Cardiovascular diseases (CVD) is a major threat to human health and the leading cause of death worldwide.[1] The incidence of CVD caused 17.6 million deaths in 2016, an increase of 14.5% from 2006 to 2016.[2] Unfortunately, the mortality and morbidity rates of CVD are increasing year by year, especially in developing regions. Studies have shown that approximately 80% of CVD-related deaths occur in low- and middle-income countries. Besides, these deaths occur at a younger age than in high-income countries.[3]
In developing countries, rapid economic transformation leads to environmental changes and unhealthy lifestyles; in addition, population ageing may increase cardiovascular risk factors and increase the incidence of CVD.[4] CVD has placed a heavy burden on patients and society as a whole. Therefore, it is necessary to provide strategies for improving the diagnosis and treatment of CVD in the future. Currently, artificial intelligence (AI) may have the potential to solve this problem. However, it has been more than sixty years since the introduction of the concept of AI. The application of AI in medicine is still unclear. Furthermore, the role of AI in medicine in the future? Whether it will lead to a large number of unemployed clinicians due to the development of AI technology, the current research results cannot provide an answer. This article attempts to make a brief review of the current state of AI in clinical applications based on available information based on the following six themes.
1. What is AI?
2. The value of medical AI.
3. The application of AI in CVD.
4. Future prospect.
5. Current shortcomings.
6. Possible solution—“the primary use of AI” and a novel medical model.
1. What is AI?
AI, also known as machine intelligence, can be defined as a branch of computer science that mimics the human mind process.[5] It was first proposed by Alan Mathison Turing more than sixty years ago. According to the Turing test, if a human being could not distinguish whether a machine's responses are from a machine or a human, then the machine could be considered “intelligent”.[6] Although Turing proposed the idea of AI in 1950, the definition of AI is still unclear. At present, no one has explained the exact concept of AI; we only know that AI is a kind of computer science, is multidisciplinary in theory and practice, and AI can improve the quality of our lives.
Although the specific definition of AI is still controversial, many researchers are still optimistic about the future of AI and believe that it will have a profound influence on society, but also beneficial to everyone.[7] In the medical field, AI is likely to be implemented in the fields of medical diagnosis, treatment, risk prediction, clinical care and drug discovery.[8] Moreover, the application of AI in medicine is accelerating at an impressive rate. AI technologies mainly include machine learning, cognitive computing and big data analytics.
1.1. Machine learning (the hotspot of AI)
One of the most popular technologies of AI is called machine learning, which enables algorithms to understand and learn data. In fact, machine learning is usually synonymous with AI. Additionally, the key of machine learning is to find the regular pattern behind an observed data and build a model based on that data. Therefore, the machine can use this model to predict and determine future data.[9] Besides, machine learning can be categorized into supervised learning, unsupervised learning and reinforcement learning, depending on the amount and type of supervision that the algorithms receive during training.
1.2. Three classic genres of machine learning
Supervised learning plays an important role not only in the operation of many biological networks but also plays an important role in the operation of artificial neural networks.[10] Moreover, supervised learning has been widely applied and can solve any problem. In supervised learning, manually set labels to help the machine achieve the desired results. Therefore, supervised learning is applicable to medical diagnosis and treatment, and has clear clinical guiding significance.
In contrast, the unsupervised learning data set does not have a given label, which means that the machine must find the label itself. Furthermore, unsupervised learning algorithms have been successfully implemented in problems such as CVD prediction, diagnosis and treatment, and cardiovascular image analysis.[5]
Reinforcement learning has two different characteristics. First, there is no need to complete the proposed goals. Humans propose a goal and require AI to achieve this goal through supervised learning and unsupervised learning.
