This survey study examines how older adults perceive factors used in diabetes guidelines for individualizing glycemic targets.
Key Points
Question
How do older adults perceive factors used in diabetes guidelines to individualize glycemic targets?
Findings
In this cross-sectional national online survey of 818 US adults 65 years and older with type 2 diabetes conducted from December 13, 2018, to January 3, 2019, the importance of 7 factors in diabetes treatment decisions and perceptions of how factors affected treatment intensity were assessed. Participants considered the factors important when adding medicines to their treatment plans but less important when removing medicines from their treatment plans; participants believed that patients with longer disease duration, more established complications, and more other health conditions should receive more aggressive treatment, which is opposite to guideline recommendations.
Meaning
Older adults’ beliefs about certain guideline factors for diabetes treatment are in opposition to what the guidelines recommend, which may present substantial barriers to appropriate treatment goals and care.
Abstract
Importance
Diabetes guidelines recommend considering specific factors, such as diabetes duration and life expectancy, to individualize treatment in older adults. These individualized glycemic targets inform decisions on whether to intensify or deintensify medication treatment plans. How older adults with diabetes perceive these factors used to individualize glycemic targets is unknown.
Objectives
To examine how older adults perceive factors used in diabetes guidelines for individualizing glycemic targets.
Design, Setting, and Participants
A cross-sectional national survey was conducted from December 13, 2018, to January 3, 2019, of a nationally representative, probability-based online survey panel (KnowledgePanel). A total of 1364 KnowledgePanel members who were 65 years or older and had type 2 diabetes were invited to participate in the survey; 836 (61.3%) responded, and 818 (60.0%) completed the survey.
Main Outcomes and Measures
The study randomized participants to 2 vignettes: one about adding and the other about removing diabetes medications from treatment plans. Participants rated the importance of 7 factors (diabetes duration, established diabetes complications, other health conditions, life expectancy, risk of adverse effects, cost, and treatment effort) in these treatment decisions using binary (yes/no) responses and the best-worst scaling method to quantify the factors’ relative importance. All participants then answered questions on how different levels of each factor were associated with aggressiveness of diabetes treatment.
Results
The sample included 818 participants (mean [SD] age, 74.0 [6.8] years; 469 [53.7%] male; and 668 [67.7%] white). A total of 410 participants answered questions about adding medicine, whereas 408 participants answered questions about stopping medicine. Of the 7 factors to consider for adding a diabetes medication to the treatment plan, the number who deemed each factor important ranged from 197 (45.6%) to 263 (62.8%). In contrast, these same factors were considered important by only 29 (8.4%) to 146 (37.7%) of participants when deciding to stop use of a diabetes medication. In both decisions, participants perceived the risk of adverse effects as the most important factor (relative importance was 22.8 for adding a medicine and 25.0 for stopping a medicine on a ratio scale in which, for each decision, the relative importance of the 7 factors adds up to 100, with 0 indicating complete indifference and 100 complete priority). In contrast to current guideline recommendations, most participants believed that patients with longer disease duration (498 [60.1%]), more established complications (632 [75.6%]), and greater number of other health conditions (545 [67.5%]) should receive more aggressive diabetes treatment.
Conclusions and Relevance
Many older adults do not place high importance on factors recommended by guidelines to individualize diabetes treatment, especially when deciding to stop use of diabetes medications. Moreover, when considering treatment aggressiveness, many older adults weighted several factors in the opposite direction than suggested by the guidelines. Individualizing diabetes care in older adults will require effective communication regarding the benefits and consequences of making changes to treatment plans.
Introduction
Type 2 diabetes is a common condition among older adults, but the optimal treatment target for this population remains uncertain.1,2 The benefit of tight glycemic control is often delayed by many years, but the risks of hypoglycemia and polypharmacy and the burden of intensive treatment occur in the short term and are more common in older adults.1,2,3,4,5,6,7,8 Guidelines increasingly recognize that tight glycemic control may at times pose more harms than benefits and recommend individualized glycemic targets in older adults based on consideration of specific patient factors.9,10,11,12,13 For example, multiple guidelines recommend considering the patient’s life expectancy when choosing glycemic targets. Specifically, a less stringent glycemic target is recommended in people with short life expectancy, whereas a more stringent target is recommended in those with long life expectancy.9,10,11,12,13 Other factors mentioned in the guidelines for individualizing glycemic targets include diabetes duration, other comorbidities, diabetes complications, risk of adverse effects or hypoglycemia, patient preference, treatment burden, cost, patient resources, and patient motivation.9,10,11,12,13 The individualized glycemic target then, in turn, informs decisions about whether to intensify or deintensify medication treatment plans. However, despite the guidelines, glycemic control among older adults is suboptimal and overtreatment is common.14,15,16,17,18
How older adults with diabetes perceive the factors used to individualize glycemic targets and decide on medication intensification or deintensification is unknown. Existing literature on patient preferences in diabetes often focuses on comparing specific treatment options or weighing treatment outcomes against specific adverse effects and/or cost.19,20,21,22,23,24 Glucose control and avoiding hypoglycemia are important concerns for patients, but patient priorities in this tradeoff are mixed.24 To our knowledge, no prior study has examined how patients view the factors used in guidelines to determine individualized glycemic targets. If the guideline rationales for how to individualize diabetes treatment are not intuitive to patients, the ability for engaging patients in collaborative goal setting and shared decision-making, both of which are important for high-quality diabetes care, could be severely impaired.25,26
This study used a national survey to examine how older adults perceive and prioritize the factors (eg, shorter life expectancy) used to individualize diabetes treatment in clinical practice guidelines.9,10,11,12,13 Given the prevalence of potential overtreatment,14,15,16,17,18 we were particularly interested in treatment deintensification and examined separately the importance of these factors in the decision to add medicines vs the decision to remove medicines from the treatment plans.
