Supplemental Digital Content is available in the text.
Keywords: advanced practice provider, critical care, intensive care unit, nurse practitioner, outcomes, physician assistant
Objectives:
To provide a concise review of the literature and data pertaining to the use of nurse practitioners and physician assistants, collectively called advanced practice providers, in ICU and acute care settings.
Data Sources:
Detailed search strategy using the databases PubMed, Ovid MEDLINE, and the Cumulative Index of Nursing and Allied Health Literature for the time period from January 2008 to December 2018.
Study Selection:
Studies addressing nurse practitioner, physician assistant, or advanced practice provider care in the ICU or acute care setting.
Data Extraction:
Relevant studies were reviewed, and the following aspects of each study were identified, abstracted, and analyzed: study population, study design, study aims, methods, results, and relevant implications for critical care practice.
Data Synthesis:
Five systematic reviews, four literature reviews, and 44 individual studies were identified, reviewed, and critiqued. Of the research studies, the majority were retrospective with others being observational, quasi-experimental, or quality improvement, along with two randomized control trials. Overall, the studies assessed a variety of effects of advanced practice provider care, including on length of stay, mortality, and quality-related metrics, with a majority demonstrating similar or improved patient care outcomes.
Conclusions:
Over the past 10 years, the number of studies assessing the impact of advanced practice providers in acute and critical care settings continue to increase. Collectively, these studies identify the value of advanced practice providers in patient care management, continuity of care, improved quality and safety metrics, patient and staff satisfaction, and on new areas of focus including enhanced educational experience of residents and fellows.
Each year, 6 million patients are admitted to ICUs across the United States (1). These patients have complex care requirements, high acuity levels, and often, concurrent comorbidities that compound their clinical care management needs. However, national projections for the healthcare workforce identify that a number of factors will continue to lead to a shortage of physicians, especially intensivists, to manage the growing number of critically ill patients (2, 3). A recent Society of Critical Care Medicine Academic Leaders in Critical Care Medicine taskforce identified that the increasing number of patients with complex, life-threatening diseases, combined with the varied concentration of ICU beds in few centralized hospitals, growth of specialty ICU services, and desire for full time around the clock availability, have contributed to growing intensivist staffing concerns (4).
The use of nurse practitioners (NPs) and physician assistants (PAs) in the ICU is an established model of care for providing care for acute and critically ill patients. Collectively termed advanced practice providers (APPs), the integration of NPs and PAs as part of the medical team in acute, emergent, and intensive care has grown significantly, due in part to increasing numbers of complex care patients, changing work hour restrictions of medical residents, and increasing availability of APP practitioners (4–6). Since the original recognition of the role of APPs in the management of critically ill patients by the LeapFrog Group in 2000 when recommendations for ICU physician staffing were specified, their guidelines have continued to identify APPs as an acknowledged provider in critical care (7). Additionally, a number of workforce documents have identified that integrating APPs is one solution to meeting staffing needs in the ICU (5, 6, 8–10).
Nationally, of the 270,000 NPs, over 20,000 are certified as adult or pediatric acute care providers with 28% working in hospital settings, 5.8% working in emergency department (ED) or urgent care settings, and 12% working in critical care (11). Of the 123,000 PAs nationally, almost 38.5% report that a hospital is their primary practice setting (12), and recent estimates are that 1.4% (1,371) work in critical care (13). Although the APP role is recognized in many countries, no data exists on the specific number practicing internationally. Information on models of care that integrate NPs and PAs in acute and critical care settings and their outcomes of care is essential in order to adequately plan optimal workforce strategies to meet the needs of acute and critically ill patients.
An evidence-based review published in 2008 identified that of 145 articles related to the use of APPs, the majority focused on role development, education and training, scope of practice, and role expansion (14). At that time, 31 studies (and no systematic reviews) were available which had explored various aspects of integrating APPs into ICU and acute care teams to assist with patient care management, reinforce practice guidelines, educate patients, families and ICU staff; and assist with research and quality improvement initiatives (14).
In order to evaluate the change in type of APP models of care and the impact of these roles in the ICU and acute care settings in the past 10 years, a concise literature review was conducted of studies published from January 2008 to December 2018.
MATERIALS AND METHODS
A detailed search strategy was developed and revised using the databases PubMed, Ovid MEDLINE, and the Cumulative Index of Nursing and Allied Health Literature for the time period from January 2008 to December 2018. The search strategy combinations of key terms for inclusion and exclusion criteria are outlined in the supplemental content (Supplemental Digital Content 1, http://links.lww.com/CCM/E743). Each of the articles retrieved was assessed for relevance by reading the abstract (and where necessary the entire paper) using the inclusion and exclusion criteria to exclude those papers that were not relevant to this review.
Search limits included the regions of the United States, Canada, Australia, United Kingdom, and Europe, of English language publications. A medical librarian was used to assist with the conduct of the literature review. The obtained literature was then reviewed by the authors, who are practicing APPs, and the following aspects of each study were identified, abstracted, and analyzed: study population, study design, study aims, methods, and results, and relevant implications for acute and critical care practice were summarized.
