Abstract
Objectives
Frailty, an aggregate expression of risk resulting from age- or disease-associated physiologic accumulation, is responsible for large economic and societal costs. Little is known about how the context in which older adult’s live may contribute to differences in frailty. This study clarifies the role of neighborhood structural characteristics and social processes for understanding declines in health status.
Method
Data from two waves of the National Social Life, Health and Aging Project were linked to tract-level information from the 2000 Census (n = 1,925). Frailty was measured with in-home assessments and self-report. Ordered logistic regressions were employed to estimate the role of tract-level structural and social process indicators at baseline on frailty at follow-up.
Results
Living in a neighborhood characterized with a higher density of African Americans and with more residential instability was associated with higher odds of frailty. Adults in neighborhoods with increasing levels of physical disorder had higher odds of frailty (adjusted odds ratio [AOR]: 1.20, 95% confidence interval [CI]: 1.03, 1.39), while those exposed to more social cohesion had lower odds (AOR: 0.87, CI: 0.78, 0.97).
Discussion
For older adults, both neighborhood structural and social process characteristics appear to be independently associated with frailty.
Keywords: Frailty, Minority aging (race/ethnicity), Neighborhood context, Physical disorder, Social cohesion
Neighborhoods in the United States remain strongly patterned by race and class. This patterning creates vastly different local social and physical neighborhood contexts (Massey, 1993; Rugh & Massey, 2014). Despite older adults potentially increased vulnerability to their local context (Robert & Li, 2001), little is known about contextual-level risk conditions specific to developing frailty. This study investigates the role of neighborhood structural characteristics and social processes and their contribution to differences in frailty among community-dwelling older adults.
Frailty is an aggregate expression of risk resulting from age- or disease-associated physiologic accumulation, including a combination of weakness, exhaustion, weight loss, lack of physical activity, and slow walking speed (Fried et al., 2001). Frailty increases the risk for falls and disability and is responsible for substantial social and economic costs for individuals and health care systems (Clegg, Young, Iliffe, Rikkert, & Rockwood, 2013). While frailty generally accompanies increasing age, racial/ethnic minorities, women, and those with chronic disease often have accelerated rates (Fried et al., 2001; Hirsch et al., 2006; Morley, 2008; Usher et al., 2015).
Few studies document the simultaneous impact of neighborhood structural characteristics, including racial/ethnic density, socioeconomic disadvantage, and residential instability on frailty, above and beyond individual-level characteristics (Duppen, Elst, Dury, Lambotte, & Donder, 2017). Specifically, findings from studies that have examined the effect of living in a neighborhood with a higher proportion of minority residents (i.e., racial/ethnic density) and frailty have been mixed. Some show a detrimental association between Hispanic density and frailty and disability status (Beard et al., 2009; Espinoza & Hazuda, 2008), while others indicate that living in a dense Mexican American tract has a protective association with frailty (Aranda, Ray, Snih, Ottenbacher, & Markides, 2011). To our knowledge, no study considers the relationship between African American population density and frailty. Studies focused on neighborhood socioeconomic disadvantage have generally been more consistently associated with frailty (Lang et al., 2009; Lurie, Myers, Goldbourt, & Gerber, 2015). And residential instability has been found to be associated with more physical disability later in life (Beard et al., 2009). The limited number of neighborhood and frailty studies, however, can be situated within a broader body of research linking neighborhood structural inequalities to poor health and mortality risk among older adults (Beard et al., 2009; White & Borrell, 2006; Wight, Cummings, Karlamangla, & Aneshensel, 2010). Attention to neighborhood context may provide greater insight into why certain adults develop greater levels of frailty.
Social disorganization theory provides a useful frame for examining frailty in context. According to the theory, racial/ethnic density, socioeconomic disadvantage, and residential instability are key structural characteristics which may undermine a community’s ability to control behavior (i.e., informal social control) leading to social problems such as crime (Sampson, Raudenbush, & Earls, 1997; Shaw & McKay, 1969). Contemporary elaborations of social disorganization theory show that lack of informal social control may contribute to poor self-rated health, psychological distress, and hypertension (Browning & Cagney, 2002; Kim, 2010; Morenoff et al., 2007). Structural characteristics may differentially impact the health of older adults by compromising resources and social connections that are necessary to mobilize for health-enhancing environments, including health services or maintenance of recreational spaces (Cagney, Browning, & Wen, 2005). Neighborhoods with higher proportions of African American and Hispanic residents may also disproportionately experience spending cuts and political leaders may also be less likely to experience opposition when services are reduced (Massey, 1993; Williams & Collins, 2001). Residential instability or population turnover may further disrupt community social networks necessary for community organization and may lead to tensions between long time and newer residents. Residential instability has been correlated with social problems (e.g., criminal activity, loitering) which may have negative health implications (Schulz et al., 2008).
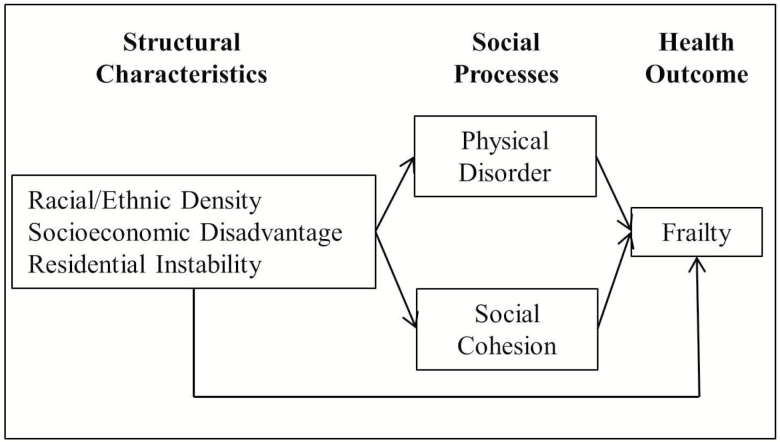
Two constructs have emerged as potentially important social processes within the neighborhood context, physical disorder (i.e., physical deterioration) and social cohesion (i.e., mutual trust and solidarity among residents) (Browning & Cagney, 2002; Echeverría, Diez-Roux, Shea, Borrell, & Jackson, 2008; Sampson & Raudenbush, 1999). Figure 1 shows the connections among these two social processes, neighborhood structural characteristics, and frailty. Below we describe possible reasons these social processes may contribute to frailty, including residents’ use of public spaces (i.e., parks), their mental health, and health behaviors.