Methods
Study Design and Sample
This cross-sectional online survey used the KnowledgePanel, the largest national probability-based online panel, with more than 55 000 members representing the US adult population. Panel members were randomly recruited by random digit dialing (until 2009) and address-based sampling (since 2009).27 Households without computers or internet access were provided with both. A total of 1364 panel members were invited to participate via email if they were at least 65 years old, spoke English, and had type 2 diabetes according to KnowledgePanel’s baseline information on members. A total of 836 (61.3%) responded, and 818 (60.0%) completed the survey (the other 18 did not confirm that they have type 2 diabetes). We independently confirmed whether a person had been told by a physician that they had type 2 diabetes and those who answered yes were invited to complete the survey. This study was approved by a Johns Hopkins University School of Medicine Institutional Review Board. The beginning of the survey stated that completion of the survey serves as consent to be in this research study. The data from KnowledgePanel were deidentified.
Survey Instrument
Details about the survey instrument are included in the eMethods in the Supplement. We briefly described the benefits of lowering blood glucose levels in patients with diabetes (reducing the risk of damage to eyes, kidneys, heart, and nerves) and the risks of intensive treatment (increased adverse effects and burden). To limit survey length and response burden, we randomized participants to 1 of 2 modules that asked about the importance of 7 predefined factors in the decision to add a diabetes medication (module 1A) or the decision to remove a diabetes medication (module 1B) from the treatment plan. Then, all participants completed a module that asked how aggressive diabetes treatment should be at different levels of each factor (module 2), which was designed to assess how participants perceived the directionality of the effect for each factor (eg, if shorter vs longer life expectancy was perceived to be associated with aggressive diabetes treatment). We pilot tested the survey instrument with 11 older adults who were not included in the study and iteratively revised the instrument based on feedback.
Factors Tested in the Survey
In modules 1A and 1B, we asked about the perceived importance of 7 factors in the decision to add or remove a diabetes medication from a treatment plan: (1) diabetes duration, (2) established diabetes complications, (3) other health conditions, (4) life expectancy, (5) risk of adverse effects from treatment (referred to in the survey as "side effects"), (6) treatment cost, and (7) treatment effort. We chose the factors primarily based on the American Diabetes Association’s framework for individualizing glycemic targets. We also reviewed other relevant major clinical guidelines and modified the factor descriptions to be consistent9,10,11,12,13; the factor descriptions were also informed by feedback during pilot testing.
Module 1A: Decision About Adding a Medicine
We described a hypothetical patient with a hemoglobin A1c (HbA1c) level of 8.0% who was deciding whether to add a diabetes medication to his/her treatment plan and asked whether each of the 7 factors described above was a good reason to add a diabetes medication. We chose this HbA1c value because it was mentioned in the American Diabetes Association guideline as a less stringent treatment target.10
Guidelines recommend less aggressive diabetes treatment for patients with longer diabetes duration, established vascular complications, shorter life expectancy, more comorbidities, and higher risk of adverse effects.9,10,11,12,13 In addition, high treatment cost and high treatment effort are barriers to medication adherence.28 Therefore, each factor is described in a way that reflects its directional effect per the guidelines or literature. For example, diabetes duration is described as “has had diabetes a short time” when asking whether it is a good reason for adding a medicine to the treatment plan.
We first asked these questions with binary responses (yes/no); we also used a stated preference method called best-worst scaling to assess the relative importance among the factors. The best-worst scaling technique presents participants with a list of items and asks them to choose the 1 item that they consider the best (most important) and the 1 item that they consider the worst (least important).29,30,31 This technique allows for comparison of relative values across items, something that is not possible with traditional Likert scale surveys.29,30,31 As part of this technique, only a subset of all items is presented at a given time in a single choice task, and the participant is asked to complete a series of choice tasks in which the items in each choice task are systematically varied. The survey included 7 choice tasks, each displaying 4 of the 7 factors. An example of a best-worst scaling choice task is included in the eMethods in the Supplement.
Module 1B: Decision About Removing a Medicine
We described a hypothetical patient with an HbA1c value less than 7.0% who is deciding whether to stop use of a diabetes medication. We chose this HbA1c value because it is considered a more stringent treatment target in clinical guidelines.9,10,12 We stated that the physician will monitor the patient’s response after stopping use of the medicine and make changes if needed. We asked about the importance of the same 7 factors in module 1A, with the factor descriptions now reflecting the opposite extreme; for example, diabetes duration is described as “has had diabetes a long time” when asking about whether it is a good reason for stopping use of a medicine.