After that, there is a feedback mechanism, often described as a ‘reward’.[11] The aim of reinforcement learning is not to reach the proposed goal, but to maximize the reward for the model during the learning process. This reinforcement learning has been deployed in intensive care units (ICU) to optimize the process of patients off of mechanical ventilation.[12]
1.3. The next step of machine learning-deep learning
In recent years, Geoffrey Hinton has proposed deep learning and quickly became a hot topic in the field of AI. Deep learning is a subset of machine learning that can be described as the next generation of machine learning.[13],[14] It is a computational method that enables the algorithm to automatically program and learns from big data.[8] The purpose of deep learning is to train the artificial neural network,[8] which is composed of artificial neurons, or nodes. So far, it has made significant breakthroughs in the processing of image, video, voice and audio data.[15] In general, deep learning is very powerful and is especially suitable for medical imaging or radiology. When considering AI or machine learning, it is not known what practical medical value these systems have.
2. The value of medical AI
In general, governments and authorities around the world have developed and implemented laws and regulations to establish a better medical environment for patients. The current medical system still has many shortcomings, including uneven distribution of senior clinicians, high rate of misdiagnosis of primary clinicians, long training period for clinicians, shortage of clinicians in undeveloped areas, and high medical expenses for patients.
However, with the development and advancement of machine learning technology in recent years, AI has gradually changed from theory to practicality. The multiple applications of AI in medicine are being proven. Additionally, AI technology has become an important factor that may affect the development of the medical industry and may improve the level of medical services.
AI has several applications in the medical field. Firstly, AI can help clinicians diagnose disease and optimize treatment processes. After being applied to traditional medical procedures, AI can reduce the rate of misdiagnosis and improve diagnostic efficiency. Then, with the advent of deep learning, AI has the ability to recognize medical images and provide clinicians with more reliable imaging diagnostic information. Thirdly, by using big data analysis (AI can analyze extremely large data sets that are difficult to analyze by traditional data processing methods),[5] AI algorithms can often provide more accurate results for patient prediction. AI can also help support drug research and improve the efficiency of new drug development. Finally, the combination of AI and surgical robots will improve the accuracy of many complex and difficult operations. With the development of AI, big data analysis and cloud computing technologies, AI can provide patients with high quality medical services. Besides, AI will enhance the advancement of smart medical and precision medicine, which will reduce patient waiting time and cost, and obtain safe, convenient and high quality medical services. Therefore, the implementation of deep learning of AI will benefit cardiovascular medicine.
3. The application of AI in CVD
As mentioned above, AI has been around for a long time. At present, AI technologies have been applied in cardiovascular medicine including precision medicine, clinical prediction, cardiac imaging analysis and intelligent robots. There are optimistic prospects of the use of AI in cardiovascular medicine.
3.1. Precision medicine
From the patient aspect, AI can be initially applied for remote follow-ups, medication reminders, real-time disease counseling and early warnings of symptoms. At the same time, from the perspective of clinicians, AI can help collect voice information (such as medical history), connect electronic medical records systems and reduce the workload of clinicians.[11] In the future, cognitive computers (devices that are trained through machine learning or deep learning algorithms and can solve problems without human assistance) will help clinicians make accurate decisions and predict patient outcomes. With the help of AI, it is most likely to implement an accurate medical plan that customizes healthcare for each patient. People think that AI will not replace clinicians. In contrast, clinicians should know how to use AI technology and gain experience in the clinical practice of applying AI to improve cardiovascular disease diagnosis and treatment by analyzing big data. Will help enter the era of precision medicine. Precision medicine will customize healthcare for each individual patient, is most likely to be achieved with the help of AI. It is thought that AI will not replace clinicians.
