Background:
Learning Health Systems strive to continuously integrate innovations and evidence-based practices (EBPs) into routine care settings. Few models provide a specified pathway to accelerate adoption and spread of EBPs across diverse settings.
Objective:
The US Department of Veterans Affairs Quality Enhancement Research Initiative (QUERI) Implementation Roadmap facilitates uptake of EBPs in routine practice by aligning research and health system priorities.
Methods:
The Roadmap is based on earlier iterations of the QUERI translational research pipeline, incorporating recent advancements in quality improvement and implementation science. Progressive, dynamic phases were operationalized to form an implementation process that promoted a participatory approach which enables stakeholders (health care consumers, clinicians, administrators, and leaders) to systematically plan, deploy, evaluate, and sustain EBPs using implementation strategies within a Learning Health System framework.
Results:
The Roadmap consists of Preimplementation, Implementation, and Sustainment phases. Preimplementation identifies a high-priority need, selects EBPs to address the need, engages stakeholders to build implementation capacity, specifies needed EBP adaptions and evaluation goals, and activates leadership support. During Implementation, clinical and research leaders use implementation strategies to promote EBP technical competency and adaptive skills to motivate providers to own and sustain EBPs. Sustainment includes evaluation analyses that establish the EBP business case, and hand-off to system leadership to own EBP implementation maintenance over time.
Conclusions:
The QUERI Implementation Roadmap systematically guides identification, implementation, and sustainment of EBPs, demystifying implementation science for stakeholders in a Learning Health System to ensure that EBPs are more rapidly implemented into practice to improve overall consumer health.
Key Words: implementation science, quality improvement, veteran health
The mission of the US Department of Veterans Affairs (VA) Quality Enhancement Research Initiative (QUERI) is to improve the health of the US military veterans by accelerating the adoption of evidence-based practices (EBPs) into routine health care settings.1 EBPs are clinical innovations, interventions, or programs derived from randomized controlled trials showing a positive impact on the quality, timeliness, and efficiency of care for patients (consumers). Research programs such as QUERI that are embedded in health system operations are especially valuable in promoting direct implementation of EBPs. This embedded research-operations model is essential to reduce the gap between research evidence and routine practice. Currently, <1 in 5 EBPs are adopted in routine health care settings,2 wasting millions of health care dollars that would otherwise benefit consumers.3 The reasons for this gap are well-documented and are mainly attributed to: failure to adapt EBPs to new populations without adequate input from stakeholders including frontline clinicians, administrators, and consumers; inadequate resources for frontline clinicians and administrators to implement EBPs effectively; and limited organizational strategies beyond health care leadership endorsement to integrate EBPs into routine care processes and workflows.4
Since its inception in 1998, QUERI has accelerated the implementation of EBPs into routine care settings through unique partnerships between research investigators and health system leaders.1,5,6 Established in 1998, QUERI supports investigators employed by the US Department of VA across over 40 centers in the United States to implement EBPs and evaluate the results of these efforts.5,6 QUERI has also led the development and application of implementation strategies, or theory-based methods designed to reduce barriers to EBP uptake in routine care.5–9 Over 70 implementation strategies have been identified8,9 with the most effective strategies including a combination of technical and adaptive skill application.10,11 Technical skills such as performance metrics, policies, and provider training “push” the EBP throughout the health system by supporting the capacity of frontline providers to deliver the EBP with quality and competence. Adaptive skills promote “pull,” or intrinsic motivation among frontline clinicians to use the EBP by enhancing their ownership of the local implementation process while ensuring their efforts remain strategically aligned with stakeholder priorities.12–14 QUERI-funded investigators employ a combination of technical and adaptive skills to scale-up and spread EBPs. As of mid-2019, QUERI centers have collectively implemented over 60 EBPs and trained over 3500 clinicians, directly serving close to 100,000 veterans across the United States.
To date there are no comprehensive, pragmatic approaches for researchers and health system leaders to apply implementation strategies to reduce barriers to EBP adoption. This is primarily due to limited awareness of their value and limited opportunities to evaluate them without access to multiple health care sites. The advent of the Learning Health System framework,15 which uses data and technology to identify gaps in quality and reduces care variation by deploying and monitoring improvement efforts over time, has led to the realization that specific implementation strategies are required to reduce barriers to EBP implementation. Traditional approaches to quality improvement, which are mainly derived from manufacturing processes,16 may be inadequate for implementing EBPs without implementation strategies that encourage multiple stakeholder buy-in to overcome barriers to EBP uptake.12–14
This paper describes the QUERI Implementation Roadmap, designed to support stakeholders (health care researchers, consumers, clinicians, administrators, and leaders) in systematically planning, deploying, and sustaining EBPs in routine health care settings. The Roadmap pays particular attention to pragmatic approaches for frontline clinicians and administrators to overcome barriers through implementation strategies.
