Abstract
Continuing medical education (CME) is meant to not only improve clinicians’ knowledge and skills but also lead to better patient care processes and outcomes. The delivery of CME should be able to encourage the health providers to accept new evidence-based practices, and discard or discontinue less effective care. However, continuing use of expensive yet least effective and inappropriate tools and techniques predominates for CME delivery. Hence, the evidence shows a disconnect between evidence-based recommendations and real-world practice – borne out by less than optimal patient outcomes or treatment targets not being met especially in low- to middle-income countries. There is an ethical and professional obligation on CME-providers and decision-makers to safeguard that CME interventions are appraised not only for their quality and effectiveness but also for cost-effectiveness. The process of learning needs to be engaging, convenient, user-friendly and of minimal cost, especially where it is most needed. Today’s technology permits these characteristics to be integrated, along with further enhancement of the engagement process. We review the literature on the mechanics of CME learning that utilizes today’s technology tools and propose a framework for more engaging, efficient and cost-effective approach that implements massive open online courses for CME, adapted for the twenty-first century.
Keywords: continuing medical education, health care, learning management system, massive open online courses, non-communicable diseases
Continuing medical education (CME) for effective clinical practice
Introduction
Physicians exert a deep impact on human life and are under constant pressure to learn when to intervene proactively, how to use complex investigative screening tools, and to be familiar with a vast variety of newly developed, potent yet potentially harmful, therapeutic agents.1 They have to deal with an aging population amidst changing population demographics and an increasing trend for non-communicable diseases (NCDs).1,2 The pressure will be more intense on low- to middle-income countries (LMICs), where 80% of the world’s aging population will reside by 2050, adding to the burden of NCDs atop that of communicable diseases.2 In the USA, the National Academy of Medicine (NAM) has prioritized chronic conditions as a focus to drive high-quality health care; most of these conditions being prevalent globally.3
To meet these extraordinary challenges of the twenty-first century, it is even more critical for today’s clinicians to actively engage in CME. CME bridges the gap between academic research and clinical practice, and plays a critical role in health care by providing clinicians with well-balanced education aligned to patient needs and evidence-based medicine.2–4
Advantages
The objective of CME is to help clinicians keep up-to-date about advances in patient care, train them to adopt the most beneficial care available, and encourage them to stop using interventions that confer lesser benefit.5 Evidence-based CMEs that translate scientific knowledge into practice and train clinicians to provide high-value evidence-based care can save significant cost to the health care system when doctors change their practice as a result of what they have learned.6 Systematic reviews have confirmed that CME improves not only physician performance but also patient health outcomes, although more positive impact is exerted on the former.7 Activities that are more interactive, involve multiple exposures and are focused on outcomes can lead to more positive outcomes.7
Challenges
Irrelevant content
CME is required for licensing and in many instances, this is only a compulsory “check box” requirement – at least in developed countries.8 However, providers are neither obliged nor mandated to create relevant content which can force clinicians to disengage from irrelevant educational activities.8 A review of 26 systematic reviews or meta-analyses of CME curricula that improved clinician behavior and/or patient outcomes examined the spectrum from most to least effective techniques used to conduct CME.5 Interactive techniques were found to be most effective at improving change in care and patient outcomes.5 Didactic presentations or printed education materials, on the contrary, demonstrated very little beneficial effect.9 Still, quite often, CME is didactic and passive, associated largely with conferences or other in-person meetings, e.g., formal courses, symposia, etc.1 Despite proof of more effective CME techniques, the use of these less-effective techniques predominate.5,9 This continuing use of unproductive CME not only reduces the quality of patient care but also contributes to poor utilization of scarce resources.
Although many licensing boards mandate that physicians participate in a certain number of CME hours, some also require physicians to participate in mandatory topics that might have little to do with their clinical practice.10 In most countries, physicians are required to obtain CME credits, with assessment or documentation of clinical performance improvement.1,11 CME interventions can be more rewarding if they are designed for individual learning needs and preferences. Unfortunately, many CME activities in current practice are not based on these principles.12
CME needs to evolve from counting the hours of participation to recognizing achievement in physician knowledge, competency, and performance.
