Abstract
Introduction:
Current economic evaluations of school-based caries prevention programs (SCPPs) do not compare multiple types of SCPPs against each other and do not consider teeth beyond permanent first molars.
Objectives:
To assess the cost-effectiveness of a comprehensive SCPP relative to an SCPP focused on delivering sealants for permanent first molars only and to a default of no SCPP. Based on a societal perspective, a simulation model was used that compared the health and cost impacts on 1) permanent first molars only and 2) all posterior teeth.
Methods:
To calibrate the model, we used data from CariedAway, a comprehensive SCPP that used glass ionomer to prevent and arrest active decay among children. We then evaluated the incremental cost-effectiveness of implementing 3 alternate school-based approaches (comprehensive, sealant only, and no program) on only first molars and all posterior teeth. Probabilistic, 1-, and 2-way sensitivity analyses are included for robustness. Cost-effectiveness is assessed with a threshold of $54,639 per averted disability-adjusted life year (DALY).
Results:
We first compared the 3 programs under the assumption of treating only first molars. This assessment indicated that CariedAway was less cost-effective than school-based sealant programs (SSPs): the resulting incremental cost-effectiveness ratio (ICER) for CariedAway versus SSPs was $283,455 per averted DALY. However, when the model was extended to include CariedAway’s treatment of all posterior teeth, CariedAway was not only cost-effective but also cost-saving relative to SSPs (ICER, –$943,460.88 per averted DALY; net cost, –$261.45) and no SCPP (ICER, –$400,645.52 per averted DALY; net cost, –$239.77).
Conclusions:
This study finds that economic evaluations assessing only cost and health impacts on permanent first molars may underestimate the cost-effectiveness of comprehensive SCPPs 1) preventing and arresting decay and 2) treating all teeth. Hence, there is an urgent need for economic evaluations of SCPPs to assess cost and health impacts across teeth beyond only permanent first molars.
Knowledge Transfer Statement:
The results of this study can be used by policy makers to understand how to evaluate economic evaluations of school-based caries prevention programs and what factors to consider when deciding on what types of programs to implement.
Keywords: cost-benefit analysis, school health services, preventive dentistry, evidence-based dentistry, dental care for children, economics
Introduction
School-based sealant programs (SSPs) delivering focused prevention for permanent first molars (1Ms) were found to be effective and cost-saving for high-risk populations relative to the alternative of no treatment (Griffin et al. 2016; Griffin et al. 2017; Akinlotan et al. 2018). Given the limited public resources for oral health care (Mariño et al. 2013), the economic evaluations generating these conclusions should be lauded for highlighting that community-level preventive dental interventions can improve population oral health and be an economically feasible area in which to invest (Griffin et al. 2016; Griffin et al. 2017; Akinlotan et al. 2018). However, economic evaluations of SSPs have 2 existing critical flaws: 1) they do not compare SSPs with alternative school-based caries prevention programs (SCPPs), and 2) they do not include outcomes for non-1M teeth. Hence, current economic evaluations of SSPs are critically flawed because they do not represent real-world scenarios for decision makers.
As a concrete example of point 1, SCPPs can provide comprehensive care by incorporating multiple caries prevention treatments on multiple teeth. This is in contrast to the focused treatment currently delivered by and recommended for SSPs for 1Ms only (Griffin et al. 2016; Griffin et al. 2017; Akinlotan et al. 2018). Although the impact on health outcomes and costs is unknown (Community Preventive Services Task Force 2016), prior work hypothesized that comprehensive SCPPs implementing primary and secondary prevention for all teeth may offer significant clinical and cost benefits (Niederman et al. 2017). The additional primary preventive agents could include, for example, toothpaste and fluoride varnish to prevent smooth surface caries and silver diamine fluoride to prevent pit and fissure caries. Secondary preventive agents to arrest frank caries could include interim therapeutic restorations and silver diamine fluoride. These SCPPs have already existed, but no economic evaluation to date has compared SSPs delivering focused prevention for only 1Ms with comprehensive SCPPs providing primary and secondary prevention for all teeth.
These 2 flaws are critical because economic evaluations should represent the decision-making processes faced by stakeholders and include all relevant alternatives. Economic evaluations not comparing focused SSPs with comprehensive SCPPs are not applicable to stakeholders who can choose among multiple types of SCPPs. Even if this first flaw was to be rectified, the second flaw of not including outcomes for non-1Ms would introduce bias into the economic evaluations if non-SSP programs treated non-1M teeth.
At best, flawed economic evaluations of SSPs are not used to inform decision making. At worst, current economic evaluations of SSPs may lead to suboptimal resource use. Determining whether SSPs with targeted care are a better use of resources relative to other types of SCPPs is impossible given current economic evaluations. Suboptimal resource use can severely limit the potential impact of SCPPs on oral health or spending on oral health. Even worse, suboptimal resource use and poor prior experiences with SCPPs may lead to a decreased willingness to participate in future iterations.
The research question of this article is therefore the following: What is the impact of including 1) SCPP with primary and secondary prevention into the typical “SSP versus no program” comparison and 2) non-1M outcomes in the conclusions of an economic evaluation?