Figure 1.
Conceptual model of neighborhood characteristics and frailty.
Physical disorder is the physical deterioration of buildings, streets, sidewalks, and other visible characteristics of a local area and is often indicative of neighborhood socioeconomic disadvantage and weak neighborhood social control (Sampson et al., 1997). The presence of problems could make residents uneasy in their own surroundings and deter them from outdoor activity (Li et al., 2005). For instance, living in a neighborhood with more physical disorder limited the extent to which older adults walk outside (Mendes de Leon et al., 2009). Restricted access to public spaces may prevent opportunities for social interaction and physical activity, which may protect against frailty. Those living in neighborhoods with worse physical features (e.g., no sidewalks, trash/litter) may also have worse health behaviors including more depressive symptoms, smoking, and drinking (Echeverría et al., 2008). Residents were found to have more overall and lower-extremity functional loss when they lived in areas with excessive noise, inadequate lighting, and heavy traffic (Balfour & Kaplan, 2002).
Social cohesion is the concept of mutual trust and solidarity among residents, and along with informal social control enhances residents’ ability to intervene on each others’ behalf beyond their own social ties (Sampson et al., 1997). Neighborhood social cohesion may discourage unhealthy behaviors and encourage health promoting behaviors and activities (Kim, Subramanian, & Kawachi, 2008) which may protect against frailty. For instance, among older adults, social cohesion had a protective association against physical disability (Beard et al., 2009). Social cohesion may also provide residents with a sense of purpose contributing to better mental health (Kawachi & Berkman, 2000). For instance, among older adults higher levels of social cohesion were positively associated with social and physical well-being (Cramm, Van Dijk, & Nieboer, 2013).
Given the documented importance of neighborhood context for understanding the health of older adults, we take a neighborhood based approach to the study of frailty, a condition that will become more common in the population due to increased life expectancy. Previous studies that examine neighborhood context and older adult health often are restricted by cross-sectional designs, are focused on select geographical regions that may lack generalizability, and do little to consider the combination of neighborhood social processes with structural characteristics. We aim to address these gaps by using two waves of data from a nationally representative survey of older adults to examine the role of neighborhood context in frailty. We hypothesize that living in a neighborhood characterized by higher racial/ethnic density, socioeconomic disadvantage, and residential instability corresponds with greater frailty. We further hypothesize that while living in a neighborhood with greater physical disorder and less social cohesion will be positively associated with frailty, the relationship between structural-level neighborhood characteristics and frailty will remain due to the uneven distribution and spatial clustering of resources and opportunities. Our study focuses on racial/ethnic density as a key structural characteristic, since residential segregation has created distinctive ecological environments that can perpetuate health disparities. By simultaneously considering racial/ethnic density with other neighborhood structural and social processes, we provide a new lens by which to understand frailty.
Methods
The National Social Life, Health, and Aging Project (NSHAP) is a longitudinal, population-based study of community-dwelling older adults conducted by NORC at the University of Chicago. The first wave of NSHAP was administered in 2005 and 2006 to a nationally representative sample of adults born between 1920 and 1947 (Wave 1 = baseline). The second wave of NSHAP was administered in 2010 and 2011 (Wave 2 = follow-up). For both waves, respondents were also administered a leave-behind-questionnaire. To obtain baseline neighborhood estimates for each NSHAP respondent, NORC facilitated linking NSHAP address data to tract-level data from the 2000 Census. NSHAP respondents who were interviewed at both waves lived in 807 census tracts across the country, with an average of 2.8 respondents per tract.
The current analysis includes Wave 1 and Wave 2. Of the original 3,005 respondents interviewed at Wave 1, we excluded 430 of respondents who died, 139 with health so poor that it restricted them from being reinterviewed, 4 who moved into a nursing home, and 171 who were lost to follow up. An additional 336 respondents were excluded because they were missing data on our dependent variable. The final analytic sample included 1,925 NSHAP respondents interviewed at both waves. Respondents who died reported higher levels of exhaustion and physical inactivity at Wave 1 (the two components of frailty assessed at baseline).
Measures
Dependent Variable
Frailty is a biologic condition of decreased reserve and resistance to stressors, resulting from cumulative declines across multiple physiologic systems. We operationalized frailty using an adapted phenotypic six-point continuum collected at follow-up, with higher values indicating greater levels of frailty (Fried et al., 2001; Huisingh-Scheetz et al., 2014). The first dimension of frailty was gait speed, a 3-m timed walk assessed by the interviewer. A point for slow gait speed was given to those requiring ≥ 5.7 s to complete the walk, were wheel chair bound, or could not complete the task. Second, the interviewer assessed the ability of the respondent to perform five sequential chair stands. A point for a slow chair stand was given to respondents that required ≥ 16.7 s to complete the task, were wheelchair bound, or could not complete the task. Third, weight loss was calculated by determining the difference in measured weight between Waves 1 and 2. A weight loss point was assigned to individuals losing 10% of their weight or more. Fourth, physical activity was assessed using a self-reported question; “on average over the last 12 months, how often have you participated in vigorous physical activity or exercise?” A point for low physical activity was given to those answering “1 to 3 times per month”, “less than 1 time per month”, or “never.” Last, presence of exhaustion was captured using two modified Center for Epidemiologic Studies Depression (CES-D) questions; how often over the last week they felt that everything was an effort and how often they felt that they could not get going. Those answering “occasionally” or “most of the time” were assigned a point for exhaustion.
By summing the points for each of the five criteria, respondents were assigned a score ranging from 0 to 5. We collapsed the outcome into three ordered categories; nonfrail (score = 0), prefrail (score = 1, 2), or frail (score = 3, 4, 5) based on recommendations (Fried et al., 2001; Huisingh-Scheetz et al., 2014). Differentiating prefrail status is important because this group is more likely to become frail in 3–4 years, when compared to those with no frailty criteria at baseline (Fried et al., 2001).
