Abstract
Background:
It is unclear what the optimal graft choice is for performing anterior cruciate ligament (ACL) reconstruction in a skeletally immature patient.
Purpose:
To evaluate outcomes and complications of skeletally immature patients undergoing transphyseal ACL reconstruction with a hamstring tendon autograft versus a quadriceps tendon autograft.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
Between 2012 and 2016, 90 skeletally immature patients from a single institution underwent primary transphyseal ACL reconstruction with either a quadriceps tendon autograft or a hamstring tendon autograft based on surgeon preference (n = 3). Patient demographic, injury, radiographic, and surgical variables were documented. Outcome measures included the Lysholm score, Single Assessment Numeric Evaluation (SANE), Tegner activity score, pain, satisfaction, and complications such as graft tears and physeal abnormalities.
Results:
A total of 83 patients (56 hamstring tendon, 27 quadriceps tendon) were available for a minimum follow-up of 2 years or sustained graft failure. The mean age of the patients was 14.8 ± 1.4 years at the time of ACL reconstruction. No differences in chronological age, bone age, sex, patient size, or mechanism of injury were noted between groups. There were no differences in surgical variables, except that the quadriceps tendon grafts were larger than the hamstring tendon grafts (9.6 ± 0.6 mm vs 7.8 ± 0.7 mm, respectively; P < .001). Patient outcomes at a mean follow-up of 2.8 ± 0.9 years revealed no differences based on graft type, with mean Lysholm, SANE, pain, satisfaction, and Tegner scores of 96, 93, 0.6, 9.6, and 6.6, respectively, for the quadriceps tendon group and 94, 89, 0.9, 9.2, and 7.1, respectively, for the hamstring tendon group. While there were no physeal complications in either group, patients undergoing ACL reconstruction with a hamstring tendon autograft were more likely to tear their graft (21% vs 4%, respectively; P = .037).
Conclusion:
Skeletally immature patients undergoing ACL reconstruction can be successfully managed with either a quadriceps tendon autograft or a hamstring tendon autograft with good short-term outcomes, high rates of return to sport, and low rates of physeal abnormalities. The primary differences between grafts were that the quadriceps tendon grafts were larger and were associated with a lower retear rate. ACL reconstruction performed with a quadriceps tendon autograft may reduce early graft failure in skeletally immature patients.
Keywords: transphyseal ACL reconstruction, quadriceps tendon, skeletally immature
Anterior cruciate ligament (ACL) injuries are being diagnosed and treated more frequently in the skeletally immature population.30 Historically, many of these patients were managed nonoperatively with activity modification, physical therapy, and bracing until they reached skeletal maturity, at which time an adult reconstructive technique was performed. Over the past 2 decades, there has been increased recognition that this delay in treatment may result in further meniscal and chondral damage.1,11,17,21,23,24 As a result, there has been an increasing trend toward early reconstruction in this patient population.3,7
Several graft options have been described and are currently utilized in the management of skeletally immature patients with complete ACL tears, including the hamstring tendon, the quadriceps tendon, the iliotibial band, and various soft tissue allografts.2,14–16 While each graft has certain advantages and disadvantages, there are no clear indications in the literature as to which approach is optimal for skeletally immature patients. The purpose of the current study was to compare clinical outcomes and complications of skeletally immature patients undergoing transphyseal ACL reconstruction with either a hamstring tendon autograft or a quadriceps tendon autograft. We hypothesized that both surgical techniques would provide good functional outcomes with high rates of return to sport and low rates of graft failure and physeal injuries.
Methods
After institutional review board approval was obtained, a retrospective study was performed on skeletally immature patients undergoing primary ACL reconstruction using a transphyseal technique with a hamstring tendon autograft or a quadriceps tendon autograft. Inclusion criteria were patients undergoing surgery between December 2012 and October 2016 with preoperative imaging confirming open growth plates and who had a minimum follow-up of 2 years or documented graft failure before the 2-year mark. Patients who underwent multiligamentous knee reconstruction as well as those with a congenital absence of the cruciate ligaments were excluded. Preoperative demographic variables were recorded, including patient age, sex, weight, body mass index, sport of injury, and mechanism of injury. The mechanism of injury was classified as contact, noncontact, or device-associated. Preoperative images including all radiographs and magnetic resonance imaging (MRI) scans were reviewed to confirm the open growth plate status. Additionally, bone age was calculated using either a left-hand radiograph with the Greulich and Pyle10 atlas or a preoperative MRI scan with the knee MRI bone age atlas.25 Concomitant collateral ligament injuries and posterior cruciate ligament injuries were documented based on preoperative MRI and examinations. Intraoperative data points included the presence of a meniscal or chondral injury and any subsequent treatment, graft choice (hamstring tendon autograft vs quadriceps tendon autograft), graft diameter (mm), and whether the autograft was supplemented with a soft tissue allograft.