METHODS—ROADMAP DEVELOPMENT
The Roadmap was commissioned by QUERI leadership to extend the previous “pipeline” framework for implementation that reflected a traditional, linear research process.17 It originated from an increased demand in health systems to have a more user-friendly approach for planning implementation of EBPs in routine care, especially for frontline clinicians and administrators.6 The Roadmap is based on a review of current implementation and quality improvement frameworks described below, a recent evidence review of implementation strategies used in real-world health systems to improve adoption of EBPs,18 and the experience of the 15 QUERI programs.6 Overarching observations from these resources were summarized by the QUERI Center for Evaluation and Implementation Resources (CEIR) to form the QUERI Implementation Roadmap. The Roadmap incorporates 3 key lessons from QUERI’s experience in implementation of EBPs. First, implementation is a dynamic process that incorporates multiple stakeholder input in the process of identifying, implementing, and sustaining EBPs. Second, EBP uptake requires ongoing implementation strategies that motivate and empower frontline providers and administrators. Third, the Roadmap assumes that implementation is an iterative process, whereby new questions are generated over time.
QUERI ROADMAP OVERVIEW
The Roadmap is comprised of 3 phases: Preimplementation, Implementation, and Sustainment. Figure 1 depicts the overarching questions/issues facing each phase. These phases and functions map onto the Learning Health Systems framework’s 3-part cycle of integrating data and new evidence into practice of: (1) data to knowledge; (2) knowledge to performance; and (3) performance to data.19 Each phase of the implementation process requires active participation of stakeholders including consumers, frontline clinicians, health care administrators, and leaders/policymakers. During Preimplementation (Fig. 1), health care leaders endorse system-wide priorities that are identified across stakeholders, and secure institutional commitment to apply EBPs to address these priorities. Throughout Implementation, knowledge is put into action by using implementation strategies to support the scale-up and spread of EBPs, and metrics of success are chosen based on clinical benchmarks relevant to the health care setting and stakeholders. Consumers and frontline clinicians are essential to ensuring that the implementation strategies fit within local contexts. In the Sustainability phase, the impact of EBP uptake is demonstrated with regard to benefit to stakeholders and steps are taken to transition the EBP to leadership for ongoing maintenance. Efforts to evaluate and sustain EBPs can also lead to new questions and discovery of knowledge related to performance gaps in an iterative cycle of continuous improvement through implementation and spread.
FIGURE 1.
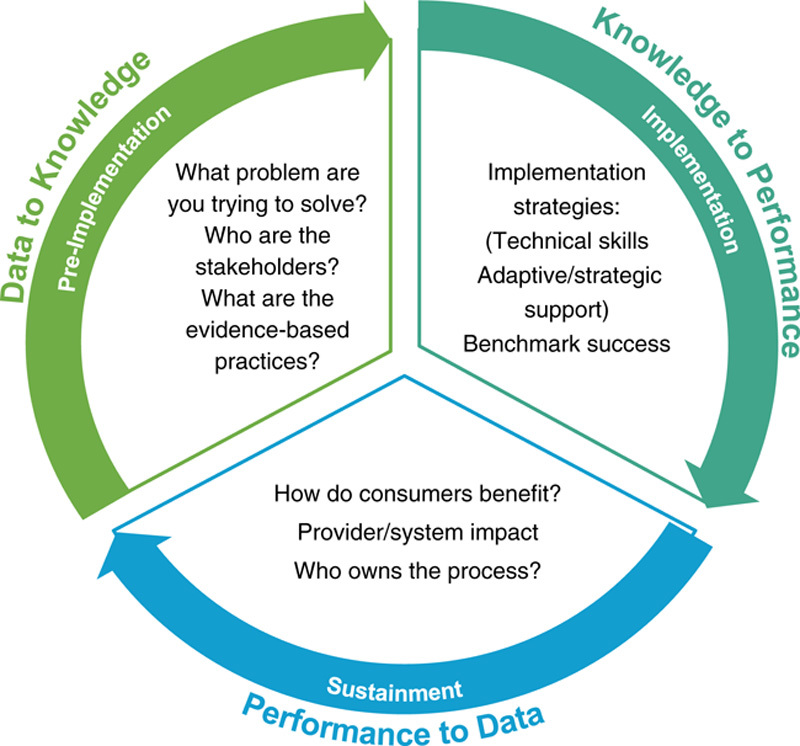
Quality Enhancement Research Initiative Implementation Roadmap.