We controlled for frailty at baseline. Two dimensions of the frailty score were administered to all respondents at Wave 1: exhaustion (i.e., in the past week respondents felt occasionally or most of the time that everything was an effort or could not get “going”) and low physical activity (i.e., ≤ 1–3 times per month). We summed the points and assigned respondents a baseline frailty score ranging from 0 to 2.
Neighborhood-Level Variables
Neighborhood racial/ethnic density was created using 2000 Census data. We measured two types of density—(a) the percent Non-Hispanic African American and (b) the percent Hispanic in the respondents’ census tract. Due to their right skew, we categorized both the density variables into quartiles. For African American density, 1 = < 0.4% African American, 2 = 0.4%–2.4% African American, 3 = 2.5%–16.1% African American, and 4 = 16.2%–99.7% African American. For Hispanic density, 1 = < 1.2% Hispanic, 2 = 1.3%–3.7% Hispanic, 3 = 3.8%–11.6% Hispanic, and 4 = 11.7%–98.2%. The reference category for both density variables was the bottom quartile (“low-density”).
We created a socioeconomic disadvantage variable by calculating a composite score for each respondent at baseline. Based on a composite measure introduced by Sampson et al. (1997), we used principal components analysis to transform four variables into one component including the tract proportion of (a) individuals living below the federal poverty level, (b) households receiving public assistance, (c) population 25 years and over with a high school diploma or less, and (d) unemployed persons 16 years and over. We categorized socioeconomic disadvantage into quartiles. We captured the residential instability of the respondent’s neighborhood by using principal components analysis to transform two variables into one component including the proportion of: (a) residents who moved in the past year; and (b) nonowner occupied dwellings. Higher scores indicate greater instability. We categorized residential instability into quartiles.
We assessed two neighborhood social process characteristics: physical disorder and social cohesion. We used field interviewer’s report of the respondent’s physical environment from NSHAP at baseline to capture the immediate degree of physical disorder on each respondents’ street. Two interviewer-rated items assessed “how well kept is the building in which the respondent lives?” and “how well kept are most of the buildings on the street (1 block, both sides) where the respondent lives?” Response categories ranged from 1 = very well kept to 4 = very poorly kept (needs major repairs). Values were averaged across the two items (α = 0.76), with higher scores indicating greater physical disorder. These items draw from approaches designed for the systematic observation of neighborhood disorder (York Cornwell, 2014; Sampson & Raudenbush, 1999). We note that our two-item measure may only capture physical deterioration, when compared to more comprehensive assessments of physical disorder (e.g., trash and graffiti) (Ross & Mirowsky, 1999).
We used respondent’s report of the social environment from NSHAP to capture the degree of connectedness between neighbors in a local area (i.e., everywhere within a 20-min walk or within a mile of their home). We created a social cohesion scale by combining five items that asked respondents whether they agreed or disagreed with the following statements; “this is a close-knit area,” “people around here are willing to help their neighbors,” “people in this area generally get along with each other,” “people in this area share the same values”, and “people in this area can be trusted.” Response categories ranged from 1 = strongly disagree to 5 = strongly agree. Values were averaged across all five items (α = 0.68) with higher scores indicating greater social cohesion. While other samples of working-age adults show higher levels of internal reliability (Mujahid, Diez Roux, Morenoff, & Raghunathan, 2007), a sample of older adults showed α values of 0.71 and 0.76 (Cagney et al., 2009). The lower scale reliability may reflect greater variation in neighborhood-based challenges faced by older adults (York Cornwell & Cagney, 2014). Both neighborhood social process variables were standardized with a mean of 0 and a standard deviation of 1.
Individual-Level Variables
We controlled for several demographic characteristics at baseline. Gender was coded as female or male, and age was included as a quadratic term. Race/ethnicity was self-reported and categorized as Non-Hispanic White, Non-Hispanic African American/Black, Hispanic, or Other race. As race/ethnicity is closely associated with socioeconomic status we controlled for education at baseline (<high school degree, high school graduate or equivalent, some college, college graduate or more) and total household assets at baseline. We log transformed household assets. We included an indicator for foreign born status (yes/no) since immigrant status is associated with health (Mehta, Elo, Engelman, Lauderdale, & Kestenbaum, 2016). We categorized respondents’ living arrangements at baseline as living alone, living with one person, or living with 2 or more persons, since living alone may be detrimental to health (Dean, Kolody, Wood, & Matt, 1992).
As the development of frailty may be determined by health differences at baseline we controlled for health conditions, behaviors, and emotional health. For health conditions, we included a self-reported count of 18 possible chronic health conditions at baseline (e.g., stroke, hypertension, diabetes). We included two health behavior measures, binge drinking (four or more drinks in the last 3 months, yes/no) and current smoking status (yes/no), due to their association with developing frailty (Hubbard, Searle, Mitnitski, & Rockwood, 2009; Ortolá et al., 2016). Since better emotional health may slow the progression of frailty, we used a single-item self-reported measure of emotional health (excellent/very good, good, fair/poor) that has been found to correlate well with other measures of psychological health (Shiovitz-Ezra, Leitsch, Graber, & Karraker, 2009). And as social support can potentially slow the progression of frailty (Peek, Howrey, Ternent, Ray, & Ottenbacher, 2012), we included two measures that captured social support: “how often can you open up to friends” and “how often can you rely on them for help if you have a problem.” Response categories ranged from 1 = never to 4 = often. Lastly, to control for the length of exposure to one’s neighborhood, we included the number of years the respondent had lived in his or her neighborhood and whether the respondent moved between waves.
Analysis
We first examine the bivariate associations between neighborhood-level variables and frailty. Ordered logistic regression models test whether these neighborhood-level variables are associated with frailty 5 years later (Wave 2), adjusting for baseline frailty. While the development of frailty may be gradual, transitioning into greater frailty may be fairly common; nearly 60% of adults age 70 years and older were found to be at a different frailty state 4.5 years later (Gill, Gahbauer, Allore, & Han, 2006). As only two dimensions of the frailty measure were assessed at baseline, we could not test the association of changes in neighborhood context on changes in frailty. Worth noting however is that the neighborhood social cohesion questions were introduced only in the second wave of NSHAP (York Cornwell & Cagney, 2014).