Cost and sustainability
The CME industry has a turnover of several billion dollars a year.13 Total revenue for CME companies that are certified by the Accreditation Council for Continuing Medical Education in the USA was around $2 billion in 2010 which implies a per attendee cost of around $2500 per year excluding hotel, travel, and other miscellaneous expenses.14 This suggests good profitability for this industry that supports physicians’ mandatory commitment to lifelong learning. This high financial burden for the development of CME, or participating in CME is not always borne by participants or their employers.15 Other issues such as the impact of carbon emissions from airtravel on the environment have also sparked a debate on sustainability of face-to-face CME and medical conferences.16
CME credits are generally obtained by attending conferences, although participating on online courses, or reading and reviewing scientific papers are emerging trends.15 Today many programs are available online at little or no cost to the participant.14 Self-directed CME at the point-of-care has been shown to reduce the overall cost of CME, mainly by saving the costs of live meetings.17 While the cost of CME in the USA had doubled in just 7 years in 2007, there was a decline in the 3 years that followed due to the increasing use of free online CME.14
Access issues
There is tremendous heterogeneity in economic prosperity, funding, and access to health care around the world. The disparities in access to training and education of health professionals are also said to contribute to significant differences in morbidity and mortality from NCDs.15 LMICs face several challenges with their CME, e.g., outdated curricula, inadequate infrastructure, fewer well-trained educators, and cultural barriers.18 In fact, most clinicians in these nations are not informed about the potential benefits of CME and many may never have attended a CME session.19
Online CME is an attractive and effective option due to its availability at any time and any place, overall low cost of delivery and its increased impact and stimulus for knowledge translation and delivery.20,21 It also offers many benefits to practitioners especially in terms of saving travel cost and time that can particularly really benefit those based in rural and remote areas.22 A systematic review funded by the National Health and Medical Research Council of Australia assessed the effectiveness of online CME for general practitioners (GPs).22 Online CME was found to exert a significant improvement in knowledge, clinical practice, and satisfaction among GPs in most of the studies reviewed.22
Massive open online courses (MOOCs) in health and medicine
Virtual worlds have now become an integral part of the educational landscape.23 A blend of self-directed CME and face-to-face meetings is recommended to ensure that CME activities offer maximum value.23 Virtual worlds also offer tremendous potential to improve learning outcomes beyond that provided by face-to-face medical educational activities. Medical students have been found to prefer such blended courses over traditional classroom courses, with flexible learning time and improvement in study skills being key advantages.24 As higher education enters the Internet era, exploiting high-quality cyber resources may be the fastest and most economical way to improve teaching efficiency and enhance students’ study experience. The results of a cost analysis study among community health workers show significant savings, by as much as 67%, through a blended eLearning approach in comparison to a traditional didactic method.25
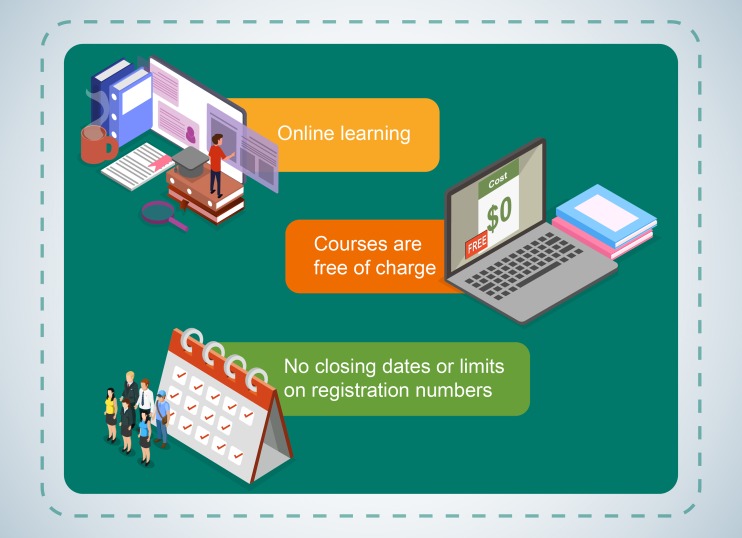
MOOCs are a form of online learning where online courses are accessible at little or no cost, and without limits on participant numbers or prerequisites (Figure 1).26 The first MOOC was set up by Stephen Downes and George Siemens at the University of Manitoba in 2008.27 Similar to other forms of online learning, MOOCs can be accessed through computers, smartphones, or other digital devices and usually consist of video lectures, interactive e-learning modules, assignments, and online discussions.27 MOCCs are kept interactive, for example, through frequent knowledge checks that make the viewers attentive, provide immediate feedback and guide them if they have not understood the key concepts.28
Figure 1.