Surgical Technique
Patient and Graft Selection
Three pediatric trained orthopaedic surgeons from a single institution (A.T.P., H.G.C., E.W.E.) performed all of the surgical procedures. The typical indication for transphyseal ACL reconstruction was a male patient with open growth plates and a bone age between 13 and 15 years or a female patient with open growth plates and a bone age between 11 and 13 years. In younger patients with significant skeletal growth remaining, the study institution utilizes either an all-epiphyseal technique or iliotibial band extra-articular/intra-articular reconstruction. These younger patients were excluded from the analysis to provide more uniform study groups with a standardized surgical technique. Initially in the study period, all 3 surgeons exclusively used hamstring tendon autografts for transphyseal ACL reconstruction. In April 2014, one surgeon (A.T.P.) converted to quadriceps tendon autografts for all transphyseal ACL reconstructions. The rationale for this surgeon’s change was the belief that the quadriceps tendon would yield a consistently larger graft (compared with the hamstring tendon) in the pediatric population and would avoid harvesting the hamstring tendons that are known dynamic stabilizers of the ACL.8,13,22
Surgical Procedure
A similar technique was utilized for all patients. The patient was placed supine on the operating room table. After the ACL tear was confirmed with an examination under anesthesia and/or arthroscopic evaluation, the hamstring tendon or quadriceps tendon was harvested. In cases in which the hamstring tendon was used, both the gracilis and the semitendinosis tendons were harvested and prepared as a quadrupled graft. If the quadrupled graft measured less than 7 mm in diameter, it was frequently augmented with an allograft.26 All of the allografts came from a single vendor who utilizes the Allowash terminal sterilization process (LifeNet Health), including detergents, antibiotics, alcohol, peroxide, and multiple water rinses, followed by low-dose radiation ranging from 0.9 to 1.3 Mrad (AlloSource). In cases in which the quadriceps tendon was used, a partial- or full-thickness segment of the quadriceps tendon was harvested to provide a graft 8 to 10 mm in diameter and 7 to 8 cm in length. No bone plug was taken from the patella at the time of quadriceps tendon harvest. All grafts were sized using a slotted sizing block (Smith & Nephew) to the nearest 0.5 mm. At the time of arthroscopic surgery, any cartilage or meniscal abnormality was documented and treated accordingly.
The femoral and tibial tunnels were both drilled slightly more vertical than for a typical ACL reconstruction procedure in a skeletally mature patient (femoral guide setting, 115°; tibial guide setting, 60°), but every attempt was made to keep the tunnel apertures within the ACL footprint. The femoral tunnel was drilled using an outside-in approach with a reverse cutting guide (Arthrex).26 Regardless of the graft choice, the graft was secured on the femur first with a cortical suspensory device (TightRope [Arthrex] or Endobutton CL Ultra [Smith & Nephew]). For the hamstring tendon grafts, the tendons were looped around the suspensory fixation device, and the free ends were whip-stitched with high-strength No. 2 nonabsorbable suture. For the quadriceps tendon grafts, both ends of the graft were whip-stitched with high-strength No. 2 nonabsorbable suture. The suture from 1 end of the graft was then sutured around the Endobutton device, creating a 10-mm closed loop (Figure 1).
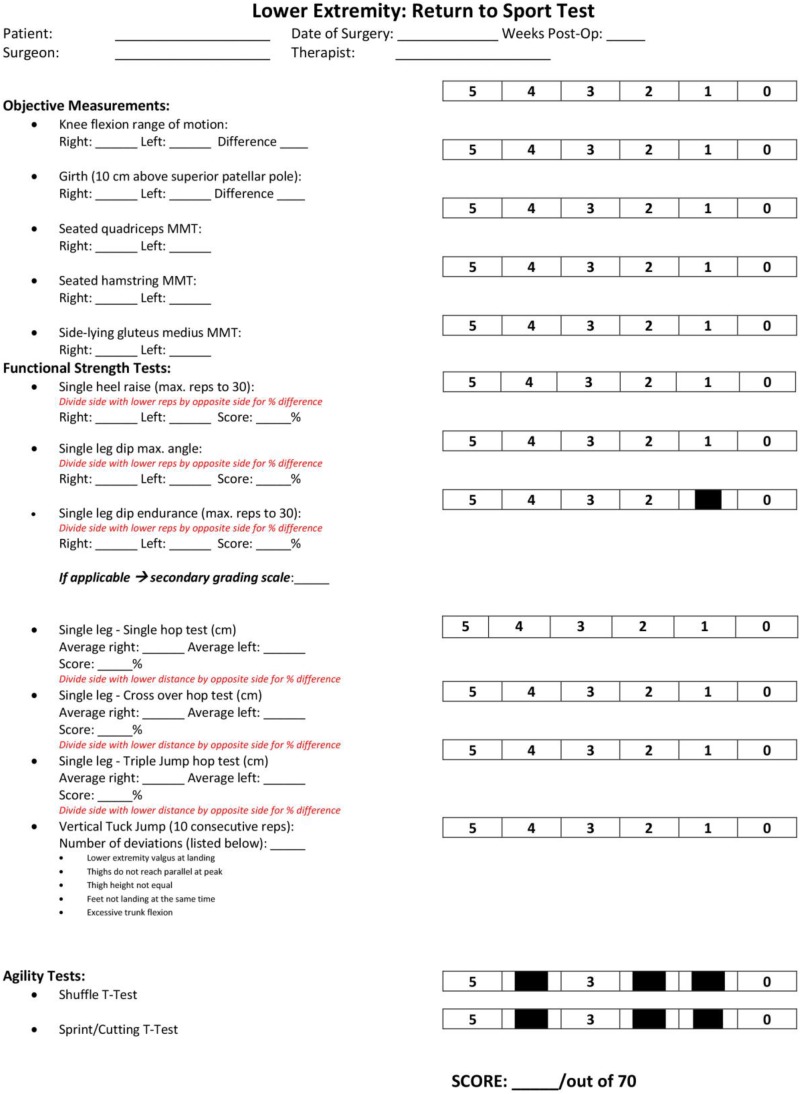
Figure 1.