3.2. Clinical predictions
Through machine learning and big data analytics, AI can help clinicians to make more accurate predictions for patients. Research from Dawes TJW suggests that AI can predict possible time periods of death for heart disease patients.[16] In their research, AI software recorded the results of cardiac magnetic resonance imaging (MRI) scans and blood tests of 256 heart disease patients. The software measured the movement of 30,000 points that are marked on the heart structures in each heartbeat. By combining these data with the patients' eight-year health records, AI could predict the abnormal conditions that will lead to patient death. Additionally, their software was able to predict the survival rates of patients for the next five years, and the prediction accuracy of the next year survival of patients could easily reach 80%. However, the prediction accuracy of the clinicians was only 60%. Furthermore, Motwani M and his colleagues established a predictive model through the use of deep learning, in order to evaluate the risk of death for the next five years, for 10,030 suspected coronary heart disease (CHD) patients. Their results indicated that the risk assessment based on AI is superior to traditional clinical judgement and coronary computed tomographic angiography.[17]
3.3. Cardiac imaging analysis
In recent years, with the advent of deep learning, cardiac imaging analysis has shown great development prospects. Deep learning can help to analyze coronary angiography, echocardiography and electrocardiogram (ECG). Cardiac intervention has been the main treatment for cardiovascular disease in recent decades, including CHD and acute coronary syndrome (ACS). In the near future, by using deep learning, AI can identify coronary atherosclerotic plaques more accurately than clinicians. In addition, AI can also be used to analyze echocardiographic images, including automatic measurement of the size of each chamber and assessment of left ventricular function. Moreover, it can be used to assess structural diseases, such as valvular disease, to help determine the classification and staging of the disease.
Rima Arnaout, an assistant professor at the University of California, San Francisco, built convolutional neural networks by using the echocardiographies of 267 randomized patients (age range: 20–96 years) between 2000 and 2017 from the university medical center. From the perspective, 223,000 images were divided into fifteen categories. Furthermore, this classification algorithm has outperformed the human cardiovascular physicians in the classification competition of cardiac ultrasound images.[18] Another study from Samad, et al.[19] demonstrated that deep learning can predict survival with higher accuracy after analyzing echocardiography of multiple cases. Other applications of AI in cardiac imaging analysis include intravascular ultrasound (for the detection of the border of the lumen and the media-adventitia),[20] optical coherence tomography (for the classification of the three layers of the coronary artery),[21] cardiac single-photon emission computed tomography (for the diagnosis of myocardial ischemia[22] and for the improvement of the diagnostic accuracy of myocardial perfusion imaging)[23] and MRI (for the efficient and fast visualization of the cardiac segmentation in short-axis MRI).[24] As is well known, cardiovascular imaging is one of the most significant standards for the diagnosis of CVD. In the future, deep learning will make imaging diagnostics more reliable, easier and faster to obtain results.
3.4. Intelligent robots
With the advent of surgical robots, the machine has been able to help clinicians perform bladder replacement surgery and hysteromyoma resection.[25],[26] In the future, the combination of AI and minimally invasive surgery technology, such as the Da Vinci Surgical Robot, can make the use of automated surgery more realistic, which will reduce trauma to patient, improve surgical safety and shorten hospital stays. Moreover, with this kind of combination, instead of clinicians, AI can perform cardiac interventional operations, such as percutaneous coronary intervention (PCI) operations and catheter ablations of atrial fibrillation, on patients; which will reduce the radiation exposure for the clinicians from the use of digital subtraction angiography. With the use of reinforcement learning, the ability of AI will be far superior to that of a human being, especially for uses in repetition drills. Thus, the AI will learn how to more quickly perform operations than human clinicians. Altogether, the combined use of AI and surgical robots will promote the revolution of traditional medicine.