Module 2: Factors and Treatment Aggressiveness
We assessed the perceived effect of each factor on the aggressiveness of diabetes treatment. The term aggressive was selected after pilot testing found it to be more preferred than tight, intensive, or stringent. Participants were presented with 2 hypothetical patients with varying levels or values of a factor and then asked which patient should have more aggressive diabetes treatment. We examined 5 factors from module 1A and module 1B, omitting treatment cost and treatment effort because they have been studied previously.19,20,23,24 Each factor was tested individually without mention of the other factors. For example, we asked whether “a person who has no complications from diabetes” or “a person who has severe complications from diabetes” should have more aggressive treatment for diabetes.
KnowledgePanel provided information on age, sex, race/ethnicity, and educational level of the study participants. We collected additional information, including self-reported diabetes duration, presence of diabetes complications, type of diabetes medications, most recent HbA1c value, willingness to stop use of diabetes medications, health literacy,32 health and functional status,33 and decision-making preferences.34 Life expectancy was estimated from these data using a validated index.33
Data Collection
Data collection occurred from December 13, 2018, to January 3, 2019. Survey weights were applied to account for any differential nonresponse that may have occurred in specific demographic groups. Responses to the binary questions in modules 1A and 1B were compared using 2-sample proportion z tests. To analyze best-worst scaling response data, we used a conditional (fixed-effects) logistic regression model in which the 7 factors were the independent variables and the dependent variable was choosing a factor as best (+1), worst (−1), or neither best nor worst (0). The SEs were clustered by respondent to account for repeated choices. Results were rescaled to a ratio scale that ranged from 0 to 100 for ease of interpretation, with a score of 0 indicating complete indifference and 100 indicating complete priority.35
Statistical Analysis
Participant characteristics and responses in module 2 were analyzed descriptively. As sensitivity analyses, we stratified the participant responses by participants’ own diabetes duration, most recent HbA1c value, and history of hypoglycemia to explore whether participants’ own experiences influenced their responses. All statistical analyses were performed using Stata, version 14 (StataCorp LLC). A 2-sided P < .05 was considered to be statistically significant.
Results
The sample included 818 participants (mean [SD] age, 74.0 [6.8] years; 469 [53.7%] male; and 668 [67.7%] white) (Table 1). A total of 371 participants (44.6%) reported having hypoglycemic symptoms in the previous 12 months. A total of 464 participants (53.8%) reported that their most recent HbA1c value was less than 7.0%, and 601 (67.5%) reported that their goal HbA1c value was less than 7.0%. Only 209 (23.5%) reported that their physician ever recommended stopping use of a diabetes medication; 719 (87.8%) would be willing to stop use of a diabetes medication if recommended by their physician.
Table 1. Participant Characteristics .
| Characteristic | Findinga (N = 818) |
|---|---|
| Age, mean (SD), y | 74.0 (6.8) |
| Male sex | 469 (53.7) |
| Race/ethnicity | |
| White, non-Hispanic | 668 (67.7) |
| Black, non-Hispanic | 67 (14.9) |
| Hispanic | 53 (9.4) |
| Other | 30 (8.0) |
| Time since diabetes diagnosis, y | |
| <5 | 141 (16.9) |
| 5 to <10 | 163 (19.0) |
| 10 to <15 | 207 (24.5) |
| 15 to <20 | 142 (19.5) |
| ≥20 | 163 (20.1) |
| Has ever had a heart attack, coronary artery disease, or stroke | 217 (27.8) |
| Has eye disease from diabetes | 81 (12.0) |
| Has kidney disease from diabetes | 80 (10.5) |
| Has nerve damage from diabetes | 265 (32.1) |
| Diabetes medications | |
| None | 64 (10.1) |
| Oral medications only | 522 (61.0) |
| Injection medications only | 58 (9.1) |
| Oral and injection medications | 168 (19.7) |
| Frequency of checking blood glucose level | |
| More than once a day | 215 (27.8) |
| Once a day | 229 (26.0) |
| One or more times a week but not every day | 157 (20.9) |
| Less than once a week | 216 (25.3) |
| Hypoglycemia in last 12 mo | |
| None | 443 (55.4) |
| 1 Time | 85 (10.5) |
| 2-5 Times | 207 (25.1) |
| >5 Times | 79 (9.0) |
| Most recent HbA1c value | |
| <7.0% | 464 (53.8) |
| 7% to <8% | 210 (26.2) |
| 8% to <9% | 47 (5.4) |
| ≥9% | 26 (3.0) |
| Don’t know | 68 (11.6) |
| Has had discussion with physician about goal HbA1c | 630 (73.3) |
| Self-reported goal HbA1c | |
| <7.0% | 601 (67.5) |
| 7% to <8% | 81 (11.9) |
| 8% to <9% | 3 (0.4) |
| ≥9% | 4 (0.6) |
| Don’t know | 123 (19.6) |
| Physician has recommended stopping use of diabetes medication | 209 (23.5) |
| Would be willing to stop use of diabetes medication | 719 (87.8) |
| Estimated life expectancy,33 y | |
| >10 | 432 (48.0) |
| 4-10 | 279 (38.6) |
| <4 | 75 (13.4) |
| Educational level | |
| Did not complete high school | 29 (6.9) |
| Completed high school | 206 (44.2) |
| <4-y College | 305 (24.6) |
| College graduate or postgraduate degrees | 278 (24.3) |
| Health literacy (possible range, 3-15),32 mean (SD) | 13.0 (2.2) |
| Decision-making preferences34 | |
| Make own decisions | 250 (31.3) |
| Make decisions together with physician | 541 (64.6) |
| Leave decision to physician | 26 (4.1) |
Abbreviation: HbA1c, hemoglobin A1c.