Methods
Overview
To compare 1M sealant programs with other comprehensive SCPPs, we implemented a model framework previously used to evaluate the cost-effectiveness of SSPs relative to a no-SCPP alternative (Griffin et al. 2016). This model framework was then adapted to reflect 1) characteristics of the population under treatment in a single comprehensive SCPP and 2) how a comprehensive SCPP may affect caries differently from SSPs. Given the variation in economic evaluation methods used to evaluate SSPs alone, especially in health outcome measures (Akinlotan et al. 2018), using comparable methods and underlying assumptions from a prior model does the following: 1) increases the transparency of a potentially complicated economic evaluation and 2) succinctly clarifies any differences in how programs being compared are implemented and how this may affect estimates of cost and oral health outcomes.
Comprehensive SCPP Description
Data for this evaluation were derived from a comprehensive SCPP (called CariedAway) simultaneously implementing sealants on all pits and fissures, interim therapeutic restorations on all asymptomatic teeth, fluoride varnish on all teeth, and fluoride toothpaste. Care was provided to all primary and permanent teeth, twice annually. The program focused on elementary schools in which >50% of children participated in free or reduced-price meals, and it encompassed children aged 5 to 12 y in 50 Massachusetts elementary schools from 2003 to 2010 (Niederman et al. 2008; Bukhari 2016). The examination was carried out by a dentist, and care was provided by a dental hygienist. Diagnoses were made per a visual-tactile oral examination as specified by the diagnostic criteria and procedures of the oral health surveys of the National Institute of Dental Research (1991). This program differed significantly from SCPPs providing focused assessment and sealants for 1Ms once per year. Further description of CariedAway and data collection is available in the Appendix. The study received Institutional Review Board approval from the Forsyth Institute and the New York University School of Medicine.
Economic Analysis
Simulation Model
We used a simulation model to compare the net costs and impact on health outcomes resulting from treating children under SCPPs 1) sealing only 1Ms and 2) providing comprehensive caries prevention to all teeth. The 2 programs are compared with each other and a no-SCPP scenario, where sealants are assumed to not be applied in private practice, following prior literature (Griffin et al. 2014; Griffin et al. 2016; Griffin et al. 2017; Griffin et al. 2018). We compare comprehensive SCPPs, SSPs, and no SCPP because focused prevention for permanent 1Ms is the current recommendation for SSPs and because no SCPP is a default option for schools. We amplified the simulation model of Griffin et al. (2016), originally used to evaluate SSPs relative to no SCPP, to include the impact of comprehensive SCPPs on active caries and to explicitly model the potential impact of comprehensive caries prevention on all posterior teeth. Like Griffin et al., we model the impact on children targeted for intervention soon after the permanent 1Ms erupt into the mouth (between ages 6 and 7 y) based on a societal perspective and over a 5-y time horizon.
The primary health outcome, as with Griffin et al. (2016), is disability-adjusted life years (DALYs), where DALYs quantify the burden of disease from mortality and morbidity and are used in economic evaluations to inform health care resource allocation decisions (Murray 1994; Rushby and Hanson 2001; Whitehead and Ali 2010). A DALY of 1 represents a year in which normal activities are limited due to disease, injury, or disability, whereas a value of 0 represents perfect health. DALYs were calculated for toothaches by multiplying the likelihood of experiencing a toothache by the disability weight for a toothache (0.012) from the World Health Organization’s Global Burden of Disease study (Murray et al. 2012).
The net cost per averted DALY was calculated following the recommendations of the Second Panel on Cost-effectiveness in Health and Medicine. All costs were estimated from the societal perspective. Costs are reported in 2014 US dollars and converted where necessary with the consumer price index. Costs and health-related benefits are discounted with an annual rate of 3%, with the assumption that good health is valued immediately instead of later (Griffin et al. 2016).
All costs and outcomes were estimated per child, not per tooth. The comparison in the difference in health outcomes and economic costs between interventions is conducted with the incremental cost-effectiveness ratio (ICER). Following Griffin et al. (2016), cost-effectiveness is assessed with a threshold of $54,639 per averted DALY (the maximum dollar amount that society would be willing to spend per averted DALY).
The first extension to Griffin et al. (2016) adjusted the equations for net cost and averted DALYs to account for the impact of comprehensive prevention. Net cost for a comprehensive SCPP relative to no SCPP equaled resource costs minus filling costs for symptomatic cavities and lost productivity due to visiting the dentist for symptomatic cavities. Averted DALYs equaled the number of years with painful untreated cavities multiplied by the associated loss in health or well-being prevented by the sealants provided and the treatment of nonsymptomatic cavities. In contrast, net cost for SSPs relative to no SCPP equaled SSP resource costs minus filling costs for all cavities and lost productivity due to visiting the dentist for all occurring cavities. Similarly, averted DALYs in SSPs were the number of years with painful untreated cavities multiplied by the loss in health prevented only by sealants based on caries prevalence.