(A) Quadrupled hamstring tendon autograft with a suspensory fixation device. (B) Quadriceps tendon autograft fixated to a suspensory fixation device using high-strength No. 2 nonabsorbable suture. Images courtesy of SD PedsOrtho.
Fixation was then achieved on the tibia with either a biocomposite interference screw, a screw and post (Synthes or Arthrex) if there was not adequate room within the tibial tunnel to accommodate a screw, or a combination of the 2 if interference screw fixation was felt to be inadequate (Figure 2). The decision for tibial fixation was made based on intraoperative fluoroscopy or by placing the arthroscope up the tibial tunnel and measuring the tunnel length from the tibial cortex to the physis. If this length was ≥23 mm, a biocomposite screw was used. If this distance was less than 23 mm or if the screw had limited purchase on the graft, a screw and post was used instead or added to the construct.
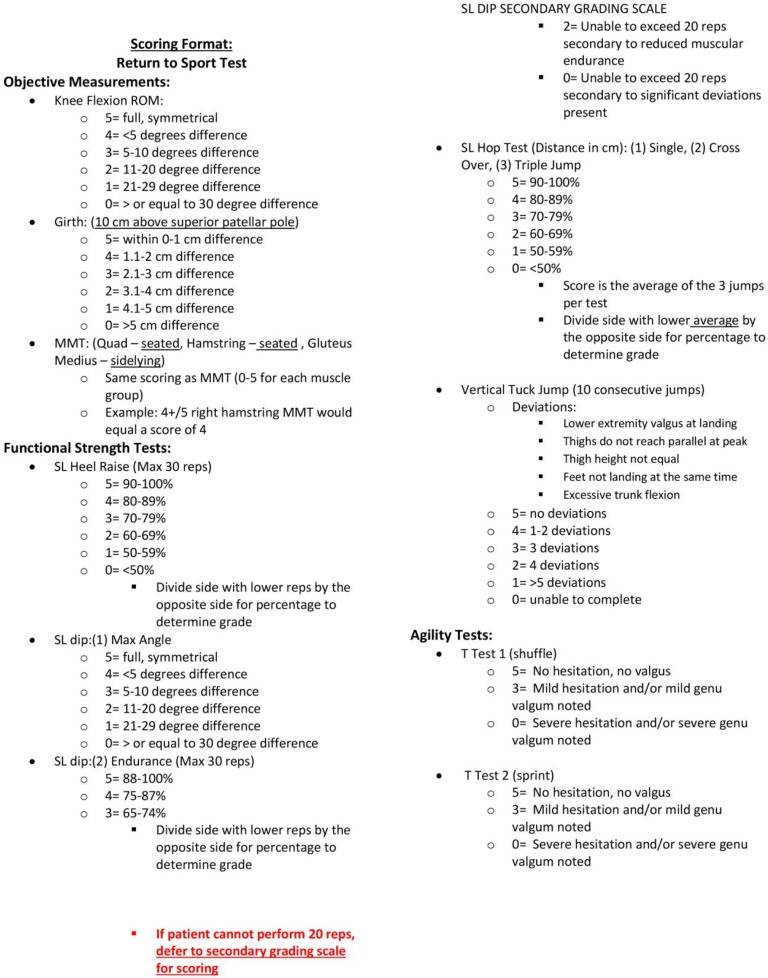
Figure 2.