Massive open online courses (MOOCs) – an overview.
Notes: MOOCs are open online learning courses freely accessible via the web. Unlike most traditional online courses, MOOC courses are free of charge and registration is often kept without any close dates.
MOOCs have attracted wide interest from universities, businesses, educators, and learners within a short time due to the fact that the content can reach large numbers of learners around the globe, and can be accessed by anyone provided they have Internet access, language proficiency, and computer literacy.26 Successful tuition MOOCs like those by the National Centre for Academic Transformation (NCAT) have returned great results with improved learning, satisfaction, and cost-savings by the selection of frequently taught courses and upgrading them through substantial redesign.29 If this approach is utilized widely, huge cost-savings are also expected.29
Pilot results from a MOOC introduced in Norway to promote clinical competency and decision-making development for health providers found the concept to be highly relevant and useful for the learners with a potential to enhance interprofessional collaboration.30 MOOC implementation at several colleges of pharmacy in the USA has diversified the models of learning with transformation and innovation in educational frameworks.31
MOOCs offer exciting opportunities to distribute knowledge on a massive and global scale to a diverse population of learners. Carefully selected and collaboratively designed MOOCs could be valuable resources for 1) unlimited access to continuing professional, and interprofessional education; 2) designing various research models to explore knowledge gaps through pre-assessment surveys and even; 3) delivering health promotion and disease awareness to the public.
MOOCs – limitations and solutions
Limitations
High number of dropouts and low completion rates
High numbers of dropouts and low average completion rates in spite of free content can be attributed to characteristics, such as non-engaging MOOC content, inadequate interactivity, low personal motivation, and course difficulty.27 As most of the MOOC content is created to be available at no cost to the learner, development costs are generally kept low.32 Hence, many courses are simply electronic pages, which achieve the tick-box requirements for CME credits or compliance.33,34 This simple “eReading” neither attracts learners’ attention nor fosters intense concentration, resulting in poor long-term knowledge retention.34
Content production and availability is expensive and generally available only in English
Production of more complex, engaging, and interactive MOOCs can be resource intensive. Teaching of advanced technologies for the prevention, detection, and treatment of diseases are often deployed only by developed countries.26 Hence, the popularity of health- and medicine-related MOOCs is limited to these nations.26 There are also constraints on the availability of experts to develop and supervise the courses and, more importantly, sponsors or funding sources to support development.28 English remains the dominant language in the provision of MOOCs.3,26 Making content available in local languages is key to wider reach.
Solutions
Improving participation and completion rates
Courses of shorter duration attract more viewers.33 However, the content needs to be carefully selected to ensure that all key points are covered in the shortest span. Incorporating media with the addition of good-quality audio, relevant images, videos, and animations provides an inspiring experience and makes e-learning much more interesting.34 Overall this will enhance the perceived value of any program and would be cost-effective, especially if it is utilized by large numbers of learners. Advertising the courses through multiple credible channels is important to ensure the benefits reach a large number of learners. Young family doctors associated with World Organization of Family Doctors from more than 20 countries recently completed a MOOC by Harvard University. The initiative included the use of various social media platforms to spread awareness and this improved the completion rate by fivefold.27 This demonstrates good practice to expand and augment CME reach within and outside organizations.