In Model 1, we examine the neighborhood structural characteristics including African American density, Hispanic density, socioeconomic disadvantage, and residential instability, controlling for frailty at baseline and all other individual-level covariates. In Models 2 and 3, we enter physical disorder and social cohesion measures separately to test their independent association with frailty. Model 4 includes all neighborhood- and individual-level variables.
To address missing data of study covariates, we used multiple imputation with chained equations (10 imputations). While our final analytic sample excludes respondents who were missing on the outcome (n = 336), we imputed all missing covariate values using all of the study variables including the outcome. Household assets had the largest amount of missing values (24.2%). Interval regression was used to impute this variable since some respondents provided an upper and lower bound. Other variables that were administered in the leave-behind questionnaire had a larger amount of missing. These included social cohesion (15.0% missing), years lived in the neighborhood (17.0%), and foreign-born status (15.4%). We conduct all analyses with Stata version 14.0 using the survey suite of commands to account for the complex sample design, which employs sampling weights and Taylor linearized standard errors, and incorporates adjustment for primary sampling units.
Results
Our analyses examined the relationship between frailty and several neighborhood structural and social processes, with a particular focus on neighborhood racial/ethnic density. Descriptive characteristics for the sample indicate that approximately 20% of respondents self-reported as Non-Hispanic African American, Hispanic, or other race (Table 1). Over three fourths of respondents had a high school degree or higher and one fifth were living alone. At baseline, approximately 66% of respondents reported no frailty (i.e., no exhaustion and higher physical activity).
Table 1.
Characteristics of the National Social Life, Health, and Aging Project study Sample (weighted); n = 1,925
| Total % or mean (SD) | |
|---|---|
| Outcome | |
| Frailty at follow-up (Score) | |
| Nonfrail (0) | 32.9 |
| Prefrail (1, 2) | 48.7 |
| Frail (3, 4, 5) | 18.4 |
| Individual-Level (range) | |
| Female | 51.1 |
| Age (57–85) | 66.9 (7.4) |
| Race/Ethnicity | |
| Non-Hispanic White | 81.4 |
| Non-Hispanic African American | 9.4 |
| Hispanic | 6.6 |
| Other | 2.6 |
| Educational Attainment | |
| <High School | 14.5 |
| High School/Equivalent | 25.1 |
| Some College | 32.5 |
| ≥Bachelors | 27.9 |
| Household Assets (1–20,000,000) | 705,073 (16,18,027) |
| Foreign Born | 7.9 |
| Household Size | |
| Living Alone | 20.3 |
| One other | 63.2 |
| ≥2 others | 16.5 |
| Frailty Baseline (Score) | |
| Nonfrail (0) | 66.1 |
| Prefrail (1) | 28.4 |
| Frail (2) | 5.5 |
| Chronic Conditions (0–9) | 1.13 (1.5) |
| Binge Drinker | 15.4 |
| Current Smoker | 13.8 |
| Self-reported emotional health | |
| Excellent/Very Good | 68.6 |
| Good | 23.7 |
| Fair/Poor | 7.7 |
| Can rely on friends | |
| Rarely/Sometimes | 14.9 |
| Sometimes | 39.9 |
| Often | 45.2 |
| Can open up to friends | |
| Rarely/Sometimes | 26.8 |
| Sometimes | 45.6 |
| Often | 27.6 |
| Moved between waves | 21.7 |
| Residential tenure (years in neighborhood) | |
| 5 years or less | 22.4 |
| 6–25 years | 39.9 |
| 26+ years | 37.7 |
The bivariate associations between the neighborhood-level variables and frailty can be found in Table 2. Each neighborhood variable was significantly associated with frailty. Specifically, compared to older adults who lived in low-density African American tracts, those in high-density tracts had higher odds of frailty at follow-up (unadjusted odds ratio [OR]: 2.36, 95% confidence interval [CI]: 1.51, 3.68). We observed no significant difference in frailty for those living in highest versus lowest-density Hispanic tracts. Adults in highly disadvantaged and more residentially unstable tracts also had higher odds of frailty. Physical disorder was associated with higher odds of frailty (OR: 1.54, CI: 1.37, 1.75) while those exposed to higher levels of social cohesion had lower odds of frailty (OR: 0.79, CI: 0.72, 0.87).
Table 2.
Odds Ratios and 95% Confidence Intervals from Bivariate Ordered Logistic Regression of Frailty at Wave 2 on Neighborhood Characteristics, National Social Life, Health, and Aging Project (n = 1,925)
| OR | 95% CI | p | |
|---|---|---|---|
| African American Density (quartile) | |||
| 1 (Lowest) | 1.00 | ||
| 2 | 0.90 | 0.63, 1.26 | |
| 3 | 1.33 | 0.96, 1.83 | † |
| 4 (Highest) | 2.36 | 1.51, 3.68 | *** |
| Hispanic Density (quartile) | |||
| 1 (Lowest) | 1.00 | ||
| 2 | 0.73 | 0.54, 0.99 | * |
| 3 | 0.83 | 0.59, 1.17 | |
| 4 (Highest) | 1.07 | 0.77, 1.48 | |
| Disadvantage (quartile) | |||
| 1 (Lowest) | 1.00 | ||
| 2 | 1.78 | 1.27, 2.49 | *** |
| 3 | 1.83 | 1.31, 2.55 | *** |
| 4 (Highest) | 3.30 | 2.15, 5.06 | *** |
| Residential Instability (quartile) | |||
| 1 (Lowest) | 1.00 | ||
| 2 | 0.94 | 0.63, 1.42 | |
| 3 | 1.35 | 0.94, 1.94 | † |
| 4 (Highest) | 1.74 | 1.20, 2.54 | ** |
| Physical Disorder | 1.54 | 1.37, 1.75 | *** |
| Social Cohesion | 0.79 | 0.72, 0.87 | *** |
Note: OR = Odds ratio.
† p < .10; *p < .05; **p < .01; ***p < .001.
