. Soobader M. J. & Berkman L. F (2005). Neighborhood contextual influences on depressive symptoms in the elderly. American Journal of Epidemiology, 162, 253–260. doi:10.1093/aje/kwi185 [DOI] [PubMed] [Google Scholar]
- Liang J., Bennett J., Krause N., Kobayashi E., Kim H., Brown J. W.,…, Jain A. (2002). Old age mortality in Japan: Does the socioeconomic gradient interact with gender and age?The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 57, S294–S307. doi:10.1093/geronb/57.5.S294 [DOI] [PubMed] [Google Scholar]
- Liang J., & Maeda D (2006). National survey of the Japanese elderly. Ann Arbor, MI: Inter-university Consortiumn for Political and Social Policy Research. doi:10.3886/ICPSR06842.v1 [Google Scholar]
- Macintyre S. Ellaway A. & Cummins S (2002). Place effects on health: How can we conceptualise, operationalise and measure them?Social Science & Medicine (1982), 55, 125–139. [DOI] [PubMed] [Google Scholar]
- Matanle P., Rausch A.,& Shrinking Regions Research Group. (2011). Japan’s shrinking regions in the 21st century: Contemporary responses to depopulation and socioeconomic decline. Amherst, NY: Cambria Press. doi:10.1017/s002191181400134x [Google Scholar]
- Matsumoto M. Inoue K. & Kajii E (2010). Policy implications of a financial incentive programme to retain a physician workforce in underserved Japanese rural areas. Social Science & Medicine (1982), 71, 667–671. doi:10.1016/j.socscimed.2010.05.006 [DOI] [PubMed] [Google Scholar]
- Moorman S. M., Stokes J. E., & Morelock J. C (2016). Mechanisms linking neighborhood age composition to health. The Gerontologist. Advance online publication. doi:10.1093/geront/gnv687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muramatsu N. & Akiyama H (2011). Japan: super-aging society preparing for the future. The Gerontologist, 51, 425–432. doi:10.1093/geront/gnr067 [DOI] [PubMed] [Google Scholar]
- Murata C. Kondo T. Tamakoshi K. Yatsuya H. & Toyoshima H (2006). Factors associated with life space among community-living rural elders in Japan. Public Health Nursing (Boston, Mass.), 23, 324–331. doi:10.1111/j.1525-1446.2006.00568.x [DOI] [PubMed] [Google Scholar]
- National Institute of Population and Social Security Research (2017). Population statistics of Japan 2017. Tokyo: National Institute of Population and Social Security Research. [Google Scholar]
- Rabe-Hesketh S., & Skrondal A (2012). Multilevel and longitudinal modeling using Stata (3rd ed Vol. 1). College Station, TX: Stata Corp LP. [Google Scholar]
- Salomon J. A. Nordhagen S. Oza S. & Murray C. J (2009). Are Americans feeling less healthy? The puzzle of trends in self-rated health. American Journal of Epidemiology, 170, 343–351. doi:10.1093/aje/kwp144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sargent-Cox K. A. Anstey K. J. & Luszcz M. A (2008). Determinants of self-rated health items with different points of reference: Implications for health measurement of older adults. Journal of Aging and Health, 20, 739–761. doi:10.1177/0898264308321035 [DOI] [PubMed] [Google Scholar]
- Seaton P. (2010). Depopulation and financial collapse in yūbari: Market forces, administrative folly, or a warning to others?Social Science Japan Journal, 13, 227–240. doi:10.1093/ssjj/jyp045 [Google Scholar]
- Shinjo D. & Aramaki T (2012). Geographic distribution of healthcare resources, healthcare service provision, and patient flow in Japan: A cross sectional study. Social Science & Medicine (1982), 75, 1954–1963. doi:10.1016/j.socscimed.2012.07.032 [DOI] [PubMed] [Google Scholar]
- Singer J. D., & Willett J. B (2003). Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press, USA. doi:10.1093/acprof:oso/9780195152968.003.0010 [Google Scholar]
- StataCorp (2015). Stata statistical software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- Subramanian S. V. Kubzansky L. Berkman L. Fay M. & Kawachi I (2006). Neighborhood effects on the self-rated health of elders: Uncovering the relative importance of structural and service-related neighborhood environments. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 61, S153–S160. [DOI] [PubMed] [Google Scholar]
- United Nations Population Fund (2012). Ageing in the 21st century: A celebration and a challenge. New York: United Nations Population Fund. [Google Scholar]
- Verhaeghe P. P. & Tampubolon G (2012). Individual social capital, neighbourhood deprivation, and self-rated health in England. Social Science & Medicine (1982), 75, 349–357. doi:10.1016/j.socscimed.2012.02.057 [DOI] [PubMed] [Google Scholar]
- Vogelsang E. M. & Raymo J. M (2014). Local-area age structure and population composition: Implications for elderly health in Japan. Journal of Aging and Health, 26, 155–177. doi:10.1177/0898264313504456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vuorisalmi M. Lintonen T. & Jylhä M (2006). Comparative vs global self-rated health: Associations with age and functional ability. Aging Clinical and Experimental Research, 18, 211–217. [DOI] [PubMed] [Google Scholar]
- Vuorisalmi M. Sarkeala T. Hervonen A. & Jylhä M (2012). Among nonagenarians, congruence between self-rated and proxy-rated health was low but both predicted mortality. Journal of Clinical Epidemiology, 65, 553–559. doi:10.1016/j.jclinepi.2011.11.001 [DOI] [PubMed] [Google Scholar]
- Wight R. G. Cummings J. R. Karlamangla A. S. & Aneshensel C. S (2009). Urban neighborhood context and change in depressive symptoms in late life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64, 247–251. doi:10.1093/geronb/gbn016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wight R. G. Cummings J. R. Karlamangla A. S. & Aneshensel C. S (2010). Urban neighborhood context and mortality in late life. Journal of Aging and Health, 22, 197–218. doi:10.1177/0898264309355980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao L., & Robert S (2008). The contributions of race, individual socioeconomic status, and neighborhood socioeconomic context on the self-rated health trajectories and mortality of older adults. Research on Aging, 30, 251–273. doi:10.1177/0164027507311155 [Google Scholar]