Abstract
Background:
With the rise of adolescent sports participation, there has been a concomitant increase in not only the incidence but also the treatment of traumatic shoulder instability. Yet, there have been limited data on the failure rates of arthroscopic shoulder stabilization in this population as well as the potential risk factors.
Purpose/Hypothesis:
The purpose of this study was to determine the failure rates of adolescent patients who underwent arthroscopic labral reconstruction for traumatic anterior shoulder instability. We hypothesized that adolescent failure rates would be significantly higher than what has been reported in the adult population with regard to recurrent instability after surgical intervention.
Study Design:
Case series; Level of evidence, 4.
Methods:
This was a retrospective cohort study performed at a single center. Inclusion criteria consisted of all adolescent-aged patients identified who (1) had traumatic anterior shoulder instability, (2) had radiographic findings consistent with anteroinferior capsulolabral injury, and (3) underwent arthroscopic shoulder stabilization. Patient demographics, clinical presentation, imaging, intraoperative findings, and postoperative outcomes were analyzed.
Results:
A total of 36 patients were identified, with a mean ± SD follow-up of 35.6 ± 13.8 months. The mean patient age at the time of the index procedure was 16.03 ± 1.67 years. All patients underwent arthroscopic shoulder stabilization consisting of arthroscopic Bankart repair. Twelve patients (33.3%) reported either recurrent instability or apprehension, of whom 9 (25.0%) developed recurrent dislocation/subluxation at a mean of 20.67 months postoperatively (range, 16-51 months). No single sport was associated with a statistically significant increased risk of redislocation, although a trend was seen toward those with postoperative participation in high-risk sporting activity. Patients who redislocated their shoulders had a higher frequency of a Hill-Sachs lesion on magnetic resonance imaging (89%) compared with those who did not (52%, P = .048). History of multiple preoperative dislocations, presence of bony Bankart pathology, off-track lesions, and number of anchors utilized were not associated with postoperative dislocation/subluxation.
Conclusion:
This study demonstrates that adolescent patients treated with arthroscopic shoulder stabilization have a high rate of recurrent instability. The adolescent population may benefit from other stabilization strategies and/or activity modification. Further studies are necessary to determine the reasons for the high rate of redislocation and to develop strategies for prevention.
Keywords: shoulder instability, adolescent, Bankart, recurrence rate, arthroscopy, stabilization
Adolescent shoulder instability makes up only about 20% of all shoulder instability cases.5 However, when treated nonoperatively, adolescents are at an increased risk of recurrent instability compared with older patients, ranging anywhere from 48% to 100% in the literature.13,17,20 The anterior capsulolabral complex is the primary stabilizer against anterior dislocation.22 Consequently, Bankart repair is the most common surgical technique employed.32 While primary shoulder dislocations may initially be treated nonoperatively with physical therapy, arthroscopic intervention has been suggested for repeat instability.17,29
Deciding between operative and nonoperative management in the adolescent population can be challenging and has been a controversial topic of discussion.34 Taking into consideration the type of sport participation and preoperative imaging findings (soft tissue and bone) can be useful in determining which patients would benefit from surgical intervention. Recurrent instability results in persistent symptoms that interfere with sport participation and activities of daily living.31 In addition, repeat dislocations predispose patients to further injury to soft tissue stabilizers as well as bony constraints, which can necessitate larger, open stabilizations.1
Early studies on shoulder instability in young patients focused on military personnel or cadets between 18 and 26 years of age.7,12 Subsequent studies focusing on adolescents have shown that arthroscopic stabilization is associated with a decreased rate of recurrent shoulder instability,3,24,27 yet the overall recurrence rate after surgery based on limited reports in the literature is still high in this population, ranging from 18.75% to 25%.11,23,33 The reasons for these high failure rates remain unclear.
The purpose of the current study was to examine the recurrence rate and reasons for treatment failure for adolescent patients treated with arthroscopic stabilization for anterior shoulder instability. We hypothesized that adolescent patients would have a higher recurrence compared with the adult population, mainly owing to participation in high-demand sporting activity postoperatively.