Results from the multivariate ordered logistic regression models examining frailty at follow-up can be found in Table 3. Several neighborhood-level variables remained significantly associated with frailty after controlling for all individual-level covariates. After adjustment, living in a high-density African American tract was associated with marginally higher odds of frailty when compared to those in low-density tracts (adjusted odds ratio [AOR]: 1.49, 95% confidence interval [CI]: 0.92, 2.40). We did not observe a significant association between Hispanic density and frailty. Model 2 introduces physical disorder, which was associated with higher odds of frailty (AOR: 1.21, CI: 1.04, 1.41). Model 3 introduces social cohesion, which was associated with lower odds of frailty (AOR: 0.86, CI: 0.77, 0.96). Both of social process variables remained statistically significant in the complete model (Model 4).
Table 3.
Odds Ratios and 95% Confidence Intervals from Multivariate Ordered Logistic Regression of Frailty at Wave 2 on Neighborhood Characteristics, National Social Life, Health, and Aging Project (n = 1,925)
| Model 1 | Model 2 | Model 3 | Model 4 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| African American Density (ref = lowest quartile) | ||||||||||||
| 2 | 0.90 | 0.64, 1.26 | 0.91 | 0.65, 1.28 | 0.89 | 0.63, 1.25 | 0.90 | 0.64, 1.27 | ||||
| 3 | 1.20 | 0.86, 1.65 | 1.20 | 0.88, 1.65 | 1.18 | 0.84, 1.64 | 1.19 | 0.86, 1.64 | ||||
| Highest | 1.49 | 0.92, 2.40 | † | 1.54 | 0.93, 2.54 | † | 1.46 | 0.90, 2.36 | 1.51 | 0.91, 2.49 | † | |
| Hispanic Density (ref = lowest quartile) | ||||||||||||
| 2 | 0.98 | 0.71, 1.36 | 0.98 | 0.72, 1.35 | 0.99 | 0.71, 1.37 | 0.99 | 0.72, 1.36 | ||||
| 3 | 0.86 | 0.64, 1.15 | 0.84 | 0.63, 1.13 | 0.87 | 0.64, 1.17 | 0.85 | 0.63, 1.15 | ||||
| Highest | 1.10 | 0.78, 1.55 | 1.11 | 0.80, 1.56 | 1.09 | 0.78, 1.54 | 1.11 | 0.80, 1.54 | ||||
| Disadvantage (ref = lowest quartile) | ||||||||||||
| 2 | 1.37 | 0.99, 1.89 | † | 1.32 | 0.96, 1.82 | † | 1.38 | 1.00, 1.92 | * | 1.34 | 0.97, 1.85 | * |
| 3 | 1.19 | 0.88, 1.60 | 1.11 | 0.82, 1.50 | 1.20 | 0.89, 1.62 | 1.12 | 0.83, 1.52 | ||||
| Highest | 1.26 | 0.82, 1.92 | 1.13 | 0.73, 1.73 | 1.26 | 0.82, 1.93 | 1.13 | 0.73, 1.75 | ||||
| Residential Instability (ref = lowest quartile) | ||||||||||||
| 2 | 1.09 | 0.77, 1.54 | 1.10 | 0.79, 1.54 | 1.07 | 0.76, 1.52 | 1.09 | 0.78, 1.52 | ||||
| 3 | 1.39 | 1.00, 1.92 | * | 1.38 | 1.01, 1.90 | * | 1.36 | 0.97, 1.89 | † | 1.35 | 0.98, 1.87 | † |
| Highest | 1.65 | 1.16, 2.36 | ** | 1.64 | 1.15, 2.33 | ** | 1.61 | 1.12, 2.30 | ** | 1.59 | 1.11, 2.28 | ** |
| Physical Disorder | - | - | 1.21 | 1.04, 1.41 | ** | - | - | 1.20 | 1.03, 1.39 | * | ||
| Social Cohesion | - | - | - | - | 0.86 | 0.77, 0.96 | ** | 0.87 | 0.78, 0.97 | ** | ||
Note: Regressions employ Wave 1 weights to account for complex survey design. All models control for respondents’ gender, age, age2, race/ethnicity, education, W1 household assets (logged), foreign born status, W1 household size, W1 frailty proxy, W1 chronic conditions, W1 binge drinker, W1 current smoker, W1 emotional health, W1 can rely on friends, W1 can open up to friends, moved between waves, W1 residential tenure. Coefficients for the individual-level variables can be found in Supplementary Table 1. OR = Odds ratio.
† p < .10; *p < .05; **p < .01; ***p < .001.
In sensitivity analyses, we investigated whether results differed by the specification of the neighborhood racial/ethnic density variables. When analyzed continuously, both the African American and Hispanic density variables were associated with marginally higher odds of frailty (p < .10) in the multivariate models. We also explored cross-level interactions between individual-level race/ethnicity and the racial/ethnic density variables, but are cautious about these results due to small samples in some cells (i.e., Hispanics who live in the lowest density Hispanic tracts). Future studies would benefit from sampling respondents across a wider distribution of percent African American and Hispanic in the tract.
Discussion
This study investigated experiences of frailty over a five-year period using a nationally representative sample of community-dwelling older adults. Drawing from social disorganization theory and its contemporary elaborations for understanding health (Browning & Cagney, 2002; Kim, 2010; Morenoff et al., 2007), we found evidence that accounting for neighborhood structural and social processes are necessary to understanding differences in frailty. In our study, adults who lived in high-density versus low-density African American tracts were more frail over time. And those in the most residentially unstable neighborhoods had worse health at follow-up. Further, frailty was higher among those exposed to more physically disordered and less socially cohesive environments.