To highlight the impact of including all posterior teeth in the analysis, results from 2 versions of the model are reported. The first model considers only 1Ms (the 1M-only model), whereas the second model considers all posterior teeth (the posterior teeth model). As a result, the 1M-only model assumes that the only teeth at risk for cavities are 1Ms, while the posterior teeth model relaxes the assumption by allowing all posterior teeth to be at risk for cavities. Because current recommendations for SSPs suggest treating 1Ms only (Gooch et al. 2009), SSPs in the posterior teeth model are modeled to treat only 1Ms. Hence, non-1M posterior teeth treated under SSPs are not modeled to be at lower risk of cavities due to sealant application.
The extended Griffin et al. (2016) model was modified to reflect characteristics of CariedAway’s treated population. Additionally, the model was modified to match the 6-mo treatment cycles of CariedAway by using 6-mo cycles in the model, instead of the original 1-y cycles (Griffin et al. 2016). Following these changes, the costs and health effects were simulated over 5 y to reflect that 1) children enrolled in CariedAway had an average number of 2 visits per children (i.e., 1 y of treatment within CariedAway) and 2) the available literature on sealants indicates efficacy over 4 y (Griffin et al. 2016; Ahovuo-Saloranta et al. 2017).
We used baseline data from CariedAway to calibrate the model to the CariedAway-treated population. Further details on reporting, data collection, calibration, and standardization for CariedAway are provided in the Appendix.
Model Parameters
Cavity Attack Rate
We first estimated the cavity attack rates for 1Ms in the 1M-only model and all posterior teeth in the posterior teeth model using a published methodology (Griffin et al. 2018). The estimated 6-mo 1M cavity attack rate (the probability that a healthy 1M becomes carious) was 0.0366, while the estimated 6-mo non-1M posterior cavity attack rate was 0.0404. The overall estimated 6-mo posterior cavity attack rate was 0.0538 (see Appendix for detailed calculations). We used this approach for both models. We assumed that the 1M attack rate was common across all 1Ms and that the non-1M posterior attack rate was common across all non-1M posterior teeth.
Probability of a Symptomatic Cavity Given Carious Tooth
A symptomatic tooth was defined as any tooth with mobility, pain, swelling, fistula, or pulpal involvement. The probability of having a symptomatic tooth given a carious tooth was calculated by taking the mean percentage of posterior teeth with active decay deemed symptomatic across children aged 7 through 12 y at the first CariedAway visit, yielding a percentage of 6.7%.
Probability of Experiencing Toothache Given a Symptomatic Cavity
A carious tooth deemed symptomatic under CariedAway is assumed to lead to toothache with probability 1.
Effectiveness of SSPs and CariedAway
SSPs were previously modeled as sealing 1Ms in the first year with no follow-up (Griffin et al. 2016). After sealant placement, the percentage reduction in incidence and increment of caries due to sealants was estimated to be 68.5% for the first year, 57.9% at 2 y, 40.1% at 3 y, and 25.8% at 4 y (Griffin et al. 2016). To convert the percentage reduction in incidence and increment of caries due to sealants over 6-mo cycles, cavities are assumed to occur at a constant rate within each year. Sealant effectiveness for each year’s two 6-mo cycles is then estimated to be 82.8% at year 1, 76.1% at year 2, 63.3% at year 3, and 50.8% at year 4.
CariedAway was a 1-arm cohort study without a control group. Hence, sealants used in CariedAway were assumed to have the same effectiveness in preventing caries as those estimated previously (Griffin et al. 2016) in years following placement.
Traditional restorations were previously modeled to be fully effective in arresting caries (Griffin et al. 2016). Systematic reviews demonstrate the equivalence of amalgam restorations and interim therapeutic restorations in efficacy and 5-y longevity (Mickenautsch et al. 2010). Therefore, we assumed that interim therapeutic restorations are also fully effective in arresting caries.
Program Resource Costs
SSP resource costs come from prior work (Griffin et al. 2016). CariedAway program resource costs were derived from prior work (Niederman et al. 2008; Bukhari 2016). Annual cost per child, with 2 visits per year, was estimated to be $185.72, with the cost per child per visit being $92.86 (Bukhari 2016).
Other Parameters
Other parameters were taken from Griffin et al. (2016), including the probability that a cavity remains untreated, the probability of a toothache in a child with at least 1 untreated cavity, the loss in health or well-being caused by a toothache, SSP resource costs (at the per-child level), cost per filling, and productivity losses due to taking children to the dentist for a filling. Annual probabilities used by Griffin et al. were converted to 6-mo probabilities to adjust for the 6-mo cycles used in the model, based on the assumption that incidence rates are constant over 2 cycles (comprising 1 full year).
Further details on parameter values, distributions, and derivations are available in the Appendix.
Sensitivity Analyses
One-way Sensitivity Analysis
One-way sensitivity analyses assess the sensitivity of the model results to underlying parameter assumptions. Each parameter value was varied between 50% to 150% of its base-case value to test whether the analysis was sensitive to individual base-case parameter assumptions.
Probabilistic Sensitivity Analysis
Probabilistic sensitivity analyses account for parameter uncertainty in the model. The probabilistic sensitivity analysis was conducted for a population of 1,000 children, with 1,000 replications in the analysis. The distributions for random variables align with those used in Griffin et al. (2016), after adjustment for 6-mo cycle lengths of the model. This is used to construct confidence intervals around the estimates generated by the model.