RESULTS
One systematic review of 18 studies of APPs in acute care (15), a systematic review of 15 studies of advanced practice nursing roles in emergency and critical care settings (16), a systematic review of 29 studies of APP care on surgical services (17), a systematic review of 14 studies of NP impact on cost, quality of care, satisfaction and wait times in ED settings (18), a literature review of 47 studies on NP care on critical care services (19), a narrative review of 29 studies related to PA satisfaction (20), a literature review of 12 studies on NP use and intensivist staffing (21), a literature review of five studies focused on APP care for ICU patients (22), a systematic review of 30 studies on the impact of APP care for adult critical care patients with a meta-analysis of eight studies (23), and 44 individual studies were identified. The studies addressed a variety of APP models of care including 24/7 ICU coverage (24), and specialty practice roles including cardiovascular surgery (25–28), neuroscience (29, 30), trauma care (31–39), pediatric critical care (40–44), oncology care (45, 46), surgical services (17, 47), ED settings (16, 19), orthopedics (48), stroke care (30), heart failure care (49), burn care (15), aneurysmal subarachnoid hemorrhage care (50), and palliative care (51), among other areas of specialty care. Other practice models included APP led rapid response teams (52–54), critical care outreach service (55, 56), nocturnist care (50), interventionalist service (for central venous catheter placement) (57), and sepsis care team (58).
Of the 44 research studies, 27 were retrospective, three were pre-post comparisons, three were prospective, two used a comparative design, two were observational, one was a cross-sectional descriptive survey, one was a secondary analysis, one was a quasi-experimental study, two were randomized studies, and two were quality improvement initiatives. Online Supplemental Table 1 (Supplemental Digital Content 1, http://links.lww.com/CCM/E743) provides a detailed outline of the most recent studies, and a comprehensive table is found in the supplemental content (Supplemental Digital Content 1, http://links.lww.com/CCM/E743). The majority of the studies used a retrospective design and focused on comparing APP care to resident or physician care; common APP patient care interventions; impact on patient care quality metrics including urinary tract infection (UTI) rates, deep vein thrombosis (DVT) prophylaxis, surgical site infection, post hospital discharge destination, or ED return rates; APP procedural skills; patient or staff satisfaction; and impact on physician workload related to APP care. For example, one study randomized 103 cardiac surgery patients to receive either acute care NP-led or hospitalist-led postoperative care. More patients in the acute care nurse practitioner (ACNP)-led group had surgery on an urgent basis (p ≤ 0.01) and had undergone more complicated surgical procedures (p ≤ 0.01) (28). After discharge, more patients in the hospitalist-led group had visited their family doctor within a week (p ≤ 0.02). Measures of satisfaction relating to teaching, answering questions, listening, and pain management were higher in the ACNP-led group (28). Another study randomized 200 elective cardiac surgery patients to NP-led post discharge follow-up care (n = 95) compared with a standard model of follow-up care (n = 105) (25). The intervention group received a telephone follow-up needs assessment by the NP approximately 3 days postdischarge; patients with significant issues/concerns were seen in the NP follow-up clinic. At 2 weeks postdischarge, the intervention group reported significantly fewer symptoms (p = 0.002) and higher physical functioning status (p = 0.04). At 2 and 6 weeks postdischarge, the intervention group was significantly more satisfied with the amount of help (p = 0.001), as well as the quality of the services received (p = 0.003). Differences in healthcare resource use were not statistically significant (25).
Comparison of APP Care to Medical Providers
A number of studies compared APP care to resident and/or fellows or house staff (24, 25, 27, 28, 30, 32, 34, 42, 45, 59–66), and demonstrated similar outcomes. Several of these studies also identified significant differences in aspects of care provided by APPs including decreased length of stay (LOS) (24, 31, 32, 39, 45), improved physician and nursing satisfaction (28, 31, 53), higher rates of discharge destinations to home (32), decreased ED time to transfer to ICU (55), decreased costs of care related to laboratory test use (67), decreased 14 day readmission rates (45), increased discharges by noon (39), decreased costs of care for heart failure patients (49), and indirect economic and patient care impacts such as increasing ED throughput, decreasing time to the operating room, operative time, and decreasing complications (48).
A number of outcome metrics were used in the studies to identify impact of the APP role, including changes in LOS, time to transfer, readmission rates, discharge disposition, mortality, mechanical ventilation rates, resource use, costs of care, procedural quality indicators, transfer rate, resource use, patient satisfaction, guideline compliance, and others. These are outlined in Supplemental Table 2 (Supplemental Digital Content 1, http://links.lww.com/CCM/E743). The majority of studies assessed APP impact on traditional outcome measures including LOS, readmission rates, DVT prophylaxis rates, or mechanical ventilation rates, whereas other studies have included patient care specific outcomes including discharge time; blood transfusion rates; patient, family and staff perceptions; as well as resource use; financial impact; and impact on hand over communication.
ICU Patient Care Management
The impact of APPs on direct patient care management has been assessed with a number of outcome measures including LOS, mortality rates, readmission rates, post hospital discharge disposition, costs of care, time-savings for physicians, rate of infections, and quality of care metrics such as DVT and stress ulcer disease prophylaxis, and patient care metrics such as time on mechanical ventilation (24, 25, 27, 31–36, 40, 45, 48, 53, 55, 60, 62–64, 68–72). These studies demonstrate similar or improved patient care outcomes.
Several studies have included assessments of patient, clinical staff, and family satisfaction with APP care; however, they are limited in scope. In a study of 103 cardiac surgery patients managed by NPs and hospitalists, NPs were rated to perform better at teaching, answering questions, and listening (28). In a single-center study focused on assessing the impact of NP care on a trauma service, physician satisfaction with NP care was rated high, with 76.9% strongly agreeing that the ACNP improved their workflow, 83.3 strongly agreeing that patient care was improved and 100% strongly agreeing that adding NPs to the multidisciplinary team helped throughput (31). Similarly, 96% of staff nurses felt that patients and families were better informed of the plan of care, and 100% felt that ACNP care improved patient care overall (31). In a study evaluating the impact of adding PAs to the trauma care team at a level I trauma setting, no differences in mortality or mean ICU LOS were found, while mean unadjusted hospital length of stay was found to be lower for 2,333 patients over a 1-year period (36).