Older adults had more frailty when they lived in neighborhoods characterized by having more African American residents, although this relationship was marginally significant. To our knowledge, no study of frailty has produced these results using a national sample of older adults. This health disadvantage can be somewhat expected given the broader body of research showing that older adults have more disability and worse health when they live in tracts with a higher density of African Americans (Beard et al., 2009; White & Borrell, 2006; Wight et al., 2010). Older adults may do worse in these neighborhoods given the historical and current realities of residential segregation that continue to restrict educational and employment opportunities and concentrate poverty (Massey, 1993). Studies show that areas with higher proportions of racial/ethnic minority residents have fewer recreational facilities and health-related destinations that can be reached by foot, potentially restricting ones’ ability to walk (Lovasi, Neckerman, Quinn, Weiss, & Rundle, 2009; Smiley et al., 2010). Racial/ethnic density may also compromise certain social processes that are necessary to maintain and improve access to public resources and future investments by political leaders (Williams & Collins, 2001). In contrast, our findings provide little support for an association between Hispanic density and frailty, possibility highlighting the mixed findings of past studies on Hispanic density and frailty (Aranda et al., 2011; Espinoza & Hazuda, 2008). However, in subsequent analyses when Hispanic density was analyzed continuously, results suggested a detrimental association with frailty. This difference in results may underscore concerns raised about the specification of neighborhood racial/ethnic density variables and whether more formal measures of segregation better capture the complex processes of racial inequality (Kramer, Cooper, Drews-Botsch, Waller, & Hogue, 2010).
In addition to racial/ethnic density, residential instability appeared particularly problematic for the health of older adults. This finding aligns with research showing that residents of areas with higher levels of residential instability are more likely to be strangers and are less likely to be embedded in social networks that are necessary for the exchange of information and resources (Sampson et al., 1997). Specific to older adults, one study found that when neighborhoods seem unfamiliar and unstable, older residents had a higher likelihood of a physical disability and difficulty going outside alone to shop or to visit a doctor (Beard et al., 2009). A withdrawal from public space may compromise key opportunities for social interaction and physical activity that can protect against frailty. Withdrawal from public space may also further compromise the social processes needed at the neighborhood-level to effectively manage neighborhood conditions.
Our findings confirmed that local neighborhood social processes, as captured through physical disorder and social cohesion, may affect the health of older adults. Specifically, visible signs of physical disorder of the immediate street and buildings could lead to unhealthy coping behaviors. For instance, one study found that middle-aged and older adults had higher rates of depressive symptoms, smoking, and drinking when they lived in neighborhoods with more problems including heavy traffic or lack of parks (Echeverría et al., 2008). Physical disorder may also be a deterrent for leaving the house among older adults (Beard et al., 2009).
Higher levels of social cohesion appeared to have a protective association with frailty. This may be because socially cohesive neighborhoods promote feelings of responsibility for safety and the livability of the neighborhood. One study found that adults living in more socially cohesive neighborhoods had lower levels of depressive symptoms and smoking, and walked more for exercise (Echeverría et al., 2008). These health behaviors could reduce levels of obesity and premature development of chronic diseases, both of which are important contributors to frailty (Ferraro & Kelley-Moore, 2003). However, it is concerning that racial/ethnic segregation and the concentration of poverty can weaken neighborhood social cohesion. “Equalizing” exposure to socially cohesive environments could mitigate some social differences in health at older ages. One study of older adults suggests that social cohesion can buffer against the effect of being poor on lower reports of well-being (Cramm et al., 2013).
A strength of our study is the use of a high-quality nationally representative sample in which we incorporated measures of the older adult’s immediate physical and social environment. Our findings help clarify how unequal exposure to neighborhood structural and social processes are critical to understanding frailty, an increasing reality for a greater proportion of adults with longer life expectancy. Another strength is that we used longitudinal models to assess the associations between several neighborhood characteristics and frailty. Such an approach potentially reduces the risk of reverse causality incurred by cross-sectional analysis. However, only two components of the frailty measure were assessed at baseline. Future research should examine multiple waves of data with consistent measurement of frailty.
Our study has a number of limitations. First, our use of census tracts are a crude proxy for the environment, because we know people spend time in other neighborhoods apart from their own. Second, while we can better establish temporal ordering by examining baseline predictors on frailty at follow-up, our measure of social cohesion was only administered at follow-up. Recognizing that neighborhoods may undergo change, we expect that experiences of social cohesion remained relatively stable (Sampson, 2012). Third, selection is a key issue for studies that link neighborhoods to health. Persons may select into neighborhoods based on individual attributes that are related to health. Lastly, we may underestimate the effect of neighborhood context on health since we could expect that the worst off did not survive between the waves.
This study provides evidence that neighborhood structural characteristics and social processes contribute to the development of frailty. Independent of individual-level factors, racial/ethnic density may produce unequal health disadvantages for older adults. With nearly one-third of older adults living in the same residence for more than 30 years (Bryan & Morrison, 2004), future studies would benefit from examining neighborhood context over time. Urban planning advancements that facilitate the opportunity to spend more time outdoors and which encourage social interaction are critical to helping older adults stay in their communities for the longest possible time.
Supplementary Material
Supplementary data is available at The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences online.
Funding
This work was supported by the Agency for Healthcare Research and Quality (4T32-HS78-18) and the National Institutes of Health, including the National Institute on Aging (32AG000243; P30AG012857).
Author Contributions
J. T. Caldwell led the conceptualization of the study, analysis of the data, and writing of the manuscript. H. Lee and K. Cagney assisted in conceptualizing the study, interpretation of results, and editing of the manuscript.
Conflict of Interest
None reported.
Supplementary Material
Acknowledgments
The authors thank NORC at the University of Chicago for providing access to the National Social Life, Health, and Aging Project.