Methods
This was a retrospective cohort study of a consecutive series of patients treated for traumatic shoulder instability at a single tertiary-care pediatric center. Institutional review board exemption status was obtained. A fellowship-trained pediatric orthopedic surgeon (N.K.P.) who had received training in pediatric and adolescent shoulder instability performed all surgical procedures.
Inclusion criteria consisted of patients between the ages of 13 and 18 years identified over a 4-year period (2012-2016) who (1) had reported traumatic anterior shoulder instability, (2) had radiographic findings consistent with anteroinferior capsulolabral injury, and (3) underwent arthroscopic anterior shoulder stabilization. Patients were excluded if they had multidirectional instability, ligamentous laxity, posterior instability, and >25% initial glenoid bone loss, which necessitated an open stabilization.
From the electronic medical record, patient age, sex, mechanism of injury, sporting activity, and number of prior shoulder dislocations were recorded. Patients were grouped as having a single dislocation versus multiple dislocations. Patients who had multiple dislocations could not reliably state the number of dislocations that they had, so the exact number was not recorded. Magnetic resonance imaging (MRI) was evaluated for labral injury pattern, Hill-Sachs lesions, glenoid bone loss, and the presence of on-track/off-track lesions as described by Gyftopoulos et al.18 Briefly, the glenoid track theory by Yamamoto et al28,37 emphasized the importance of evaluating both the glenoid and the humeral head. The glenoid track is defined as the contact area between the glenoid and the humeral head. If a Hill-Sachs lesion width is less than the glenoid track width, there is a decreased risk on engagement of the Hill-Sachs lesion on the glenoid defect, known as an “on-track” lesion. In contrast, if the width of the Hill-Sachs lesion is greater than the width of the glenoid track, there is a greater risk of engagement and persistent instability, known as an “off-track” lesion.
Intraoperative findings were recorded, including confirmation of labral and bony pathology, as well as procedures performed. Postoperative complications were noted, including recurrent dislocation/subluxation. This was defined as a documented dislocation or subluxation event as described by the patient and/or diagnosed by a health care provider. Patient-reported apprehension and repeat surgical procedures were also recorded. Total follow-up and time to return to sports were calculated as well. Those unable to attend the later follow-up appointments in person were interviewed by telephone, or a query of the electronic medical record was performed to determine if they had presented to other providers for recurrent instability or apprehension.
Surgical Procedure
Patients were treated surgically in the lateral decubitus position with a traction device after undergoing an interscalene block. Patients first had an examination under anesthesia, performed to confirm the degree of anterior instability as well as to assess range of motion. They then underwent a standard diagnostic arthroscopy to confirm the Bankart lesion and assess for bone loss, quality of labral tissue, and presence of an engaging Hill-Sachs lesion, as well as to treat additional pathology. Three portals were made in a standard fashion: a posterior viewing portal, with anteroinferior and anterosuperior portals for suture passage. After completion of diagnostic arthroscopy, the anteroinferior labrum was first liberated and mobilized off of the glenoid with a rasp. This glenoid was then prepared with a bur until bleeding bone was encountered for healing. A suture lasso device was then used to grasp the capsulolabral complex and to reestablish it on the glenoid as well as perform a capsular shift. The labrum was then fixed to the glenoid with 3 or 4 anchors (standard or knotless) based on the extent of the tear.
If an off-track lesion was identified, a remplissage was performed as described by Wolf et al.30,36 In brief, the suture anchor for the remplissage was placed prior to repair of the Bankart lesion. The arthroscope was placed through the anterior portal to confirm the Hill-Sachs lesion on the posterior aspect of the humeral head. A bur was used to decorticate the posterior aspect of the humeral head. A double-loaded biocomposite rotator cuff anchor was inserted into the defect. The Bankart repair was then performed as described here. At the completion of the anterior repair, the posterior sutures were then passed through the infraspinatus tendon and the posterior capsule, which was then tied in a “parachute” fashion, filling the defect.
Patients were placed into a shoulder immobilizer postoperatively for 6 weeks in 30° of external rotation. They progressed through a standard rehabilitation program concentrating on range of motion until 3 months postoperatively, strengthening from months 3 to 6, and sport-specific training from months 6 to 9. Patients returned to sport after sport-specific training was initiated and on the basis of their sport and activity demands. Patients were regularly evaluated at approximately 6 weeks, 3 months, 6 months, and 12 months and annually thereafter.