4. Future prospect
AI is the next step in cardiovascular medicine practice. The integration of AI and cardiovascular medicine requires professional skills, advanced technologies and substantial investment. Therefore, in the near future, AI projects are most likely to be conducted by large technology corporations such as Apple, Google and Microsoft, which have invested heavily in AI to improve the productivity of clinical staff. Last year, Apple and Stanford launched a project called “Apple Heart Study” with the help of machine learning. In addition, the development of sensor technology has furthered the application of AI in cardiovascular medicine. The latest Apple watch series 4 has a new transducer that measure ECG. This new feature has been approved by the US Food and Drug Administration (FDA). In early 2018, scientists from Verily (Google Life Sciences-Alphabet Inc.'s research organization) used machine learning to assess the risk of a patient suffering from cardiovascular disease. They successfully developed an algorithm to analyze the scanned image of the patient's eye, then accurately inferred various types of data, including the patient's age, blood pressure and smoking status. Consequently, this allowed the scientists to predict the patient's risk of cardiovascular disease. To train the algorithm, they used machine learning to analyze the medical data of nearly 300,000 patients. As a result, the accuracy of the algorithm in identifying patients with cardiovascular disease was as high as 70%, which is close to the accuracy of traditional cardiovascular disease risk prediction methods, such as the measurement of blood cholesterol levels.[27] Furthermore, Microsoft recently announced that they are going to cooperate with Apollo Hospital in India in writing algorithms to help clinicians in predicting the risk factors for CVD. On January 9, 2017, the FDA gave clearance for the use of a cardiac MRI analysis software called Cardio DL (from Arterys), which uses deep learning for medical image analysis and provides automated ventricular segmentation for traditional cardiac MRI scans. By using cloud computing, Cardio DL can automatically complete image processing in less than 10 seconds, and can draw the outline of the ventricular epicardium and subcardium, so as to accurately evaluate the function of the ventricle.[28] Siemens has built a large database of more than 250 million related images, reports, surgical data and other materials for training its AI calculation programs. A team of cardiologists at the University Hospital of Heidelberg conducted a six-year trial. They used data from patients with heart failure to generate 100 digitally simulated hearts and used AI to predict the prognosis of these patients, and then compared the predicted results with the actual situation of the patients. Clinicians can even use 3D printing technology to create models of the heart, in order to develop a more appropriate treatment.
All these data suggest that a major revolution in the clinical application of AI in cardiovascular medicine (analogous to a Cambrian explosion) may occur soon, and this application is only the beginning of the overall use of AI.
5. Current shortcomings
At present, the application of AI in cardiovascular medicine is very close to reality. Nowadays, getting personal medical advice from virtual assistants such as Alexa or Siri is no longer a far-fetched attachment.[29] However, some researchers are concerned about the rapid development of AI, and they believe that guidelines should be created in artificial-intelligence research to protect human rights.[30]
Besides, there are still several unsolved technical problems in the clinical application of AI. The human brain can solve highly abstract reasoning problems by using physical neural networks. However, the mechanism of the network is only partially understood; therefore, artificial networks can only provide narrow insights.[31] A key factor in preventing the implementation of machine learning in medicine is that the training of a model requires massive datasets, which are not easily accessible. Additionally, without a large amount of high-quality data, the model can likely be influenced, which will lead to biases and inevitably cause the failure of the model when it makes predictions about future data. Furthermore, the difficulty of AI in making differential diagnoses is another major problem, which can be attributed to the relatively slow development of AI use in medicine. Ultimately, the superficial knowledge of the human brain's processing, the poor data quality, the complex computational processes, the difficulty in measuring antidiastole and the inaccessibility to traditional clinical workflow have led to controversy in the clinical application of AI.[32] Medicine is considered to be the first field of application of AI. However, clinical applications require higher quality than AI applications in other fields. Therefore, the application and acceptance of AI will be a very long process.
6. Possible solution—“the primary use of AI” (PUAI) and a novel medical model
6.1. Phenomenon of PUAI
Due to the issues that the entire medical industry has encountered, most of the current implications of AI in cardiovascular medicine can be described as ‘PUAI’. In clinical practice, the main problem faced by doctors every day should be solved first, such as the correct diagnosis and effective treatment for patient.
The application and capabilities of AI are based on large-scale and mature clinical information on machine learning. Currently, it can be applied in certain specific environments, such as emergency room and chest pain center (CPC).
With the improvement of AI technology, we still cannot guarantee that the technology is absolutely reliable. Some experts worry that some clinicians will rely entirely on AI to deal with patients.[33] At any time, doctors are the mainstay, and AI can help doctors improve the effectiveness of their treatment. Verghese, et al.[34] pointed out that clinicians can use AI to better serve patients. Studies have suggested that the combination of clinicians and AI skills will provide patients with higher quality diagnostic results than experience alone.[35] To this end, based on the fact that our team has invented a new regional cooperative rescue model to optimize the diagnosis and treatment system for CPCs,[36] we have designed a new medical model that may help young clinicians reduce the rate of misdiagnosis.