APP Staffing Models
Several studies have evaluated the impact of different APP staffing models such as nocturnist, weekend coverage, or 24/7 coverage. In a prospective cohort study comparison of 90-day survival between NP and resident teams in a medical ICU, Landsperger et al (24) found no difference in 90-day survival for patients cared for by NP or resident teams over a 3-year period involving 9,066 admissions. Critical care fellows and attending physicians rounded with each team twice a day, were onsite most of each day, and were available for night consultation. Although patients cared for by the NP teams had lower ICU mortality (6.3%) than resident team patients (11.6%), hospital mortality was not different. ICU LOS was similar between the NP and resident teams while hospital LOS was shorter for patients cared for by NPs (7.9 d) than for resident patients (9.1 d) (p = 0.001) (24).
In a review of night coverage by APPs for 289 patients over an 8-month period in a trauma ICU, no differences were found between APP coverage 7pm to 7am Sunday to Wednesday compared with resident physician coverage Thursday to Saturday on a number of outcomes (34). Both teams were supervised by an on-call trauma fellow and attending surgeon in house. In a multiple logistic regression analysis, APP care was not associated with any clinical outcome differences including mortality, LOS, or ventilator days. Given the fact that APP coverage varies significantly from day shift coverage, night shift coverage, weekend coverage, and 24/7 models of care (73), additional research is needed to identify optimal models of care and associated return on investment, including the value of 24/7 models of care and cost effectiveness of having APP staffing 24 hours a day.
Quality Improvement, Patient Safety, and Financial Impact
Over the past 10 years, a number of studies have highlighted the role that the APP brings in improving quality of care, enhancing patient safety, and providing continuity of care. These studies have identified the impact of APP care on reducing UTI rates, increasing DVT prophylaxis rates, and early identification of patients with sepsis, among others (33, 37, 48, 58). A limited number of studies have assessed costs of care related to APP care. In a retrospective secondary analysis of return on investment after adding NPs to four ICU teams, the cardiovascular ICU’s NP’s gross collections exceeded the salary and fringe expenses for a positive margin of 32% (72). One study assessing the outcomes of an NP-led rapid response team demonstrated that NP-led calls generated a critical care billable note in 30% of cases whereas previously no billing occurred (54). The addition of PAs to a critical care outreach team was found to result in reduction in the time to transfer to ICU (55). A cost-effective analysis of an NP-led heart failure service demonstrated a reduction in costs per visit and costs per consumer (49). In another study, resource utilization of an NP-staffed ICU compared with a resident-staffed ICU, both with intensivist-led care, demonstrated no differences (70). A single-center study of NP care conducted in the United Kingdom demonstrated a reduction in staffing costs with an NP-intensivist collaborative care model (74). These study examples showcase the impact of APP care on additional areas of care with respect to quality improvement, patient safety, and costs of care.
An evaluation of the impact of adding PAs to an orthopedic trauma service found that patients were seen in the ED 205 minutes faster (p = 0.006), total ED time decreased by 175 minutes (p = 0.001), time to surgery improved by 360 minutes (p < 0.03), postoperative DVT prophylaxis increased by a mean of 6.73% (p = 0.03), and average LOS decreased by 0.61 days (p = 0.276) (48).
Impact on Resident and Fellow Education
The impact of APPs on resident and fellow education represents a new area of focus that has developed in the past 10 years. Several studies have examined the impact of APP utilization and the perceptions of critical care physicians, residents, and fellows (9, 42, 75–79). In a cross-sectional national survey to program directors of 331 adult Accreditation Council for Graduate Medical Education-approved critical care fellowship training programs in U.S. academic medical centers, Joffe et al (9) found that 65% of respondents (n = 134; 37.5% response rate) identified that APPs were part of the care team in the ICU. The majority reported that patient care was positively affected by APP care, and nearly two-thirds of program directors reported that fellowship training was also positively impacted. Sixty-two percent identified that APPs aided in fellow training, 72% identified that APPs participate in didactic discussions during rounds/conferences, and 35% reported that APPs participate in ICU-related research activities. Fifty-four percent identified that APPs perform procedures traditionally done by fellows (9).
A cross-sectional descriptive survey 1 year after introduction of pediatric NPs to a pediatric neurosurgery group assessed physician, nurse, and allied staff perceptions of satisfaction with availability, responsiveness, and patient clinical satisfaction (42). Satisfaction scores in all categories, including overall satisfaction, significantly improved (p = 0.001). The number of paging calls received by the residents was reduced (91% were managed independently by NP) and there were no sentinel event reports noted. The majority (84.8% of 66 residents) agreed that the NPs on the service reduced their daily workload and provided continuity of care (42).
In a study assessing the impact of APPs on 354 surgical resident’s critical care experience, Kahn et al (76) found that residents identified benefits to working with APPs. A total of 79.8% reported a reduced resident workload, 51.6% identified enhance continuity of care, 49.8% reported APPs fill resident shift work and cross coverage gaps, 50.5% identified that APPs enhance communication with families and patients, and 48.4% related that APPs enhance communication with other providers. Additionally, 60.3% reported that APPs teach ICU protocols and guidelines to residents, and 60.3% identified that APPs enhance patient care (Fig. 1) (76).
Figure 1.