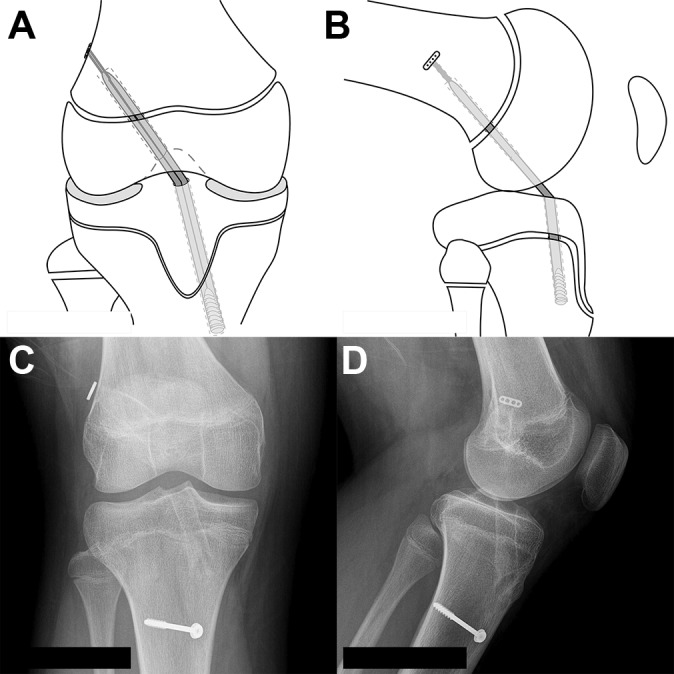
(A, B) Schematic drawing in the coronal and sagittal planes demonstrating the transphyseal technique utilized by our institution. (C, D) Anteroposterior and lateral views demonstrating the transphyseal technique with slightly vertical tunnels and a screw and post for tibial fixation. Images courtesy of SD PedsOrtho.
Postoperative Protocol
Postoperatively, all patients were allowed immediate motion of the knee and were kept toe-touch weightbearing for 1 week. Formal therapy was initiated at that time. A running progression was started 3 months after surgery, and patients were allowed to return to sport 6 to 12 months after surgery if they passed a return-to-sport test (see the Appendix).
Patient outcomes were obtained at a minimum 2-year follow-up unless the patient underwent revision ACL reconstruction, in which case outcome scores were not obtained. Outcome measures included patient satisfaction (0-10), the Single Assessment Numeric Evaluation (SANE; 0-100), pain (0-10), the Lysholm score, and the Tegner activity score. Complications were also documented, including graft failure, time to graft failure, need for subsequent surgical intervention, presence of an angular deformity greater than 5° compared with the contralateral extremity, or leg length discrepancy of greater than 10 mm compared with the contralateral extremity. These measurements were typically performed with a long-leg alignment film using a digital measuring device from our MERGE PACS system (Watson Health Imaging). If a family or surgeon deferred the long-leg alignment film for radiation exposure concerns, these measurements were made clinically with the patient in the prone position. Subsequent contralateral ACL tears were also recorded. Graft failure and contralateral ACL tears were confirmed when both the patient’s physical examination findings (positive Lachman and pivot-shift test results) and the MRI findings were consistent with a complete rupture of the native ACL or graft.
Statistical Analysis
Statistical analysis was performed to evaluate any differences in outcome scores or complications between the quadriceps tendon grafts and hamstring tendon grafts. Continuous dependent variables were checked for normality and homogeneity of variances. If neither assumption was violated, analysis of variance was utilized to compare means between groups. If one or both assumptions were violated, the nonparametric Mann-Whitney U test was utilized. The chi-square or Fisher exact test was used to compare categorical variables. All statistical analyses were performed using SPSS v24 (IBM), and alpha was set at P < .05 to declare significance.
Results
Between December 2012 and October 2016, 90 ACL reconstructions (62 hamstring tendon and 28 quadriceps tendon) were performed at our institution in the skeletally immature population that met the inclusion criteria. Of these patients, 83 (92%) had a minimum follow-up of 2 years or had documented graft failure before this point. The mean age of the cohort was 14.8 ± 1.4 years, and the mean bone age was 14.6 ± 1.1 years. The majority of the patients were male (69%), and most of the injuries were sustained while playing soccer or football (71%), with noncontact being the most common mechanism of injury. There were no significant differences in preoperative, radiographic, or surgical variables between the quadriceps tendon or hamstring tendon groups (P > .05), except that the quadriceps tendon grafts were larger than the hamstring tendon grafts (9.6 mm vs 7.8 mm, respectively; P < .001) (Table 1).
Table 1.