Data are presented as number (percentage) of survey respondents unless otherwise indicated. Means and percentages are weighted.
Module 1A: Decision About Adding a Medicine to a Diabetes Treatment Plan
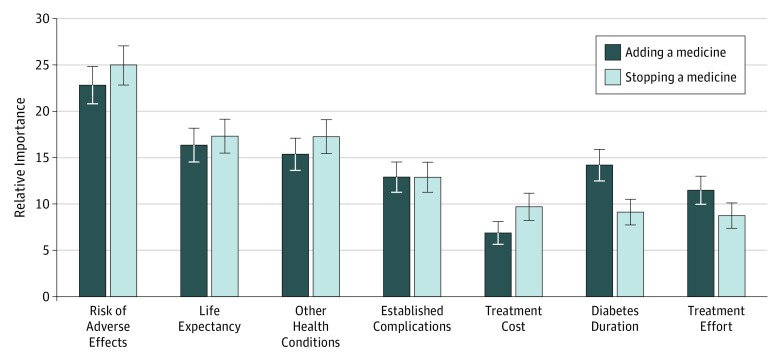
For each of the 7 factors, we asked 410 participants whether the factor was a good reason to add a medicine to a diabetes treatment plan. Responses ranged from 197 (45.6%) who considered having “few other health conditions” to be a good reason to add a medicine to a treatment plan to 263 (62.8%) who considered having “had diabetes for a short time” to be a good reason to add a medicine (Table 2). A total of 346 (86.0%) considered at least 1 of the 7 factors a good reason for adding a diabetes medication to a treatment plan, and 108 (23.3%) considered all 7 factors to be good reasons. According to the best-worst scaling, the most important reason to add a medicine to a treatment plan was low risk of adverse effects from diabetes treatment, whereas the least important reason to add a diabetes medication to a treatment plan was low treatment cost (Figure).
Table 2. Participants’ Perceptions of Factor Importance in Diabetes Treatment Decisionsa,b.
| Factor | Good Reason to Add a Medicine to a Treatment Plan? (n = 410) | No. (%) | Good Reason to Remove a Medicine From a Treatment Plan? (n = 408) | No. (%) |
|---|---|---|---|---|
| Diabetes duration | Has had diabetes a short time | 263 (62.8) | Has had diabetes a long time | 37 (9.4) |
| Established complications | Has no significant diabetes complications | 213 (48.8) | Already has severe diabetes complications | 62 (18.4) |
| Other health conditions | Has few other health conditions | 197 (45.6) | Has many other serious health conditions | 52 (15.1) |
| Life expectancy | Expected to live a long time | 230 (51.9) | Not expected to live a long time | 42 (9.6) |
| Risk of adverse effects | Has a low chance of adverse effects from diabetes treatment | 226 (54.6) | Has a high chance of adverse effects from diabetes treatment | 146 (37.7) |
| Treatment cost | Has to pay little money for diabetes treatment | 209 (51.2) | Has to pay a lot of money for diabetes treatment | 63 (14.8) |
| Treatment effort | Has to spend little effort to manage diabetes | 221 (53.4) | Has to spend a lot of effort to manage diabetes | 29 (8.4) |
| None of the factors | NA | 64 (14.0) | NA | 202 (46.9) |
| All the factors | NA | 108 (23.3) | NA | 4 (0.5) |
Abbreviation: NA, not applicable.
Percentages are weighted.
Comparison used 2-sample proportion z test. P < .001 for all comparisons.
Figure. Relative Importance of the 7 Factors in Diabetes Treatment Decisions .
The results are plotted on a ratio scale in which, for each decision, the relative importance of the 7 factors adds up to 100.35 A score of 0 indicates complete indifference, and 100 indicates complete priority at the expense of all other factors. A factor with a score of 10 indicates that it is twice as important as a factor with a score of 5.
Module 1B: Decision About Removing a Medicine From a Diabetes Treatment Plan
We asked 408 participants whether each of the 7 factors was a good reason to stop use of a diabetes medication. Responses ranged from 29 (8.4%) who considered having “to spend a lot of effort to manage diabetes” as a good reason to stop use of a medicine to 146 (37.7%) who considered having “a high chance of side effects” as a good reason to stop use of a medicine (Table 2). A total of 202 participants (46.9%) thought that none of the 7 factors was a good reason to stop use of a diabetes medication. In contrast to the results about adding a medicine to a treatment plan, far fewer participants considered the same factors important for stopping use of a medicine (Table 2).
Despite the marked difference in how participants perceived the absolute importance of the factors in the 2 treatment decisions, the relative importance of the factors was similar (Figure). The risk of adverse effects was the most important factor in both decisions (its relative importance was 22.8 for adding a medicine and 25.0 for stopping a medicine on a ratio scale in which, for each decision, the relative importance of the 7 factors adds up to 100, with 0 indicating complete indifference and 100 complete priority), followed by life expectancy and other health conditions. Factors with lower relative importance were treatment effort and treatment cost.