Two-way Sensitivity Analysis
As there are not yet comprehensive data on how costs can vary across multiple comprehensive SCPPs or on how posterior attack rates can vary across SCPPs, we conducted a 2-way sensitivity analysis for posterior attack rates and CariedAway costs. As the underlying costs of comprehensive SCPPs may be higher with greater unmet need or higher attack rates in the population treated, these 2 parameters may be significantly correlated in practice. To examine how these correlations might affect conclusions of an economic evaluation, the 2 parameters were allowed to vary simultaneously between 50% and 150% of their base case values.
Results
Under the posterior teeth model, CariedAway is determined to be cost-saving relative to both alternative scenarios of no SCPP and SSPs. In Table 1, CariedAway averts an additional 364.6 fillings (95% CI, 320.8 to 379.4) per 1,000 children relative to SSPs and 640.5 fillings (95% CI, 559.0 to 710.4) relative to no SCPP. Averted fillings directly affect treatment costs for caries. As a result, CariedAway averts $375.80 (95% CI, $336.61 to $438.05) in treatment costs for caries relative to SSPs and $417.45 (95% CI, $367.45 to $497.84) relative to no SCPP. When averted treatment costs are compared with program costs, the resulting net costs are negative for CariedAway under all comparisons: CariedAway costs per child are $261.45 (95% CI, –$377.98 to –$245.50) less than the money saved in treatment and productivity costs relative to SSPs and $239.77 (95% CI, –$375.36 to –$214.70) relative to no SCPP. CariedAway also prevents losses in quality of life due to symptomatic untreated decay relative to SSPs, averting 0.025 y with a toothache per child (95% CI, 0.0164 to 0.0298). Hence, CariedAway unambiguously improves tooth-related outcomes and financial outcomes relative to SSPs.
Table 1.
Cost per Child: All Scenarios in the Posterior Teeth Model.
| Comparisons | Baseline Value | 95% CI |
|---|---|---|
| SSP vs. no school-based program | ||
| Averted treatment and productivity costs, $ | 41.65 | 30.26 to 59.97 |
| Net cost, $ | 21.68 | 3.36 to 33.07 |
| Averted fillings | 0.2760 | 0.1952 to 0.3755 |
| Averted years with toothache | 0.0292 | 0.0198 to 0.0418 |
| Averted DALYs | 0.0004 | 0.0002 to 0.0005 |
| Net cost per averted DALY, $ | 67,480.90 | 9,053.41 to 140,835.40 |
| CariedAway vs. SSP | ||
| Averted treatment and productivity costs, $ | 375.80 | 336.62 to 438.05 |
| Net cost, $ | –261.45 | –377.98 to –245.50 |
| Averted fillings | 0.3646 | 0.3208 to 0.3794 |
| Averted years with toothache | 0.0250 | 0.0164 to 0.0298 |
| Averted DALYs | 0.0003 | 0.0002 to 0.0003 |
| Net cost per averted DALY, $ | –943,460.88 | –1,900,602.29 to –843,620.50 |
| CariedAway vs. no school-based program | ||
| Averted treatment and productivity costs, $ | 417.45 | 367.45 to 497.84 |
| Net cost, $ | –239.77 | –375.36 to –214.70 |
| Averted fillings | 0.6405 | 0.5590 to 0.7104 |
| Averted years with toothache | 0.0499 | 0.0363 to 0.0635 |
| Averted DALYs | 0.0006 | 0.0004 to 0.0008 |
| Net cost per averted DALY, $ | –400,645.52 | –717,980.96 to –359,738.33 |
DALY, disability-adjusted life year; SSP, school-based sealant program.
In contrast to the posterior teeth model, the 1M-only model concludes that SSPs unambiguously dominate CariedAway (Table 2), but it is inconclusive on whether SSPs are cost-effective relative to the no-SCPP scenario. The first conclusion results from the 1M-only model not accounting for the impact of CariedAway on active decay and decay prevention across non-1M posterior teeth. Although CariedAway averted 232.8 more fillings per 1,000 children than SSPs (95% CI, 212.0 to 236.1) and prevented 0.0252 y with a toothache per child (95% CI, 0.0163 to 0.0298), the number of averted fillings and the gain in quality of life due to averted toothaches was not sufficient to overcome the higher program costs of CariedAway relative to SSPs. The resulting ICER for CariedAway versus SSPs was $283,455.81 per averted DALY, which was over the cost-effectiveness threshold of $54,639 per averted DALY. This indicates that CariedAway is not cost-effective when compared with SSPs. However, the ICER for SSPs versus no SCPP was $67,019.10 per averted DALY, indicating that no SCPP is the dominant scenario. The 1M-only model is ultimately inconclusive on SSPs versus no SCPP because of significant uncertainty surrounding the comparison: the 95% CI for SSP versus no SCPP in the 1M-only model (between $10,236.26 and $87,105.05 per DALY averted) includes the cost-effectiveness threshold of $54,639 per DALY averted. The 1M-only model unambiguously concludes, however, that SSPs dominate CariedAway when only 1Ms are considered in the analysis.
Table 2.