6.2. Novel medical model
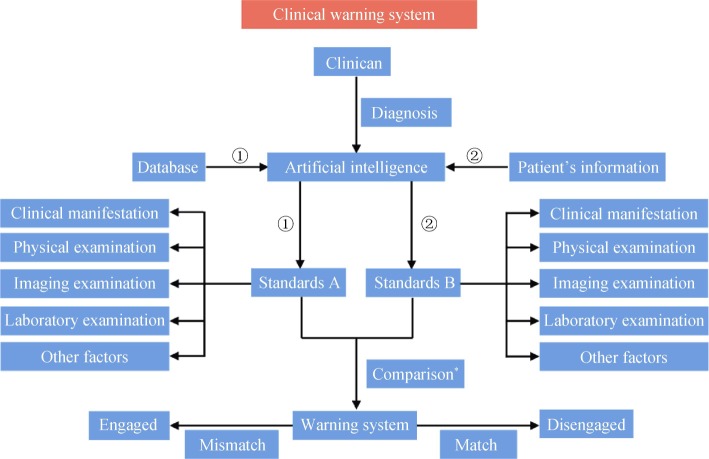
Currently, clinicians provide patients with direct treatment options based on their own judgment. However, due to the clinician's experience, stress, or overwork, other reasons may make a wrong judgment, and even lead to catastrophic consequences. In the new model (Figure 1), the clinician can pass the diagnosis plan through AI, and if the instructions are correct, the AI will execute. If the instructions are unclear, ignore the instructions given by the AI based on machine learning and ask the senior clinician for assistance. It is hoped that this new model will reduce the incidence of medical malpractice caused by clinician errors.
Figure 1. Traditional mode and novel mode.
AI: artificial intelligence.
6.3. Novel medical mode plus PUAI
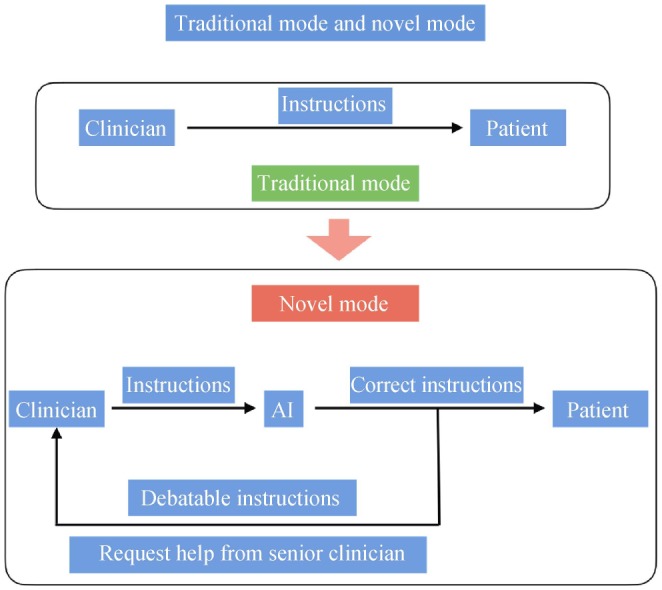
Moreover, we are able to incorporate the concept of PUAI into this novel medical model. We may find an easier way to build an AI model. Currently, the limited use of AI for clinical diagnosis involves the differential diagnosis of CVD. There are several types of CVD, each with different diagnostic methods; therefore, complex algorithms and models, such as deep learning and reinforcement learning, are required to increase the difficulty of writing algorithms and increase the size of training data sets and AI models.[5] However, by incorporating PUAI into a new medical model, it is only necessary to design a small and simple model for the diagnosis of critical diseases such as ACS and aortic dissection by using simpler algorithms. There is no need to worry about the limitations of current AI resistance between these diseases. For example, these types of ideas can be applied to establish a warning system in the current medical system (Figure 2).