Strategic involvement of both commercial and non-commercial organizations as sponsors
Even in developed nations, CMEs cost many billions per year and only less than half of this revenue is contributed by the learners themselves.35 CME is largely supported by commercial sponsors, such as manufacturers of pharmaceuticals and medical devices, who contribute through unrestricted educational grants and other funding approaches to cover the costs of CME activities.35,36 In certain European countries and Canada, this accounts for about 75% of all CME provision.37,38 While some have voiced ethical concerns regarding commercial involvement in CMEs, industry will continue to play a critical role in helping organizations such as medical societies develop novel and innovative e-learning education and CMEs.39
The major drawback of MOOC CME is a viable economic model. The cost of producing and maintaining a MOOC has been increasing steadily.33 Universities can cover the costs and perhaps even gain revenue from their MOOCs by attracting students to fee-paying courses.33 This, however, is not possible for not-for-profit medical associations or societies. There is a continuing need for a collaborative model with contributions from both commercial and non-commercial sponsors.
Activities that are funded and conducted by commercial organizations can carry a high risk of being biased.4 Defining educational objectives in partnership with independent organizations, aligning the content with evidence-based data, obtaining endorsement from accreditation sources, and using an independent partner to co-ordinate the delivery of the program, can lead to credible industry-funded CME.15 Expert review of content by independent organizations would ensure that CME programs are not used for commercial promotion.38 Any organization that funds, develops, and approves the education content should adopt evidence-based, unbiased and practice-transforming information and techniques with equity and transparency. NAM also encourages collaborative partnerships, between professional and patient groups; physicians; health care organizations; and universities, to identify and include evidence- and best practice-based care processes when developing key preventive curricula for health risk behaviors; and the use of structures to measure and appraise any resulting improvement in health care.3
Proposed model for MOOC CME implementation
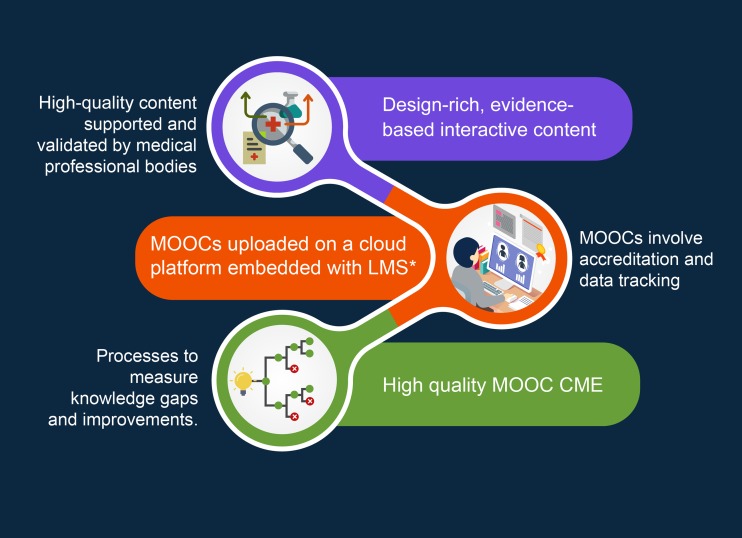
There is no doubt that CME delivery needs to evolve due to growing and variable educational needs of clinicians, and to benefit from technological innovations. Perhaps leadership of this reform should fall on specialty medical societies who are uniquely placed to deliver balanced, disease-oriented and patient-centered education;15 are agencies for the accreditation of learning; and are responsible for maintaining professional standards.40 Where possible, CME content needs to evolve from its largely face-to-face delivery to take advantage of the capability of MOOCs. Needs assessment is essential to generate a list of specific “hot topics” through surveying CME stakeholders.1 Multi-media MOOCs with case-based active and interactive education are likely to become the preferred option for most CMEs and can ensure wider reach and long-term sustainability (Figure 2).