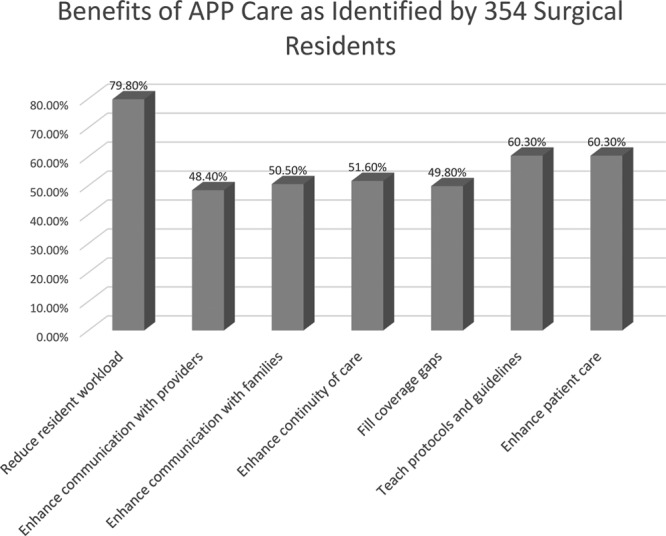
Surgical residents perceptions of benefits of working with advanced practice providers (APPs). Source: Kahn et al (76).
Similarly, a study of 66 surgical residents found that 84.4% identified that APPs decrease resident workload, 75.8% identified that APPs contribute to resident education, and 60.6% reported that APPs help to provide better continuity of care (77). Additionally, Skinner et al (78) evaluated the impact of NP care on surgical trainees experience, finding that time in the operating room increased from 68% to 80% (p < 0.001), and that for 57% of the after-hour calls by NPs, advice sufficed to meet the clinical care situation.
Recently, the Association of Surgeons in Training outlined consensus recommendations on the use of the nonmedical workforce, including APPs (75). Using a survey of trainees attitudes and experiences from a sample of 112 medical students to senior level trainees in the United Kingdom where the APP role is not as developed as in the United States, respondents agreed that APPs could improve service delivery (72%) and patient care (58%). There was a trend toward trainees feeling that APPs took away training opportunities away from them (65%), although it was also felt that APPs could support trainees on the wards (74%), in clinic (59%), and less so in the theater setting (48%), or assessing acute admissions (47%) (75).
Just under half of respondents (46%) thought that APPs could enhance surgical training. A similar proportion reported that they would be happy for APPs to look after their relatives (47%), and suggested there should be more APPs (46%). Over half (54%) of respondents stated that they would like to work with APPs as consultants (75). Based on the results of this study, an overarching primary objective was identified that the APP position should be further developed in such a way that their roles are accepted, understood, and beneficial to patients.
DISCUSSION
In the past 10 years, collectively over 150 studies have been conducted on an aspect of APP care in acute, critical care, and emergency care settings. Compared to studies on APPs that were available for review in a 2008 concise literature review (14) which focused predominantly on ICU settings, the number of studies addressing APP roles in acute, trauma, and ED settings has increased, possibly reflecting the expansion of the acute care APP role beyond the walls of the ICU. Overall, the studies demonstrate impact of the APP role through improved patient flow and clinical outcomes including reducing complications and improved patient care management with reduced time on mechanical ventilation, increased use of clinical practice guidelines, improved laboratory test use, and increased palliative care consultations, among other areas of impact. Studies also demonstrate positive financial outcomes with reduced ICU LOS, hospital LOS, (re)admission rates, and improved discharge time among others (16–19, 24, 28, 31–35, 37, 45, 48, 50, 51, 55, 60–66, 72, 75).
Studies have demonstrated that in the ICU setting (24, 32, 51, 60, 62, 63–66, 79), as well as in acute care settings such as the ED (16), and specialty care settings such as surgery (17), and burn care (15), among others, the involvement of APPs in managing patients allows for greater continuity of care as APPs do not have to be on frequent rotation coverage such as that of residents and fellows (16). The involvement of APPs also provides unit-based clinical staff with a consistent point of contact for the multidisciplinary team (27). The institution of daily multidisciplinary rounds by APPs has been demonstrated to improve care coordination including discharge planning, post ICU discharge follow-up, and cross-disciplinary communication (32).
The impact of specific APP models of care including 24/7 coverage in the ICU, nocturnist coverage, APP led rapid response teams utilizing intensivist presence via telehealth (53), or formation of ICU alert teams to manage patients held in the ED prior to ICU transfer (80), need to be further explored. Limited information is available on the differences in impact based on APP staffing models, as well as the type and degree of physician consultation and oversight.
Although several studies have focused on the impact of APPs on resident and fellow education and training, demonstrating enhance training and ICU experience, others have found varied understanding of the role (9, 42, 75–78, 81).
Additional studies assessing the financial impact as well as the “value-added” aspect of the APP role are needed. Only one study was found that has assessed APP career satisfaction in the role (20). This information is crucial to ensuring APP professional role satisfaction and maximizing retention rates.
A number of studies have been reported in over 20 published abstracts from presentations at critical care conferences (supplemental content, Supplemental Digital Content 1, http://links.lww.com/CCM/E743). These studies report on new roles such as APP staffed mobile stroke teams (82), the impact of NP-led care for acute ischemic stroke care in reducing costs and decreasing LOS (83), and the impact of APP care in reducing trauma readmissions (84), among others. Although this source of information is useful, extending abstract reports into published manuscripts is most beneficial in ensuring wide-scale dissemination of efforts to assess APP outcomes of care.
LIMITATIONS
Although a number of studies examining impact of APP roles in the ICU exist, a significant limitation is the lack of information related to the specific model of care employed. Few studies describe the APP coverage of the unit—whether it was weekday, weekend only, 24/7 coverage, or another modified staffing coverage of APPs. The description of the specific roles of APPs with respect to patient care was also lacking in many studies. Although a comprehensive search strategy was used, this concise review included only papers in English, and as such, other relevant studies published in other languages, if any exist, were not included.
CONCLUSIONS
A growing number of studies continue to demonstrate the impact of APPs in acute and critical care settings (16–24, 83). Collectively, these studies identify the value of APPs in patient care management, continuity of care, decreasing costs of care, decreasing resource use, improving quality and safety metrics, patient and staff satisfaction, and enhancing educational experiences of residents and fellows. It is evident from this review that collectively, NPs and PAs are essential members of the ICU and acute care teams who can assist in patient care management as well as promote implementation of evidence-based practice and continuity of care.
