Background:
One of the most distinctive management competencies is related to the ability to structure the strategic vision, develop long-term plans, and communicate them efficiently to the employees in order to empower them to enact. These managerial competencies in complex organizations are strongly related to the capacity to engage professionals as a predictor of high-performing organizations.
Purpose:
The aim of this study was to investigate the relationship between top management competencies, information sharing, and organizational performance in public health care system and to look at the management role in assuring information sharing on organizational strategies to achieve professionals’ engagement.
Methodology/Approach:
This relationship is empirically tested using the longitudinal data of public health care organizations from the Tuscany Region (Italy). The top management competencies and information sharing are evaluated by the heads of the departments. While information sharing refers to the organizational level (e.g., to convey the objectives), managerial competencies refer to the individual level (e.g., to manage conflict). A random effect regression model is estimated using average responses by the health organization. Data come from the multidimensional performance evaluation system (2008 to 2014 years).
Results:
Findings show that managerial competencies are positively associated to organizational performance. Moreover, managerial competencies are strongly linked to the information sharing process developed into the organizations. In particular, managerial competencies play a significant role on whole performance, and results are mediated by the use of mature information sharing instruments such as benchmarking of performance results.
Conclusion:
Systematic information sharing process regarding performance results, goals, and organizational structure provided by top management seems an effective strategy to engage professionals. Control variables suggest that top management tenure and turnover do not have an effect, whereas bigger health care organizations seem to negatively influence this relation.
Practice Implications:
Information sharing is the basis for clinicians’ engagement and adds value to organizational performance.
Key words: competencies, human resources, organizational climate, performance management, top management
Performance measurement has a long tradition in public policy and management, and it has found a fertile ground in the public health care sector (Arah, Klazinga, Delnoij, ten Asbroek, & Custers, 2003). Since the 1990s, the traditional control measurement systems, based on accounting-based metrics alone, have been complemented by multidimensional performance measurements in both for-profit and not-for-profit sectors (such as Balanced Scorecard, Stakeholders Approach, or European Foundation for Quality Management), in order to capture both financial and nonfinancial results. Moreover, the literature highlights other critical factors, leading to successful performance management systems, including the development of user-friendly and practical reporting system and the identification and inclusion of performance targets/trends or definition of systematic benchmark. Target setting and development of a relative plan to achieve targets lead stakeholders toward desired goals (Brown, Closson, Sullivan, & Baker, 2012). Benchmarking helps managers and policy makers to learn from other’s experiences (best practice), detect unwarranted variations, and overcome self-referential behaviors. Public data disclosure is essential to stimulate engaged interests and responsibilities of stakeholders (Nuti & Vainieri, 2016).
Among the dimensions to be evaluated in performance management systems, strategic management scholars have suggested the inclusion of employee perception, retention, and productivity. Taking into account the importance of employee satisfaction is also linked to the evidence coming from the management literature, which advises that satisfied employees tend to be more productive, creative, and enthusiastic (Judge, Thoresen, Bono, & Patton, 2001). This, in turn, has a direct and positive impact on the functioning of the whole organization, and it strongly affects organizational performance (Judge et al., 2001; Schneider, 1980). Other scholars have also studied organizational and psychological climate as predictor of good work performance (Patterson et al., 2005) where supportive management, clear work roles, and challenging tasks have a positive effect on job involvement, together with free expression of one’s self and appropriate work recognition.
Moreover, in the public health care sector, assessment tools for nonfinancial dimensions of performance are needed, as conventional financial reporting would not include performance in a full and exhaustive way (Guthrie & English, 1997). For example, public health systems that spend more do not necessarily have better performance. Indeed, the opposite may be true as it has been found in the relationship between Italian per-capita expenditure and overall performance (Nuti, Daraio, Speroni, & Vainieri, 2011). The empirical evidence supports the idea that better performance is not the mere function of higher financial capacity but the efficient and effective combination of available resources to meet population needs. Resource combination is a fundamental part of management, where organizational goals can be achieved by working with and through people and other organizational resources. Among the most distinctive management competencies are those that create the most functional organizational conditions to achieve goals. This article aims at empirically investigating the relationship between managerial competencies and the organizational performance of public health care organizations considering also the role played by information shared by top management. In many health care management studies, attention has been devoted to the question of whether management matters, how it matters, and what management style and managerial practices should be used in order to improve performance. The review by Lega, Prenestini, and Spurgeon (2013) found four major research approaches investigating the impact of management on health care performance: (a) the impact of management practices on performance, (b) the impact of managers’ characteristics on healthcare performance, (c) the impact of the engagement of professionals in performance management, and (d) the impact of organizational features and management styles on performance.
Although there is still controversy among scholars, the first research stream suggests that better managerial practices (i.e., planning, organizing, coordinating, and controlling) are significantly related to better clinical and financial performance (Bloom, Propper, Seiler, & Van Reenen, 2009). The second research stream highlights that if top management has a clinical background this could be a predictor of high performance (Bloom et al., 2009; Veronesi, Kirkpatrick, & Vallascas, 2013). The third research stream shows strong association between engagement of physicians in management practices and improved performance (Macinati & Rizzo, 2016; Spurgeon, Mazelan, & Barwell, 2011). The fourth research stream investigates the relation between performance, organizational features, and management styles. In particular, a study comparing hospitals with different levels of performance (Mannion, Davies, & Marshall, 2005) shows that high-performing structures differ from others in that they have some common features such as the prevailing approach to transactional leadership (rather than the charismatic one), a multidimensional performance management system, clarity of goals, and the use of managerial operating systems (e.g., strategic planning, budgeting, and business planning).