ROADMAP THEORETICAL ORIGINS
In addition to the Learning Health System framework,19 the Roadmap is based on previously established implementation theories that describe an iterative, multiphased process to adapt and adopt EBPs. The Roadmap reflects the concepts from the Interactive Systems Framework for dissemination and implementation,20 which emphasizes processes that accelerate the integration of EBPs into routine care through interactive and supportive strategies among frontline clinicians and employees. Roadmap components are also based on implementation process frameworks such as Replicating Effective Programs,21 the Dynamic Adaptation Process,22 and Interventional Mapping.23 These frameworks describe systematic approaches to planning, packaging, deploying, and rigorously evaluating effective innovations with stakeholder input to ensure their sustained use over time. They also emphasize methods to maintain fidelity to core EBP components while allowing for provider-driven adaptations that allow for variation in resource constraints and capabilities across sites and settings. The Roadmap also incorporates concepts from the Evidence-based System for Innovation Support framework,20,24 which recommends tailoring implementation strategies5,7,8 to local contextual factors that build local stakeholder capacity to deliver EBPs effectively.
ROADMAP ADDRESSES BARRIERS TO IMPLEMENTATION
A core function of the Roadmap is to support the deployment of the implementation strategies that target multilevel contextual factors that may act as facilitators or barriers to EBP uptake. Several implementation frameworks25 can be used to help identify barriers to EBP uptake.22,24,25 The Theoretical Domains Framework26 focuses on provider-level behavioral barriers to EBP adoption. The Consolidated Framework for Implementation Research27 identifies implementation barriers and facilitators across 5 domains: characteristics of the EBP, inner setting of the implementing organization, factors outside the implementing organization, individuals involved in the implementation effort, and the process of implementation itself.
INCORPORATING USER-CENTERED DESIGN, DEIMPLEMENTATION, AND EBP ADAPTATION
The Roadmap is also based on emerging implementation practices such as user-centered design,28 which enable consumers and frontline clinicians to own the EBP implementation process by adapting EBPs to local contexts.21,24,29,30 Given the increased demands on clinicians to implement more EBPs, the Roadmap also considers deimplementation of low-value care as an important implementation strategy to consider. Deimplementation represents a situation when an established practice should be reduced and stopped because it is ineffective, harmful, inefficient, or no longer necessary even in the absence of a specific superior alternative practice.31 The Roadmap also assumes that the adaption of EBPs and implementation strategies should happen routinely given different contextual factors. Key frameworks that inform adaptation processes for both EBPs and their implementation strategies include the Dynamic Adaption Process,22 Dynamic Sustainability,29 Intervention Mapping,23 and the Wiltsey-Stirman frameworks.32
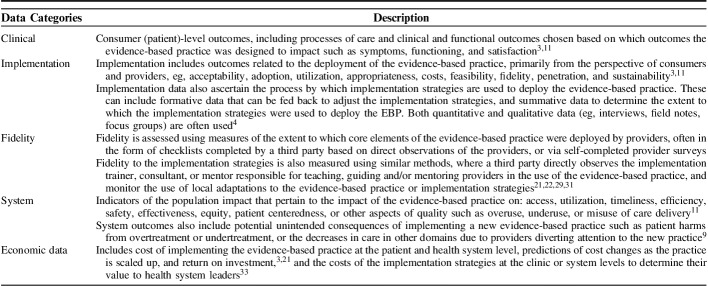
ROADMAP: CONTINUOUS IMPLEMENTATION EVALUATION
The Roadmap also supports demonstrable improvements in clinical outcomes based on a continuous evaluation of the implementation process using common measures3,32 (Table 1). The key frameworks for identifying measures of implementation success at a population-level impact include RE-AIM (Reach, Effectiveness, Implementation, Adoption, and Sustainability)34 and COINS (Cost of Implementing New Strategies).33 A business case analysis is also recommended for implementation,35 which determines the overall impact of the implementation process on the health care setting. A business case analysis focuses on perspectives across multiple stakeholders (eg, provider turnover, consumer satisfaction, in addition to health care costs), which can facilitate ownership for EBP implementation maintenance by health system leaders or policymakers over time.
TABLE 1.