Studies are needed which demonstrate the unique role and value that APPs bring to patient care, not as a physician replacement model, but rather an advanced practice model of care. It is evident from this review that sufficient comparison studies of APP and physician care exist. Future studies to develop roles and expectations of an APP beyond medical management are needed. Outcome measures should focus on the impact of APPs to reduce cost and improve efficiencies, improve quality and safety outcomes, improve patient access and outcomes, and finally, improve fulfillment and well-being of all members of the interprofessional. Until acute care and critical care APP team roles, expectations, and privileges are more standardized (nationally or state determined), the true benefit and value of APPs will remain unknown. Assessing impact in areas such as patient and family satisfaction, staff nurse retention, as well as those related to expanding roles such as ICU outreach and rapid response team roles on outcomes such as unplanned ICU readmission rates, can provide additional information on APP impact. The impact of specialty roles on other outcomes such as patient discharge destination; increasing patient throughput; improving guideline-based care; or contributing to high-value care by decreasing unnecessary laboratory, diagnostic, or antibiotic duration, for example, may also provide additional information on outcomes more reflective of the comprehensive care nature of the APP role. Additional information is also needed on the impact of various models of APP care and whether coverage models such as nocturnist, 24/7 coverage, or specialty based models of care produce optimal outcomes for acute and critically ill patients.
It is evident from this review that in the last 10 years, a significant number of studies as well as synthesis reviews have been conducted which have examined the impact of APP care for acute and critically ill patients. As APP roles continue to evolve, evaluating specific aspects such as promoting continuity of care, impact on patient and family-centered care, effect on nursing staff job satisfaction and retention rates, impact on physician workload and satisfaction, and the role of APPs in enhancing the professional environment in acute and critical care settings remain needed.
Supplementary Material
Footnotes
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal’s website (http://journals.lww.com/ccmjournal).
Dr. Kleinpell received funding from the Society of Critical Care Medicine (SCCM) (past 2017 president). Dr. Constantine disclosed that he was on the Board of the Council of Surgical and Perioperative Safety and chaired the safety committee for the Surgery Section of the SCCM and the SCCM Advanced Practice Provider Resource Committee. The remaining authors have disclosed that they do not have any potential conflicts of interest.
REFERENCES
- 1.Halpern NA, Goldman DA, Tan KS, et al. Trends in critical care beds and use among population groups and Medicare and Medicaid beneficiaries in the United States: 2000-2010. Crit Care Med 2016; 44:1490–1499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Center for Health Workforce Analysis: Health Workforce Projections: Critical Care Physicians and Nurse Practitioners. Available at: https://bhw.hrsa.gov/sites/default/files/bhw/health-workforce-analysis/research/projections/critical-care-fact-sheet.pdf. Accessed August 25, 2018
- 3.American Association of Medical Colleges: 2018 Update: The Complexities of Physician Supply and Demand: Projections From 2016 to 2030. 2018. Washington, DC, American Association of Medical Colleges; Available at: https://www.accenture.com/_acnmedia/PDF-95/Accenture-Aamc-2018-Workforce-Rrojections-Update-April-11-2018.pdf Accessed September 9, 2018 [Google Scholar]
- 4.Pastores SM, Kvetan V, Coopersmith CM, et al. ; Academic Leaders in Critical Care Medicine (ALCCM) Task Force of the Society of the Critical Care Medicine: Workforce, workload, and burnout among intensivists and advanced practice providers: A narrative review. Crit Care Med 2019; 47:550–557 [DOI] [PubMed] [Google Scholar]
- 5.Pastores SM, Halpern NA, Oropello JM, et al. Critical care organizations in academic medical centers in North America: A descriptive report. Crit Care Med 2015; 43:2239–2244 [DOI] [PubMed] [Google Scholar]
- 6.Ward NS, Afessa B, Kleinpell R, et al. ; Members of Society of Critical Care Medicine Taskforce on ICU Staffing: Intensivist/patient ratios in closed ICUs: A statement from the Society of Critical Care Medicine Taskforce on ICU staffing. Crit Care Med 2013; 41:638–645 [DOI] [PubMed] [Google Scholar]
- 7.The Leapfrog Group: ICU Physician Staffing 2018. Available at: https://www.leapfroggroup.org/sites/default/files/Files/2018%20IPS%20Fact%20Sheet.pdf. Accessed November 20, 2018
- 8.Kerlin MP, Adhikari NK, Rose L, et al. ; ATS Ad Hoc Committee on ICU Organization: An Official American Thoracic Society Systematic Review: The effect of nighttime intensivist staffing on mortality and length of stay among intensive care unit patients. Am J Respir Crit Care Med 2017; 195:383–393 [DOI] [PubMed] [Google Scholar]