Figure 2.
Proposed framework for MOOC implementation for CME.
Notes: *LMS is a platform that hosts and tracks data related to MOOCs, e.g., learner’s registration, knowledge assessment, certification, content management, and other “back-end” services. MOOCs can also run without LMS if they do not involve – tracking of learners’ data, e.g., for knowledge assessment or instructor’s interaction.
Abbreviations: MOOCs, massive open online courses; CME, continuing medical education; LMS, learning management system.
As MOOC CMEs would generally involve accreditation and tracking, they need to be delivered via a platform that has a learning management system (LMS) embedded within it.41 This would necessitate working with external enterprises (both for-profit and not-for-profit) to ensure their delivery systems can cope with very large number of learners. Institutions can and should host CME-accredited MOOCs on their world wide web presence. However, most medical society websites use older technology, especially in developing nations. This would preclude embedding an efficient LMS on their web presence. To overcome this challenge, MOOCs can be hosted by a dedicated, third-party technology service provider who would facilitate user registration, content management, pre-deployment testing and other “back-end” services including assessing learning gaps, training needs analysis and knowledge retention among learners (Figure 2). Medical society websites can seamlessly direct learners to relevant content on independently hosted LMS.
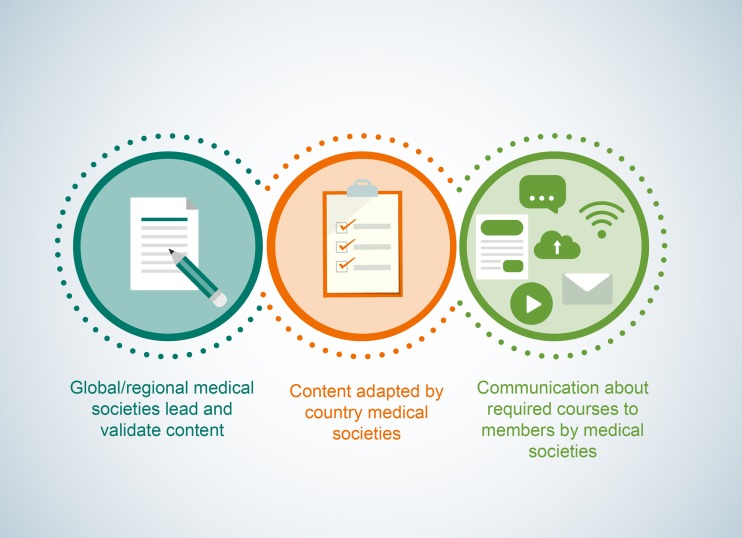
Global or regional medical societies, as recognized subject-matter experts, are ideally placed to lead and develop content. It would be highly cost-effective and efficient if that content could be simply adapted by national medical societies or associations. Figure 3 explains the possible roles of global, regional, and local medical societies in providing CME via MOOCs. In many situations, local medical societies may need to lead content generation and validation for example, for many country-specific needs and challenges. Nevertheless, they should always have the flexibility to adapt training curricula to meet unique needs within their territory. Design-rich, evidence-based, and interactive content should be actively communicated to their members after validation by professional bodies. As engaged learners are active learners, it is necessary for medical societies to ensure through regular and frequent communication with members on available learning modules, feedback and preference surveys, knowledge assessment results, etc. Regular communications are also a very powerful tool to boost member engagement and most of these can also be system generated or automated (Figure 3).
Figure 3.
Role of global, regional, and local medical societies in providing CME via MOOCs.
Notes: Highly cost-effective and efficient MOOCs can be generated if global or regional medical societies lead and develop content which can then be adapted by country medical associations. However, in many situations, local medical societies may also lead content generation and validation, for example, for many country-specific needs and challenges.