Figure 2. Clinical warning system.
*Comparison: the comparison uses supervised learning to optimize the percentages of each standard.
After the patient enters the hospital, the patient's information is simultaneously entered into the database when the clinician collects the history. Based on the clinician's diagnosis, the AI will according the diagnostic criteria for the disease (Standard A) from the database, compared to the patient's actual condition (Standard B). If the comparison results match, the warning system will not be alerting. In the event of conflicting results, the AI will generate an alert alerting the clinician to carefully examine his/her diagnosis.
This new clinical warning system is suitable for ICUs, including the coronary care unit and CPC, which is especially useful during night shifts. Because, in these specific areas, the performance of night shifts doctors has a direct impact on patient safety.[37] Studies from Maltese, et al.[38] have shown that the decision-making ability of ICU doctors has dropped significantly. Currently, this new clinical early warning system shows great potential for avoiding misdiagnosis caused by night shift clinicians' cognitive decline. Besides, the warning system is easy to apply. Our team has designed a new regional cooperative rescue model to optimize the diagnosis and treatment system for CPCs.[36] It provides timely and effective PCI for patients with ST-segment elevation myocardial infarction, especially in developing countries such as China. The key point of this model is to reduce the time from symptom onset to reperfusion and cardiovascular mortality. In the future, our goal is to apply this novel medical model to existing systems. By using a machine learning-based algorithm, AI can carefully examine the clinician's diagnosis and treatment plan. The goal is to save more lives. We will continue to refine this novel medical model and test its practical application value in clinical practice.
At present, CVD remains a major health problem affecting the entire world, especially in low- and middle-income countries. It will continue to be the main cause of mortality in the next twenty years.[3],[39] The use of AI, especially machine learning, has shown great potential in managing and treating this troublesome disease. Besides, we firmly believe that in the future, AI will be an assistant to clinicians, not an adversary, because AI was originally designed to mimic human thinking processes rather than innovation. Therefore, the clinician should understand the meaning of AI and be familiar with its application value. The ability of AI will increase as clinicians become more aware of the disease. The development of clinical skills and in-depth clinical research is the basis for the development of AI. Clinicians must not neglect to continuously learn to improve their ability to serve patients, and not to rely too much on machines and AI.
Acknowledgments
This work was supported by grants from the National Key Research and Development Program of China (2018YFC1312800), National Science Fund for Distinguished Young Scholars (81625002). All authors had no conflicts of interest to disclose.
References
- 1.Thomas H, Diamond J, Vieco A, et al. Global atlas of cardiovascular disease 2000-2016: the path to prevention and control. Glob Heart. 2018;13:143–163. doi: 10.1016/j.gheart.2018.09.511. [DOI] [PubMed] [Google Scholar]
- 2.Naghavi M, Abajobir AA, Abbafati C, et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390:1151–1210. doi: 10.1016/S0140-6736(17)32152-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gersh BJ, Sliwa K, Mayosi BM, et al. Novel therapeutic concepts: the epidemic of cardiovascular disease in the developing world: global implications. Eur Heart J. 2010;31:642–648. doi: 10.1093/eurheartj/ehq030. [DOI] [PubMed] [Google Scholar]
- 4.Wu Y, Benjamin EJ, MacMahon S. Prevention and control of cardiovascular disease in the rapidly changing economy of China. Circulation. 2016;133:2545–2560. doi: 10.1161/CIRCULATIONAHA.115.008728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krittanawong C, Zhang H, Wang Z, et al. Artificial intelligence in precision cardiovascular medicine. J Am Coll Cardiol. 2017;69:2657–2664. doi: 10.1016/j.jacc.2017.03.571. [DOI] [PubMed] [Google Scholar]