References
- Aranda M. P., Ray L. A., Snih S. A., Ottenbacher K. J., & Markides K. S (2011). The protective effect of neighborhood composition on increasing frailty among older Mexican Americans: A barrio advantage?Journal of Aging and Health, 23, 1189–1217. doi:10.1177/0898264311421961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balfour J. L., & Kaplan G. A (2002). Neighborhood environment and loss of physical function in older adults: Evidence from the Alameda County Study. American Journal of Epidemiology, 155, 507–515. doi:10.1093/aje/155.6.507 [DOI] [PubMed] [Google Scholar]
- Beard J. R., Blaney S., Cerda M., Frye V., Lovasi G. S., Ompad D., … Vlahov D (2009). Neighborhood characteristics and disability in older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64, 252–257. doi:10.1093/geronb/gbn018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browning C. R., & Cagney K. A (2002). Neighborhood structural disadvantage, collective efficacy, and self-rated physical health in an urban setting. Journal of Health and Social Behavior, 43, 383–399. doi:10.2307/3090233 [PubMed] [Google Scholar]
- Bryan T. M., & Morrison P. A (2004). New approaches to spotting enclaves of the elderly who have aged in place. Unpublished manuscript presented at 2004 Population Association of America Annual Meeting.. [Google Scholar]
- Cagney K. A., Browning C. R., & Wen M (2005). Racial disparities in self-rated health at older ages: What difference does the neighborhood make?The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 60, S181–S190. doi:10.1093/geronb/60.4.S181 [DOI] [PubMed] [Google Scholar]
- Cagney K. A., Glass T. A., Skarupski K. A., Barnes L. L., Schwartz B. S., & Mendes de Leon C. F (2009). Neighborhood-level cohesion and disorder: Measurement and validation in two older adult urban populations. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64, 415–424. doi:10.1093/geronb/gbn041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clegg A., Young J., Iliffe S., Rikkert M. O., & Rockwood K (2013). Frailty in elderly people. Lancet (London, England), 381, 752–762. doi:10.1016/S0140-6736(12)62167-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramm J. M., van Dijk H. M., & Nieboer A. P (2013). The importance of neighborhood social cohesion and social capital for the well being of older adults in the community. The Gerontologist, 53, 142–152. doi:10.1093/geront/gns052 [DOI] [PubMed] [Google Scholar]
- Dean A., Kolody B., Wood P., & Matt G. E (1992). The influence of living alone on depression in elderly persons. Journal of Aging and Health, 4, 3–18. doi:10.1177/089826439200400101 [Google Scholar]
- Duppen D., Elst M. C. J. V. D., Dury S., Lambotte D., & Donder L. D (2017). The social environment’s relationship with frailty. Journal of Applied Gerontology, 1–24. doi:10.1177/0733464816688310 [DOI] [PubMed] [Google Scholar]
- Echeverría S., Diez-Roux A. V., Shea S., Borrell L. N., & Jackson S (2008). Associations of neighborhood problems and neighborhood social cohesion with mental health and health behaviors: The Multi-Ethnic Study of Atherosclerosis. Health & Place, 14, 853–865. doi:10.1016/j.healthplace.2008.01.004 [DOI] [PubMed] [Google Scholar]
- Espinoza S. E., & Hazuda H. P (2008). Frailty in older Mexican-American and European-American adults: Is there an ethnic disparity?Journal of the American Geriatrics Society, 56, 1744–1749. doi:10.1111/j.1532-5415.2008.01845.x [DOI] [PubMed] [Google Scholar]
- Ferraro K. F., & Kelley-Moore J. A (2003). Cumulative disadvantage and health: Long-term consequences of obesity?American Sociological Review, 68, 707–729. [PMC free article] [PubMed] [Google Scholar]
- Fried L. P., Tangen C. M., Walston J., Newman A. B., Hirsch C., Gottdiener J., … Burke G; Cardiovascular Health Study Collaborative Research Group (2001). Frailty in older adults: Evidence for a phenotype. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 56, M146–M156. doi:10.1093/gerona/56.3.M146 [DOI] [PubMed] [Google Scholar]
- Gill T. M., Gahbauer E. A., Allore H. G., & Han L (2006). Transitions between frailty states among community-living older persons. Archives of Internal Medicine, 166, 418–423. doi:10.1001/archinte.166.4.418 [DOI] [PubMed] [Google Scholar]
- Hirsch C., Anderson M. L., Newman A., Kop W., Jackson S., Gottdiener J., … Fried L. P; Cardiovascular Health Study Research Group (2006). The association of race with frailty: The cardiovascular health study. Annals of Epidemiology, 16, 545–553. doi:10.1016/j.annepidem.2005.10.003 [DOI] [PubMed] [Google Scholar]
- Hubbard R. E., Searle S. D., Mitnitski A., & Rockwood K (2009). Effect of smoking on the accumulation of deficits, frailty and survival in older adults: A secondary analysis from the Canadian Study of Health and Aging. The Journal of Nutrition, Health & Aging, 13, 468–472. doi:10.1007/s12603-009-0085-y [DOI] [PubMed] [Google Scholar]
- Huisingh-Scheetz M., Kocherginsky M., Schumm P. L., Engelman M., McClintock M. K., Dale W., … Waite L (2014). Geriatric syndromes and functional status in nshap: Rationale, measurement, and preliminary findings. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(Suppl. 2), S177–S190. doi:10.1093/geronb/gbu091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawachi I., & Berkman L (2000). Social cohesion, social capital, and health. In Berkman L., & Kawachi I. (Eds.), Social epidemiology (pp. 174–190). New York, NY: Oxford University Press, Inc. [Google Scholar]
- Kim D., Subramanian S., & Kawachi I (2008). Social capital and physical health: A systematic review of the literature Social capital and health (pp. 139–190). New York: Springer-Verlag. [Google Scholar]
- Kim J. (2010). Neighborhood disadvantage and mental health: The role of neighborhood disorder and social relationships. Social Science Research, 39, 260–271. doi:10.1016/j.ssresearch.2009.08.007 [Google Scholar]
- Kramer M. R., Cooper H. L., Drews-Botsch C. D., Waller L. A., & Hogue C. R (2010). Do measures matter? Comparing surface-density-derived and census-tract-derived measures of racial residential segregation. International Journal of Health Geographics, 9, 29. doi:10.1186/1476-072X-9-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang I. A., Hubbard R. E., Andrew M. K., Llewellyn D. J., Melzer D., & Rockwood K (2009). Neighborhood deprivation, individual socioeconomic status, and frailty in older adults. Journal of the American Geriatrics Society, 57, 1776–1780. doi:10.1111/j.1532-5415.2009.02480.x [DOI] [PubMed] [Google Scholar]
- Li F., Fisher K. J., Bauman A. et al. (2005). Neighborhood influences on physical activity in middle-aged and older adults: A multilevel perspective. Journal of Aging and Physical Activity, 13, 87–114. doi:10.1123/japa.13.1.87 [DOI] [PubMed] [Google Scholar]