Module 2: Association Between Levels of Each Factor and Aggressiveness of Diabetes Treatment
We found that the 818 participants’ perceptions regarding how different levels of each factor related to aggressiveness of treatment were the opposite of guideline recommendations for 3 of the 5 factors (Table 3). Although guidelines recommend less aggressive treatment for patients with longer diabetes duration,10,13 498 participants (60.1%) believed that someone with longer diabetes duration should be treated more aggressively than someone with shorter duration. In opposition to guidelines,10,11,12,13 632 participants (75.6%) chose more aggressive diabetes treatment for a person who already has severe complications from diabetes compared with no complications, and 545 (67.5%) chose more aggressive treatment for a person with many other health conditions compared with no other health conditions. The participants’ perceptions agreed with guideline recommendations for life expectancy (613 [72.7%]) and risk of adverse effects (672 [78.2%]).9,10,11,12,13 In sensitivity analyses, we found that participants’ responses did not vary by their own HbA1c value or history of hypoglycemia. We observed some differences in responses when stratified by participants’ diabetes duration but did not find a clear pattern (eTable in the Supplement).
Table 3. Participant Perceptions of the Association Between Different Factor Levels and Aggressiveness of Diabetes Treatmenta.
| Hypothetical Patient | No. (%) of Participants (n = 818) | Participant Perception Relative to Guideline Recommendations9,10,11,12,13 |
|---|---|---|
| Diabetes duration | ||
| A person who has had diabetes for 5 yb | 319 (39.9) | Discordant |
| A person who has had diabetes for 15 y | 498 (60.1) | |
| Established complications | ||
| A person who has no complications from diabetesb | 185 (24.4) | Discordant |
| A person who has severe complications from diabetes | 632 (75.6) | |
| Other health conditions | ||
| A person who has no other health conditionsb | 273 (32.5) | Discordant |
| A person who has many other health conditions | 545 (67.5) | |
| Life expectancy | ||
| A person who will live for another 5 y | 204 (27.3) | Concordant |
| A person who will live for another 15 yb | 613 (72.7) | |
| Risk of adverse effects | ||
| A person who probably will have adverse effects | 144 (21.8) | Concordant |
| A person who probably will not have adverse effectsb | 672 (78.2) |
Participants were asked, “Which hypothetical patient should have more aggressive treatment for diabetes?”
The choice recommended by guidelines.
Discussion
We conducted a national survey examining how older adults perceived the importance of factors used in diabetes guidelines to individualize glycemic targets and how older adults perceived the association between these factors and aggressiveness of diabetes treatment. This study had several key findings. Participants viewed the factors as important in the decision to add a diabetes medication to a treatment plan. However, in the decision to remove a medicine from a treatment plan, nearly half did not think any of the 7 factors was important. The relative importance of the different factors in adding and removing medicines from treatment plans was similar, with concern about treatment adverse effects being the most important. Finally, participants’ beliefs about how these factors affect diabetes treatment were often opposite to the guideline recommendations.
Our finding that the participants considered all 7 factors more important for adding than for removing medicines from treatment plans has important implications in light of the high rate of potential overtreatment for diabetes in older adults and the increasing attention on deprescribing.14,15,16,17,18,36,37 Our result suggests that diabetes medication intensification and deintensification may not merely be the reverse of one another but may represent distinct processes. Even though most participants reported willingness to stop use of a diabetes medication, almost half of the participants did not consider any of the 7 factors that we examined in this study to be an important reason for doing so, raising significant questions as to what patients think should drive the decision-making. Literature38,39,40 on patient experiences of stopping or reducing use of medications is limited, and none focused on diabetes medications. A study41 of long-term care residents found that continuity of care and focus on patient well-being were highly ranked concerns for patients when deprescribing medications. Another study42 found that patients were passive toward medication reduction and depended on their physicians to initiate medication changes. These factors (ie, practitioner recommendation) can be explored in future studies to better understand patient priorities in deprescribing decisions.
Using the method of best-worst scaling, we identified the relative priority of the 7 factors in diabetes treatment decisions. Previous studies19,20,23,24 have examined patients’ priorities regarding 3 of the factors examined in this study (cost, treatment burden, and risk of adverse effects), whereas the other 4 have not been systematically studied to our knowledge. Risk of adverse effects was the most important factor in both decisions to add and remove a diabetes medication. Extensive literature20,24 has demonstrated that adverse effects are an important consideration for patients when choosing among alternative therapies; our result adds to this literature by reporting that adverse effects are also important in the context of stopping use of medications. We were surprised that life expectancy was the second most important factor in both decisions. A previous study43 found that, in the context of cancer screening, there was significant mismatch between the guidelines and patient understanding about using life expectancy in decision-making. How older adults with diabetes view life expectancy and consider it in diabetes decisions needs to be examined further. We found that treatment cost and effort were among the least important factors in both decisions. Previous studies23,24 often examined cost in terms of willingness to pay for a better treatment effect and/or fewer adverse effects. Our study extends this prior research by showing that cost, at least in abstract form (ie, described as having to spend “a little” vs “a lot” on diabetes treatment), is of low relative importance. Consistent with our results, treatment burden in terms of mode or frequency of drug administration has not been found in prior studies20,24 to be a strong factor in treatment preference.