Statistical Analysis
Statistical analysis was performed to assess the relationship between recurrent dislocation/subluxation and the variables collected. Data analysis was performed with the Student t test and Fisher exact test with JMP statistical software v 14 (SAS). Statistical significance was set at a level of .05.
Results
A total of 36 study patients were identified, with a mean ± SD follow-up of 35.6 ± 13.8 months (range, 12.3-69.9 months). The mean patient age at the time when the index procedure was performed was 16.03 ± 1.67 years. There was a history of multiple dislocations prior to surgery in 33 of the patients (92%), and 29 patients were involved in sports at the time of initial injury. Table 1 presents characteristics of the initial injury.
Table 1.
Demographics and History of Patients With and Without Dislocation/Subluxation After Surgery
| Did Not Redislocate (n = 27) | Redislocated (n = 9) | ||||
|---|---|---|---|---|---|
| n | % | n | % | P Value | |
| Sports related | 18 | 66.67 | 6 | 66.67 | >.999 |
| History of multiple dislocations | 24 | 88.89 | 9 | 100.00 | .558 |
All patients underwent arthroscopic shoulder stabilization consisting of arthroscopic Bankart repair. In addition, 6 patients who had off-track lesions underwent a remplissage; 5 patients also underwent a posterior labral repair; and 2 patients underwent concurrent repair for a SLAP (superior labrum anterior and posterior) lesion.
Overall, 9 patients (25%) developed repeat instability following surgery. This occurred on average 20.67 months postoperatively (range, 16-51 months). Of those who had repeat instability, 2 underwent revision surgery, which consisted of a Latarjet procedure performed by another surgeon. The other 7 patients elected to perform physical therapy. Three patients (8.3%) noted feelings of apprehension in their shoulder at final follow-up, without documented dislocation or subluxation.
Of the 29 patients who were involved in sports prior to surgery, 24 (82.8%) returned to sports at a mean 7 months after surgery (range, 5-12 months). Five patients (17.2%) did not return to sports during the follow-up period. Engagement in sporting activity preoperatively (66.7% sport-related dislocation vs 66.7% non–sports related dislocations, P ≥ .999) was not associated with a risk of recurrent dislocation after surgery.
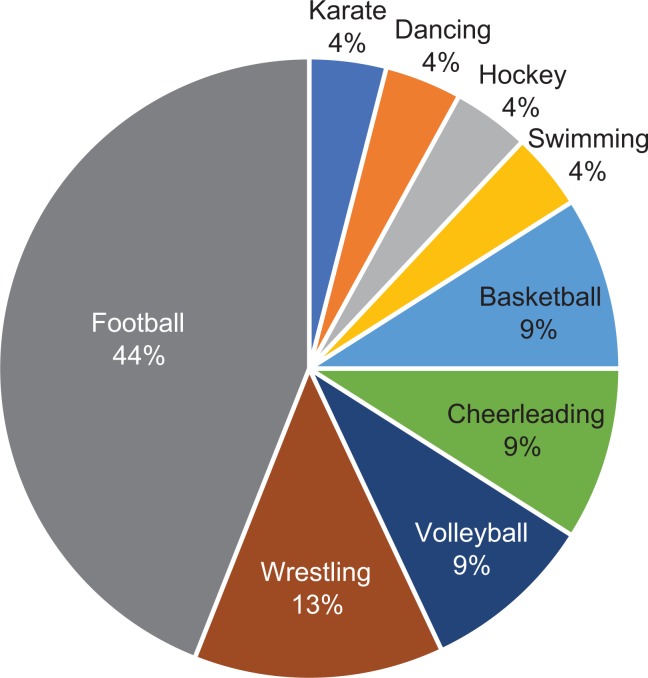
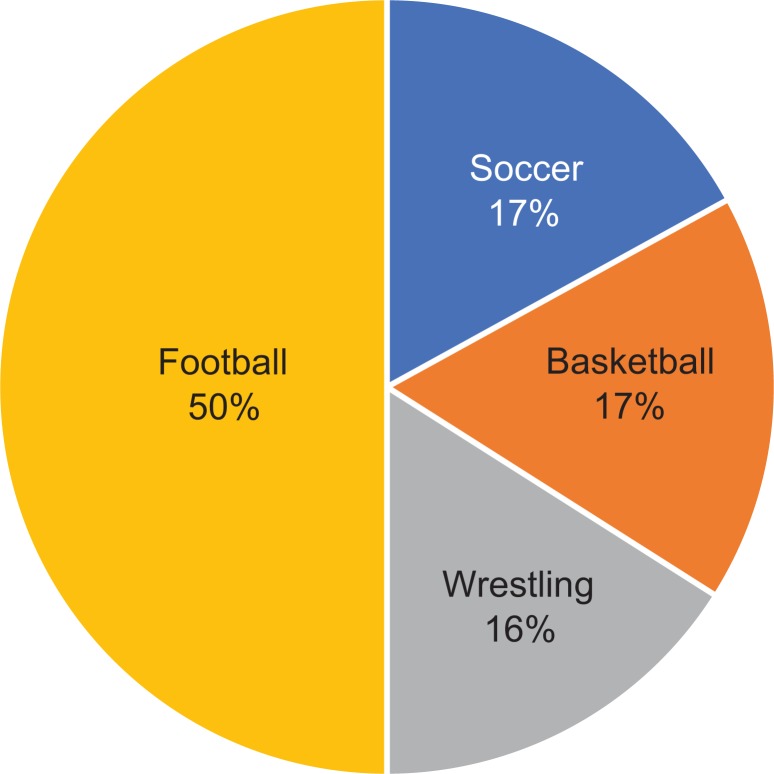