Categories of Common Implementation Benchmarks and Data
QUERI ROADMAP COMPONENTS
Each phase (Preimplementation, Implementation, and Sustainment) of the Roadmap is detailed in Figure 2. Each phase is organized around 3 questions regarding activities necessary to: (1) support uptake of the EBP; (2) activate stakeholders and delivery capability; and (3) optimize the use of data and measures to assess progress. Each phase is linked by iterative cycles of experimentation and refinement consistent with rapid-cycle testing.9,13,32 A use case for how each Roadmap phase was operationalized is also provided below, based on the QUERI-Veterans Integrated Service Networks (VISN, the regional health care systems within the VA) Partnered Implementation Initiatives.
FIGURE 2.
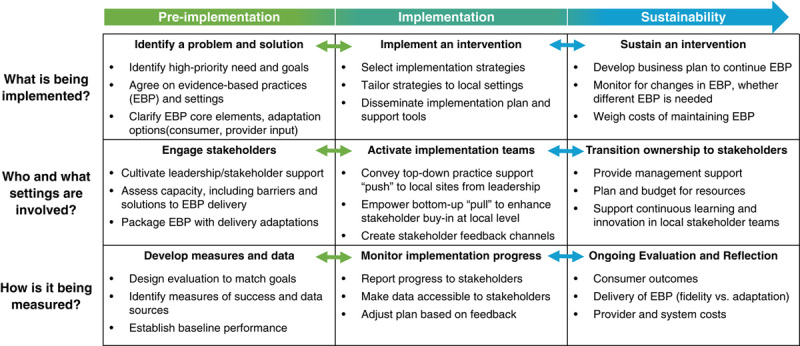
Quality Enhancement Research Initiative Implementation Roadmap Components.
PREIMPLEMENTATION
Preimplementation18 focuses on the problem to be solved, identifies stakeholders who will select and prepare EBPs for deployment, and establishes measures to assess success. In this phase, consensus is reached among leaders, clinicians, and consumers regarding the clinical priority area and goals (metrics) for improvement and an EBP is identified (solution) to address this quality gap.9,21 In identifying a high-priority need, the clinical problem should be clearly defined, and measures of success aligned with existing performance goals within the organization’s mission.13,23,24,27,36
When selecting EBPs, it is important to conduct an evidence review of relevant clinical trials, including the clinical settings of the studies. In almost all cases, EBPs will need to be adapted to the health system’s population and settings.21,22,29,31 It may also be helpful to assess capacity to implement EBPs20–22,24,31 at the consumer (eg, age, medical complexity); provider/staff (eg, skills, knowledge, attitudes, and provider mix); organization (leadership, culture, space, and resources); and health system levels (eg, policies, funding).22,37 Practice fidelity and adaptability concerns need to be balanced to respond to these unique multilevel contextual factors.22,29
Preimplementation also includes the development of EBP toolkits or resources to address implementation barriers and facilitators, and frontline clinicians are often the best source for this information. Toolkits specify the EBP core elements, which are the components of the intervention that achieve its desired effects on outcomes. They also specify the process by which clinicians are trained to use the EBP, common barriers to implementation and how to overcome them, and opportunities to adapt the EBPs without compromising the EBP’s core elements.29,32 The toolkits also include measures of success to demonstrate EBP impact (Table 1).
Finally, during preimplementation, it is vital for stakeholders to establish open lines of communication related to the implementation process38 and have a shared understanding of the populations affected, implementation plan, resources required, and persons who will “own” implementation efforts over time.21,38,39
PREIMPLEMENTATION EXAMPLE: EMBEDDED FUNDING OPPORTUNITY
In 2018, QUERI established a VA funding mechanism (Partnered Implementation Initiative) based on the Roadmap to support implementation projects embedded within the health system that are co-led by implementation scientists and health system leaders, to scale-up and spread effective practices addressing clinical priorities. Regional VA health system (VISN) leaders were very receptive to this initiative because they were able to choose the clinical priorities collectively. Moreover, it enabled more rapid buy-in because the goal of the initiative was to promote direct implementation EBPs to improve clinical performance.
In November 2017, regional health system leadership teams, including the VISN Director, their Chief Medical Officers, Quality Management Officers, and local facility leaders within the region were asked to submit nominations for clinical priorities which could benefit from additional implementation support. During a live voting session, regional health system leaders selected 3 priorities from a list of the top 10 nominations as targets for enhanced implementation support. The priorities chosen were access to medication-assisted treatment (MAT) for opioid use disorder treatment, implementation of suicide prevention services, and effective care coordination models for community care. In addition, regional health system leaders indicated a preference to select which of the 3 priorities they would like implementation teams to focus on for their region.