Health care organizations are considered complex and adaptive systems characterized by various organizational designs, multiple vertical and horizontal interconnections, and a high level of formal control coupled with a high degree of individual professional autonomy and influence. Indeed, health care institutions are strongly dependent on their physicians in order to deliver high-quality care, to improve the health of populations, and to enhance health care’s sustainability (Berwick, Nolan, & Whittington, 2008; Kaissi, 2014). As a result, health care organizations should present a “reverse hierarchy” (or inverted pyramid), in which professionals take action on the delivery of quality and appropriate care whereas top management not only facilitates change but also orients their actions by communicating organizational strategies and vision (Bini, 2015). Indeed, top management competencies include the unique capabilities of the organization’s strategic leaders to articulate strategic vision, communicate it throughout the organization, and empower organizational members to realize it (Hambrick & Mason, 1984). Overall performance is the result of interdependent work of highly specialized employees that directly engage with patients (or customers more in general) and create value across the organization. Indeed, authors have highlighted a strong positive link between an organization’s clinical and financial performance and the degree to which physicians are engaged with the organization (Kaissi, 2014; Macinati & Rizzo, 2016; Spurgeon et al., 2011). In this context, information sharing about organizational goals and achieved outcomes is a key mechanism to foster the functioning of this “reverse hierarchy” model.
This article analyzes the relationship between top management competencies and the whole organizational performance of health care organizations focusing, in particular, on the role of information sharing that should support the flow of the strategic and operational vision and engage professionals in enacting their role.
The study measures the impact of top management competencies on public health care organizational performance using longitudinal data from Tuscany, a region in the Italian health care system. Tuscan public health care organizations provide prevention and primary care as well as hospital services. In particular, two data sources are used: the routine organizational climate survey (to measure the top management competencies) and the yearly results of the Tuscan Performance Evaluation System (PES) that measures and evaluates multiple health care performance dimensions of public health care organizations, from financial viability to quality and patient satisfaction, through a systematic and publicly disclosed benchmarking (Nuti & Vainieri, 2016; Nuti, Vola, Bonini, & Vainieri, 2016). Usually, authors who dealt with this topic measured both organizational performance and competencies throughout the staff self-assessment as reported by the quite recent large-scale study conducted in the English National Health System on the relationships between effective board governance (including analysis on competencies) and safe care (Mannion, Freeman, Millar, & Davies, 2016). Hence, the peculiarity of this research is to provide supporting empirical evidence using longitudinal and objective data from a large multidimensional PES and employees’ perception of top management competencies.
The article is structured as follows. Next section examines the three concepts upon which the relationship is investigated: performance, managerial competencies, and information sharing. It introduces the hypotheses that will be tested throughout the empirical investigation. The following section on the methodology explains how variables are operationalized and how data are sourced. The statistical analysis is then presented, and the section with the results reports considerations on the empirical analyses and the limitations of the study. The final sections provide conclusions and implications for practice.
Theory
Performance and Employees’ Perception of Managerial Competencies
In decentralized health care systems such as the Italian one, the highest organizational positions in public health authorities, for example, the General Manager (GM), are critical for the smooth operation and performance of the organization. The importance of top management leadership is not justified only because of its hierarchical role, but also because it connects the political level of the decentralized institution and the operational core of the organizations (Del Vecchio & Carbone, 2002). Indeed, strategies starting from political agendas developed at a regional level are then translated and operationalized in organizational goals and activities by top management. Several factors that can positively influence the effectiveness of top management actions in strategy definition and implementation are related with background and experience (Veronesi et al., 2013), the prevailing organizational culture (Lega et al., 2013), and managerial competencies (i.e. body of knowledge, Bloom et al., 2009).
These managerial competencies, together with others (e.g., communication, leadership, knowledge of health care environment, and professionalism), potentially create a sustained competitive advantage over those that lack such capabilities because they focus and channel organizational competencies (resources) toward effective accomplishment (Lado & Wilson, 1994). Hence, performance is expected to be influenced by how top management is able to engage employees in tasks and activities to improve individual job performance, which is strictly linked to better organizational outcomes (MacLeod & Clarke, 2011).
Different scales have been proposed to group competencies that both top and senior healthcare managers should acquire to get better results; a very basic distinction is between managerial and relational competencies as proposed by Pizzini and Furlan (2012). Following these authors, managerial competencies related to the top management are (a) a clear definition of strategy and goal setting, (b) the involvement in decision-making, (c) the encouragement of knowledge sharing, (d) conflict management, (e) feedback provision, and (f) overall satisfaction with top management’s role. These competencies are also included into the business skills and knowledge domains of the American health care leadership alliance model (Stefl, 2008). Considering the six managerial competencies, we expect that top management with higher managerial competencies is associated to higher level of organizational performance.
H1. Managerial competencies are positively associated with organizational performance.
Considering the internal focus, effective managers should help to connect their staff with the overarching goals and priorities of their organization, facilitate the spread of organizational knowledge, and provide feedback on organizational outcomes. Among the relational competencies, (a) the level of knowledge of the organization of chart, (b) the level of knowledge of the overall organization annual targets/goals, and (c) the level of knowledge of the overall annual organization results (Pizzini & Furlan, 2012) are those related to the communication of the functioning of the overall organization. The first two mirrors the vision and strategies of top management, whereas the third is linked to the overall feedback about the organization results. These aspects can be seen as a proxy of the first Weberian model for social action: shared purpose (Lee & Cosgrove, 2014). Because this information is linked to the way of sharing strategies and vision, we expect these factors to be highly correlated to managerial competencies.
H2. Managerial competencies are positively associated with information sharing.
An extensive body of research on relational coordination indicates that the reinforcing process of internal communication and relation for the purpose of task alignment and integration is significantly associated with organizational performance in the health sector (Gittell, 2009). Relational coordination dimensions include both shared goals and shared knowledge of team members’ tasks-relevant ideas, information, and suggestions (Srivastava, Bartol, & Locke, 2006) and frequency, timeliness, and accuracy of communication. Specifically, information sharing is a critical team process because if knowledge is not socialized, then the cognitive resources available within individuals remain underused (Argote, Ingram, Levine, & Moreland, 2000), and it plays a relevant role in enhancing performance (Srivastava et al., 2006). Indeed, information sharing is one tool adapted to engage doctors in the health care organizations (Lee & Cosgrove, 2014). Moreover, leaders believe that relational dimensions contribute to the development of care management, including contributions to standardization of care, patient engagement, coordination of care, and care planning (Rundall, Wu, Lewis, Schoenherr, & Shortell, 2016).