- 6.Turing AM. Computing machinery and intelligence. Mind. 1950;49:433–460. [Google Scholar]
- 7.Anticipating artificial intelligence. Nature. 2016;532:413–413. doi: 10.1038/532413a. [DOI] [PubMed] [Google Scholar]
- 8.Gulshan V, Peng L, Coram M, et al. Development and validation of a deep learning algorithm for detection of diabetic retinopathy in retinal fundus photographs. JAMA. 2016;316:2402–2410. doi: 10.1001/jama.2016.17216. [DOI] [PubMed] [Google Scholar]
- 9.Ghahramani Z. Probabilistic machine learning and artificial intelligence. Nature. 2015;521:452–459. doi: 10.1038/nature14541. [DOI] [PubMed] [Google Scholar]
- 10.Raymond JL, Medina JF. Computational principles of supervised learning in the cerebellum. Annu Rev Neurosci. 2018;41:233–253. doi: 10.1146/annurev-neuro-080317-061948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Johnson KW, Torres Soto J, Glicksberg BS, et al. Artificial intelligence in cardiology. J Am Coll Cardiol. 2018;71:2668–2679. doi: 10.1016/j.jacc.2018.03.521. [DOI] [PubMed] [Google Scholar]
- 12.Prasad N, Cheng LF, Chivers C, et al. A reinforcement learning approach to weaning of mechanical ventilation in intensive care units. 2017. [(accessed April 20, 2017)]. arXiv.org. https://arxiv.org/abs/1704.06300.
- 13.Hosny A, Parmar C, Quackenbush J, et al. Artificial intelligence in radiology. Nat Rev Cancer. 2018;18:500–510. doi: 10.1038/s41568-018-0016-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Camacho DM, Collins KM, Powers RK, et al. Next-generation machine learning for biological networks. Cell. 2018;173:1581–1592. doi: 10.1016/j.cell.2018.05.015. [DOI] [PubMed] [Google Scholar]
- 15.LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436–444. doi: 10.1038/nature14539. [DOI] [PubMed] [Google Scholar]
- 16.Dawes TJW, de Marvao A, Shi W, et al. Machine learning of three-dimensional right ventricular motion enables outcome prediction in pulmonary hypertension: a cardiac MR imaging study. Radiology. 2017;283:381–390. doi: 10.1148/radiol.2016161315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Motwani M, Dey D, Berman DS, et al. Machine learning for prediction of all-cause mortality in patients with suspected coronary artery disease: a 5-year multicentre prospective registry analysis. Eur Heart J. 2017;38:500–507. doi: 10.1093/eurheartj/ehw188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Madani A, Arnaout R, Mofrad M, et al. Fast and accurate view classification of echocardiograms using deep learning. NPJ Digit Med. doi: 10.1038/s41746-017-0013-1. Published Online First: 21 March 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Samad MD, Ulloa A, Wehner GJ, et al. Predicting survival from large echocardiography and electronic health record datasets: optimization with machine learning. JACC Cardiovasc Imaging. 2019;12:681–689. doi: 10.1016/j.jcmg.2018.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Su S, Hu Z, Lin Q, et al. An artificial neural network method for lumen and media-adventitia border detection in IVUS. Comput Med Imaging Graph. 2017;57:29–39. doi: 10.1016/j.compmedimag.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 21.Abdolmanafi A, Duong L, Dahdah N, et al. Deep feature learning for automatic tissue classification of coronary artery using optical coherence tomography. Biomed Opt Express. 2017;8:1203–1220. doi: 10.1364/BOE.8.001203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nakajima K, Kudo T, Nakata T, et al. Diagnostic accuracy of an artificial neural network compared with statistical quantitation of myocardial perfusion images: a Japanese multicenter study. Eur J Nucl Med Mol Imaging. 2017;44:2280–2289. doi: 10.1007/s00259-017-3834-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Betancur J, Commandeur F, Motlagh M, et al. Deep learning for prediction of obstructive disease from fast myocardial perfusion SPECT: a multicenter study. JACC Cardiovasc Imaging. 2018;11:1654–1663. doi: 10.1016/j.jcmg.2018.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tran PV. A fully convolutional neural network for cardiac segmentation in short-axis MRI. 2016. [(accessed April 27, 2017)]. arXiv.org. https://arxiv.org/abs/1604.00494.