- 9.Joffe AM, Pastores SM, Maerz LL, et al. Utilization and impact on fellowship training of non-physician advanced practice providers in intensive care units of academic medical centers: A survey of critical care program directors. J Crit Care 2014; 29:112–115 [DOI] [PubMed] [Google Scholar]
- 10.Ward NS, Chong DH. Critical care beds and resource utilization: Current trends and controversies. Semin Respir Crit Care Med 2015; 36:914–920 [DOI] [PubMed] [Google Scholar]
- 11.Kleinpell R, Cook ML, Padden DL. American Association of Nurse Practitioners National Nurse Practitioner sample survey: Update on acute care nurse practitioner practice. J Am Assoc Nurse Pract 2018; 30:140–149 [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Physician Assistants: 2018 AAPA Salary Report. 2018. Available at: https://www.aapa.org/shop/salary-report/. Accessed November 1, 2018
- 13.National Commission on Certification of Physician Assistants: 2017 Statistical Profile of Certified Physician Assistants: An Annual Report of the National Commission on Certification of Physician Assistants. 2018. Available at: http://www.nccpa.net/research. Accessed September 9, 2018
- 14.Kleinpell RM, Ely EW, Grabenkort R. Nurse practitioners and physician assistants in the intensive care unit: An evidence-based review. Crit Care Med 2008; 36:2888–2897 [DOI] [PubMed] [Google Scholar]
- 15.Edkins RE, Cairns BA, Hultman CS. A systematic review of advance practice providers in acute care: Options for a new model in a burn intensive care unit. Ann Plast Surg 2014; 72:285–288 [DOI] [PubMed] [Google Scholar]
- 16.Woo BFY, Lee JXY, Tam WWS. The impact of the advanced practice nursing role on quality of care, clinical outcomes, patient satisfaction, and cost in the emergency and critical care settings: A systematic review. Hum Resour Health 2017; 15:63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johal J, Dodd A. Physician extenders on surgical services: A systematic review. Can J Surg 2017; 60:172–178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jennings N, Clifford S, Fox AR, et al. The impact of nurse practitioner services on cost, quality of care, satisfaction and waiting times in the emergency department: A systematic review. Int J Nurs Stud 2015; 52:421–435 [DOI] [PubMed] [Google Scholar]
- 19.Fry M. Literature review of the impact of nurse practitioners in critical care services. Nurs Crit Care 2011; 16:58–66 [DOI] [PubMed] [Google Scholar]
- 20.Hooker RS, Kuilman L, Everett CM. Physician assistant job satisfaction: A narrative review of empirical research. J Physician Assist Educ 2015; 26:176–186 [DOI] [PubMed] [Google Scholar]
- 21.White T, Kokiousis J, Ensminger S, et al. Supplementing intensivist staffing with nurse practitioners: Literature review. AACN Adv Crit Care 2017; 28:111–123 [DOI] [PubMed] [Google Scholar]
- 22.Medeiros RS, NeSmith EG, Heath JA, et al. Midlevel health providers impact on ICU length of stay, patient satisfaction, mortality, and resource utilization. J Trauma Nurs 2011; 18:149–154 [Google Scholar]
- 23.Kreeftenberg HG, Pouwels S, Bindels AJ, et al. Impact of the advanced practice provider in adult critical care: A systematic review and meta-analysis. Crit Care Med 2019; 47:722–730 [DOI] [PubMed] [Google Scholar]
- 24.Landsperger JS, Semler MW, Wang L, et al. Outcomes of nurse practitioner-delivered critical care: A prospective cohort study. Chest 2016; 149:1146–1154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sawatzky JA, Christie S, Singal RK. Exploring outcomes of a nurse practitioner-managed cardiac surgery follow-up intervention: A randomized trial. J Adv Nurs 2013; 69:2076–2087 [DOI] [PubMed] [Google Scholar]
- 26.Devlin MC, Holcomb E, Kern M. Cardiothoracic intensive care: An emerging setting for NP practice. Adv Nurse Pract 2010; 18:41–42 [PubMed] [Google Scholar]
- 27.David D, Britting L, Dalton J. Cardiac acute care nurse practitioner and 30-day readmission. J Cardiovasc Nurs 2015; 30:248–255 [DOI] [PubMed] [Google Scholar]
- 28.Goldie CL, Prodan-Bhalla N, Mackay M. Nurse practitioners in postoperative cardiac surgery: Are they effective? Can J Cardiovasc Nurs 2012; 22:8–15 [PubMed] [Google Scholar]
- 29.Moran JL, Nakagawa K, Asai SM, et al. 24/7 Neurocritical care nurse practitioner coverage reduced door-to-needle time in stroke patients treated with tissue plasminogen activator. J Stroke Cerebrovasc Dis 2016; 25:1148–1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Young PJ, Bowling WM. Midlevel practitioners can safely place intracranial pressure monitors. J Trauma Acute Care Surg 2012; 73:431–434 [DOI] [PubMed] [Google Scholar]
- 31.Collins N, Miller R, Kapu A, et al. Outcomes of adding acute care nurse practitioners to a level I trauma service with the goal of decreased length of stay and improved physician and nursing satisfaction. J Trauma Acute Care Surg 2014; 76:353–357 [DOI] [PubMed] [Google Scholar]
- 32.Morris DS, Reilly P, Rohrbach J, et al. The influence of unit-based nurse practitioners on hospital outcomes and readmission rates for patients with trauma. J Trauma Acute Care Surg 2012; 73:474–478 [DOI] [PubMed] [Google Scholar]
- 33.Sherwood KL, Price RR, White TW, et al. A role in trauma care for advanced practice clinicians. JAAPA 2009; 22:33–36, 41 [DOI] [PubMed] [Google Scholar]
- 34.Matsushima K, Inaba K, Skiada D, et al. A high-volume trauma intensive care unit can be successfully staffed by advanced practitioners at night. J Crit Care 2016; 33:4–7 [DOI] [PubMed] [Google Scholar]