H3. Information sharing is positively associated with organizational performance.
Moreover, these competencies interact with each other and in turn with organizational performance. Indeed, information sharing (i.e., a perception regarding top management’s effective and timely diffusion of information on planning and monitoring activities) is a potentially important intervening dependent variable into the managerial competencies and organizational performance relation (Smith et al., 1994). The way in which top management communicates with and engages its employees is likely to have strong implications for how they are perceived in their role.
Figure 1 shows the model used to test the relationships between organizational performance, top management competencies, and information sharing. The model takes into account the role of information sharing on the relation between performance and managerial competencies. Given the variables included in the scale selected as reference (Pizzini & Furlan, 2012), although information competencies refer to the organizational level (to convey strategies to the staff), managerial competencies refer to the individual level (e.g., to manage feedback, conflict). As it was highlighted by other authors who studied the characteristics of high-performing hospitals, “information-based systems of accountability, empowered middle management and pro-performance values seem to be important underpinnings of a clearly articulated corporate strategy” (Mannion et al., 2005). Effective information sharing between top management and professionals relies on several conditions: among these, public disclosure of benchmarking plays a fundamental role. Indeed, systematic benchmarking regarding clinical issues fosters reputational pressure among clinicians by means of peer-to-peer comparison on quality of care and clinical results.
Figure 1.
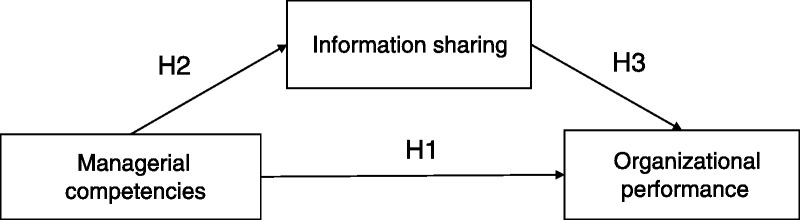
The mediation model and the three tested hypoteses
Hence, we assume that information sharing about the annual strategy, results, and organization structure may mediate the relationship between managerial competencies and organizational performance.
In particular, the model will test if communication and information sharing mediates the relationship between top management competencies and organizational performance.
Method
Sample and Data Collection
To test the hypotheses, we use a 4-year panel data set from all the 16 public health organizations of the Tuscany Region (Italy), of which 4 are teaching hospitals and 12 are local health authorities. We excluded one hospital foundation from the analysis, because it provides only cardiovascular care; thus, its overall performance is not comparable with the other health care organizations. In total, 62 observations (16 health care organizations across 4 years minus two because of missing observations on the independent variables) are included in the analysis.
Currently, the Tuscany regional health care system covers 3.7 million inhabitants and has about 50,000 professionals with annual expenditures of over 6.5 million euros. Employees within the organizations range between 1,011 and 6,380, whereas heads of the departments range between 37 and 301. The local health authorities provide preventive medicine and public health services, primary care, and secondary care, whereas the teaching hospitals focus their activities on acute care and professional training. Public health organizations are directly dependent on the regional government, which funds them on a capitation basis (Ferré et al., 2014).
The dependent variable is gathered from the PES that publicly discloses multidimensional health care performance indicators (Nuti & Vainieri, 2016). The PES has been active since 2005, and it includes 60 composite indicators and more than 600 simple indicators, which measure the performance of each health care organization considering (Nuti & Vainieri, 2016) population’s health status, capacity to timely pursue regional strategies, clinical performance, efficiency and financial performance, patient satisfaction, and staff satisfaction. Indicators are yearly calculated for each public health organization by using administrative and standardized clinical databases anonymized by the region. Each performance indicator is assessed in benchmarking considering international or national/local standards by using five colored evaluation bands (where dark green is the best performance and red is the worst; Nuti &Vainieri, 2016). As a result, for each evaluation measure, five different performance levels define the performance of each health organization in each category, from worst to best on a scale from 0 (worst) to 5 (best). In addition, color bands are assigned: 1, red; 2, orange; 3, yellow; 4, green; 5, dark green.
The independent variables are measured using data from the routine organizational climate survey administered to the heads of departments working in all the regional public health organizations via computer-assisted Web interviewing on a census base (full details about the questionnaire can be found in Pizzini & Furlan, 2012). Following the literature on attitude and competencies evaluation (Shipper & Davy, 2002), this study uses the rating of the employees closely working with top management (i.e., heads of department) as an observed measure of top management competencies instead of employing self-rating instruments. Indeed, heads of departments are—by role—the ones experiencing frequent interactions with top management teams. They are mainly health care professionals who are called to cover a managerial role because they are responsible for short-term operational planning and monitoring of their departments and report directly to top management. Top management roles are a limited number; usually the GM (or the chief executive officer) chooses the Chief Health Officer, the Chief Financial Officer, and, in some cases, other figures (such as the Chief Social Services Officer), depending on the health care systems. The regional health councilor, following the spoil system, appoints top management every 3–5 years based on the regional contract. Instead, the heads of departments are a larger number of professionals directly appointed by GM. In Italy, for instance, top management roles generally lead organizations of around 2,500 employees (the size can vary from less than 1,000 to more than 10,000) whereas the ratio of the heads of the departments is around 50–60 every 1,000 employees. Thus, health care heads of departments are in the best position to evaluate how the GM and his/her team (top management in general) are doing.