Demographic, Injury, and Surgical Data for All 90 Patients Undergoing Transphyseal ACL Reconstructiona
| Hamstring Tendon (n = 62) | Quadriceps Tendon (n = 28) | P Value | |
|---|---|---|---|
| Patient age, y | 14.8 ± 1.4 | 14.8 ± 1.3 | .804 |
| Bone age, y | 14.6 ± 1.1 | 14.4 ± 0.9 | .274 |
| Male sex, n (%) | 43 (69) | 19 (68) | .887 |
| Body mass index, kg/m2 | 23.9 ± 5.7 | 21.5 ± 3.2 | .065 |
| Weight, kg | 67.9 ± 18.0 | 61.3 ± 11.3 | .163 |
| Mechanism of injury, n (%) | .192 | ||
| Contact | 14 (22) | 9 (32) | |
| Noncontact | 32 (52) | 17 (61) | |
| Mechanized | 11 (18) | 2 (7) | |
| Not recorded | 5 (8) | 0 (0) | |
| Meniscal procedure, n (%) | .526 | ||
| Debridement | 11 (28) | 6 (21) | |
| Repair | 18 (28) | 10 (36) | |
| None | 33 (44) | 12 (43) | |
| Chondroplasty, n (%) | 1 (2) | 0 (0) | .499 |
| Allograft augmentation, n (%) | 5 (8) | 0 (0) | .122 |
| Graft size, mm | 7.8 ± 0.7 | 9.6 ± 0.6 | <.001 |
aValues are reported as mean ± SD unless otherwise specified. Bolded values indicate significance (P < .05). ACL, anterior cruciate ligament.
At a mean follow-up of 2.8 ± 0.9 years (2.9 ± 0.9 years for hamstring tendon group vs 2.4 ± 0.7 years for quadriceps tendon group), the mean patient satisfaction, SANE, and Lysholm scores for the entire cohort were 9.3 ± 1.1, 91 ± 11, and 95 ± 7, respectively. The mean postoperative Tegner activity score was 6.9 ± 1.9. There were no differences in outcomes based on graft choice. The rate of ACL graft failure did differ based on graft choice, with the quadriceps tendon grafts failing less frequently than the hamstring tendon grafts (4% vs 21%, respectively; P = .037). The hamstring tendon grafts failed at a mean time of 1.5 years (range, 0.5-3.2 years), whereas the 1 quadriceps tendon graft failure occurred at 2.5 years. Of the 5 hamstring tendon grafts augmented with an allograft, 1 failed at 6 months and had to be revised. With the numbers available in the cohort, graft diameter size was not significantly associated with ACL retears (P = .12). Contralateral ACL tears were similar between the groups and occurred in 12% of the entire patient cohort. No patient in either group had a documented leg length discrepancy greater than 10 mm or an angular deformity greater than 5° at final follow-up (Table 2). There was no difference between the groups with respect to the need for a second procedure (P = .201). Six patients in the hamstring tendon group underwent an additional 9 procedures that were not revision ACL reconstructions, including 4 meniscal debridements, 1 meniscal repair, and 4 lyses of adhesions. Three patients in the quadriceps tendon group underwent 3 additional procedures that were not revision ACL reconstruction, including 1 removal of a tibial screw, 1 lysis of adhesions, and 1 synovectomy.
Table 2.
Outcomes and Complications for 83 Patients Undergoing Transphyseal ACL Reconstruction Who Had a Minimum Follow-up of 2 Years or Had Documented Graft Failure Before 2 Yearsa
| Hamstring Tendon (n = 56) | Quadriceps Tendon (n = 27) | P Value | |
|---|---|---|---|
| Lysholm score | 94 ± 6 | 96 ± 8 | .095 |
| Satisfaction (0-10) | 9.2 ± 1.2 | 9.6 ± 0.8 | .096 |
| SANE score (0-100) | 89 ± 11 | 93 ± 9 | .227 |
| Pain score (0-10) | 0.9 ± 1.5 | 0.6 ± 1.4 | .163 |
| Tegner activity score | 7.1 ± 2.0 | 6.6 ± 1.6 | .229 |
| Graft failure, n (%) | 12 (21) | 1 (4) | .037 |
| Time to graft failure, y | 1.5 ± 0.9 | 2.5 ± 0.0 | .900 |
| Growth abnormality, n (%) | 0 (0) | 0 (0) | N/A |
| Contralateral ACL tear, n (%) | 5 (9) | 5 (19) | .270 |
aValues are reported as mean ± SD unless otherwise specified. Bolded values indicate significance (P < .05). ACL, anterior cruciate ligament; N/A, not applicable; SANE, Single Assessment Numeric Evaluation.
Discussion
Over 3 decades ago, Lipscomb and Anderson18 described a transphyseal technique using the hamstring tendons to reconstruct the knees of skeletally immature patients with ACL injuries. Their report on 24 patients showed good functional outcomes with only 2 cases of recurrent instability and 2 cases of a clinically significant leg length discrepancy. Since this initial description, multiple other modifications of this technique have been described and reported with good outcomes.4,15,29 To date, the most common complication of ACL reconstruction in skeletally immature patients continues to be graft failure. This rate varies in the literature but typically ranges from 10% to 25% in this younger population.20,27,28,31 In the present study, we observed a similar failure rate of our hamstring tendon grafts of 21%.