No single sport was associated with a statistically significantly increased risk of recurrence after surgery. American football was the most common sport in both the stable and redislocated groups, constituting 44% and 50% of cases, respectively, as seen in Figures 1 and 2.
Figure 1.
Most common sports-related shoulder dislocations for patients who did not redislocate after surgery. Represents sports played prior to surgery.
Figure 2.
Most common sports-related shoulder dislocations for patients who redislocated after surgery.
Although involvement in high-risk (contact) sports did show a trend (P = .07) toward recurrent dislocation after surgery, with 100% involvement in the recurrent group (soccer, football, basketball, wrestling) versus 64% in the nonrecurrent group (football, wrestling, karate, hockey, basketball), the difference was not statistically significant. In addition, history of multiple dislocations prior to surgery was not associated with a risk of recurrence (89% in the nonrecurrent group vs 100% in the recurrent group; P = .55).
There was a statistically significant increase in redislocation in patients who had evidence of a Hill-Sachs lesion on MRI (52% vs 88.9%; P = .048). Other preoperative MRI findings, including bony Bankart and off-track lesions, were not associated with a risk of redislocation (Table 2).
Table 2.
MRI Findings in Patients With and Without Dislocation/Subluxation After Surgerya
| Did Not Redislocate (n = 27) | Redislocated (n = 9) | ||||
|---|---|---|---|---|---|
| n | % | n | % | P Value | |
| Bankart | |||||
| Soft tissue | 20 | 74.07 | 6 | 66.67 | .686 |
| Bony | 7 | 25.93 | 3 | 33.33 | .686 |
| Hill-Sachs | 14 | 51.85 | 8 | 88.89 | .048b |
| Off-track glenoid | 5 | 18.52 | 1 | 11.11 | >.999 |
| Rotator cuff tendinosis | 14 | 51.85 | 4 | 44.44 | >.999 |
| Posterior labral tear | 2 | 7.41 | 1 | 11.11 | >.999 |
| SLAP tear | 7 | 25.93 | 1 | 11.11 | .648 |
aMRI, magnetic resonance imaging; SLAP, superior labrum anterior and posterior.
bStatistically significant difference between groups (P < .05).
Finally, neither intraoperative stabilization strategy nor intraoperative findings (Table 3) were associated with a higher incidence of postoperative recurrence. On average, 3.78 ± 1.19 anchors were used in patients who did not dislocate after surgery, compared with 4.11 ± 0.89 in patients who did redislocate (P = .45).
Table 3.