The participants in this study believed that 3 of the factors (diabetes duration, established complications, and other health conditions) should influence aggressiveness of diabetes treatment in the opposite direction than what guidelines recommend.9,10,11,12,13 The study design did not allow us to explore the reasons for these responses. They may reflect low awareness and knowledge of the guidelines among patients.44 The results may also reflect different values and priorities among the patients compared with the guidelines. This area is important to explore in future studies. This finding suggests that the rationales explaining how guidelines use diabetes duration, established diabetes complications, and the presence of other health conditions to individualize glycemic targets are not intuitive to many patients. These participants’ opposite beliefs can make it more difficult for practitioners to discuss individualized diabetes treatment and lead to misguided preferences, contributing to both overtreatment and undertreatment. It is important to make clinical practice guidelines more transparent and accessible to patients and make guideline language more patient centered. The results also suggest that individualized glycemic targets are not easy or intuitive concepts for patients to grasp and developing effective strategies to communicate with patients and engage patients in making individualized treatment decisions is critical.
Limitations
Our study has several limitations. First, the survey used hypothetical scenarios, and participants’ responses may not fully reflect their behaviors. However, prior studies45,46 in vaccination and diabetes treatment suggest that participants’ stated preferences in hypothetical situations can be highly predictive of actual behaviors. In the absence of validated instruments, descriptions of the hypothetical scenarios were developed by the study team and revised based on feedback during pilot testing. Second, we examined a limited number of factors and did not include others that may be important to patients’ treatment decisions, such as practitioner recommendation. Therefore, we cannot determine what the main factors are for patients to add or remove diabetes medications from treatment plans. Third, the factors tested in modules 1A and 1B were described in a directional manner according to the guidelines (eg, we asked whether “expected to live a long time” is a good reason to add a medicine to a treatment plan), and thus the participants’ responses may have been affected by different beliefs of the intended effect of the factors. Fourth, our study participants, although recruited from a nationally representative online survey panel, may not be representative of certain subgroups of older adults, such as those with low health literacy. Our findings could also be susceptible to nonresponse bias. However, we achieved a relatively high response rate and used survey weights to adjust for nonresponse. Our study participants were also similar to other national studies14,17,47 of older adults with diabetes in terms of mean age, proportion with HbA1c level less than 7.0%, and self-reported frequency of hypoglycemic symptoms. Fifth, the best-worst scaling method may be unfamiliar to participants and lead to misunderstanding of questions. However, we did not note confusion about the best-worst scaling tasks during pilot testing.
Conclusions
Individualized diabetes care is essential for older adults, yet older adults’ beliefs about certain guideline factors for individualizing glycemic targets are contrary to what the guidelines recommend, and older adults may not consider these factors important in treatment deintensification. These findings may present substantial barriers to share decision-making and contribute to inappropriate treatment goals and care, especially when stopping use of a diabetes medication may be beneficial. Developing strategies to communicate the rationales promoting individualized diabetes treatment to patients and to effectively engage patients in these treatment decisions are important next steps.
eMethods. Survey Instrument Content
eTable. Participant Perceptions of the Relationship Between Different Factor Levels and Aggressiveness of Diabetes Treatment, Stratified by Self-reported Diabetes Duration
References
- 1.Lipska KJ, Krumholz H, Soones T, Lee SJ. Polypharmacy in the aging patient: a review of glycemic control in older adults with type 2 diabetes. JAMA. 2016;315(10):1034-1045. doi: 10.1001/jama.2016.0299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kirkman MS, Briscoe VJ, Clark N, et al. Diabetes in older adults. Diabetes Care. 2012;35(12):2650-2664. doi: 10.2337/dc12-1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pathak RD, Schroeder EB, Seaquist ER, et al. ; SUPREME-DM Study Group . Severe hypoglycemia requiring medical intervention in a large cohort of adults with diabetes receiving care in U.S. integrated health care delivery systems: 2005-2011. Diabetes Care. 2016;39(3):363-370. doi: 10.2337/dc15-0858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the Diabetes and Aging Study. JAMA Intern Med. 2014;174(2):251-258. doi: 10.1001/jamainternmed.2013.12956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dumbreck S, Flynn A, Nairn M, et al. Drug-disease and drug-drug interactions: systematic examination of recommendations in 12 UK national clinical guidelines. BMJ. 2015;350:h949. doi: 10.1136/bmj.h949 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vijan S, Hayward RA, Ronis DL, Hofer TP. Brief report: the burden of diabetes therapy: implications for the design of effective patient-centered treatment regimens. J Gen Intern Med. 2005;20(5):479-482. doi: 10.1111/j.1525-1497.2005.0117.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Arnaud M, Pariente A, Bezin J, Bégaud B, Salvo F. Risk of serious trauma with glucose-lowering drugs in older persons: a nested case-control study. J Am Geriatr Soc. 2018;66(11):2086-2091. doi: 10.1111/jgs.15515 [DOI] [PubMed] [Google Scholar]