The two variables from the climate survey about management competencies and information sharing represent the average assessment that head of departments give to the items of the questionnaire on a 5-point Likert scale. The individual responses are transformed into a 100-point scale by following the methodology already applied in other experience surveys (Murante, Seghieri, Brown, & Nuti, 2014), and average responses grouped by health organization are used in the analysis. Indeed, dependent and independent variables are intended to represent the organizational values. The data have a time series structure with measurements for an even number of years from 2008 to 2014 (2008, 2010, 2012, and 2014) because the survey is conducted every 2 years. Around 1,000 senior managers per year replied to the survey (e.g., for 2014 responses ranged from 16 to 156 for each health care organizations) with the following response rates: 72% (standard deviation of 19%) for 2008, 65% (standard deviation of 13%) for 2010, 67% (standard deviation of 16%) for 2012, and 61% (standard deviation of 14%) for 2014 (see Annex 1 for yearly response rate by health organizations).
For the control variables, the data are extracted from public data on GMs’ work experience and public health authorities’ organizational features.
Measures
As defined earlier, organizational performance has several components. The PES indicators of the Tuscany Region were used to define it for the years 2008, 2010, 2012, and 2014.
The dependent variable for each public health organization is defined as the overall net performance of the 60 indicators or the overall average performance of the 60 indicators.
Overall net performance is calculated using data from the PES (http://performance.sssup.it/toscval) following the same algorithm of Nuti et al. (2011). PES covers a wide range of indicators (around 60 composite indicators) related to population’s health status, capacity to timely pursue regional strategies, clinical performance, efficiency and financial performance, patient satisfaction, and staff satisfaction. Indicators are evaluated attaching the five colored bands and the 0–5 score. For each year, the overall assessment is the difference between the excellent and good performance scores (dark green and green) and the poor and very poor performance scores (orange and red) on the total of indicators, with the exclusion of the population health status domain since the data has a 3-year time lag. We also use the average yearly health care organization performance calculated as the average of the performance scores of all the indicators within the Tuscan PES, always excluding the population health status.
Managerial competencies are operationalized as the health care organization score given by heads of the departments to top management on six items: (a) the top management clearly defines strategy, (b) the top management involves me in decision-makings related to my unit, (c) the top management encourages knowledge sharing among departments, (d) the top management is able to manage conflicts, (e) the top management provides feedback about my work, and (f) I like the way the top management is working.
Information sharing is operationalized as the health care organization score given by heads of the departments to three items: (a) I am familiar with the organization of chart, (b) I am familiar with the overall organization annual goals, and (c) I am familiar with the overall annual performance results.
External variables may cloud the relationship between top management competency, information and communication, and performance. A variety of contextual factors are controlled for the type of health organization (teaching hospitals vs. local health authorities) because of the different activities and expectations of the employees. Another control is made on to the size of the health organization because complexity and interdependency across departments might vary. Size is measured as the number of personnel: less than 3,000 and more than 3,000 using the median distribution as threshold to identify the two groups. The influence of several factors used in previous studies is tested to mitigate the effect of top management turnover on organizational performance (Del Vecchio & Carbone, 2002) and career experience. Specifically, we considered two dimensions: organizational tenure of the GM, which is measured as the number of years spent in the health organization as a member of top management team, and GM turnover, a dummy variable that indicates if the health organization has undergone a change in the GM within the year. In addition, past performance is included to control for the possible effects of prior organizational performance that might influence employees’ evaluation of top management. Finally, we included the response rate to the organizational climate survey. This is a proxy measure of organizational commitment since evidence suggests that organizations with best performance are often those that invest more on management commitment (Pizzini & Furlan, 2012).
Statistical Analyses
To test the three hypotheses and the mediation effect of information sharing and communication on organizational performance, a linear panel data regression analysis is conducted following Baron and Kenny’s (1986) mediation model. Three conditions have to be met to establish mediation:
The causal variable (perception of top management competency) should be significantly related to the outcome (performance).
The causal variable (perception of top management competencies) should be related to the mediator (information sharing).
The mediator should be related to the outcome variable with the causal variable included in the equation. This step essentially involves treating the mediator as if it were an outcome variable. To establish that mediation has occurred, a significant relationship between the independent variable(s) (top management competency) and a dependent variable(s) (organizational performance) is reduced (partial mediation) or is no longer significant (full mediation) when controlling for the mediator (information sharing).
A random effect regression model is estimated using responses by health organization. Postestimation tests are performed for serial correlation (Lagrange Multiplier test) and heteroscedasticity (Breusch–Pagan test). For net performance, autocorrelation was not an issue but confirmed the presence of heteroscedasticity. This is taken into account by using robust standard error estimates. Multicollinearity is tested using the variance inflator factor, and no significant collinearity exists—small average standard error (less than 3) for the coefficient of the predictor if the predictor variable is correlated with other predictor variables. STATA (version 12) software package is used to perform all statistical analysis.
Results
Table 1 provides descriptive statistics and correlations for managerial competencies, information sharing, organizational performance, and control variables. Net performance has a distribution that includes negative value, meaning that organizations can have a negative balance in their yearly performance if they have a poor performance in several dimensions of the performance management system. Health care organizations on average present 26% of the indicators with a positive performance, but this varies significantly across years and health care organizations, displaying a normal distribution. The perception of managerial competencies registers on average a score of 62.13 out of 100 points; a little bit higher is the level of information sharing with an average value of 64.58 out of 100 points. The organizational climate survey is filled out on average by 67% of the heads of the departments, with lower commitment levels among teaching hospitals (less than 50% on average). On average, in Tuscany the years of experience that GMs accumulate while working within an organization in the top management team is 3 years and a half. On average GM turnover is low and is negatively associated to the dependent variable, but it is not significant. The number of personnel employed in public health organizations in Tuscany is variable, ranging from more than 6,500 employees to less than 800. Interestingly, when personnel number increases, there is a significant inverse relationship with net performance, and this might be explained by the higher complexity level.
Table 1.