Costs per Child: All Scenarios in the 1M-Only Model (Permanent First Molars Only).
| Baseline Value | 95% CI | |
|---|---|---|
| SSP vs. no school-based program | ||
| Averted treatment and productivity costs, $ | 41.64 | 29.52 to 57.86 |
| Net cost, $ | 21.69 | 5.47 to 33.81 |
| Averted fillings | 0.2759 | 0.1946 to 0.3755 |
| Averted years with toothache | 0.0294 | 0.0192 to 0.0416 |
| Averted DALYs | 0.0004 | 0.0002 to 0.0005 |
| Net cost per averted DALY, $ | 67,019.10 | 13,654.33 to 149,054.09 |
| CariedAway vs. SSP | ||
| Averted treatment and productivity costs, $ | 35.22 | 30.78 to 37.76 |
| Net cost, $ | 79.13 | 76.60 to 83.57 |
| Averted fillings | 0.2328 | 0.2120 to 0.2361 |
| Averted years with toothache | 0.0252 | 0.0163 to 0.0298 |
| Averted DALYs | 0.0002 | 0.0002 to 0.0003 |
| Net cost per averted DALY, $ | 283,455.81 | 236,310.95 to 449,453.12 |
| CariedAway vs. no school-based program | ||
| Averted treatment and productivity costs, $ | 76.86 | 63.79 to 91.14 |
| Net cost, $ | 100.83 | 86.55 to 113.90 |
| Averted fillings | 0.5087 | 0.4304 to 0.5881 |
| Averted years with toothache | 0.0502 | 0.0356 to 0.0622 |
| Averted DALYs | 0.0006 | 0.0004 to 0.0007 |
| Net cost per averted DALY, $ | 167,242.23 | 124,027.26 to 253,259.32 |
The 95% CIs are constructed with the probabilistic sensitivity analysis, which was conducted with 1,000 replications. Each replication was composed of a random draw from each distribution for input parameters in the model and generated cost and health outcome outputs.
1M, first molar; DALY, disability-adjusted life year; SSP, school-based sealant program.
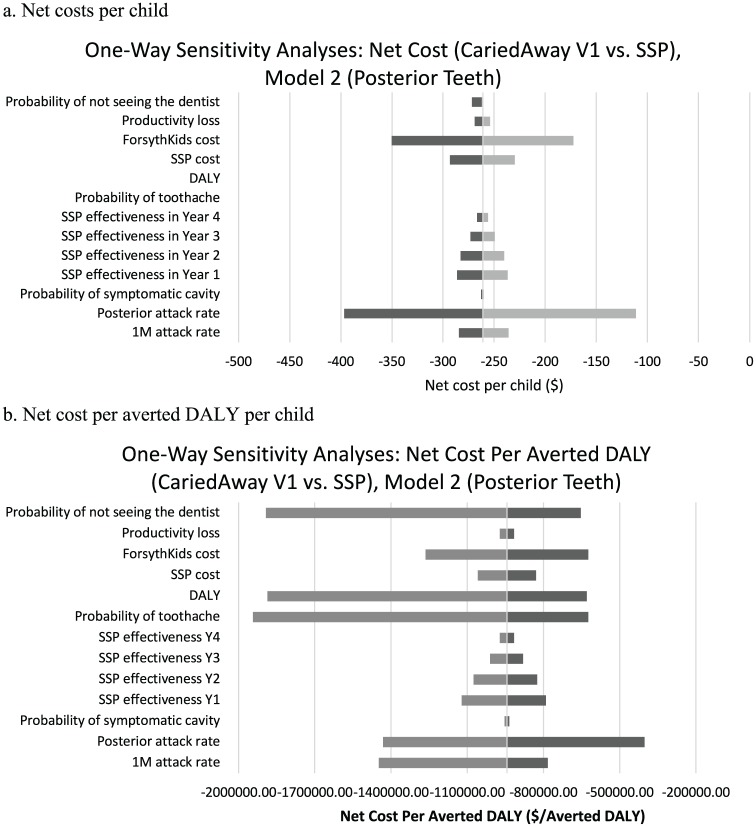
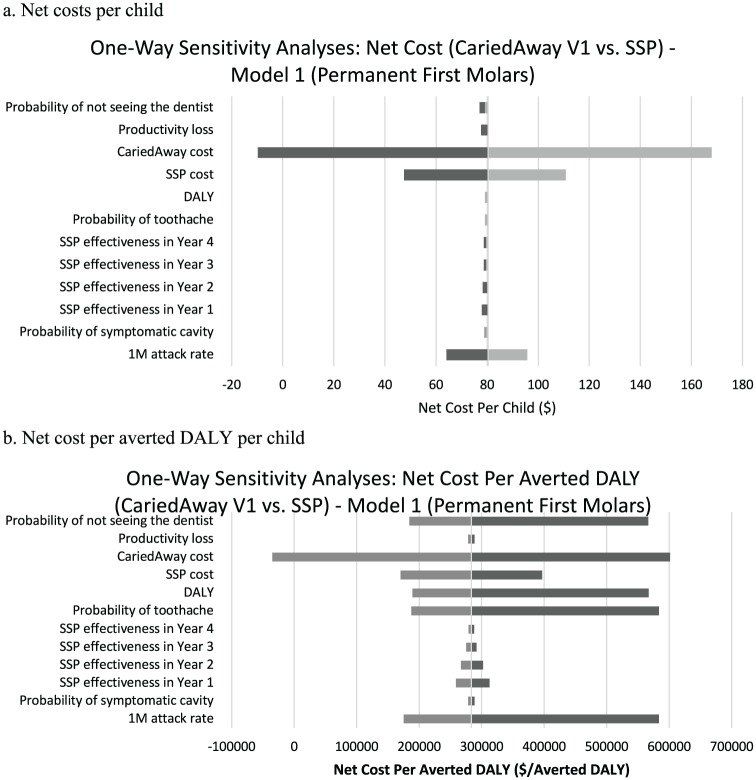
The main conclusions of the posterior teeth model and the 1M-only model are robust to 1-way sensitivity analyses. The 1-way sensitivity analyses examined the impact of allowing each parameter to vary between 50% and 150% of the base-case value. For the posterior teeth model, CariedAway unambiguously dominates SSPs, although the degree to which CariedAway is cost-saving relative to SSPs relies heavily on the cost of CariedAway and the caries attack rate for non-1M posterior teeth (Fig. 1). The lower the CariedAway cost and the higher the caries attack rate for posterior teeth, the more cost-saving CariedAway is relative to SSPs. For the 1M-only model, the most influential parameter is the CariedAway program cost (Fig. 2). When CariedAway program costs fall to low levels, CariedAway can be cost-saving relative to SSPs. However, SSPs unambiguously dominate CariedAway in all other sensitivity analyses for the 1M-only model.
Figure 1.
One-way sensitivity analyses for the posterior teeth model: net cost (a) per child and (b) per averted DALY per child. When posterior teeth are included in the model, the conclusion that CariedAway is cost-saving and cost-effective relative to SSPs is robust to 1-way sensitivity analyses. Data are shown for 1-way sensitivity analyses where individual parameters are varied between 50% and 150% of the base-case value in the model examining outcomes among all posterior teeth. 1M, first molar; DALY, disability-adjusted life year; SSP, school-based sealant program.