Intraoperative Findings in Patients With and Without Dislocation/Subluxation After Surgerya
| Did Not Redislocate (n = 27) | Redislocated (n = 9) | ||||
|---|---|---|---|---|---|
| n | % | n | % | P Value | |
| Friable anterior labral tissue | 16 | 59.26 | 6 | 66.67 | >.999 |
| Bankart | |||||
| Soft tissue | 22 | 81.48 | 6 | 66.67 | .384 |
| Bony | 5 | 18.52 | 3 | 33.33 | .384 |
| Hill-Sachs | |||||
| Nonengaging | 15 | 55.56 | 4 | 44.44 | .706 |
| Engaging | 3 | 11.11 | 1 | 11.11 | >.999 |
| Posterior labral tear | 3 | 11.11 | 2 | 22.22 | .581 |
| SLAP lesion | 4 | 14.81 | 1 | 11.11 | >.999 |
aSLAP, superior labrum anterior and posterior.
Discussion
The principal finding of this study was the 33.3% rate of either a recurrent instability event or apprehension after surgery, with 25% of patients having a full dislocation/subluxation event following surgery. This is consistent with other studies in the literature.11,23,33 The recurrence rate of 25% in this cohort was similar to the 14% to 21% reported in a recent systematic review by Longo et al.26 Furthermore, in a retrospective cohort study of 65 adolescent patients who underwent arthroscopic stabilization, Castagna et al10 determined the rate of recurrence after arthroscopic capsulolabral repair to be 21%.
Some studies have demonstrated lower failure rates. A larger comparative study by Gigis et al16 compared recurrence rates between first-time shoulder dislocations in an adolescent population treated with and without surgery. They found a recurrence rate of 70.3% in 27 adolescents treated nonoperatively, as opposed to 13.1% of 43 patients treated operatively. However, we believe that the lower failure rates seen in a subset of studies are in part due to the fact that certain patients were treated with stabilization after their first dislocation.
In the present study, 33 of the 36 patients had multiple dislocations prior to undergoing surgical intervention. Capsular, labral, and bony restraints can become attenuated with repeat dislocations.4,15 In addition, the lower failure rate seen in other studies may be attributed to the fact that many of these surgical procedures were performed on patients with first-time dislocations. As long-term outcome studies have demonstrated, not all adolescent patients with first-time dislocations treated nonoperatively will develop repeat instability.20 It is possible that some of these patients who underwent stabilization after their initial dislocation may have been successfully treated without surgery. Of note, the patients in our series who were treated after a first-time dislocation had pure soft tissue injuries (no bony involvement) intraoperatively, with excellent tissue quality in comparison with the multiple dislocators. Hence, part of the reason for the higher failure rate in this population may be the greater number of dislocations prior to intervention. The patients in our series who had multiple dislocations presented to our facility after having been treated nonoperatively at other institutions. Rarely are patients who have suffered multiple dislocations treated nonoperatively after entering our care.
Unlike other studies, we examined additional factors, such as preoperative MRI findings, including the presence of an off-track versus on-track glenoid, as well as intraoperative findings. These additional factors (ie, bony pathology) can be postulated to be the reasons for the higher rate of repeat instability in the adolescent population compared with the rate in the adult population, which ranges between 7% and 15% in the literature.2,6,12 Patients who redislocated had a higher frequency of a Hill-Sachs lesion on MRI (89%) compared with those who did not redislocate (52%; P = .048). In addition, only 1 of 6 patients who had off-track lesions had a postoperative dislocation/subluxation (all of whom had remplissage procedures). This may indicate that we should have a lower threshold for performing a remplissage in this population. In a systematic review, Buza et al9 found a repeat recurrence rate of 5.4% in patients who underwent a remplissage. Furthermore, Hughes et al21 compared a cohort of patients who underwent Bankart-only repair with a cohort that had Bankart repair with remplissage and found a significantly higher rate of recurrence in the Bankart-only group. Hence, the addition of a remplissage in this population may be advocated to prevent repeat instability, particularly when there is an off-track or engaging Hill-Sachs lesion. In addition, it is important to note that none of our patients had >25% glenoid bone loss at the time of their stabilization procedure; therefore, our cohort was not a population for which the indications for arthroscopy were stretched.