Descriptive statistics and correlation matrix
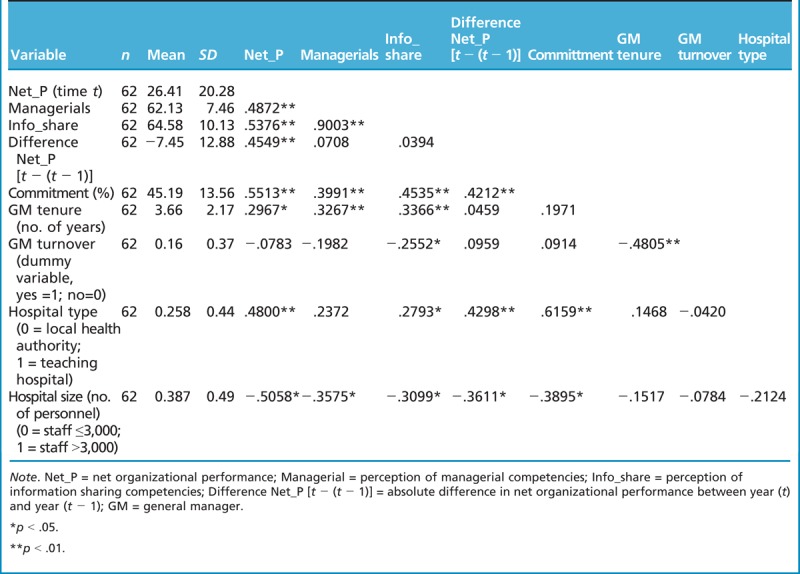
Table 2 indicates the results of the multiple regression analysis that considers net performance as the dependent variable. Results remain constant when using average performance as a dependent variable. The influence of control variables is first tested by regressing organizational performance on all the controls, and two regression coefficients are found to be statistically significant. Size of the health organization and the level of the heads of departments’ organizational commitment are both significant at 90%. The level of organizational tenure of the GM and turnover are not significant in explaining performance. Three regression models are examined (Table 2).
Table 2.
Regression results for main effects and mediation hypotheses
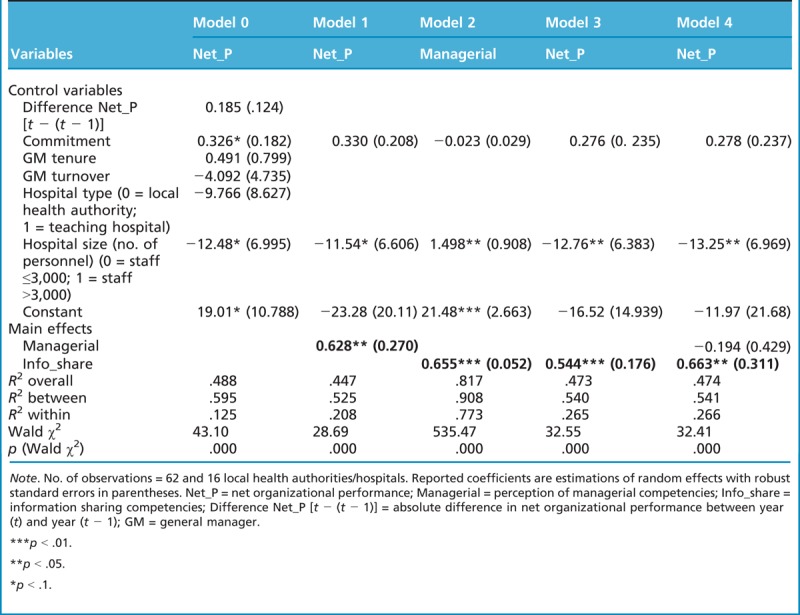
The models presented in Table 2 shed light on the nature of the relationship between the perceptions that heads of departments have of top management core competencies and organizational performance.
All the control variables are entered only in Model 0.
Results confirm the first hypothesis (H1) that managerial competencies are positively associated with organizational performance. Indeed, in Model 1, the positive relationship between the perception of top management competencies and performance is supported, and the coefficient is significant at p < .05. According to heads of departments, top management has a key role in performance achievement. In particular, an increase of 1 point in the perception of managerial competencies is associated to an increase of the overall net performance of 0.628.
Model 2 confirms also the second hypothesis (H2): Managerial competencies are positively associated with information sharing. An increase of 1 point in the information sharing leads to an increase of 0.655 in the evaluation of managerial competencies. Moreover, the importance of a statistically significant relationship between the two variables is an assumption of the mediation model.
Model 3 supports the sentence of the third hypothesis (H3): Information sharing is positively associated with organizational performance. Heads of departments’ perception of increased level and intensity of information sharing within the organization has a significant (p < .01) and positive effect on performance.
The last model (Model 4), together with the previous ones, sheds light on the mediating effect of information sharing in the relationship between managerial competencies and performance. In particular, Model 4 looks at the effect of both heads of departments’ perception of top management competencies and the cascade of organizational information on yearly organizational performance. As expected, the signs of both coefficients are positive, but magnitude and significance are lower if we compared Models 1–3 and they become not significant for management competencies. The near zero coefficient and the low variance in the direct pathway indicate that clear information on organizational structure and strategies fully mediate the effect of managerial competencies on whole organizational performance. This occurs if we assume that mediation includes a unidirectional relationship between the independent and mediating factor and a unidirectional arrow from the mediating factor and the independent variable (Baron & Kenny, 1986). The indirect effect is tested using the bootstrapping method with 1,000 replications (Bollen & Stinet, 1990). The observed coefficient is 0.037, and we can conclude that the indirect effect of information sharing on organizational performance is indeed significantly different from zero at p < .05 (CI [0.0795, 2.4752], percentile CI [0.138, 2.517], bias-corrected CI [0.118, 2.499]; Hayes & Scharkow, 2013).
In all models, size of the health organization—expressed in number of personnel—is significant and negatively related to organizational net performance, whereas level of commitment and GM tenure and stability are not significant. The effect of committed organizations disappears when inserted in the relational model, indicating that high commitment is not significant in the mediation. The lack of a statistically significant impact of leadership change over performance level can be explained by the smoothness of change.