Currently, it is not known whether this relatively high failure rate is intrinsic to this younger athletic patient population or innate to hamstring tendon grafts. Some authors have suggested that hamstring tendon grafts may be at an increased risk of failure because of their inconsistent and smaller size in the pediatric population.6,26 In the current study, the hamstring tendon grafts averaged 7.8 mm in size, with 35% of grafts having a diameter ≤7 mm, and 8% of hamstring tendon grafts had to be augmented with an allograft. Another explanation for the higher failure rate may be that the hamstring tendons are important dynamic stabilizers of the ACL, and harvesting these tendons may predispose patients to graft failure.8,13,22 For these reasons, there has recently been increased interest in alternative graft sources in this skeletally immature population.
The utilization of the quadriceps tendon as a graft source for ACL reconstruction is not a novel concept, with case reports dating back to the 1990s in the skeletally immature population.19 Over the past 2 decades, however, there have been only a few studies reporting patient outcomes with this graft type. In 2006, Gebhard et al9 performed a multicenter study, reporting on 40 skeletally immature cases, of which 12 used a quadriceps tendon autograft. While their reported outcomes were good, they pooled their data using multiple different techniques, making larger generalizations about the performance of the quadriceps tendon graft impossible. A second study in 2014 by Kohl et al16 reported on 15 patients with a mean age of 12.8 years who had undergone a transphyseal technique with a soft tissue quadriceps tendon autograft. At a mean follow-up of 4 years, the study's authors documented a mean Lysholm score of 94 with no traumatic reruptures and 1 case of valgus deformity.
In the current study, good outcomes were achieved in the quadriceps tendon group with mean SANE, Lysholm, and satisfaction scores of 93, 96, and 9.6, respectively. The quadriceps tendon grafts had a consistently larger diameter than the hamstring tendon grafts (9.6 vs 7.8 mm, respectively; P < .001), which equates to a cross-sectional area that was nearly 60% larger than the hamstring tendons. While larger femoral and tibial tunnels had to be drilled to accommodate this larger graft, there was no increased incidence of physeal abnormalities in this specific patient population (boys with a bone age between 13 and 15 years and girls with a bone age between 11 and 13 years). Perhaps most importantly, the quadriceps tendon grafts had a lower failure rate than the hamstring tendon grafts (4% vs 21%, respectively; P = .037). This is a particularly important finding because graft failure is the most common complication in this patient population. Longer term follow-up will be necessary to assess the durability of these results as well as the risk of future posttraumatic arthritis.
As with all grafts, there are potential drawbacks of a quadriceps tendon graft that must be considered by the surgeon, patient, and family. Strength recovery of the extensor mechanism has been shown to be adversely affected by harvesting a quadriceps tendon graft, but the functional implications of this weakness are unclear.8,13 However, recent data would suggest that these residual deficits largely normalize with time.5 Furthermore, proponents of quadriceps tendon grafts often point to the better hamstring-to-quadriceps ratios that are observed after harvesting a quadriceps tendon graft compared with a hamstring tendon graft.22 While formal strength testing was not performed as part of the current study, we have anecdotally noted an initial extensor strength deficit in patients undergoing quadriceps tendon harvest that appears to largely recover 6 to 12 months after surgery. A second potential concern with the quadriceps tendon as a graft source is that it may predispose patients to arthrofibrosis. A recent study by Huleatt et al12 demonstrated that patients undergoing ACL reconstruction with a quadriceps tendon had a relative risk increase of 2.7 for requiring manipulation under anesthesia compared with other graft options. In the current study, 1 patient with a quadriceps tendon graft (4%) developed arthrofibrosis, requiring manipulation under anesthesia and lysis of adhesions, compared with no patients in the hamstring tendon group. Potential causes of this stiffness include postoperative quadriceps inhibition from tendon harvest, the quadriceps tendon being a stiffer graft, or the larger quadriceps tendon graft predisposing patients to notch impingement and loss of extension.12
There are several limitations to the current study, including its nonrandomized and retrospective design. Additionally, the follow-up was relatively short. This fact may cause the study to underrepresent future failure rates, and it does not identify the rates or progression of future posttraumatic arthritis. Another limitation was that objective testing of ACL graft integrity as well as postoperative quadriceps and hamstring strength testing were not performed, which potentially would have identified more subtle differences in the 2 techniques. Finally, the sizes of the patient groups were relatively small, using 3 different surgeons with slightly different techniques, limiting our ability to identify all risk factors for failure and poor outcomes. A future prospective multicenter study with larger numbers and longer term follow-up will be necessary to validate these early findings and can account for selection, surgeon, and temporal bias.