Subsequently, QUERI requested applications for the Partnered Implementation Initiative from implementation scientist-health system leadership teams. The application had to describe how the team would implement EBPs to address the regional health system’s selected clinical priority using implementation strategies, and the national quality measures for which they would benchmark success. Applications were rigorously peer reviewed by content experts. Seven implementation teams from 6 regional health systems were funded in 2018–2019, focusing on opioid use disorder/pain treatment and suicide prevention.
Overall, selection of clinical priority areas by VISN leadership encouraged local ownership of the initiative while allowing for a collective understanding of common national clinical priorities. Measures of implementation success were directly derived from the regional leaders’ performance plan criteria (eg, number of patients with opioid use disorder receiving MAT). This enabled regional leaders and investigators to have a shared understanding of the problem and work together to deploy implementation strategies to scale-up and spread the EBPs at sites with the most significant gaps in quality based on VHA performance metrics. The Partnered Implementation Initiatives also benefited from national VA leadership endorsement of the EBPs, including provider training and technical support in using the EBPs.
IMPLEMENTATION
A core component of the Implementation phase is the selection and deployment of an implementation plan that applies implementation strategies to enhance EBP uptake. There has been limited guidance on how to systematically match barriers and facilitators with these strategies to optimize EBP uptake.40 However, recent research has proposed methods to select and tailor implementation strategies,18,31,40 and that a combination of strategies that use technical (transactional) and adaptive (transformational) leadership skills is ideal for addressing organizational barriers.31,41,42 Described by Avolio et al,43 transactional skills develop delivery capacity44 by aligning EBP implementation with organizational performance metrics and by adjusting implementation strategies to improve performance. Transactional strategies typically involve methods such as EBP tools/toolkits development, provider training, technical assistance, provider incentives, or audit and feedback20,24 so that clinicians are encouraged to meet performance targets.45 Adaptive, or transformative, leadership skills are instrumental in bringing stakeholders together via a shared vision to implement the EBP and help engage frontline clinicians in owning the EBP implementation process (via “pull” motivators to change). Transformational strategies include skill development to encourage innovation and fostering ownership among frontline clinicians in the process of implementing EBPs.13,45,46
Ultimately, implementation plans should include operationally defined implementation strategies, identification of persons who will deploy the strategies (and mentor other clinicians in implementation of the EBP), development of a guide for using the strategies, and operationalization of measures to benchmark success which can be fed back to operations leaders and frontline clinicians to adjust implementation as necessary.41,47
IMPLEMENTATION USE CASE
For the QUERI-VISN Partnered Implementation Initiatives that focused on opioid use disorder, the primary implementation strategy chosen to scale-up and spread EBP delivery was Facilitation. Developed by QUERI investigators, Facilitation was selected for the Partnered Implementation Initiatives in partnership with national VA leadership. Facilitation helps providers improve the uptake of effective practices by teaching them strategic thinking skills to overcome organizational barriers.42,48 Selection of a common implementation strategy across the Partnered Implementation Initiatives programs that was endorsed by national VA leadership enabled the opioid use disorder teams to use a learning collaborative to share information, including common implementation approaches and outcome measures. Facilitation was also selected due to its flexibility in promoting EBP adoption across multiple care settings (eg, inpatient, outpatient, telehealth).48
Facilitation for MAT was deployed with QUERI support after the VA national program office responsible for the EBP disseminated a toolkit and training program in the EBP. Providers were selected by each VISN to receive the EBP toolkit on opioid stepped care and MAT and to attend a national training on EBP opioid stepped care. The toolkit included tools designed to allow frontline stakeholders to plan and implement MAT (eg, suboxone), the training content, and measures of success including number of eligible consumers receiving MAT.24 QUERI also provided supplemental support to the Partnered Implementation Initiatives to hire Facilitators to work with the VA national program office responsible for MAT national policy, to help consult frontline clinicians in the implementation of MAT prescribing in sites in need of additional support.
SUSTAINMENT
Sustainment (performance to data18) includes an assessment of the performance of the EBP, the decision of whether the EBP will be sustained over time, and the creation of a plan to support ongoing EBP delivery. This phase also involves identification of an EBP maintenance “owner” once external funding for implementation ends.41 Sustainment includes continuous monitoring of EBP fidelity, quality, outcomes, system impacts, and return-on-investment (eg, how much will it cost to maintain implementation over time per site) of the EBP over time. The goal of this phase is for the EBP to be maintained internally without the need for external support or management. For the EBP to be sustained, leaders should be provided with guidance for how to encourage EBP sustainability, including program monitoring and resourcing, independent of outside support.