Discussion
Scholars and health professionals have always considered the health care context as an area of particular complexity where stakeholder’s roles, relations, and powers are interconnected. In this context, top management plays a peculiar role: they are liable for the financial sustainability of the health care system and overall performance obtained by their organization, even though the decisions regarding most of the expenditure and the type of services to be delivered to meet the patient’s needs are taken by the health professionals. Often, because of this unconventional hierarchical position, it is questioned to what extent GM managerial capabilities can make “the difference” on the performance of public health care organizations. Indeed, very often, at least in the Italian context, it is believed that public health care organizations, given their large size (3,000–6,000 employees), are run primarily by regulatory mechanisms and rules rather than by management tools and by the management roles.
To expand this research stream, we empirically investigate the relationships between managerial competencies and organizational performance by using longitudinal data from the multidimensional PES adapted by the Tuscany Region between 2008 and 2014.
Findings from the empirical study show that the managerial competencies of top management (measured throughout the heads of departments’ assessment) seem to have a significant positive effect on overall performance (0.628, p < .05, Model 1; Table 2). This relation is fully mediated by information sharing strategies on organizational structure, goals, and overall performance results (Model 4; Table 2). Hence, strategies for increased use and active diffusion of information about organizational structure, goals, and performance achievements are key elements that managers, especially GMs, should acquire and practice to facilitate goal attainment.
This empirical evidence supports the idea that in a reverse hierarchy the GM is able to enable professionals’ engagement to organizational performance throughout the communication of organizational vision. In particular, the study analyzed the influence of key information sharing related to both organizational strategies (roles and responsibility through the organization chart and goals) and results. However, it has to be acknowledged that the analyses were carried out in a particular environment where performance, including clinical results, is yearly publicly disclosed in benchmarking. These last two elements foster reputational pressure among professionals. We believe that this situation has influenced the mediating effect of information sharing.
Interestingly, it is worth noticing that a significant effect of GM tenure or GM turnover on the organizational performance of public health care organizations is not found. This evidence is consistent with other findings (Ballantine, Forker, & Greenwood, 2008), but it seems to be partially in contrast with general Italian GM turnover results, which seem to be related to single health care performance indicators (especially financial and efficiency-based indicators) as well as executives tenure (Ballardini & Fabbri, 2011). However, the authors suggest that the regional political cycle is one of the principal factors influencing turnover levels supporting our data. The Tuscany Region is an exception; in fact, it has been characterized by a certain level of regional political continuity, where the 2007 health councilor became the regional governor in 2010 yielding smooth GM turnovers.
Moreover, the size of the organization is a quite debated issue in both general and health care literature. In particular in Tuscan health care system, even the smallest of the health care organization is, in absolute term, a large organization, whereas the largest can be compared to multinational firms. The larger the organization, the larger is the distance between GM and the heads of the departments. Hence, the larger the organization, the higher is the effort that should be put by top management in conveying strategies and information. This evidence is particularly interesting because it seems to challenge the trend currently emerging among Italian regions, which are deciding to merge health care organizations.
The findings of this analysis are subject to limitations. First, the small sample size (62 observations in total) can yield an influence on the models’ internal validity, so the results should be interpreted with caution. Control for measure reliability was introduced in the posttest analysis using the Breusch–Pagan test for heteroskedasticity that showed a low variance of error terms and used robust standard error. Moreover, there are several measurement challenges regarding both dependent and independent variables. The causal measurements included capturing only a limited aspect of the concept of managerial capabilities, and this is an even more demanding task when assessing individuals in specific managerial positions. Often authors measure top management or board of directors competencies throughout self-assessment questionnaire or mixed-methods where self-rated assessment is combined with semistructured interviews as recently reported by Mannion et al. (2016). Our approach tries to overcome the self-assessment bias and relies on objective organizational performance results and external observations of GM competencies using ratings of heads of departments’ perception of top management capabilities since they are in the best position to evaluate GMs (e.g., easy access to information about managerial behavior, organizational morale, environmental demands, and performance). Moreover, we think that the misrepresentation of generous assessments given to GMs (because they appoint heads of the department) is not relevant in the relation and does not influence the real overall performance of the organizations. Instead, the high correlation of top management competencies and information sharing found in the data could be interpreted as a source of measurement error (common method bias) since the same survey is used to collect both measures from the head of departments. However, the two variables constitute two different constructs as reported in the validation study of the organizational climate survey (Pizzini & Furlan, 2012).
Of further importance is the causality of the relationship found. One important explanation of the results—a possible reverse-causal impact of organizational performance on employees’ perception of top management capabilities and process variables—can be attenuated by the statistical control of the difference (or trend) in the previous year’s financial performance. Nonetheless, alternative causal sequences must not be dismissed. In addition, there may be other constructs, such as process variables that are worthy of study. Follow-up research is needed to elaborate alternative process explanations and sequences to explain how top management affects performance.
Despite these qualifiers, a particular strength of this study is that our analyses relate to both perception and objective measurements. In particular, performance is based on the results of a well-established multidimensional PES that considers all the different aspects of health care organizations instead of a single measurement or dimension. Even though researchers recognize the importance of this topic, most take a relatively descriptive approach to emphasize top management demographics, leadership styles and culture, presence of managerial tools and practices looking at a selection of variables, which are namely financial performance or clinical outcomes. In addition, the study highlights the important role played by top management in the process of information sharing on organizational strategies and results across professionals confirming that the reverse hierarchy could lead to positive results in health care.