- 8.Huang ES, Karter AJ, Danielson KK, Warton EM, Ahmed AT. The association between the number of prescription medications and incident falls in a multi-ethnic population of adult type-2 diabetes patients: the Diabetes and Aging Study. J Gen Intern Med. 2010;25(2):141-146. doi: 10.1007/s11606-009-1179-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA; Clinical Guidelines Committee of the American College of Physicians . Hemoglobin a1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: a guidance statement update from the American College of Physicians. Ann Intern Med. 2018;168(8):569-576. doi: 10.7326/M17-0939 [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes Association Glycemic targets: standards of medical care in diabetes – 2018. Diabetes Care. 2018;41(suppl 1):S55-S64. doi: 10.2337/dc18-S006 [DOI] [PubMed] [Google Scholar]
- 11.Moreno G, Mangione CM, Kimbro L, Vaisberg E; American Geriatrics Society Expert Panel on Care of Older Adults with Diabetes Mellitus . Guidelines abstracted from the American Geriatrics Society Guidelines for improving the care of older adults with diabetes mellitus: 2013 update. J Am Geriatr Soc. 2013;61(11):2020-2026. doi: 10.1111/jgs.12514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Conlin PR, Colburn J, Aron D, Pries RM, Tschanz MP, Pogach L. Synopsis of the 2017 US Department of Veterans Affairs/US Department of Defense clinical practice guideline: management of type 2 diabetes mellitus. Ann Intern Med. 2017;167(9):655-663. doi: 10.7326/M17-1362 [DOI] [PubMed] [Google Scholar]
- 13.Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American Association of Clinical Endocrinologists and American College of Endocrinology: clinical practice guidelines for developing a diabetes mellitus comprehensive care plan 2015. Endocr Pract. 2015;21(suppl 1):1-87. doi: 10.4158/EP15672.GLSUPPL [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Arnold SV, Lipska KJ, Wang J, Seman L, Mehta SN, Kosiborod M. Use of intensive glycemic management in older adults with diabetes mellitus. J Am Geriatr Soc. 2018;66(6):1190-1194. doi: 10.1111/jgs.15335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tseng CL, Soroka O, Maney M, Aron DC, Pogach LM. Assessing potential glycemic overtreatment in persons at hypoglycemic risk. JAMA Intern Med. 2016;176(7):969-978. doi: 10.1001/jamainternmed.2013.12963 [DOI] [PubMed] [Google Scholar]
- 16.Maciejewski ML, Mi X, Sussman J, et al. Overtreatment and deintensification of diabetic therapy among Medicare beneficiaries. J Gen Intern Med. 2018;33(1):34-41. doi: 10.1007/s11606-017-4167-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lipska KJ, Ross JS, Miao Y, Shah ND, Lee SJ, Steinman MA. Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. JAMA Intern Med. 2015;175(3):356-362. doi: 10.1001/jamainternmed.2014.7345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McCoy RG, Lipska KJ, Yao X, Ross JS, Montori VM, Shah ND. Intensive treatment and severe hypoglycemia among adults with type 2 diabetes. JAMA Intern Med. 2016;176(7):969-978. doi: 10.1001/jamainternmed.2016.2275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vijan S, Sussman JB, Yudkin JS, Hayward RA. Effect of patients’ risks and preferences on health gains with plasma glucose level lowering in type 2 diabetes mellitus. JAMA Intern Med. 2014;174(8):1227-1234. doi: 10.1001/jamainternmed.2014.2894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Purnell TS, Joy S, Little E, Bridges JF, Maruthur N. Patient preferences for noninsulin diabetes medications: a systematic review. Diabetes Care. 2014;37(7):2055-2062. doi: 10.2337/dc13-2527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Huang ES, Brown SE, Ewigman BG, Foley EC, Meltzer DO. Patient perceptions of quality of life with diabetes-related complications and treatments. Diabetes Care. 2007;30(10):2478-2483. doi: 10.2337/dc07-0499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chin MH, Drum ML, Jin L, Shook ME, Huang ES, Meltzer DO. Variation in treatment preferences and care goals among older patients with diabetes and their physicians. Med Care. 2008;46(3):275-286. doi: 10.1097/MLR.0b013e318158af40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joy SM, Little E, Maruthur NM, Purnell TS, Bridges JFP. Patient preferences for the treatment of type 2 diabetes: a scoping review. Pharmacoeconomics. 2013;31(10):877-892. doi: 10.1007/s40273-013-0089-7 [DOI] [PubMed] [Google Scholar]
- 24.von Arx LB, Kjeer T. The patient perspective of diabetes care: a systematic review of stated preference research. Patient. 2014;7(3):283-300. doi: 10.1007/s40271-014-0057-0 [DOI] [PubMed] [Google Scholar]