Conclusion
The majority of skeletally immature patients with complete ACL tears can be successfully managed with either a quadriceps tendon autograft or a hamstring tendon autograft in ACL reconstruction with good functional outcomes, relatively high rates of return to sport, and low rates of physeal complications. However, the quadriceps tendon autograft appears to have a lower graft failure rate in this high-risk patient population. A future multicenter prospective or randomized controlled study will be necessary to better assess these differences and to see if one graft is clearly preferable for this unique patient population.
Acknowledgment
The authors thank James Bomar from Rady Children’s Hospital for preparing the figures for this article.
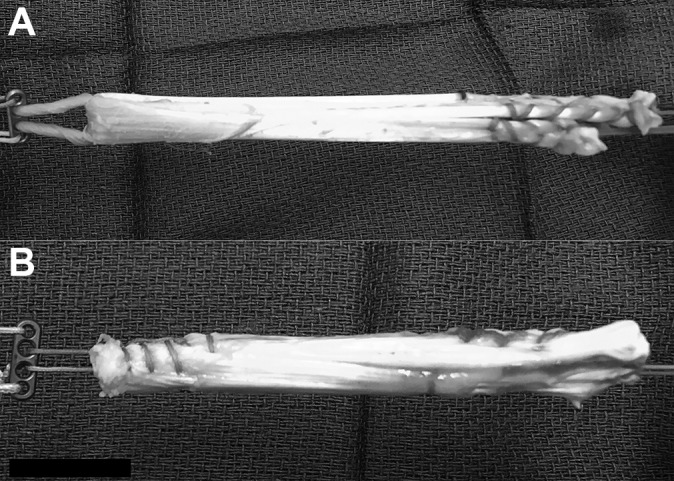
APPENDIX
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: A.T.P. has received nonconsulting fees from Smith & Nephew and educational support from Sportstek Medical. H.G.C. has received consulting fees from OrthoPediatrics and Roche Molecular Systems. E.W.E. has received nonconsulting fees from Arthrex and consulting fees from OrthoPediatrics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the institutional review board at the University of California, San Diego (project 161895X).
References
- 1. Anderson AF, Anderson CN. Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med. 2015;43(2):275–281. [DOI] [PubMed] [Google Scholar]
- 2. Andrews M, Noyes FR, Barber-Westin SD. Anterior cruciate ligament allograft reconstruction in the skeletally immature athlete. Am J Sports Med. 1994;22(1):48–54. [DOI] [PubMed] [Google Scholar]
- 3. Buller LT, Best MJ, Baraga MG, Kaplan LD. Trends in anterior cruciate ligament reconstruction in the United States. Orthop J Sports Med. 2015;3(1):2325967114563664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Calvo R, Figueroa D, Gili F, et al. Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-year follow-up study. Am J Sports Med. 2015;43(2):289–294. [DOI] [PubMed] [Google Scholar]
- 5. Cavaignac E, Coulin B, Tscholl P, Nik Mohd Fatmy N, Duthon V, Menetrey J. Is quadriceps tendon autograft a better choice than hamstring autograft for anterior cruciate ligament reconstruction? A comparative study with a mean follow-up of 3.6 years. Am J Sports Med. 2017;45(6):1326–1332. [DOI] [PubMed] [Google Scholar]
- 6. Darnley JE, Leger-St-Jean B, Pedroza AD, Flanigan DC, Kaeding CC, Magnussen RA. Anterior cruciate ligament reconstruction using a combination of autograft and allograft tendon: a MOON cohort study. Orthop J Sports Med. 2016;4(7):2325967116662249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 8. Fischer F, Fink C, Herbst E, et al. Higher hamstring-to-quadriceps isokinetic strength ratio during the first post-operative months in patients with quadriceps tendon compared to hamstring tendon graft following ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2018;26(2):418–425. [DOI] [PubMed] [Google Scholar]
- 9. Gebhard F, Ellermann A, Hoffmann F, Jaeger JH, Friederich NF. Multicenter study of operative treatment of intraligamentous tears of the anterior cruciate ligament in children and adolescents: comparison of four different techniques. Knee Surg Sports Traumatol Arthrosc. 2006;14(9):797–803. [DOI] [PubMed] [Google Scholar]
- 10. Greulich WW, Pyle SI. Radiographic Atlas of Skeletal Development of the Hand and Wrist. 2nd ed Stanford, California: Stanford University Press; 1959. [Google Scholar]
- 11. Henry J, Chotel F, Chouteau J, Fessy MH, Berard J, Moyen B. Rupture of the anterior cruciate ligament in children: early reconstruction with open physes or delayed reconstruction to skeletal maturity? Knee Surg Sports Traumatol Arthrosc. 2009;17(7):748–755. [DOI] [PubMed] [Google Scholar]