Practice Implications
There are implications for practice that can be drawn from these data. First, it is important to promote the development of multidimensional PESs across health care organizations that disclose results in benchmarking. Indeed, benchmarking is a stimuli source that drives health professionals’ actions via reputation (Nuti & Vainieri, 2016), especially when clinicians participate in the selecting process of the indicators. Second, behavioral change efforts directed at engaging clinicians are likely to pay off in terms of organizational performance. Information sharing is indeed a key to stimulate internal commitment that ensures also a trustworthy environment (Brown et al., 2012; Rundall et al., 2014). Indeed, shared purpose is the first Weberian model for social action. Specificities of reverse hierarchy urge to consider two-way communication and information sharing approaches, aimed not only at making professionals participate in decision-making but also at enabling their engagement by, for instance, unifying language or narrative sets in the context of organizational vision and issues (Kaissi, 2014).
Indeed, the role of top management is to put in place information tools and strategies for sharing information regarding the goals, the achievement of performance results, and the organizational structure. In particular, sharing information on results, especially if they are shown in benchmarking, on different aspects of the health care organization, as it happens in the Tuscan context, seems to heighten the pressure on clinicians for achieving better results and making themselves feel responsible for finding solutions to emerging challenges. In fact, when professionals declare to be informed on aspects that they value (such as patient experience on doctors’ communication; Murante, Vainieri, Rojas, & Nuti, 2014), organizations perform better. Indeed, if performance in health care depends massively on the clinicians’ activity, the role of top management should be to support and facilitate this.
A final practical implication deriving from this study may concern a revision of the traditional training programs (even required by law in Italy) for both those already covering the top management roles and those aspiring to. Training programs should include more and more strategies and tactics related to how to effectively communicate and share information in large and complex organizations like the ones of health care.
Acknowledgments
We wish to thank all researchers of Laboratorio Management e Sanità who hardly work to develop and improve the performance evaluation system, which is the main source of information for this article. We are particularly grateful to Domenico Cerasuolo for his effort and stimuli in easing the job of all the team. Finally, we want to thank the anonymous reviewers. Their suggestions significantly contribute to the improvement of the article.
Footnotes
The authors have disclosed that they have no significant relationship with, or financial interest in, any commercial companies pertaining to this article.
References
- Arah O. A., Klazinga N. S., Delnoij D. M., ten Asbroek A. H., & Custers T. (2003). Conceptual frameworks for health systems performance: A quest for effectiveness, quality, and improvement. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care/ISQua, 15(5), 377–98. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/14527982 [DOI] [PubMed] [Google Scholar]
- Argote L., Ingram P., Levine J. M., & Moreland R. L. (2000). Knowledge transfer in organizations: Learning from the experience of others. Organizational Behavior and Human Decision Processes, 82(1), 1–8. doi:10.1006/obhd.2000.2883 [Google Scholar]
- Ballantine J., Forker J., & Greenwood M. (2008). The governance of CEO incentives in English NHS Hospital Trust. Financial Accountability & Management, 24(November), 385–410. [Google Scholar]
- Ballardini E., & Fabbri D. (2011). Top executives turnover, politics and performance of healthcare providers: Evidence from the Italian NHS. Pavia 19–20 Settembre.
- Baron R. M., & Kenny D. A. (1986). The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182. [DOI] [PubMed] [Google Scholar]
- Berwick D. M., Nolan T. W., & Whittington J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27(3), 759–769. doi:10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- Bini B. (2015). From performance measurement to performance management: Engaging physicians in decision-making processes and quality improvement strategies. Scuola Superiore Sant’Anna of Pisa; Retrieved from www.phdmanagement.sssup.it/awarded.php [Google Scholar]
- Bloom N., Propper C., Seiler S., & Van Reenen J. (2009). Management practices in hospitals (Health, Econometrics and Data Group No. 09/23).
- Bollen K. A., & Stinet R. (1990). Direct and indirect effects: Classical and bootstrap estimates of variability. Sociological Methodology, 20(1), 115–140. [Google Scholar]
- Brown A., Baker G. R., Closson T., & Sullivan T. (2012). The journey toward high performance and excellent quality. Healthcare Quarterly, 15(Spec No), 6–9. [DOI] [PubMed] [Google Scholar]
- Del Vecchio M., & Carbone C. (2002). Stabilità dei Direttori Generali nelle aziende sanitarie. In Pessina E. A., Cantù E. (Eds.), Rapporto OASI 2002 L ’ aziendalizzazione della sanità in Italia (pp. 268–301). Milano, Italy: Egea. [Google Scholar]
- Ferré F., de Belvis A. G., Valerio L., Longhi S., Lazzari A., Fattore G., Maresso A. (2014). Health system review: Italy. Health Systems in Transition, 16(4), 1–168. [PubMed] [Google Scholar]
- Gittell J. H. (2009). High performance healthcare: Using the power of relationships to achieve quality, efficiency and resilience. New York: McGraw Hill Professional. [Google Scholar]
- Guthrie J., & English L. (1997). Performance information and programme evaluation in the Australian public sector. International Journal of Public Sector Management, 10(3), 154–164. doi:10.1108/09513559710166039 [Google Scholar]
- Hambrick D. C., & Mason P. A. (1984). Upper echelons: The organization as a reflection of its top managers. Academy of Management Review, 9(2), 193–206. doi:10.5465/AMR.1984.4277628 [Google Scholar]
- Hayes A. F., & Scharkow M. (2013). The relative trustworthiness of inferential tests of the indirect effect in statistical mediation analysis. Does method really matter? Psychological Science, 24(10), 1918–1927. [DOI] [PubMed] [Google Scholar]