- 25.Lafata JE, Morris HL, Dobie E, Heisler M, Werner RM, Dumenci L. Patient-reported use of collaborative goal setting and glycemic control among patients with diabetes. Patient Educ Couns. 2013;92(1):94-99. doi: 10.1016/j.pec.2013.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tamhane S, Rodriguez-Gutierrez R, Hargraves I, Montori VM. Shared decision-making in diabetes care. Curr Diab Rep. 2015;15(12):112. doi: 10.1007/s11892-015-0688-0 [DOI] [PubMed] [Google Scholar]
- 27.Growth From Knowledge KnowledgePanel recruitment and sample survey methodologies. http://www.gfk.com/fileadmin/user_upload/dyna_content/US/documents/KnowledgePanel_Recruitment_Sample_Survey_Methodology.pdf. Accessed April 1, 2019
- 28.Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32(6):725-737. doi: 10.1111/dme.12651 [DOI] [PubMed] [Google Scholar]
- 29.Flynn TN, Louviere JJ, Peters TJ, Coast J. Best-worst scaling: what it can do for health care research and how to do it. J Health Econ. 2007;26(1):171-189. doi: 10.1016/j.jhealeco.2006.04.002 [DOI] [PubMed] [Google Scholar]
- 30.Cheung KL, Wijnen BF, Hollin IL, et al. Using best-worst scaling to investigate preferences in health care. Pharmacoeconomics. 2016;34(12):1195-1209. doi: 10.1007/s40273-016-0429-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wittenberg E, Bharel M, Bridges JF, Ward Z, Weinreb L. Using best-worst scaling to understand patient priorities: a case example of Papanicolaou tests for homeless women. Ann Fam Med. 2016;14(4):359-364. doi: 10.1370/afm.1937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Fam Med. 2004;36(8):588-594. [PubMed] [Google Scholar]
- 33.Cruz M, Covinsky K, Widera EW, Stijacic-Cenzer I, Lee SJ. Predicting 10-year mortality for older adults. JAMA. 2013;309(9):874-876. doi: 10.1001/jama.2013.1184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolff JL, Boyd CM. A look at person- and family-centered care among older adults: results from a national survey. J Gen Intern Med. 2015;30(10):1497-1504. doi: 10.1007/s11606-015-3359-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sawtooth Software Inc The MaxDiff System technical paper, version 8. Sawtooth Software Technical Paper Series. https://www.sawtoothsoftware.com/download/techpap/maxdifftech.pdf. Published February 2013. Accessed April 2019.
- 36.Farrell B, Black C, Thompson W, et al. Deprescribing antihyperglycemic agents in older persons: evidence-based clinical practice guideline. Can Fam Physician. 2017;63(11):832-843. [PMC free article] [PubMed] [Google Scholar]
- 37.Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Review of deprescribing processes and development of an evidence-based, patient-centered deprescribing process. Br J Clin Pharmacol. 2014;78(4):738-747. doi: 10.1111/bcp.12386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Black CD, Thompson W, Welch V, et al. Lack of evidence to guide deprescribing of antihyperglycemics: a systematic review. Diabetes Ther. 2017;8(1):23-31. doi: 10.1007/s13300-016-0220-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Reeve E, To J, Hendrix I, Shakib S, Roberts MS, Wiese MD. Patient barriers to and enablers of deprescribing: a systematic review. Drugs Aging. 2013;30(10):793-807. doi: 10.1007/s40266-013-0106-8 [DOI] [PubMed] [Google Scholar]
- 40.Holmes HM, Todd A. The role of patient preferences in deprescribing. Clin Geriatr Med. 2017;33(2):165-175. doi: 10.1016/j.cger.2017.01.004 [DOI] [PubMed] [Google Scholar]
- 41.Turner JP, Edwards S, Stanners M, Shakib S, Bell JS. What factors are important for deprescribing in Australian long-term care facilities? perspectives of residents and health professionals. BMJ Open. 2016;6(3):e009781. doi: 10.1136/bmjopen-2015-009781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Palagyi A, Keay L, Harper J, Potter J, Lindley RI. Barricades and brickwalls: a qualitative study exploring perceptions of medication use and deprescribing in long-term care. BMC Geriatr. 2016;16:15. doi: 10.1186/s12877-016-0181-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schoenborn NL, Lee K, Pollack CE, et al. Older adults’ views and communication preferences around cancer screening cessation. JAMA Intern Med. 2017;177(8):1121-1128. doi: 10.1001/jamainternmed.2017.1778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Loudon K, Santesso N, Callaghan M, et al. Patient and public attitudes to and awareness of clinical practice guidelines: a systematic review with thematic and narrative syntheses. BMC Health Serv Res. 2014;14:321. doi: 10.1186/1472-6963-14-321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lambooij MS, Harmsen IA, Veldwijk J, et al. Consistency between stated and revealed preferences: a discrete choice experiment and a behavioural experiment on vaccination behaviour compared. BMC Med Res Methodol. 2015;15:19. doi: 10.1186/s12874-015-0010-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salampessy BH, Veldwijk J, Jantine Schuit A, et al. The predictive value of discrete choice experiments in public health: an exploratory application. Patient. 2015;8(6):521-529. doi: 10.1007/s40271-015-0115-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Silbert R, Salcido-Montenegro A, Rodriguez-Gutierrez R, Katabi A, McCoy RG. Hypoglycemia among patients with type 2 diabetes: epidemiology, risk factors, and prevention strategies. Curr Diab Rep. 2018;18(8):53. doi: 10.1007/s11892-018-1018-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Survey Instrument Content
eTable. Participant Perceptions of the Relationship Between Different Factor Levels and Aggressiveness of Diabetes Treatment, Stratified by Self-reported Diabetes Duration