Yet, while accounting for other factors, such as mechanism of injury, sports participation, and pre- and intraoperative pathology, there was still a high rate of recurrent instability that cannot be simply explained by the presence of a Hill-Sachs lesion. As with anterior cruciate ligament tears, the increased rate of recurrent dislocation in adolescents versus older patients has been attributed to the active nature of adolescents, who often engage in early high-risk activities, particularly collision sports.23 Although not statistically significant, involvement in high-risk sports did show a trend (P = .07) toward recurrent dislocation after surgery, with 100% involvement in the recurrent group. Previous reports had similar findings.33 Torrance et al35 examined 67 adolescent rugby patients and found a recurrence rate of 51% in this high-demand cohort.
Although not studied directly in our population, younger patients may be less compliant with physical therapy and activity restrictions. Because physical therapy has been shown to be an important component of management of shoulder instability,19 limited access to or noncompliance with physical therapy among adolescents could certainly be a contributing factor in the higher incidence of recurrent instability. Further, multicenter study is necessary to determine modifiable risk factors beyond more aggressive stabilization strategies. In addition, a larger sample is needed to apply logistic regression to address covariables that we were unable to address in this study, given the relatively small sample. It is possible that there were interactions among covariates whose effect on recurrence could be studied with a larger sample.
The study has several limitations, including the relatively midterm follow-up (mean ± SD, 35.6 ± 13.8 months). However, the majority of patients in this study who did redislocate did so within 12 months. Another limitation is the lack of pre- and postoperative clinical outcome scores. However, the primary outcome measure of repeat instability may be independent of functional outcome scores. In a retrospective cohort study by Jones et al,23 adolescent patients who underwent nonoperative treatment had similar scores on the Single Assessment Numerical Evaluation (SANE) to patients undergoing early arthroscopic Bankart repair. In addition, the retrospective study by Castagna et al10 of 65 adolescent patients who underwent arthroscopic stabilization found that the recurrence rate following surgery was not correlated with postoperative scores (P = .556 for SANE score, P = .753 for Rowe score, and P = .478 for American Shoulder and Elbow Surgeons score). Although postoperative scores did not correlate with recurrence rate in these studies, benefit from surgery has been well established.26 A systematic review by Zaremski et al38 found an increased risk of repeat instability in patients treated nonoperatively versus surgically (odds ratio = 13.41; 99% CI, 3.60-49.93; P < .001). Recurrent instability can negatively affect quality of life and prohibit patients from participating in or returning to sports.14,25 It has also been postulated that recurrent shoulder instability can contribute to early degenerative change.8,20
In light of the findings of this study as well as the findings in the existing literature highlighted here, we believe that more aggressive stabilization to prevent recurrent instability in adolescent patients may be warranted. This population has consistently demonstrated a relatively high rate of failure after arthroscopic stabilization, which may be due to not only the degree of bony injury (ie, Hill-Sachs) but also involvement in high-risk activities such as collision sports. The addition of a remplissage to Bankart repair, a lower threshold for open stabilization procedures, and modification of postoperative activity may be components of a multipronged prevention program. Prospective, multicenter studies are necessary to determine the reasons for the high rate of redislocation in this population and develop strategies for prevention. Operative intervention may be indicated in first-time dislocators in this age group to prevent repeat instability.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: N.K.P. is a consultant for OrthoPediatrics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the institutional review board of University of California, San Francisco Benioff Children’s Hospital Oakland (160929B).