Abbreviations: MOOCs, massive open online courses; CME, continuing medical education.
Additionally, to replicate the value of face-to-face CME, the platform for MOOCs should have the functionality for learners to 1) raise questions; 2) share and discuss different practices, issues, and local data; and in the longer term, 3) connect and network with fellow learners and others, for research and other purposes.
Financial sustainability of CME via MOOC: unexplored areas
While the potential is unlimited, we need to be mindful that the evidence to support the value of MOOCs in CME is limited at present. Also, apart from a high establishment cost, the incorporation of an LMS platform (required for knowledge assessments, instructor interaction, etc.) and data tracking will incur annual maintenance costs. The long-term financial sustainability of MOOC CMEs in the context of their enduring availability over time and unlimited participation needs to be explored. A practical approach for long-term viability and sustainability is to ensure that sponsors commit for a defined period, at least for several years and to consider attracting sponsorships from multiple sources.
Conclusion
CME should strive to be needs-based, credible and accessible education, which is not only balanced and without bias, but also improves health care outcomes. MOOC-based CME is an interesting approach that holds a great potential to offer credible, cost-effective and readily accessible content to health providers, and meet their flexible schedules. Its implementation will however require careful planning and collaboration between CME makers, validators, and sponsors. Consumer and professional groups, health care organizations, medical societies, and clinicians need to work together to identify and create evidence-based MOOCs that are consistent with evidence-based best practices and to develop processes to measure improvements patient and health care.
Author contributions
All authors contributed to conception, acquisition and interpretation of data, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
Dr Sajita Setia is an executive director of Transform Medical Communications. Professor Jam Chin Tay is the current President of Singapore Hypertension Society and Professor Yook Chin Chia is the immediate past president of Malaysian Society of Hypertension. Dr Kannan Subramaniam is an employee of Pfizer. None of the authors have received any compensation for this manuscript. This publication contains personal views and opinions of authors and no inference should be derived related to their current or previous employers.
References
- 1.Stevenson R, Pozniak E. European CME needs the European specialist societies. J Eur CME. 2017;6(1):1319728. doi: 10.1080/21614083.2017.1319728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tham TY, Tran TL, Prueksaritanond S, Isidro JS, Setia S, Welluppillai V. Integrated health care systems in Asia: an urgent necessity. Clin Interv Aging. 2018;13:2527–2538. doi: 10.2147/CIA.S185048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg LR, Crocombe LA. Advances in medical education and practice: role of massive open online courses. Adv Med Edu Pract. 2017;8:603–609. doi: 10.2147/AMEP.S115321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.ESC Board. Relations between professional medical associations and the health-care industry, concerning scientific communication and continuing medical education: a Policy Statement from the European Society of Cardiology. Eur Heart J. 2012;33(5):666–74. doi: 10.1093/eurheartj/ehr480. [DOI] [PubMed] [Google Scholar]
- 5.Bloom BS. Effects of continuing medical education on improving physician clinical care and patient health: a review of systematic reviews. Int J Technol Assess Health Care. 2005;21(3):380–385. [DOI] [PubMed] [Google Scholar]