- Judge T. A., Thoresen C. J., Bono J. E., & Patton G. K. (2001). The job satisfaction–job performance relationship: A qualitative and quantitative review. Psychological Bulletin, 127(3), 376–407. doi:10.1037/0033-2909.127.3.376 [DOI] [PubMed] [Google Scholar]
- Kaissi A. (2014). Enhancing physician engagement: An international perspective. International Journal of Health Services: Planning, Administration, Evaluation, 44(3), 567–592. doi:10.2190/HS.44.3.h [DOI] [PubMed] [Google Scholar]
- Lado A. A., & Wilson M. C. (1994). Human resource systems and sustained competitive advantage: A competency-based perspective. The Academy of Management Review, 19(4), 699–727. [Google Scholar]
- Lee T. H., & Cosgrove T. (2014). Engaging doctors in the health care revolution. Harvard Business Review, 92(6), 104–111, 138. [PubMed] [Google Scholar]
- Lega F., Prenestini A., & Spurgeon P. (2013). Is management essential to improving the performance and sustainability of health care systems and organizations? A systematic review and a roadmap for future studies. Value in Health, 16(1 Suppl.), S46–S51. doi:10.1016/j.jval.2012.10.004 [DOI] [PubMed] [Google Scholar]
- Macinati M. S., & Rizzo M. G. (2016). Exploring the link between clinical managers involvement in budgeting and performance: Insights from the Italian public health care sector. Health Care Management Review. 41(3), 213–223. doi:10.1097/HMR.0000000000000071 [DOI] [PubMed] [Google Scholar]
- MacLeod D., & Clarke N. (2011). Engaging for success: Enhancing performance through employee engagement, a report to Government. Richmond Surrey: Office of Public Sector Information. [Google Scholar]
- Mannion R., Davies H. T., & Marshall M. N. (2005). Cultural characteristics of “high” and “low” performing hospitals. Journal of Health Organisation and Management, 19(6), 431–439. doi:10.1108/14777260510629689 [DOI] [PubMed] [Google Scholar]
- Mannion R., Freeman T., Millar R., & Davies H. (2016). Effective board governance of safe care: A (theoretically underpinned) cross-sectioned examination of the breadth and depth of relationships through national quantitative surveys and in-depth qualitative case studies. Health Service Delivery Research, 4(4). doi:10.3310/hsdr04040 [PubMed] [Google Scholar]
- Murante A. M., Seghieri C., Brown A., & Nuti S. (2014). How do hospitalization experience and institutional characteristics influence inpatient satisfaction? A multilevel approach. International Journal of Health Planning and Management, 29(3), e247–e260. doi:10.1002/hpm.2201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murante A. M., Vainieri M., Rojas D., & Nuti S. (2014). Does feedback influence patient–professional communication? Empirical evidence from Italy. Health Policy, 116(2–3), 273–280. [DOI] [PubMed] [Google Scholar]
- Nuti S., Daraio C., Speroni C., & Vainieri M. (2011). Relationships between technical efficiency and the quality and costs of health care in Italy. International Journal for Quality in Health Care, 23(3), 324–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuti S., & Vainieri M. (2016). Strategies and tools to manage variation in regional governance systems. In Stukel T. A., & Johnson C. C. A. (Eds.), Medical practice variations (pp. 433–457). New York: Springer; doi:10.1007/978-1-4899-7573-7 [Google Scholar]
- Nuti S., Vola F., Bonini A., & Vainieri M. (2016). Making governance work in the health care sector: Evidence from a “natural experiment” in Italy. Health Economics, Policy and Law, 11(1), 17–38. doi:10.1017/S1744133115000067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson M. G., West M. A., Shackleton V. J., & Dawson J. F., Lawthom R., Maitlis S., Wallace A. M. (2005). Validating the organizational climate measure: Links to managerial practices, productivity and innovation. Journal of Organizational Behavior, 26(4), 379–408. doi:10.1002/job.312 [Google Scholar]
- Pizzini S., & Furlan M. (2012). L’esercizio delle competenze manageriali e il clima interno. Il Caso del Servizio Sanitario della Toscana. Psicologia Sociale, 18(3), 429–446. [Google Scholar]
- Rundall T. G., Davies H. T., & Hodges C. L. (2004). Doctor–manager relationships in the United States and the United Kingdom. Journal of Healthcare Management, 49(4), 251–268. [PubMed] [Google Scholar]
- Rundall T. G., Wu F. M., Lewis V. A., Schoenherr K. E., & Shortell S. M. (2016). Contributions of relational coordination to care management in accountable care organizations: Views of managerial and clinical leaders. Health Care Management Review, 41(2), 88–100. doi:10.1097/HMR.0000000000000064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider B. (1980). The service organization: Climate is crucial. Organizational Dynamics, 9(2), 52–65. doi:10.1016/0090-2616(80)90040-6 [Google Scholar]
- Shipper F., & Davy J. (2002). A model and investigation of managerial skills, employees’ attitudes, and managerial performance. Leadership Quarterly, 13(2), 95–120. doi:10.1016/S1048-9843(02)00098-X [Google Scholar]
- Smith K. G., Smith K. A., Olian J. D., Sims H. P., Douglas P., Smith K. G., Scully J. A. (1994). Top management team demography and process: The role of social integration and communication. Administrative Science Quarterly, 39(3), 412–438. [Google Scholar]
- Spurgeon P., Mazelan P. M., & Barwell F. (2011). Medical engagement: A crucial underpinning to organizational performance. Health Services Management Research: An Official Journal of the Association of University Programs in Health Administration/HSMC, AUPHA, 24(3), 114–120. doi:10.1258/hsmr.2011.011006 [DOI] [PubMed] [Google Scholar]
- Srivastava A., Bartol K. M., & Locke E. A. (2006). Empowering leadership in management teams: Effects on knowledge sharing, efficacy, and performance. Academy of Management Journal, 49(6), 1239–1251. doi:10.5465/amj.2006.23478718 [Google Scholar]
- Stefl M. E. (2008). Common competencies for all healthcare managers: The Healthcare Leadership Alliance Model. Journal of Healthcare Management, 53(6), 360–374. [PubMed] [Google Scholar]
- Veronesi G., Kirkpatrick I., & Vallascas F. (2013). Clinicians on the board: What difference does it make? Social Science and Medicine, 77, 147–155. doi:10.1016/j.socscimed.2012.11.019. [DOI] [PubMed] [Google Scholar]