References
- 1. Allain J, Goutallier D, Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80:841–852. [DOI] [PubMed] [Google Scholar]
- 2. Bacilla P, Field LD, Savoie FH. Arthroscopic Bankart repair in a high demand patient population. Arthroscopy. 1997;13:51–60. [DOI] [PubMed] [Google Scholar]
- 3. Baumgartner G, Slongo T, Kohler G, Horst M, Lampert C. Traumatic shoulder dislocation in children and adolescents. European Journal of Trauma. 2003;29:375–378. [Google Scholar]
- 4. Bigliani LU, Newton PM, Steinmann SP, Connor PM, Mcllveen SJ. Glenoid rim lesions associated with recurrent anterior dislocation of the shoulder. Am J Sports Med. 1998;26:41–45. [DOI] [PubMed] [Google Scholar]
- 5. Bishop JY, Flatow EL. Pediatric shoulder trauma. Clin Orthop Relat Res. 2005;432:41–48. [DOI] [PubMed] [Google Scholar]
- 6. Boileau P, Villalba M, Héry J-Y, Balg F, Ahrens P, Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88:1755–1763. [DOI] [PubMed] [Google Scholar]
- 7. Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med. 2002;30:576–580. [DOI] [PubMed] [Google Scholar]
- 8. Brophy RH, Marx RG. Osteoarthritis following shoulder instability. Clin Sports Med. 2005;24:47–56. [DOI] [PubMed] [Google Scholar]
- 9. Buza JA, Iyengar JJ, Anakwenze OA, Ahmad CS, Levine WN. Arthroscopic Hill-Sachs remplissage: a systematic review. J Bone Joint Surg Am. 2014;96:549–555. [DOI] [PubMed] [Google Scholar]
- 10. Castagna A, Delle Rose G, Borroni M, et al. Arthroscopic stabilization of the shoulder in adolescent athletes participating in overhead or contact sports. Arthroscopy. 2012;28:309–315. [DOI] [PubMed] [Google Scholar]
- 11. Chapus V, Rochcongar G, Pineau V, Salle de Chou É, Hulet C. Ten-year follow-up of acute arthroscopic Bankart repair for initial anterior shoulder dislocation in young patients. Orthop Traumatol Surg Res. 2015;101:889–893. [DOI] [PubMed] [Google Scholar]
- 12. DeBerardino TM, Arciero RA, Taylor DC, Uhorchak JM. Prospective evaluation of arthroscopic stabilization of acute, initial anterior shoulder dislocations in young athletes: two- to five-year follow-up. Am J Sports Med. 2001;29:586–592. [DOI] [PubMed] [Google Scholar]
- 13. Deitch J, Mehlman CT, Foad SL, Obbehat A, Mallory M. Traumatic anterior shoulder dislocation in adolescents. Am J Sports Med. 2003;31:758–763. [DOI] [PubMed] [Google Scholar]
- 14. Dickens JF, Owens BD, Cameron KL, et al. Return to play and recurrent instability after in-season anterior shoulder instability: a prospective multicenter study. Am J Sports Med. 2014;42:2842–2850. [DOI] [PubMed] [Google Scholar]
- 15. Edwards TB, Boulahia A, Walch G. Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy. 2003;19:732–739. [DOI] [PubMed] [Google Scholar]
- 16. Gigis I, Heikenfeld R, Kapinas A, Listringhaus R, Godolias G. Arthroscopic versus conservative treatment of first anterior dislocation of the shoulder in adolescents. J Pediatr Orthop. 2014;34:421–425. [DOI] [PubMed] [Google Scholar]
- 17. Good CR, MacGillivray JD. Traumatic shoulder dislocation in the adolescent athlete: advances in surgical treatment. Curr Opin Pediatr. 2005;17:25–29. [DOI] [PubMed] [Google Scholar]
- 18. Gyftopoulos S, Beltran LS, Bookman J, Rokito A. MRI evaluation of bipolar bone loss using the on-track off-track method: a feasibility study. AJR Am J Roentgenol. 2015;205:848–852. [DOI] [PubMed] [Google Scholar]
- 19. Hayes K, Callanan M, Walton J, Paxinos A, Murrell GAC. Shoulder instability: management and rehabilitation. J Orthop Sports Phys Ther. 2002;32:497–509. [DOI] [PubMed] [Google Scholar]
- 20. Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–1684. [DOI] [PubMed] [Google Scholar]