SUSTAINMENT USE CASE
To promote sustainment across the QUERI VISN Partnered Implementation Initiatives, the QUERI CEIR established the learning collaborative to facilitate the sharing of implementation best practices and the discussion of shared process and outcomes metrics. This collaborative supported the development of a regional health system consortium focused on opioid/pain stepped care. Further, CEIR established an evaluation toolkit and program evaluation training resource which include information on joint expectations among the Partnered Implementation Initiative stakeholders and clarifies key roles, responsibility, timelines shared resources, deliverables, and preferences for ongoing communications and products within the PII teams. Finally, the QUERI VISN Partnered Implementation Initiative required common benchmarks to assess ongoing implementation, including those derived from VA national performance metrics, to allow leaders to see the added benefit of implementing the EBP in their regions and conduct a business case analysis.
Other health systems can apply common elements of the QUERI-VISN Partnered Implementation Initiative approach which seek to leverage multilevel partnerships to tailor clinical practices and implementation approaches to meet regional needs while aligning with national priorities. Notably, it was helpful to have an internal funding program (QUERI) support request for applications and engage the regional health system leaders by having them proactively identify and select clinical priorities to focus funding efforts. Second, the requirement that the Partnered Implementation Initiatives be co-led by a health system leader and implementation scientist ensured that the project goals were aligned with local stakeholder needs. It also ensured that the implementation methods were demystified and practical for the regional health systems to deploy and that implementation efforts focused on nationally endorsed performance plan measures to which the health system was accountable. Third, having a central resource center (CEIR) provide implementation and evaluation consultation throughout the Initiative ensured a sound business case for the implementation plan and hand-off to leadership. Finally, having the national health system endorse both the use of the EBPs and the implementation strategies (Facilitation) ensured ongoing ownership.
CONCLUSIONS
The QUERI Implementation Roadmap provides the implementation guidance beyond traditional research-to-practice frameworks by emphasizing collaboration and alignment of leadership support with frontline employee engagement and consumer needs. The Roadmap also enhances the evolution of the Learning Health System by providing a guide for ongoing deployment and evaluation of implementation strategies to scale-up, spread, and ultimately sustain EBPs in routine care. Implementation strategies that focus on engaging frontline clinicians are vital to implementation success because top-down directives, training, or performance metrics alone are insufficient to change clinical practice. The Roadmap provides a process to support EBP implementation which involves both top-down and bottom-up implementation strategies, and modification of interventions and assessment to meet clinical priorities, and evaluation of the business case for EBP sustainment based on multiple stakeholder input. These are all essential components of an effective practice spread plan but are rarely presented together or within a unifying framework.
The Roadmap is also a practical tool for other large health systems that face challenges in implementing and sustaining EBPs. Specifically, the key lessons learned from the QUERI-VISN Partnered Implementation Initiative were integrated into this Roadmap and are applicable to other health systems. First, it is vital to specify expectations from health system leaders in terms of resources, support, and measures of success, especially for long-term maintenance of the EBP. In support of the Partnered Implementation Initiatives, the VA national program office responsible for substance use treatment made opioid stepped care a clinical priority and rolled out a toolkit before the Partnered Implementation Initiatives were launched. Second, regional leaders interested in implementing EBPs should ensure a process to garner buy-in from their frontline clinicians, especially through their administrators (middle managers) so that the EBP is viewed as acceptable and feasible at the clinic level.49 National VA leadership asked each regional health system to send clinicians to be trained in the EBP which helped to garner frontline buy-in. Finally, the evaluation of EBP implementation should include the estimated costs of maintaining implementation support, including provider training, toolkit updating, technical assistance, and where necessary, consultation (eg, Facilitation) to promote adaptive skills to ensure leaders provide adequate support to its sustainability.
Over time the QUERI Implementation Roadmap will be enhanced by further research on the use of implementation strategies to improve uptake of EBPs and care quality. Much of the research on implementation strategies to inform Roadmap components is emerging within VA’s Health Services Research and Development Program, and other federal funding agencies such as the Agency for Health Care Research and Quality, the Patient Centered Outcomes Research Initiative, and increasingly, health systems themselves. Like other implementation frameworks, further work will be needed to better specify each phase and to develop common metrics of contextual factors, uptake, and outcomes where appropriate.50
Overall, the QUERI Implementation Roadmap is a practical, user-friendly guide for frontline clinicians, administrators, consumers, and researchers to plan out EBP implementation approaches. It serves to demystify implementation science for these stakeholders by outlining the specific steps to drive development and execution of an implementation spread plan which is informed by the unique characteristics of the problem, the stakeholders, and the priorities of the health care setting in which the practice is to be implemented. Currently VA leaders have sought out QUERI training implementation strategies based on the Roadmap, and more health system leaders have invested in QUERI implementation strategies such as Facilitation and Evidence-based Quality Improvement6 as tools to scale-up and spread their practices and policies nationally. The QUERI Implementation Roadmap systematically guides identification, implementation, and sustainment of EBPs to ultimately improve overall quality of care for consumers.