- Lovasi G. S., Neckerman K. M., Quinn J. W., Weiss C. C., & Rundle A (2009). Effect of individual or neighborhood disadvantage on the association between neighborhood walkability and body mass index. American Journal of Public Health, 99, 279–284. doi:10.2105/AJPH.2008.138230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lurie I., Myers V., Goldbourt U., & Gerber Y (2015). Perceived social support following myocardial infarction and long-term development of frailty. European Journal of Preventive Cardiology, 22, 1346–1353. doi:10.1177/2047487314544575 [DOI] [PubMed] [Google Scholar]
- Massey D. S., Denton N. A (1993). American apartheid segregation and the making of the underclass. Cambridge, MA: Harvard University Press. [Google Scholar]
- Mehta N. K., Elo I. T., Engelman M., Lauderdale D. S., & Kestenbaum B. M (2016). Life expectancy among U.S.-born and foreign-born older adults in the United States: Estimates from linked social security and medicare data. Demography, 53, 1109–1134. doi:10.1007/s13524-016-0488-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon C. F., Cagney K. A., Bienias J. L., Barnes L. L., Skarupski K. A., Scherr P. A., & Evans D. A (2009). Neighborhood social cohesion and disorder in relation to walking in community-dwelling older adults a multilevel analysis. Journal of Aging and Health, 21, 155–171. doi:10.1177/0898264308328650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morenoff J. D., House J. S., Hansen B. B., Williams D. R., Kaplan G. A., & Hunte H. E (2007). Understanding social disparities in hypertension prevalence, awareness, treatment, and control: The role of neighborhood context. Social science & medicine (1982), 65, 1853–1866. doi:10.1016/j.socscimed.2007.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morley J. E. (2008). Diabetes, sarcopenia, and frailty. Clinics in Geriatric Medicine, 24, 455–69, vi. doi:10.1016/j.cger.2008.03.004 [DOI] [PubMed] [Google Scholar]
- Mujahid M. S., Diez Roux A. V., Morenoff J. D., & Raghunathan T (2007). Assessing the measurement properties of neighborhood scales: From psychometrics to ecometrics. American Journal of Epidemiology, 165, 858–867. doi:10.1093/aje/kwm040 [DOI] [PubMed] [Google Scholar]
- Ortolá R., García-Esquinas E., León-Muñoz L. M., Guallar-Castillon P., Valencia-Martin J. L., Galan I., & Rodriguez-Artalejo F (2016). Patterns of alcohol consumption and risk of frailty in community-dwelling older adults. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 71, 251–258. doi:10.1093/gerona/glv125 [DOI] [PubMed] [Google Scholar]
- Peek M. K., Howrey B. T., Ternent R. S., Ray L. A., & Ottenbacher K. J (2012). Social support, stressors, and frailty among older Mexican American adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67, 755–764. doi:10.1093/geronb/gbs081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert S. A., & Li L. W (2001). Age variation in the relationship between community socioeconomic status and adult health. Research on Aging, 23, 234–259. doi:10.1177/0164027501232005 [Google Scholar]
- Ross C. E., & Mirowsky J (1999). Disorder and decay. Urban Affairs Review, 34, 412–432. doi:10.1177/107808749903400304 [Google Scholar]
- Rugh J. S., & Massey D. S (2014). Segregation in post-civil rights america. Du Bois Review: Social Science Research on Race, 11, 205–232. doi:10.1017/S1742058X13000180 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson R. J. (2012). Great american city: Chicago and the enduring neighborhood effect. Chicago, IL: University of Chicago Press. [Google Scholar]
- Sampson R. J., & Raudenbush S. W (1999). Systematic social observation of public spaces: A new look at disorder in urban neighborhoods. American Journal of Sociology, 105, 603–651. doi:10.1086/210356 [Google Scholar]
- Sampson R. J., Raudenbush S. W., & Earls F (1997). Neighborhoods and violent crime: A multilevel study of collective efficacy. Science (New York, N.Y.), 277, 918–924. doi:10.1126/science.277.5328.918 [DOI] [PubMed] [Google Scholar]
- Schulz A. J., Zenk S. N., Israel B. A., Mentz G., Stokes C., & Galea S (2008). Do neighborhood economic characteristics, racial composition, and residential stability predict perceptions of stress associated with the physical and social environment? Findings from a multilevel analysis in Detroit. Journal of Urban Health: bulletin of the New York Academy of Medicine, 85, 642–661. doi:10.1007/s11524-008-9288-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw C. R., & McKay H. D (1969). Juvenile delinquency and urban areas. Chicago, IL: University of Chicago Press. [Google Scholar]
- Shiovitz-Ezra S., Leitsch S., Graber J., & Karraker A (2009). Quality of life and psychological health indicators in the national social life, health, and aging project. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 64(Suppl. 1), i30–i37. doi:10.1093/geronb/gbn020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smiley M. J., Diez Roux A. V., Brines S. J., Brown D. G., Evenson K. R., & Rodriguez D. A (2010). A spatial analysis of health-related resources in three diverse metropolitan areas. Health & Place, 16, 885–892. doi:10.1016/j.healthplace.2010.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Usher T., Thorpe R., Huang J., Samuel L., Kasper J., & Bandeen-Roche K (2015). Dissecting the race disparity in frailty in nhats by income, region, and obesity. The Gerontologist, 55(Suppl. 2), 600. doi:10.1093/geront/gnv311.03 [Google Scholar]
- White K., & Borrell L. N (2006). Racial/ethnic neighborhood concentration and self-reported health in New York City. Ethnicity & Disease, 16, 900–908. [PubMed] [Google Scholar]
- Wight R. G., Cummings J. R., Karlamangla A. S., & Aneshensel C. S (2010). Urban neighborhood context and mortality in late life. Journal of Aging and Health, 22, 197–218. doi:10.1177/0898264309355980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D. R., & Collins C (2001). Racial residential segregation: A fundamental cause of racial disparities in health. Public Health Reports (Washington, D.C.: 1974), 116, 404–416. doi:10.1093/phr/116.5.404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- York Cornwell E. (2014). Social resources and disordered living conditions evidence from a national sample of community-residing older adults. Research on Aging, 36, 399–430. doi:10.1177/0164027513497369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- York Cornwell E., & Cagney K. A (2014). Assessment of neighborhood context in a nationally representative study. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(Suppl. 2), S51–S63. doi:10.1093/geronb/gbu052 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.