- 6.Ravyn D, Ravyn V, Lowney R, Ferraris V. Estimating health care cost savings from an educational intervention to prevent bleeding‐related complications: the outcomes impact analysis model. J Continuing Edu Health Prof. 2014;34(S1):S41–S46. doi: 10.1002/chp.21236 [DOI] [PubMed] [Google Scholar]
- 7.Cervero RM, Gaines JK. The impact of CME on physician performance and patient health outcomes: an updated synthesis of systematic reviews. J Continuing Edu Health Prof. 2015;35(2):131–138. doi: 10.1002/chp.21290 [DOI] [PubMed] [Google Scholar]
- 8.Nelson BA. Creating effective and efficient pediatric-specific CME content: more than just checking a box. J Contin Educ Health Prof. 2019. doi: 10.1097/CEH.0000000000000237 [DOI] [PubMed] [Google Scholar]
- 9.Davis DA, Thomson MA, Oxman AD, Haynes RB. Changing physician performance: a systematic review of the effect of continuing medical education strategies. JAMA. 1995;274(9):700–705. doi: 10.1001/jama.274.9.700 [DOI] [PubMed] [Google Scholar]
- 10.Miller SH, Thompson JN, Mazmanian PE, et al. Continuing medical education, professional development, and requirements for medical licensure: a white paper of the conjoint committee on continuing medical education. J Continuing Edu Health Prof. 2008;28(2):95–98. doi: 10.1002/chp.164 [DOI] [PubMed] [Google Scholar]
- 11.Collier R. Addressing bias in industry-funded CME. Can Med Assoc. 2014. doi: 10.1503/cmaj.109-4918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amin Z. Theory and practice in continuing medical education. Ann Acad Med Singapore. 2000;29(4):498–502. [PubMed] [Google Scholar]
- 13.Hawkes N. What price education? BMJ. 2008;337:a2333. doi: 10.1136/bmj.a2333 [DOI] [PubMed] [Google Scholar]
- 14.Kempen PM. Maintenance of Certification (MOC), Maintenance of Licensure (MOL), and Continuing Medical Education (CME): the regulatory capture of medicine. J Am Phys Surg. 2012;17:P72–P75. [Google Scholar]
- 15.ESC Board. The future of continuing medical education: the roles of medical professional societies and the health care industry. Eur Heart J. 2019. 1;40(21):1720–1727. doi: 10.1093/eurheartj/ehy003 [DOI] [PubMed] [Google Scholar]
- 16.Hemmer NM. Flying for CME—a big carbon footprint. Wilderness Environ Med. 2015;26(1):107–108. doi: 10.1016/j.wem.2014.08.003 [DOI] [PubMed] [Google Scholar]
- 17.Walsh K. Self-directed continuing medical education at the point-of-care: implications for cost and value. Annali dell’Istituto Superiore Di Sanita. 2018;54(1):67–71. doi: 10.4415/ANN_18_01_13 [DOI] [PubMed] [Google Scholar]
- 18.Liyanagunawardena TR, Aboshady OA. Massive open online courses: a resource for health education in developing countries. Glob Health Promot. 2018;25(3):74–76. doi: 10.1177/1757975916680970 [DOI] [PubMed] [Google Scholar]
- 19.Ali SA, ul Fawwad SH, Ahmed G, Naz S, SA Waqar, Hareem A. Continuing medical education: a cross sectional study on a developing country’s perspective. Sci Eng Ethics. 2018;24(1):251–260. doi: 10.1007/s11948-017-9900-8 [DOI] [PubMed] [Google Scholar]
- 20.Williams JG. Are online learning modules an effective way to deliver hand trauma management continuing medical education to emergency physicians? Plast Surg. 2014;22(2):75–78. [PMC free article] [PubMed] [Google Scholar]
- 21.Vollmar HC, Schürer-Maly CC, Frahne J, Lelgemann M, Butzlaff M. An E-learning platform for guideline implementation. Methods Inf Med. 2006;45(04):389–396. [PubMed] [Google Scholar]
- 22.Thepwongsa I, Kirby C, Schattner P, Piterman L. Online continuing medical education (CME) for GPs: does it work?: a systematic review. Aust Fam Physician. 2014;43(10):717. [PubMed] [Google Scholar]
- 23.Wiecha J, Heyden R, Sternthal E, Merialdi M. Learning in a virtual world: experience with using second life for medical education. J Med Internet Res. 2010;12(1). doi: 10.2196/jmir.1587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shang F, Liu C-Y. Blended learning in medical physiology improves nursing students’ study efficiency. Adv Physiol Educ. 2018;42(4):711–717. doi: 10.1152/advan.00021.2018 [DOI] [PubMed] [Google Scholar]