Footnotes
Supported by the US Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development Service. The views expressed are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs of the US Government.
The authors declare no conflict of interest.
REFERENCES
- 1.Rubenstein LV, Mittman BS, Yano EM, et al. From understanding health care provider behavior to improving health care: the QUERI framework for quality improvement. Quality Enhancement Research Initiative. Med Care. 2000;38:I129–I141. [PubMed] [Google Scholar]
- 2.Chalmers I, Glasziou P. Avoidable waste in the production and reporting of research evidence. Lancet. 2009;374:86–89. [DOI] [PubMed] [Google Scholar]
- 3.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38:65–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauer MS, Damschroder L, Hagedorn H, et al. An introduction to implementation science for the non-specialist. BMC Psychol. 2015;3:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kilbourne AM, Elwy AR, Sales AE, et al. Accelerating research impact in a learning health care system: VA’s quality enhancement research initiative in the choice act era. Med Care. 2017;55(suppl 7 suppl 1):S4–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Atkins D, Kilbourne AM, Shulkin D. Moving from discovery to system-wide change: the role of research in a learning health care system: experience from three decades of health systems research in the veterans health administration. Annu Rev Public Health. 2017;38:467–487. [DOI] [PubMed] [Google Scholar]
- 7.Solberg L. Lessons for non-VA care delivery systems from the US Department of Veterans Affairs Quality Enhancement Research Initiative: QUERI Series. Implement Sci. 2009;4:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Langley GJ, Moen RD, Nolan KM, et al. The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. San Francisco, CA: Jossey-Bass; 2009. [Google Scholar]
- 10.Rogal SS, Yakovchenko V, Waltz TJ, et al. The association between implementation strategy use and the uptake of hepatitis C treatment in a national sample. Implement Sci. 2017;12:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Proctor EK, Landsverk J, Aarons G, et al. Implementation research in mental health services: an emerging science with conceptual, methodological, and training challenges. Adm Policy Ment Health. 2009;36:24–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parker LE, de Pillis E, Altschuler A, et al. Balancing participation and expertise: a comparison of locally and centrally managed health care quality improvement within primary care practices. Qual Health Res. 2007;17:1268–1279. [DOI] [PubMed] [Google Scholar]
- 13.Edmondson AC. The competitive imperative of learning. Harv Bus Rev. 2008;86:160. [PubMed] [Google Scholar]
- 14.Aarons GA, Ehrhart MG, Farahnak LR, et al. Aligning leadership across systems and organizations to develop a strategic climate for evidence-based practice implementation. Annu Rev Public Health. 2014;35:255–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America. Washington, DC: The National Academies Press; 2013. [PubMed] [Google Scholar]
- 16.Koczwara B, Stover AM, Davies L, et al. Harnessing the synergy between improvement science and implementation science in cancer: a call to action. J Oncol Pract. 2018;14:335–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stetler CB, McQueen L, Demakis J, et al. An organizational framework and strategic implementation for system-level change to enhance research-based practice: QUERI Series. Implement Sci. 2008;3:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miake-Lye IM, Mak SS, Lambert-Kerzner AC, et al. Scaling Beyond Early Adopters: A Systematic Review and Key Informant Perspectives VA ESP Project #05-226. Washington, DC: US Department of Veterans Affairs; 2019. [PubMed] [Google Scholar]
- 19.Guise JM, Savitz LA, Friedman CP. Mind the gap: putting evidence into practice in the era of learning health systems. J Gen Intern Med. 2018;33:2237–2239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wandersman A, Chien VH, Katz J. Toward an evidence-based system for innovation support for implementing innovations with quality: tools, training, technical assistance, and quality assurance/quality improvement. Am J Community Psychol. 2012;50:445–459. [DOI] [PubMed] [Google Scholar]
- 21.Kilbourne AM, Neumann MS, Pincus HA, et al. Implementing evidence-based interventions in health care: application of the replicating effective programs framework. Implement Sci. 2007;2:42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aarons GA, Green AE, Palinkas LA, et al. Dynamic adaptation process to implement an evidence-based child maltreatment intervention. Implement Sci. 2012;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bartholomew-Eldredge LK, Markham CM, Ruiter RAC, et al. Planning Health Promotion Programs: An Intervention Mapping Approach. San Francisco, CA: Jossey-Bass; 2016. [Google Scholar]