Figure 2.
One-way sensitivity analyses for 1M-only model: net cost (a) per child and (b) per averted DALY per child. When only 1Ms are included in the model, the conclusion that SSPs are cost-effective relative to CariedAway is largely robust. Only when the program cost of CariedAway is low does it become cost-saving and cost-effective relative to SSPs. Data are shown for 1-way sensitivity analyses where individual parameters are varied between 50% and 150% of the base-case value in the model examining outcomes among permanent 1Ms. 1M, first molar; DALY, disability-adjusted life year; SSP, school-based sealant program.
A 2-way sensitivity analysis was then used to examine the impact of allowing the CariedAway cost and the posterior caries attack rate to vary together in the posterior teeth model (Table 3). For high posterior caries attack rates (>0.04), CariedAway is generally cost-saving relative to SSPs for the range considered for the cost of CariedAway ($40 to $210 per child per visit). If the cost per child per visit in CariedAway was ≤$190, CariedAway would be considered cost-effective or cost-saving relative to SSPs for posterior caries attack rates ≥0.03.
Table 3.
Two-way Sensitivity Analysis.
| Annual Non-1M Posterior Cavity Attack Rate | ||||||
|---|---|---|---|---|---|---|
| CariedAway Cost, $ | 0.01 | 0.02 | 0.03 | 0.04 | 0.05 | 0.06 |
| 40 | CS | CS | CS | CS | CS | CS |
| 50 | CS | CS | CS | CS | CS | CS |
| 60 | CS | CS | CS | CS | CS | CS |
| 70 | CS | CS | CS | CS | CS | CS |
| 80 | CS | CS | CS | CS | CS | CS |
| 90 | CS | CS | CS | CS | CS | CS |
| 100 | CS | CS | CS | CS | CS | CS |
| 110 | 25,655.27 | CS | CS | CS | CS | CS |
| 120 | 68,223.91 | CS | CS | CS | CS | CS |
| 130 | 110,792.54 | CS | CS | CS | CS | CS |
| 140 | 153,361.18 | CS | CS | CS | CS | CS |
| 150 | 195,929.81 | 20,375.21 | CS | CS | CS | CS |
| 160 | 238,498.44 | 62,943.84 | CS | CS | CS | CS |
| 170 | 281,067.08 | 105,512.47 | CS | CS | CS | CS |
| 180 | 323,635.71 | 148,081.11 | CS | CS | CS | CS |
| 190 | 366,204.34 | 190,649.74 | 25,230.50 | CS | CS | CS |
| 200 | 408,772.98 | 233,218.37 | 67,799.14 | CS | CS | CS |
| 210 | 451,341.61 | 275,787.01 | 110,367.77 | CS | CS | CS |
Impact of simultaneously varying CariedAway cost per visit and posterior cavity attack rate on cost-effectiveness (net cost per averted disability-adjusted life year) relative to the school-based sealant program scenario. Numbers shown that are not shaded gray are scenarios where CariedAway is cost-effective relative to school-based sealant programs. The cost-effectiveness ratios shaded gray are scenarios where CariedAway is not cost-effective relative to school-based sealant programs.