- 25.Cacciamani GE, De Marco V, Sebben M, et al. Robot-assisted Vescica Ileale Padovana: a new technique for intracorporeal bladder replacement reproducing open surgical principles. Eur Urol. doi: 10.1016/j.eururo.2018.11.037. Published Online First: 30 November 2018. [DOI] [PubMed] [Google Scholar]
- 26.Lonnerfors C. Robot-assisted myomectomy. Best Pract Res Clin Obstet Gynaecol. 2018;46:113–119. doi: 10.1016/j.bpobgyn.2017.09.005. [DOI] [PubMed] [Google Scholar]
- 27.Poplin R, Varadarajan AV, Blumer K, et al. Predicting cardiovascular risk factors from retinal fundus photographs using deep learning. Nat Biomed Eng. 2018;2:158–164. doi: 10.1038/s41551-018-0195-0. [DOI] [PubMed] [Google Scholar]
- 28.Arterys cardio DL cloud MRI analytics software receives FDA clearance. In: editor book arterys cardio DL cloud MRI analytics software receives FDA clearance, 2017. Diagnostic and Interventional Cardiology. [(accessed January 27, 2017)]. https://www.dicardiology.com/product/arterys-cardio-dl-cloud-mri-analytics-software-receives-fda-clearance.
- 29.The Lancet. Artificial intelligence in health care: within touching distance. Lancet. 2018;390:2739–2739. doi: 10.1016/S0140-6736(17)31540-4. [DOI] [PubMed] [Google Scholar]
- 30.Ramesh S. A checklist to protect human rights in artificial-intelligence research. Nature. 2017;552:334–334. doi: 10.1038/d41586-017-08875-1. [DOI] [PubMed] [Google Scholar]
- 31.Jaeger H. Artificial intelligence: deep neural reasoning. Nature. 2016;538:467–468. doi: 10.1038/nature19477. [DOI] [PubMed] [Google Scholar]
- 32.Wilensky GR. Will MACRA improve physician reimbursement? N Engl J Med. 2018;378:1269–1271. doi: 10.1056/NEJMp1801673. [DOI] [PubMed] [Google Scholar]
- 33.Russell S, Bohannon J. Artificial intelligence. Fears of an AI pioneer. Science. 2015;349:252–252. doi: 10.1126/science.349.6245.252. [DOI] [PubMed] [Google Scholar]
- 34.Verghese A, Shah NH, Harrington RA. What this computer needs is a physician: humanism and artificial intelligence. JAMA. 2018;319:19–20. doi: 10.1001/jama.2017.19198. [DOI] [PubMed] [Google Scholar]
- 35.Chen JH, Asch SM. Machine learning and prediction in medicine-beyond the peak of inflated expectations. N Engl J Med. 2017;376:2507–2509. doi: 10.1056/NEJMp1702071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Yan J, Wang Z, Xu LJ, et al. Effects of new regional cooperative rescue model on patients with ST-elevation myocardial infarction. Int J Cardiol. 2014;177:494–496. doi: 10.1016/j.ijcard.2014.08.074. [DOI] [PubMed] [Google Scholar]
- 37.Reinke L, Özbay Y, Dieperink W, et al. The effect of chronotype on sleepiness, fatigue, and psychomotor vigilance of ICU nurses during the night shift. Intensive Care Med. 2015;41:657–666. doi: 10.1007/s00134-015-3667-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Maltese F, Adda M, Bablon A, et al. Night shift decreases cognitive performance of ICU physicians. Intensive Care Med. 2016;42:393–400. doi: 10.1007/s00134-015-4115-4. [DOI] [PubMed] [Google Scholar]
- 39.Hu J, Cui X, Gong Y, et al. Portable microfluidic and smartphone-based devices for monitoring of cardiovascular diseases at the point of care. Biotechnol Adv. 2016;34:305–320. doi: 10.1016/j.biotechadv.2016.02.008. [DOI] [PubMed] [Google Scholar]