- 12. Huleatt J, Gottschalk M, Fraser K, et al. Risk factors for manipulation under anesthesia and/or lysis of adhesions after anterior cruciate ligament reconstruction. Orthop J Sports Med. 2018;6(9):2325967118794490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Iriuchishima T, Ryu K, Okano T, Suruga M, Aizawa S, Fu FH. The evaluation of muscle recovery after anatomical single-bundle ACL reconstruction using a quadriceps autograft. Knee Surg Sports Traumatol Arthrosc. 2017;25(5):1449–1453. [DOI] [PubMed] [Google Scholar]
- 14. Kocher MS, Heyworth BE, Fabricant PD, Tepolt FA, Micheli LJ. Outcomes of physeal-sparing ACL reconstruction with iliotibial band autograft in skeletally immature prepubescent children. J Bone Joint Surg Am. 2018;100(13):1087–1094. [DOI] [PubMed] [Google Scholar]
- 15. Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. J Bone Joint Surg Am. 2007;89(12):2632–2639. [DOI] [PubMed] [Google Scholar]
- 16. Kohl S, Stutz C, Decker S, et al. Mid-term results of transphyseal anterior cruciate ligament reconstruction in children and adolescents. Knee. 2014;21(1):80–85. [DOI] [PubMed] [Google Scholar]
- 17. Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med. 2011;39(12):2582–2587. [DOI] [PubMed] [Google Scholar]
- 18. Lipscomb AB, Anderson AF. Tears of the anterior cruciate ligament in adolescents. J Bone Joint Surg Am. 1986;68(1):19–28. [PubMed] [Google Scholar]
- 19. Lo IK, Kirkley A, Fowler PJ, Miniaci A. The outcome of operatively treated anterior cruciate ligament disruptions in the skeletally immature child. Arthroscopy. 1997;13(5):627–634. [DOI] [PubMed] [Google Scholar]
- 20. Longo UG, Ciuffreda M, Casciaro C, et al. Anterior cruciate ligament reconstruction in skeletally immature patients: a systematic review. Bone Joint J. 2017;99-B(8):1053–1060. [DOI] [PubMed] [Google Scholar]
- 21. Mansson O, Sernert N, Rostgard-Christensen L, Kartus J. Long-term clinical and radiographic results after delayed anterior cruciate ligament reconstruction in adolescents. Am J Sports Med. 2015;43(1):138–145. [DOI] [PubMed] [Google Scholar]
- 22. Martin-Alguacil JL, Arroyo-Morales M, Martin-Gomez JL, et al. Strength recovery after anterior cruciate ligament reconstruction with quadriceps tendon versus hamstring tendon autografts in soccer players: a randomized controlled trial. Knee. 2018;25(4):704–714. [DOI] [PubMed] [Google Scholar]
- 23. Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18(9):955–959. [DOI] [PubMed] [Google Scholar]
- 24. Newman JT, Carry PM, Terhune EB, et al. Factors predictive of concomitant injuries among children and adolescents undergoing anterior cruciate ligament surgery. Am J Sports Med. 2015;43(2):282–288. [DOI] [PubMed] [Google Scholar]
- 25. Pennock AT, Bomar JD, Manning JD. The creation and validation of a knee bone age atlas utilizing MRI. J Bone Joint Surg Am. 2018;100(4):e20. [DOI] [PubMed] [Google Scholar]
- 26. Pennock AT, Ho B, Parvanta K, et al. Does allograft augmentation of small-diameter hamstring autograft ACL grafts reduce the incidence of graft retear? Am J Sports Med. 2017;45(2):334–338. [DOI] [PubMed] [Google Scholar]
- 27. Peterson DC, Ayeni OR. Pediatric anterior cruciate ligament reconstruction outcomes. Curr Rev Musculoskelet Med. 2016;9(4):339–347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Pierce TP, Issa K, Festa A, Scillia AJ, McInerney VK. Pediatric anterior cruciate ligament reconstruction: a systematic review of transphyseal versus physeal-sparing techniques. Am J Sports Med. 2017;45(2):488–494. [DOI] [PubMed] [Google Scholar]
- 29. Schmale GA, Kweon C, Larson RV, Bompadre V. High satisfaction yet decreased activity 4 years after transphyseal ACL reconstruction. Clin Orthop Relat Res. 2014;472(7):2168–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Werner BC, Yang S, Looney AM, Gwathmey FW., Jr Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. J Pediatr Orthop. 2016;36(5):447–452. [DOI] [PubMed] [Google Scholar]
- 31. Wong SE, Feeley BT, Pandya NK. Complications after pediatric ACL reconstruction: a meta-analysis. J Pediatr Orthop. 2019;39(8):e566–e571. [DOI] [PubMed] [Google Scholar]