- 35.Hiza EA, Gottschalk MB, Umpierrez E, et al. Effect of a dedicated orthopaedic advanced practice provider in a level I trauma center: Analysis of length of stay and cost. J Orthop Trauma 2015; 29:e225–e230 [DOI] [PubMed] [Google Scholar]
- 36.Mains C, Scarborough K, Bar-Or R, et al. Staff commitment to trauma care improves mortality and length of stay at a level I trauma center. J Trauma 2009; 66:1315–1320 [DOI] [PubMed] [Google Scholar]
- 37.Gillard JN, Szoke A, Hoff WS, et al. Utilization of PAs and NPs at a level I trauma center: Effects on outcomes. JAAPA 2011; 20:34, 40–43 [DOI] [PubMed] [Google Scholar]
- 38.Sise CB, Sise MJ, Kelley DM, et al. Resource commitment to improve outcomes and increase value at a level I trauma center. J Trauma 2011; 70:560–568 [DOI] [PubMed] [Google Scholar]
- 39.Holliday A, Samanta D, Budinger J, et al. An outcome analysis of nurse practitioners in acute care trauma services. J Trauma Nurs 2017; 24:365–370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gilliland J, Donnellan A, Justice L, et al. Establishment of pediatric cardiac intensive care advanced practice provider services. World J Pediatr Congenit Heart Surg 2016; 7:72–80 [DOI] [PubMed] [Google Scholar]
- 41.Cramer CL, Orlowski JP, DeNicola LK. Pediatric intensivist extenders in the pediatric ICU. Pediatr Clin North Am 2008; 55:687–708, xixii [DOI] [PubMed] [Google Scholar]
- 42.Holleman J, Johnson A, Frim DM. The impact of a ‘resident replacement’ nurse practitioner on an Academic Pediatric Neurosurgical service. Pediatr Neurosurg 2010; 46:177–181 [DOI] [PubMed] [Google Scholar]
- 43.Hascall RL, Perkins RS, Kmiecik L, et al. PAs reduce rounding interruptions in the pediatric intensive care unit. JAAPA 2018; 31:41–45 [DOI] [PubMed] [Google Scholar]
- 44.Custer JW, White E, Fackler JC, et al. A qualitative study of expert and team cognition on complex patients in the pediatric intensive care unit. Pediatr Crit Care Med 2012; 13:278–284 [DOI] [PubMed] [Google Scholar]
- 45.Glotzbecker BE, Yolin-Raley DS, DeAngelo DJ, et al. Impact of physician assistants on the outcomes of patients with acute myelogenous leukemia receiving chemotherapy in an academic medical center. J Oncol Pract 2013; 9:e228–e233 [DOI] [PubMed] [Google Scholar]
- 46.D’Agostino R, Halpern NA. Acute care nurse practitioners in oncologic critical care: The memorial Sloan-Kettering cancer center experience. Crit Care Clin 2010; 26:207–217 [DOI] [PubMed] [Google Scholar]
- 47.Robles L, Slogoff M, Ladwig-Scott E, et al. The addition of a nurse practitioner to an inpatient surgical team results in improved use of resources. Surgery 2011; 150:711–717 [DOI] [PubMed] [Google Scholar]
- 48.Althausen PL, Shannon S, Owens B, et al. Impact of hospital-employed physician assistants on a level II community-based orthopaedic trauma system. J Orthop Trauma 2016; 30(Suppl 5):S40–S44 [DOI] [PubMed] [Google Scholar]
- 49.Craswell A, Dwyer T, Rossi D, et al. Cost-effectiveness of nurse practitioner-led regional titration service for heart failure patients. J Nurse Pract 2018; 14:105–111 [Google Scholar]
- 50.McLaughlin DC, Margretta MM, Freeman WD. Aneurysmal subarachnoid hemorrhage mortality after implementation of nocturnist advanced practice provider coverage. J Neurosci Nurs 2018; 50:102–104 [DOI] [PubMed] [Google Scholar]
- 51.O’Mahony S, Johnson TJ, Amer S, et al. Integration of palliative care advanced practice nurses into intensive care unit teams. Am J Hosp Palliat Care 2017; 34:330–334 [DOI] [PubMed] [Google Scholar]
- 52.Scherr K, Wilson DM, Wagner J, et al. Evaluating a new rapid response team: NP-led versus intensivist-led comparisons. AACN Adv Crit Care 2012; 23:32–42 [DOI] [PubMed] [Google Scholar]
- 53.Kapu AN, Wheeler AP, Lee B. Addition of acute care nurse practitioners to medical and surgical rapid response teams: A pilot project. Crit Care Nurse 2014; 34:51–59 [DOI] [PubMed] [Google Scholar]
- 54.Hellervik SM, Chassan CB, Landsperger JS, et al. Effect of adding an acute care nurse practitioner to a staff nurse led rapid response team (RRT) in a University Medical Center. Crit Care Med 2011; 39(Suppl 12):171 [Google Scholar]
- 55.Gershengorn HB, Xu Y, Chan CW, et al. The impact of adding a physician assistant to a critical care outreach team. PLoS One 2016; 11:e0167959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pirret AM. The role and effectiveness of a nurse practitioner led critical care outreach service. Intensive Crit Care Nurs 2008; 24:375–382 [DOI] [PubMed] [Google Scholar]
- 57.Alexandrou E, Murgo M, Calabria E, et al. Nurse-led central venous catheter insertion-procedural characteristics and outcomes of three intensive care based catheter placement services. Int J Nurs Stud 2012; 49:162–168 [DOI] [PubMed] [Google Scholar]
- 58.Jones SL, Ashton CM, Kiehne L, et al. Reductions in sepsis mortality and costs after design and implementation of a nurse-based early recognition and response program. Jt Comm J Qual Patient Saf 2015; 41:483–491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bevis LC, Berg-Copas GM, Thomas BW, et al. Outcomes of tube thoracostomies performed by advanced practice providers vs trauma surgeons. Am J Crit Care 2008; 17:357–363 [PubMed] [Google Scholar]