- 21. Hughes JL, Bastrom T, Pennock AT, Edmonds EW. Arthroscopic Bankart repairs with and without remplissage in recurrent adolescent anterior shoulder instability with Hill-Sachs deformity. Orthop J Sports Med. 2018;6(12):2325967118813981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Jobe FW, Giangarra CE, Kvitne RS, Glousman RE. Anterior capsulolabral reconstruction of the shoulder in athletes in overhand sports. Am J Sports Med. 1991;19:428–434. [DOI] [PubMed] [Google Scholar]
- 23. Jones KJ, Wiesel B, Ganley TJ, Wells L. Functional outcomes of early arthroscopic Bankart repair in adolescents aged 11 to 18 years. J Pediatr Orthop. 2007;27:209–213. [DOI] [PubMed] [Google Scholar]
- 24. Khan A, Samba A, Pereira B, Canavese F. Anterior dislocation of the shoulder in skeletally immature patients: comparison between non-operative treatment versus open Latarjet’s procedure. Bone Joint J. 2014;96:354–359. [DOI] [PubMed] [Google Scholar]
- 25. Kirkley A, Griffin S, McLintock H, Ng L. The development and evaluation of a disease-specific quality of life measurement tool for shoulder instability: the Western Ontario Shoulder Instability Index (WOSI). Am J Sports Med. 1998;26:764–772. [DOI] [PubMed] [Google Scholar]
- 26. Longo UG, van der Linde JA, Loppini M, Coco V, Poolman RW, Denaro V. Surgical versus nonoperative treatment in patients up to 18 years old with traumatic shoulder instability: a systematic review and quantitative synthesis of the literature. Arthroscopy. 2016;32:944–952. [DOI] [PubMed] [Google Scholar]
- 27. Ochs BG, Rickert M, Schmelzer-Schmied N, Loew M, Thomsen M. Posttraumatische Schulterinstabilitt im Wachstumsalter. Orthopade. 2005;34:152–158. [DOI] [PubMed] [Google Scholar]
- 28. Omori Y, Yamamoto N, Koishi H, et al. Measurement of the glenoid track in vivo as investigated by 3-dimensional motion analysis using open MRI. Am J Sports Med. 2014;42:1290–1295. [DOI] [PubMed] [Google Scholar]
- 29. Pandya NK, Namdari S. Shoulder arthroscopy in children and adolescents. J Am Acad Orthop Surg. 2013;21:389–397. [DOI] [PubMed] [Google Scholar]
- 30. Purchase RJ, Wolf EM, Hobgood ER, Pollock ME, Smalley CC. Hill-Sachs “remplissage”: an arthroscopic solution for the engaging Hill-Sachs lesion. Arthroscopy. 2008;24:723–726. [DOI] [PubMed] [Google Scholar]
- 31. Robinson CM, Howes J, Murdoch H, Will E, Graham C. Functional outcome and risk of recurrent instability after primary traumatic anterior shoulder dislocation in young patients. J Bone Joint Surg Am. 2006;88:2326–2336. [DOI] [PubMed] [Google Scholar]
- 32. Rowe CR, Patel D, Southmayd WW. The Bankart procedure: a long-term end-result study. J Bone Joint Surg Am. 1978;60:1–16. [PubMed] [Google Scholar]
- 33. Shymon SJ, Roocroft J, Edmonds EW. Traumatic anterior instability of the pediatric shoulder: a comparison of arthroscopic and open Bankart repairs. J Pediatr Orthop. 2015;35:1–6. [DOI] [PubMed] [Google Scholar]
- 34. Taylor DC, Krasinski KL. Adolescent shoulder injuries: consensus and controversies. J Bone Joint Surg Am. 2009;91:462–473. [PubMed] [Google Scholar]
- 35. Torrance E, Clarke CJ, Monga P, Funk L, Walton MJ. Recurrence after arthroscopic labral repair for traumatic anterior instability in adolescent rugby and contact athletes. Am J Sports Med. 2018;46(12):2969–2974. [DOI] [PubMed] [Google Scholar]
- 36. Wolf EM, Arianjam A. Hill-Sachs remplissage, an arthroscopic solution for the engaging Hill-Sachs lesion: 2- to 10-year follow-up and incidence of recurrence. J Shoulder Elbow Surg. 2014;23:814–820. [DOI] [PubMed] [Google Scholar]
- 37. Yamamoto N, Itoi E, Abe H, et al. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: a new concept of glenoid track. J Shoulder Elbow Surg. 2007;16:649–656. [DOI] [PubMed] [Google Scholar]
- 38. Zaremski JL, Galloza J, Sepulveda F, Vasilopoulos T, Micheo W, Herman DC. Recurrence and return to play after shoulder instability events in young and adolescent athletes: a systematic review and meta-analysis. Br J Sports Med. 2017;51:177–184. [DOI] [PubMed] [Google Scholar]