1M, first molar; CS, cost saving (i.e., negative net cost).
Discussion
In contrast to SSPs delivering focused prevention for only 1Ms, comprehensive SCPPs can deliver prevention to both prevent and arrest decay in deciduous and adult teeth. Hence, comprehensive SCPPs avert dental care costs for active decay among program participants, which SSPs did not do (any active decay is generally referred to a private dentist for care in SSPs). However, prior current economic evaluations of SSPs were not structured to evaluate the impact of delivering comprehensive care across teeth versus focused prevention for specific teeth, due to the focus on clinical and economic outcomes pertaining only to 1Ms. As a result, prior economic evaluations of SSPs concluded that SSPs were the most cost-effective option without considering alternative models for school-based caries prevention. Hence, this study sought to rectify this gap in the literature by extending outcomes to posterior teeth and comparing comprehensive SCPPs with SSPs.
The Griffin et al. (2016) model was selected for this economic evaluation to evaluate the impact of different SCPPs on quality-of-life outcomes and economic outcomes. This contrasts other studies using tooth-related outcomes with ramifications for dental treatment but ambiguous ramifications for patient quality of life. However, quality-of-life measures such as DALYs are typically used to evaluate the health effects of nondental health-related programs. Tooth-related outcomes may have limited meaning for decision makers constrained by an overall budget for health programs. DALYs therefore were selected to facilitate comparisons between caries prevention programs and nondental health-related programs. Using DALYs improves the usefulness of economic evaluations of dental programs and interventions for individuals deciding between funding dental and medical measures.
Prior simulation models of SSPs do not model the treatment of active decay or teeth other than 1Ms. Including posterior teeth into the modeling of the health and cost impacts of SCPPs significantly alters conclusions of the economic evaluation. Considering only 1M outcomes yields the conclusion that SSPs are cost-effective relative to CariedAway but not relative to no SCPP. SSPs are not dominant relative to no SCPP, primarily because of the low 1M attack rate in this population: Griffin et al. (2016) used a 1M annual attack rate of 0.078, whereas CariedAway faced a 1M attack rate of 0.0366. Once all posterior teeth are included in the analysis, the posterior teeth model concludes that CariedAway is cost-effective and cost-saving relative to all other options. The reason is that CariedAway addresses not only caries prevention but also caries arrest for nonsymptomatic teeth, regardless of whether they are 1Ms or not. CariedAway had a limited impact on health and cost outcomes relative to SSPs in the 1M-only model because only active decay on 1Ms was addressed. However, once posterior teeth were included, the costs averted and health outcome improvement from addressing dental needs on more teeth led to a substantive impact on health and cost outcomes relative to SSPs.
The reversal of conclusions between the 1M-only model and the posterior teeth model highlight the importance of considering teeth beyond 1Ms, which have traditionally been the focus of economic evaluations of SSPs. This is important especially when alternate designs of SCPPs may treat not only 1Ms but all teeth.
Limitations
Selection bias is an inherent limitation in school-based prevention programs due to the nature of informed consent. The CariedAway data contain information only on students who opted into participating in the study and not the overall school population of potential participants. This bias affects the estimated caries attack rate and the program cost, but the direction of the bias is unknown. To date, this source of bias in economic evaluations has not been addressed in evaluations of SCPPs. Huang and Niederman (2019) provide recommendations for future work to address this bias.
Due to the inclusion of deciduous teeth into the calculation of attack rates for posterior teeth, the attack rates may be biased downward for the CariedAway study population. The reason is that prior caries experience in deciduous teeth may be underreported if some deciduous teeth fell out prior to examination. However, this is a general problem in dental research and cannot be addressed unless the oral health condition of children is consistently observed from birth to participation in an SCPP.
Tooth development is not considered explicitly in the model. This would require considerable additional complexity in the model, which would limit the comparability of this analysis with prior analyses. Future work should incorporate tooth development into economic evaluations of SCPPs. Such work would also allow for comparisons with alternative SSPs (e.g., onetime placement of sealants on deciduous posterior teeth).
Economic evaluations for developed countries more commonly use quality-adjusted life years (QALYs) instead of DALYs. DALYs were used in this analysis to allow for comparability with the work of Griffin et al. (2016) and because the available CariedAway data did not enable mapping to QALYs. Future work should use QALYs when possible.
Future work may also address the following model assumptions: 1) preventing or arresting caries in 1 tooth does not affect caries risk among surrounding teeth, and 2) there are no impacts of SCPPs past 5 y. These assumptions were chosen for model tractability. Models with longer time horizons should also consider assessing the relative failure rates of atraumatic and traditional restorations past 5 y.
Conclusion
This study demonstrates that economic evaluations of SCPPs can be significantly influenced by the choices of 1) what teeth to examine outcomes upon and 2) what comparator programs to include in the analysis. As SCPPs increase in prevalence and diversity, there is an increasing need to conduct robust economic evaluations to compare health and cost impacts across all teeth and to compare different designs for SCPPs against one another. Economic evaluations not addressing these needs may lead to suboptimal resource use that does not maximize the potential gains in oral health from school-based delivery of caries prevention. Economic evaluations addressing these needs will improve decision making on whether to invest in implementing SCPPs and what types of programs to implement.