- 25.Sissine M, Segan R, Taylor M, et al. Cost comparison model: blended eLearning versus traditional training of community health workers. Online J Public Health Inform. 2014;6(3). doi: 10.5210/ojphi.v6i3.5533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liyanagunawardena TR, Williams SA. Massive open online courses on health and medicine. J Med Internet Res. 2014;16(8). doi: 10.2196/jmir.3439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoedebecke K, Mahmoud M, Yakubu K, et al. Collaborative global health E-learning: a massive open online course experience of young family doctors. J Family Med Prim Care. 2018;7(5):884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hoy MB. MOOCs 101: an introduction to massive open online courses. Med Ref Serv Q. 2014;33(1):85–91. doi: 10.1080/02763869.2014.866490 [DOI] [PubMed] [Google Scholar]
- 29.Ruth S. Can MOOCs help reduce college tuition?: MOOCs and technology to advance learning and learning research (Ubiquity symposium). Ubiquity. 2014;3:1530–2180. [Google Scholar]
- 30.Lunde L, Moen A, Rosvold EO. Learning clinical assessment and interdisciplinary team collaboration in primary care. MOOC for healthcare practitioners and students. Stud Health Technol Inform. 2018;250:68. [PubMed] [Google Scholar]
- 31.Maxwell WD, Fabel PH, Diaz V, et al. Massive open online courses in US healthcare education: practical considerations and lessons learned from implementation. Curr Pharm Teach Learn. 2018;10(6):736–743. doi: 10.1016/j.cptl.2018.03.013 [DOI] [PubMed] [Google Scholar]
- 32.Using MOOCs to transform traditional training; 2014. Available from: www.towardsmaturity.org/in-focus/MOOC2014 Accessed February26, 2019
- 33.Daniel J. Massive open online courses: what will be their legacy? FEMS Microbiol Lett. 2016;363(8). doi: 10.1093/femsle/fnw055 [DOI] [PubMed] [Google Scholar]
- 34.In-Focus: Lessons from MOOCs for Corporate Learning; 2014. Available from: https://towardsmaturity.org/2014/05/12/in-focus-lessons-from-moocs-for-corporate-learning-2014/ Accessed February26 , 2019.
- 35.Morris L, Taitsman JK. The agenda for continuing medical education–limiting industry’s influence. N Engl J Med. 2009;361(25):2478. doi: 10.1056/NEJMsb0905411 [DOI] [PubMed] [Google Scholar]
- 36.Setia S, Ryan NJ, Nair PS, Ching E, Subramaniam K. Evolving role of pharmaceutical physicians in medical evidence and education. Adv Med Edu Pract. 2018;9:777. doi: 10.2147/AMEP.S175683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ahmed K, Wang TT, Ashrafian H, Layer GT, Darzi A, Athanasiou T. The effectiveness of continuing medical education for specialist recertification. Can Urol Assoc J. 2013;7(7–8):266. doi: 10.5489/cuaj.378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Marlow B. Rebuttal: Is CME a drug-promotion tool?: NO. Can Family Physician. 2007;53(11):1877. [PMC free article] [PubMed] [Google Scholar]
- 39.Wieting MW, Mevis H, Zuckerman JD. The role of industry in internet education. Clin Orthop Relat Res. 2003;412:28–32. doi: 10.1097/01.blo.0000074406.99625.2e [DOI] [PubMed] [Google Scholar]
- 40.Abrahamson S, Baron J, Elstein AS, et al. Continuing medical education for life: eight principles. Acad Med. 1999;74(12):1288–1294. doi: 10.1097/00001888-199912000-00008 [DOI] [PubMed] [Google Scholar]
- 41.Nielson B. What’s the difference between a MOOC and an LMS? CapitalWave Inc; 2015. Available from: https://www.yourtrainingedge.com/whats-the-difference-between-a-mooc-and-an-lms/ Accessed February 26, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Using MOOCs to transform traditional training; 2014. Available from: www.towardsmaturity.org/in-focus/MOOC2014 Accessed February26, 2019