- 60.Kawar E, DiGiovine B. MICU care delivered by PAs versus residents: Do PAs measure up? JAAPA 2011; 24:36–41 [DOI] [PubMed] [Google Scholar]
- 61.Rayo MF, Mount-Campbell AF, O’Brien JM, et al. Interactive questioning in critical care during handovers: A transcript analysis of communication behaviours by physicians, nurses and nurse practitioners. BMJ Qual Saf 2014; 23:483–489 [DOI] [PubMed] [Google Scholar]
- 62.Sirleaf M, Jefferson B, Christmas AB, et al. Comparison of procedural complications between resident physicians and advanced clinical providers. J Trauma Acute Care Surg 2014; 77:143–147 [DOI] [PubMed] [Google Scholar]
- 63.Scherzer R, Dennis MP, Swan BA, et al. A comparison of usage and outcomes between nurse practitioner and resident-staffed medical ICUs. Crit Care Med 2017; 45:e132–e137 [DOI] [PubMed] [Google Scholar]
- 64.Gershengorn HB, Wunsch H, Wahab R, et al. Impact of nonphysician staffing on outcomes in a medical ICU. Chest 2011; 139:1347–1353 [DOI] [PubMed] [Google Scholar]
- 65.Gracias VH, Sicoutris CP, Stawicki SP, et al. Critical care nurse practitioners improve compliance with clinical practice guidelines in “semiclosed” surgical intensive care unit. J Nurs Care Qual 2008; 23:338–344 [DOI] [PubMed] [Google Scholar]
- 66.Tsai CL, Sullivan AF, Ginde AA, et al. Quality of emergency care provided by physician assistants and nurse practitioners in acute asthma. Am J Emerg Med 2010; 28:485–491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jefferson BK, King JE. Impact of the acute care nurse practitioner in reducing the number of unwarranted daily laboratory tests in the intensive care unit. J Am Assoc Nurse Pract 2018; 30:285–292 [DOI] [PubMed] [Google Scholar]
- 68.Butler KL, Calabrese R, Tandon M, et al. Optimizing advanced practitioner charge capture in high-acuity surgical intensive care units. Arch Surg 2011; 146:552–555 [DOI] [PubMed] [Google Scholar]
- 69.Gershengorn HB, Johnson MP, Factor P. The use of nonphysician providers in adult intensive care units. Am J Respir Crit Care Med 2012; 185:600–605 [DOI] [PubMed] [Google Scholar]
- 70.Alexandrou E, Spencer TR, Frost SA, et al. Central venous catheter placement by advanced practice nurses demonstrates low procedural complication and infection rates–a report from 13 years of service*. Crit Care Med 2014; 42:536–543 [DOI] [PubMed] [Google Scholar]
- 71.Costa DK, Wallace DJ, Barnato AE, et al. Nurse practitioner/physician assistant staffing and critical care mortality. Chest 2014; 146:1566–1573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Kapu AN, Kleinpell R, Pilon B. Quality and financial impact of adding nurse practitioners to inpatient care teams. J Nurs Adm 2014; 44:87–96 [DOI] [PubMed] [Google Scholar]
- 73.Kleinpell R, Ward NS, Kelso LA, et al. Provider to patient ratios for nurse practitioners and physician assistants in critical care units. Am J Crit Care 2015; 24:e16–e21 [DOI] [PubMed] [Google Scholar]
- 74.Skinner H, Skoyles J, Redfearn S, et al. Advanced care nurse practitioners can safely provide sole resident cover for level three patients: Impact on outcomes, cost and work patterns in a cardiac surgery programme. Eur J Cardiothorac Surg 2013; 43:19–22 [DOI] [PubMed] [Google Scholar]
- 75.Gokani VJ, Peckham-Cooper A, Bunting D, et al. Council of the Association of Surgeons in Training: The non-medical workforce and its role in surgical training: Consensus recommendations by the Association of Surgeons in Training. Int J Surg 2016; 36(Suppl 1):S14–S19 [DOI] [PubMed] [Google Scholar]
- 76.Kahn SA, Davis SA, Banes CT, et al. Impact of advanced practice providers (nurse practitioners and physician assistants) on surgical residents’ critical care experience. J Surg Res 2015; 199:7–12 [DOI] [PubMed] [Google Scholar]
- 77.Buch KE, Genovese MY, Conigliaro JL, et al. Non-physician practitioners’ overall enhancement to a surgical resident’s experience. J Surg Educ 2008; 65:50–53 [DOI] [PubMed] [Google Scholar]
- 78.Skinner H, Skoyles J, Redfeam S, et al. Resident cardiac ICU nurse practitioners make a non-resident junior doctor rotation feasible. Anaesthesia 2012; 67:3 [Google Scholar]
- 79.Lunn J, Sandor P, Lavender Z, et al. Nurses’ perception of resident and advanced practice provider critical care teams. Crit Care Med 2016; 44(12 Suppl 1):365 [Google Scholar]
- 80.Elliott DJ, Williams KD, Wu P, et al. An interdepartmental care model to expedite admission from the emergency department to the medical ICU. Jt Comm J Qual Patient Saf 2015; 41:542–549 [DOI] [PubMed] [Google Scholar]
- 81.Dalton MA. Perceptions of the advanced nurse practitioner role in a hospital setting. Br J Nurs 2013; 22:48–53 [DOI] [PubMed] [Google Scholar]
- 82.Alexandrov AW, Dusenbury W, Swatzell V, et al. Staffing the mobile stroke unit: Nurse practitioners measure up to physician-led care. Int J Stroke 2017; 12:2 [Google Scholar]
- 83.Roering L, Peterson M, Miran MS, et al. Reduced cost and decreased length of stay associated with acute ischemic stroke care provided by NPs: A single primary stroke center experience. Stroke 2017; 48(Suppl 1):AWP399 [Google Scholar]
- 84.Smith G, Waibel B, Evans P, et al. A recipe for success: Advanced Practice Professionals decrease trauma readmissions. Crit Care Med 2013; 41(12 Suppl 1):A149 [Google Scholar]