Author Contributions
S.S. Huang, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript; R.R. Ruff, R. Niederman, contributed to conception, design, and data interpretation, critically revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work.
Supplemental Material
Supplemental material, DS_10.1177_2380084419837587 for An Economic Evaluation of a Comprehensive School-Based Caries Prevention Program by S.S. Huang, R.R. Ruff and R. Niederman in JDR Clinical & Translational Research
Acknowledgments
We gratefully acknowledge Susan Griffin, PhD, for generously providing information about her original model.
Footnotes
Research reported in this work was partially funded by the National Institute on Minority Health and Health Disparities of the National Institutes of Health (awards R01MD011526 and U24 006964). The views presented in this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
A supplemental appendix to this article is available online.
References
- Ahovuo-Saloranta A, Forss H, Walsh T, Nordblad A, Mäkelä M, Worthington HV. 2017. Pit and fissure sealants for preventing dental decay in permanent teeth. Cochrane Database Syst Rev. 7:CD001830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akinlotan M, Chen B, Fontanilla TM, Chen A, Fan VY. 2018. Economic evaluation of dental sealants: a systematic literature review. Community Dent Oral Epidemiol. 46(1):38–46. [DOI] [PubMed] [Google Scholar]
- Bukhari OM. 2016. Longitudinal clinical outcomes and cost-effectiveness evaluation of a comprehensive school-based dental prevention program—ForsythKids. Doctoral dissertation. Boston (MA): Harvard School of Dental Medicine. [Google Scholar]
- Community Preventive Services Task Force. 2016. Guide to community preventive services. Preventing dental caries: School-based dental sealant delivery programs. Washington (DC): US Department of Health and Human Services. [Google Scholar]
- Gooch BF, Griffin SO, Gray SK, Kohn WG, Rozier RG, Siegal M, Fontana M, Brunson D, Carter N, Curtis DK, et al. ; Centers for Disease Control and Prevention. 2009. Preventing dental caries through school-based sealant programs: updated recommendations and reviews of evidence. J Am Dent Assoc. 140(11):1356–1365. [DOI] [PubMed] [Google Scholar]
- Griffin S, Naavaal S, Scherrer C, Griffin PM, Harris K, Chattopadhyay S. 2016. School-based dental sealant programs prevent cavities and are cost-effective. Health Aff (Millwood). 35(12):2233–2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SO, Jones K, Crespin M. 2014. Calculating averted caries attributable to school-based sealant programs with a minimal data set. J Public Health Dent. 74(3):202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SO, Jones K, Naavaal S, O’Connell JM, Demopoulos C, Arlotta D. 2018. Estimating the cost of school sealant programs with minimal data. J Public Health Dent. 78(1):17–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin SO, Naavaal S, Scherrer C, Patel M, Chattopadhyay S. 2017. Evaluation of school-based dental sealant programs: an updated community guide systematic economic review. Am J Prev Med. 52(3):407–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang SS, Niederman R. 2019. Economic evaluations of school sealant programs and the consent conundrum. J Dent Res. 98(2):145–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mariño R, Khan A, Morgan M. 2013. Systematic review of publications on economic evaluations of caries prevention programs. Caries Res. 47(4):265–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mickenautsch S, Yengopal V, Banerjee A. 2010. Atraumatic restorative treatment versus amalgam restoration longevity: a systematic review. Clin Oral Investig. 14(3):233–240. [DOI] [PubMed] [Google Scholar]
- Murray CJ. 1994. Quantifying the burden of disease: the technical basis for disability-adjusted life years. Bull World Health Organ. 72(3):429–445. [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, Naghavi M, Salomon JA, Shibuya K, Vos T. 2012. GBD 2010: design, definitions, and metrics. Lancet. 380(9859):2063–2066. [DOI] [PubMed] [Google Scholar]
- National Institute of Dental Research. 1991. Oral health surveys of the National Institute of Dental Research: diagnostic criteria and procedures. Bethesda (MD): National Institute of Dental Research. [Google Scholar]
- Niederman R, Gould E, Soncini J, Tavares M, Osborn V, Goodson JM. 2008. A model for extending the reach of the traditional dental practice: the ForsythKids program. J Am Dent Assoc. 139(8):1040–1050. [DOI] [PubMed] [Google Scholar]
- Niederman R, Huang SS, Trescher AL, Listl S. 2017. Getting the incentives right: improving oral health equity with universal school-based caries prevention. Am J Public Health. 107 Suppl 1:S50–S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rushby JF, Hanson K. 2001. Calculating and presenting disability adjusted life years (DALYs) in cost-effectiveness analysis. Health Policy Plan. 16(3):326–331. [DOI] [PubMed] [Google Scholar]
- Whitehead SJ, Ali S. 2010. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull. 96:5–21. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, DS_10.1177_2380084419837587 for An Economic Evaluation of a Comprehensive School-Based Caries Prevention Program by S.S. Huang, R.R. Ruff and R. Niederman in JDR Clinical & Translational Research