- 24.Leeman J, Calancie L, Hartman MA, et al. What strategies are used to build practitioners’ capacity to implement community-based interventions and are they effective? A systematic review. Implement Sci. 2015;10:80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nilsen P. Making sense of implementation theories, models and frameworks. Implement Sci. 2015;10:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Atkins L, Francis J, Islam R, et al. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci. 2017;12:77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Damschroder LJ, Aron DC, Keith RE, et al. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lyon AR, Koerner K. User-centered design for psychosocial intervention development and implementation. Clin Psychol. 2016;23:180–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci. 2013;8:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Leeman J, Calancie L, Kegler MC, et al. Developing theory to guide building practitioners’ capacity to implement evidence-based interventions. Health Educ Behav. 2017;44:59–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wang V, Maciejewski ML, Helfrich CD, et al. Working smarter not harder: coupling implementation to de-implementation. Healthcare. 2017;6:104–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stirman SW, Miller CJ, Toder K, et al. Development of a framework and coding system for modifications and adaptations of evidence-based interventions. Implement Sci. 2013;8:65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saldana L, Chamberlain P, Bradford WD, et al. The cost of implementing new strategies (coins): a method for mapping implementation resources using the stages of implementation completion. Child Youth Serv Rev. 2014;39:177–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Glasgow RE, McKay HG, Piette JD, et al. The RE-AIM framework for evaluating interventions: what can it tell us about approaches to chronic illness management? Patient Educ Couns. 2001;44:119–127. [DOI] [PubMed] [Google Scholar]
- 35.Leatherman S, Berwick D, Iles D, et al. The business case for quality: case studies and an analysis. Health Aff (Millwood). 2003;22:17–30. [DOI] [PubMed] [Google Scholar]
- 36.Sullivan JL, Adjognon OL, Engle RL, et al. Identifying and overcoming implementation challenges: Experience of 59 noninstitutional long-term services and support pilot programs in the Veterans Health Administration. Health Care Manage Rev. 2018;43:193–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Flaspohler P, Duffy J, Wandersman A, et al. Unpacking prevention capacity: an intersection of research-to-practice models and community-centered models. Am J Community Psychol. 2008;41:182–196. [DOI] [PubMed] [Google Scholar]
- 38.Midboe AM, Elwy AR, Durfee JM, et al. Building strong research partnerships between public health and researchers: a VA case study. J Gen Intern Med. 2014;29(suppl 4):831–834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bergman AA, Delevan DM, Miake-Lye IM, et al. Partnering to improve care: the case of the Veterans’ Health Administration’s Quality Enhancement Research Initiative. J Health Serv Res Policy. 2017;1:1355819617693871. [DOI] [PubMed] [Google Scholar]
- 40.Powell BJ, Beidas RS, Lewis CC, et al. Methods to improve the selection and tailoring of implementation strategies. J Behav Health Serv Res. 2017;44:177–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Leeman J, Birken SA, Powell BJ, et al. Beyond “implementation strategies”: classifying the full range of strategies used in implementation science and practice. Implement Sci. 2017;12:125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ritchie MJ, Dollar KM, Miller CJ, et al. Implementation Facilitation Training Manual: Using Implementation Faciliation to Improve Care in the Veterans Health Administration (Version 2). 2017. Available at: www.queri.research.va.gov/tools/implementation/Facilitation-Manual.pdf. Accessed January 1, 2019.
- 43.Avolio BJ, Bass BM. The Full Range of Leadership Development. Binghamton, NY: Bass, Avolio & Associates; 1991. [Google Scholar]
- 44.Rodgers E. Diffusion of Innovations. New York: Free Press; 2003. [Google Scholar]
- 45.Aarons GA. Transformational and transactional leadership: association with attitudes toward evidence-based practice. Psychiatr Serv. 2006;57:1162–1169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Bass BM, Avolio BJ. Improving Organizational Effectiveness Through Transformational Leadership. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 47.Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kirchner JE, Ritchie MJ, Pitcock JA, et al. Outcomes of a partnered facilitation strategy to implement primary care-mental health. J Gen Intern Med. 2014;22:139–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Birken S, Clary A, Tabriz AA, et al. Middle managers’ role in implementing evidence-based practices in healthcare: a systematic review. Implement Sci. 2018;13:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Moullin JC, Dickson KS, Stadnick NA, et al. Systematic review of the Exploration, Preparation, Implementation, Sustainment (EPIS) framework. Implement Sci. 2019;14:1. [DOI] [PMC free article] [PubMed] [Google Scholar]